Abstract
Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis belong to a severe dermatopathic spectrum that includes frequently fatal mucocutaneous manifestations consisting of whole epidermal necrosis and sloughing with bullous transformation, blistering, and further skin detachment. Notably, cancer patients are at higher risk of developing SJS than the general population as a consequence of both the nature of neoplastic disease and frequent exposure to anticancer drugs. Ribociclib is a newly approved cycline-dependent kinase inhibitor that has been recently associated with a single case of SJS. We hereby present a case of ribociclib-related SJS. Early detection of threatening skin lesions is crucial to permit the immediate discontinuation of ribociclib given the predictable and unacceptable risk level. In cases of established SJS, early aggressive support should be initiated, ribociclib should be abruptly discontinued, and specific treatment based on actual evidence should be started.
Keywords: Cycline-dependent kinase inhibitor, Ribociclib, Skin toxicity, Stevens-Johnson syndrome, Toxic epidermal necrolysis
INTRODUCTION
Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) represent a life-threatening condition defined by immune-mediated skin injury resulting in whole epidermal necrosis with subsequent skin sloughing and further detachment. This leads to extensive skin barrier loss, fluid extravasation, dehydration, and, eventually, multi-organ failure and death. Both entities belong to a continuum that is arbitrarily defined by an injury extension along the total body surface of less than 10% in SJS and greater than 30% in TEN. Mortality is proportionally related to the percentage of affected area, which has reached up to > 40% in a case series on TEN [1,2].
Ribociclib is a newly approved cycline-dependent kinase 4 and 6 (CDK 4/6) inhibitor used in the setting of locally advanced or metastatic hormone-dependent and Her2-negative breast cancer. Thus far, 2 main cases of the SJS spectrum related to the CDK 4/6 inhibitors ribociclib and palbociclib have been reported [3,4]. We hereby present a second case of SJS related to ribociclib that started with mild cutaneous irritation with subacute worsening and final spread. Grade 1 skin rash is a common ribociclib-related adverse event that occurs in up to 17% of patients taking ribociclib [5]. However, the acute onset of blistering skin lesions, regardless of their extension, should prompt awareness of their potential severity and lead to the immediate discontinuation of the drug and further dermatological assessment, as well as close follow-up.
CASE REPORT
We present the case of a 77-year-old woman who presented to the ER complaining of subacute onset of rapidly evolving skin lesions. Past medical history was remarkable for locally advanced right breast infiltrating lobular carcinoma, with a primary mass measuring up to 10 cm (cT3) and positive lymph node involvement (N3 for ipsilateral supraclavicular nodes). Pathology revealed 100% estrogen receptor expression and negative Her2 amplification with histological characteristics of the luminal A phenotype. Given the non-resectable nature of a locally advanced tumor, the patient was started on ribociclib and letrozol, which were started 4 months prior to the onset of the chief complaint. The patient was not taking any other medication.
At the first examination 3 weeks prior to the clinical development, the patient reported a new onset of symmetric erythematous plaques along the extensor surface of both upper limbs with further development of tender and brittle lesions with spontaneous sloughing and bleeding. At that time, skin biopsies were obtained, and the patient was put on topical corticosteroids and discharged home. At the time of the next examination, the skin lesions had rapidly relapsed during the past 72 hours and involved the face and lips, both upper and lower limbs, the chest, the back, and the gluteal and perianal regions. She reported a fever of up to 38.8°C and intense pain associated with the skin blisters. She also reported mouth pain and dysphagia. She denied herpetiform lesions prior to the onset of symptoms. No use of new medications or other substances was reported.
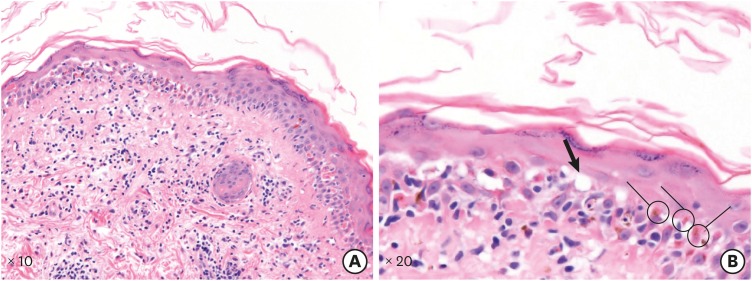
On physical examination, the patient was clearly experiencing pain and discomfort. She had coalescing erythematous maculae, some of which presented with central purpuric lesions along the whole back area and chest, as well as symmetric and bilaterally evolving lesions on both upper and lower limbs (Figure 1). The scalp, palms, and soles seemed to have been spared. Tender and disrupted lesions with active necrohemorrhagic exudate were identified within the extensor surface of both upper limbs with symmetric distribution, as well as on the lips, preauricular area, ear scaphae, gluteal and perianal areas, and shoulders (Figure 1). Approximately > 20% of the total body surface was affected, which was consistent with grade 4 skin involvement following the Common Terminology Criteria for Adverse Events v5.0) classification. The Nikolsky sign appeared positive with spontaneous detachment of the healthy skin surrounding the lesion. The mucous membranes were spared, although local candidiasis was identified. Blood testing showed toxic pancytopenia and a normal eosinophil count.
Figure 1. Image shows coalescing erythematous maculae along whole dorsal (A) aspect and chest as well as symmetric and bilaterally evolving lesions on both upper and lower limbs (B, C). Active exudative bleeding was identified within the extensor surface of both upper limbs (B, C), lips (D), preauricular area, ear scaphae (E), and shoulders (F).
Given the suspicion of ribociclib-mediated SJS, the patient was started on aggressive intravenous fluid therapy. A single dose of 40 mg subcutaneous etanercept was administered, and the patient was started on daily cyclosporine at 4 mg/kg. She was admitted to the inpatient burn unit for further support.
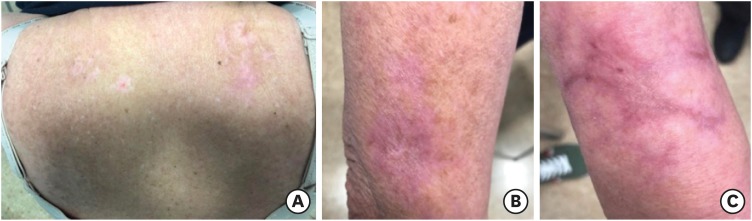
Skin biopsies obtained at the first evaluation, 3 weeks prior to the acute worsening of the lesions, showed vacuolar degeneration of the dermo-epidermal junction with scattered apoptotic keratinocytes (Figure 2). The specimen also revealed dense perivascular infiltration of mononuclear cells within an edematous papillary dermis.
Figure 2. Image shows hematoxylin and eosin stain staining of skin specimen (A, B) showing vacuolar degeneration of the dermo-epidermal junction (B, full arrow) with abundant images of apoptotic keratinocytes (B, circled cells). Specimen did also reveal dense perivascular infiltration of mononuclear cells within an edematous papillary dermis.
Intensive Care Unit care was mandatory during the first 6 days of inpatient admission given the very early decline of the hemodynamic status. During admission to the burn unit, the patient experienced early worsening with acute renal failure, which improved after aggressive intravenous fluid replacement without further need for a vasoactive intravenous drug regimen. On the 4th day of burn unit admission, the patient presented with a fever of 38.5°C, for which empirical antibiotics based on glomerular filtration rate-adjusted meropenem and vancomycin were started. Blood cultures and urinalysis as well as the chest X-ray and electrocardiogram studies all appeared normal. Her febrile status resolved within 24 hours, and the antibiotic regimen was withdrawn after completion of a 14 day-course. At the 6th day of inpatient admission, the patient was admitted at the oncology inpatient unit and further medical stabilization was needed with close monitoring of her skin care and rehabilitation. The patient progressively experienced full re-epithelization of the skin lesions with residual hypopigmented scarring within the healed areas (Figure 3). Ribociclib was definitively discontinued.
Figure 3. Image shows full re-epithelization of primary blistering lesions with residual hypopigmentation and scarring along superior dorsal aspect (A) as well as brachial area (B, C).
DISCUSSION
The pathobiology of SJS relies on the direct attack of keratinocytes by immune activation of reactive T-cells and NK, which is primarily mediated by a drug-mediated cross-reactivity with the subsequent triggering of type IV cell-mediated acute toxicity. Extensive apoptosis of keratinocytes induces progressively evolving spongiosis with further detachment of the entire epidermal layer and eventual necrosis. Among the various damage-perpetuating factors that have been studied, granulysin, interleukin 15, Fas ligand, and tumor necrosis factor alpha (TNF-α) have proven to be closely related to that type of hyperimmunity leading to skin disruption. Moreover, genetic variability, particularly that involving human leukocyte antigen polymorphisms, appears to play a role in determining the baseline predisposition to such an event [6].
The primary therapeutic approach is based on aggressive support in burn units with aggressive intravenous fluid replacement along with early detection and the treatment of disease-related complications such as infections and organ failure. The specific use of corticosteroids is controversial, with the latest meta-analysis suggesting a mild tendency toward better outcomes in patients receiving intravenous glucocorticoids, without statistical significance [7]. The use of intravenous immunoglobulins has not shown benefit in terms of either mortality or disease-progression control [7,8]. Most updated literature supports the use of cyclosporine in the early setting of SJS, as it has been proven to reduce overall mortality in patients affected by the SJS spectrum [9,10]. In addition, a recent phase III study assessing the feasibility of the TNF-α inhibitor etanercept showed a significant mortality reduction in the etanercept group compared to the group receiving glucocorticoid-based therapy. Moreover, etanercept has been found to effectively enhance skin and oral mucosa healing, along with aiding the normalization of granulysin and plasma TNF-α levels [11].
As shown in many different studies, oncologic patients are at higher risk of developing severe cutaneous adverse reactions and SJS [12,13,14]. Exposure to anticancer drugs is an independent risk factor for SJS given their intrinsic immunogenic nature. Indeed, the SJS spectrum has been associated with a wide variety of anticancer drugs including alkylating agents, plant alkaloids, anthracyclines, antimetabolites, mustards, and immunomodulatory agents. Lenalidomide, methotrexate, and docetaxel are the drugs most frequently associated with SJS [15].
Herein, we have presented a case of CDK 4/6 inhibitor ribociclib-mediated SJS. The literature published thus far includes 2 different CDK 4/6-related SJS cases [3,4]. We would like to emphasize the importance of the multidisciplinary management of oncologic patients in light of the complexity of their medical condition. General recommendations for the administration of ribociclib in terms of follow-up and scheduling indicate regular visits every 3 weeks, though the question remains whether such a regimen is sufficient for the general oncologic population receiving ribociclib treatment. In our experience, patients with insidious skin toxicity should be more closely followed up to ensure the early identification of any further complications. Given the frequent use of ribociclib in the setting of disseminated breast cancer, the period of time since its commercialization, and the potential for lethal skin complications, which may occur more frequently than anticipated, our goal with the presentation of this case was to raise awareness of the need for closer monitoring of patients on this therapeutic regimen.
Footnotes
Conflict of Interest: The authors declare that they have no competing interests.
- Writing - original draft: López-Gómez V, Yarza R, Muñoz-González H, Revilla E, Enrech S, González-Valle O, Tolosa P, Ciruelos E.
- Writing - review & editing: Yarza R, Ciruelos E.
References
- 1.Stern RS, Divito SJ. Stevens-Johnson syndrome and toxic epidermal necrolysis: associations, outcomes, and pathobiology-thirty years of progress but still much to be done. J Invest Dermatol. 2017;137:1004–1008. doi: 10.1016/j.jid.2017.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sekula P, Dunant A, Mockenhaupt M, Naldi L, Bouwes Bavinck JN, Halevy S, et al. Comprehensive survival analysis of a cohort of patients with Stevens-Johnson syndrome and toxic epidermal necrolysis. J Invest Dermatol. 2013;133:1197–1204. doi: 10.1038/jid.2012.510. [DOI] [PubMed] [Google Scholar]
- 3.Widmer S, Grossman M. Chemotherapy patient with Stevens-Johnson syndrome presents to the emergency department: a case report. Am J Emerg Med. 2018;36:1325.e3–1325.e4. doi: 10.1016/j.ajem.2018.04.019. [DOI] [PubMed] [Google Scholar]
- 4.Karagounis T, Vallurupalli M, Nathan N, Nazarian R, Vedak P, Spring L, et al. Stevens-Johnson syndrome-like eruption from palbociclib in a patient with metastatic breast cancer. JAAD Case Rep. 2018;4:452–454. doi: 10.1016/j.jdcr.2017.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hortobagyi GN, Stemmer SM, Burris HA, Yap YS, Sonke GS, Paluch-Shimon S, et al. Ribociclib as first-line therapy for HR-positive, advanced breast cancer. N Engl J Med. 2016;375:1738–1748. doi: 10.1056/NEJMoa1609709. [DOI] [PubMed] [Google Scholar]
- 6.Harris V, Jackson C, Cooper A. Review of toxic epidermal necrolysis. Int J Mol Sci. 2016;17:E2135. doi: 10.3390/ijms17122135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zimmermann S, Sekula P, Venhoff M, Motschall E, Knaus J, Schumacher M, et al. Systemic immunomodulating therapies for Stevens-Johnson syndrome and toxic epidermal necrolysis: a systematic review and meta-analysis. JAMA Dermatol. 2017;153:514–522. doi: 10.1001/jamadermatol.2016.5668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Faye O, Roujeau JC. Treatment of epidermal necrolysis with high-dose intravenous immunoglobulins (IV Ig): clinical experience to date. Drugs. 2005;65:2085–2090. doi: 10.2165/00003495-200565150-00002. [DOI] [PubMed] [Google Scholar]
- 9.González-Herrada C, Rodríguez-Martín S, Cachafeiro L, Lerma V, González O, Lorente JA, et al. Cyclosporine use in epidermal necrolysis is associated with an important mortality reduction: evidence from three different approaches. J Invest Dermatol. 2017;137:2092–2100. doi: 10.1016/j.jid.2017.05.022. [DOI] [PubMed] [Google Scholar]
- 10.Ng QX, De Deyn ML, Venkatanarayanan N, Ho CY, Yeo WS. A meta-analysis of cyclosporine treatment for Stevens-Johnson syndrome/toxic epidermal necrolysis. J Inflamm Res. 2018;11:135–142. doi: 10.2147/JIR.S160964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang CW, Yang LY, Chen CB, Ho HC, Hung SI, Yang CH, et al. Randomized, controlled trial of TNF-α antagonist in CTL-mediated severe cutaneous adverse reactions. J Clin Invest. 2018;128:985–996. doi: 10.1172/JCI93349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gillis NK, Hicks JK, Bell GC, Daly AJ, Kanetsky PA, McLeod HL. Incidence and triggers of Stevens-Johnson syndrome and toxic epidermal necrolysis in a large cancer patient cohort. J Invest Dermatol. 2017;137:2021–2023. doi: 10.1016/j.jid.2017.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gravante G, Delogu D, Marianetti M, Esposito G, Montone A. Toxic epidermal necrolysis and Steven-Johnson syndrome in oncologic patients. Eur Rev Med Pharmacol Sci. 2007;11:269–274. [PubMed] [Google Scholar]
- 14.Rosen AC, Balagula Y, Raisch DW, Garg V, Nardone B, Larsen N, et al. Life-threatening dermatologic adverse events in oncology. Anticancer Drugs. 2014;25:225–234. doi: 10.1097/CAD.0000000000000032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ng CY, Chen CB, Wu MY, Wu J, Yang CH, Hui RC, et al. Anticancer drugs induced severe adverse cutaneous drug reactions: an updated review on the risks associated with anticancer targeted therapy or immunotherapies. J Immunol Res. 2018;2018:5376476. doi: 10.1155/2018/5376476. [DOI] [PMC free article] [PubMed] [Google Scholar]