Abstract
Multiple Sclerosis (MS) is a chronic disabling neuroinflammatory disease. Psychiatric manifestations have a high prevalence in MS patients and may worsen the illness progression and the patients’ quality of life (QoL). Depression is a highly prevalent condition in MS patients, associated with poorer adherence to treatment, decreased functional status and QoL, and increased suicide risk. Diagnosis and treatment of this disorder is challenging because of symptom overlap. Other prevalent psychiatric comorbidities are anxiety disorders, bipolar disorder, psychotic disorders, substance misuse and personality disorders. As the illness progresses, personality changes can happen, as well as affect abnormalities. Cognitive changes occur frequently in MS patients, and affect features like processing speed, attention, learning, memory, visual spatial capabilities, and some language deficits. Disease-modifying treatments may reduce cognitive impairment because of their container action on the brain’s lesion burden. Other QoL determinants such as fatigue, pain, sexual dysfunction, exercise, resilience and social support should be taken into account, in order to promote the individuals’ well-being. Further studies are needed in order to elucidate the effectiveness of pharmacotherapy and more neuroimaging studies are required to clarify the relationship between structural changes and psychiatric comorbidities.
Keywords: Multiple sclerosis, Psychiatric disorders, Cognition, Quality of life
INTRODUCTION
Multiple Sclerosis (MS) is a chronic, autoimmune inflammatory disease of the Central Nervous System (CNS). It is the most common chronic disabling disease of the CNS in young adults, affecting 2.3 million people worldwide, is two times more common in females than in males and its onset is usually at young ages, namely around 30 years of age [1].
The course of MS is variable and unpredictable. According to the National Multiple Sclerosis Society, there are four types of MS: Clinically isolated syndrome (CIS), Relapsing-remitting MS (RRMS), Primary progressive MS (PPMS) and Secondary progressive MS (SPMS). CIS is a first episode of neurologic symptoms caused by inflammation and demyelination in the CNS, lasting for at least 24 hours, that does not meet the criteria for MS. RRMS is characterized by the occurrence of defined attacks (relapses or exacerbations) of new or increasing neurologic symptoms, followed by periods of partial or complete recovery (remissions). During remission periods, there seems to be no apparent progression of the disease. At the time of diagnosis, around 85% of patients had this type of MS [1]. Eighty per cent of RRMS patients will eventually transition to a secondary progressive course (SPMS) [1], with a gradual and progressive worsening of neurologic function (accumulation of disability) over time. If this progressive course occurs since the onset of the illness, without early relapses or remissions, the patient develops PPMS, which counts for 10% of patients [1].
It’s a disease that affects all the brain, including white and gray matters. The neurological lesions begin in early stages and affect all aspects of CNS functioning [2].
MS symptoms include muscle weakness, visual acuity loss, sphincter incontinence, fatigue, anxiety, depression and cognitive deficits.
Upon receiving the diagnosis, MS patients can report various conflicting emotional reactions, like shock, anxiety, fear, sadness, sorrow or anger [3]. This way, physicians should adopt an empathic, supportive attitude towards the patient. In fact, when physicians recognize and respond empathically to patient concerns, patient-physician communication improves [4].
Being an incurable and destructive disease, with a high risk of disability, MS shows significant neuropsychiatric complications that may threaten the autonomy of the affected individuals, their socioeconomic status, dignity and possible projects for a better life [5].
PSYCHIATRIC DISORDERS
In the nineteenth century, Charcot made the first detailed clinicopathological description of “Disseminated Sclerosis” or “Sclérose en Plaques” in his lectures at the Salpêtrière hospital. Among the observed psychiatric symptoms were pathological laughing and weeping, euphoria, mania, hallucinations and depression. He also stated that those patients might show “marked enfeeblement of the memory, conceptions are formed slowly and intellectual and emotional faculties are blunted in their totality.” [6]
From then, many studies tried to approach the psychiatric comorbity in MS. In the 1920’s, Cottrell and Wilson [7] identified symptoms of depression in 10% of patients of their sample. It was also one of the first studies to address pathological laughing and crying, which had a prevalence of 95% in their sample [7]. In the same decade, Ombredane [8] identified three categories of mental disorder: “sclerotic mental state,” which included mood and cognitive impairment; dementia; and psychosis. He also stated that “the mental symptoms were related less to the existence and distribution of plaques than to a diffuse toxic state.” [8]
Over the years, more authors dedicated themselves to the study of the psychiatric comorbidities in MS, exponentially increasing the literature on this subject.
Depression is one of the most prevalent psychiatric conditions in these patients. Today, lifetime prevalence of major depression in MS patients is estimated to be around approximately 25–50%, a number two to five times greater than in general population [9].
The most common depressive symptoms in MS include irritability, discouragement, memory/concentration problems, fatigue, insomnia and poor appetite. Guilt and poor self-esteem are rarer in these patients [10].
Depression can occur throughout the course of MS, even in mild forms of the disease [11], and has a reported higher risk of depression in the first years after the diagnosis [12]. Disease activity, but not its duration, was associated with depression and anxiety [13].
Studies suggest that there are neurobiological risk factors associated with MS that determine the increased incidence of depressive disorders in these patients, such as higher lesion load in the left arcuate fasciculus [14], as well as in the prefrontal cortex, anterior temporal lobe and parietal lobe [15]. Cortical atrophy in regions located in the bilateral frontal lobes, as well as of the parietal and occipital lobes, was associated with depression in patients with MS [16]. The hippocampus plays a key role in mood regulation. A study found right hippocampal shape variations in depressed female MS patients and that these changes were linked to affect symptoms but not to vegetative symptoms of depression [17]. Another study showed changes in the cortico-striatal-pallido-thalamic loop in depressed MS patients, namely progressive gray matter loss in limbic basal ganglia structures, such as the globus pallidus, and the thalamus, which may lead to depression-typical deficits in hedonic motivation; on the other hand atrophy of the prefrontal cortex may contribute to maladaptive coping strategies, promoting the development of depressive symptoms [18].
Neuroendocrine factors like hypothalamus-pituitary-adrenal (HPA) axis dysfunction may be implicated in disease progression and comorbid mood disorders. Studies found a hyperactivity of the HPA axis in RRMS patients with comorbid depression, with normal morning cortisol but elevated evening levels, even in early stages of the illness [19]. A study found that affective and neuroendocrine disorders were related to inflammatory disease activity but not to degree of disability [20].
Regarding treatment with beta-interferon (INFβ), earlier studies report an increase in depression in patients during the first 2 to 6 months of treatment with INFβ-1a and INFβ-1b, respectively; however, these increases seemed to be more related to pretreatment levels of depression than to the administration of INFβ [21,22]. On the other hand, more recent studies, like the SPECTRIMS and COGIMUS trials, have shown no clear evidence of this drug increasing the risk for depressive disorders [23,24].
Psychosocial factors may be linked to depression in MS. A study found that there was a significant interaction between level of neurologic impairment, coping behaviors and depression in patients with MS [25]. Cognitive reframing (active attempt to acquire new perspectives on a problem) was related to lower levels of depression. On the other hand, strategies like escapeavoidance (e.g., wishing the problem would disappear, using daydreams) and emotional respite (e.g., using fantasy and daydreams) were associated with higher levels of depression [25].
There is an overlap between symptoms of depression and symptoms of MS, such as fatigue, insomnia and cognitive dysfunction [26], which complicates the diagnosis of this condition. In order to avoid symptom overlap, the American Academy of Neurology (AAN) proposed the Beck Depression Inventory (BDI-II) to be psychometric scale of choice for assessing patients with MS and depression [27].
Treatment of depression should be individualized and involve an association between pharmacological and psychotherapeutic measures. In the absence of more studies conducted specifically in MS patients, treatment should follow the same guidelines as for the general population. So, treatment should start with selective serotonin reuptake inhibitors (SSRI) with second-line treatments including serotonin-norepinephrine reuptake inhibitors (SNRI)—Venlafaxine and Duloxetine—Tricyclic Antidepressants and Mirtazapine [28]. Particular attention should be paid to the side effects of the drugs and the treatment should always start with low doses. In addition, cognitive behavioral therapy (CBT) is an effective intervention for the treatment of mild to moderate depression in patients and might also improve the patient’s QoL [29]. When these options have been exhausted and the patient maintains severe depressive symptoms, psychotic symptoms or structured suicidal ideation, electroconvulsive therapy (ECT) should be considered, with anecdotal reports suggesting its benefits [30].
Depression is associated with poor adherence to immunomodulatory treatments [31] and increased number of hospital admissions and relapses [32].
Suicidal ideation in MS patients is 2.3 to 14 times higher than in the general population and estimated rates of suicide vary from 1.8% to 15.1% of all the deaths [33]. The relative suicide risk is higher in the first 5 years after diagnosis, with 50% of all suicides occurring in that interval [28]. The strongest predictors of suicide attempts in patients with MS are depression, social isolation and alcohol abuse [34]. Suicidal ideation can also be associated with illness severity (not the disability status), depression, low QoL, male gender and being unmarried [28]. Early diagnosis and treatment of this comorbidity is essential, not only to improve the patient’s QoL, but also to decrease the suicide risk.
Because taking care of these patients can be an emotionally draining experience, caregivers can experience depressive symptoms and, as such, can have lower QoL. Hence, early recognition of caregiver burden is important in determining appropriate interventions and treatment [35].
Anxiety disorders have been the target of fewer studies. The prevalence of anxiety disorders in people with MS is estimated to be around 13% to 31.7% and anxiety symptoms from 26% to 63.4% [36]. The prevalence of these disorders is three times greater in MS patients than in the general population, with an estimated lifetime prevalence of 36%, versus 25% in the general population [2]. Generalized Anxiety Disorder (18.6%) is the most common anxiety disorder in MS patients, followed by Panic Disorder (10%) and Obsessive Compulsive Disorder (8.6%) [37].
One recent study, using MRI, found an association between atrophy in the superior and middle gyri of the right frontal lobe and anxiety scores in MS patients [38].
Anxiety frequently co-occurs with depression and is associated with increased physical complaints, social dysfunction, alcohol consumption and suicidal ideation, and, like depression, is often considered as precipitant of relapse in MS patients [39].
Because anxiety symptoms can overlap with some somatic manifestations of MS, scales like HADS may help the clinician rule out the differences, reducing the risk of anxiety overdiagnosis [40].
For the treatment of anxiety disorders, no pharmacological or psychological controlled trial was performed on MS patients, with the exception of CBT intervention against injection anxiety [28], a specific condition leading to anxiety in MS patients related to self-injectable immunomodulatory drugs [3]. As so, treatment of anxiety disorders should follow the same guidelines as for the general population, with SSRI and CBT as first line interventions, and SNRI as a pharmacological alternative [28].
BD is also a prevalent psychiatric disorder in MS patients. A recent population-based study estimated the lifetime prevalence of bipolar disorder to be 5.8% in MS patients [41].
Manic and depressive episodes precipitated by steroid therapy are well documented in the literature. Other potential etiologies for this disorder in MS are being the subject of numerous investigations. There is an increasing body of evidence that supports organic changes in the brain as a potential cause for the development of affective disturbances. For example, there is MRI evidence of the existence of plaques in the temporal horn areas, in MS patients and mania episodes [42]. A recent case series with MS patients with BD showed, through cerebral and cerebrospinal MRI, T2-weighted hyperintense lesions in periventricular white matter, corpus callosum, subcortical “white matter”, mainly in frontal and temporal lobes and right cerebellar peduncle [43].
Some BD symptoms are present in MS patients throughout the evolution of the illness. For example, impulsivity is a common manifestation in patients with MS [44] and emotional lability may occur with the MS exacerbations [2].
For the treatment of mania episodes, anecdotal reports suggest treatment with mood stabilizers, antipsychotics and benzodiazepines. In the case of steroid-induced mania, in order to avoid steroid treatment discontinuation, lithium prophylaxis and reduction of steroid doses are recommended [39].
Recent epidemiological studies have documented that the prevalence of psychotic symptoms in MS is two to three times higher than in the general population [45]. Various epidemiological studies determined an estimated prevalence of Psychosis that ranged from 0.41% and 7.46%, and more specifically 0% to 7.4% of Schizophrenia [36].
Psychotic symptoms in MS are associated with a higher lesion load in the medial temporal lobe [46]. Also, a retrospective case series found that in 73% of the MS patients with psychosis MRI scans showed lesions in the periventricular white matter [47].
Schizophrenia and other psychotic disorders were associated with genetic markers of immune activation, which suggested a potential etiological relationship between MS and psychosis [48].
Psychotic symptoms reported in MS patients include hallucinations and delusions (mostly paranoid), irritability/agitation, sleep disturbance, grandiosity, blunted affect, and rare symptoms like catatonia and transient catalepsy [45].
Medications used in the treatment of MS may have a direct effect in the development of psychosis, although the mechanisms are not yet well understood. This effect is common with corticosteroids, but psychotic episodes have also been reported in patients treated with interferon-beta [49].
For the treatment of psychosis, the clinician should consider adjusting MS medication (in the case of medication-induced psychosis) and start treatment with an antipsychotic drug. There is little empirical information to guide the clinicians in the choice of antipsychotic and dosage, however, there is evidence of good results using clozapine, risperidone, ziprasidone, low-dose chlorpromazine or prophylactic use of lithium alongside corticosteroid therapy [45].
The prevalence of Personality Disorders was found to be about 2.6% in people with MS [50].
A study evaluated personality traits of MS patients, using Hogan Empathy Scale and the NEO Personality Inventory, and found that they were more neurotic and less empathic, agreeable and conscientious, in comparison to the general population [51].
Personality changes are correlated with the brain lesions, namely the orbital-frontal-subcortical circuits, which can produce uninhibited and socially inappropriate behavior, and cingular-anterior-subcortical circuits, linked to apathetic and indifferent behavior [52]. A recent study, using the NEO Five-Factor Inventory, found personality changes in MS patients over a period of five years, namely in the Extraversion and Conscientiousness parameters, regardless of the presence or absence of cognitive decline [53].
Treatment, namely medication and behavior modification strategies, is usually palliative [52], helping control the symptoms and behavioural changes.
Substance misuse seems to be more problematic in people with MS, comparatively to the general population, because of the potential to cause more neurological damage to the already compromised CNS and to interact with MS medications [2]. It is also associated with worst psychosocial adjustment, can exacerbate depressive symptoms, complicate the treatment of a pre-existing depression and increase the number of suicide attempts [54].
There is a prevalence of alcohol abuse or dependence ranging between 3.96% and 18.2% among MS patients [36]. Alcohol abuse may potentiate the mild cognitive deficit associated with MS; as MS progresses, it may decrease alcohol tolerance leading to aggravated problems of motor coordination and balance [55].
Drug abuse prevalence is estimated to be 2.5% to 7.4% [36]. Patients seem to try cannabis mostly for symptom control, namely spasticity, pain, tremor and bladder dysfunction, but globally the benefit is not clinically significant [56].
Clinicians should be aware of substance misuse in MS patients, how they may complicate the course of the disease and warn patients to stop consumption. Measures like advice to reduce or stop alcohol use should present as an effective means to reduce abusive alcohol consumption and associated medical consequences.
Individuals with neurological diseases may experience abnormalities in affect. One of these abnormalities is pseudobulbar affect or emotional incontinence, which is an alteration of affect not representing an underlying emotion, such as pathological crying/laughter. It occurs in approximately 10% of MS patients and is very troubling for the patient, family and caregivers [57]. Its etiology is still poorly explained. However, it is considered to be a disconnection syndrome, which results in the loss of brainstem inhibition in a putative control center on crying and laughter [58]. It is also associated with greater cognitive deficits mediated by the frontal lobe [59]. Usually it is more frequent among patients with greater physical incapacity and in more advanced stages of the illness [2]. SSRI [60] and the association between dextromethorphan and quinidine seem to be effective in these situations [61].
Other changes in affect were described by Cottrell and Wilson [7]. They studied a group of one hundred MS patients and found they showed incongruent expressions of affect regarding their marked physical disability: 1) feelings of serenity and cheerfulness-euphoria sclerotica (EpS); 2) feelings of well-being and the belief that they will resume all previous activities-eutonia sclerotica (EtS); 3) or an incongruous and misplaced optimism of eventual full recovery-spes sclerotica (SS). The authors found a prevalence of 63% of EpS, 84% of EtS and 84% of SS in their sample [7]. These defects of affection are associated with significant cognitive decline, heavy lesion load (revealed by brain imaging), marked cerebral atrophy and extensive involvement of the frontal lobe [62]. There is no treatment recommended, as they cause no distress to patients, in spite of the frustration and perplexity of caregivers at the patients’ lack of insight [52].
The main characteristics of psychiatric disorders associated with MS are summarized in Table 1.
Table 1.
Psychiatric disorders in multiple sclerosis
| Psychiatric disorders | Prevalence | Etiological considerations | Clinical features | Treatment |
|---|---|---|---|---|
| Depression | 25-50% | Structural changes: | Most common symptoms: irritability, discouragement, memory and concentration problems, fatigue, insomnia and poor appetite | 1st line: SSRI |
| 2 to 5 times higher than GP | • Higher lesion load in the left arcuate fasciculus, prefrontal cortex, anterior temporal lobe and parietal lobe | 2nd line: SNRI, TCA, Mirtazapine CBT: mild to moderate depression | ||
| • Shape variations of hippo campus; | Symptom overlap: fatigue, insomnia and cognitive dysfunction | ECT: last resort treatment | ||
| • Changes in the cortico-striatal-pallido-thalamic loop | Suicidality: | |||
| Neuroendocrine changes: | • Prevalence: | |||
| • HPA axis dysfunction | - Suicidal ideation: 2.3 to 14 times higher than GP | |||
| MS treatment: | - Suicide rate: 1.8-15.1% | |||
| • INFβ: controversial issue | - Suicide risk: higher in the first 5 years after diagnosis; 50% of all suicides | |||
| Psychosocial factors: | • Predictors: depression, social isolation and alcohol abuse | |||
| • Coping mechanisms: | ||||
| - Cognitive reframing: lower levels of depression | ||||
| - Escape-avoidance and emotional respite: higher levels of depression | ||||
| Anxiety disorders | Anxiety disorders: 13-31.7%; 3 times higher than GP | Structural: atrophy in the superior and middle gyri of the right frontal lobe | Symptom overlap between MS somatic manifestations and anxiety symptoms | 1st line: SSRI and CBT |
| Alternative: SNRI | ||||
| Anxiety symptoms: 26% to 63.4% | MS specific: injection anxiety | Anxiety and depression: | ||
| • Increased physical complaints | ||||
| • Social dysfunction | ||||
| • Alcohol consumption | ||||
| • Suicidal ideation | ||||
| Precipitant of relapse in MS patients | ||||
| Bipolar disorder | 5.8% | Structural: plaques in the temporal horn areas; periventricular white matter, corpus callosum, subcortical “white matter”, frontal and temporal lobes and right cerebellar peduncle | BD symptoms throughout the evolution of the illness: impulsivity; emotional lability may occur during exacerbations | Treatment of mania: mood stabilizers, antipsychotics and benzodiazepines |
| Therapy: steroid therapy | Steroid-induced mania: lithium prophylaxis and reduction of steroid doses | |||
| Psychotic disorders | Psychotic symptoms: 2 to 3 times higher than GP | Structural: medial temporal lobe; lesions in the periventricular white matter | Hallucinations and delusions (mostly paranoid), irritability/agitation, sleep disturbance, grandiosity, blunted affect, and rare symptoms like catatonia and transient catalepsy | Antipsychotics: clozapine, risperidone, ziprasidone, low-dose chlorpromazine |
| Psychosis: 0.41-7.46% | Genetic: genetic markers of immune activation | Prophylactic use of lithium alongside corticosteroid therapy | ||
| Schizophrenia: 0-7.4% | Therapy: corticosteroids; INFβ | |||
| Personality disorders | 2.6% | Structural: orbital-frontal-subcortical circuits; cingular-anterior-subcortical circuits | More neurotic features and less empathic, agreeable and conscientious | Palliative medication and behavior modification strategies |
| Substance misuse | Alcohol: 3.96–18.2% | Alcohol: potentiate mild cognitive deficit; decreased alcohol tolerance; aggravated neurological symptoms | Psychoeducational measures | |
| Drug abuse: 2.5–7.4% | Cannabis use for symptom control | |||
| Affect abnormalities | Pseudobulbar affect: 10% | Disconnection syndrome: loss of brainstem inhibition in a putative control center on crying and laughter | Alteration of affect not representing an underlying emotion, such as pathological crying/laughter | SSRI |
| Dextromethorphan+quinidine |
GP: general population, HPA: hypothalamus-pituitary-adrenal, INFβ: interferon-beta, SSRI: selective serotonine reuptake inhibitors, SNRI: serotonine and norepinephrine reuptake inhibitors, TCA: tricyclic antidepressants, CBT: cognitive behavioral therapy, ECT: eletroconvulsivetherapy
COGNITION
MS has a varied effect on individual’s cognitive functioning. More than 50% of MS patients present some type of cognitive decline during the course of the illness [63]. Cognitive problems can occur since the earliest stages of the disease, with the most vulnerable stage for the occurrence of cognitive impairment being the first five years of illness [64].
Information processing abilities, complex visuospatial tasks, conceptual reasoning, sustained attention, working memory and retrieval functions in short-term and long-term memory are often impaired in MS while primary language functions, immediate and implicit memory and verbal intellectual skills typically remain resistant to deterioration [63].
Men appear to be more vulnerable to the negative cognitive effects of MS. This cognitive impairment in the male gender has been associated with disease duration, disability level and low educational level, as well as the presence of the ε4 allele of the APOE gene; these factors don’t seem to have the same association in females [65].
Slower processing speed, difficulties in attention and concentration, memory and impaired abstract reasoning are considered a sign of subcortical pathology [44]. Lesions in the corpus callosum appear to be important indicatives of poor cognitive performance. A study found that these are two times more frequently in MS patients with cognitive impairment, in comparison with MS patients without cognitive impairment [66]. Microstructural changes in the normal appearing white matter are predictive of the global cognitive state and the evolution of cognitive functionality in a period of seven years [67].
Concerning gray matter, a significant association was found between executive deficits and damage in the prefrontal cortex [68], and also between frontal and parietal lesion burden and deficits in complex attention and verbal working memory [69]. Also, a study concluded that patients with cognitive impairment had lower normalised brain volume and gray matter volume in comparison to patients without cognitive impairment, most prominently in the left putamen, thalamus bilaterally, and the insula bilaterally [70].
Brain atrophy is the strongest correlate for cognitive decline, even at early stages of the illness [71]. One recent study found that patients with MS have lower thalamic volume, when compared with healthy controls, and even lower in patients with MS and cognitive impairment [72].
Depression can also affect cognitive functioning in MS, including aspects like working memory, processing speed, learning and memory functions, abstract reasoning, and executive functioning [73].
Treatments with anti-inflammatory and immunosuppressive immunomodulators appear to be beneficial in the cognitive deficit because of its container action on the brain’s lesion burden [44]. For example, people treated with INF β-1b showed improvements in complex attention, concentration, and visual learning/recall after one year, when compared with untreated controls [74]; treatment with cyclophosphamide combined with methylprednisolone lead to significant improvements in global cognitive efficiency, learning, organizational and planning abilities, and inhibition [75]. Concerning other nonpharmacological treatments like cognitive training or rehabilitation, the evidence for treatment efficacy is not strong, although the results have been promising [76].
Figure 1 summarizes the characteristics of the main cognitive manifestations in MS.
Figure 1.
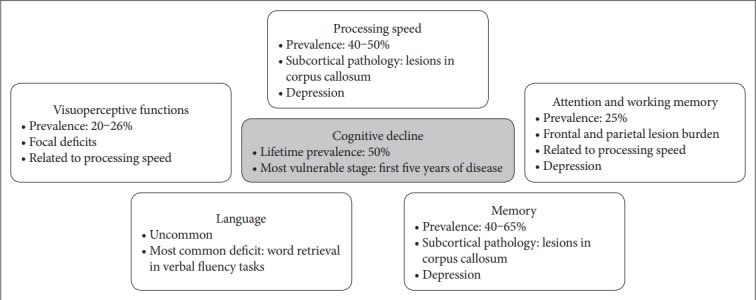
Cognitive decline in Multiple Sclerosis patients.
Processing speed
Processing speed can be defined as the ability to automatically and fluently perform relatively easy or over-learned elementary cognitive tasks, especially when high mental efficiency (that is, attention and focused concentration) is required.
This is the most frequently affected cognitive function in MS patients, with a prevalence of 40% to 50% of all patients [77].
The deficits appear to be secondary to the process of demyelination [78].
Attention and working memory
Attention is a cognitive process that involves passive or active focus of consciousness on an experience, such as sensory inputs, motor acts, memories or internal representations.
In MS, attention is compromised in up to 25% of the patients, especially selective and divided attention [79].
A related problem is that of working memory, a cognitive system linked to attention, with a limited capacity, that is responsible for temporarily holding information available for processing.
Frontal and parietal lesion burden was shown in a study to correlate with performance on tests of complex attention and verbal working memory [69].
Also, difficulties experienced by patients in these areas can be related to processing speed deficits, which in turn are thought to be secondary to the demyelination process [78].
Memory
Memory deficits are seen in 40–65% of MS patients [80]. MSrelated memory impairments’ nature is a controversial topic in the literature, with studies suggesting that memory dysfunctions in MS result primarily from impaired retrieval from longterm memory [81] and others pinpointing difficulties with acquisition of new knowledge [73].
Tasks related to implicit memory seem to be more preserved compared to those of explicit memory. A better use of implicit memory could be an effective compensatory strategy for MS patients in trying to make up for their memory issues [44].
Language
As said before, comprehensive language is typically resistant to deterioration in MS. However, it may be compromised during the progression of the illness, particularly due to slowed processing speed [82].
Other areas of language may be affected in MS patients. The most commonly identified language deficit in these patients is impaired word retrieval in verbal fluency tasks, which may be affected early in the course of MS [63].
More severe deficits, such as aphasia, are relatively uncommon in MS, which has been associated with large demyelinating lesions within the white matter of the left hemisphere [83].
Visuoperceptive functions
Visuoperceptive functions (visuospatial and visuoconstructive) include recognition of visual stimulus and the ability to detect with details the stimulus characteristics.
Impairments in this area seem to result from focal deficits or, like comprehensive language, a result of reduced processing speed [84]. They can be present in around 20% to 26% of MS patients [85].
These deficits can endanger the patients’ lives. So, it is no surprise that road and machinery accidents could happen as consequence of implications on this executive function [44].
OTHER QUALITY OF LIFE DETERMINANTS
Fatigue is defined by the Multiple Sclerosis Council for Clinical Practice Guideline as a subjective state of physical and/or mental lack of energy that is perceived by the individual as interfering with habitual or desired activities and is described many times as a feeling of exhaustion, lassitude and lethargy [86].
Fatigue is the most commonly reported symptom in patients with MS, with a prevalence up to 75% to 85% [39].
Up to 50–60% of patients consider it as the most disabling symptom of the illness, as it can cause adverse effects on the patients’ quality of life, mood, cognitive and social functioning [39].
Fatigue was associated with a disruption of brain networks involved in motor preparation processes, depending on several frontal-thalamic pathways [87]. Alterations were also found in the bilateral pre- and postcentral gyrus, supplementary motor area, caudate nucleus, putamen, thalamus, paracingulate gyrus, precuneus and insula, as well as alterations of basal ganglia functional connectivity, that suggest a disruption of motor and nonmotor basal ganglia functions, including motivation and reward processing, which may contribute to fatigue pathophysiology in multiple sclerosis [88].
Other possible etiologies involve immune phenomena, with endocrine abnormalities like hypothyroidism or HPA axis dysfunction [89]. Fatigue may also arise independently of depression or manifest as a symptom of it, making the relationship between the two a complex one in MS patients [9].
Studies found correlations between fatigue, disability level, depression and sleep quality [90,91] and the MS patients’ QoL. On the other hand, a study found that fatigue was independent from physical disability, but was associated with depression, which might suggest the presence of common mechanisms in fatigue and depression, including psychological factors or brain lesions in specific neuroanatomic pathways [92].
For the treatment of fatigue in MS, individual cognitive behavioral therapy, group psychotherapy and SSRI treatment were associated with reductions in the severity of fatigue symptoms, primarily due to treatment related changes in mood [93]. However, this approach would not be expected to be as effective in patients without depressive symptoms [94]. For the treatment of fatigue in non-depressed MS patients, the most commonly used agents are amantadine (an antiviral agent with dopaminergic properties) and modafinil (an agent developed for the treatment of narcolepsy) [39], with only little to moderate efficacy [39,94].
Sexual dysfunction (SD) was found to be present in about 60.7% of MS patients, with women appearing to have a higher prevalence in SD complains, in comparison to men [95].
On MS patients, it could be secondary to disease progression, deregulation of the hypothalamic-pituitary-gonadal axis, intense fatigue, depression, or side effects of antidepressants [96]. Brain lesions like pontine atrophy and insular lesions were associated with SD and erectile dysfunction, respectively [97,98].
Frustration and anger with their sexual performance, may also have a negative impact in the patients’ QoL and interpersonal relationships [44].
Pain is also a common symptom in MS, affecting approximately two thirds of patients [76].
This symptom may be secondary to trigeminal or glossopharyngeal neuralgia, transverse myelitis, optic neuritis or associated with sensory impairment [44].
Due to the high discomfort it causes, MS patients with pain may report poorer mental health and more social-role handicap.
Resilience is the ability to maintain psychological well-being and the level of functioning in the face of adversity (such as loss, trauma and serious medical illness).
Resilience, avoidance and emotion-focused coping strategies are considered predictors of depression and anxiety symptoms in newly diagnosed MS patients [99].
Posttraumatic growth, that is positive psychologic changes that result from or in response to challenging circumstances, can lead to increased appreciation of life, feelings of increased personal strength, experiencing improved interpersonal relationships, changing life priorities, or finding new meaning and purpose in life [2].
Social support is very important in the mental health and QoL of these patients. In fact, in a study it was found that social support made a significant contribution to the mental health dimension of quality of life (MHD/QoL) beyond all the other variables and that the number of young children in the family, illness duration, cognitive impairment and social support were predictors of MHD/QoL [100].
A summary of the determinants of QoL in MS can be found in Table 2.
Table 2.
Other predictors of quality of life in multiple sclerosis patients
| Fatigue | Prevalence: 75–85% | ||
| Etiology: | |||
| • | Structural: disruption of frontal-thalamic pathways; bilateral pre- and postcentral gyrus, supplementary motor area, caudate nucleus, putamen, thalamus, paracingulate gyrus, precuneus and insula, as well as alterations of basal ganglia functional connectivity | ||
| • | Endocrine: hypothyroidism; HPA axis dysfunction | ||
| • | Depression: independent vs. symptom of it | ||
| Treatment: | |||
| • | Depressed patients: individual CBT, group psychotherapy and SSRI treatment | ||
| • | Non-depressed patients: amantadine or modafinil (little to moderate efficacy) | ||
| Sexual dysfuncion | Prevalence: 60.7%; higher in women | ||
| Etiology: | |||
| • | Structural: pontine atrophy and insular lesions | ||
| • | Endocrine: HPG axis deregulation | ||
| Related factors: disease progression; intense fatigue; depression; side effects of antidepressants; frustration and anger with sexual performance | |||
| Pain | Prevalence: two thirds of patients | ||
| Etiology: trigeminal or glossopharyngeal neuralgia; transverse myelitis; optic neuritis; sensory impairment | |||
| Resilience | Predictors of depression and anxiety symptoms: resilience, avoidance, emotion-focused coping strategies | ||
| Posttraumatic growth → better coping | |||
| Social support | Predictors QoL: social support; number of young children in the family | ||
HPA: hypothalamus-pituitary-adrenal, CBT: cognitive behavioral therapy, SSRI: selective serotonine reuptake inhibitors, HPG: hypothalamus-pituitary-gonadal, QoL: quality of life
CONCLUSIONS
Neuropsychiatric manifestations are an important issue in MS. Psychiatric comorbidities are very prevalent in MS patients and are linked to various negative consequences, like decreases in QoL and functional status, non-adherence to MS treatment, negative influence in the progression of the illness, and increase of suicide risk. Early diagnosis and treatment of these disorders are of vital importance to the patients and health care professionals must be aware of those consequences in order to promote comfort and patients’ biopsychosocial well-being.
Although not all patients develop cognitive impairments, some will be experienced by individuals throughout the course of the illness, contributing to a degradation of their independent daily life functioning. Early treatment may reduce the level of cognitive impairment, helping to delay those deficits and allowing the patient to live more years without or with little deficit.
All QoL determinants should be taken into account in order to prevent psychosocial dysfunction. Aspects usually unexplored in consultation such as sexuality are also important to address, although often the patient does not feel comfortable talking about it. Somatic symptoms, like fatigue, are considered by the patients as the most disabling and alongside pain contribute to lower the patients’ notion of physical and mental wellbeing, to limit their functionality in everyday activities and interfere with interpersonal relations. Social support, exercise and individuals’ resilience can have beneficial effects in the QoL of the patients and be protective for psychiatric disorders.
The diagnosis of MS can be very troubling for the patients and can trigger several non-adaptive reactions. A comprehensive and empathic approach is half way to a better acceptance of the diagnosis by the patient and, therefore, improvements in the clinical status and QoL.
Further investigation is required in order to clarify the intricate relationship between MS and psychiatric disorders, especially the interaction between depression and somatic symptoms, influence of factors such as the location of lesions, involvement of neuroendocrine factors and possible psychiatric side effects of disease modifying treatments. Larger randomized, controlled trials will be needed to clarify even more the effectiveness of pharmacological therapy and psychotherapy in these patients. The prevalence and impact of psychiatric disorders and cognitive impairments remain understudied and existing study designs are highly heterogeneous. This issue is of major importance because these disorders are often undetected and inadequately treated and may have a major impact on the individuals’ sense of well-being and can contribute to poor adjustment and psychosocial dysfunction.
Footnotes
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Celeste Silveira, Renato Guedes. Data curation: Celeste Silveira, Renato Guedes. Formal analysis: Rosário Curral, Rui Coelho. Funding acquisition: Celeste Silveira, Renato Guedes. Investigation: Celeste Silveira, Renato Guedes. Methodology: Celeste Silveira, Renato Guedes. Project administration: Celeste Silveira, Renato Guedes. Resources: Celeste Silveira, Renato Guedes. Software: Diana Maia. Supervision: Rosário Curral, Rui Coelho. Validation: Rosário Curral, Rui Coelho. Visualization: Diana Maia. Writing—original draft: Celeste Silveira, Renato Guedes. Writing— review & editing: Celeste Silveira, Renato Guedes, Diana Maia, Rosário Curral, Rui Coelho.
REFERENCES
- 1.Browne P, Chandraratna D, Angood C, Tremlett H, Baker C, Taylor BV, et al. Atlas of Multiple Sclerosis 2013: a growing global problem with widespread inequity. Neurology. 2014;83:1022–1024. doi: 10.1212/WNL.0000000000000768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chwastiak LA, Ehde DM. Psychiatric issues in multiple sclerosis. Psychiatry Clin N Am. 2007;30:803–817. doi: 10.1016/j.psc.2007.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.José Sá M. Psychological aspects of multiple sclerosis. Clin Neurol Neurosurg. 2008;110:868–877. doi: 10.1016/j.clineuro.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Adams K, Cimino JE, Arnold RM, Anderson WG. Why should I talk about emotion? Communication patterns associated with physician discussion of patient expressions of negative emotion in hospital admission encounters. Patient Educ Couns. 2012;89:44–50. doi: 10.1016/j.pec.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boeije HR, Duijnstee MS, Grypdonck MH, Pool A. Encountering the downward phase: biographical work in people with multiple sclerosis living at home. Soc Sci Med. 2002;55:881–893. doi: 10.1016/s0277-9536(01)00238-6. [DOI] [PubMed] [Google Scholar]
- 6.Butler MA, Bennett TL. In search of a conceptualization of multiple sclerosis: a historical perspective. Neuropsychol Rev. 2003;13:93–112. doi: 10.1023/a:1023884322540. [DOI] [PubMed] [Google Scholar]
- 7.Cottrell SS, Wilson SAK. Original Papers: the affective symptomatology of disseminated sclerosis: a study of 100 cases. J Neurol Psychopathol. 1926;7:1–30. doi: 10.1136/jnnp.s1-7.25.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ombredane A. Les Troubles Mentaux de la Sclérose en Plaques. Paris: Presses Universitaires de France; 1929. [Google Scholar]
- 9.Feinstein A, Magalhães S, Richard JF, Audet B, Moore C. The link between multiple sclerosis and depression. Nat Rev Neurol. 2014;10:507–517. doi: 10.1038/nrneurol.2014.139. [DOI] [PubMed] [Google Scholar]
- 10.Minden SL, Orav J, Reich P. Depression in multiple sclerosis. Gen Hosp Psychiatry. 1987;9:426–434. doi: 10.1016/0163-8343(87)90052-1. [DOI] [PubMed] [Google Scholar]
- 11.Sullivan MFI, Weinshenker B, Mikai S, Edgley K. Depression before and after diagnosis of multiple sclerosis. Mult Scler. 1995;1:104–108. doi: 10.1177/135245859500100208. [DOI] [PubMed] [Google Scholar]
- 12.Possa MF, Minacapelli E, Canale S, Comi G, Martinelli V, Falautano M. The first year after diagnosis: psychological impact on people with multiple sclerosis. Psychol Health Med. 2017;22:1063–1071. doi: 10.1080/13548506.2016.1274043. [DOI] [PubMed] [Google Scholar]
- 13.Noy S, Achiron A, Gabbay U, Barak Y, Rotstein Z, Laor N, SarovaPinhas I. A new approach to affective symptoms in relapsing-remitting multiple sclerosis. Compr Psychiatry. 1995;36:390–395. doi: 10.1016/s0010-440x(95)90121-3. [DOI] [PubMed] [Google Scholar]
- 14.Pujol J, Bello J, Deus J, Martí-Vilalta JL, Capdevila A. Lesions in the left arcuate fasciculus region and depressive symptoms in multiple sclerosis. Neurology. 1997;49:1105–1110. doi: 10.1212/wnl.49.4.1105. [DOI] [PubMed] [Google Scholar]
- 15.Bakshi R, Czarnecki D, Shaikh ZA, Priore RL, Janardhan V, Kaliszky Z, et al. Brain MRI lesions and atrophy are related to depression in multiple sclerosis. Neuroreport. 2000;11:1153–1158. doi: 10.1097/00001756-200004270-00003. [DOI] [PubMed] [Google Scholar]
- 16.Gobbi C, Rocca MA, Riccitelli G, Pagani E, Messina R, Preziosa P, et al. Influence of the topography of brain damage on depression and fatigue in patients with multiple sclerosis. Mult Scler. 2014;20:192–201. doi: 10.1177/1352458513493684. [DOI] [PubMed] [Google Scholar]
- 17.Gold SM, O’Connor MF, Gill R, Kern KC, Shi Y, Henry RG, et al. Detection of altered hippocampal morphology in multiple sclerosis-associated depression using automated surface mesh modeling. Hum Brain Mapp. 2014;35:30–37. doi: 10.1002/hbm.22154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stuke H, Hanken K, Hirsch J, Klein J, Wittig F, Kastrup A, et al. Cross-sectional and longitudinal relationships between depressive symptoms and brain atrophy in MS patients. Front Hum Neurosci. 2016;10:622. doi: 10.3389/fnhum.2016.00622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kern S, Schultheiss T, Schneider H, Schrempf W, Reichmann H, Ziemssen T. Circadian cortisol, depressive symptoms and neurological impairment in early multiple sclerosis. Psychoneuroendocrinology. 2011;36:1505–1512. doi: 10.1016/j.psyneuen.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 20.Fassbender K, Schmidt R, Mössner R, Kischka U, Kühnen J, Schwartz A, et al. Mood disorders and dysfunction of the hypothalamic-pituitary-adrenal axis in multiple sclerosis. Arch Neurol. 1998;55:66–72. doi: 10.1001/archneur.55.1.66. [DOI] [PubMed] [Google Scholar]
- 21.Mohr DC, Goodkin DE, Likosky W, Gatto N, Baumann KA, Rudick RA. Treatment of depression improves adherence to interferon beta1b therapy for multiple sclerosis. Arch Neurol. 1997;54:531–533. doi: 10.1001/archneur.1997.00550170015009. [DOI] [PubMed] [Google Scholar]
- 22.Mohr DC, Likosky W, Dwyer P, Van Der Wende J, Boudewyn AC, Goodkin DE. Course of depression during the initiation of interferon beta-1a treatment for multiple sclerosis. Arch Neurol. 1999;56:1263–1265. doi: 10.1001/archneur.56.10.1263. [DOI] [PubMed] [Google Scholar]
- 23.Patten SB, Metz LM. Interferon beta1a and depression in secondary progressive MS: data from the SPECTRIMS Trial. Neurology. 2002;59:744–746. doi: 10.1212/wnl.59.5.744. [DOI] [PubMed] [Google Scholar]
- 24.Patti F, Amato MP, Trojano M, Bastianello S, Tola MR, Picconi O, et al. Quality of life, depression and fatigue in mildly disabled patients with relapsing-remitting multiple sclerosis receiving subcutaneous interferon beta-1a: 3-year results from the COGIMUS (COGnitive Impairment in MUltiple Sclerosis) study. Mult Scler. 2011;17:991–1001. doi: 10.1177/1352458511401943. [DOI] [PubMed] [Google Scholar]
- 25.Mohr DC, Goodkin DE, Gatto N, Van Der Wende J. Depression, coping and level of neurological impairment in multiple sclerosis. Mult Scler. 1997;3:254–258. doi: 10.1177/135245859700300408. [DOI] [PubMed] [Google Scholar]
- 26.Randolph JJ, Arnett PA, Higginson CI, Voss WD. Neurovegetative symptoms in multiple sclerosis: relationship to depressed mood, fatigue, and physical disability. Arch Clin Neuropsychol. 2000;15:387–398. [PubMed] [Google Scholar]
- 27.Minden SL, Feinstein A, Kalb RC, Miller D, Mohr DC, Patten SB, et al. Evidence-based guideline: assessment and management of psychiatric disorders in individuals with MS: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2014;82:174–181. doi: 10.1212/WNL.0000000000000013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brenner P, Piehl F. Fatigue and depression in multiple sclerosis: pharmacological and non-pharmacological interventions. Acta Neurol Scand. 2016;134:47–54. doi: 10.1111/ane.12648. [DOI] [PubMed] [Google Scholar]
- 29.Hind D, Cotter J, Thake A, Bradburn M, Cooper C, Isaac C, et al. Cognitive behavioural therapy for the treatment of depression in people with multiple sclerosis: a systematic review and meta-analysis. BMC Psychiatry. 2014;14:5. doi: 10.1186/1471-244X-14-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rasmussen KG, Keegan BM. Electroconvulsive therapy in patients with multiple sclerosis. J ECT. 2007;23:179–180. doi: 10.1097/YCT.0b013e31806548c6. [DOI] [PubMed] [Google Scholar]
- 31.Tarrants M, Oleen-Burkey M, Castelli-Haley J, Lage MJ. The impact of comorbid depression on adherence to therapy for multiple sclerosis. Mult Scler Int. 2011;2011:1–10. doi: 10.1155/2011/271321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mullins LL, Cote MP, Fuemmeler BF, Jean VM, Beatty WW, Paul RH. Illness intrusiveness, uncertainty, and distress in individuals with multiple sclerosis. Rehabil Psychol. 2001;46:139–153. [Google Scholar]
- 33.Pompili M, Forte A, Palermo M, Stefani H, Lamis DA, Serafini G, et al. Suicide risk in multiple sclerosis: a systematic review of current literature. J Psychosom Res. 2012;73:411–417. doi: 10.1016/j.jpsychores.2012.09.011. [DOI] [PubMed] [Google Scholar]
- 34.Feinstein A. An examination of suicidal intent in patients with multiple sclerosis. Neurology. 2002;59:674–678. doi: 10.1212/wnl.59.5.674. [DOI] [PubMed] [Google Scholar]
- 35.Buhse M. Assessment of caregiver burden in families of persons with multiple sclerosis. J Neurosci Nurs. 2008;40:25–31. doi: 10.1097/01376517-200802000-00005. [DOI] [PubMed] [Google Scholar]
- 36.Marrie RA, Reingold S, Cohen J, Stuve O, Trojano M, Sorensen PS, et al. The incidence and prevalence of psychiatric disorders in multiple sclerosis: a systematic review. Mult Scler. 2015;21:305–317. doi: 10.1177/1352458514564487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Korostil M, Feinstein A. Anxiety disorders and their clinical correlates in multiple sclerosis patients. Mult Scler. 2007;13:67–72. doi: 10.1177/1352458506071161. [DOI] [PubMed] [Google Scholar]
- 38.Lin A, Chen F, Liu F, Li Z, Liu Y, Lin S, et al. Regional gray matter atrophy and neuropsychologcal problems in relapsing-remitting multiple sclerosis. Neural Regen Res. 2013;8:1958–1965. doi: 10.3969/j.issn.1673-5374.2013.21.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Paparrigopoulos T, Ferentinos P, Kouzoupis A, Koutsis G, Papadimitriou GN. The neuropsychiatry of multiple sclerosis: focus on disorders of mood, affect and behaviour. Int Rev Psychiatry. 2010;22:14–21. doi: 10.3109/09540261003589323. [DOI] [PubMed] [Google Scholar]
- 40.Honarmand K, Feinstein A. Validation of the Hospital Anxiety and Depression Scale for use with multiple sclerosis patients. Mult Scler. 2009;15:1518–1524. doi: 10.1177/1352458509347150. [DOI] [PubMed] [Google Scholar]
- 41.Marrie RA, Fisk JD, Yu BN, Leung S, Elliott L, Caetano P, et al. Mental comorbidity and multiple sclerosis: validating administrative data to support population-based surveillance. BMC Neurol. 2013;13:16. doi: 10.1186/1471-2377-13-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Feinstein A, Du Boulay G, Ron MA. Psychotic illness in multiple sclerosis. A clinical and magnetic resonance imaging study. Brit J Psychiatry. 1992;161:680–685. doi: 10.1192/bjp.161.5.680. [DOI] [PubMed] [Google Scholar]
- 43.Sidhom Y, Ben Djebara M, Hizem Y, Abdelkefi I, Kacem I, Gargouri A, et al. Bipolar disorder and multiple sclerosis: a case series. Behav Neurol. 2014;2014:1–4. doi: 10.1155/2014/536503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pinkston JB, Kablinger A, Alekseeva N. Multiple sclerosis and behavior. Int Rev Neurobiol. 2007;79:323–339. doi: 10.1016/S0074-7742(07)79014-1. [DOI] [PubMed] [Google Scholar]
- 45.Kosmidis MH, Giannakou M, Messinis L, Papathanasopoulos P. Psychotic features associated with multiple sclerosis. Int Rev Psychiatry. 2010;22:55–66. doi: 10.3109/09540261003589612. [DOI] [PubMed] [Google Scholar]
- 46.Fricchione GL, Carbone L, Bennett WI. Psychotic disorders caused by a general medical condition, with delusions. Secondary ‘organic’ delusional syndromes. Psychiatr Clin North Am. 1995;18:363–378. [PubMed] [Google Scholar]
- 47.Gilberthorpe TG, O’Connell KE, Carolan A, Silber E, Brex PA, Sibtain NA, et al. The spectrum of psychosis in multiple sclerosis: a clinical case series. Neuropsychiatr Dis Treat. 2017;13:303–318. doi: 10.2147/NDT.S116772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sperner-Unterweger B, Fuchs D. Schizophrenia and psychoneuroimmunology. Curr Opin Psychiatry. 2015;28:201–206. doi: 10.1097/YCO.0000000000000153. [DOI] [PubMed] [Google Scholar]
- 49.Goeb JL, Cailleau A, Laine P, Etcharry-Bouyx F, Maugin D, Duverger P, et al. Acute delirium, delusion and depression during INF-beta-1a therapy for multiple sclerosis: a case report. Clin Neuropharmacol. 2003;26:5–7. doi: 10.1097/00002826-200301000-00002. [DOI] [PubMed] [Google Scholar]
- 50.Harel Y, Barak Y, Achiron A. Dysregulation of affect in multiple sclerosis: new phenomenological approach. Psychiatry Clin Neurosci. 2007;61:94–98. doi: 10.1111/j.1440-1819.2007.01616.x. [DOI] [PubMed] [Google Scholar]
- 51.Benedict RH, Priore RL, Miller C, Munschauer F, Jacobs L. Personality disorder in multiple sclerosis correlates with cognitive impairment. J Neuropsychiatry Clin Neurosci. 2001;13:70–76. doi: 10.1176/jnp.13.1.70. [DOI] [PubMed] [Google Scholar]
- 52.Feinstein A. Neuropsychiatric syndromes associated with multiple sclerosis. J Neurol. 2007;254(Suppl 2):ii73–ii76. doi: 10.1007/s00415-007-2017-2. [DOI] [PubMed] [Google Scholar]
- 53.Roy S, Drake A, Fuchs T, Dwyer MG, Zivadinov R, Chapman BP, et al. Longitudinal personality change associated with cognitive decline in multiple sclerosis. Mult Scler. 2018 doi: 10.1177/1352458517753720. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 54.Sullivan LE, Fiellin DA, O’Connor PG. The prevalence and impact of alcohol problems in major depression: a systematic review. Am J Med. 2005;118:330–341. doi: 10.1016/j.amjmed.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 55.Lechtenberg R. Multiple Sclerosis Fact Book. 2nd Edition. Philadelphia: FA Davis; 1995. [Google Scholar]
- 56.Chong MS, Wolff K, Wise K, Tanton C, Winstock A, Silber E. Cannabis use in patients with multiple sclerosis. Mult Scler. 2006;12:646–651. doi: 10.1177/1352458506070947. [DOI] [PubMed] [Google Scholar]
- 57.Feinstein A, Feinstein K, Gray T, O’Connor P. Prevalence and neurobehavioral correlates of pathological laughing and crying in multiple sclerosis. Arch Neurol. 1997;54:1116–1121. doi: 10.1001/archneur.1997.00550210050012. [DOI] [PubMed] [Google Scholar]
- 58.Minden SL, Schiffer RB. Affective disorders in multiple sclerosis. Arch Neurol. 1990;47:98–104. doi: 10.1001/archneur.1990.00530010124031. [DOI] [PubMed] [Google Scholar]
- 59.Hübers A, Kassubek J, Grön G, Gorges M, Aho-Oezhan H, Keller J, et al. Pathological laughing and crying in amyotrophic lateral sclerosis is related to frontal cortex function. J Neurol. 2016;263:1788–1795. doi: 10.1007/s00415-016-8201-5. [DOI] [PubMed] [Google Scholar]
- 60.Seliger GM, Hornstein A. Serotonin, fluoxetine, and pseudobulbar affect. Neurology. 1989;39:1400–1400. doi: 10.1212/wnl.39.10.1400. [DOI] [PubMed] [Google Scholar]
- 61.Panitch HS, Thisted RA, Smith RA, Wynn DR, Wymer JP, Achiron A, et al. Randomized controlled trial of dextromethorphan/quinidine for pseudobulbar affect in multiple sclerosis. Ann Neurol. 2006;59:780–787. doi: 10.1002/ana.20828. [DOI] [PubMed] [Google Scholar]
- 62.Rabins PV. Euphoria in Multiple Sclerosis. In: Rao SM, editor. Neurobehavioural Aspects of Multiple Sclerosis. New York: Oxford University Press; 1990. pp. 180–185. [Google Scholar]
- 63.Calabrese P. Neuropsychology of multiple sclerosis-- an overview. J Neurol. 2006;253(Suppl 1):i10–i15. doi: 10.1007/s00415-006-1103-1. [DOI] [PubMed] [Google Scholar]
- 64.Reuter F, Zaaraoui W, Crespy L, Faivre A, Rico A, Malikova I, et al. Frequency of cognitive impairment dramatically increases during the first 5 years of multiple sclerosis. J Neurol Neurosurg Psychiatry. 2010;82:1157–1159. doi: 10.1136/jnnp.2010.213744. [DOI] [PubMed] [Google Scholar]
- 65.Savettieri G, Messina D, Andreoli V, Bonavita S, Caltagirone C, Cittadella R, et al. Gender-related effect of clinical and genetic variables on the cognitive impairment in multiple sclerosis. J Neurol. 2004;251:1208–1214. doi: 10.1007/s00415-004-0508-y. [DOI] [PubMed] [Google Scholar]
- 66.Rossi F, Giorgio A, Battaglini M, Stromillo ML, Portaccio E, Goretti B, et al. Relevance of brain lesion location to cognition in relapsing multiple sclerosis. PLoS One. 2012;7:e44826. doi: 10.1371/journal.pone.0044826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pinter D, Khalil M, Pichler A, Langkammer C, Ropele S, Marschik PB, et al. Predictive value of different conventional and non-conventional MRI-parameters for specific domains of cognitive function in multiple sclerosis. Neuroimage Clin. 2015;7:715–720. doi: 10.1016/j.nicl.2015.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Foong J, Rozewicz L, Quaghebeur G, Davie CA, Kartsounis LD, Thompson AJ, et al. Executive function in in multiple sclerosis. The role of frontal lobe pathology. Brain. 1997;120(Pt1):15–26. doi: 10.1093/brain/120.1.15. [DOI] [PubMed] [Google Scholar]
- 69.Sperling RA, Guttmann CR, Hohol MJ, Warfield SK, Jakab M, Parente M, et al. Regional magnetic resonance imaging lesion burden and cognitive function in multiple sclerosis: a longitudinal study. Arch Neurol. 2001;58:115–121. doi: 10.1001/archneur.58.1.115. [DOI] [PubMed] [Google Scholar]
- 70.Hulst HE, Steenwijk MD, Versteeg A, Pouwels PJ, Vrenken H, Uitdehaag BM, et al. Cognitive impairment in MS: impact of white matter integrity, gray matter volume, and lesions. Neurology. 2013;80:1025–1032. doi: 10.1212/WNL.0b013e31828726cc. [DOI] [PubMed] [Google Scholar]
- 71.Calabrese M, Agosta F, Rinaldi F, Mattisi I, Grossi P, Favaretto A, et al. Cortical lesions and atrophy associated with cognitive impairment in relapsing-remitting multiple sclerosis. Arch Neurol. 2009;66:1144–1150. doi: 10.1001/archneurol.2009.174. [DOI] [PubMed] [Google Scholar]
- 72.Schoonheim MM, Hulst HE, Brandt RB, Strik M, Wink AM, Uitdehaag BM, et al. Thalamus structure and function determine severity of cognitive impairment in multiple sclerosis. Neurology. 2015;84:776–783. doi: 10.1212/WNL.0000000000001285. [DOI] [PubMed] [Google Scholar]
- 73.Chiaravalloti ND, DeLuca J. Cognitive impairment in multiple sclerosis. Lancet Neurol. 2008;7:1139–1151. doi: 10.1016/S1474-4422(08)70259-X. [DOI] [PubMed] [Google Scholar]
- 74.Barak Y, Achiron A. Effect of interferon-beta-1b on cognitive functions in multiple sclerosis. Eur Neurol. 2002;47:11–14. doi: 10.1159/000047940. [DOI] [PubMed] [Google Scholar]
- 75.Zéphir H, De Seze J, Dujardin K, Dubois G, Cabaret M, Bouillaguet S, et al. One-year cyclophosphamide treatment combined with methylprednisolone improves cognitive dysfunction in progressive forms of multiple sclerosis. Mult Scler. 2005;11:360–363. doi: 10.1191/1352458505ms1172sr. [DOI] [PubMed] [Google Scholar]
- 76.Penner IK. Evaluation of cognition and fatigue in multiple sclerosis: daily practice and future directions. Acta Neurol Scand. 2016;134(Suppl 200):19–23. doi: 10.1111/ane.12651. [DOI] [PubMed] [Google Scholar]
- 77.Patti F, Nicoletti A, Messina S, Bruno E, Fermo SL, Quattrocchi G, et al. Prevalence and incidence of cognitive impairment in multiple sclerosis: a population-based survey in Catania, Sicily. J Neurol. 2015;262:923–930. doi: 10.1007/s00415-015-7661-3. [DOI] [PubMed] [Google Scholar]
- 78.Lengenfelder J, Bryant D, Diamond BJ, Kalmar JH, Moore NB, DeLuca J. Processing speed interacts with working memory efficiency in multiple sclerosis. Arch Clin Neuropsychol. 2006;21:229–238. doi: 10.1016/j.acn.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 79.Nebel K, Wiese H, Seyfarth J, Gizewski ER, Stude P, Diener HC, et al. Activity of attention related structures in multiple sclerosis. Brain Res. 2007;1151:150–160. doi: 10.1016/j.brainres.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 80.Rao SM, Grafman J, DiGuilio D, Mittenberg W, Bernardin L, Leo GJ, et al. Memory dysfunction in multiple sclerosis: its relation to working memory, semantic encoding and implicit learning. Neuropsychology. 1993;7:364–374. [Google Scholar]
- 81.Thornton AE, Raz N, Tucke KA. Memory in multiple sclerosis: contextual encoding deficits. J Int Neuropsychol Soc. 2002;8:395–409. doi: 10.1017/s1355617702813200. [DOI] [PubMed] [Google Scholar]
- 82.Grossman M, Robinson KM, Onishi K, Thompson H, Cohen J, D’Esposito M. Sentence comprehension in multiple sclerosis. Acta Neurol Scand. 1995;92:324–331. doi: 10.1111/j.1600-0404.1995.tb00137.x. [DOI] [PubMed] [Google Scholar]
- 83.Rao SM. Neuropsychology of multiple sclerosis. Curr Opin Neurol. 1995;8:216–220. doi: 10.1097/00019052-199506000-00010. [DOI] [PubMed] [Google Scholar]
- 84.Vleugels L, Lafosse C, Van Nunen A, Charlier M, Ketelaer P, Vandenbussche E. Visuoperceptual impairment in MS patients: nature and possible neural origins. Mult Scler. 2001;7:389–401. doi: 10.1177/135245850100700608. [DOI] [PubMed] [Google Scholar]
- 85.Rao SM. Neuropsychological Aspects of Multiple Sclerosis. In: Raine CS, editor. Multiple Sclerosis: Clinical and Pathogenic Basis. London: Chapman and Hall; 1997. pp. 365–372. [Google Scholar]
- 86.Guidelines MSCP. Fatigue and Multiple Sclerosis: Evidence-Based Management Strategies for Fatigue in Multiple Sclerosis. Washington D.C: Paralyzed Veterans of America; 1998. [Google Scholar]
- 87.Russo M, Calamuneri A, Cacciola A, Bonanno L, Naro A, Dattola V, et al. Neural correlates of fatigue in multiple sclerosis: a combined neurophysiological and neuroimaging approach (R1) Arch Ital Biol. 2017;155:142–151. doi: 10.12871/00039829201735. [DOI] [PubMed] [Google Scholar]
- 88.Finke C, Schlichting J, Papazoglou S, Scheel M, Freing A, Soemmer C, et al. Altered basal ganglia functional connectivity in multiple sclerosis patients with fatigue. Mult Scler. 2015;21:925–934. doi: 10.1177/1352458514555784. [DOI] [PubMed] [Google Scholar]
- 89.Krupp LB, Christodoulou C. Fatigue in multiple sclerosis. Curr Neurol Neurosci Rep. 2001;1:294–298. doi: 10.1007/s11910-001-0033-7. [DOI] [PubMed] [Google Scholar]
- 90.Karatepe AG, Kaya T, Günaydn R, Demirhan A, Ce P, Gedizlioğlu M. Quality of life in patients with multiple sclerosis: the impact of depression, fatigue, and disability. Int J Rehabil Res. 2011;34:290–298. doi: 10.1097/MRR.0b013e32834ad479. [DOI] [PubMed] [Google Scholar]
- 91.Lobentanz IS, Asenbaum S, Vass K, Sauter C, Klösch G, Kollegger H, et al. Factors influencing quality of life in multiple sclerosis patients: disability, depressive mood, fatigue and sleep quality. Acta Neurol Scand. 2004;110:6–13. doi: 10.1111/j.1600-0404.2004.00257.x. [DOI] [PubMed] [Google Scholar]
- 92.Bakshi R, Shaikh ZA, Miletich RS, Czarnecki D, Dmochowski J, Henschel K, et al. Fatigue in multiple sclerosis and its relationship to depression and neurologic disability. Mult Scler. 2000;6:181–185. doi: 10.1177/135245850000600308. [DOI] [PubMed] [Google Scholar]
- 93.Mohr DC, Hart SL, Goldberg A. Effects of treatment for depression on fatigue in multiple sclerosis. Psychosom Med. 2003;65:542–547. doi: 10.1097/01.psy.0000074757.11682.96. [DOI] [PubMed] [Google Scholar]
- 94.Siegert RJ, Abernethy DA. Depression in multiple sclerosis: a review. J Neurol Neurosurg Psychiatry. 2005;76:469–475. doi: 10.1136/jnnp.2004.054635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Çelik DB, Poyraz EÇ, Bingöl A, Idiman E, Ozakbaş S, Kaya D. Sexual dysfunction ın multiple sclerosis: gender differences. J Neurol Sci. 2013;324:17–20. doi: 10.1016/j.jns.2012.08.019. [DOI] [PubMed] [Google Scholar]
- 96.Guo ZN, He SY, Zhang HL, Wu J, Yang Y. Multiple sclerosis and sexual dysfunction. Asian J Androl. 2012;14:530–535. doi: 10.1038/aja.2011.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zorzon M, Zivadinov R, Locatelli L, Stival B, Nasuelli D, Bratina A, et al. Correlation of sexual dysfunction and brain magnetic resonance imaging in multiple sclerosis. Mult Scler. 2003;9:108–110. doi: 10.1191/1352458503ms881sr. [DOI] [PubMed] [Google Scholar]
- 98.Winder K, Linker RA, Seifert F, Deutsch M, Engelhorn T, Dörfler A, et al. Insular multiple sclerosis lesions are associated with erectile dysfunction. J Neurol. 2018;265:783–792. doi: 10.1007/s00415-018-8763-5. [DOI] [PubMed] [Google Scholar]
- 99.Tan-Kristanto S, Kiropoulos LA. Resilience, self-efficacy, coping styles and depressive and anxiety symptoms in those newly diagnosed with multiple sclerosis. Psychol Health Med. 2015;20:635–645. doi: 10.1080/13548506.2014.999810. [DOI] [PubMed] [Google Scholar]
- 100.Schwartz C, Frohner R. Contribution of demographic, medical, and social support variables in predicting the mental health dimension of quality of life among people with multiple sclerosis. Health Soc Work. 2005;30:203–212. doi: 10.1093/hsw/30.3.203. [DOI] [PubMed] [Google Scholar]


