Abstract
Objectives:
Financial exploitation (FE) in old age is poorly understood, particularly among those without significant cognitive impairment. The Finance, Cognition, and Health in Elders Study (FINCHES) aims to identify factors associated with FE among cognitively-healthy older adults. Preliminary findings regarding physical and mental health correlates in the pilot phase of FINCHES are reported.
Method:
Sixteen older adults who self-reported FE were demographically-matched on age, education, sex, and race/ethnicity to eighteen older adults who did not report past FE.
Results:
Those who believed they were exploited endorsed significantly greater symptoms of depression (p = 0.014) and marginally greater symptoms of anxiety (p = 0.062). Participants trended towards lower perceived successful aging (p = 0.094). Perceived FE participants also endorsed greater medical conditions (p = 0.047), but follow-up individual item analyses suggest that this was driven by problems with sleep (p = 0.030).
Conclusions:
These preliminary findings from the pilot phase of FINCHES highlight negative mental health factors associated with perceived FE among cognitively-intact older adults.
Keywords: Financial exploitation, aging, mental health, physical health, sleep
Introduction
Older adults are estimated to lose 3 billion (MetLife, 2011) to 36 billion dollars (True Link Financial, 2015) annually to financial exploitation (FE), scams, and fraud. A recent meta-analysis found the one-year prevalence of elder financial fraud to be 5.4%, likely an underestimate of the true population prevalence (Burnes et al., 2017). According to the Federal Trade Commission (FTC), certain types of financial scams are specifically targeted towards older adults (FTC, 2011), and seniors are disproportionally impacted by scams (FTC, 2011; 2018; Templeton & Kirkman, 2007). Additionally, many older adults are retired and live on fixed incomes; thus, assets that are lost cannot be easily replaced through additional earnings in the workplace (Nerenberg, 1999). Despite the significant personal, familial, and societal impact of FE, the factors associated with FE in old age are poorly understood. Identifying these factors is imperative to protecting the wellbeing of older adults and reducing the economic burden to society. This study aimed to identify physical and mental health correlates of perceived FE in older adults.
Relatively few studies have examined factors associated with perceived FE among older adults, partially due to the challenge of recruiting and retaining individuals who have been exploited into research studies (Acierno et al., 2010; Spreng et al., 2017). Circumventing this challenge, some studies have utilized experimental paradigms that estimate an individual’s risk for being financially exploited (James, Boyle, & Bennett, 2014; Kircanski et al., 2018). For example, susceptibility to scams was observed to be negatively associated with psychological wellbeing, cognition, social support, and financial and health literacy in a large community-based cohort of older adults (James et al., 2014). Other studies have examined associations of perceived FE using large-scale survey methods, such as telephone interviewing (e.g., Acierno et al., 2010; 2018; Beach, Schulz, Castle, & Rosen, 2010; FINRA foundation, 2015; Laumann, Leitsch, & Waite, 2008; Lichtenberg, Stickney, & Paulson, 2013; Peterson et al., 2014; Schafer & Koltai, 2014). Through these survey studies, factors such as poverty, impairments in activities of daily living, cognition, social support, social networks, and depression have been identified as important considerations (Acierno et al., 2010; 2018; Beach et al., 2010; Ganzini, McFarland, & Cutler, 1990; Lichtenberg et al., 2013, 2016a; 2016b; Peterson et al., 2014; Schafer & Koltai, 2014). Despite these efforts, there is not a clear consensus regarding specific correlates of perceived FE, likely due to differences in definitions of exploitation, methodology used, and samples targeted.
While previous work has been useful in identifying potential factors associated with perceived FE in old age, more work is needed to build consensus regarding the profile of associated factors and to further characterize older adults who perceived to have been financially exploited. The most common factor found to be associated with perceived FE in old age has been cognitive impairment (Choi, Kulik, & Mayer, 1999; Dong, Simon, Rajan, & Evans, 2011; Gamble et al., 2014; Han, Boyle, James, Yu, & Bennett, 2016; James et al., 2014; Lichtenberg et al., 2016a; Spreng, Karlawish, & Marson, 2016 for review; S. Wood et al., 2014). However, while it is generally accepted that cognitive impairment is a strong risk factor for perceived FE, there are many examples of older adults without apparent cognitive impairment who have been financially exploited (Jackson & Hafemeister, 2011; Spreng et al., 2017; Templeton & Kirkman, 2007), and the reasons for this remain elusive. The overall goal of the Finance, Cognition, and Health in Elders Study (FINCHES) is to identify factors associated with perceived FE in old age among cognitively healthy older adults. Participants without significant cognitive impairment in the Greater Los Angeles area were enrolled into the study. Those who endorsed FE were demographically-matched to older adults who had not been exploited. Here we present preliminary results specific to physical and mental health outcomes from 34 participants recruited in the pilot phase of FINCHES. We hypothesized that older adults who endorsed a financial exploitation experience would also report higher rates of medical illnesses, anxiety symptoms, and depressive symptoms than demographically-matched older adults.
Method
Participants
Thirty-four older adults aged 50 or older were recruited from senior centers, elder abuse awareness events, and community outreach programs in the greater Los Angeles area to participate in the pilot phase of the Finance, Cognition, and Health in Elders Study (FINCHES). Prior to study enrollment, participants were screened via telephone for eligibility into the study. Participants were excluded if they had known signs of cognitive impairment or a diagnosis of dementia, a neurological or psychiatric illness, or current problems with drugs or alcohol.
Participants were further screened for any significant cognitive impairment on the day of their evaluation using the Montreal Cognitive Assessment (MoCA) screening instrument. Per FINCHES protocol, those who score 23 or below (Carson, Leach, & Murphy, 2018) on this test were excused from further participation in the study and thanked for their time. None of the 34 participants in the present study scored 23 or below and thus all were deemed eligible to continue with study procedures. Participants then underwent a series of behavioral measures. All study procedures were approved by the University of Southern California institutional review board. Consent to participate was documented according to institutional review board guidelines. Participants who request further resources regarding financial exploitation are referred to the National Center on Elder Abuse (NCEA, https://ncea.acl.gov/, 1–855-500–3537) which is directed by co-author Dr. Laura Moqueda and currently co-located in the same academic department as the FINCHES study.
Participants were asked two questions regarding perceived history of FE: (1) “Do you feel you have been taken advantage of financially?” and (2) “Does someone you know feel that you have been taken advantage of financially?” If a participant responded affirmatively to either question, he or she was included in the perceived financial exploitation (FE) group for this pilot phase. Those who responded “no” to both questions were placed in the non-financially exploited (non-FE) group. These specific questions were chosen to capture a wide range of perceived FE experiences and are consistent with previously published work (Gamble et al., 2013; 2014; Licthenberg et al., 2016b). Although certain definitions of FE limit abuse to that committed by a trusted other (e.g., CDC definition, Hall et al., 2016), we chose not to limit our definition in this way as this would exclude individuals who are victims of some scams which specifically target seniors (e.g., grandparent scams). Details of FE experiences were not evaluated in this study. Thus, those who endorsed “yes” to either of these two questions reflect individuals who have the perception that they experienced FE rather than a confirmed experience of FE.
Behavioral measures
Depressive symptomatology was assessed with the nine-item Patient Health Questionnaire (PHQ-9; Kroenke, Spitzer, & Williams, 2001). The questionnaire assesses symptoms of depression over the past two weeks on a scale of 0 (not at all) to 3 (nearly every day) for a total score ranging from 0 to 27.
Anxious symptomatology was assessed with the seven-item Generalized Anxiety Disorder scale (GAD-7; Spitzer, Kroenke, Williams, & Lowe, 2006). The measure assesses symptoms of generalized anxiety over the past two weeks on a scale of 0 (not at all) to 3 (nearly every day) for a total score ranging from 0 to 21.
To evaluate overall health status, participants were administered the Medical History Checklist (MHC) subscale of the Multi-level Assessment Instrument (Lawton, Moss, Fulcomer, & Kleban, 1982). Participants were asked to indicate whether or not they have experienced a range of 23 medical conditions (e.g., diabetes, high blood pressure, arthritis, asthma, anemia, specific organ problems, etc.) over the past year. Those who endorsed the “other” option (item 23) were asked to specify the medical condition. These were cross-referenced with the other 22 items to ensure that the medical condition was not repetitive with a previous item. The total number of reported health conditions were summed to create a total score ranging from 0–23.
To assess whether participants believed that they were successfully aging (Successful Aging question), participants were asked, “Do you think of yourself as someone who is aging successfully (whatever that means to you)?” Participants responded with either “yes” or “no” to this question.
Statistical analyses
Perceived FE older adults were compared to non-financially exploited (non-FE) older adults on measures described above. All continuous variables were assessed for normality and outliers. Independent t-tests or Mann-Whitney tests for non-normally distributed variables were run to examine group differences across demographic variables, PHQ-9, GAD-7, and MHC total scores. To examine group differences on sex and the Successful Aging question, Fisher’s Exact Tests were conducted.
We ran a series of exploratory post-hoc analyses to explore differences between groups across the individual items within each measure. Wilcoxon-Mann-Whitney non-parametric tests were conducted for ordinal items (i.e., individual items on PHQ-9 and GAD-7) and Fisher’s Exact Tests were conducted for binary items (i.e., MHC items). As this is a preliminary study, we did not make corrections for multiple comparisons.
Results
Sixteen of the thirty-four (47.1%) participants responded yes to at least one of the two FE questions during the behavioral assessment and were included in the perceived FE group. Fifteen of the 16 perceived FE older adults responded yes to “Do you feel you have been taken advantage of financially?” One participant responded no to this question but yes to “Does someone you know feel that you have been taken advantage of financially?” Of the fifteen that responded yes to the first question, seven also responded yes to the second question. Eighteen participants answered no to both questions and were included in the non-FE group. Participant characteristics and scores on the questionnaires are presented in Table 1. Participants did not differ on age, education, sex, race/ethnicity, and total score on the MoCA (all ps ≥ 0.35). In regard to race and ethnicity breakdown, 11 perceived FE and nine non-FE were non-Hispanic White, two perceived FE and four non-FE were African American, two perceived FE and three non-FE were Asian, and one perceived FE and one non-FE self-reported Hispanic ethnicity but chose not to indicate race. One perceived FE participant chose not to indicate both race and ethnicity.
Table 1.
Participant demographic characteristics and responses to questionnaires.
| Perceived FE (n = 16) | Non-FE (n = 18) | |||
|---|---|---|---|---|
| M | SD | M | SD | |
| Age | 66.88 | 12.40 | 67.22 | 10.04 |
| Education | 15.88 | 2.78 | 15.17 | 3.15 |
| Sex (%F) | 50% | - | 44% | - |
| Race/Ethnicity | 69% | - | 53% | - |
| (% Non-Hispanic White)1 | ||||
| MoCA | 27.81 | 1.33 | 27.50 | 1.65 |
| PHQ-9 Total* | 3.38 | 2.73 | 1.39 | 1.72 |
| GAD-7 Total* | 3.31 | 3.32 | 1.50 | 2.50 |
| MHC Total* | 3.19 | 1.56 | 2.06 | 1.63 |
| Successful Aging (%yes)† | 81% | - | 100% | - |
Note: FE = financially exploited; Non-FE = non-financially exploited; MoCA = Montreal Cognitive Assessment; PHQ-9 = Patient Health Questionnaire, 9-item; GAD-7 = Generalized Anxiety Disorder scale, 7-item; MHC = Medical Health Checklist subscale of the Multi-level Assessment Instrument; Successful Aging = participants were asked, “Do you think of yourself as someone who is aging successfully (whatever that means to you)?”.
n = 1 non-FE participant chose not to respond to race and ethnicity questions; n = 1 FE participant and n = 1 non-FE participant indicated Hispanic ethnicity but did not respond to race question.
statistically significant difference between groups (p < 0.05); Mann-Whitney tests were used for PHQ-9 and GAD-7, and independent t-test for MHC Total Score. Following removal of an outlier, GAD-7 becomes a marginal difference (p = 0.062).
marginal difference between groups (Fisher’s Exact Test p = 0.09).
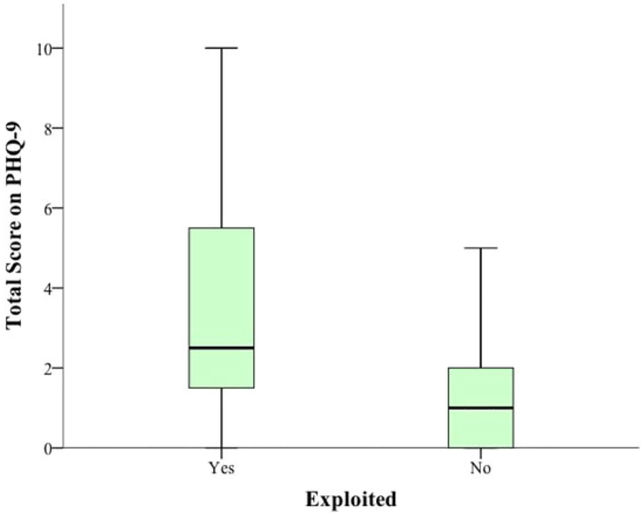
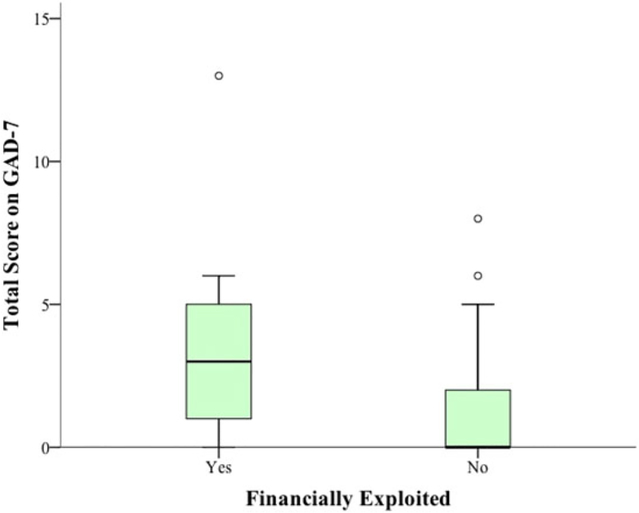
Older adults who endorsed FE reported significantly greater total symptoms of depression on the PHQ-9 (Mann-Whitney test U = 73.00, p = 0.014) and significantly greater overall generalized anxiety symptoms (Mann-Whitney test U = 83.50, p = 0.036) than non-FE older adults. Notably, one perceived FE participant’s score on the GAD-7 is an outlier (score = 13; median score for FE group = 3). Excluding this individual from the analysis changed the finding from a significant difference between perceived FE and non-FE groups for the GAD-7 (p = 0.036) to a marginal trend (p = 0.062). In regard to the MHC, perceived FE participants indicated significantly more medical conditions than non-FE participants (t(32) = 2.07, p = 0.047). Perceived FE participants were less likely to endorse “yes” on the Successful Aging question than non-FE peers, a marginal trend towards significance (Fisher’s Exact Test, p = 0.094). Group differences on the PHQ-9 and GAD-7 can be visualized in Figures 1–2.
Figure 1.
Boxplot display of total scores on the 9-item version of the Patient Health Questionnaire (PHQ-9) for perceived financially exploited (n = 16) and non-exploited (n = 18) older adults.
Figure 2.
Boxplot display of total scores on the 7-item version of the Generalized Anxiety Disorder Scale (GAD-7) for perceived financially exploited (n = 16) and non-exploited (n = 18) older adults. Outlier for the FE group was removed prior to statistical analysis.
Exploratory analyses
To further characterize the physical and mental health status of perceived FE and non-FE older adults, we examined individual item responses from the questions. On the PHQ-9, perceived FE participants reported marginally higher symptoms on item 1 (“little interest or pleasure in doing things”; Mann-Whitney test U = 94.50, p = 0.088) and item 3 (“trouble falling asleep, staying asleep, or sleeping too much”; Mann-Whitney test U = 90.00, p = 0.064). Groups did not differ in symptom report across the remaining items of the PHQ-9, including item 2 (“feeling down, depressed, or hopeless”), item 4 (“feeling tired or having little energy”), item 5 (“poor appetite or overeating”), item 6 (“feeling bad about yourself – or that you’re a failure or have let yourself or your family down”), item 7 (“trouble concentrating on things, such as reading the newspaper or watching television”), item 8 (“moving or speaking so slowly that other people could have noticed. Or, the opposite – being so fidgety or restless that you have been moving around a lot more than usual”), and item 9 (“thoughts that you would be better off dead or hurting yourself in some way”), (all ps ≥ 0.10). On the GAD-7, perceived FE participants reported marginally higher symptoms on item 1 (“feeling nervous, anxious, or on edge”; Mann-Whitney test U = 93.00, p = 0.081), item 3 (“worrying too much about different things”; Mann-Whitney test U = 93.00, p = 0.081), and item 6 (“becoming easily annoyed or irritable”; Mann-Whitney test U = 95.50, p = 0.095). Groups did not differ in their symptom reports across the remaining items of the GAD-7, including item 2 (“not being able to stop or control worrying”), item 4 (“trouble relaxing”), item 5 (“being so restless that it is hard to sit still”), and item 7 (“feeling afraid that something awful might happen”), (all ps ≥ 0.20). Importantly, removing the perceived FE outlier participant with a total score of 13 removed the marginal differences for GAD-7 items 1, 3, and 6.
The average scores on the PHQ-9 and GAD-7 for each group (Table 1) did not surpass the established clinical cutoffs for even mild levels (scores between 5 and 9) of depression and anxiety on these scales (Kroenke et al., 2001; Spitzer et al., 2006). However, individual cases that met mild levels of anxiety and depression based on published cut-offs were apparent for both groups when examining the boxplot displays (Figures 1–2). In additional post-hoc analyses, we therefore categorized each participant’s score on the GAD-7 and PHQ-9 based on the clinical cutoffs (PHQ-9: 0–4 = minimal, 5–9 = mild, 10–14 = moderate; GAD-7: 0–4 = minimal, 5–9 = mild, 10–14 = moderate) and then compared groups using Fisher’ Exact Test. On the PHQ-9, groups significantly differed in the frequency of clinical ratings (Fisher’s Exact Test p = 0.021), with a greater frequency of mild levels of depression based on cut-offs in the perceived FE group compared to the non-FE group (62.5% perceived FE and 94.4% non-FE fell in the minimal range; 37.5% perceived FE and 5.6% non-FE fell in the mild range). Groups did not significantly differ in frequencies of clinical ratings for the GAD-7 (11/16 perceived FE and 15/16 non-FE fell in the minimal range; 5/16 perceived FE and 3/18 non-FE fell in the mild range; Fisher’s Exact Test p = 0.32).
We also examined group differences across each of the individual medical conditions listed in the MHC using Fisher’s Exact Test. Participants did not differ across any of the individual medical conditions (all ps ≥ 0.16), with the exception of the “trouble sleeping or insomnia” item (Fisher’s Exact Test, p = 0.030). Given that poor sleep is a condition highly related to anxiety and depression, we reran the t-test for the MHC with the sleep item excluded from the total score to investigate whether individuals with perceived FE still endorse greater medical conditions. The finding was no longer significant (p = 0.17).
Discussion
This pilot study compared individuals who self-reported a history of FE to demographically-matched individuals who denied a history of FE on responses to physical and mental health questionnaires. We found that perceived FE older adults self-reported significantly more depressive symptoms and sleep difficulties than non-FE older adults, and marginally greater symptoms of anxiety. Findings are cautiously considered preliminary but suggest that depressive symptoms, sleep difficulties, and possibly anxiety symptoms, are important correlates of a perceived history of FE. Exploratory analyses also found marginally greater sleep difficulties on the PHQ-9 in the perceived FE older adults than non-FE older adults. Consistent with these findings, perceived FE older adults were marginally more likely to believe that they are not aging successfully.
Overall, findings suggest greater depressive symptoms in perceived FE older adults, a finding that is consistent with previous research on mental health correlates of FE (Acierno et al., 2018; Beach et al., 2010; FINRA Foundation, 2015; Ganzini et al., 1990; Lichtenberg et al., 2013) and elder abuse more generally (Dong & Simon, 2014; Roepke-Buehler et al., 2015; Santos et al., 2017). Due to the cross-sectional nature of the study, it is unclear whether depressive symptoms are a cause or an effect of perceived FE. One possibility for increased depressive symptoms in perceived FE older adults may be that the experience of FE, or even just the perception that FE has occurred, results in devastating consequences, such as loss of life-savings, relationships, or independence, that can subsequently lead to symptoms of depression. In support of the possibility that depression results from perceiving an experience FE, a recent survey of 600 self-reported victims of financial fraud (FINRA Foundation, 2015) found that a significant proportion of self-reported fraud victims attributed a variety of negative feelings to the fraudulent incident, including sadness, embarrassment, and guilt. Additionally, 35% of respondents endorsed experiencing depression to a serious degree as a result of the fraudulent incident (FINRA Foundation, 2015).
Another possibility is that older adults who suffer from depressive symptoms are at greater risk for FE, or the perception that FE has occurred. Consistent with this, Lichtenberg et al. (2013; also see Lichtenberg et al., 2016b) found depression to be predictive of future self-reported financial fraud in the Health and Retirement Study cohort, a large national longitudinal study based on telephone surveys. Two prospective studies investigating risk factors for elder abuse more generally found conflicting results, with one study finding support (Dong & Simon, 2014), and the other not finding support (Lachs et al., 1997) for depression as a risk factor of elder abuse.
Depression may increase risk of FE via compromised decision making. Studies report impaired decision-making in individuals with depressive symptoms (e.g., Blanco, Otto, Maddox, Beevers, & Love, 2013; Harle, Allen, & Sanfey, 2010) compared to non-depressed individuals. For example, one study used a laboratory task in which individuals made monetary offers to others. This study found that even though depressed individuals reacted more negatively to unfair monetary offers, they were more likely to accept unfair offers than non-depressed individuals (Harle et al., 2010). The authors speculate that depressed individuals’ larger negative emotional responses to unfair offers may have prompted a stronger reliance on regulating these emotions, which may have in turn helped them manage their emotional responses, ultimately leading to more acceptances. The above studies point to the possibility that individuals with greater symptoms of depression are at increased risk for FE due to shifts in their motivation, risk assessments, and/or emotion regulation mechanisms. Future research is needed to elucidate such possibilities.
We found a significant difference in the number of medical conditions reported between the perceived FE group and the non-FE group on the Medical History Checklist; however, post-hoc analyses suggest that this was driven by problems with sleep. A previous survey-based study found associations between self-reported FE and poorer self-reported physical health (Acierno et al., 2018). Other population-based studies also report greater rates of hospitalization (Dong & Simon, 2013b), admittance to skilled nursing facilities (Dong & Simon, 2013a), and mortality (Burnett et al., 2016) in older adults who have experienced FE compared to those who have not. It is possible that the lack of a larger physical health difference in our study is due to our small sample size.
Investigating individual questionnaire items revealed that the perceived FE group rated sleep to be marginally worse on the PHQ-9 and indicated significantly more problems with sleep in the past year on the MHC compared to the non-FE group. The nature of this finding remains unclear. Poor sleep may be a consequence of other factors associated with FE, such as stress, poverty, and poorer physical and mental health (Haan, Kaplan, & Camacho, 1987; Spreng et al., 2017). Alternatively, those with poorer sleep may be at greater risk for FE, possibly due to poorer decision making abilities as a result of sleep deprivation (Harrison & Horne, 2000; Killgore, Balkin, & Wesensten, 2006). Future research is needed to replicate this finding with more detailed sleep assessments and, if replicable, explore potential mechanisms for the association between sleep and FE.
Findings from the present study align well with two recent studies (Acierno et al., 2018; Wood, Liu, Hanoch, & Estevez-Cores, 2016) that also found mental health to be an important correlate of self-reported FE among older adults. Wood et al. (2016) found that numeracy (11-item scale), physical and mental health (as indicated by the 12-Item Short Form Health Survey, SF-12), younger age, and male sex were related to increased risk of FE. Additionally, in a telephone-based survey, Acierno et al. (2018) found that past financial mistreatment was associated with an increased likelihood of self-reported depression, increased generalized anxiety and PTSD, and poorer self-rated health. Our study builds upon these findings by examining these relationships in a carefully selected and well-matched sample of older adults who are cognitively healthy. Taken together, these consistent findings highlight the importance of considering non-economic consequences of FE (Acierno et al., 2018; FINRA Foundation, 2015), and suggest that mental health and poor sleep may be key considerations for developing interventions targeted towards preventing and addressing FE among older adults.
Conclusions and limitations
There are a number of limitations of the present study to acknowledge. The cross-sectional nature of our study precludes any conclusions regarding causality, and direction of associations cannot be determined. However, it is important to note that associations may be bidirectional in that certain risk factors (e.g., depression) may be exacerbated following the experience of FE. In support of this, one large scale telephone survey of 1,246 respondents found a substantial proportion of individuals to report more than one experience of FE (Titus, Heinzelmann, & Boyle, 1995), suggesting that consequences of FE may also be antecedents to future exploitation (also suggested by Beach et al., 2010).
There are several notable limitations related to our sample of older adults that may limit genreliazability of our findings to the larger United States population of older adults. First, study participants were volunteers thus introducing potential self-selection bias. Second, we chose to focus on participants who are 50 years or older, which may introduce heterogeneity to our data (e.g., different severity of effects across different age brackets) and limit generalizability to older populations. We made this decision given recent statistics put forth by the Consumer Sentinel Network (FTC, 2018) that found that adults between the ages of 50–59 had the second highest percentage of individuals who reported fraud (17%; closely following 19% adults aged 60–69). This age group also reported the highest total money lost ($117 million), above older age groups (e.g., 60–69 reported $109 million lost; 70–79 reported $80 million lost; 80 and over reported $6 million lost). These statistics suggest that this age group is particularly vulnerable to financial exploitation (also see Lichtenberg et al., 2013). Nevertheless, this study’s findings may not generalize to much older cohorts. Investigating differential effects of FE across different age groups (e.g., 50–64, 65+) is a future endeavor. Additionally, our sample is highly educated, with 61.8% reporting 16 years or more of education, and generally healthy. For these reasons, our participants may not reflect important segments of the United States adult population over the age of 50 who do not match these characteristics. In particular, higher education may impact how one interprets and responds to the FE questions in our study in unknown ways, and future research may consider exploring such questions. Another notable limitation is that the FE and non-FE group sample sizes are small and thus the findings of the present pilot study are preliminary and interpreted with caution. Further replication with larger samples is necessary. Additionally, we utilized self-report to identify perceived FE among older adults. This may introduce some inaccuracies as some older adults may falsely believe they have been exploited, while others may falsely believe that they have not. The perception of FE may be inherently different from an actual experience of FE. For example, situations in which someone falsely believes they have been exploited may reflect mood, personality, or other characteristics. Thus, these findings may not be generalizable to studies of confirmed FE. The FE questions also did not allow for elaboration on the severity of the specific FE experience, the possibility of polyvictimization, or the victim-perpetrator relationship, all of which may have implications on the degree of mental and physical health outcomes observed. Nevertheless, findings reflect the mental and physical health of individuals who believe that they have experienced FE, regardless of severity, characteristics, and accuracy of the perceived experience.
The present study also has some notable strengths. We employed robust and widely-utilized clinical research measures of physical and mental health and explored differences in a demographically-matched racially-diverse sample of non-demented older adults, mirroring the rich diversity of the greater Los Angeles area. The preliminary findings suggest negative mental health factors and poor sleep are associated with self-reported FE. Prospective research studies that are specifically designed to understand the mechanisms underlying these associations are needed as a next step towards developing interventions that target the prevention of FE in vulnerable older adults.
Acknowledgments
This work is supported by the Elder Justice Foundation and the Cathay Bank Foundation awarded to SDH, as well as the Department of Family Medicine of the University of Southern California. The authors would like to acknowledge Emanuil Parunakian and Jacqueline Chen for their help with data collection and management.
Footnotes
Disclosure of interest
The authors report no conflicts of interest.
References
- Acierno R, Hernandez MA, Amstadter AB, Resnick HS, Steve K, Muzzy W, & Kilpatrick DG (2010). Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: The National Elder Mistreatment Study. American Journal of Public Health, 100(2),292–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acierno R, Watkins J, Hernandez-Tejada MA, Muzzy W, Frook G, Steedley M, & Anetzberger G (2018). Mental health correlates of financial mistreatment in theNational Elder Mistreatment Study Wave II. Journal of Aging and Health. doi: 10.1177/0898264318767037 [DOI] [PubMed] [Google Scholar]
- Beach SR, Schulz R, Castle NG, & Rosen J (2010). Financial exploitation and psychological mistreatment among older adults: differences between African Americans and non-African Americans in a population-based survey. Gerontologist, 50(6),744–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco NJ, Otto AR, Maddox WT, Beevers CG, & Love BC (2013). The influence of depression symptoms on exploratory decision-making. Cognition, 129(3),563–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnes D, Henderson CR Jr., Sheppard C, Zhao R, Pillemer K, & Lachs MS (2017). Prevalence of Financial Fraud and Scams Among Older Adults in the United States: A Systematic Review and Meta-Analysis. American Journal of Public Health, 107(8),e13–e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnett J, Jackson SL, Sinha AK, Aschenbrenner AR, Murphy KP, Xia R, & Diamond PM (2016). Five-year all-cause mortality rates across five categories of substantiated elder abuse occurring in the community. J Elder Abuse Negl, 28(2),59–75. [DOI] [PubMed] [Google Scholar]
- Carson N, Leach L, & Murphy KJ (2018). A re-examination of Montreal Cognitive Assessment (MoCA) cutoff scores. International Journal of Geriatric Psychiatry, 33(2),379–388. [DOI] [PubMed] [Google Scholar]
- Choi NG, Kulick DB, & Mayer J (1999). Financial exploitation of elders: Analysis of risk factors based on county adult protective services data. Journal of Elder Abuse & Neglect, 10(3–4),39–62. [Google Scholar]
- Dong X, Simon M, Rajan K, & Evans DA (2011). Association of cognitive function and risk for elder abuse in a community-dwelling population. Dementia and Geriatric Cognitive Disorders, 32(3),209–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong X, & Simon MA (2013a). Association between reported elder abuse and rates of admission to skilled nursing facilities: findings from a longitudinal population-based cohort study. Gerontology, 59(5),464–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong X, & Simon MA (2013). Elder abuse as a risk factor for hospitalization in older persons. JAMA Internal Medicine, 173(10),911–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong X, & Simon MA (2014). Vulnerability risk index profile for elder abuse in a community-dwelling population. Journal of the American Geriatrics Society, 62(1),10–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Trade Commission (2011). Consumer Fraud in the United States, 2011: The Third FTC Survey. [Google Scholar]
- Federal Trade Commission (2018). Consumer Sentinel Network Data Book 2017. Washington, DC: Retrieved from https://www.ftc.gov/policy/reports/policy-reports/commission-and-staff-reports [Google Scholar]
- FINRA Investor Education Foundation (2015). The non-traditional costs of financial fraud: Report of survey findings Report prepared by Applied Research and Consulting: New York, NY. [Google Scholar]
- Gamble KJ, Boyle PA, Yu L, & Bennett DA (2013). Aging, financial literacy, and fraud. (Netspar Discussion Paper No. 11/2013–066). [Google Scholar]
- Gamble KJ, Boyle P, Yu L, & Bennett D (2014). The causes and consequences of financial fraud among older Americans. Boston College Center for Retirement Research WP, 2014–13. Retrieved from https://ssrn.com/abstract=2523428. [Google Scholar]
- Ganzini L, McFarland BH, & Cutler D (1990). Prevalence of mental disorders after catastrophic financial loss. J Nerv Ment Dis, 178(11),680–685. [DOI] [PubMed] [Google Scholar]
- Haan M, Kaplan GA, & Camacho T (1987). Poverty and health prospective evidence from the alameda county study. American Journal of Epidemiology, 125(6),989–998. [DOI] [PubMed] [Google Scholar]
- Hall J, Karch D, & Crosby A (2016). Elder abuse surveillance: Uniform definitions and recommended core data elements for use in elder abuse surveillance, Version 1.0 Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Han SD, Boyle PA, James BD, Yu L, & Bennett DA (2016). Mild cognitive impairment and susceptibility to scams in old age. Journal of Alzheimer’s Disease: Jad, 49(3),845–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harle KM, Allen JJ, & Sanfey AG (2010). The impact of depression on social economic decision making. J Abnorm Psychol, 119(2),440–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison Y, & Horne JA (2000). The impact of sleep deprivation on decision making: a review. Journal of Experimental Psychology. Applied, 6(3),236–249. [DOI] [PubMed] [Google Scholar]
- Jackson SL, & Hafemeister TL (2011). Risk factors associated with elder abuse: The importance of differentiating by type of elder maltreatment. Violence and Victims, 26(6),738. [DOI] [PubMed] [Google Scholar]
- James BD, Boyle PA, & Bennett DA (2014). Correlates of susceptibility to scams in older adults without dementia. Journal of Elder Abuse & Neglect, 26(2),107–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore WD, Balkin TJ, & Wesensten NJ (2006). Impaired decision making following 49 h of sleep deprivation. Journal of Sleep Research, 15(1),7–13. [DOI] [PubMed] [Google Scholar]
- Kircanski K, Notthoff N, DeLiema M, Samanez-Larkin GR, Shadel D, Mottola G, … Gotlib IH (2018). Emotional arousal may increase susceptibility to fraud in older and younger adults. Psychol Aging, 33(2),325–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9),606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachs MS, Williams C, O’Brien S, Hurst L, & Horwitz R (1997). Risk factors for reported elder abuse and neglect: A nine-year observational cohort study. The Gerontologist, 37(4),469–474. [DOI] [PubMed] [Google Scholar]
- Laumann EO, Leitsch SA, & Waite LJ (2008). Elder mistreatment in the United States: prevalence estimates from a nationally representative study. J Gerontol B Psychol Sci Soc Sci, 63(4),S248–S254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton MP, Moss M, Fulcomer M, & Kleban MH (1982). A research and service oriented multilevel assessment instrument. Journal of Gerontology, 37(1),91–99. [DOI] [PubMed] [Google Scholar]
- Lichtenberg PA, Ficker LJ, & Rahman-Filipiak A (2016a). Financial decision-making abilities and financial exploitation in older African Americans: Preliminary validity evidence for the Lichtenberg Financial Decision Rating Scale (LFDRS). J Elder Abuse Negl, 28(1),14–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtenberg PA, Stickney L, & Paulson D (2013). Is psychological vulnerability related to the experience of fraud in older adults?. Clinical Gerontologist, 36(2),132–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtenberg PA, Sugarman M, Paulson D, Ficker LJ, & Rahman-Filipiak A (2016b). Psychological and functional vulnerability predicts fraud cases in older adults: Results of a longitudinal study. Clinical Gerontologist, 39(1),48–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MetLife (2011). The MetLife study of elder financial abuse crimes of occasion, desperation, and predation against America’s elders. In: Metlife Mature Market Institute/National Committee for Prevention of Elder Abuse/Virginia Polytechnic Institute and State University, Metlife Mature Market Institute; Westport, CT. [Google Scholar]
- Nerenberg L (1999). Forgotten victims of elder financial crime and abuse (Vol. 4): A Report and Recommendation. [Google Scholar]
- Peterson JC, Burnes DPR, Caccamise PL, Mason A, Henderson CR, Wells MT, … Lachs MS (2014). Financial exploitation of older adults: a population-based prevalence study. Journal of General Internal Medicine, 29(12),1615–1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roepke-Buehler SK, Simon M, & Dong X (2015). Association between depressive symptoms, multiple dimensions of depression, and elder abuse: A cross-sectional, population-based analysis of older adults. Journal of Aging and Health, 27(6),1003–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos AJ, Nunes B, Kislaya I, Gil AP, & Ribeiro O (2017). Exploring thecorrelates to depression in elder abuse victims: Abuse experience or individual characteristics? Journal of Interpersonal Violence. doi: 10.1177/0886260517732346 [DOI] [PubMed] [Google Scholar]
- Schafer MH, & Koltai J (2014). Does embeddedness protect? Personal network density and vulnerability to mistreatment among older American adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 70(4),597–606. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, & Lowe B (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine, 166(10),1092–1097. [DOI] [PubMed] [Google Scholar]
- Spreng RN, Cassidy BN, Darboh BS, DuPre E, Lockrow AW, Setton R, & Turner GR (2017). Financial Exploitation Is Associated With Structural and Functional Brain Differences in Healthy Older Adults. The Journals of Gerontology: Series A, 72(10),1365–1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spreng RN, Karlawish J, & Marson DC (2016). Cognitive, social, and neural determinants of diminished decision-making and financial exploitation risk in aging and dementia: A review and new model. Journal of Elder Abuse & Neglect, 28(4–5),320–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Templeton VH, & Kirkman DN (2007). Fraud, vulnerability, and aging: Case studies. Alzheimer’s Care Today, 8(3),265–277. [Google Scholar]
- Titus RM, Heinzelmann F, & Boyle JM (1995). Victimization of persons by fraud. Crime & Delinquency, 41(1),54–72. [Google Scholar]
- True Link Financial (2015). The True Link Report on Elder Financial Abuse. San Francisco, CA: Retrieved from https://www.truelinkfinancial.com/research [Google Scholar]
- Wood S, Rakela B, Liu P-J, Navarro AE, Bernatz S, Wilber KH, … Homier D (2014). Neuropsychological profiles of victims of financial elder exploitation at the los angeles county elder abuse forensic center. J Elder Abuse Negl, 26(4),414–423. [DOI] [PubMed] [Google Scholar]
- Wood SA, Liu P-J, Hanoch Y, & Estevez-Cores S (2016). Importance of numeracy as a risk factor for elder financial exploitation in a community sample. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 71(6),978–986. [DOI] [PubMed] [Google Scholar]