Abstract
Cancer Stem Cells (CSCs) are self-renewing cancer cells responsible for expansion of the malignant mass in a dynamic process shaping the tumor microenvironment. CSCs may hijack the host immune surveillance resulting in typically aggressive tumors with poor prognosis.
In this review, we focus on neurotrophic control of cellular substrates and molecular mechanisms involved in CSC-driven tumor growth as well as in host immune surveillance. Neurotrophins have been demonstrated to be key tumor promoting signaling platforms. Particularly, Nerve Growth Factor (NGF) and its specific receptor Tropomyosin related kinase A (TrkA) have been implicated in initiation and progression of many aggressive cancers. On the other hand, an active NGF pathway has been recently proven to be critical to oncogenic inflammation control and in promoting immune response against cancer, pinpointing possible pro-tumoral effects of NGF/TrkA-inhibitory therapy.
A better understanding of the molecular mechanisms involved in the control of tumor growth/immunoediting is essential to identify new predictive and prognostic intervention and to design more effective therapies. Fine and timely modulation of CSCs-driven tumor growth and of peripheral lymph nodes activation by the immune system will possibly open the way to precision medicine in neurotrophic therapy and improve patient’s prognosis in both TrkA- dependent and independent cancers.
Keywords: cancer stem cells, NGF, immunesurveillance, tumor microenvironment, cancer innervation
Introduction
Cancer stem cells niche
Tumor tissues consist of heterogeneous cancer cells, including stem-cell-like subsets of cancer stem cells (CSCs), characterized by self-renewal and long-term clonal maintenance [1]. Thus, CSCs are not only responsible for initiating the tumor process, but they have long-term repopulation capacity in recurrent tumors. Also, CSCs show significant DNA repair capability and resistance to current chemo, radio, and immune therapies [2].
Based on the revised CSCs model, several genetically different subclones of CSCs may co-exist and expand according to their own hierarchy within the tumor bulk, and contribute to overall cancer heterogeneity [3]. The first evidence for CSCs came from the observation of a small subset of clonogenic cancer cells in acute myeloblastic leukaemia (AML) [4]. CSCs were subsequently identified in other tumor types, including multiple myeloma, breast, brain, prostate, and lung cancers. CSCs are tumorigenic even when transplanted in low numbers in experimental models [5,6]. They carry the neural stem cells marker CD133, which was identified first in human brain tumors, and then in many other solid tumors, like prostate, colon, and pancreas tumors [7].
Tumor aggressiveness is strictly linked to a process known as Epithelial-Mesenchymal Transition (EMT). Subpopulations of tumor cells that undergo EMT [8] induce apoptosis of neighboring non-cancerogenic endothelial cells [9] and disrupt epithelial junctions, becoming metastatic as Circulating Tumor Cells (CTCs). Above described events have been found to be common in distinct types of carcinoma, like head and neck cancer, esophageal cancer, breast cancer, lung cancer and melanoma.
In hematological malignancies the disease reinitiates from microscopic residual tumor, known as minimal residual disease (MRD), routinely analyzed through a technique called “liquid biopsy” [10]. Maintenance of undifferentiated and self-renewing CSCs relies on the “stem cell niche”, a microenvironment mainly represented by dendritic cells (DCs), tumor associated macrophages (TAMs), fibroblasts, tumor-specific T cells, and neutrophils [11,12]. The niche is enriched in factors promoting CSCs self-renewal, angiogenesis, tumor invasion and metastasis, as reviewed in [13,14]. To avoid tumor relapse and improve patient prognosis, several molecular targets and biomarkers have been suggested. The nuclear factor-kB (NF-kB), Notch, and phosphatidylinositol 3-kinase/AKT/mammalian Target of Rapamycin (PI3K/AKT/mTOR) pathways are the most relevant signaling platforms targeted for their involvement in CSCs metabolism, survival, proliferation, growth, invasion, and resistance to therapy [15,16]. Notch pathway is also involved in the immune surveillance process, promotes M1 macrophage polarization [17] and CD8+ T cells activation, and acts as a tumor-suppressor [18]. Furthermore, activation of the Interleukin-6 (IL-6)/ Signal transducer and activator of transcription 3 (STAT3)/Aldehyde Dehydrogenase 1 (ALDH1) pathway by adipose tissue-derived vesicles, cytokines, and circulating factors has been recently implicated in tumor stemness and aggressiveness, particularly in breast cancer [19–21].
Several inhibitors preferentially targeting CSCs have been tested in vitro and in preclinical studies, like the pan-PI3K inhibitor B591 [22] and the dual PI3K/mTOR inhibitor VS-5584 [23]. However, novel therapies are still demanding, because of the limited efficacy and side effects of currently available CSCs-based targeting approaches.
Nowadays, immunotherapy represents the latest frontier of CSCs-based cancer therapy due to its broader range application over different cancer types. Here below, we will focus on the role of immune system attempted control against cancer growth and spreading, highlighting the double-edged sword of neurotrophins in cancer immunity and inflammation, of interest for the design of novel and efficient therapies targeting CSCs-driven tumors and metastasis.
CSCs and tumor immune surveillance
The immune surveillance hypothesis
The immune surveillance hypothesis states that the immune control of cellular homeostasis is the first line of host defense against carcinogenesis. The host immune system-tumor interplay consists of three essential phases: elimination, equilibrium and escape (reviewed in [24,25]).
Elimination. Exposure of immunogenic antigens by mutated or dying cells activates Natural Killer (NK) receptors NKGD and promotes proliferation of infiltrating CD8+ T cells by induction of major histocompatibility complex (MHC) class Ia, resulting in their clearance. In particular, a subset of high Interferon -γ (IFN-γ) secreting NK cells is at the forefront of innate response against cancer and it is responsible for Tumor Necrosis Factor (TNF)-related apoptosis-inducing ligand (TRAIL)-dependent lysis of tumor cells in mice [26]. Stress or necrosis induced signals, like Danger Associated Molecular Patterns (DAMP), are crucial for stimulating Pattern recognition receptor (PRR), like Toll-like receptor (TLR) and Nod-like receptor (NLR), elective effectors of innate immunity. Equilibrium. Premalignant stem cells are maintained in equilibrium with the adaptive immune response, which selects low-dividing and immune tolerant emerging subclones in a process called immunoediting Tumor stem cells are still dependent upon their niche and cancer metastasis is unlike to occur. Escape. The immune escape mainly relies on immune system aging and expansion of less immunogenic (immuneselection) and/or less immunosuppressive (immunesubversion) CSCs subclones (reviewed in [25]), resulting in overt tumors.
CSCs driven immuneselection and immunesubversion
CSCs may escape the active clearance by hiding themselves to the immune system via the downregulation or lack of MHC class I (MHC-I) molecules, as observed in melanoma, prostate cancer, bladder, and colorectal carcinoma (CRC). In particular, CSCs undergo a switch in the MHC-I expression, reducing immune-activator MHC class Ia (HLA A-C) in favor of immune-inhibitory MHC class Ib (HLA E-G) molecules, and suppressing MHC class II (MHC-II) and costimulatory molecules, like CD40, B7-1 and B7-2. Moreover, CSCs lack the expression of ligand for activator NK receptors (NKp44, NKp30, NKp46 and CD16) and in turn upregulate ligands for inhibitor NK receptors (HLA-G), resulting in innate immunity repression.
Overall, immune escaping CSCs subclones hijack the host immune system response. They are able to 1) reduce the expression of M1 macrophages inhibitors CD200 and CD44 blocking macrophage M2 polarization and phagocytic activity, 2) produce several cytokines in the TME, like Transforming Growth Factor β (TGF-β), IL-4, IL-6, IL-10, paralyzing the immune system responses, 3) convert a subset of immature myeloid DCs into TGF-β-secreting cells, thus driving expansion of immunosuppressive regulatory T cells (Tregs) in lymphoid organs of tumor bearing mice [27,28], and 4) attract Tregs and Myeloid-Derived Stem Cells (MDSC), facilitating CSCs spreading and metastatization [29]. Further, mutations promoting CSCs survival outside the CSCs niche favor CSCs spreading and cancer metastasis. Tumor variants emerging after lymphocyte and cytokines selection are the first cause of mortality, because of their resistance to both chemo/radiotherapies and adoptive cell therapies.
Immunotherapy
Accumulating results indicate that CSCs may develop resistance to standard cancer therapies, including chemo-radiotherapy and molecular targeted therapy, making more difficult to fight cancer with available clinical approaches. A recently adopted treatment is immunotherapy, stimulating the immune system surveillance against the tumor, and combining monoclonal antibodies, immune response modifiers, and vaccines. Unlike conventional chemotherapy resulting in secondary resistance, the co-inhibitory immune checkpoints (ICI) therapy revealed a significant long-lasting clinical effect in melanoma, non-small cell lung cancer, renal and bladder cancers, HNSC, CRC, and Hodgkin lymphoma [30–32]. ICI therapy with monoclonal antibodies anti-PD-1 and anti-Cytotoxic T-Lymphocyte Antigen 4 (anti-CTLA-4) promoted T cells migration and intratumoral invasion, thus supporting effective tumor elimination. Nowadays, the design of novel therapies facilitating tumor immunoediting by immune cells and/or exposing CSCs to the host immune response represent promising prospective treatments in solid tumor therapy.
CSCs in oncogenic and therapeutic inflammation
The induction of chronic oncogenic inflammation by CSCs favors the release of pro-tumorigenic chemokines by innate immune cells, thus resulting in tumor cell growth, survival, and angiogenesis [33–35]. Indeed, the tumor itself has the chance to promote cancer metastasis taking advantage of oncogenic inflammation. The same chemokines, like INF-γ or TGF-β, seem to be involved in both immune surveillance and pro-oncogenic inflammation. Indeed, tumor promoting inflammation and tumor-suppressive immunity co-exist, rendering it more difficult to distinguish two phenomena with common patterns of immune cells and cytokines. A further level of complexity is introduced by therapeutic inflammation induced by chemotherapic drugs and radiotherapy. It subserves the effective eradication of the tumor mass by helping antigen-immune system cross-talk [24]. The deeper comprehension of the inflammasome regulation in CSCs metabolism and cancer might improve efficacy of molecular and cellular targeting in current therapy.
Neurotrophins in CSCs-driven tumor growth
Neurotrophins and neurotrophins receptors expression in cancer
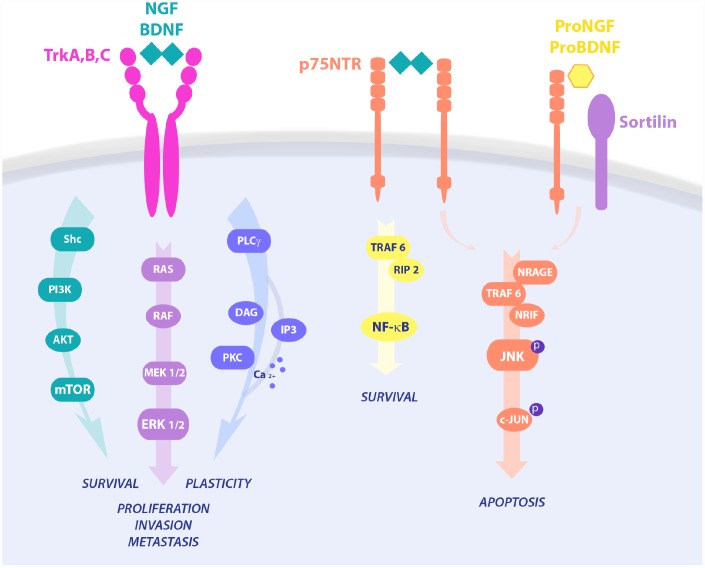
Neurotrophic signaling has been strongly implicated in cell survival, proliferation and apoptosis (Figure 1). Unbalanced expression of neurotrophins Nerve Growth Factor (NGF), Brain-Derived Neurotrophic Factor (BDNF), Neurotrophin3 (NT3), and/or their receptors Tropomyosin related kinase A (TrkA), Tropomyosin receptor kinase B (TrkB), Tropomyosin receptor kinase C (TrkC), and common Neurotrophin Receptor p75 (p75NTR) have been reported in cancer [36,37]. Increased evidence pinpoints a central role of the neurotrophic pathways in cancer growth and progression. In particular, NGF and BDNF are considered diagnostic biomarkers for hepatic cancer (HC) and CRC. NGF level is 57.3 times higher in CRC than in normal colon tissue [38] and significantly correlates with esophageal squamous cell carcinoma (ESCC) and CRC growth and metastasis [39]. Moreover, NGF overexpression is sufficient per se to induce gastric cancer (GC) in rodent animal models [40]. In line with this, anti-NGF based therapies have been demonstrated to be a promising approach in tumor treatment, as well as in tumor associated cancer pain [41]. Further, inhibition of TrkA blocked tumor growth and reinforced chemotherapy in pancreatic ductal adenocarcinoma (PDAC) [39].
Figure 1.
Neurotrophins signaling pathways in cell survival and death. NGF binds TrkA and p75 in a trimeric complex and mediates proliferation, differentiation, and survival via activation of different pathways, like PI3K/AKT, Ras/MAPK and PLC-γ. Upon p75NTR homo-dimerization, NGF is also able to activate NF-κB or JNK, resulting in RIP2 and NRAGE/NRIF signalings, respectively. On the contrary, proneurotrophins, and proNGF in particular, complex with p75NTR and sortilin, leading to activation of pro-apoptotic pathways and cell death.
TrkA, TrkB, and TrkC proteins derive from NTRK1, NTRK2 and NTRK3 genes, respectively. Genetic aberrations of the NTRK genes, like point mutations, gene fusions, constitutively active splice variants are the most well validated oncogenic events in both infantile and adult cancers [42–44]. NTRK1 genetic variants occur in tumors of neuronal type (neuroblastoma and medulloblastoma), but also in non-neuronal cancers, like thyroid, breast, lung, prostate, ESCC, PDAC, GC, HC, and CRC (reviewed in [39,45–48]).
Constitutively active TrkA isoforms generated by alternative splicing rearrangement, like TrkAIII (spliced exons 6, 7 and 9), lack the extracellular signal for membrane localization, induce sustained PI3K/AKT/NF-kB signaling, and cause DNA instability [49]. Oncogenic TrkA fusion products [50] potentiate NGF-dependent carcinogenesis in CRC, thyroid cancer, and AML, leading to the concept of NTRK1 functioning as an oncogene [39]. Treatment of cancers presenting TrkA fusion proteins with selective Trk inhibitors resulted in a better prognosis [51,52]. Further, over-expression of the NGF specific receptor TrkA is considered a reliable index of tumorigenicity, invasiveness, and chemotherapy resistance in several types of squamous cancers [53].
NTRK2 variants have been observed in glioblastoma and HNSC [54]. Also, TrkB overexpression has been observed in ESCC and GC, associated to anoikosis caused by decreased E-cadherin in GC, and to higher chemoresistance in ESCC, being thus considered a metastasis predictor and a strong indicator of bad prognosis [55].
On the contrary, TrkC is a conditional tumor suppressor acting as a dependence receptor and able to induce the caspase cascade in absence of its ligand NT3. NTRK3 is a conditional tumor suppressor epigenetically or genetically downregulated in CRC [56]. Thus, CRC cells characterized by the loss/dysfunctional mutation in the NTRK3 gene acquire a selective advantage and contribute to CRC expansion.
As for the common neurotrophin receptor, p75NTR belongs to the tumor necrosis factor family of receptors. The expression studies on p75NTR led to conflicting results, with p75NTR demonstrated to be a tumor suppressor and a good prognostic factor in digestive cancers or a valuable index of tumor aggressiveness in ESCC and prostatic cancers [39,57–59]. In fact, p75NTR expression is negatively regulated and sometimes null in HC and GC as compared to normal mucosa [60], while its re-activation induces apoptosis through cell cycle arrest, as observed in vitro in HC cells [61]. Moreover, p75NTR is specifically overexpressed in prostate cancer cells, where its level correlates with high-risk prostate tumors with a poor prognosis (Gleason score >7), but not in normal and benign hyperplastic prostate epithelial cells [62]. On the other hand, p75NTR is a marker of chemo-resistant CSCs population in ESCC [59].
Neurotrophins signaling pathway promoting CSCs survival/proliferation
Neurotrophins are regulators of developmental neuronal survival, growth and differentiation and mediate higher-order functions, like synaptic plasticity, learning, memory and behavior in adulthood, after injury, and in age-related neurodegeneration. NGF, BDNF, NT-3, and NT-4/5 are members of the neurotrophin family of growth factors [63,64]. Neurotrophins have preferential binding for specific receptors of the Trk family of receptor tyrosine kinases: NGF binds to TrkA, BDNF and NT-4 to TrkB, and NT-3 to TrkC. All neurotrophins are able to bind the common p75NTR. Further, the association of p75NTR with Trk receptors stabilizes Trk binding to its neurotrophin. Neurotrophin signaling includes Ras, PI3K, Phospholipase C-γ (PLC-γ), and mitogen-activated protein kinase (MAPK) activation leading to survival, proliferation and/or differentiation of target cells. Opposite, activation of p75NTR stimulates NF-κB and c-Jun N-terminal kinase (JNK), promoting inflammation and apoptosis, respectively [65]. In many cancers TrkA activates prosurvival downstream pathways upon NGF binding, while p75NTR binding to its preferred ligand proNGF and co-interactors, like sortilin, instructs pro-apoptotic signaling leading to cell death [66]. In particular, proNGF/p75NTR activates cell death in prostate cells, while their loss in prostate cancer allows tumor expansion and spreading [36]. However, ligand neurotrophins also show ambiguous behavior in carcinogenesis. In line, proNGF binds TrkA and sortilin in breast cancer, inducing the Sex Determining Region Y-box 2 (Sox2) and conferring higher invasiveness to CSCs in a p75NTR-independent manner [67]. Of note, both precursor and mature neurotrophins have been reported to promote tumor growth in breast cancer [68], where p75NTR has been also associated to a pro-survival effect [69].
NGF, BDNF and NT3 pathways represent survival and proliferation signals in CSCs, by activating the Son of Sevenless (Sos)-Ras-MAPK and Fibroblast growth factor receptor substrate 2 (Frs2)/Ankyrin Repeat-Rich Membrane Spanning (ARMS)-Crk pathways, leading to cAMP response element-binding protein (CREB) and NF-kB stimulation, and finally controlling key cellular check-points implicated in CSCs proliferation in glioma, HNSC, melanoma, and breast cancer [37]. BDNF/TrkB and NT3/TrkC signaling complexes have been shown to promote CSCs survival via AKT and Extracellular signal–Regulated Kinases (ERK) pathways in glioma [70]. Further, TrkB deletion in CSCs prevents tumor reappearance in recurrent triple negative breast cancer [71].
NGF survival signaling through the TrkA pathway follows three main routes of intracellular second messengers: 1) Src homology 2 domain containing (Shc)/PI3K/AKT leading to survival of breast and prostate cancers, 2) the Ras/MAPK induced proliferation and invasion in breast and prostate cancer, and cell death by autophagy in medulloblastoma and glioblastoma, 3) PLC-γ/PKC signaling involved in metastasis [36]. Interestingly, signaling via p75NTR strongly depends on binding to its interactors sortilin, Leucine Rich Repeat and Ig Domain Containing 1 (LINGO1), and Neurite outgrowth inhibitor (NOGO), switching from survival to cell death pathways, growth regulation and macrophage clearance, respectively. Indeed, p75NTR via Tumor necrosis factor receptor type 1-associated DEATH domain-dependent (TRADD-dependent), NF-kB and Brain expressed X-linked (BEX) drives a prosurvival effect in breast cancer and schwannoma, while being anti-cancerogenic via JNK-mediated apoptosis in prostate cancer cells and neurons [72–74]. Constitutive active TrkAIII variant induces an undifferentiated stem-like phenotype through increased expression of stemness genes like Nanog, Nestin, Sox2 and CD117, leading to the formation of larger neurospheres in SH-SY5Y neuroblastoma cell line [75]. The NGF-TrkA pathway induces p75NTR proteolytic processing and the release of the soluble p75NTR intracellular domain (ICD), which is central to AKT signaling and CSCs sustained proliferation in several tumor types [76,77], suggesting that the generation of the ICD domain is crucial for the NGF/TrkA pro-oncogenic pathway [39]. Of note, Rho GTPase-mediated recruitment of CD44 to the cell membrane by NGF-TrkA further contributes to CSCs stemness maintenance and survival, resulting in higher tumor aggressiveness [78]. According to this, pharmacological TrkA inhibition prevents p75NTR shedding and the proliferative effect of NGF observed in CSCs. Interestingly, the p75NTR has been observed in the mitotically quiescent CSCs population of the basal epithelia [59,79,80], and activates intracellular signals regulating cell survival, proliferation, and DNA stability, through key oncogenic molecules, like NF-κB [81] and p53 [82]. Furthermore, p75NTR regulates the expression of pluripotency transcription factors, including Sox2, Nanog, and MYC, promotes CSCs self-renewal in breast cancer, and facilitates symmetric divisions in slow-proliferating or quiescent CSCs [83]. The p75NTR neutralization with a specific monoclonal antibody prevents CSCs survival signaling mediated by ERK in HNSC, and genetic loss of p75NTR in melanoma cells completely inhibits tumorigenicity in the xenograft model [84].
Insulin and NGF signalings cross-talk in CSCs metabolism
CSCs expansion and spreading strictly depend on the energy intake by glucose uptake. The insulin/ insulin-like growth factor (IGF) pathway is well known to control glucose uptake in the peripheral organs, as well as in the nervous system. Disturbances in the insulin/IGF pathways have been linked to the pathogenesis of cancer [85]. CSCs stemness maintenance depends on the IGF-1 receptor activation in HNSCC [86]. Accordingly, metformin, the most used drug against insulin resistance in Type 2 Diabetes, has been shown to reduce CSCs reservoir in breast cancer [87]. In particular, the insulin receptor substrate 1 (IRS1)/PI3K/AKT pathway leads to Glycogen synthase kinase 3β (GSK3β) inactivation by serine 9 phosphorylation, thus preventing Snail and Slug proteasome targeting, and activating the NF-kB transcription factor, which in turn increases Snail and Zinc finger E-box-binding homeobox (ZEB) 1 transcription for EMT (reviewed in [88]). Thus, the insulin/IGF pathway induces EMT transcription factors by cross-talking with the signaling platforms implicated in cell proliferation and pluripotency. NGF has been demonstrated to control insulin signaling and improve insulin resistance by promoting glucose uptake in degenerating neurons [89]. Noteworthy, the insulin receptor (IR) signaling has been demonstrated to be transactivated by the NGF receptor TrkA via the IR or the IRS1 in neurons and in the pheochromocytoma cell line PC12 [89,90], and by oncogenic fusion protein Trk-T1 from thyroid carcinoma triggering the IRS-Growth factor receptor-bound protein 2 (IRS-Grb2) complex [91]. Of note, Grb2 and Shc signalings are sufficient per se to induce transformation of fibroblasts [92] and intestinal epithelial cells [93], suggesting Grb-Shc as a crucial molecular hub for common downstream pro-oncogenic pathway. These findings pinpoint a role for the NGF-TrkA/Shc and insulin/IR-IRS axes and reciprocal interplay in the regulation of CSCs glucose metabolism and tumor expansion, highlighting a novel target for precision medicine.
Neurotrophins contribution to CSCs Epithelial-mesenchymal transition
Neurotrophins have been implicated in EMT, a process of genetic reprogramming and morphological shift from elongated epithelial cells to migrating mesenchymal-like cells, with further conversion to CSCs, leading to CSCs enrichment in the tumor microenvironment (TME). Three different transcription factors protein families, the Snail (including Snail and Slug), ZEB (ZEB1, ZEB2), and basic helix–loop–helix (including TWIST1, TWIST2, and TCF3) induce the EMT program by chromatin rearrangement and/or promoter regulation [8]. As a result, proteins of epithelial origin, like E-cadherin, are downregulated and N-cadherin, fibronectin, and vimentin are upregulated to facilitate cell motility and autonomy from niche signals [8,94]. Other EMT transcription factors are common regulator of both CSCs proliferation and EMT commitment, like CD44, Sox2, Sox9, Nanog [8].
In breast cancer, NGF/p75NTR affects epithelial markers like keratin 18, keratin 19 and E-cadherin, while promoting mesenchymal markers, like SLUG, to sustain CSCs migratory behavior [37]. NGF stimulates the expression of SNAIL1, SNAIL2 and TWIST1 in breast cancer cells [68]. Indeed, p75NTR knock-out induces loss of stemness markers, like Sox2 and Sox10, and reconverts spindle-shaped melanoma cells in epithelial-like cells [84]. The p75NTR appears to be involved in EMT phenotypic acquisition and invasiveness. The p75NTR is developmentally expressed in the nervous system and in the neural crest, where it guides fine migration of neural crest cells to form the neural tube. Interestingly enough, the same p75NTR/sortilin signaling system is involved in neural cell migration and cancer metastasis in several tumor types [95].
BDNF/TrkB signaling through AKT and MAPK downstream effectors stimulates the expression of the TWIST-SNAIL axis in rat kidney epithelial cells inducing EMT and CSCs spreading [96]. BDNF through p75NTR activates PI3K/AKT pathway interfering with the RhoA pathway, causing cytoskeletal rearrangement, and promoting CSCs invasiveness in lung cancer, ESCC [97], and head and neck cancer [98]. siRNA silencing or Trk inhibitors prevented BDNF-mediated expression of EMT transcription factors and affected melanoma sphere-forming potential [99].
Angiogenesis in tumor immune evasion
Sufficient blood supply to the tumor comes from neoformation of vessels through endothelial cells angiogenesis and vasculogenesis, as well as by vasculogenic mimicry. CSCs have been observed to be involved in both mechanisms [100]. Interestingly, angiogenic factors overexpressed in many cancers, like Vascular Endothelial Growth Factor (VEGF), Cyclooxygenase 2 (COX-2), and Prostaglandin E2 (PGE2) have an immunosuppressive action, supporting tumor immune evasion. VEGF also inhibits T cell development and is associated with high metastatic potential and poor prognosis in ovarian cancer. COX-2 is implicated in the production of immunosuppressive prostaglandins, like PGE2 and Prostaglandin D2 (PGD2). PGE2 downregulates TNF-α, inhibits T and B cells proliferation, and NK-mediated tumor clearance, while PGD2 favors T helper 2 cells activation at the expenses of tumor eradicating T helper 1 immune response. Also, proangiogenic microRNA (miRNA), like miR-126 sustain cancer metabolism through the IRS1-mediated pathway of glucose uptake [101]. Overall, angiogenesis favors tumor growth by a dual mechanism: on one side facilitating blood supply, on the other side through active suppression of innate and adaptive immune responses. Neurotrophins released by stromal or immune cells in the TME are known to exert a strong proangiogenic effect in in vitro models and in vivo [102–104]. In particular, NGF is known to induce angiogenesis in endothelial cells of several origins through VEGF expression. In line, NGF promotes angiogenesis by TrkA-mediated activation of PI3K and matrix metalloproteinase 2 (MMP2) in breast [105], ovarian [106], hepatocellular [107] cancers. Opposite, proNGF has a net anti-angiogenic effect, increasing angiostatin and thrombospondin-1, and decreasing angiopoietin and angiopoietin-like 1.
Neurotrophins in cholinergic nerve-cancer interplay
Cancer cells growth around nerve terminals and subsequent neural invasion is a process known as perineural invasion (PNI). The presence of nerve endings within the tumors has been described for GC, colon, prostate, breast, pancreatic, bladder, eye cancers [108–112] (reviewed in [113]). Also, neoneurogenesis with the ex novo formation of axons within the tumor has been observed in prostate cancer [114]. Opposite, denervation is known to positively impact on cancer dissemination and patient’s outcome since 1940 in both human and animal studies [115–117]. PNI results from a crosstalk between cancer cells releasing neurotrophins and neuropeptides, and nerve ends expressing TrkA and p75NTR receptors. CSCs respond to NGF by TrkA-mediated autocrine proliferation [118,119] and neurotransmitter release leading to axonal growth around the tumors, tumor expansion and long distance CSCs spreading through the nerves (reviewed in [113]). The neurotrophin family of Trk receptors is well known to support neuron survival and axonal growth in the nervous system, during development and after injury. Similarly to Schwann cells induced axonal regeneration upon nerve injury, NGF, BDNF, NT3 or IGF-II produced by cancer cells sustain cancer growth and PNI through the expression of neurites chemoattractant and guidance molecules associated with poor prognostic outcome (netrin, semaphorins, ephrins, and Slits) [120,121]. NGF, in its precursor or mature form, has been strongly implicated in PNI and neoneurogenesis in prostate cancer [62,122]. Cathecolaminergic, dopaminergic, serotoninergic, glutammatergic, gabaergic, and cholinergic tumor infiltrating nerves have been described so far [123]. In particular, cholinergic nerves within the stem cell-niche help regulate stem cell dynamics in both normal and neoplastic condition [124–126] (reviewed in [40]).
Acetylcholine (Ach) is one of the most important neurotransmitters targeted by cancer pharmacotherapy and its metabolism is dependent upon NGF supply [40]. Nicotine has been indicated as a key driver of tumor cells growth in mesothelioma and colon cancer, and of proliferation, cell migration, and angiogenesis in GC [127]. Nicotine and nicotinic agonists, like 4-(methylnitrosoamino)-1-(3-pyridyl)-1-butanone (NNK), lead to human small cell lung cancer (SCLC) proliferation, while the Ach functional antagonist isoproterenol induced growth of lung adenocarcinoma cells [128]. Cholinergic stimulation through muscarinic receptors induces neurotrophic molecules expression [129–131]. Among neurotrophins, NGF was specifically upregulated (20 times higher) by the cholinergic agonist carbachol in GC mouse models, as well as in human GC [40]. A cholinergic/NGF interplay has been reported in GC, with tuft cells-derived Ach inducing NGF release by CSCs expressing the muscarinic receptor 3 (M3R). In turn, the NGF released in the TME promotes nerve growth and further Ach release in a feedback loop sustaining tumor growth and metastasis. In a similar manner, PNI and lymph node spreading is sustained by a catecholamine/NGF axis in PDAC [132]. On the other hand, M3R antagonists inhibited cell growth of non-small cell lung carcinoma (NSCLC) both in vitro and in vivo [133]. Indeed, the increase of cholinergic parasympathetic fibers by neurogenesis and axonogenesis in prostate cancer xenografts model correlates with metastasis [134]. Similarly, proNGF favors tumor infiltration and affects patient’s survival in human prostate cancer [62].
Taken together, these findings strongly pinpoint the neurotrophin/Trk signaling as messengers between nerves and cancer cells, driving peritumoral innervation and consequent tumor growth and dissemination.
Neurotrophins and exosomes-driven tumorigenesis
Tumors release extracellular vesicles, called exosomes, regulating the TME and promoting disease progression by induction of tumor tolerance and spreading, and axonogenesis (reviewed in [135]). Exosomes are 30–150 nm vesicles expressing marker proteins, such as CD63, Alix, Tsg, CD9, and CD81, and delivering cargo of intercellular messenger proteins, mRNA, non-coding RNA like long non-coding RNA (lncRNA), miRNA, DNA, and lipids [136]. Exosomes facilitate intratumoral axon growth by releasing axonal guidance molecule, like EphrinB1 [136]. Indeed, tumors compromised in exosome release are less innervated than controls and pharmacological blockade of exosome release by the multi-vesicular body (MVB) inhibitor GW4869 is effective in diminishing tumoral innervations by β-III tubulin positive “nerve twigs” [136]. Opposite, exosomes from “non-metastatic” melanoma are able to trigger NK and TRAIL-driven macrophage clearance of tumor cells, reinforcing immune surveillance at the pre-metastatic niche and exerting a pro-apoptotic effect on lung carcinoma cells [137]. Of note, neuronal exosomes are enriched with p75NTR [138], and prostate cancer exosomes carry tyrosin kinases, such as Src tyrosine kinase and IGF-1R, promoting tumor expansion and angiogenesis [139,140]. Furthermore, the BDNF receptor TrkB transfers glioblastoma aggressiveness to recipient cancer cells [141]. CSCs exosomes from a CSCs clonal line transfer SLUG and Sox2 and induce EMT through lnc-Regulator of Reprogramming (lnc-ROR) [142]. Plus, exosomal transfer of miRNA-142 from bone marrow-derived mesenchymal stem/stromal cells (BM-MSCs) stimulates colon CSCs proliferation by NUMB-mediated activation of Notch signaling [143]. Thus, active signaling molecules are transported by cancer exosomes contributing to CSCs communication with the TME and modulating cancer outgrowth metastasis and immune cells evasion. Additionally, CSCs exosomes are potential nano-carriers for drugs and vaccines, and their cargos provide potential biomarkers for early diagnosis and improved prognosis in cancer.
Evidence of neurotrophins actions in tumor immune surveillance
Nowadays, a deeper comprehension of neurotrophins involvement in cancer immune surveillance is of foremost relevance. In fact, neurotrophins and their receptors are key molecules in survival and functions of cells of both the innate and adaptive immune system. NGF is produced in an autocrine manner by cells of the immune system, such as B and T cells, monocytes/macrophages, eosinophils, granulocytes, and mast cells [144–146]. NGF is a growth and survival factor also for B cells [147]. During inflammation, NGF synthesis is induced by inflammatory cytokines (IL-1β, TNF-α, IL-6) in different cell types. Both NGF receptors TrkA and p75NTR are expressed by immune cells, the first being anti-apoptotic and survival stimulating [148,149], the latter transmitting pro-apoptotic signals [144].
Nonetheless, it is not clear whether and through which mechanisms neurotrophins, and especially NGF, may eventually be implicated in the modulation and refinement of tumor editing/escape.
Indeed, the most relevant known effects of NGF and its receptors on key cellular substrates and molecular mechanisms of the tumor immune surveillance are reported here below (Table 1).
Table 1. Main findings on the role of neurotrophin NGF and its receptors TrkA and p75NTR in tumor surveillance by innate and adaptive immune cells.
| Neurotrophins and receptors | Target immune cells | Function/effect | References | ||
| NGF | NK cells | negative influence on NK cell degranulation | [161] | ||
| CD4+ T-cells | regulation of immune response | [153,156] | |||
| CD8+ T cells | regulation of immune response | [153,156] | |||
| TrkA | NK cells | anti-tumoral effect | [161] | ||
| Monocytes | anti-inflammatory effect (by blocking NF-kB proinflammatory pathways and inducing anti-inflammatory cytokines) | [169] | |||
| CD4+ T cells | activation and NGF synthesis and release | [155] | |||
| p75NTR | Dendritic cells | activation and induction of TLR4 expression | [162] | ||
| γδ T cells | regulation of γδ T cells activation in autoimmune inflammation | [169,170] | |||
| CD8+ T cells | activation by TCR stimulation | [178] | |||
| Monocytes/Macrophages | increased calcium spiking, phagocytosis, TGF-β secretion, and reduced M2 marker CD206 by NGF binding; proNGF increased migration through podosome formation and neurotoxin secretion by proNGF binding | [173] | |||
Innate immunity
NK cells
NK cells show the ability to selectively kill human colon-derived CSCs, melanoma, and glioblastoma without any pharmacological pretreatment in vitro [150–153]. Mouse resting NK cells express physiological level of TrkA, which is dramatically upregulated upon activation of NK cells by IL-2 [154], suggesting an immune stimulatory and anti-tumoral effect of the NGF-TrkA pathway mediated by NK cells. A NK subpopulation expressing the neural adhesion molecule (N-CAM) and driving local response to IL-2 has been proposed to be crucial for immune surveillance of neoplasia.
Dendritic cells
The activation of human DCs requires signaling driven by Toll-like Receptor 4 (TLR4). Noteworthy, NGF has been shown to promote TLR4 expression following Lipopolysaccharide (LPS) treatment by p75NTR-dependent activation of p38 MAPK and NF-κB pathways [155]. On the other hand, neurotrophins have been shown to promote release of several growth factors reducing the effectiveness of DCs for immune surveillance of tumors, like IL-6, IL-10, macrophage colony-stimulating factor (MCSF), VEGF, and PGE2 [156].
Patrolling monocytes
Non-classical patrolling monocytes are known to be early interactors of metastasizing tumor cells and to promote NK cells recruitment and activation [157,158], thus contributing to cancer immune surveillance and representing putative targets for cancer immunotherapy. Human monocytes have been reported to respond to an immunogenic stimulus by increasing TrkA mRNA expression [159].
γδ T cells
Unlike the αβ T cells commonly used in Chimeric Antigen Receptor Therapy (CAR-T), γδ T cells play a role in the innate immune response, which constitutes the first, faster line of defense of the immune system. The γδ T cells are major players in the “lymphoid stress surveillance,” i.e., by early activation following infections or non-microbial stress. This peculiar type of T cells does not require clonal expansion or differentiation, as it occurs in the prototypic innate immunity [160]. Tumor-infiltrating γδ T cells are an important subset of “unconventional” T lymphocytes as they have the ability to recognize a broad range of antigens without the presence of MHC. The γδ T cells have been demonstrated to be the most favorable prognostic immune population among many cancer types, in agreement with their killing capacity against leukaemia, neuroblastoma, and carcinoma. By applying CIBERSORT, a computational method for inferring leukocyte representation in bulk tumors, the most favorable predictor gene is CD161, a surface molecule associated to tumor infiltration by γδ T cells [161]. They produce IL-17, IFN-γ and TNF-α, leading to DCs maturation, and prime CD4+ and CD8+ T cells.
The p75NTR has a regulatory effect on immune cells activation during autoimmunity [162] and, noteworthy, it is involved in control of γδ T cells activation in inflammation [163].
Innate lymphoid cells
Innate lymphoid cells (ILCs) represent a constitutive patrolling immune unit aimed at tissue homeostasis maintenance at the mucosal barriers. Three main distinct ILCs subpopulations have been described, based on their phenotype and functions. ILCs type 1 produce IFN-γ; ILCs type 2 secrete IL-5 and IL-13; ILCs type 3 release IL-17 and/or IL-22 [164,165]. ILCs play an essential role in tissue inflammation and remodeling, and in cancer as well [166,167].
Of note, the localization of ILCs at cholinergic, adrenergic, and nociceptor sensory neuronal terminals in several tissues led the hypothesis of a key role in neuro‐immune interactions in normal tissue physiology and in the perineural cancer niche. In line with this, ILCs express receptors for neurotransmitters and neuropeptides, like β2‐adrenergic receptor (β2‐AR), muscarinic cholinergic receptor, vasoactive intestinal peptide receptor (VPAC1/2), and calcitonin receptor‐like for CGRP [168].
Acquired immunity
The γδ T cells, NK cells, and Cytotoxic T Lymphocytes (CTLs) are important players in the eradication of CSCs. However, only effector cells of the adaptive immunity system may specifically recognize CSCs.
Disabled antigen presenting cells
The presence of MHC proteins at the CSCs membrane surface is crucial for T cells-dependent anti-cancer immunity [25]. Lack or de novo mutation in the antigen presentation machinery may result in immune escape of malignant cells. Indeed, MHC-I down-regulation has been reported in around 40% of common solid malignancies (melanoma, lung, breast, renal, prostate, and bladder cancers). Accordingly, alterations in MHC expression have been found to correlate with the clinical outcome in cancer patients. Although CD8+ CTLs are deficitary in targeting CSCs with low MHC-I expression, recent in vitro findings suggest that human γδ T cells are able to target CSCs upon CSCs sensitization by bisphosphonate zoledronate [169]. Noteworthy, TrkA-positive neuroblastoma cells have higher amount of MHC-I complexes and a less malignant phenotype, pin-pointing the role of TrkA in neuroblastoma spontaneous regression [170].
While M1 macrophages are implicated in eradication of the foreign cell during acute phase inflammation, their polarization switch to an anti-inflammatory tumor-permissive phenotype (M2) allowing metastatic spreading is typical of TAMs and it is associated with poor prognosis. Noteworthy, cultured human macro-phages express both TrkA and p75NTR receptors and differently respond to NGF and proNGF by augmenting calcium spiking, phagocytosis, TGF-β secretion and by a slight reduction of the M2 marker CD206 in the first case, while increasing migration by podosome formation and neurotoxin secretion, in the latter [171].
Cell dysfunction/tolerance
Main effectors of cellular acquired immunity against cancer are CD8+ and CD4+ T cells [172]. Tumor infiltration by CD8+ T cells is associated with prolonged patient survival [172,173]. Malignant cells elimination by CD8+ CTLs has been considered for decades as a master regulator of anti-tumor immunity, confining CD4+ T cells to a supportive action.
Nonetheless, CD4+ T cells have been recently found to exert a broad range of action in tumor rejection. They show cytotoxic effects on tumor cells, upregulate MHC molecules expression, are anti-angiogenic, and are able to promote tumor dormancy. By partnering with NK cells, CD4+ T cells maximize their ability to eliminate tumors resistant to CD8-mediated rejection, even in case of MHC-II negative tumors [174]. Noteworthy, CD4+ T cells are critical for expansion, trafficking and functioning of cytotoxic CD8+ and memory T cells, an effect known as “CD4+ T-cell help” fostering tumor destruction through cytokine signaling, especially IFN-γ and TNF-α [175]. Of note, CD4+ T-cell line 9/6 express the NGF receptor TrkA after TCR-mediated activation by the antigens and/or the antigen presenting cells (APC [148];). Activated CD4+ T-cell clones not only express TrkA but they also produce NGF, further pinpointing the NGF/TrkA system in an autocrine/paracrine loop modulating the maturation and activity of T cells [146,149]. As for the common neurotrophins receptor, p75NTR is implicated in antigen-driven T cell responses in vivo and contribute to T cell activation upon stimulation [176]. p75NTR genetic ablation in vivo leads to an hypoproliferative response to TCR agonists, decreased expression of the activation markers CD25 and CD69, of IL-2, and IFN-γ [176]. Moreover, activation threshold CD8+ CTLs upon TCR stimulation depends on p75NTR and increases following p75NTR deletion [176].
However, CD8+ CTLs are often unable to eradicate the tumor because of inhibition by other, immunosuppressive cells in the TME, such as Tregs. Tregs are a specialized subpopulation of CD4+CD25+ T cells producing IL-17, also called T helper 17 cells. Their induction of self-tolerance and inhibition of both natural and induced anti-tumor immunity are considered key events in cancer immune evasion. Consequently, there is considerable interest in therapeutic Tregs blockade to treat cancer [177]. Noteworthy, NGF anti-inflammatory effect through IL-6 and IL-10 down-regulate Tregs homeostatic responses and reduces IL-17 level in airway allergy [178]. It would be interesting to find out whether a similar mechanism under the control of neurotrophins takes place to counteract Tregs immune tolerance in cancer.
Neurotrophins control of oncogenic inflammation
NGF increase at the sites of inflammation and in systemic circulation is a common event in different inflammatory and autoimmune diseases, and in cancer. Inflammatory cytokines, like IL-1β, IL-6, and TNF-α stimulate production of NGF in several cell types. In turn, NGF induces IL-10 and IL-1 receptor antagonist via the PI3K/AKT pathway and facilitates TLR4-mediated inhibition of NF-kB, leading to resolution of the inflammation [179]. The findings reported above on the role of neurotrophin signaling in the activation of immune surveillance mechanisms could be in apparent contradiction with their role in oncogenic inflammation and their classic anti-inflammatory effect reported in the Central Nervous System in vitro and in vivo [179–181]. On the contrary, NGF exerts a dual role by activating immune responses following acute insult, while concomitantly avoiding tumor growth sustained by chronic inflammation via a timely resolution of the immune response.
Conclusions
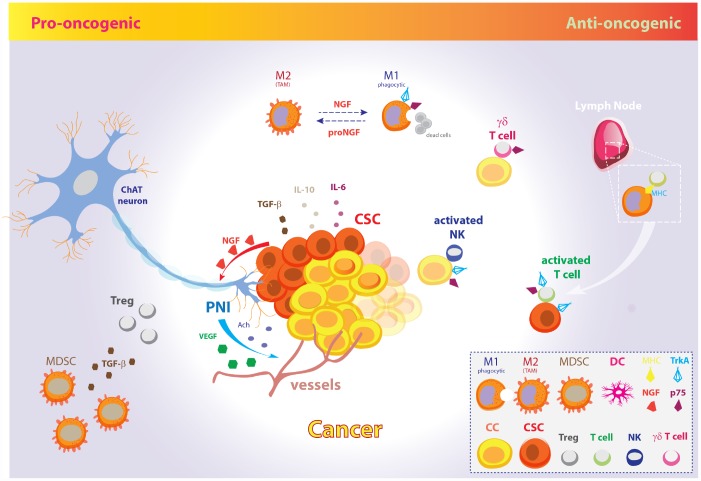
Taken together, the experimental findings here reported suggest opposite pro-oncogenic and anti-oncogenic actions of the NGF signaling pathway in the control of CSCs growth and cancer evasion from the host immune system (Figure 2). NGF/TrkA signaling and cholinergic innervation of the tumor niche take central stage in tumor initiation and progression, as well as metastatic spreading. In line with this, the targeting of neurotrophic growth factors in cancer has been suggested to halt tumor progression through direct CSCs targeting, to achieve control of nerve infiltration and angiogenesis, and minimize cancer pain [182–184]. Accordingly, selective and in situ treatment with potent Trk kinase inhibitors, clinical development of drugs targeting NTRK genetic rearrangement combined with canonical cancer therapy, and/or novel encouraging CAR-T immunotherapy are all promiseful neurotrophin-based strategies to improve cancer patients outcome.
Figure 2.
The pro-oncogenic and anti-oncogenic effects of the NGF signaling pathway in CSC metabolism and EMT. Schematic model illustrating the opposite pro-oncogenic (left) and anti-oncogenic (right) actions of NGF signaling pathway in the control of CSCs growth and cancer evasion from the host immune system. Pro-oncogenic pathway. CSCs promote tumor growth, perineural invasion, CSCs proliferation and spreading through vessels and nerves by NGF release. In fact, tumor-released NGF attracts cholinergic endings and promotes cancer expansion and neoangiogenesis through neuronal-derived Ach and VEGF. Further, CSCs inhibit the host immune response and facilitate metastatic spreading through IL-10, IL-6, and TGF-β. Excess amount of proNGF stimulates macrophages polarization toward the M2 phenotype, giving rise to TAMs, which are unable to phagocytize cancer cells. Moreover, MDSCs induce Tregs expansion by TGF-β release and contribute to dismount the T-cells mediated immune response. Anti-oncogenic pathway. On the other hand, increasing evidences pinpoint a role for NGF pathway in promoting tumor surveillance by both natural and adaptive immune cells. The NGF-TrkA signaling system induces phagocytic M1 macrophages, thus resolving cancerogenic inflammation. Moreover, NGF receptors allow membrane exposure of activatory NK receptors. The p75-expressing γδ T cells are phagocytic T cells of the so-called “lymphoid stress surveillance” system. NGF-TrkA promotes MHC-I and MHC-II expression by cancer cells and CSCs, and allow recruitment of IL-2 activated T cells in lymph- , promoting the tumor mass eradication. The illustration includes images modified from “freevector.com”, distributed under the Creative Commons Attribution 4.0 license (CC BY 4.0).
Nonetheless, increasing evidences pinpoint the involvement of neurotrophins, and specially NGF, in tumor immune surveillance through cytokines-driven modulation of the innate and acquired immune system cells. In particular, given the Tregs and PD1 control by p75NTR and NGF, NGF pathway inhibition would result in immune tolerance induction, thus challenging the use tout-court of TrkA inhibitors to dampen tumor growth. Moreover, the activation of the neurotrophic pathway is fundamental in order to downregulate oncogenic inflammation during self-promoted tumor growth. To overcome this dichotomy, fine understanding of the molecular targets and cellular substrates of NGF/TrkA involved in tumor growth on one side and immune surveillance on the other side is demanding nowadays in order to design selective and coordinated therapies against tumor characterized by uncontrolled overactivation of the NGF pathway as oncogenic driver.
Abbreviations
- AML
Acute Myeloblastic Leukaemia
- APCs
Antigen-Presenting Cells
- BCL-2
B-cell lymphoma-2
- BCL-XL
B-cell lymphoma-Extra Large
- ICI
co-Inhibitory Immune Checkpoints
- CTL
Cytotoxic T Lymphocytes
- CTLA-4
Cytotoxic T-Lymphocyte Antigen-4
- CTCs
Circulating Tumour Cells
- CSCs
Cancer Stem Cells
- DCs
Dendritic Cells
- EMT
Epithelial-Mesenchymal Transition
- GC
Gastric Cancer
- HNSC
Head and Neck Squamous Carcinoma
- MCSF
Macrophage Colony-Stimulating Factor
- MDSC
Myeloid-Derived Stem Cells
- MHC
Major Histocompatibility Complex
- NSCLC
Non-Small Cell Lung Carcinoma
- PDL1
Programmed Death-Ligand 1
- PGE2
Prostaglandin E2
- SCLC
Small Cell Lung Cancer
- TAMs
Tumour Associated Macrophages
- Tregs
Regulatory T cells
- IGF
Insulin-like Growth Factor
- NGF
Nerve Growth Factor
- NT
Neurotrophin
- VEGF
Vascular Endothelial Growth Factor
- P75NTR
p75 neurotrophic receptor
- TrkA
Tropomyosin related kinase A
- TrkB
Tropomyosin related kinase B
- TrkC
Tropomyosin related kinase C
- BEX
Brain Expressed X-linked
- COX-2
Cyclooxygenase-2
- CREB
cAMP Response Element-Binding protein
- DAMP
Danger Associated Molecular Patterns
- IDO
Indoleamine 2,3-Dioxygenase
- INF- γ
Interferon-γ
- LINGO1
Leucine Rich Repeat And Ig Domain Containing 1
- JNK
c-Jun N-terminal kinases
- mTOR
mammalian Target Of Rapamicin
- MAPK
Mitogen-Activated Protein Kinase
- MVB
Multi-Vesicular Body
- NOGO
Neurite Outgrowth inhibitor
- NF- kB
Nuclear Factor- kB
- NLR
Nod-like Receptor
- PI3K
phosphatidylinositol 3-kinase
- PLC-γ
Phospholipase C-γ
- PRR
Pattern Recognition Receptor
- STAT3
Signal Transducer and Activator of Transcription-3 (STAT-3)
- TLR
Toll Like Receptor
- TEM
Tumor Micro Environment
- TRADD
Tumor necrosis factor receptor type 1-associated DEATH domain-dependent
- TRAL
TNF-related apoptosis-inducing ligand
Footnotes
CONFLICTS OF INTEREST: The authors declare that they have no conflicts of interests.
References
- 1.Bomken S, Fiser K, Heidenreich O, Vormoor J. Understanding the cancer stem cell. Br J Cancer. 2010; 103:439–45. 10.1038/sj.bjc.6605821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vermeulen L, de Sousa e Melo F, Richel DJ, Medema JP. The developing cancer stem-cell model: clinical challenges and opportunities. Lancet Oncol. 2012; 13:e83–89. 10.1016/S1470-2045(11)70257-1 [DOI] [PubMed] [Google Scholar]
- 3.Kreso A, Dick JE. Evolution of the cancer stem cell model. Cell Stem Cell. 2014; 14:275–91. 10.1016/j.stem.2014.02.006 [DOI] [PubMed] [Google Scholar]
- 4.Wang X, Huang S, Chen JL. Understanding of leukemic stem cells and their clinical implications. Mol Cancer. 2017; 16:2. 10.1186/s12943-016-0574-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hanahan D, Coussens LM. Accessories to the crime: functions of cells recruited to the tumor microenvironment. Cancer Cell. 2012; 21:309–22. 10.1016/j.ccr.2012.02.022 [DOI] [PubMed] [Google Scholar]
- 6.Gaspar C, Fodde R. APC dosage effects in tumorigenesis and stem cell differentiation. Int J Dev Biol. 2004; 48:377–86. 10.1387/ijdb.041807cg [DOI] [PubMed] [Google Scholar]
- 7.Prieto-Vila M, Takahashi RU, Usuba W, Kohama I, Ochiya T. Drug Resistance Driven by Cancer Stem Cells and Their Niche. Int J Mol Sci. 2017; 18:E2574. 10.3390/ijms18122574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shibue T, Weinberg RA. EMT, CSCs, and drug resistance: the mechanistic link and clinical implications. Nat Rev Clin Oncol. 2017; 14:611–29. 10.1038/nrclinonc.2017.44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feoktistova M, Leverkus M. Programmed necrosis and necroptosis signalling. FEBS J. 2015; 282:19–31. 10.1111/febs.13120 [DOI] [PubMed] [Google Scholar]
- 10.Pantel K, Alix-Panabières C. Liquid biopsy and minimal residual disease - latest advances and implications for cure. Nat Rev Clin Oncol. 2019; 16:409–24. 10.1038/s41571-019-0187-3 [DOI] [PubMed] [Google Scholar]
- 11.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011; 144:646–74. 10.1016/j.cell.2011.02.013 [DOI] [PubMed] [Google Scholar]
- 12.Kraman M, Bambrough PJ, Arnold JN, Roberts EW, Magiera L, Jones JO, Gopinathan A, Tuveson DA, Fearon DT. Suppression of antitumor immunity by stromal cells expressing fibroblast activation protein-alpha. Science. 2010; 330:827–30. 10.1126/science.1195300 [DOI] [PubMed] [Google Scholar]
- 13.Oskarsson T, Batlle E, Massagué J. Metastatic stem cells: sources, niches, and vital pathways. Cell Stem Cell. 2014; 14:306–21. 10.1016/j.stem.2014.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ye J, Wu D, Wu P, Chen Z, Huang J. The cancer stem cell niche: cross talk between cancer stem cells and their microenvironment. Tumour Biol. 2014; 35:3945–51. 10.1007/s13277-013-1561-x [DOI] [PubMed] [Google Scholar]
- 15.Janku F, Yap TA, Meric-Bernstam F. Targeting the PI3K pathway in cancer: are we making headway? Nat Rev Clin Oncol. 2018; 15:273–91. 10.1038/nrclinonc.2018.28 [DOI] [PubMed] [Google Scholar]
- 16.Ghoneum A, Said N. PI3K-AKT-mTOR and NFκB Pathways in Ovarian Cancer: Implications for Targeted Therapeutics. Cancers (Basel). 2019; 11:949. 10.3390/cancers11070949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith HA, Kang Y. The metastasis-promoting roles of tumor-associated immune cells. J Mol Med (Berl). 2013; 91:411–29. 10.1007/s00109-013-1021-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khosla R, Vyas AK, Trehanpati N. Dichotomy of Notch signalling in regulating tumour immune surveillance. Scand J Immunol. 2019; 89:e12744. 10.1111/sji.12744 [DOI] [PubMed] [Google Scholar]
- 19.Robado de Lope L, Alcíbar OL, Amor López A, Hergueta-Redondo M, Peinado H. Tumour-adipose tissue crosstalk: fuelling tumour metastasis by extracellular vesicles. Philos Trans R Soc Lond B Biol Sci. 2018; 373:20160485. 10.1098/rstb.2016.0485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fletcher SJ, Hapon MB, Callegari EA, Crosbie ML, Santiso N, Ursino A, Amato AR, Gutiérrez A, Sacca PA, Dreszman R, Pérez A, Carón RW, Calvo JC, Pistone-Creydt V. Comparative proteomics of soluble factors secreted by human breast adipose tissue from tumor and normal breast. Oncotarget. 2018; 9:31007–17. 10.18632/oncotarget.25749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hao J, Zhang Y, Yan X, Yan F, Sun Y, Zeng J, Waigel S, Yin Y, Fraig MM, Egilmez NK, Suttles J, Kong M, Liu S, et al. Circulating Adipose Fatty Acid Binding Protein Is a New Link Underlying Obesity-Associated Breast/Mammary Tumor Development. Cell Metab. 2018; 28:689–705.e5. 10.1016/j.cmet.2018.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou H, Yu C, Kong L, Xu X, Yan J, Li Y, An T, Gong L, Gong Y, Zhu H, Zhang H, Yang X, Li Y. B591, a novel specific pan-PI3K inhibitor, preferentially targets cancer stem cells. Oncogene. 2019; 38:3371–86. 10.1038/s41388-018-0674-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kolev VN, Wright QG, Vidal CM, Ring JE, Shapiro IM, Ricono J, Weaver DT, Padval MV, Pachter JA, Xu Q. PI3K/mTOR dual inhibitor VS-5584 preferentially targets cancer stem cells. Cancer Res. 2015; 75:446–55. 10.1158/0008-5472.CAN-14-1223 [DOI] [PubMed] [Google Scholar]
- 24.Chow MT, Möller A, Smyth MJ. Inflammation and immune surveillance in cancer. Semin Cancer Biol. 2012; 22:23–32. 10.1016/j.semcancer.2011.12.004 [DOI] [PubMed] [Google Scholar]
- 25.Bruttel VS, Wischhusen J. Cancer stem cell immunology: key to understanding tumorigenesis and tumor immune escape? Front Immunol. 2014; 5:360. 10.3389/fimmu.2014.00360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Taieb J, Chaput N, Ménard C, Apetoh L, Ullrich E, Bonmort M, Péquignot M, Casares N, Terme M, Flament C, Opolon P, Lecluse Y, Métivier D, et al. A novel dendritic cell subset involved in tumor immunosurveillance. Nat Med. 2006; 12:214–19. 10.1038/nm1356 [DOI] [PubMed] [Google Scholar]
- 27.Shang B, Liu Y, Jiang SJ, Liu Y. Prognostic value of tumor-infiltrating FoxP3+ regulatory T cells in cancers: a systematic review and meta-analysis. Sci Rep. 2015; 5:15179. 10.1038/srep15179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sharma A, Rudra D. Emerging Functions of Regulatory T Cells in Tissue Homeostasis. Front Immunol. 2018; 9:883. 10.3389/fimmu.2018.00883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ghiringhelli F, Puig PE, Roux S, Parcellier A, Schmitt E, Solary E, Kroemer G, Martin F, Chauffert B, Zitvogel L. Tumor cells convert immature myeloid dendritic cells into TGF-beta-secreting cells inducing CD4+CD25+ regulatory T cell proliferation. J Exp Med. 2005; 202:919–29. 10.1084/jem.20050463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pardoll DM. Immunology beats cancer: a blueprint for successful translation. Nat Immunol. 2012; 13:1129–32. 10.1038/ni.2392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Topalian SL, Wolchok JD, Chan TA, Mellman I, Palucka K, Banchereau J, Rosenberg SA, Dane Wittrup K. Immunotherapy: the path to win the war on cancer? Cell. 2015; 161:185–86. 10.1016/j.cell.2015.03.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sharma P, Hu-Lieskovan S, Wargo JA, Ribas A. Primary, Adaptive, and Acquired Resistance to Cancer Immunotherapy. Cell. 2017; 168:707–23. 10.1016/j.cell.2017.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sultan M, Coyle KM, Vidovic D, Thomas ML, Gujar S, Marcato P. Hide-and-seek: the interplay between cancer stem cells and the immune system. Carcinogenesis. 2017; 38:107–18. 10.1093/carcin/bgw115 [DOI] [PubMed] [Google Scholar]
- 34.Jinushi M. Role of cancer stem cell-associated inflammation in creating pro-inflammatory tumorigenic microenvironments. Oncoimmunology. 2014; 3:e28862. 10.4161/onci.28862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wu JK, Adepoju O, De Silva D, Baribault K, Boscolo E, Bischoff J, Kitajewski J. A switch in Notch gene expression parallels stem cell to endothelial transition in infantile hemangioma. Angiogenesis. 2010; 13:15–23. 10.1007/s10456-009-9161-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Molloy NH, Read DE, Gorman AM. Nerve growth factor in cancer cell death and survival. Cancers (Basel). 2011; 3:510–30. 10.3390/cancers3010510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chopin V, Lagadec C, Toillon RA, Le Bourhis X. Neurotrophin signaling in cancer stem cells. Cell Mol Life Sci. 2016; 73:1859–70. 10.1007/s00018-016-2156-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yu X, Liu Z, Hou R, Nie Y, Chen R. Nerve growth factor and its receptors on onset and diagnosis of ovarian cancer. Oncol Lett. 2017; 14:2864–68. 10.3892/ol.2017.6527 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 39.Blondy S, Christou N, David V, Verdier M, Jauberteau MO, Mathonnet M, Perraud A. Neurotrophins and their involvement in digestive cancers. Cell Death Dis. 2019; 10:123. 10.1038/s41419-019-1385-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hayakawa Y, Sakitani K, Konishi M, Asfaha S, Niikura R, Tomita H, Renz BW, Tailor Y, Macchini M, Middelhoff M, Jiang Z, Tanaka T, Dubeykovskaya ZA, et al. Nerve Growth Factor Promotes Gastric Tumorigenesis through Aberrant Cholinergic Signaling. Cancer Cell. 2017; 31:21–34. 10.1016/j.ccell.2016.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ghilardi JR, Freeman KT, Jimenez-Andrade JM, Mantyh WG, Bloom AP, Kuskowski MA, Mantyh PW. Administration of a tropomyosin receptor kinase inhibitor attenuates sarcoma-induced nerve sprouting, neuroma formation and bone cancer pain. Mol Pain. 2010; 6:87. 10.1186/1744-8069-6-87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cocco E, Scaltriti M, Drilon A. NTRK fusion-positive cancers and TRK inhibitor therapy. Nat Rev Clin Oncol. 2018; 15:731–47. 10.1038/s41571-018-0113-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Albert CM, Davis JL, Federman N, Casanova M, Laetsch TW. TRK Fusion Cancers in Children: A Clinical Review and Recommendations for Screening. J Clin Oncol. 2019; 37:513–24. 10.1200/JCO.18.00573 [DOI] [PubMed] [Google Scholar]
- 44.Amatu A, Sartore-Bianchi A, Siena S. NTRK gene fusions as novel targets of cancer therapy across multiple tumour types. ESMO Open. 2016; 1:e000023. 10.1136/esmoopen-2015-000023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Faulkner S, Jobling P, Rowe CW, Rodrigues Oliveira SM, Roselli S, Thorne RF, Oldmeadow C, Attia J, Jiang CC, Zhang XD, Walker MM, Hondermarck H. Neurotrophin Receptors TrkA, p75NTR, and Sortilin Are Increased and Targetable in Thyroid Cancer. Am J Pathol. 2018; 188:229–41. 10.1016/j.ajpath.2017.09.008 [DOI] [PubMed] [Google Scholar]
- 46.Geldof AA, Van Haarst EP, Newling DW. Neurotrophic factors in prostate and prostatic cancer. Prostate Cancer Prostatic Dis. 1998; 1:236–41. 10.1038/sj.pcan.4500247 [DOI] [PubMed] [Google Scholar]
- 47.Hondermarck H. Neurotrophins and their receptors in breast cancer. Cytokine Growth Factor Rev. 2012; 23:357–65. 10.1016/j.cytogfr.2012.06.004 [DOI] [PubMed] [Google Scholar]
- 48.Ricci A, Greco S, Mariotta S, Felici L, Bronzetti E, Cavazzana A, Cardillo G, Amenta F, Bisetti A, Barbolini G. Neurotrophins and neurotrophin receptors in human lung cancer. Am J Respir Cell Mol Biol. 2001; 25:439–46. 10.1165/ajrcmb.25.4.4470 [DOI] [PubMed] [Google Scholar]
- 49.Tacconelli A, Farina AR, Cappabianca L, Desantis G, Tessitore A, Vetuschi A, Sferra R, Rucci N, Argenti B, Screpanti I, Gulino A, Mackay AR. TrkA alternative splicing: a regulated tumor-promoting switch in human neuroblastoma. Cancer Cell. 2004; 6:347–60. 10.1016/j.ccr.2004.09.011 [DOI] [PubMed] [Google Scholar]
- 50.Vaishnavi A, Le AT, Doebele RC. TRKing down an old oncogene in a new era of targeted therapy. Cancer Discov. 2015; 5:25–34. 10.1158/2159-8290.CD-14-0765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Drilon A, Laetsch TW, Kummar S, DuBois SG, Lassen UN, Demetri GD, Nathenson M, Doebele RC, Farago AF, Pappo AS, Turpin B, Dowlati A, Brose MS, et al. Efficacy of Larotrectinib in TRK Fusion-Positive Cancers in Adults and Children. N Engl J Med. 2018; 378:731–39. 10.1056/NEJMoa1714448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Doebele RC, Davis LE, Vaishnavi A, Le AT, Estrada-Bernal A, Keysar S, Jimeno A, Varella-Garcia M, Aisner DL, Li Y, Stephens PJ, Morosini D, Tuch BB, et al. An Oncogenic NTRK Fusion in a Patient with Soft-Tissue Sarcoma with Response to the Tropomyosin-Related Kinase Inhibitor LOXO-101. Cancer Discov. 2015; 5:1049–57. 10.1158/2159-8290.CD-15-0443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gao F, Griffin N, Faulkner S, Rowe CW, Williams L, Roselli S, Thorne RF, Ferdoushi A, Jobling P, Walker MM, Hondermarck H. The neurotrophic tyrosine kinase receptor TrkA and its ligand NGF are increased in squamous cell carcinomas of the lung. Sci Rep. 2018; 8:8135. 10.1038/s41598-018-26408-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wu G, Diaz AK, Paugh BS, Rankin SL, Ju B, Li Y, Zhu X, Qu C, Chen X, Zhang J, Easton J, Edmonson M, Ma X, et al. The genomic landscape of diffuse intrinsic pontine glioma and pediatric non-brainstem high-grade glioma. Nat Genet. 2014; 46:444–50. 10.1038/ng.2938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Smit MA, Peeper DS. Zeb1 is required for TrkB-induced epithelial-mesenchymal transition, anoikis resistance and metastasis. Oncogene. 2011; 30:3735–44. 10.1038/onc.2011.96 [DOI] [PubMed] [Google Scholar]
- 56.Luo Y, Kaz AM, Kanngurn S, Welsch P, Morris SM, Wang J, Lutterbaugh JD, Markowitz SD, Grady WM. NTRK3 is a potential tumor suppressor gene commonly inactivated by epigenetic mechanisms in colorectal cancer. PLoS Genet. 2013; 9:e1003552. 10.1371/journal.pgen.1003552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Okumura T, Shimada Y, Imamura M, Yasumoto S. Neurotrophin receptor p75(NTR) characterizes human esophageal keratinocyte stem cells in vitro. Oncogene. 2003; 22:4017–26. 10.1038/sj.onc.1206525 [DOI] [PubMed] [Google Scholar]
- 58.Okumura T, Tsunoda S, Mori Y, Ito T, Kikuchi K, Wang TC, Yasumoto S, Shimada Y. The biological role of the low-affinity p75 neurotrophin receptor in esophageal squamous cell carcinoma. Clin Cancer Res. 2006; 12:5096–103. 10.1158/1078-0432.CCR-05-2852 [DOI] [PubMed] [Google Scholar]
- 59.Huang SD, Yuan Y, Liu XH, Gong DJ, Bai CG, Wang F, Luo JH, Xu ZY. Self-renewal and chemotherapy resistance of p75NTR positive cells in esophageal squamous cell carcinomas. BMC Cancer. 2009; 9:9. 10.1186/1471-2407-9-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jin H, Pan Y, Zhao L, Zhai H, Li X, Sun L, He L, Chen Y, Hong L, Du Y, Fan D. p75 neurotrophin receptor suppresses the proliferation of human gastric cancer cells. Neoplasia. 2007; 9:471–78. 10.1593/neo.07175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yuanlong H, Haifeng J, Xiaoyin Z, Jialin S, Jie L, Li Y, Huahong X, Jiugang S, Yanglin P, Kaichun W, Jie D, Daiming F. The inhibitory effect of p75 neurotrophin receptor on growth of human hepatocellular carcinoma cells. Cancer Lett. 2008; 268:110–19. 10.1016/j.canlet.2008.03.038 [DOI] [PubMed] [Google Scholar]
- 62.Pundavela J, Demont Y, Jobling P, Lincz LF, Roselli S, Thorne RF, Bond D, Bradshaw RA, Walker MM, Hondermarck H. ProNGF correlates with Gleason score and is a potential driver of nerve infiltration in prostate cancer. Am J Pathol. 2014; 184:3156–62. 10.1016/j.ajpath.2014.08.009 [DOI] [PubMed] [Google Scholar]
- 63.Skaper SD. The neurotrophin family of neurotrophic factors: an overview. Methods Mol Biol. 2012; 846:1–12. 10.1007/978-1-61779-536-7_1 [DOI] [PubMed] [Google Scholar]
- 64.Chao MV, Rajagopal R, Lee FS. Neurotrophin signalling in health and disease. Clin Sci (Lond). 2006; 110:167–73. 10.1042/CS20050163 [DOI] [PubMed] [Google Scholar]
- 65.Chao MV. Neurotrophins and their receptors: a convergence point for many signalling pathways. Nat Rev Neurosci. 2003; 4:299–309. 10.1038/nrn1078 [DOI] [PubMed] [Google Scholar]
- 66.Bradshaw RA, Pundavela J, Biarc J, Chalkley RJ, Burlingame AL, Hondermarck H. NGF and ProNGF: regulation of neuronal and neoplastic responses through receptor signaling. Adv Biol Regul. 2015; 58:16–27. 10.1016/j.jbior.2014.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Demont Y, Corbet C, Page A, Ataman-Önal Y, Choquet-Kastylevsky G, Fliniaux I, Le Bourhis X, Toillon RA, Bradshaw RA, Hondermarck H. Pro-nerve growth factor induces autocrine stimulation of breast cancer cell invasion through tropomyosin-related kinase A (TrkA) and sortilin protein. J Biol Chem. 2012; 287:1923–31. 10.1074/jbc.M110.211714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tomellini E, Touil Y, Lagadec C, Julien S, Ostyn P, Ziental-Gelus N, Meignan S, Lengrand J, Adriaenssens E, Polakowska R, Le Bourhis X. Nerve growth factor and proNGF simultaneously promote symmetric self-renewal, quiescence, and epithelial to mesenchymal transition to enlarge the breast cancer stem cell compartment. Stem Cells. 2015; 33:342–53. 10.1002/stem.1849 [DOI] [PubMed] [Google Scholar]
- 69.Verbeke S, Tomellini E, Dhamani F, Meignan S, Adriaenssens E, Xuefen B. Extracellular cleavage of the p75 neurotrophin receptor is implicated in its pro-survival effect in breast cancer cells. FEBS Lett. 2013; 587:2591–96. 10.1016/j.febslet.2013.06.039 [DOI] [PubMed] [Google Scholar]
- 70.Lawn S, Krishna N, Pisklakova A, Qu X, Fenstermacher DA, Fournier M, Vrionis FD, Tran N, Chan JA, Kenchappa RS, Forsyth PA. Neurotrophin signaling via TrkB and TrkC receptors promotes the growth of brain tumor-initiating cells. J Biol Chem. 2015; 290:3814–24. 10.1074/jbc.M114.599373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yin B, Ma ZY, Zhou ZW, Gao WC, Du ZG, Zhao ZH, Li QQ. The TrkB+ cancer stem cells contribute to post-chemotherapy recurrence of triple-negative breast cancers in an orthotopic mouse model. Oncogene. 2015; 34:761–70. 10.1038/onc.2014.8 [DOI] [PubMed] [Google Scholar]
- 72.Descamps S, Toillon RA, Adriaenssens E, Pawlowski V, Cool SM, Nurcombe V, Le Bourhis X, Boilly B, Peyrat JP, Hondermarck H. Nerve growth factor stimulates proliferation and survival of human breast cancer cells through two distinct signaling pathways. J Biol Chem. 2001; 276:17864–70. 10.1074/jbc.M010499200 [DOI] [PubMed] [Google Scholar]
- 73.Naderi A, Teschendorff AE, Beigel J, Cariati M, Ellis IO, Brenton JD, Caldas C. BEX2 is overexpressed in a subset of primary breast cancers and mediates nerve growth factor/nuclear factor-kappaB inhibition of apoptosis in breast cancer cell lines. Cancer Res. 2007; 67:6725–36. 10.1158/0008-5472.CAN-06-4394 [DOI] [PubMed] [Google Scholar]
- 74.Lagadec C, Meignan S, Adriaenssens E, Foveau B, Vanhecke E, Romon R, Toillon RA, Oxombre B, Hondermarck H, Le Bourhis X. TrkA overexpression enhances growth and metastasis of breast cancer cells. Oncogene. 2009; 28:1960–70. 10.1038/onc.2009.61 [DOI] [PubMed] [Google Scholar]
- 75.Ruggeri P, Farina AR, Di Ianni N, Cappabianca L, Ragone M, Ianni G, Gulino A, Mackay AR. The TrkAIII oncoprotein inhibits mitochondrial free radical ROS-induced death of SH-SY5Y neuroblastoma cells by augmenting SOD2 expression and activity at the mitochondria, within the context of a tumour stem cell-like phenotype. PLoS One. 2014; 9:e94568. 10.1371/journal.pone.0094568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Forsyth PA, Krishna N, Lawn S, Valadez JG, Qu X, Fenstermacher DA, Fournier M, Potthast L, Chinnaiyan P, Gibney GT, Zeinieh M, Barker PA, Carter BD, et al. p75 neurotrophin receptor cleavage by α- and γ-secretases is required for neurotrophin-mediated proliferation of brain tumor-initiating cells. J Biol Chem. 2014; 289:8067–85. 10.1074/jbc.M113.513762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Johnston AL, Lun X, Rahn JJ, Liacini A, Wang L, Hamilton MG, Parney IF, Hempstead BL, Robbins SM, Forsyth PA, Senger DL. The p75 neurotrophin receptor is a central regulator of glioma invasion. PLoS Biol. 2007; 5:e212. 10.1371/journal.pbio.0050212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Aubert L, Guilbert M, Corbet C, Génot E, Adriaenssens E, Chassat T, Bertucci F, Daubon T, Magné N, Le Bourhis X, Toillon RA. NGF-induced TrkA/CD44 association is involved in tumor aggressiveness and resistance to lestaurtinib. Oncotarget. 2015; 6:9807–19. 10.18632/oncotarget.3227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yamaguchi T, Okumura T, Hirano K, Watanabe T, Nagata T, Shimada Y, Tsukada K. p75 neurotrophin receptor expression is a characteristic of the mitotically quiescent cancer stem cell population present in esophageal squamous cell carcinoma. Int J Oncol. 2016; 48:1943–54. 10.3892/ijo.2016.3432 [DOI] [PubMed] [Google Scholar]
- 80.Okumura T, Yamaguchi T, Watanabe T, Nagata T, Shimada Y. Clinical Relevance of a Candidate Stem Cell Marker, p75 Neurotrophin Receptor (p75NTR) Expression in Circulating Tumor Cells. Adv Exp Med Biol. 2017; 994:247–54. 10.1007/978-3-319-55947-6_13 [DOI] [PubMed] [Google Scholar]
- 81.Carter BD, Kaltschmidt C, Kaltschmidt B, Offenhäuser N, Böhm-Matthaei R, Baeuerle PA, Barde YA. Selective activation of NF-kappa B by nerve growth factor through the neurotrophin receptor p75. Science. 1996; 272:542–45. 10.1126/science.272.5261.542 [DOI] [PubMed] [Google Scholar]
- 82.Aloyz RS, Bamji SX, Pozniak CD, Toma JG, Atwal J, Kaplan DR, Miller FD. p53 is essential for developmental neuron death as regulated by the TrkA and p75 neurotrophin receptors. J Cell Biol. 1998; 143:1691–703. 10.1083/jcb.143.6.1691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tomellini E, Lagadec C, Polakowska R, Le Bourhis X. Role of p75 neurotrophin receptor in stem cell biology: more than just a marker. Cell Mol Life Sci. 2014; 71:2467–81. 10.1007/s00018-014-1564-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Redmer T, Welte Y, Behrens D, Fichtner I, Przybilla D, Wruck W, Yaspo ML, Lehrach H, Schäfer R, Regenbrecht CR. The nerve growth factor receptor CD271 is crucial to maintain tumorigenicity and stem-like properties of melanoma cells. PLoS One. 2014; 9:e92596. 10.1371/journal.pone.0092596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chang WW, Lin RJ, Yu J, Chang WY, Fu CH, Lai A, Yu JC, Yu AL. The expression and significance of insulin-like growth factor-1 receptor and its pathway on breast cancer stem/progenitors. Breast Cancer Res. 2013; 15:R39. 10.1186/bcr3423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Leong HS, Chong FT, Sew PH, Lau DP, Wong BH, Teh BT, Tan DS, Iyer NG. Targeting cancer stem cell plasticity through modulation of epidermal growth factor and insulin-like growth factor receptor signaling in head and neck squamous cell cancer. Stem Cells Transl Med. 2014; 3:1055–65. 10.5966/sctm.2013-0214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zhang ZJ, Yuan J, Bi Y, Wang C, Liu Y. The effect of metformin on biomarkers and survivals for breast cancer- a systematic review and meta-analysis of randomized clinical trials. Pharmacol Res. 2019; 141:551–55. 10.1016/j.phrs.2019.01.036 [DOI] [PubMed] [Google Scholar]
- 88.Malaguarnera R, Belfiore A. The emerging role of insulin and insulin-like growth factor signaling in cancer stem cells. Front Endocrinol (Lausanne). 2014; 5:10. 10.3389/fendo.2014.00010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sposato V, Canu N, Fico E, et al. The Medial Septum Is Insulin Resistant in the AD Presymptomatic Phase: Rescue by Nerve Growth Factor-Driven IRS1 Activation. Mol Neurobiol. 2019; 58:535–52 10.1007/s12035-018-1038-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Geetha T, Rege SD, Mathews SE, Meakin SO, White MF, Babu JR. Nerve growth factor receptor TrkA, a new receptor in insulin signaling pathway in PC12 cells. J Biol Chem. 2013; 288:23807–13. 10.1074/jbc.M112.436279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Miranda C, Greco A, Miele C, Pierotti MA, Van Obberghen E. IRS-1 and IRS-2 are recruited by TrkA receptor and oncogenic TRK-T1. J Cell Physiol. 2001; 186:35–46. [DOI] [PubMed] [Google Scholar]
- 92.Saucier C, Papavasiliou V, Palazzo A, Naujokas MA, Kremer R, Park M. Use of signal specific receptor tyrosine kinase oncoproteins reveals that pathways downstream from Grb2 or Shc are sufficient for cell transformation and metastasis. Oncogene. 2002; 21:1800–11. 10.1038/sj.onc.1205261 [DOI] [PubMed] [Google Scholar]
- 93.Pomerleau V, Landry M, Bernier J, Vachon PH, Saucier C. Met receptor-induced Grb2 or Shc signals both promote transformation of intestinal epithelial cells, albeit they are required for distinct oncogenic functions. BMC Cancer. 2014; 14:240. 10.1186/1471-2407-14-240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.De Craene B, Berx G. Regulatory networks defining EMT during cancer initiation and progression. Nat Rev Cancer. 2013; 13:97–110. 10.1038/nrc3447 [DOI] [PubMed] [Google Scholar]
- 95.Wislet S, Vandervelden G, Rogister B. From Neural Crest Development to Cancer and Vice Versa: How p75NTR and (Pro)neurotrophins Could Act on Cell Migration and Invasion? Front Mol Neurosci. 2018; 11:244. 10.3389/fnmol.2018.00244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Smit MA, Geiger TR, Song JY, Gitelman I, Peeper DS. A Twist-Snail axis critical for TrkB-induced epithelial-mesenchymal transition-like transformation, anoikis resistance, and metastasis. Mol Cell Biol. 2009; 29:3722–37. 10.1128/MCB.01164-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gomez DR, Byers LA, Nilsson M, Diao L, Wang J, Li L, Tong P, Hofstad M, Saigal B, Wistuba I, Kalhor N, Swisher S, Fan Y, et al. Integrative proteomic and transcriptomic analysis provides evidence for TrkB (NTRK2) as a therapeutic target in combination with tyrosine kinase inhibitors for non-small cell lung cancer. Oncotarget. 2018; 9:14268–84. 10.18632/oncotarget.24361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Jiang L, Wang Z, Liu C, Gong Z, Yang Y, Kang H, Li Y, Hu G. TrkB promotes laryngeal cancer metastasis via activation PI3K/AKT pathway. Oncotarget. 2017; 8:108726–37. 10.18632/oncotarget.21711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ricci A, De Vitis C, Noto A, Fattore L, Mariotta S, Cherubini E, Roscilli G, Liguori G, Scognamiglio G, Rocco G, Botti G, Giarnieri E, Giovagnoli MR, et al. TrkB is responsible for EMT transition in malignant pleural effusions derived cultures from adenocarcinoma of the lung. Cell Cycle. 2013; 12:1696–703. 10.4161/cc.24759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Fan YL, Zheng M, Tang YL, Liang XH. A new perspective of vasculogenic mimicry: EMT and cancer stem cells (Review). Oncol Lett. 2013; 6:1174–80. 10.3892/ol.2013.1555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Tomasetti M, Lee W, Santarelli L, Neuzil J. Exosome-derived microRNAs in cancer metabolism: possible implications in cancer diagnostics and therapy. Exp Mol Med. 2017; 49:e285. 10.1038/emm.2016.153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Nico B, Mangieri D, Benagiano V, Crivellato E, Ribatti D. Nerve growth factor as an angiogenic factor. Microvasc Res. 2008; 75:135–41. 10.1016/j.mvr.2007.07.004 [DOI] [PubMed] [Google Scholar]
- 103.Kermani P, Hempstead B. Brain-derived neurotrophic factor: a newly described mediator of angiogenesis. Trends Cardiovasc Med. 2007; 17:140–43. 10.1016/j.tcm.2007.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Blais M, Lévesque P, Bellenfant S, Berthod F. Nerve growth factor, brain-derived neurotrophic factor, neurotrophin-3 and glial-derived neurotrophic factor enhance angiogenesis in a tissue-engineered in vitro model. Tissue Eng Part A. 2013; 19:1655–64. 10.1089/ten.tea.2012.0745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Romon R, Adriaenssens E, Lagadec C, Germain E, Hondermarck H, Le Bourhis X. Nerve growth factor promotes breast cancer angiogenesis by activating multiple pathways. Mol Cancer. 2010; 9:157. 10.1186/1476-4598-9-157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Vera C, Tapia V, Vega M, Romero C. Role of nerve growth factor and its TRKA receptor in normal ovarian and epithelial ovarian cancer angiogenesis. J Ovarian Res. 2014; 7:82. 10.1186/s13048-014-0082-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kishibe K, Yamada Y, Ogawa K. Production of nerve growth factor by mouse hepatocellular carcinoma cells and expression of TrkA in tumor-associated arteries in mice. Gastroenterology. 2002; 122:1978–86. 10.1053/gast.2002.33581 [DOI] [PubMed] [Google Scholar]
- 108.Ceyhan GO, Liebl F, Maak M, Schuster T, Becker K, Langer R, Demir IE, Hartel M, Friess H, Rosenberg R. The severity of neural invasion is a crucial prognostic factor in rectal cancer independent of neoadjuvant radiochemotherapy. Ann Surg. 2010; 252:797–804. 10.1097/SLA.0b013e3181fcab8d [DOI] [PubMed] [Google Scholar]
- 109.Albo D, Akay CL, Marshall CL, Wilks JA, Verstovsek G, Liu H, Agarwal N, Berger DH, Ayala GE. Neurogenesis in colorectal cancer is a marker of aggressive tumor behavior and poor outcomes. Cancer. 2011; 117:4834–45. 10.1002/cncr.26117 [DOI] [PubMed] [Google Scholar]
- 110.Deng J, You Q, Gao Y, Yu Q, Zhao P, Zheng Y, Fang W, Xu N, Teng L. Prognostic value of perineural invasion in gastric cancer: a systematic review and meta-analysis. PLoS One. 2014; 9:e88907. 10.1371/journal.pone.0088907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ayala GE, Dai H, Ittmann M, Li R, Powell M, Frolov A, Wheeler TM, Thompson TC, Rowley D. Growth and survival mechanisms associated with perineural invasion in prostate cancer. Cancer Res. 2004; 64:6082–90. 10.1158/0008-5472.CAN-04-0838 [DOI] [PubMed] [Google Scholar]
- 112.Chen JW, Xie JD, Ling YH, Li P, Yan SM, Xi SY, Luo RZ, Yun JP, Xie D, Cai MY. The prognostic effect of perineural invasion in esophageal squamous cell carcinoma. BMC Cancer. 2014; 14:313. 10.1186/1471-2407-14-313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Mancino M, Ametller E, Gascón P, Almendro V. The neuronal influence on tumor progression. Biochim Biophys Acta. 2011; 1816:105–18. 10.1016/j.bbcan.2011.04.005 [DOI] [PubMed] [Google Scholar]
- 114.Ayala GE, Wheeler TM, Shine HD, Schmelz M, Frolov A, Chakraborty S, Rowley D. In vitro dorsal root ganglia and human prostate cell line interaction: redefining perineural invasion in prostate cancer. Prostate. 2001; 49:213–23. 10.1002/pros.1137 [DOI] [PubMed] [Google Scholar]
- 115.De Sousa Pereira A. A basis for sympathectomy for cancer of the cervix uteri. Arch Surg. 1946; 52:260–85. 10.1001/archsurg.1946.01230050265003 [DOI] [PubMed] [Google Scholar]
- 116.Barnbrook DH. Pheochromocytoma; an alternative surgical approach. Can Med Assoc J. 1953; 68:245–47. [PMC free article] [PubMed] [Google Scholar]
- 117.Batkin S, Piette LH, Wildman E. Effect of muscle denervation on growth of transplanted tumor in mice. Proc Natl Acad Sci USA. 1970; 67:1521–27. 10.1073/pnas.67.3.1521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Dollé L, Adriaenssens E, El Yazidi-Belkoura I, Le Bourhis X, Nurcombe V, Hondermarck H. Nerve growth factor receptors and signaling in breast cancer. Curr Cancer Drug Targets. 2004; 4:463–70. 10.2174/1568009043332853 [DOI] [PubMed] [Google Scholar]
- 119.Weeraratna AT, Dalrymple SL, Lamb JC, Denmeade SR, Miknyoczki S, Dionne CA, Isaacs JT. Pan-trk inhibition decreases metastasis and enhances host survival in experimental models as a result of its selective induction of apoptosis of prostate cancer cells. Clin Cancer Res. 2001; 7:2237–45. [PubMed] [Google Scholar]
- 120.Bixby JL, Harris WA. Molecular mechanisms of axon growth and guidance. Annu Rev Cell Biol. 1991; 7:117–59. 10.1146/annurev.cb.07.110191.001001 [DOI] [PubMed] [Google Scholar]
- 121.Latil A, Chêne L, Cochant-Priollet B, Mangin P, Fournier G, Berthon P, Cussenot O. Quantification of expression of netrins, slits and their receptors in human prostate tumors. Int J Cancer. 2003; 103:306–15. 10.1002/ijc.10821 [DOI] [PubMed] [Google Scholar]
- 122.Bapat AA, Hostetter G, Von Hoff DD, Han H. Perineural invasion and associated pain in pancreatic cancer. Nat Rev Cancer. 2011; 11:695–707. 10.1038/nrc3131 [DOI] [PubMed] [Google Scholar]
- 123.Liebig C, Ayala G, Wilks JA, Berger DH, Albo D. Perineural invasion in cancer: a review of the literature. Cancer. 2009; 115:3379–91. 10.1002/cncr.24396 [DOI] [PubMed] [Google Scholar]
- 124.Stopczynski RE, Normolle DP, Hartman DJ, Ying H, DeBerry JJ, Bielefeldt K, Rhim AD, DePinho RA, Albers KM, Davis BM. Neuroplastic changes occur early in the development of pancreatic ductal adenocarcinoma. Cancer Res. 2014; 74:1718–27. 10.1158/0008-5472.CAN-13-2050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zhao CM, Hayakawa Y, Kodama Y, Muthupalani S, Westphalen CB, Andersen GT, Flatberg A, Johannessen H, Friedman RA, Renz BW, Sandvik AK, Beisvag V, Tomita H, et al. Denervation suppresses gastric tumorigenesis. Sci Transl Med. 2014; 6:250ra115. 10.1126/scitranslmed.3009569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Venkatesh HS, Johung TB, Caretti V, Noll A, Tang Y, Nagaraja S, Gibson EM, Mount CW, Polepalli J, Mitra SS, Woo PJ, Malenka RC, Vogel H, et al. Neuronal Activity Promotes Glioma Growth through Neuroligin-3 Secretion. Cell. 2015; 161:803–16. 10.1016/j.cell.2015.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Shin VY, Jin HC, Ng EK, Cho CH, Leung WK, Sung JJ, Chu KM. 4-(Methylnitrosamino)-1-(3-pyridyl)-1-butanone promoted gastric cancer growth through prostaglandin E receptor (EP2 and EP4) in vivo and in vitro. Cancer Sci. 2011; 102:926–33. 10.1111/j.1349-7006.2011.01885.x [DOI] [PubMed] [Google Scholar]
- 128.Wen J, Fu JH, Zhang W, Guo M. Lung carcinoma signaling pathways activated by smoking. Chin J Cancer. 2011; 30:551–58. 10.5732/cjc.011.10059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.da Penha Berzaghi M, Cooper J, Castrén E, Zafra F, Sofroniew M, Thoenen H, Lindholm D. Cholinergic regulation of brain-derived neurotrophic factor (BDNF) and nerve growth factor (NGF) but not neurotrophin-3 (NT-3) mRNA levels in the developing rat hippocampus. J Neurosci. 1993; 13:3818–26. 10.1523/JNEUROSCI.13-09-03818.1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Knipper M, da Penha Berzaghi M, Blöchl A, Breer H, Thoenen H, Lindholm D. Positive feedback between acetylcholine and the neurotrophins nerve growth factor and brain-derived neurotrophic factor in the rat hippocampus. Eur J Neurosci. 1994; 6:668–71. 10.1111/j.1460-9568.1994.tb00312.x [DOI] [PubMed] [Google Scholar]
- 131.Auld DS, Mennicken F, Day JC, Quirion R. Neurotrophins differentially enhance acetylcholine release, acetylcholine content and choline acetyltransferase activity in basal forebrain neurons. J Neurochem. 2001; 77:253–62. [DOI] [PubMed] [Google Scholar]
- 132.Renz BW, Takahashi R, Tanaka T, Macchini M, Hayakawa Y, Dantes Z, Maurer HC, Chen X, Jiang Z, Westphalen CB, Ilmer M, Valenti G, Mohanta SK, et al. β2 Adrenergic-Neurotrophin Feedforward Loop Promotes Pancreatic Cancer. Cancer Cell. 2018; 33:75–90.e7. 10.1016/j.ccell.2017.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Song P, Sekhon HS, Lu A, Arredondo J, Sauer D, Gravett C, Mark GP, Grando SA, Spindel ER. M3 muscarinic receptor antagonists inhibit small cell lung carcinoma growth and mitogen-activated protein kinase phosphorylation induced by acetylcholine secretion. Cancer Res. 2007; 67:3936–44. 10.1158/0008-5472.CAN-06-2484 [DOI] [PubMed] [Google Scholar]
- 134.Ayala GE, Dai H, Powell M, Li R, Ding Y, Wheeler TM, Shine D, Kadmon D, Thompson T, Miles BJ, Ittmann MM, Rowley D. Cancer-related axonogenesis and neurogenesis in prostate cancer. Clin Cancer Res. 2008; 14:7593–603. 10.1158/1078-0432.CCR-08-1164 [DOI] [PubMed] [Google Scholar]
- 135.Kosaka N, Yoshioka Y, Fujita Y, Ochiya T. Versatile roles of extracellular vesicles in cancer. J Clin Invest. 2016; 126:1163–72. 10.1172/JCI81130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Madeo M, Colbert PL, Vermeer DW, Lucido CT, Cain JT, Vichaya EG, Grossberg AJ, Muirhead D, Rickel AP, Hong Z, Zhao J, Weimer JM, Spanos WC, et al. Cancer exosomes induce tumor innervation. Nat Commun. 2018; 9:4284. 10.1038/s41467-018-06640-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Plebanek MP, Angeloni NL, Vinokour E, Li J, Henkin A, Martinez-Marin D, Filleur S, Bhowmick R, Henkin J, Miller SD, Ifergan I, Lee Y, Osman I, et al. Pre-metastatic cancer exosomes induce immune surveillance by patrolling monocytes at the metastatic niche. Nat Commun. 2017; 8:1319. 10.1038/s41467-017-01433-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Escudero CA, Lazo OM, Galleguillos C, Parraguez JI, Lopez-Verrilli MA, Cabeza C, Leon L, Saeed U, Retamal C, Gonzalez A, Marzolo MP, Carter BD, Court FA, Bronfman FC. The p75 neurotrophin receptor evades the endolysosomal route in neuronal cells, favouring multivesicular bodies specialised for exosomal release. J Cell Sci. 2014; 127:1966–79. 10.1242/jcs.141754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Hikita T, Kuwahara A, Watanabe R, Miyata M, Oneyama C. Src in endosomal membranes promotes exosome secretion and tumor progression. Sci Rep. 2019; 9:3265. 10.1038/s41598-019-39882-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.DeRita RM, Zerlanko B, Singh A, Lu H, Iozzo RV, Benovic JL, Languino LR. c-Src, Insulin-Like Growth Factor I Receptor, G-Protein-Coupled Receptor Kinases and Focal Adhesion Kinase are Enriched Into Prostate Cancer Cell Exosomes. J Cell Biochem. 2017; 118:66–73. 10.1002/jcb.25611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Pinet S, Bessette B, Vedrenne N, Lacroix A, Richard L, Jauberteau MO, Battu S, Lalloué F. TrkB-containing exosomes promote the transfer of glioblastoma aggressiveness to YKL-40-inactivated glioblastoma cells. Oncotarget. 2016; 7:50349–64. 10.18632/oncotarget.10387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Hardin H, Helein H, Meyer K, Robertson S, Zhang R, Zhong W, Lloyd RV. Thyroid cancer stem-like cell exosomes: regulation of EMT via transfer of lncRNAs. Lab Invest. 2018; 98:1133–42. 10.1038/s41374-018-0065-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Li H, Li F. Exosomes from BM-MSCs increase the population of CSCs via transfer of miR-142-3p. Br J Cancer. 2018; 119:744–55. 10.1038/s41416-018-0254-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Vega JA, García-Suárez O, Hannestad J, Pérez-Pérez M, Germanà A. Neurotrophins and the immune system. J Anat. 2003; 203:1–19. 10.1046/j.1469-7580.2003.00203.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Sariola H. The neurotrophic factors in non-neuronal tissues. Cell Mol Life Sci. 2001; 58:1061–66. 10.1007/PL00000921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Santambrogio L, Benedetti M, Chao MV, Muzaffar R, Kulig K, Gabellini N, Hochwald G. Nerve growth factor production by lymphocytes. J Immunol. 1994; 153:4488–95. [PubMed] [Google Scholar]
- 147.Torcia M, Bracci-Laudiero L, Lucibello M, Nencioni L, Labardi D, Rubartelli A, Cozzolino F, Aloe L, Garaci E. Nerve growth factor is an autocrine survival factor for memory B lymphocytes. Cell. 1996; 85:345–56. 10.1016/S0092-8674(00)81113-7 [DOI] [PubMed] [Google Scholar]
- 148.Ehrhard PB, Erb P, Graumann U, Schmutz B, Otten U. Expression of functional trk tyrosine kinase receptors after T cell activation. J Immunol. 1994; 152:2705–09. [PubMed] [Google Scholar]
- 149.Ehrhard PB, Erb P, Graumann U, Otten U. Expression of nerve growth factor and nerve growth factor receptor tyrosine kinase Trk in activated CD4-positive T-cell clones. Proc Natl Acad Sci USA. 1993; 90:10984–88. 10.1073/pnas.90.23.10984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Tallerico R, Todaro M, Di Franco S, Maccalli C, Garofalo C, Sottile R, Palmieri C, Tirinato L, Pangigadde PN, La Rocca R, Mandelboim O, Stassi G, Di Fabrizio E, et al. Human NK cells selective targeting of colon cancer-initiating cells: a role for natural cytotoxicity receptors and MHC class I molecules. J Immunol. 2013; 190:2381–90. 10.4049/jimmunol.1201542 [DOI] [PubMed] [Google Scholar]
- 151.Pietra G, Manzini C, Vitale M, Balsamo M, Ognio E, Boitano M, Queirolo P, Moretta L, Mingari MC. Natural killer cells kill human melanoma cells with characteristics of cancer stem cells. Int Immunol. 2009; 21:793–801. 10.1093/intimm/dxp047 [DOI] [PubMed] [Google Scholar]
- 152.Castriconi R, Daga A, Dondero A, Zona G, Poliani PL, Melotti A, Griffero F, Marubbi D, Spaziante R, Bellora F, Moretta L, Moretta A, Corte G, Bottino C. NK cells recognize and kill human glioblastoma cells with stem cell-like properties. J Immunol. 2009; 182:3530–39. 10.4049/jimmunol.0802845 [DOI] [PubMed] [Google Scholar]
- 153.Tallerico R, Garofalo C, Carbone E. A New Biological Feature of Natural Killer Cells: The Recognition of Solid Tumor-Derived Cancer Stem Cells. Front Immunol. 2016; 7:179. 10.3389/fimmu.2016.00179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Ralainirina N, Brons NH, Ammerlaan W, Hoffmann C, Hentges F, Zimmer J. Mouse natural killer (NK) cells express the nerve growth factor receptor TrkA, which is dynamically regulated. PLoS One. 2010; 5:e15053–15053. 10.1371/journal.pone.0015053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Jiang Y, Chen G, Zhang Y, Lu L, Liu S, Cao X. Nerve growth factor promotes TLR4 signaling-induced maturation of human dendritic cells in vitro through inducible p75NTR 1. J Immunol. 2007; 179:6297–304. 10.4049/jimmunol.179.9.6297 [DOI] [PubMed] [Google Scholar]
- 156.Lanitis E, Dangaj D, Irving M, Coukos G. Mechanisms regulating T-cell infiltration and activity in solid tumors. Ann Oncol. 2017 (suppl_12); 28:xii18–32. 10.1093/annonc/mdx238 PMID:29045511 [DOI] [PubMed]
- 157.Cassetta L, Pollard JW. Cancer immunosurveillance: role of patrolling monocytes. Cell Res. 2016; 26:3–4. 10.1038/cr.2015.144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Hanna RN, Cekic C, Sag D, Tacke R, Thomas GD, Nowyhed H, Herrley E, Rasquinha N, McArdle S, Wu R, Peluso E, Metzger D, Ichinose H, et al. Patrolling monocytes control tumor metastasis to the lung. Science. 2015; 350:985–90. 10.1126/science.aac9407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Ehrhard PB, Ganter U, Stalder A, Bauer J, Otten U. Expression of functional trk protooncogene in human monocytes. Proc Natl Acad Sci USA. 1993; 90:5423–27. 10.1073/pnas.90.12.5423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Hayday AC. Gammadelta T cells and the lymphoid stress-surveillance response. Immunity. 2009; 31:184–96. 10.1016/j.immuni.2009.08.006 [DOI] [PubMed] [Google Scholar]
- 161.Gentles AJ, Newman AM, Liu CL, Bratman SV, Feng W, Kim D, Nair VS, Xu Y, Khuong A, Hoang CD, Diehn M, West RB, Plevritis SK, Alizadeh AA. The prognostic landscape of genes and infiltrating immune cells across human cancers. Nat Med. 2015; 21:938–45. 10.1038/nm.3909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Copray S, Küst B, Emmer B, Lin MY, Liem R, Amor S, de Vries H, Floris S, Boddeke E. Deficient p75 low-affinity neurotrophin receptor expression exacerbates experimental allergic encephalomyelitis in C57/BL6 mice. J Neuroimmunol. 2004; 148:41–53. 10.1016/j.jneuroim.2003.11.008 [DOI] [PubMed] [Google Scholar]
- 163.Kanehiro A, Lahn M, Mäkelä MJ, Dakhama A, Joetham A, Rha YH, Born W, Gelfand EW. Requirement for the p75 TNF-alpha receptor 2 in the regulation of airway hyperresponsiveness by gamma delta T cells. J Immunol. 2002; 169:4190–97. 10.4049/jimmunol.169.8.4190 [DOI] [PubMed] [Google Scholar]
- 164.Hazenberg MD, Spits H. Human innate lymphoid cells. Blood. 2014; 124:700–09. 10.1182/blood-2013-11-427781 [DOI] [PubMed] [Google Scholar]
- 165.Eberl G, Colonna M, Di Santo JP, McKenzie AN. Innate lymphoid cells. Innate lymphoid cells: a new paradigm in immunology. Science. 2015; 348:aaa6566. 10.1126/science.aaa6566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Bruchard M, Ghiringhelli F. Deciphering the Roles of Innate Lymphoid Cells in Cancer. Front Immunol. 2019; 10:656. 10.3389/fimmu.2019.00656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Vivier E, Artis D, Colonna M, Diefenbach A, Di Santo JP, Eberl G, Koyasu S, Locksley RM, McKenzie AN, Mebius RE, Powrie F, Spits H. Innate Lymphoid Cells: 10 Years On. Cell. 2018; 174:1054–66. 10.1016/j.cell.2018.07.017 [DOI] [PubMed] [Google Scholar]
- 168.Jacquelot N, Luong K, Seillet C. Physiological Regulation of Innate Lymphoid Cells. Front Immunol. 2019; 10:405. 10.3389/fimmu.2019.00405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Chen HC, Joalland N, Bridgeman JS, Alchami FS, Jarry U, Khan MW, Piggott L, Shanneik Y, Li J, Herold MJ, Herrmann T, Price DA, Gallimore AM, et al. Synergistic targeting of breast cancer stem-like cells by human γδ T cells and CD8+ T cells. Immunol Cell Biol. 2017; 95:620–29. 10.1038/icb.2017.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Pajtler KW, Rebmann V, Lindemann M, Schulte JH, Schulte S, Stauder M, Leuschner I, Schmid KW, Köhl U, Schramm A, Eggert A. Expression of NTRK1/TrkA affects immunogenicity of neuroblastoma cells. Int J Cancer. 2013; 133:908–19. 10.1002/ijc.28096 [DOI] [PubMed] [Google Scholar]
- 171.Williams KS, Killebrew DA, Clary GP, Seawell JA, Meeker RB. Differential regulation of macrophage phenotype by mature and pro-nerve growth factor. J Neuroimmunol. 2015; 285:76–93. 10.1016/j.jneuroim.2015.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Ostroumov D, Fekete-Drimusz N, Saborowski M, Kühnel F, Woller N. CD4 and CD8 T lymphocyte interplay in controlling tumor growth. Cell Mol Life Sci. 2018; 75:689–713. 10.1007/s00018-017-2686-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Sato E, Olson SH, Ahn J, Bundy B, Nishikawa H, Qian F, Jungbluth AA, Frosina D, Gnjatic S, Ambrosone C, Kepner J, Odunsi T, Ritter G, et al. Intraepithelial CD8+ tumor-infiltrating lymphocytes and a high CD8+/regulatory T cell ratio are associated with favorable prognosis in ovarian cancer. Proc Natl Acad Sci USA. 2005; 102:18538–43. 10.1073/pnas.0509182102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Perez-Diez A, Joncker NT, Choi K, Chan WF, Anderson CC, Lantz O, Matzinger P. CD4 cells can be more efficient at tumor rejection than CD8 cells. Blood. 2007; 109:5346–54. 10.1182/blood-2006-10-051318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Matsui S, Ahlers JD, Vortmeyer AO, Terabe M, Tsukui T, Carbone DP, Liotta LA, Berzofsky JA. A model for CD8+ CTL tumor immunosurveillance and regulation of tumor escape by CD4 T cells through an effect on quality of CTL. J Immunol. 1999; 163:184–93. [PubMed] [Google Scholar]
- 176.Kim EY, Teh HS. TNF type 2 receptor (p75) lowers the threshold of T cell activation. J Immunol. 2001; 167:6812–20. 10.4049/jimmunol.167.12.6812 [DOI] [PubMed] [Google Scholar]
- 177.Lu L, Barbi J, Pan F. The regulation of immune tolerance by FOXP3. Nat Rev Immunol. 2017; 17:703–17. 10.1038/nri.2017.75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Shi Y, Jin Y, Guo W, Chen L, Liu C, Lv X. Blockage of nerve growth factor modulates T cell responses and inhibits allergic inflammation in a mouse model of asthma. Inflamm Res. 2012; 61:1369–78. 10.1007/s00011-012-0538-3 [DOI] [PubMed] [Google Scholar]
- 179.Minnone G, De Benedetti F, Bracci-Laudiero L. NGF and Its Receptors in the Regulation of Inflammatory Response. Int J Mol Sci. 2017; 18:E1028. 10.3390/ijms18051028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Villoslada P, Hauser SL, Bartke I, Unger J, Heald N, Rosenberg D, Cheung SW, Mobley WC, Fisher S, Genain CP. Human nerve growth factor protects common marmosets against autoimmune encephalomyelitis by switching the balance of T helper cell type 1 and 2 cytokines within the central nervous system. J Exp Med. 2000; 191:1799–806. 10.1084/jem.191.10.1799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Flügel A, Matsumuro K, Neumann H, Klinkert WE, Birnbacher R, Lassmann H, Otten U, Wekerle H. Anti-inflammatory activity of nerve growth factor in experimental autoimmune encephalomyelitis: inhibition of monocyte transendothelial migration. Eur J Immunol. 2001; 31:11–22. [DOI] [PubMed] [Google Scholar]
- 182.Adriaenssens E, Vanhecke E, Saule P, Mougel A, Page A, Romon R, Nurcombe V, Le Bourhis X, Hondermarck H. Nerve growth factor is a potential therapeutic target in breast cancer. Cancer Res. 2008; 68:346–51. 10.1158/0008-5472.CAN-07-1183 [DOI] [PubMed] [Google Scholar]
- 183.Krüttgen A, Schneider I, Weis J. The dark side of the NGF family: neurotrophins in neoplasias. Brain Pathol. 2006; 16:304–10. 10.1111/j.1750-3639.2006.00037.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Jimenez-Andrade JM, Bloom AP, Stake JI, Mantyh WG, Taylor RN, Freeman KT, Ghilardi JR, Kuskowski MA, Mantyh PW. Pathological sprouting of adult nociceptors in chronic prostate cancer-induced bone pain. J Neurosci. 2010; 30:14649–56. 10.1523/JNEUROSCI.3300-10.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]