Abstract
The homebound population relies on both paid and family caregivers to meet their complex care needs. In order to examine the association between intensity of caregiving support and leaving the home, we identified a population of community-dwelling, homebound Medicare beneficiaries age ≥65 (n=1,852) enrolled in the 2015 National Health and Aging Trends Study and measured the support they received from paid and family caregivers. Those who had ≥20 hours of caregiving support per week had 50% less odds of being “exclusively homebound” (rarely or never leave home) (OR 0.56, p<0.01). Policies that facilitate increased support for family caregivers and better access to paid caregivers may allow homebound individuals who would otherwise be isolated at home to utilize existing community-based long-term care services and supports.
Keywords: Homebound, family caregiving, paid caregiving, long-term care, home and community-based services
Introduction
Population estimates suggest that approximately 2 million Americans currently report leaving the home once a week or less. An additional 5.3 million Americans report leaving only with the help of others or “with difficulty” (Ornstein et al., 2015). While the frequency and manner in which these individuals leave home varies, they all meet the Medicare Home Health Care Benefit definition of “homebound:” they need the help of another person or an assistive device to leave the home, have a normal inability to leave the home, and find leaving the home requires a considerable and taxing effort (CentersforMedicareandMedicaidServices, 2018). The number of homebound individuals is expected to grow in the coming years due not only to shifts in national demographics towards an older population, but also because of a nationwide policy shift in the provision of long-term care policy from institutions to the community (Kaye, 2014; Kaye, Harrington, & LaPlante, 2010; Wysocki et al., 2015).
The homebound have more medical and psychiatric disease, increased functional impairment, and increased symptom burden as compared to the non-homebound (Ornstein et al., 2015; Qiu et al., 2010; Wajnberg, Ornstein, Zhang, Smith, & Soriano, 2013). In addition, the homebound are more socially isolated, endorse more loneliness and depressed mood (Cohen-Mansfield, Shmotkin, & Hazan, 2012; Qiu et al., 2010) and have difficulty accessing valued activities in their community (Cohen-Mansfield et al., 2012; Qiu et al., 2010; Szanton et al., 2016). Being homebound is independently associated with poor outcomes, including higher hospitalization and mortality rates (Cohen-Mansfield, Shmotkin, & Hazan, 2010; Musich, Wang, Hawkins, & Yeh, 2015; Soones, Federman, Leff, Siu, & Ornstein, 2017). Innovative care delivery models such as the Independence at Home Demonstration attempt to the meet the unique needs of this complex population (Rotenberg, Kinosian, Boling, Taler, & Independence at Home Learning Collaborative Writing, 2018).
While increasing home-based services is a key strategy to meet the needs of a growing homebound population, demand for home-based services such as skilled home health care (Wang et al., 2017), home-based primary medical care (Leff et al., 2015; Mahon, 2014), or social services like meal-delivery services or help with transportation (Sonnega, Robinson, & Levy, 2017) often outstrips supply. For example, only 12% of those who never or rarely leave home reported receiving primary care at home (Ornstein et al., 2015). In order to better inform long-term care policy at the state and national level, it is therefore essential to understand factors that may impact the ability of homebound older adults to leave the home so that they can continue to access existing services and supports in the community despite their functional impairment (Kaye & Harrington, 2015).
Prior work has outlined a conceptual model of the multiple predisposing (demographic, socioeconomic), enabling (caregivers, home and community resources), and need (functional impairment, multi-morbidity) factors that contribute to homebound status (Soones et al., 2017). While existing research highlights the clinical, functional, and demographic factors that define the homebound population (Cohen-Mansfield et al., 2012; Ornstein et al., 2015; Qiu et al., 2010), minimal work has focused on the contribution of paid and family caregiving to homebound status. Paid caregivers (i.e., home health aides, personal care attendants, or other direct care workers) are caregivers associated with a formal care system. Family caregivers (usually unpaid) include not only relatives but also friends, neighbors, and others who have a significant personal relationship with the care-recipient. Caregivers provide a significant amount of often highly specialized care to functionally impaired individuals in the community (Wolff, Spillman, Freedman, & Kasper, 2016) and the spread of legislation such as the CARE Act nationally reflect the growing recognition of the importance of integration of caregivers into the care for complex patients (AARP, 2014).
While healthcare providers rely on their patients’ caregivers to facilitate treatment adherence, monitor treatment response, and ensure access to needed care (Wolff et al., 2016), there is a surprising lack of research evaluating the impact of caregivers on patient outcomes. This is in part due to a paucity of data collected in research studies and routine clinical practice about caregiver support systems. Thus the potential impact of caregiver-related factors such as caregiver availability and intensity of care provided is overlooked. While it is clear that caregiver availability impacts nursing home placement (Afram et al., 2014; Charles & Sevak, 2005; Gaugler, Duval, Anderson, & Kane, 2007; Gaugler, Kane, Kane, Clay, & Newcomer, 2003; Van Houtven & Norton, 2004), it is not known how caregivers may impact other key health outcomes for vulnerable older adults. The purpose of this study was to 1) characterize the amount and sources of family and/or paid caregiving received by the homebound, and to 2) determine the association between receipt of caregiving support and the ability of older adults to leave the home.
Methods
Study Population
Our sample was drawn from the 2015 National Health and Aging Trends Study (NHATS), a survey of Medicare recipients age 65 and over (NationalHelathandAgingTrendsStudy, 2018). NHATs began in 2011 with a nationally representative cohort that was followed annually. In 2015, this cohort was replenished. In-person interviews were conducted with study participants or with proxy respondents if the participant was unable to respond. Study participants were asked detailed questions about how they performed daily activities in the month before the interview as well as their medical comorbidities, socioeconomic status, and home environment. Among older adults who received assistance with daily activities, information about who provides help, their relationship with the respondent, and what specific assistance they provide was obtained.
Measures
Homebound status.
All community-dwelling NHATS participants were asked how often they went out in the last month, if anyone helped them, and how much difficulty they had leaving the home alone. Consistent with previous research (Ornstein et al., 2015), we categorized older adults who met the Medicare definition of homebound as described above into three groups based on if and how they left the home: 1) “exclusively homebound” left home one or fewer times per week, 2) “completely dependent” left home twice or more per week but never by themselves, or 3) “limited ability” left home twice or more per week, sometimes received help, and reported difficulty when leaving alone. If participants did not meet any of the above criteria, they were considered not homebound and not included in analyses.
Caregiving status.
All NHATs participants were asked about their ability to perform basic and instrumental activities of daily living (ADLs and iADLs) and related tasks. If help was needed to perform a particular task, participants are asked to identify their relationship to the helper, the hours of caregiving provided, and the source of pay if any, for up to 5 helpers per participant. For each participant we calculated total number of caregivers, whether any paid care was received, and total weekly hours of care provided. As in previous work, we defined high intensity caregiving support as ≥ 20 hours per week from all caregiving sources (Wolff et al., 2016). In secondary analysis, we examined two alternative measures of intensity of caregiving support: ≥4 caregivers, which represents the upper quartile of caregiver number, and receipt of paid caregiving.
Other measures.
Caregiving is one of a wide range of clinical, sociodemographic, functional, home environment, and geographic variables identified in previous research (Cohen-Mansfield et al., 2012; Ornstein et al., 2015; Qiu et al., 2010) or postulated in conceptual models (Soones et al., 2017) to be associated with the ability to leave the home. We included many these variables as covariates (Table 1.) Clinical variables included self-reported general health, number of hospitalizations in the prior 12 months, and count of chronic conditions (anxiety, arthritis, dementia, depression, diabetes, cancer, heart disease, hip fracture, hypertension, lung disease, osteoporosis, and stroke.) Depression was assessed with the Patient Health Questionnaire PHQ-2 depression screen (Lowe, Kroenke, & Grafe, 2005), anxiety with the Generalized Anxiety Disorder GAD-2 scale (Wild et al., 2014), and all other medical conditions were self-reported. Probable dementia was based on criteria established by NHATs (Kasper, Freedman, & Spillman, 2013), which incorporated self- report of dementia, the Alzheimer’s Disease (AD)-8 screening tool (Galvin et al., 2005), and a cognitive interview that assessed memory, orientation, and executive function. Functional impairment was assessed as follows: (1) use of assistive devices (walker, wheelchair, or scooter, inside or outside of the home); (2) ADL impairment (eating, getting out of bed, showering, toileting, dressing); and (3) iADL impairment (laundry, shopping, meal preparation, medication management, getting around outside, bills and banking.) Impairment in a given ADL or iADL was defined as any of the following: (1) was done by others/ with the help of others because of health or function (2) went without doing the activity because no one was available to help, or (3) performed the activity by their self with at least some difficulty.
Table 1:
Characteristics of homebound population grouped by if and how they left the home*, 2015 (n=1,852)
| Sample characteristics | Group-wise comparisons | |||||
|---|---|---|---|---|---|---|
| Limited Ability (LA) | Completely dependent (CD) | Exclusively Homebound (EH) | P-value: LA-EH | P-value: CD-EH | P-value: LA-CD | |
| Sample N | 994.00 | 326.00 | 532.00 | |||
| Sample N weighted | 4,876,363 | 1,245,044 | 2,131,372 | |||
| Age, mean (SD) | 76.6 (7.9) | 82.3 (8.6) | 80.6 (9.0) | <0.01 | 0.04 | <0.01 |
| Female (%) | 62.8 | 70.8 | 73.0 | <0.01 | 0.59 | 0.04 |
| White, Non-Hispanic (%) | 75.5 | 61.6 | 60.0 | <0.01 | 0.71 | <0.01 |
| Hispanic (%) | 5.7 | 12.4 | 20.1 | <0.01 | 0.03 | <0.01 |
| Black, non-Hispanic (%) | 10.7 | 10.7 | 11.7 | 0.47 | 0.59 | 0.99 |
| Other, non- Hispanic (%) | 4.4 | 10.6 | 4.7 | 0.87 | 0.03 | <0.01 |
| ≥ High school education (%) | 76.9 | 65.7 | 60.1 | <0.01 | 0.19 | <0.01 |
| Annual household income, mean | 44,359 | 33,521 | 32,024 | 0.01 | 0.79 | 0.02 |
| Medicaid (%) | 20.1 | 33.9 | 35.5 | <0.01 | 0.73 | <0.01 |
| Married (%) | 44.3 | 29.3 | 33.0 | <0.01 | 0.36 | <0.01 |
| Number of living children, mean (SD) | 3.0 (2.0) | 3.2 (2.3) | 3.2 (2.3) | 0.12 | 0.81 | 0.11 |
| Home Environment and Geographic Factors | ||||||
| Lives alone (%) | 34.8 | 32.0 | 32.2 | 0.40 | 0.96 | 0.45 |
| Non-nursing home residential care (%) | 7.1 | 18.5 | 19.6 | <0.01 | 0.75 | <0.01 |
| Stairs to enter home (%) | 77.4 | 58.5 | 65.3 | <0.01 | 0.10 | <0.01 |
| Region | ||||||
| Northeast (%) | 19.7 | 24.2 | 20.4 | 0.78 | 0.32 | 0.18 |
| Midwest (%) | 22.0 | 11.7 | 18.9 | 0.24 | 0.01 | <0.01 |
| South (%) | 38.3 | 39.2 | 35.1 | 0.32 | 0.32 | 0.80 |
| West (%) | 20.1 | 25.0 | 25.6 | 0.06 | 0.87 | 0.15 |
| Lives in metropolitan area (%) | 77.6 | 89.0 | 82.6 | 0.05 | 0.03 | <0.01 |
| Functional Impairment and Clinical Factors | ||||||
| Assistive Device (%) | 23.5 | 61.0 | 49.1 | <0.01 | <0.01 | <0.01 |
| ADL impairment, mean (SD) | 1.3 (1.4) | 2.8 (2.0) | 2.3 (2.0) | <0.01 | <0.01 | <0.01 |
| iADL impairment, mean (SD) | 1.6 (1.5) | 3.4 (1.7) | 2.9 (1.8) | <0.01 | <0.01 | <0.01 |
| Count medical conditions, mean (SD) | 4.1 (1.8) | 4.5 (2.0) | 4.6 (2.2) | <0.01 | 0.73 | <0.01 |
| Lung disease (%) | 26.8 | 18.1 | 25.8 | 0.74 | 0.03 | 0.01 |
| Depression (%) | 23.9 | 32.9 | 40.8 | <0.01 | 0.07 | 0.01 |
| Dementia (%) | 12.4 | 49.2 | 39.3 | <0.01 | 0.02 | <0.01 |
| Self-reported health fair/poor (%) | 49.3 | 54.0 | 59.7 | <0.01 | 0.18 | 0.23 |
| Hospital stay in the last year (%) | 35.9 | 44.1 | 37.9 | 0.52 | 0.15 | 0.03 |
Subgroup definitions: “exclusively homebound” left home one or fewer times per week, “completely dependent” left home ≥2 times per week but never by themselves, and “limited ability” left home ≥2 per week, sometimes received help, and reported difficulty when leaving alone.
Analysis
In order to characterize the caregivers of the homebound population, we applied NHATS sampling weights to adjust for differential nonresponse based on participant demographic characteristics and location, and produced national prevalence estimates of homebound individuals and their caregivers based on homebound group. We used Chi-square and Student’s t-test to compare the functional, clinical, sociodemographic, and environmental characteristics among the groups as well as to compare the paid and family caregiver support.
In order to determine the association between receipt of caregiving support and the ability of older adults to leave the home, we limited our analysis to the “exclusively homebound” and “completely dependent” homebound subgroups. This is because, as shown in Table 1, the “limited ability” group was markedly different than the other homebound categories across key attributes variables. For example, they were younger (mean age 76.6 versus 82.3 in “completely dependent”, p<0.01 and 80.6 in “exclusively homebound”, p<0.01) with less functional impairment (mean ADL impairment 1.3 versus 2.8 in “completely dependent”, p<0.01 and 2.3 in “exclusively homebound”, p<0.01) and less chronic disease (count of chronic medical conditions 4.1 versus 4.5 in “completely dependent”, p<0.01 and 4.6 in “exclusively homebound”, p<0.01.). As a result, and in order to minimize the impact of unmeasured factors that could confound the relationship, we focused on the role of high intensity caregiving support among the “exclusively homebound” and “completely dependent” groups. Many of the factors that contribute to ability to leave the home also likely contribute to receipt of caregiving (e.g. income and functional impairment). We used propensity score matching to simultaneously account for the multiple factors associated with high intensity caregiver support among the “exclusively homebound” and “completely dependent” groups. Variables included in the propensity matching were chosen from our conceptual model, prior work, and observed differences in the groups. If two factors were highly correlated, only one factor was included. Thus, we modeled intensity of caregiving support as a function of age, gender, race, marital status, number of children, income, Medicaid coverage, education, general health, count of medical conditions, lung disease, depression, dementia, impairment in ≥3 ADLs, impairment in ≥3 iADLs, use of assistive devices, region of residence, and living in a metropolitan area.
Balance between high and low intensity caregiving support within the strata of the propensity score was verified by examining standardized differences in covariates and variance of covariates before and after matching. Consistent with the existing literature, we tested multiple methods to determine the optimal approach for balancing covariates (Garrido et al., 2014). Inverse propensity weighting (IPW) was selected because it resulted in the best balance across covariates. Standardized differences less than 10% were considered to be adequate balance.
Using the IPW sample, we estimated a multivariable logistic regression model and regressed homebound category (“exclusively homebound” versus “completely dependent”) on receipt of high intensity caregiving further adjusting for all the covariates included in the propensity score matching procedure. This doubly robust technique adjusts for any remaining imbalance in the groups. In secondary analyses, we examined two alternative markers of high intensity caregiving support: having four or more caregivers and presence of a paid caregiver.
The Johns Hopkins University Institutional Review Board approved the NHATS protocol and all participants provided written informed consent. Analyses were performed using SAS, version 9.4 (SAS Institute, Inc., Cary, NC.)
Results
Of the 8,334 NHATS participants in 2015, 7,499 were community-dwelling and 7,494 reported their ability to leave the home. Of these, 5,642 were non-homebound. Our final sample included 1,852 homebound individuals: 532 (28.7%) “exclusively homebound,” 326 (17.6%) “completely dependent,” and 994 (53.7%) “limited ability.”
While the “limited ability” group differed from the rest of the homebound in most measured variables, the “exclusively homebound” and “completely dependent” groups had few substantive differences across a range of measured factors (Table 1) including gender, marital status, income, insurance, chronic conditions, or general health. Differences that did emerge between the “exclusively homebound” and “completely dependent” groups were as follows: less functional impairment (mean ADL and iADL impairment 2.3 vs 2.8, p<0.01 and 2.9 vs. 3.4, p<0.01 in the “exclusively homebound” and “completely homebound” groups respectively), less commonly use of assistive devices (49.1% vs 61.0%, p<0.01), younger (mean age 80.6 vs. 82.2, p=0.04), less likely to have dementia (56.4% vs 65.9%, p=0.03), more likely to report lung disease (25.8% vs 18.1%, p=0.03), more likely to be from the Midwest (18.9% vs 11.7%, p=0.01,) less likely to live in a metropolitan area (82.0% vs 88.9%, p=0.03), and more likely to be Hispanic (20.1% vs. 12.4%, p=0.03).
Table 2 characterizes the paid and family caregiving received by the “exclusively homebound”, “completely dependent”, and “limited ability” groups. As compared to the “exclusively homebound” group, the “limited ability” group received significantly less caregiving support: 2.4 vs 2.2 (p=0.01) total caregivers, 29.7% vs. 19.7% (p<0.01) with a paid caregiver, and 24.7 vs 45.8 (p<0.01) total hours of caregiving support received per week. As compared to the “exclusively homebound” group, the “completely dependent” group received significantly more caregiving support: 2.4 vs 3.0 (p<0.01) total caregivers, 29.7% vs. 41.6% (p<0.01) with a paid caregiver, and 45.8 vs 66.7 (p<0.01) total hours of caregiving support received per week. Increased hours of caregiving support from both child and paid caregivers (regardless of funding sources) accounted for the observed differences between groups.
Table 2:
Receipt of paid and unpaid caregiving among the homebound grouped by if and how they left the home* (n=1,852)
| Sample characteristics | Group-wise comparisons | |||||
|---|---|---|---|---|---|---|
| Limited Ability (LA) | Completely dependent (CD) | Exclusively Homebound (EH) | P-value: LA-EH | P-value: CD-EH | P-value: LA-CD | |
| Sample N | 994 | 326 | 532 | |||
| Caregivers, N | 2267 | 1037 | 1378 | |||
| Caregivers N (Weighted) | 10,532,944 | 3,735,033 | 5,115,293 | |||
| Number of caregivers per participant, mean (SD) | 2.2 (1.4) | 3.0 (1.7) | 2.4 (1.5) | 0.01 | <0.01 | <0.01 |
| Has paid caregiver, % | 18.5 | 41.1 | 28.3 | <0.01 | <0.01 | <0.01 |
| Source of paid caregiver funding, % | ||||||
| Self/family | 9.3 | 17.5 | 11.6 | 0.22 | 0.03 | <0.01 |
| Government program | 5.5 | 15.0 | 8.2 | 0.08 | 0.01 | <0.01 |
| Private insurance | 2.8 | 8.7 | 5.9 | 0.02 | 0.23 | <0.01 |
| Total hours per week, mean (SD) | 24.7 | 66.7 | 45.7 | <0.01 | <0.01 | <0.01 |
| ≥20 hours of caregiving support per week, % | 31.8 | 69.6 | 51.9 | <0.01 | <0.01 | <0.01 |
| 4+ helpers, % | 14.6 | 29.4 | 20.1 | 0.02 | 0.01 | <0.01 |
| Hours of caregiving support per week by caregiver relationship, mean (SD) | ||||||
| Spouse | 12.0 (31.6) | 17.7 (43.7) | 13.7 (37.1) | 0.52 | 0.31 | 0.10 |
| Child | 6.7 (19.5) | 28.0 (48.7) | 19.2 (40.5) | <0.01 | 0.01 | <0.01 |
| Other non-paid | 3.2 (11.7) | 6.1 (18.0) | 4.9 (18.8) | 0.05 | 0.38 | 0.01 |
| Paid | 2.8 (13.3) | 14.9 (33.6) | 8.0 (22.3) | <0.01 | <0.01 | <0.01 |
Subgroup definitions: “exclusively homebound” left home one or fewer times per week, “completely dependent” left home ≥2 times per week but never by themselves, and “limited ability” left home ≥2 per week, sometimes received help, and reported difficulty when leaving alone.
The propensity score weighted sample included all “exclusively homebound” individuals (n=532) and all “completely dependent” individuals (n=326) for a total of 858 individuals (46% of total homebound population). Observed confounders were balanced (<10% standardized difference) (Figure 1.) In multivariable logistic regression of propensity-score weighted groups (Table 3), observed differences in receipt of high intensity caregiving support persisted and those who received high intensity caregiving support were 50% less odds of being in the “exclusively homebound” group (OR 0.56, p<0.01). In secondary analyses, propensity-score groups were re-weighted to assess alternative markers of high intensity caregiving support. Those with four or more caregivers were less likely to be in the “exclusively homebound” group (OR 0.74, p=0.08) but the result was not significant. Those with any paid help were less likely to be in the “exclusively homebound” group (OR 0.68, p=0.03). Our findings were robust to alternative matching techniques (data not shown.)
Figure 1.
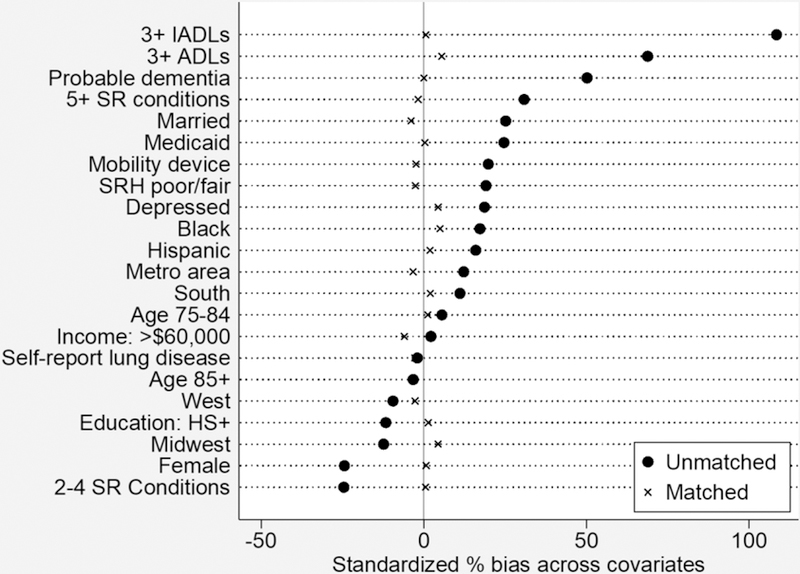
Matching variables before and after match (n=858)
Table 3:
Association between high intensity caregiving support and “exclusively homebound” status (propensity weighted sample*) (n=858), 2015
| Odds Ratio | P-value | 95% CI | |
|---|---|---|---|
| Primary analysis: high intensity caregiving | |||
| ≥20 hours of caregiving support per week | 0.56 | <0.01 | 0.38–0.83 |
| Secondary analysis: alternative definitions of high intensity caregiving | |||
| ≥4 caregivers | 0.74 | 0.08 | 0.52–1.04 |
| Any paid help | 0.68 | 0.03 | 0.49–0.96 |
Included factors were age, female gender, race, marital status number of children, income, Medicaid status, high school education or greater, self-reported health fair or poor, count of medical conditions, lung disease, depression, dementia, impairment in 3+ ADLs, impairment in 3+ iADLs, use of assistive devices, region of residence, and living in a metropolitan area.
Discussion
Among those who meet the Medicare definition of homebound, high intensity caregiving support is associated with leaving the home even after controlling for factors like functional status, clinical status, dementia, insurance, income, and geographic location. Because older adults prefer to live at home (AARP, 2014; Gillsjo, Schwartz-Barcott, & von Post, 2011) while simultaneously engaging in meaningful activities in their communities (Szanton et al., 2016), our findings confirm the key role caregivers play in the important patient outcome of ability to leave the home and have significant implications for how we provide care in the community.
Those in the “completely dependent” group received more support from both family and paid caregivers. An important consideration in interpreting the significance of these findings is the degree to which caregiving factors are modifiable and may therefore lead to interventions that improve patient outcomes. While an older individual cannot themselves have more children, availability of family caregiver support may be modifiable. The pool of potential caregivers extends beyond first-degree relatives (Hanyok, Mullaney, Finucane, & Carrese, 2009) and living environments like the “village” model of aging in place have been shown to promote social engagement and access to services (Graham, Scharlach, & Stark, 2017). Further work should examine interventions to expand the caregiving networks of those who rarely or never leave home in order to increase the likelihood that they can access care and social supports in their community. In addition, state and federal policies such as paid family leave that support caregivers should be amplified in order to expand supports for existing caregivers and ensure they have the time and resources to meet the complex needs of their loved ones.
Increasing use of paid caregivers in the home is another important way to increase overall receipt of caregiving support among functionally impaired older adults. While there are over two million paid caregivers providing direct care in the community and this number is projected to increase significantly as the population ages (ParaprofessionalHealthcareInstitute, 2017), the current system of paid care in the home relies on a patchwork of public and private payers and state-by-state variation in both Medicaid-funded service availably and oversight requirement for paid caregivers varies significantly (Kaye et al., 2010). This has hindered the study of how paid caregivers impact patient outcomes such as change in health status, nursing home placement, and ability to remain living at home (Hewko et al., 2015). Our study is the first to our knowledge to characterize paid caregiver support among the homebound. Future study should assess the impact of having paid caregivers on patient outcomes. This is necessary to guide utilization of publicly funded sources of paid care at home (e.g. Medicare Home Health, Hospice, Medicaid) and to inform national efforts to improve long-term care services and supports available in the community.
Limitations
An important limitation of this study is its cross-sectional design, which does not take into account the potentially dynamic nature of both ability to leave the home and caregiver support. While we see a clear association between caregiving support and homebound status, we cannot determine causality. Regardless of the causal direction of this relationship, these findings have important implications for policies that support the caregivers of individuals who wish to age in place. In addition, the complex and overlapping factors that contribute to both ability to leave the home and receipt of caregiving complicate efforts to isolate the relationship between these variables. While propensity score matching seeks to mitigate this effect, it is not able to account for unmeasured confounding. Future research will require longitudinal analyses to better understand how both changes in need for care and availability of family and paid caregivers over time impacts patient’s ability to leave home. Finally, because the individuals who meet the homebound definition likely have at least minimal caregiving support, our analyses are focused on high intensity caregiving and don’t specifically address those who have no caregiving support at all.
Conclusion
Those with functional impairment living at home rely on a network of caregivers who often provide high levels of care to remain safely in the community (Wolff et al., 2016) Our findings indicate that there is an association between these caregivers and an individual’s ability to leave home, which is necessary for utilizing existing social and medical services in the community. Our findings highlight importance of growing, national efforts to recognize, support, and study the essential role that caregivers play in the lives of the homebound.
References
- AARP. (2014). Home and Commmunity Preferences of the 45+ Population 2014 from https://www.aarp.org/content/dam/aarp/research/surveys_statistics/il/2015/home-community-preferences.doi.10.26419%252Fres.00105.001.pdf
- Afram B, Stephan A, Verbeek H, Bleijlevens MH, Suhonen R, Sutcliffe C, … RightTimePlaceCare, C. (2014). Reasons for institutionalization of people with dementia: informal caregiver reports from 8 European countries. J Am Med Dir Assoc, 15(2), 108–116. doi: 10.1016/j.jamda.2013.09.012 [DOI] [PubMed] [Google Scholar]
- CentersforMedicareandMedicaidServices. (2018). Medicare Home Health Care Services Retrieved January 8, 2018, from https://www.medicare.gov/coverage/home-health-services.html#1334
- Charles KK, & Sevak P (2005). Can family caregiving substitute for nursing home care? J Health Econ, 24(6), 1174–1190. doi: 10.1016/j.jhealeco.2005.05.001 [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Shmotkin D, & Hazan H (2010). The effect of homebound status on older persons. J Am Geriatr Soc, 58(12), 2358–2362. doi: 10.1111/j.1532-5415.2010.03172.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Shmotkin D, & Hazan H (2012). Homebound older persons: prevalence, characteristics, and longitudinal predictors. Arch Gerontol Geriatr, 54(1), 55–60. doi: 10.1016/j.archger.2011.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galvin JE, Roe CM, Powlishta KK, Coats MA, Muich SJ, Grant E, … Morris JC (2005). The AD8: a brief informant interview to detect dementia. Neurology, 65(4), 559–564. doi: 10.1212/01.wnl.0000172958.95282.2a [DOI] [PubMed] [Google Scholar]
- Garrido MM, Kelley AS, Paris J, Roza K, Meier DE, Morrison RS, & Aldridge MD (2014). Methods for constructing and assessing propensity scores. Health Serv Res, 49(5), 1701–1720. doi: 10.1111/1475-6773.12182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler JE, Duval S, Anderson KA, & Kane RL (2007). Predicting nursing home admission in the U.S: a meta-analysis. BMC Geriatr, 7, 13. doi: 10.1186/1471-2318-7-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler JE, Kane RL, Kane RA, Clay T, & Newcomer R (2003). Caregiving and institutionalization of cognitively impaired older people: utilizing dynamic predictors of change. Gerontologist, 43(2), 219–229. [DOI] [PubMed] [Google Scholar]
- Gillsjo C, Schwartz-Barcott D, & von Post I (2011). Home: the place the older adult cannot imagine living without. BMC Geriatr, 11, 10. doi: 10.1186/1471-2318-11-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham CL, Scharlach AE, & Stark B (2017). Impact of the Village Model: Results of a National Survey. J Gerontol Soc Work, 60(5), 335–354. doi: 10.1080/01634372.2017.1330299 [DOI] [PubMed] [Google Scholar]
- Hanyok LA, Mullaney J, Finucane T, & Carrese J (2009). Potential caregivers for homebound elderly: more numerous than supposed? J Fam Pract, 58(7), E1–6. [PubMed] [Google Scholar]
- Hewko SJ, Cooper SL, Huynh H, Spiwek TL, Carleton HL, Reid S, & Cummings GG (2015). Invisible no more: a scoping review of the health care aide workforce literature. BMC Nurs, 14, 38. doi: 10.1186/s12912-015-0090-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasper JD, Freedman VA, & Spillman BC (2013). Classification of Persons by Dementia Status in the National Health and Aging Trends Study. Technical Paper #5 Baltimore: Johns Hopkins University School of Public Health. [Google Scholar]
- Kaye HS (2014). Toward a model long-term services and supports system: state policy elements. Gerontologist, 54(5), 754–761. doi: 10.1093/geront/gnu013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye HS, & Harrington C (2015). Long-term services and supports in the community: toward a research agenda. Disabil Health J, 8(1), 3–8. doi: 10.1016/j.dhjo.2014.09.003 [DOI] [PubMed] [Google Scholar]
- Kaye HS, Harrington C, & LaPlante MP (2010). Long-term care: who gets it, who provides it, who pays, and how much? Health Aff (Millwood), 29(1), 11–21. doi: 10.1377/hlthaff.2009.0535 [DOI] [PubMed] [Google Scholar]
- Leff B, Weston CM, Garrigues S, Patel K, Ritchie C, National Home-Based Primary C., & Palliative Care N. (2015). Home-based primary care practices in the United States: current state and quality improvement approaches. J Am Geriatr Soc, 63(5), 963–969. doi: 10.1111/jgs.13382 [DOI] [PubMed] [Google Scholar]
- Lowe B, Kroenke K, & Grafe K (2005). Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res, 58(2), 163–171. doi: 10.1016/j.jpsychores.2004.09.006 [DOI] [PubMed] [Google Scholar]
- Mahon GM (2014). Home care, need for increased physician involvement in the 21st century. J Am Med Dir Assoc, 15(8), 538–540. doi: 10.1016/j.jamda.2014.04.020 [DOI] [PubMed] [Google Scholar]
- Musich S, Wang SS, Hawkins K, & Yeh CS (2015). Homebound older adults: Prevalence, characteristics, health care utilization and quality of care. Geriatr Nurs, 36(6), 445–450. doi: 10.1016/j.gerinurse.2015.06.013 [DOI] [PubMed] [Google Scholar]
- NationalHelathandAgingTrendsStudy. (2018). National Helath and Aging Trends Study at a Glance from https://www.nhats.org/scripts/aboutNHATS.htm
- Ornstein KA, Leff B, Covinsky KE, Ritchie CS, Federman AD, Roberts L, … Szanton SL (2015). Epidemiology of the Homebound Population in the United States. JAMA Intern Med, 175(7), 1180–1186. doi: 10.1001/jamainternmed.2015.1849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ParaprofessionalHealthcareInstitute. (2017). U.S. Home Care Workers: Key Facts Retrieved 4/9/18, from https://phinational.org/resource/u-s-home-care-workers-key-facts/
- Qiu WQ, Dean M, Liu T, George L, Gann M, Cohen J, & Bruce ML (2010). Physical and mental health of homebound older adults: an overlooked population. J Am Geriatr Soc, 58(12), 2423–2428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotenberg J, Kinosian B, Boling P, Taler G, & Independence at Home Learning Collaborative Writing, G. (2018). Home-Based Primary Care: Beyond Extension of the Independence at Home Demonstration. J Am Geriatr Soc, 66(4), 812–817. doi: 10.1111/jgs.15314 [DOI] [PubMed] [Google Scholar]
- Sonnega A, Robinson K, & Levy H (2017). Home and community-based service and other senior service use: Prevalence and characteristics in a national sample. Home Health Care Serv Q, 36(1), 16–28. doi: 10.1080/01621424.2016.1268552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soones T, Federman A, Leff B, Siu AL, & Ornstein K (2017). Two-Year Mortality in Homebound Older Adults: An Analysis of the National Health and Aging Trends Study. J Am Geriatr Soc, 65(1), 123–129. doi: 10.1111/jgs.14467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szanton SL, Roberts L, Leff B, Walker JL, Seplaki CL, Soones T, … Ornstein KA (2016). Home but still engaged: participation in social activities among the homebound. Qual Life Res, 25(8), 1913–1920. doi: 10.1007/s11136-016-1245-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Houtven CH, & Norton EC (2004). Informal care and health care use of older adults. J Health Econ, 23(6), 1159–1180. doi: 10.1016/j.jhealeco.2004.04.008 [DOI] [PubMed] [Google Scholar]
- Wajnberg A, Ornstein K, Zhang M, Smith KL, & Soriano T (2013). Symptom Burden in Chronically Ill Homebound Individuals. J Am Geriatr Soc, 61(1), 126–131. doi: 10.1111/jgs.12038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Leifheit-Limson EC, Fine J, Pandolfi MM, Gao Y, Liu F, … Lichtman JH (2017). National Trends and Geographic Variation in Availability of Home Health Care: 2002–2015. J Am Geriatr Soc, 65(7), 1434–1440. doi: 10.1111/jgs.14811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wild B, Eckl A, Herzog W, Niehoff D, Lechner S, Maatouk I, … Lowe B (2014). Assessing generalized anxiety disorder in elderly people using the GAD-7 and GAD-2 scales: results of a validation study. Am J Geriatr Psychiatry, 22(10), 1029–1038. doi: 10.1016/j.jagp.2013.01.076 [DOI] [PubMed] [Google Scholar]
- Wolff JL, Spillman BC, Freedman VA, & Kasper JD (2016). A National Profile of Family and Unpaid Caregivers Who Assist Older Adults With Health Care Activities. JAMA Intern Med, 176(3), 372–379. doi: 10.1001/jamainternmed.2015.7664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wysocki A, Butler M, Kane RL, Kane RA, Shippee T, & Sainfort F (2015). Long-Term Services and Supports for Older Adults: A Review of Home and Community-Based Services Versus Institutional Care. J Aging Soc Policy, 27(3), 255–279. doi: 10.1080/08959420.2015.1024545 [DOI] [PubMed] [Google Scholar]


