Abstract
Very early stage hepatocellular carcinoma (HCC) is defined as a single tumor with the largest diameter of the lesion measuring 2 cm or less according to Barcelona Liver Cancer staging system. Detection of very early stage HCC is clinically important as it confers an excellent prognosis with the 5-year survival rates over 60 to 80% after patients receive curative treatments. While diagnosing HCC at a very early stage is crucial, it is technically challenging and may come with the physical or psychosocial harms related to diagnostic tests. It is further complicated by the fact that patients with very early stage HCC are not prioritized for liver transplant (LT) in the United States organ allocation system. When LT-eligible patients present with an indeterminate lesion measuring between 1 and 2 cm on the multiphasic computed tomography or magnetic resonance imaging, clinicians often observe patients carefully until the lesion grows up to 2 cm so that patients can be eligible to receive a Model for End-Stage Liver Disease (MELD) exception score for HCC in the United States. The European guideline recommends a routine biopsy of such lesion. In conclusion, attempting to detect very early stage HCC is difficult to achieve and controversial. Clinicians should take into account of the risk and the benefit of diagnostic tests, LT candidacy of patients and the local organ allocation system.
Keywords: Liver cancer, Hepatocellular cancer, Diagnosis, Hepatocellular carcinoma (HCC)
INTRODUCTION
Early detection of hepatocellular carcinoma (HCC) is important as a tumor stage at the time of diagnosis is closely related to the clinical outcomes [1,2]. While patients with very early stage HCC have excellent clinical outcome, diagnosing cancer at a very early stage is technically challenging. Noninvasive diagnosis of HCC is established by characteristic radiologic features in the liver specific multiphasic computed tomography (CT) or magnetic resonance imaging (MRI) in cirrhotic patients [3-5]. Attempting to establish HCC diagnosis at a very early stage may come with risks. For instance, biopsy could be considered in further interrogation of indeterminate lesions on CT or MRI. It can cause complications, including but not limited to bleeding and needle track tumor seedings [6,7]. Although biopsy is highly specific for HCC diagnosis, but it is not sensitive for the diagnosis of very early stage HCC due to difficulties with accurate targeting of the small lesion [8]. Furthermore, patients with very early stage HCC are not eligible to receive a Model for End-Stage Liver Disease (MELD) exception score in the current organ allocation system in the United States, hampering the enthusiasm for detection of HCC at a very early stage especially in the liver transplant (LT) candidates [9]. This article discussed the definition of very early stage HCC, rationales and challenges in attempting to detect tumors at a very early stage, recall policy for indeterminate liver nodule and implication of the United States organ allocation system in the clinical practice.
DEFINITION OF VERY EARLY STAGE HCC
While a number of staging systems have been proposed for HCC, only few of them have specific definition of very early stage of HCC [10,11]. Very early stage of HCC has clearly distinct clinical characteristics in diagnosis and prognosis and detection of cancers at a very early stage is a goal of liver cancer surveillance program in high risk individuals. The Barcelona Liver Cancer (BCLC) classification is a standard staging system endorsed by the American Association for the Study of Liver Diseases (AASLD) and the European Association for the Study of the Liver (EASL) [3,4,12]. According to the BCLC staging system, very early stage HCC is defined as a single tumor with the largest diameter of 2 cm or less, well-preserved liver function without vascular invasion or metastasis [10]. Patients with very early stage HCC are recommended to undergo ablation or resection for potentially curative treatments and their outcome is excellent with the 5-year overall survival over 60–80% [13,14]. ITA.LI.CA tumor staging system also had the same definition for very early stage HCC, namely, a single nodule and 2 cm or less in size from the extent of tumor standpoint [11,15].
RATIONALE FOR DETECTING VERY EARLY STAGE HCC
Detection of very early stage HCC is crucial as patients presenting at this stage have excellent prognosis [13,14]. A multicenter surgical series of 132 patients in the United States and Italy showed the median survival of 75 months with the 5-year survival rate of 70% after surgical resection of HCC [13]. Japanese nationwide survey of patients who underwent curative treatments for very early stage HCC with preserved liver function (Child-Turcotte-Pugh [CTP] class A) had the 5-year survival of 84% after surgical resection (n=785) and 77% after percutaneous ethanol ablation (n=543) [14]. The study demonstrated that the size of the lesions is closely associated with the prognosis of patients after curative treatment even when the size of the tumor is still small [14]. The 5-year- overall survival rate decreased by 10% after curative resection or ablation once tumor size was between 2-3 cm compared to survival probability of patients with tumor size 2 cm or less, highlighting the clinically meaningful superiority in overall survival in patients with a very early stage HCC over an early stage HCC [14].
Attempting to diagnose a very early stage HCC may also help clinicians to find different types of liver cancer, most commonly intrahepatic cholangiocarcinoma (iCCA), which can affect transplant candidacy of the patients and their long-term outcome. For instance, several studies showed that a small subgroup of patients with iCCA could potentially benefit from LT [16-18]. A recent retrospective multicenter study of 81 patients from 17 LT centers showed that patients with a very early stage iCCA (single nodule and 2 cm or smaller in the tumor size) at explant had the 5-year post-transplant tumor recurrence rates of 18% and the 5-year overall survival rates of 65% [16]. On the other hand, patients with beyond very early stage disease, of whom 80% were still within Milan criteria, had the 5-year post-transplant recurrence rates of 61% and the 5-year overall survival rates of 45%. Author also reported an outcome of group of patients with single tumor, size between 2.1 and 3 cm without poor differentiation on histology. The 5-year overall survival rates were 61%, which is within acceptable range for LT. Given promising outcome of selected subgroup of patients with small solitary iCCA after LT, several transplant centers adopted a LT protocol for iCCA. The iCCA protocol at the Mayo clinic was summarized in Table 1. Currently, most transplant center in the United States would not consider LT in patients with multifocal iCCA even if patients present within Milan criteria due to poor post-LT outcomes.
Table 1.
Liver transplant criteria for intrahepatic cholangiocarcinoma at Mayo Clinic
| Biopsy proven unresectable intrahepatic cholangiocarcinoma |
| Single lesion ≤3 cm in diameter |
| No macrovascular invasion |
| No microvascular invasion |
| No poorly differentiated histology |
| No evidence of extrahepatic disease |
| No attempted prior resection with violation of tumor plane |
| Reasonable candidate for liver transplant |
Patients should meet all listed criteria.
DIAGNOSTIC CHALLENGES
Diagnosing a very early stage HCC is challenging to achieve in the western population. A previous study showed that up to 15 to 20% of HCC seen in the explant were incidental finding, meaning that these tumors were not recognized in routine pre-transplant liver images [19]. A recent multicenter study showed that almost half of the patients with a very early stage iCCA (46.7%) had been transplanted without pre-transplant radiologic recognition of a suspicious hepatic nodule. One study showed that underlying etiology of alcohol or hepatitis C virus (HCV), old age, and increased alpha-fetoprotein (AFP) were associated with presence of incidental HCC [20].
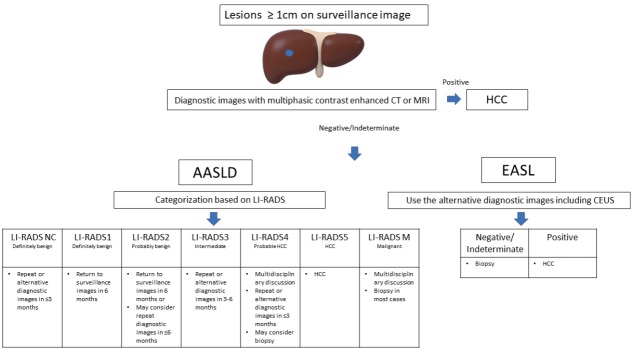
Liver ultrasound is a standard surveillance imaging test for HCC [3,4]. However, quality of liver ultrasound as a surveillance test is often limited due to high prevalence of obesity and metabolic liver disease in the western countries [21,22]. A recent retrospective multicenter study evaluated the quality of ultrasonography (US) image as a surveillance test. Radiologists reviewed all ultrasound exams in 941 cirrhosis patients and 20% of ultrasound images were inadequate for excluding HCC. Male gender, body mass index, CTP B or C cirrhosis, alcohol-related and non-alcoholic steatohepatitis-related cirrhosis were independently associated with inadequate US [22]. A recent meta-analysis showed that ultrasound alone has 47% sensitivity for detection of early stage HCC. Although there was an increase in sensitivity in the recent era (50% for study conducted after 2000), it did not reach a statistical significance [23]. Due to limited sensitivity of liver US for detection of HCC, cross-sectional images have been entertained as a surveillance test. Four phasic CT or dynamic MRI are essential non-invasive diagnostic modalities for HCC [24,25]. Diagnosis is achieved when the lesion is at least 1 cm or larger in size with characteristic enhancement patterns, namely arterial phase hyperenhancement and washout in the portal venous or delayed phase on CT or MRI (Fig. 1) [3,26]. More recently, AASLD adopted the Liver Imaging Reporting And Data System (LI-RADS) for non-invasive diagnosis of HCC, which was originally developed to standardize radiological diagnosis and reporting, define minimum imaging technical requirements, and create a mechanism for formal data collection in patients at risk for HCC [27,28]. According to the most recent LIRADS, size of the lesion affects the diagnostic criteria for HCC. For lesion ≥2 cm, non-rim arterial phase hyperenhancement and one more feature (enhancing capsule, non-peripheral washout, or threshold growth) are diagnostic for HCC. For lesion between 1 and 2 cm, non-rim arterial phase hyperenhancement and one more feature (non-peripheral washout or threshold growth) are diagnostic for HCC (Fig. 1) [28]. The non-invasive criteria should be applied only in patients with underlying cirrhosis of the liver given high pretest probability. One positive test is enough to confirm the diagnosis [29].
Figure 1.
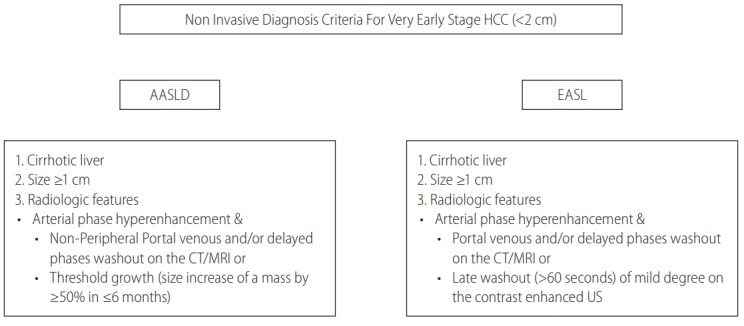
Noninvasive diagnosis criteria for very early stage hepatocellular carcinoma (HCC). Modified from European Association for the Study of the Liver [3] and Marrero et al. [4] AASLD, the American Association for the Study of Liver Diseases; EASL, the European Association for the Study of the Liver; CT, computed tomography; MRI, magnetic resonance images; US, ultrasonography.
Several studies compared the diagnostic performance of multiphasic CT, MRI and liver US for detection of HCC [29-33]. One study reviewed CT or MRI features in the 101 nodules (34% were malignant lesions) of 84 cirrhosis patients. The sensitivity of CT and MRI was only 53% and 62%, respectively for the diagnosis of HCC. A recent study investigated the performance of MRI with liver-specific contrast (gadoxetic acid) for detection of HCC in the surveillance setting [32]. This study analyzed 407 high-risk cirrhosis patients (estimated annual risk of HCC development >5%) who underwent 1,100 surveillance tests with paired US and MRI. The HCC detection rate was much higher with MRI (86.0%) than US (27.9%). MRI showed a significantly lower rate of false-positive findings than US. Of the 43 patients with HCC, 32 (74.4%) had very early stage HCC, suggesting that MRI with liver-specific contrast may be an excellent surveillance test although it still missed to detect very early stage HCC in a quarter of the patients. Overall, MRI appears to have a higher sensitivity in detecting HCC over CT scan [34]. A recent meta-analysis showed a pooled sensitivity of 82% and 66% for MRI and CT for detection of HCC, respectively (P<0.01) [34]. A subgroup analysis showed a numerically higher sensitivity of 76% for MRI than 68% for CT for the detection of hepatic lesion less than 2 cm, but it did not reach a statistical significance [34]. Routine use of MRI or CT scan could be considered to increase the probability of capturing small lesions less than 2 cm, but it can pose physical or psychosocial harm and may not be cost-effective [35]. However, a recent Markov modeling study suggested that using cross-sectional images could be cost-effective in high-risk patients. The study showed that MRI is a cost-effective surveillance test in high-risk HCC patients with an annual incidence rate of 1.81% or higher when the incremental cost-effectiveness ratio becomes $50,000 or less per one quality-adjusted life-years [36].
With regard to blood-based diagnostic tests, AFP alone appears to have suboptimal performance for detection of early stage HCC [27,37]. But it appears to be helpful in detecting early stage HCC as combination of the other diagnostic test [38]. A recent study showed that AFP is an independent risk factor of HCC development in cirrhotic patients with indeterminate nodules (<2 cm) detected on the CT scan [39]. It should be noted that AFP levels can be falsely elevated in patients with underlying hepatic inflammation, particularly with hepatitis B virus (HBV) or C virus infection, but appear to be an excellent biomarker in patients with normal alanine aminotransferase (ALT) [40,41]. Several studies showed that longitudinal measurement of tumor markers might be helpful for the detection of HCC too [42,43]. AFP-L3% and des-gamma-carboxy prothrombin (DCP) appear to have complementary roles for detection of HCC [27,44]. A recent phase 3 diagnostic biomarker study showed that the combination of AFP (5 ng/mL) and AFP-L3 (4%) provide a sensitivity and specificity of 79% and 87% for detection of HCC, respectively [42]. Over 90% had HCC within Milan criteria and 74% had very early stage HCC in that study [42]. HBV (79%) was the leading etiology of HCC and most patients had normal ALT (87%), due to successful control of viral replication with potent antiviral treatment. Overall performance of AFP L3% was superior to liver ultrasound whose sensitivity was only 49%. A recent United States study showed that the GALAD score, a composite of demographic risk factors (age and male gender) and three serum-based biomarkers (AFP, AFP-L 3% and DCP) might be a promising risk score for detection of very early stage HCC with the sensitivity of 100% at the specificity of 79% with the area under the curve (AUC) of 0.91 [21]. A multicenter study from UK, Germany and Japan showed similar results with the AUC ranging between 0.89 and 0.92 for detection of very early stage HCC [45]. More recently, improvement of next-generation sequencing technology and better understanding of genetic or epigenetic alteration of HCC have allowed comprehensive analysis of mutational and methylation landscape of circulating nucleic acid-based biomarkers. Circulating cell free DNA (cfDNA) is a fragmented DNA subtype, found in the blood circulation. Circulating tumor DNA is the fraction of total cfDNA, which originates from the primary tumor or metastases in patients with cancer. One study reported 6-marker cfDNA methylation panel and it yielded the 95% sensitivity and the 92% specificity with the AUC of 0.96 for HCC detection [46]. Of note, the cfDNA methylation panel detected 75% of very early stage HCC and 93% of patients meeting Milan criteria for HCC [46]. So far, none of circulating nucleic acid-based biomarkers have yet been validated in longitudinal cohorts for pre-clinical detection of HCC. Overall, data in the literature highlight the limited sensitivity of current radiologic and blood-based tests for very early stage HCC detection and fine characterization of these small lesions.
LIVER TRANSPLANT FOR HCC; ORGAN ALLOCATION HISTORY IN THE UNITED STATES
LT is a potentially curative treatment option for HCC. While it is a highly resource intensive treatment, it is the most definitive treatment for HCC as it removes not only the tumor, but also the diseased liver, which may contain foci of microscopic metastasis or serve as nidus for the development of de novo HCC [47]. Hence, recurrence rate of HCC after LT is less than 15%, which is substantially lower than 70% recurrence rate after other curative treatments such as resection or ablation [13,14,48]. For this reason, LT has been increasingly utilized for the treatment of HCC and a recent study showed that HCC is the leading indication for LT listing and surgery in the United States [49].
The MELD score was developed to predict 3-month mortality in patients with end-stage liver disease and was adopted by United Network for Organ Sharing for organ allocation [50,51]. Patients listed for LT with HCC typically have lower MELD scores than patients listed without HCC, thus MELD score underestimated the risk of mortality on the waitlisted HCC patients. Thus, MELD exception point was granted in HCC patients since 2002 if the tumors were within Milan criteria (one lesion less than 5 cm or up to 3 lesions with the largest lesion less than 3 cm). As patients with larger tumor burden had an increased risk of tumor progression and subsequent dropout of the listing, patients with T2 disease (1 lesion between 2 and 5 cm or 2–3 lesions with none larger than 3 cm) received a MELD exception score of 29. Those with T1 (solitary lesion <2 cm) disease received 24 instead of 29 as their risk of tumor progression and likelihood of subsequent dropout of the listing and death was lower than those with T2 disease. However, concerns were raised that patients with HCC were advantageous due to excessive exception point. To address this limitation, several revisions were made for MELD exception policy for HCC to achieve the balance of benefit between HCC and non-HCC patients [9]. HCC MELD exception point has been decreasing over time since and no exception point was granted for T1 lesions since 2004. Most recent change was made in 2015 and patient should now remain on their biologic MELD score for the first 6 months after listing and patients are granted MELD score of 28 after 6 months of waiting on the list with the cap MELD of 34 [52].
Lack of MELD exception point for T1 lesion has made a huge impact on the approach for detection of very early stage HCC especially in patients who are eligible for LT as patients with very early stage HCC are no longer prioritized for LT in the United States organ allocation system. Patients with very early stage HCC often have to wait until tumor grows beyond the very early stage when they are eligible to receive MELD exception score. Patients with indeterminate small lesions on diagnostic images (multiphasic CT or MRI) often have been closely followed up without percutaneous biopsy of the liver lesion. A recent study from University of California, San Francisco investigated the outcome of the “wait and not ablate” approach in 114 patients with T1 HCC (1 lesion <2 cm) [53]. Patients were monitored with cross-sectional images every 3 months. Vast majority of HCC patients (88%) had stage progression from T1 to T2 (1 lesion 2–5 cm or 2–3 lesions ≤3 cm) at a median duration of 6.9 months. Only six (5.3%) patients progressed from T1 directly to beyond T2 criteria at a median duration of 5.1 months [53]. While tumor biology may change with the progression of disease, the probability of tumor progression appears to be low enough that most transplant centers favor close observation in this setting rather than subjecting patients to percutaneous biopsy in otherwise good candidate for LT. For patients who would not be a good candidate for LT, attempting to establish a very early stage HCC is crucial to improve clinical outcome. Percutaneous biopsy is often performed followed by a local ablation in such patients with indeterminate lesion on CT or MRI measured between 1 and 2 cm.
RECALL POLICY FOR INDETERMINATE LIVER MASS ON SURVEILLANCE ULTRASOUND
In the setting of HCC surveillance, liver ultrasound may show small indeterminate lesions. The algorithm to be followed abnormal surveillance tests is called a recall policy. A recall policy is essentially the same between the AASLD and the EASL when the lesion is less than 1 cm in size (Fig. 2) [3,4]. Probability of these lesions measuring 1 cm or less representing HCC is very slim [8]. Therefore, diagnostic image is not recommended but follow up liver ultrasound is recommended between 3 and 6 months. The recall policy is somewhat different when the lesion is between 1 and 2 cm between the AASLD and the EASL. The AASLD and the EASL both recommend that the lesions be further characterized by multiphasic liver-specific CT or MRI. The AASLD adopted LIRADS for noninvasive diagnosis of HCC [54]. LI-RADS system classifies lesions into 7 different categories (Fig. 2) [28,55]. LI-RADS 1 lesions are definitively benign and return to regular surveillance imaging every 6 months is recommended. LI-RADS 2 lesions are probably benign and return to regular surveillance imaging every 6 months is recommended although further diagnostic imaging could be considered in 6 months or less depending on other risk factors. LI-RADS 3 lesions has intermediate probability for HCC and repeat or alternative diagnostic imaging is recommended in 3–6 months. LI-RADS 4 lesions are probably HCC and repeat or alternative diagnostic imaging is recommended in less than 3 months. Biopsy of the LI-RADS 4 lesion could be considered after multi-disciplinary discussion in selected cases. LI-RADS 5 lesions are diagnostic for HCC. LI-RADS added two additional categories. LI-RADS NC refers to non-categorizable lesions due to images omission or severe degradation and LI-RADS M refers to lesions that are consistent with malignancy, but not definitively HCC. A recent meta-analysis reported the pooled percentages of observations confirmed as HCC in 3,556 observations from 2,760 patients, of whom 2,482 had HCCs [56]. The pooled percentages for the lesions representing HCC were 94% for LR-5, 74% for LR-4, 38% for LR-3, 13% for LR-2, 0% for LR-1 and 36% for the LR-M group. AASLD does not recommend a routine biopsy of indeterminate lesion as it may harm patients with complications including bleeding or tumor seeding [6,7]. However, biopsy would be an excellent diagnostic tool for detection of very early stage HCC especially in selected cases of LI-RADS 4 lesions as it may facilitate early diagnosis of HCC.
Figure 2.
Comparison of recall policy between the American Association for the Study of Liver Diseases (AASLD) and the European Association for the Study of the Liver (EASL) guideline. Adapted from European Association for the Study of the Liver [3] and Marrero et al. [4] CT, computed tomography; MRI, magnetic resonance imaging; HCC, hepatocellular carcinoma; LI-RADS, Liver Imaging Reporting And Data System; CEUS, contrast-enhanced ultrasound.
The EASL proposes different approaches (Fig. 2) [3]. When a surveillance US shows lesions less than 1 cm, repeat US is recommended in 4 months without diagnostic images. Once the lesion measures 1 cm or over, diagnostic tests should be performed for further characterization. The EASL recommends a multiphasic CT or MRI as a first-line diagnostic test, but also consider contrastenhanced ultrasound (CEUS) as a diagnostic test. A recent retrospective study showed that characteristic features of CEUS (arterial enhancement followed by late washout, onset >60 seconds after contrast injection) have a positive predictive value of HCC at 99% without misclassification for cholangiocarcinoma [57]. A recent multicenter prospective study showed that the specificity of CEUS for the diagnosis of HCC in 1–2 cm lesion is 93%, which is higher than 83% for MRI and 77% for CT [58]. However, CEUS has a relatively low sensitivity and cannot examine the entire liver due to very short arterial phase. Its performance may also be affected by body habitus of the patients and location of the lesion. Further, patients will need a staging cross-sectional image once HCC is confirmed. Hence, CEUS is not recommended as a first-line diagnostic images but could be an effective diagnostic test in patients when CT and MRI are contraindicated or show inconclusive lesions [3]. If any of three images shows diagnostic features of HCC, then HCC diagnosis can be secured. However, if any of the three images fail to show characteristic features of HCC, then biopsy is recommended. This contrasts to the recommendation from the AASLD where routine biopsy of such lesions is discouraged. The rationales to establish the diagnosis early on is because delaying it until tumor reaches 2 cm or larger can increase the probability of treatment failure or recurrence as tumor start developing satellite nodules or microscopic vascular invasion once it transitions from very early stage to early stage HCC [3]. For this reason, the EASL recommends a routine biopsy of these lesions regardless of LI-RADS classification as lower LI-RADS classes do not rule out the presence of HCC. It is therefore controversial as to how aggressively clinicians should diagnose HCC at a very early stage especially in LT candidates in the United States. It is less debatable in patients who would not be a candidate for LT because detection of very early stage HCC seems to improve clinical outcome.
CONCLUSIONS
In conclusion, detection of very early stage HCC is important as it leads to an excellent overall survival after curative treatment. However, diagnosis of HCC at a very early stage is technically challenging due to limited performance and risk of available diagnostic tests. The current organ allocation system in the United States made a huge impact on diagnostic approaches in patients with small indeterminate lesions seen in the surveillance ultrasound and subsequent diagnostic image tests. Use of liver biopsy for the detection of very early stage HCC is particularly controversial between the United States and European guideline. Novel blood-based biomarkers showed promising performances for the detection of very early stage HCC. Circulating DNA-based biomarkers in combination with images may improve the diagnostic performance and safety of surveillance tests, which can facilitate the diagnosis of very early stage HCC in the near future.
Abbreviations
- AASLD
the American Association for the Study of Liver Diseases
- AFP
alphafetoprotein
- ALT
alanine aminotransferase
- AUC
area under the curve
- BCLC
Barcelona Liver Cancer
- CEUS
contrast-enhanced ultrasound
- CT
computed tomography
- ctDNA
circulating tumor DNA
- CTP
Child-Turcotte-Pugh
- DCP
desgamma-carboxy prothrombin
- EASL
the European Association for the Study of the Liver
- HBV
hepatitis B virus
- HCC
hepatocellular carcinoma
- HCV
hepatitis C virus
- iCCA
intrahepatic cholangiocarcinoma
- LI-RADS
Liver Imaging Reporting And Data System
- LT
liver transplant
- MELD
Model for End-Stage Liver Disease
- MRI
magnetic resonance imaging
- US
ultrasonography
Footnotes
Conflicts of Interest The author has no conflicts to disclose.
REFERENCES
- 1.Yang JD, Harmsen WS, Slettedahl SW, Chaiteerakij R, Enders FT, Therneau TM, et al. Factors that affect risk for hepatocellular carcinoma and effects of surveillance. Clin Gastroenterol Hepatol. 2011;9:617–623.:e1. doi: 10.1016/j.cgh.2011.03.027. [DOI] [PubMed] [Google Scholar]
- 2.Yang JD, Kim WR, Park KW, Chaiteerakij R, Kim B, Sanderson SO, et al. Model to estimate survival in ambulatory patients with hepatocellular carcinoma. Hepatology. 2012;56:614–621. doi: 10.1002/hep.25680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.European Association for the Study of the Liver EASL Clinical Practice Guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69:182–236. doi: 10.1016/j.jhep.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 4.Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS, Abecassis MM, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018;68:723–750. doi: 10.1002/hep.29913. [DOI] [PubMed] [Google Scholar]
- 5.Omata M, Cheng AL, Kokudo N, Kudo M, Lee JM, Jia J, et al. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int. 2017;11:317–370. doi: 10.1007/s12072-017-9799-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Silva MA, Hegab B, Hyde C, Guo B, Buckels JA, Mirza DF. Needle track seeding following biopsy of liver lesions in the diagnosis of hepatocellular cancer: a systematic review and meta-analysis. Gut. 2008;57:1592–1596. doi: 10.1136/gut.2008.149062. [DOI] [PubMed] [Google Scholar]
- 7.Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD, American Association for the Study of Liver Diseases Liver biopsy. Hepatology. 2009;49:1017–1044. doi: 10.1002/hep.22742. [DOI] [PubMed] [Google Scholar]
- 8.Forner A, Vilana R, Ayuso C, Bianchi L, Solé M, Ayuso JR, et al. Diagnosis of hepatic nodules 20 mm or smaller in cirrhosis: prospective validation of the noninvasive diagnostic criteria for hepatocellular carcinoma. Hepatology. 2008;47:97–104. doi: 10.1002/hep.21966. [DOI] [PubMed] [Google Scholar]
- 9.Rich NE, Parikh ND, Singal AG. Hepatocellular carcinoma and liver transplantation: changing patterns and practices. Curr Treat Options Gastroenterol. 2017;15:296–304. doi: 10.1007/s11938-017-0133-3. [DOI] [PubMed] [Google Scholar]
- 10.Llovet JM, Brú C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis. 1999;19:329–338. doi: 10.1055/s-2007-1007122. [DOI] [PubMed] [Google Scholar]
- 11.Farinati F, Vitale A, Spolverato G, Pawlik TM, Huo TL, Lee YH, et al. Development and validation of a new prognostic system for patients with hepatocellular carcinoma. PLoS Med. 2016;13:e1002006. doi: 10.1371/journal.pmed.1002006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet. 2003;362:1907–1917. doi: 10.1016/S0140-6736(03)14964-1. [DOI] [PubMed] [Google Scholar]
- 13.Roayaie S, Obeidat K, Sposito C, Mariani L, Bhoori S, Pellegrinelli A, et al. Resection of hepatocellular cancer ≤2 cm: results from two Western centers. Hepatology. 2013;57:1426–1435. doi: 10.1002/hep.25832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hasegawa K, Kokudo N, Makuuchi M, Izumi N, Ichida T, Kudo M, et al. Comparison of resection and ablation for hepatocellular carcinoma: a cohort study based on a Japanese nationwide survey. J Hepatol. 2013;58:724–729. doi: 10.1016/j.jhep.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 15.Borzio M, Dionigi E, Rossini A, Marignani M, Sacco R, De Sio I, et al. External validation of the ITA.LI.CA prognostic system for patients with hepatocellular carcinoma: a multicenter cohort study. Hepatology. 2018;67:2215–2225. doi: 10.1002/hep.29662. [DOI] [PubMed] [Google Scholar]
- 16.Sapisochin G, Facciuto M, Rubbia-Brandt L, Marti J, Mehta N, Yao FY, et al. Liver transplantation for “very early” intrahepatic cholangiocarcinoma: international retrospective study supporting a prospective assessment. Hepatology. 2016;64:1178–1188. doi: 10.1002/hep.28744. [DOI] [PubMed] [Google Scholar]
- 17.Sapisochin G, Rodríguez de Lope C, Gastaca M, Ortiz de Urbina J, Suarez MA, Santoyo J, et al. “Very early” intrahepatic cholangiocarcinoma in cirrhotic patients: should liver transplantation be reconsidered in these patients? Am J Transplant. 2014;14:660–667. doi: 10.1111/ajt.12591. [DOI] [PubMed] [Google Scholar]
- 18.Sapisochin G, de Lope CR, Gastaca M, de Urbina JO, López-Andujar R, Palacios F, et al. Intrahepatic cholangiocarcinoma or mixed hepatocellular-cholangiocarcinoma in patients undergoing liver transplantation: a Spanish matched cohort multicenter study. Ann Surg. 2014;259:944–952. doi: 10.1097/SLA.0000000000000494. [DOI] [PubMed] [Google Scholar]
- 19.Sotiropoulos GC, Malagó M, Molmenti EP, Nadalin S, Radtke A, Brokalaki EI, et al. Liver transplantation and incidentally found hepatocellular carcinoma in liver explants: need for a new definition? Transplantation. 2006;81:531–535. doi: 10.1097/01.tp.0000198739.42548.3e. [DOI] [PubMed] [Google Scholar]
- 20.Senkerikova R, Frankova S, Sperl J, Oliverius M, Kieslichova E, Filipova H, et al. Incidental hepatocellular carcinoma: risk factors and long-term outcome after liver transplantation. Transplant Proc. 2014;46:1426–1429. doi: 10.1016/j.transproceed.2014.03.010. [DOI] [PubMed] [Google Scholar]
- 21.Yang JD, Addissie BD, Mara KC, Harmsen WS, Dai J, Zhang N, et al. GALAD score for hepatocellular carcinoma detection in comparison to liver ultrasound and proposal of GALADUS Score. Cancer Epidemiol Biomarkers Prev. 2019;28:531–538. doi: 10.1158/1055-9965.EPI-18-0281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Simmons O, Fetzer DT, Yokoo T, Marrero JA, Yopp A, Kono Y, et al. Predictors of adequate ultrasound quality for hepatocellular carcinoma surveillance in patients with cirrhosis. Aliment Pharmacol Ther. 2017;45:169–177. doi: 10.1111/apt.13841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tzartzeva K, Obi J, Rich NE, Parikh ND, Marrero JA, Yopp A, et al. Surveillance imaging and alpha fetoprotein for early detection of hepatocellular carcinoma in patients with cirrhosis: a meta-analysis. Gastroenterology. 2018;154:1706–1718. doi: 10.1053/j.gastro.2018.01.064. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bruix J, Sherman M, Llovet JM, Beaugrand M, Lencioni R, Burroughs AK, et al. Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol. 2001;35:421–430. doi: 10.1016/s0168-8278(01)00130-1. [DOI] [PubMed] [Google Scholar]
- 25.Bruix J, Sherman M, Practice Guidelines Committee, American Association for the Study of Liver Diseases Management of hepatocellular carcinoma. Hepatology. 2005;42:1208–1236. doi: 10.1002/hep.20933. [DOI] [PubMed] [Google Scholar]
- 26.Bruix J, Sherman M, American Association for the Study of Liver Diseases Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–1022. doi: 10.1002/hep.24199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marrero JA, Feng Z, Wang Y, Nguyen MH, Befeler AS, Roberts LR, et al. Alpha-fetoprotein, des-gamma carboxyprothrombin, and lectinbound alpha-fetoprotein in early hepatocellular carcinoma. Gastroenterology. 2009;137:110–118. doi: 10.1053/j.gastro.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tang A, Singal AG, Mitchell DG, Hecht EM, Fowler KJ, Kulik L, et al. Introduction to the Liver Imaging Reporting and Data System (LI-RADS) for hepatocellular carcinoma. Clin Gastroenterol Hepatol. 2019;17:1228–1238. doi: 10.1016/j.cgh.2018.10.014. [DOI] [PubMed] [Google Scholar]
- 29.Khalili K, Kim TK, Jang HJ, Haider MA, Khan L, Guindi M, et al. Optimization of imaging diagnosis of 1-2 cm hepatocellular carcinoma: an analysis of diagnostic performance and resource utilization. J Hepatol. 2011;54:723–728. doi: 10.1016/j.jhep.2010.07.025. [DOI] [PubMed] [Google Scholar]
- 30.Pocha C, Dieperink E, McMaken KA, Knott A, Thuras P, Ho SB. Surveillance for hepatocellular cancer with ultrasonography vs. computed tomography -- a randomised study. Aliment Pharmacol Ther. 2013;38:303–312. doi: 10.1111/apt.12370. [DOI] [PubMed] [Google Scholar]
- 31.Van Thiel DH, Yong S, Li SD, Kennedy M, Brems J. The development of de novo hepatocellular carcinoma in patients on a liver transplant list: frequency, size, and assessment of current screening methods. Liver Transpl. 2004;10:631–637. doi: 10.1002/lt.20120. [DOI] [PubMed] [Google Scholar]
- 32.Kim SY, An J, Lim YS, Han S, Lee JY, Byun JH, et al. MRI with liverspecific contrast for surveillance of patients with cirrhosis at high risk of hepatocellular carcinoma. JAMA Oncol. 2017;3:456–463. doi: 10.1001/jamaoncol.2016.3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shah TU, Semelka RC, Pamuklar E, Firat Z, Gerber RD, Shrestha R, et al. The risk of hepatocellular carcinoma in cirrhotic patients with small liver nodules on MRI. Am J Gastroenterol. 2006;101:533–540. doi: 10.1111/j.1572-0241.2006.00450.x. [DOI] [PubMed] [Google Scholar]
- 34.Roberts LR, Sirlin CB, Zaiem F, Almasri J, Prokop LJ, Heimbach JK, et al. Imaging for the diagnosis of hepatocellular carcinoma: a systematic review and meta-analysis. Hepatology. 2018;67:401–421. doi: 10.1002/hep.29487. [DOI] [PubMed] [Google Scholar]
- 35.Atiq O, Tiro J, Yopp AC, Muffler A, Marrero JA, Parikh ND, et al. An assessment of benefits and harms of hepatocellular carcinoma surveillance in patients with cirrhosis. Hepatology. 2017;65:1196–1205. doi: 10.1002/hep.28895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim HL, An J, Park JA, Park SH, Lim YS, Lee EK, et al. Magnetic resonance imaging is cost-effective for hepatocellular carcinoma surveillance in high risk patients with cirrhosis. Hepatology. 2019;69:1599–1613. doi: 10.1002/hep.30330. [DOI] [PubMed] [Google Scholar]
- 37.Forner A, Reig M, Bruix J. Alpha-fetoprotein for hepatocellular carcinoma diagnosis: the demise of a brilliant star. Gastroenterology. 2009;137:26–29. doi: 10.1053/j.gastro.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 38.Chang TS, Wu YC, Tung SY, Wei KL, Hsieh YY, Huang HC, et al. Alpha-fetoprotein measurement benefits hepatocellular carcinoma surveillance in patients with cirrhosis. Am J Gastroenterol. 2015;110:836–844. doi: 10.1038/ajg.2015.100. quiz 845. [DOI] [PubMed] [Google Scholar]
- 39.Cho HJ, Kim B, Lee JD, Kang DR, Kim JK, Lee JH, et al. Development of risk prediction model for hepatocellular carcinoma progression of indeterminate nodules in hepatitis B virus-related cirrhotic liver. Am J Gastroenterol. 2017;112:460–470. doi: 10.1038/ajg.2016.480. [DOI] [PubMed] [Google Scholar]
- 40.Yang JD, Dai J, Singal AG, Gopal P, Addissie BD, Nguyen MH, et al. Improved performance of serum alpha-fetoprotein for hepatocellular carcinoma diagnosis in HCV cirrhosis with normal alanine transaminase. Cancer Epidemiol Biomarkers Prev. 2017;26:1085–1092. doi: 10.1158/1055-9965.EPI-16-0747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sterling RK, Wright EC, Morgan TR, Seeff LB, Hoefs JC, Di Bisceglie AM, et al. Frequency of elevated hepatocellular carcinoma (HCC) biomarkers in patients with advanced hepatitis C. Am J Gastroenterol. 2012;107:64–74. doi: 10.1038/ajg.2011.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Choi J, Kim GA, Han S, Lee W, Chun S, Lim YS, et al. Longitudinal assessment of three serum biomarkers to detect very early stage hepatocellular carcinoma. Hepatology. 2019;69:1983–1994. doi: 10.1002/hep.30233. [DOI] [PubMed] [Google Scholar]
- 43.Tayob N, Lok AS, Do KA, Feng Z. Improved detection of hepatocellular carcinoma by using a longitudinal alpha-fetoprotein screening algorithm. Clin Gastroenterol Hepatol. 2016;14:469–475. doi: 10.1016/j.cgh.2015.07.049. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lok AS, Sterling RK, Everhart JE, Wright EC, Hoefs JC, Di Bisceglie AM, et al. Des-gamma-carboxy prothrombin and alpha-fetoprotein as biomarkers for the early detection of hepatocellular carcinoma. Gastroenterology. 2010;138:493–502. doi: 10.1053/j.gastro.2009.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Berhane S, Toyoda H, Tada T, Kumada T, Kagebayashi C, Satomura S, et al. Role of the GALAD and BALAD-2 serologic models in diagnosis of hepatocellular carcinoma and prediction of survival in patients. Clin Gastroenterol Hepatol. 2016;14:875–886. doi: 10.1016/j.cgh.2015.12.042. e6. [DOI] [PubMed] [Google Scholar]
- 46.Kisiel JB, Dukek BA, Kanipakam RVSR, Ghoz HM, Yab TC, Berger CK, et al. Hepatocellular carcinoma detection by plasma methylated DNA: discovery, phase I pilot, and phase II clinical validation. Hepatology. 2019;69:1180–1192. doi: 10.1002/hep.30244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yang JD, Roberts LR. Hepatocellular carcinoma: a global view. Nat Rev Gastroenterol Hepatol. 2010;7:448–458. doi: 10.1038/nrgastro.2010.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mehta N, Heimbach J, Harnois DM, Sapisochin G, Dodge JL, Lee D, et al. Validation of a risk estimation of tumor recurrence after transplant (RETREAT) score for hepatocellular carcinoma recurrence after liver transplant. JAMA Oncol. 2017;3:493–500. doi: 10.1001/jamaoncol.2016.5116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yang JD, Larson JJ, Watt KD, Allen AM, Wiesner RH, Gores GJ, et al. Hepatocellular carcinoma is the most common indication for liver transplantation and placement on the waitlist in the United States. Clin Gastroenterol Hepatol. 2017;15:767–775. doi: 10.1016/j.cgh.2016.11.034. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124:91–96. doi: 10.1053/gast.2003.50016. [DOI] [PubMed] [Google Scholar]
- 51.Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, et al. A model to predict survival in patients with endstage liver disease. Hepatology. 2001;33:464–470. doi: 10.1053/jhep.2001.22172. [DOI] [PubMed] [Google Scholar]
- 52.Heimbach JK, Hirose R, Stock PG, Schladt DP, Xiong H, Liu J, et al. Delayed hepatocellular carcinoma model for end-stage liver disease exception score improves disparity in access to liver transplant in the United States. Hepatology. 2015;61:1643–1650. doi: 10.1002/hep.27704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mehta N, Sarkar M, Dodge JL, Fidelman N, Roberts JP, Yao FY. Intention to treat outcome of T1 hepatocellular carcinoma with the “wait and not ablate” approach until meeting T2 criteria for liver transplant listing. Liver Transpl. 2016;22:178–187. doi: 10.1002/lt.24360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tang A, Bashir MR, Corwin MT, Cruite I, Dietrich CF, Do RKG, et al. Evidence supporting LI-RADS major features for CT- and MR imaging-based diagnosis of hepatocellular carcinoma: a systematic review. Radiology. 2018;286:29–48. doi: 10.1148/radiol.2017170554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chernyak V, Fowler KJ, Kamaya A, Kielar AZ, Elsayes KM, Bashir MR, et al. Liver Imaging Reporting and Data System (LI-RADS) version 2018: imaging of hepatocellular carcinoma in at-risk patients. Radiology. 2018;289:816–830. doi: 10.1148/radiol.2018181494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.van der Pol CB, Lim CS, Sirlin CB, McGrath TA, Salameh JP, Bashir MR, et al. Accuracy of the Liver Imaging Reporting and Data System in computed tomography and magnetic resonance image analysis of hepatocellular carcinoma or overall malignancy-a systematic review. Gastroenterology. 2019;156:976–986. doi: 10.1053/j.gastro.2018.11.020. [DOI] [PubMed] [Google Scholar]
- 57.Terzi E, Iavarone M, Pompili M, Veronese L, Cabibbo G, Fraquelli M, et al. Contrast ultrasound LI-RADS LR-5 identifies hepatocellular carcinoma in cirrhosis in a multicenter restropective study of 1,006 nodules. J Hepatol. 2018;68:485–492. doi: 10.1016/j.jhep.2017.11.007. [DOI] [PubMed] [Google Scholar]
- 58.Aubé C, Oberti F, Lonjon J, Pageaux G, Seror O, N’Kontchou G, et al. EASL and AASLD recommendations for the diagnosis of HCC to the test of daily practice. Liver Int. 2017;37:1515–1525. doi: 10.1111/liv.13429. [DOI] [PubMed] [Google Scholar]