Abstract
OBJECTIVE
To analyze data for death of veterinary professionals and veterinary students, with manner of death characterized as suicide or undetermined intent from 2003 through 2014.
SAMPLE
Death records for 202 veterinary professionals and veterinary students.
PROCEDURES
Decedents employed as veterinarians, veterinary technicians or technologists, or veterinary assistants or laboratory animal caretakers and veterinary students who died by suicide or of undetermined intent were identified through retrospective review of National Violent Death Reporting System records. Standardized mortality ratios (SMRs) and 95% confidence intervals were calculated, and mechanisms and circumstances of death were compared among veterinary occupational groups.
RESULTS
197 veterinary professionals and 5 veterinary students had deaths by suicide or of undetermined intent. Among decedents employed at the time of death, SMRs for suicide of male and female veterinarians (1.6 and 2.4, respectively) and male and female veterinary technicians or technologists (5.0 and 2.3, respectively) were significantly greater than those for the general US population, whereas SMRs for suicide of male and female veterinary assistants or laboratory animal caretakers were not. Poisoning was the most common mechanism of death among veterinarians; the drug most commonly used was pentobarbital. For most (13/18) veterinarians who died of pentobarbital poisoning, the death-related injury occurred at home. When decedents with pentobarbital poisoning were excluded from analyses, SMRs for suicide of male and female veterinarians, but not veterinary technicians or technologists, did not differ significantly from results for the general population.
CONCLUSIONS AND CLINICAL RELEVANCE
Results suggested higher SMRs for suicide among veterinarians might be attributable to pentobarbital access. Improving administrative controls for pentobarbital might be a promising suicide prevention strategy among veterinarians; however, different strategies are likely needed for veterinary technicians or technologists.
Veterinarians have a high suicide risk, compared with that for the general population, both in the United States and abroad.1–8 However, to the authors’ knowledge, there have only been 3 studies of suicides among US veterinarians,2,5,8 and 2 of these were conducted prior to 1996. This is problematic, especially given the transition in veterinary medical education enrollment since 1970 from being nearly 90% male to > 80% female9 and the well-established sex differences in suicidal behavior (eg, men are more likely to die by suicide, whereas women are more likely to attempt suicide).10 Furthermore, the amount of detail available regarding circumstances of death is limited in the available US studies, as they relied solely on review of death certificates, which do not provide comprehensive information regarding the circumstances of death, such as recent mental health treatment, job problems, and relationship problems. Another limitation for most studies of this subject to date is that they relied on PMRs to quantify the degree of suicide risk. Because PMRs represent the proportion of deaths attributable to a particular cause, they can be misleadingly high if other causes of death are lower in a particular population.1,7
Not only has past research shown that veterinarians have higher PMRs from suicide, but a recent survey of 11,627 US veterinarians also showed that veterinarians were more likely to experience current serious psychological distress, have a history of depression, and have experienced suicidal ideation, compared with the general US population.11 Surprisingly, veterinarians did not have a higher likelihood of past suicide attempts than the US population of adults.11 These findings could suggest that although veterinarians are more likely than other US adults to consider suicide, they are not particularly likely to act on these thoughts. Another more concerning possibility is that, given their access to and knowledge about lethal means, veterinarians who are suicidal might be more likely to have a fatal outcome for a suicide attempt. Indeed, results of a retrospective, nationwide study12 in Australia that included data from > 10 years revealed that persons whose occupations were characterized by greater access to and familiarity with lethal methods had higher overall suicide rates than did those without these factors and that this increase in risk was especially high for women. Additionally, a study13 that relied on data obtained from the CDC NVDRS found that physicians who died by suicide were nearly 40 times as likely to have a positive test result for barbiturates and > 20 times as likely to have a positive test result for benzodiazepines in the postmortem toxicology report as were nonphysicians, consistent with the hypothesis that increased access to lethal drugs may explain a high incidence of death attributed to suicide among physicians. It is possible that veterinarians might be even more likely than physicians to use these substances when attempting suicide, given that veterinarians are likely to have less oversight than physicians regarding access to controlled substances. Consistent with this notion, the use of pharmaceutical poisoning was among the 2 most common methods of suicide for US veterinarians in the studies that have been conducted to date.2,5,8 However, a major limitation of these studies was the amount of detail available regarding suicide methods that were used. For example, it is unclear which specific drugs are most commonly used for this purpose and whether these drugs are being used in or acquired from the workplace.
In addition to veterinarians, other professionals in the veterinary field who experience similar stressors might be even more vulnerable to negative mental health outcomes, including suicide, given their reduced workplace autonomy and generally lower socioeconomic status.14 To our knowledge, there have been no studies investigating suicide deaths among veterinary technicians, technologists, and assistants and laboratory animal caretakers. However, a recent study15 that used NVDRS data in Colorado found that health-care practitioners and technicians were among the 3 occupational groups that had the highest age- and sex-adjusted suicide rates. Veterinary professionals were included within this group of health-care practitioners and technicians, and it is possible but not currently known whether the risk of suicide for veterinary professionals other than veterinarians is different from that for other health-care workers.
In addition to the gaps in knowledge about the risk of death by suicide in subsets of veterinary professionals, a literature search by our group revealed no published studies that provided systematic information regarding prior mental health treatment among veterinary professionals who died by suicide. In the general population, approximately 27% of individuals who die by suicide have been in contact with a mental health professional in the 2 months before their suicide.16 Given the evidence that veterinarians have more negative views toward mental health treatment than the general population,11 it is possible that rates for contact with a mental health professional in this population might be even lower. To our knowledge, almost nothing is known about rates of mental health treatment or contact with mental health workers among veterinary professionals other than veterinarians.
Although mental health conditions are an important risk factor for suicide, suicide is an outcome that arises from a constellation of factors, including life circumstances. As such, it is vital that these circumstances be investigated to inform the development of comprehensive suicide prevention strategies.17 Unfortunately, there is a lack of research examining jobrelated or financial problems in the time leading up to a veterinary professional’s death by suicide. However, investigators of a 2013 study13 in which NVDRS data were used to examine the circumstances of death by suicide among physicians found that these decedents were more likely than nonphysicians to have experienced job-related problems before suicide. Moreover, results of a study18 published in 2015 revealed an increase in suicide rates related to financial and job-related stress among working-age US adults. It is unknown whether this is true of veterinary professionals; however, research over the past decade suggests that professional burnout is common among veterinarians and believed to be increasing,19,20 and job-related and financial stressors such as emotional strain from balancing human and animal needs and student loan debt have often been cited as risk factors for suicide among veterinarians.1 In contrast, little is known about how job-related and financial stressors relate to suicide risk among other veterinary professionals, although results of a survey of veterinary technicians and technologists in 2012 indicated that emotional strain and financial issues such as low wages are challenges among these professionals as well.21 Enhancing our understanding of the role that job-related and financial stressors might have in suicide could inform wellness programs for veterinary professionals.
The purpose of the study reported here was to provide a comprehensive analysis of data for death of veterinary professionals and veterinary students for whom the manner of death was characterized as suicide or undetermined intent from 2003 through 2014. Because most deaths of undetermined manner in the NVDRS records were previously found to involve poisonings16 and previous research suggests that veterinarians are particularly likely to use poisoning as a suicide method,5,8 we determined these cases should be included in the study because of the possibility that such deaths could potentially represent misclassified suicides.
Our primary aims were to determine crude suicide rates and SMRs for suicide and for suicide plus deaths of undetermined intent among veterinary professionals; to obtain updated, comprehensive information about suicide methods used by veterinary professionals through analysis of integrated information from multiple sources such as death certificates and toxicology reports, which is critically needed to identify potential avenues of intervention and policy change; and to obtain information on psychosocial circumstances of death for veterinary professionals who died by suicide or undetermined intent. As previously mentioned, improving our knowledge of jobrelated and financial problems in the time leading up to the suicide death of veterinary professionals might have implications for developing veterinary wellness programs to prevent suicide. We hypothesized that veterinarians would have higher SMRs for suicide, compared with those for the general population (consistent with past research findings), and that findings for other veterinary professionals would be similar to those for veterinarians, given the risk factors shared with veterinarians such as emotional strain and financial stressors.14 We also hypothesized that self-poisoning, and in particular the use of pentobarbital (the drug most commonly involved in euthanasia), would be among the most common suicide methods used by veterinarians. Given the lack of previous research regarding suicide methods among other veterinary professionals, we did not have a hypothesis regarding suicide methods for these individuals. The final hypotheses tested were that veterinary professional decedents would have lower prevalence of mental health treatment, compared with a previously published prevalence for individuals who died by suicide,16 and that job-related and financial stressors would be among the most commonly reported circumstances of death among veterinary professionals with this manner of death.
Materials and Methods
Data sources
Cases were identified by use of the NVDRS, a state-based surveillance system with information about violent deaths (including suicide).22 The usable, anonymous NVDRS database included > 600 variables coded by state data abstractors who were trained according to CDC standards and used all available data sources; the variables included information on the manner of death, characteristics of injury and death, and weapons, suspects, and circumstances associated with the death.23 Information in the source documents used by abstractors resulted from the death investigation process, which included coroner or medical examiner reports, toxicology reports, law enforcement reports (eg, scene investigation and interviews with key informants), and death certificates. Detailed descriptions and criteria for inclusion of variables reported in the present study, including definitions of specific methods (variables termed mechanisms of death or weapons) and circumstances of death, are available elsewhere.24
Data were accessed by study investigators by request through the NVDRS Restricted Access Database process; the datasets were submitted to our research team in September 2016. We analyzed data from January 1, 2003, to December 31, 2014, for the following 18 states that contributed cases to the NVDRS during ≥ 1 of those years: Maryland, Massachusetts, New Jersey, Oregon, South Carolina, and Virginia (2003 to 2014); Alaska, Colorado, Georgia, North Carolina, Oklahoma, Rhode Island, and Wisconsin (2004 to 2014); Kentucky, New Mexico, and Utah (2005 to 2014); Ohio (2010 to 2014); and Michigan (2014).
To protect the anonymity of decedents and in accordance with NVDRS requirements, any data with nonzero frequencies of < 5 cases were suppressed along with any data that would permit the derivation of that number through basic mathematical calculations. For example, if 3 females and 47 males in a sample of 50 died, suppression of both numbers was required.23 Because the present study did not involve living subjects, the National Institute of Occupational Safety and Health’s Institutional Review board determined that it did not require review.
Case identification
Inclusion criteria were that the decedent was employed at any time as a veterinarian, veterinary technician or technologist, or veterinary assistant or laboratory animal caretaker or was identified as a veterinary student at the time of death. Only decedents whose manner of death was either suicide or undetermined intent were included. Three string variables (termed industry text, occupation text, and occupation current) were initially used to identify relevant cases. In addition to indicating each decedent’s occupation, these variables often, but not always, included descriptors, such as unemployed, retired, or disabled, indicating that the person was not employed in the listed occupation at the time of death. However, the lack of such a descriptor did not confirm an individual was employed in that occupation at the time of death.
The initial database contained 205,294 cases. A comprehensive list of keywords was initially used to help identify records for the population of interest; these included animal, D.V.M., DVM, equine, groom, horse, L.V.T., LVT, lab, poultry, tech, vet, doctor, Dr, and student. A spreadsheet macroa was used by the first author (TKW) to identify records for decedents with a match for any of these keywords. These were coded independently by 1 author (EGS) and another GRA to determine a final occupational code for each decedent: veterinarian, veterinary technician or technologist, veterinary assistant or laboratory animal caretaker, veterinary student, or veterinary professional with no further classifying information available (ie, unspecified veterinary professional). Occupational codes for all decedents except for veterinary students and unspecified veterinary professionals were assigned regardless of whether the decedent was still employed (vs previously employed) as such at the time of death. Veterinary technicians or technologists were distinguished from veterinary assistants on the basis of string variables that included a variant of licensed veterinary technician (eg, LVT or L.V.T.) or a variant of tech (eg, technician or technologist). Veterinary technicians and technologists were grouped together and veterinary assistants and laboratory animal caretakers were grouped together because these occupations are grouped together by the BLS SOC, and these data were used in our calculations, which are described in more detail in subsequent text. All records for decedents deemed by both GRAs to have occupational categories not relevant to the study were deleted from the dataset. Records for which the GRAs disagreed on the occupational code were reviewed by the first author, who resolved the occupational code or requested input from the last author (RJN) to determine the final occupational code by consensus.
After records were screened for occupational criteria, the NVDRS abstractor manner of death code in the records was used to identify the final dataset of decedents whose manner of death was suicide (ie, intentional use of force against oneself; World Health Organization International Classification of Diseases codes25 X60 through X84 and X87.0) or undetermined intent (ie, death resulting from the use of force or power against oneself or another person for which the cause is known but for which the evidence indicating one manner of death is no more compelling than the evidence indicating another manner of death; International Classification of Diseases codes Y10 through Y34, Y87.2, and Y89.9). As described elsewhere,16 abstractors used available International Classification of Diseases codes in addition to information available in all source documents to determine final manner of death.
Demographic data for these individuals (age at the time of death, sex, marital status, race and ethnicity, and employment status) were recorded from the NVDRS records. Gender identity and sexual orientation variables were added to NVDRS in 2013 and were unavailable in most cases; thus, these variables were not included in the study. For study purposes, decedents were recorded as employed at the time of death if there were no indicators in the NVDRS record that they were not employed.
Coding and review of death-related data
Most mechanisms of death were determined on the basis of variables included for a given record in the NVDRS. More than 1 mechanism was coded only when multiple mechanisms were determined to have caused fatal injuries (a rare occurrence). If these data were missing from the record, the string variables indicating cause of death derived from the death certificate were reviewed by the first author in consultation with 2 other authors (KAF and RJN); if the mechanism could not be identified, it was recorded as unknown.
In the poisoning category for mechanism of death, information from 2 other sources was used to determine whether pentobarbital or opioid (the 2 most commonly identified substances in the dataset) poisoning had occurred. First, a string variable in the NVDRS that listed up to 3 causes of death obtained from the death certificate was reviewed and independently coded by the first author and a GRA (EGS); any disagreements were resolved with input from the last author. Second, the NVDRS substance name variables that indicated findings in toxicology reports were reviewed. These substance name variables included a string variable with the name of the substance as well as a variable indicating whether that substance had caused death. Decedents who had pentobarbital or opioid poisoning indicated as a cause of death on the death certificate, had pentobarbital or an opioid listed as a substance name variable for the cause of death in their NVDRS record, or both had poisoning by the substance listed as a mechanism of death.
The physical and psychosocial circumstances of death were recorded from coded variables in the NVDRS record. In accordance with user instructions for the NVDRS,24 records of individuals for whom circumstances of death were completely unknown were filtered out before proceeding with this analysis.
Data analysis
Intercoder agreement for occupational codes assigned during the initial screening of NVDRS records and intercoder agreement for the presence of pentobarbital or opioid poisoning during review for the mechanism of death were assessed by calculation of the Cohen κ statistic. Agreement was rated according to widely used standards for κ: almost perfect, 0.81 to 1.0; substantial, 0.61 to 0.80; moderate, 0.41 to 0.60; fair, 0.21 to 0.40; slight, 0 to 0.20; and poor, 0.26
Crude suicide rates were calculated by sex and occupational group for veterinary professionals listed as employed at the time of death by determining the number of observed deaths by suicide for the specified occupational group and sex in NVDRS-participating states during 2003 through 2014, dividing that number by the sum of people of the same sex and occupational group working in the same states during those years, and multiplying the quotient by 100,000 to yield the rate of suicides per 100,000 individuals in the specified population.
The same calculation was performed for deaths that were classified as either suicide or undetermined intent. A likely retirement age of 70 years was assumed for these analyses; therefore, we included observed deaths only for decedents ≤ 69 years of age in these rate calculations. Data from the US BLS were used to determine the number of people working in each NVDRS-participating state during each study year for the following occupational groups: veterinarians (BLS SOC, 29–1130 and 29–1131), veterinary technicians or technologists (BLS SOC 29–2056), and veterinary assistants or laboratory animal caretakers (BLS SOC 31–9096).b Because BLS data do not include the number of workers by sex, we relied on survey data from several organizations to estimate the proportion of males and females in each occupational group across the United States for each study year. The proportion of males and females determined for each occupational group and study year by use of survey data was multiplied by the BLS-derived total number of workers for each occupational group and study year. Market research statistics data,27 available from the AVMA for the years 2006 through 2014, were used to estimate the percentage of male and female US veterinarians for each study year. No data were available for the years 2003 through 2005; thus, the information from 2006 was used for each year during this period. Data from a 2012 survey conducted by the National Association of Veterinary Technicians in America (which indicated 95% of surveyed veterinary technicians were female) were used to estimate the percentage of male and female US veterinary technicians or technologists for each study year.21 To calculate the proportion of male and female veterinary assistants or laboratory animal caretakers, we made an estimate of 80% female and 20% male for each study year on the basis of national data from the Data USA website.c The proportions of male and female veterinary students were derived from data provided by the Association of American Veterinary Medical Colleges for each year of the study and each included state.d In accordance with NVDRS reporting guidelines,24 crude suicide rates were reported only for occupational groups in which there were ≥ 20 cases of suicide.
Calculation of SMRs for suicide alone (ratio of the observed to expected number of suicide deaths in the study) was performed with the observed suicide deaths of individuals 25 to 69 (veterinarians) or 20 to 69 (all other occupational groups and veterinary students) years of age for each occupational group drawn from the NVDRS records during the study period, as previously described. To provide additional information, similar SMR calculations for suicide alone and for suicide or death by undetermined intent were performed for decedents up to 74 years of age and those employed at the time of death or ever employed in their assigned occupational categories. The number of expected deaths by suicide for each of these calculations was determined by use of data from multiple sources.
First, the total number of US men and women in the general population from 25 to 69 years of age (for comparison with veterinarians) and from 20 to 69 years of age (for comparison with veterinary technicians or technologists, veterinary assistants or laboratory animal caretakers, and veterinary students) for each NVDRS-participating state in each study year was determined from US intercensal population estimates.c The difference in these age ranges reflected the fact that veterinarians are required to complete 4 years of postgraduate training before entering the workforce. Second, the US intercensal population estimates from all US states were used to determine the percentage contribution of each 5-year age category for each sex and study year for each occupational group. The 5-year categories were used to enable comparisons with available sex-specific suicide rates available for the US general population calculated for 5-year age intervals. For veterinary students, we estimated the percentage contribution of each 5-year age category for each sex and study year on the basis of data available for medical students from 2014 to 2018.28 Third, the number of people working in each NVDRS-participating state and the proportions of males and females were determined for each occupational group and study year as described for the calculation of crude suicide rates. From these data, the numbers of males and females of each 5-year age category working in each occupational group and in each state for each study year were summed.
Because the identified dataset of veterinary professionals or students who died by suicide or undetermined intent was predominantly characterized as white and non-Hispanic and, to the authors’ knowledge, detailed data on proportions of people of each race and ethnicity are unavailable for veterinary professions, the US suicide rates for white, non-Hispanic males and females were obtained from the National Center for Health Statisticse (multiple cause of death files from 1999 through 2014, compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program) and used to calculate the number of expected suicides for males and females of each 5-year age category by occupational group and study year. The numbers of expected suicides grouped by the 5-year age category for each sex, year, and occupational group were then summed. Statistical softwaref was used to calculate SMRs and 95% CIs with indirect standardization. The SMRs were considered significant when the 95% CI did not include 1.
In addition to calculating crude suicide rates and SMRs, frequencies of various demographic findings and circumstances related to death were determined and compared among occupational groups with χ2 tests. When significant (P < 0.05) differences were detected, these were investigated by use of follow-up z tests for proportions with the Bonferroni correction. These analyses were conducted with statistical software.g
Results
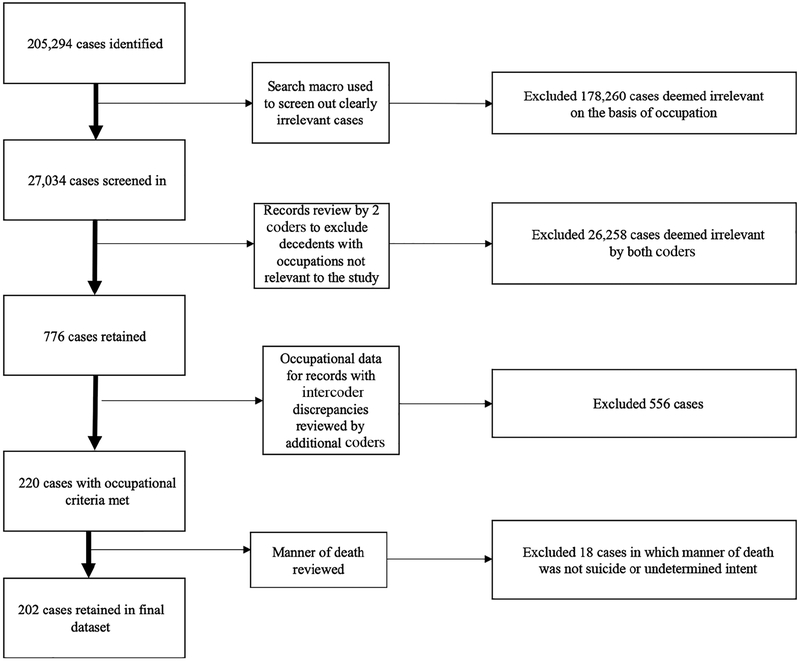
Initial screening of the 205,294 NVDRS records with the spreadsheet macro yielded 27,034 decedent records that matched keywords used to select for veterinary professional occupations (Figure 1). The codes initially assigned by the 2 GRAs were found to have almost perfect agreement (κ = 0.89). All records for decedents deemed by both GRAs to have occupational categories not relevant to the study (n = 26,258) were deleted, leaving 776 decedent records. Of these, there was occupational code disagreement for 642 (2.4% of the 27,034 records that met initial screening criteria). Review by 1 author (TKW) resolved occupational code disagreement for 510 of 642 (79.4%) records. For the remaining 132 (20.6%) records with discordant codes, consensus was reached between 2 authors (TKW and RJN) regarding the final occupational code. Of the 642 decedent records with discrepant code assignments, 556 decedents were deemed to have occupations not applicable to the study and were excluded. Screening for manner of death excluded records for 18 decedents for whom neither suicide nor undetermined intent was recorded for this variable. Records of 202 decedents (73 veterinarians, 77 veterinary technicians or technologists, 39 veterinary assistants or laboratory animal caretakers, 8 unspecified veterinary professionals, and 5 veterinary students) were included in the study.
Figure 1—
Flow diagram depicting selection, inclusion, and exclusion of NVDRS records (cases) for use in a study to analyze data regarding death of veterinary professionals and veterinary students, with manner of death characterized as suicide or undetermined intent from 2003 through 2014.
On evaluation of poisoning as a mechanism of death, there was almost-perfect intercoder agreement for the presence of pentobarbital (κ = 1.00) or opioid (κ = 0.93) poisoning. Disagreement was found for 3 of 202 (1.5%) records and was resolved for all 3 with input from the last author.
Demographic characteristics for veterinary professionals whose NVDRS records review indicated death by suicide or death of undetermined intent were summarized by occupational group (ie, excluding veterinary students and unspecified veterinary professionals; Table 1). Sex, marital status, and age distributions differed significantly among veterinarians, veterinary technicians or technologists, and veterinary assistants or laboratory animal caretakers whose manner of death was assigned to these categories. Veterinarian decedents were more likely to be male, married, and older than decedents from the other 2 occupational groups. Additionally, veterinary assistant or laboratory animal caretaker decedents were less likely to be categorized as white and non-Hispanic than were decedents from the other 2 occupational groups.
Table 1—
Demographic characteristics obtained from NVDRS records for 189 veterinary professionals who died by suicide or had death of undetermined intent from 2003 to 2014, categorized by occupational group.
| Variable | Veterinarians (n = 73) | Veterinary technicians or technologists (n = 77) | Veterinary assistants or laboratory animal caretakers (n = 39) | P value |
|---|---|---|---|---|
| Sex | < 0.001 | |||
| Male | 54 (74%)a | 21 (27%)b | 13 (33%)b | |
| Female | 19 (26%)a | 56 (73%)b | 26 (67%)b | |
| Marital status | < 0.001 | |||
| Married or part of a civil union | 37 (51%)a | 24 (31%)b | 9 (23%)b | |
| Never married | 14 (19%)a | 31 (40%)b | 20 (51%)b | |
| Widowed, divorced, or separated | 22 (30%)a | 16 (21%)a | 10 (26%)a | |
| Single (otherwise specified) or unknown | 0 (0%)a | 6 (8%)b | 0 (0%)a,b | |
| Race and ethnicity | 0.001 | |||
| White, non-Hispanic | 71 (97%)a | 72 (94%)a | 29 (74%)b | |
| Nonwhite, non-Hispanic (including multiracial) | —a | —a | —b | |
| Hispanic | —a | —a | —a | |
| Age (y) | < 0.001 | |||
| 15–19 | 0 (0%)a | —a | —a | |
| 20–29 | —a | 23 (30%)a | 12 (31%)b | |
| 30–39 | 9 (12%)a | 28 (36%)b | 10 (26%)a,b | |
| 40–49 | 14 (19%)a | 17 (22%)a | 10 (26%)a | |
| 50–59 | 26 (36%)a | 5 (7%)b | —b | |
| 60–69 | 10 (14%)a | —a | —a | |
| 70–74 | —a | 0 (0%)a | 0 (0%)a | |
| ≥ 75 | 12 (16%)a | 0 (0%)b | 0 (0%)a,b | |
| Employment status at time of death | 0.64 | |||
| Employed | 61 (84%) | 67 (87%) | — | |
| Not employed | 12 (16%) | 10 (13%) | — |
Data are shown as number (%). Values for 13 decedents (8 veterinary professionals without a specified category and 5 veterinary students) were excluded from the table. Because of rounding, some percentages do not total 100%. The NVDRS included data from 18 states during the study period (Maryland, Massachusetts, New Jersey, Oregon, South Carolina, and Virginia [2003–2014]; Alaska, Colorado, Georgia, North Carolina, Oklahoma, Rhode Island, and Wisconsin [2004–2014]; Kentucky, New Mexico, and Utah [2005–2014]; Ohio [2010–2014]; and Michigan [2014]). The P values reflect the results of χ2 analysis for a given variable; values of P < 0.05 were considered significant.
Within a row, values with different superscripted letters were significantly different by the z test for proportions with Bonferroni correction (performed when significant differences were found by χ2 analysis).
Data suppressed for protection of decedent confidentiality and compliance with NVDRS reporting requirements because of small numbers.
Crude suicide rates and SMRs
The crude rates for suicide among male veterinarians (n = 34) and female veterinary technicians or technologists (37) were 35.8 per 100,000 and 14.4 per 100,000, respectively. In accordance with NVDRS data-reporting restrictions, rates for groups with < 20 cases (all other decedent groups) could not be reported. On analysis of deaths that were classified as either suicide or undetermined intent, the pattern of results was similar to that for suicide alone; the crude rates for male veterinarians (n = 36) and female veterinary technicians or technologists (n = 47) were 37.9 per 100,000 and 18.3 per 100,000, respectively. Including this additional manner of death category also allowed calculation of a crude rate for death by suicide or of undetermined intent among female veterinary assistants or laboratory animal caretakers (n = 22; crude rate, 11.3 per 100,000).
The SMRs for suicide were summarized for decedents classified as employed at the time of death, categorized by sex and occupational group (Table 2). Overall, the SMRs for male and female veterinarians and male and female veterinary technicians or technologists were significantly higher than those of the general population, whereas the SMRs for male and female veterinary assistants or laboratory animal caretakers were not. The SMRs for each occupational group by sex were similar when broader criteria (age up to 74 years [only found for veterinarians], any employment status at the time of death, and inclusion of deaths of undetermined intent in addition to deaths by suicide in the calculations) were applied (Supplementary Table S1, available at avmajournals.avma.org/doi/suppl/10.2460/javma.255.5.595).
Table 2—
Standardized mortality ratios for suicide among 128 of the 189 decedents in Table 1 who were classified as employed at the time of death.
| No. of deaths | |||
|---|---|---|---|
| Category | Observed | Expected | SMR (95% CI) |
| Veterinarians | |||
| Male | |||
| All deaths by suicide | 34 | 21.5 | 1.6 (1.1–2.1) |
| Pentobarbital poisoning excluded | 24 | 21.5 | 1.1 (0.7–1.6) |
| Female | |||
| All deaths by suicide | 16 | 6.6 | 2.4 (1.2–3.6) |
| Pentobarbital poisoning excluded | 10 | 6.6 | 1.5 (0.6–2.5) |
| Veterinary technicians or technologists | |||
| Male | |||
| All deaths by suicide* | 15 | 3.0 | 5.0 (2.5–7.6) |
| Female | |||
| All deaths by suicide | 37 | 15.9 | 2.3 (1.6–3.1) |
| Pentobarbital poisoning excluded | 32 | 15.9 | 2.0 (1.3–2.7) |
| Veterinary assistants or laboratory animal caretakers | |||
| Male | |||
| All deaths by suicide* | 9 | 10.8 | 0.8 (0.3–1.4) |
| Female | |||
| All deaths by suicide | 17 | 12.1 | 1.4 (0.7–2.1) |
| Pentobarbital poisoning excluded | — | — | — |
Data are reported for 25- to 69-year-old veterinarians, 20- to 69-year-old veterinary technicians or technologists, and 20- to 69-year-old veterinary assistants or laboratory animal caretakers; age limits were selected on the basis of on an assumed retirement age of 70 for all decedents and additional time for postgraduate study prior to employment for veterinarians. This analysis excluded deaths of undetermined intent; the SMR for a given group indicates a significant difference in the rate of death by suicide, compared with that for the general population, when the 95% CI does not include 1.
No deaths involving pentobarbital poisoning were recorded for these groups.
See Table 1 for remainder of key.
Given the small number of records for decedents classified as veterinary students, the SMRs calculated for veterinary students included deaths by suicide and of undetermined intent. Most of these decedents were female, white and non-Hispanic, and single or never married; ages ranged from 24 to 35 years. The SMRs for male and female veterinary students were 0.8 (95% CI, 0 to 2.3) and 4.1 (95% CI, 0.1 to 8.1), respectively; neither finding was significantly different from that for the general population, and the wide CIs reflected the uncertainty of these estimates. Detailed data and statistics for other findings could not be reported because of the small sample size.
Most decedents classified as unspecified veterinary professionals were female, white and non-Hispanic, and divorced; their ages ranged from 17 to 64 years. All 8 decedents in this group were classified as employed at the time of death. Owing to the unspecified employment category, no comparison group could be established for the calculation of SMRs. Detailed data and statistics for other findings could not be reported because of the small sample size.
Manner, physical circumstances, and mechanisms of death
Death and death-related injury variables were summarized for veterinary professionals by occupational group (Table 3). The records of 2 decedents had missing mechanism or weapon variable codes; one death was attributed to firearms injury on retrospective review of the record, and the other was coded as unknown. There were few differences in the distributions of these variables among the 3 groups; however, veterinarians were more likely to have death characterized as suicide (instead of undetermined intent) than were decedents of the other 2 groups. Additionally, although self-poisoning was the most common mechanism of death for all groups, veterinarians were more likely to have poisoning with pentobarbital than decedents of the other 2 occupational groups and were less likely than veterinary technicians or technologists to have poisoning with opioids. Most (166/189 [88%]) decedents did not incur the fatal injury at work.
Table 3—
Death and death-related injury variables for the 189 decedents in Table 1.
| Variable | Veterinarians (n = 73) | Veterinary technicians or technologists (n = 77) | Veterinary assistants or laboratory animal caretakers (n = 39) | P value |
|---|---|---|---|---|
| Manner of death | 0.008 | |||
| Suicide | —a | 59 (77%)b | 31 (80%)b | |
| Undetermined intent | —a | 18 (23%)b | 8 (21%)b | |
| Alcohol use suspected in hours prior to death† | 0.73 | |||
| Yes | 17 (23%) | 19 (25%) | 12 (31%) | |
| No | 40 (55%) | 46 (60%) | 19 (49%) | |
| Unknown or not recorded | 16 (22%) | 12 (16%) | 8 (21%) | |
| Decedent seen in emergency department‡ | 0.90 | |||
| Yes | 6 (8%) | 10 (13%) | 5 (13%) | |
| No | 39 (53%) | 38 (49%) | 20 (51%) | |
| Unknown or not recorded | 28 (38%) | 29 (38%) | 14 (36%) | |
| Injury occurred at decedent’s residence | 0.20 | |||
| Yes | 56 (77%) | 55 (71%) | 23 (59%) | |
| No | — | — | — | |
| Unknown or not recorded | — | — | — | |
| Injury occurred at work | 0.23 | |||
| Yes | — | — | — | |
| No | 60 (82%) | 70 (91%) | 36 (92%) | |
| Unknown or not recorded | — | — | — | |
| Mechanism of death§ | ||||
| Poisoning | 34 (47%) | 38 (49%) | 14 (36%) | 0.38 |
| Pentobarbital | 18 (25%)a | 5 (7%)b | —b | < 0.001 |
| Opioid | —a | 16 (21%)b | 5 (13%)ab | 0.009 |
| Firearm injury | 29 (40%) | 20 (26%) | 9 (23%) | 0.10 |
| Hanging, strangulation, or suffocation | 7 (10%) | — | 9 (23%) | 0.10 |
| Other single mechanism ‖ or unknown | —a,b | —b | —a | 0.02 |
Criteria for evidence to include codes for specific death and injury-related variables in NVDRS records are described in detail elsewhere.24
Recorded on the basis of evidence at the scene, witness reports, or both (distinct from toxicological findings).
Recorded as yes for any individual who arrived at the emergency department of a human medical facility, whether alive or dead on arrival.
Three decedents each had 2 mechanisms of death listed.
Examples of other mechanisms included blunt force trauma or drowning.
See Table 1 for remainder of key.
Toxicological data for substances that were present in the decedents’ systems, regardless of whether they were listed as causes of death, were summarized (Table 4). Not all decedents were tested for every substance. There were generally no differences for the presence of various substances across occupational groups, with the exception of opioids, which were more likely to be detected for veterinary technicians or technologists than for veterinarians. There was also a significant difference in the presence of carbon monoxide as determined with the omnibus χ2 test, but follow-up tests did not reveal significant differences between occupational groups after Bonferroni correction.
Table 4—
Toxicological test results for subsets of decedents in Table 1 who died by suicide or had death of undetermined intent and were tested for each substance.
| Substance type | No. of tests | Veterinarians | Veterinary technicians or technologists | Veterinary assistants or laboratory animal caretakers | P value |
|---|---|---|---|---|---|
| Alcohol | 131 | 24/47 (51%) | 16/55 (29%) | 14/29 (48%) | 0.13 |
| Amphetamine | 98 | — | — | — | 0.92 |
| Benzodiazepines | 30 | 5/12 (42%) | — | — | 0.85 |
| Cocaine | 103 | — | 6/40 (15%) | — | 0.35 |
| Marijuana | 69 | — | — | — | 0.75 |
| Anticonvulsants | 24 | 6/14 (43%) | — | — | 0.79 |
| Muscle relaxants | 21 | — | — | 0/5 (0%) | 0.36 |
| Opioids | 109 | 5/40 (13%)a | 21/44 (48%)b | 7/25 (28%)a,b | 0.01 |
| Carbon monoxide | 7 | —a | —a | —a | 0.03 |
| Barbiturates | 29 | 7/14 (50%) | — | 0/5 (0%) | 0.12 |
| Antipsychotics | 20 | 0/9 (0%) | — | — | 0.40 |
Substances were listed in the records as present, not present, or unknown (if tested for) or not applicable (if not tested for). Data were summarized as proportion (%) of tests for each occupational group in which the substance was classified as present. Not all decedents were tested for all substances.
See Table 1 for key.
For veterinary students, most deaths were classified as suicides, and none of these decedents used pentobarbital poisoning as a mechanism of suicide. All deaths of unspecified veterinary professionals were classified as suicides; most of these decedents used a firearm, and none used pentobarbital poisoning as a mechanism of suicide. Detailed statistics could not be reported for these variables.
Psychosocial circumstances of death
Information regarding psychosocial circumstances of death for suicides and deaths of undetermined intent was tabulated for decedents by occupational group (Table 5). Generally, the distributions for these variables, when known, were similar across occupational groups; however, veterinarians were significantly less likely to have a history of a suicide attempt before the fatal incident, compared with the other 2 groups. Fifty of 177 (28.2%) decedents across all 3 occupational groups had disclosed their suicidal intent prior to their deaths, 97 of 177 (54.8%) had a history of mental health treatment, and 74 of 177 (41.8%) were undergoing mental health or substance abuse treatment at their time of death. Thirty of 141 (21.3%) veterinarians and veterinary technicians or technologists were reported to have a contributing job problem, and 15 of these 141 (10.6%) were reported to have a contributing financial problem. Results for veterinary assistants or laboratory animal caretakers could not be reported owing to small numbers. Data for veterinary students and unspecified veterinary professionals were also not reported for this reason; however, most had no known history of a suicide attempt before the fatal incident, had not disclosed suicidal intent before their deaths, had no known history of receiving mental health treatment, and did not have a contributing school, job, or financial problem recorded, and the fatal injury did not take place at work (there was no NVDRS variable for school as the site where injury occurred).
Table 5—
Psychosocial circumstances of death for 177 of the 189 decedents in Table 1 who died by suicide or had death of undetermined intent with information available in NVDRS records.
| Variable | Veterinarians (n = 67) | Veterinary technicians or technologists (n = 74) | Veterinary assistants or laboratory animal caretakers (n = 36) | P value |
|---|---|---|---|---|
| History of suicide attempt before the fatal incident | 9 (13%)a | 28 (38%)b | 13 (36%)b | 0.003 |
| Suicide intent disclosed to another person | 22 (33%) | 18 (24%) | 10 (28%) | 0.53 |
| Suicide note left | 21 (31%) | 26 (35%) | 13 (36%) | 0.85 |
| Crisis¶ | 20 (30%) | 19 (26%) | 9 (25%) | 0.81 |
| Mental health problem at time of death | 36 (54%) | 44 (60%) | 23 (64%) | 0.58 |
| Mental health or substance abuse treatment ≤ 2 mo prior to death | 23 (34%) | 34 (46%) | 17 (47%) | 0.29 |
| History of mental health or substance abuse treatment (at any time) | 33 (49%) | 41 (55%) | 23 (64%) | 0.36 |
| Depressed mood | 30 (45%) | 27 (37%) | 11 (31%) | 0.33 |
| Alcohol problem | 11 (16%) | 13 (18%) | 12 (33%) | 0.09 |
| Other substance abuse | 9 (13%) | 18 (24%) | 12 (33%) | 0.06 |
| Intimate partner problem | 16 (24%) | 24 (32%) | 10 (28%) | 0.53 |
| Family relationship (other than intimate partner) problem | — | — | 0 (0%) | 0.34 |
| Other relationship problem | 6 (9%) | — | — | 0.67 |
| Contributing criminal legal problem | 5 (8%) | 6 (8%) | — | 0.56 |
| Contributing civil legal problem | — | — | — | 0.51 |
| Contributing physical health problem | 16 (24%) | 9 (12%) | — | 0.11 |
| Contributing job problem | 14 (21%) | 16 (22%) | — | 0.09 |
| Contributing financial problem | 10 (15%) | 5 (7%) | — | 0.26 |
| Death of friend or family member | 8 (12%) | — | — | 0.10 |
Definitions of the described circumstances and criteria for evidence to include the related codes in NVDRS records are described in detail elsewhere.24 Variables were recorded as present vs unknown or not present. Some decedents had multiple circumstances of death on record.
Includes only acute events that were imminent at the time of death or had occurred up to 2 weeks earlier; a single code was used from 2003 through 2012, and separate codes were used to additionally specify types of crisis events beginning in 2013; a code applied to any crisis was used for the latter year so that the data were comparable for analysis purposes.
See Table 1 for remainder of key.
Additional analyses
Given the findings regarding pentobarbital and the unique status of this drug in the veterinary industry (ie, that pentobarbital poisoning is a suicide method unlikely to be accessible to individuals outside of the veterinary industry), several follow-up analyses were added to the investigation. First, SMRs for suicide were calculated as previously described, except that records of decedents who had pentobarbital poisoning listed as a mechanism of death were excluded; when these records were removed from the analysis, the SMRs for suicide of male and female veterinarians were no longer significantly different from those for the general population. The SMRs for female veterinary technicians or technologists and female veterinary assistants or laboratory animal caretakers, which were the only other groups with pentobarbital listed as a mechanism of death, did not change substantially with these records excluded. Second, demographic, death and death-related injury, and psychosocial variables were investigated for an association with pentobarbital poisoning (the most commonly reported self-poisoning substance) versus firearms injury (the second most common mechanism of death) of veterinarians (Supplementary Tables S2–S4, available at avmajournals.avma.org/doi/suppl/10.2460/javma.255.5.595). The only differences between these 2 groups were that decedents with pentobarbital poisoning were less likely to have data unknown or not recorded with regard to having been seen in the emergency department of a human medical facility and were more likely to have left a suicide note than were decedents with firearms injury. Similar to results when all mechanisms of death were considered, the fatal injury in most firearms-related and pentobarbital-related deaths occurred at the decedent’s residence.
Discussion
To the authors’ knowledge, the study reported here was the most comprehensive investigation of suicide among US veterinarians to date and the first to examine deaths by suicide among veterinary technicians or technologists and veterinary assistants or laboratory animal caretakers. Calculation of SMRs revealed that veterinarians and veterinary technicians or technologists had significantly higher rates of death by suicide, compared with findings for the general population, whereas veterinary assistants or laboratory animal caretakers did not. One strength of our study, compared with others in the literature, was the ability to calculate SMRs instead of PMRs.1 Overall, the SMRs for veterinarians in our study were similar to PMRs for veterinarians in the literature,8 which suggests that the high PMRs from suicide among veterinarians in previous studies are not artificially inflated by lower frequency of death from other causes. Our examination of differences among the 3 occupational groups revealed that although a number of demographic characteristics for decedents (eg, sex, age, and race and ethnicity) differed among the occupational groups, the circumstances of death were similar across occupational groups, with a few key exceptions.
The most notable difference between veterinarians and the other veterinary occupational groups was that veterinarians were significantly more likely to have used pentobarbital as a suicide method. Research has found that veterinarians who die by suicide are particularly likely to use self-poisoning as a method5,8 and that the use of barbiturates is the most common form of self-poisoning among veterinarians who die by suicide.1,2,h This is in contrast to findings for members of the general US male population, for whom firearms are the most common suicide method overall; < 10% of this population use self-poisoning as a suicide method.i Among the general US female population, self-poisoning is slightly more common than firearms as a suicide method.i The authors are unaware of any previous studies in which pentobarbital was isolated as a specific barbiturate used for suicide by veterinarians, and although it has been assumed veterinarians have a high suicide risk because of their access to certain lethal means such as pentobarbital,1,29 we believe the present study was the first to provide evidence supporting this possibility. After the records of decedents for whom pentobarbital poisoning was indicated as a mechanism of death were removed from the dataset, the SMRs for male and female veterinarians no longer indicated a difference in suicide rates, compared with the general population. This provided compelling evidence that access to pentobarbital might explain the high risk of suicide among veterinarians, and this has critical implications for prevention efforts. Specifically, restricting access to lethal methods for persons at risk of suicide is among the strategies with the best available evidence for suicide prevention30 and has been identified as such in the CDC’s technical package of suicide prevention strategies.31 Although critics of this strategy often raise the concern that method substitution will occur (ie, that restricting access to one suicide method will simply result in another method being employed), data from prior studies30,32 suggest that limiting access to widely used suicide methods tends to result in an overall decrease in the incidence of suicide within a population, without an attendant increase in the selection of other suicide methods. Additionally, limiting access to a method that is highly likely to be lethal, such as pentobarbital poisoning, can save lives even if method substitution does occur, insofar as the method being substituted is less likely to be lethal.30 Indeed, a recent meta-analysis found that among people who made a nonfatal suicide attempt, < 10% died from a subsequent suicide attempt.33 Thus, limiting access to lethal means for an initial suicide attempt can be lifesaving.
The CDC National Institute for Occupational Safety and Health describes a hierarchy of controls for limiting exposure to occupational hazards.34 Regarding pentobarbital in veterinary settings, it is neither feasible nor desirable to use elimination controls, which involve physically removing the hazard; substitution controls, which involve replacing the hazard; or engineering controls, which involve isolating people from the hazard. This leaves administrative controls, which involve changing the way people work, as the most viable option. Of course, it is important to consider how to increase administrative controls for pentobarbital without hindering veterinarians in the performance of essential job functions. One particularly relevant model comes from a study35 conducted in Hong Kong, where the use of charcoal burning (for generation of carbon monoxide) as a suicide method had become increasingly common.36 Yip et al35 investigated the effectiveness of increased administrative control of charcoal purchases as a suicide prevention strategy. This quasi-experimental study was performed in 2 neighboring districts. In the intervention district, consumers were no longer able to purchase charcoal from open shelves in retail stores. Instead, charcoal was secured in each store and had to be obtained by making a verbal request to a store clerk. In the control district, charcoal could be purchased as usual. This modification was associated with a reduced rate of suicide by this method in the intervention district but not in the control district; importantly, method substitution did not appear to occur, as there was no increase in the rate of suicide by other methods in the intervention district. It is possible that a minor change in the means by which veterinarians access pentobarbital, such as requiring a second person’s signature when accessing the drug, could have a preventive effect for suicide among veterinarians, while still allowing routine access for clinical purposes. Increased administrative controls could also make it more difficult for a veterinarian to take pentobarbital out of the clinic to be used outside of the workplace, where most of the pentobarbital-related suicides in our sample occurred. An important next step in this line of research is investigating the feasibility and acceptability of increasing administrative controls for pentobarbital in veterinary clinics; it will be crucial to do this in consultation with the veterinary community to enhance buy-in among key stakeholders. It will also be important to consider whether increasing administrative controls for other substances that could be used for suicide, such as opioids, should be pursued in tandem with increased administrative controls for pentobarbital.
Regarding toxicological data for the study sample, few differences were identified among occupational groups, except that opioids were more likely to be detected in veterinary technicians or technologists than in veterinarians. This was consistent with our finding that veterinary technicians or technologists were more likely than veterinarians to use opioids as a suicide method. However, toxicological findings of the present study should be viewed with caution, given that many substances were not routinely tested for in the study sample, and toxicological testing practices vary among states and localities.16 Most notably, only 29 decedents were tested for the presence of barbiturates. This suggested that first responders and emergency department physicians might overlook potential barbiturate poisoning and should consider barbiturates in the differential diagnoses for veterinary professionals evaluated because of loss of consciousness or potential intoxication.
Another key difference across occupational groups was that veterinarians were significantly less likely to have a history of a suicide attempt prior to the fatal incident, compared with the other 2 occupational groups. Results of a 2014 survey of US veterinarians revealed that respondents were more likely to have considered suicide but were less likely to have made a nonfatal suicide attempt, compared with the general population.11 It was proposed that veterinarians might be more likely to die by suicide on their first attempt because of increased knowledge about and access to lethal means,11 and our results were consistent with this idea. To our knowledge, the present study was the first investigation of suicide deaths of US veterinarians to provide empirical data on this subject.
We found no significant differences among occupational groups regarding the likelihood of communicating suicidal intent to another person. Consistent with previously reported findings for the general US population,16 fewer than one-third of decedents across all occupational categories had made such a disclosure before their deaths. There were also no differences among occupational groups with respect to receiving mental health or substance abuse treatment at the time of death or having a history of such treatment. A sizeable minority of the study sample had received mental health or substance abuse treatment in the 2 months before death, including 23 of 67 (34%) veterinarians, 34 of 74 (46%) veterinary technicians or technologists, and 17 of 36 (47%) veterinary assistants or laboratory animal caretakers. These findings were largely in line with the proportion of 27% among persons who died by suicide in the general US population as described by Jack et al,16 suggesting that veterinary professionals might not have a particular deficit in seeking treatment and might be more likely to access treatment than members of the general US population.
Another notable finding was the modest proportion of veterinary professionals overall who had job and financial problems perceived as contributing to their suicide; there were also no differences among occupational groups for either of these variables. The proportion of veterinary professionals who had a contributing job or financial problem (7% to 22% for groups with reportable data) varied only slightly from what has been reported among the general population of suicide decedents 40 to 64 years of age in the NVDRS (ie, 16.5% and 16.3%, respectively).18 Work-related and financial stressors have often been considered leading risk factors for suicide among veterinarians,1 but our results did not indicate that job and financial stressors are common among veterinarians who die by suicide. Likewise, the proportion of veterinary professionals in our sample with a mental health problem at the time of death (103/177 [58.2%]) was similar to that observed among the general population of suicide decedents (50.1%) according to 2015 NVDRS data.16 From a prevention standpoint, although all of these factors might be predictive of suicide in general, they did not appear to be particularly common among veterinarian suicide decedents in the present study or to account for the increased SMRs for suicide among these individuals. As such, prevention efforts that target access to lethal means such as pentobarbital could more specifically address the underlying mechanism of higher rates of death by suicide among veterinarians.
Considering that veterinary technicians or technologists had increased SMRs for suicide that did not appear to be explained by access to pentobarbital, other factors should be considered. As previously mentioned, this group had higher likelihood of opioid poisoning, compared with veterinarians; it was unknown whether these substances were obtained in clinical settings or elsewhere. If these agents were obtained in the workplace, this would suggest that greater administrative controls on these substances could also be an effective suicide prevention strategy for veterinary technicians or technologists. Otherwise, there were few differences in circumstances of death between veterinary technicians or technologists and the other veterinary occupational groups in our study. Thus, there is a critical need for additional research on suicide risk factors among veterinary technicians or technologists. Additionally, all members of the veterinary industry could potentially benefit from implementation of evidence-based upstream suicide prevention strategies, such as those that promote social connectedness, identify and support people at risk, and enhance coping and problem-solving skills.31
In addition to our primary analyses, the present study provided some preliminary data regarding veterinary student deaths by suicide. However, the small number of available cases yielded wide CIs for the SMRs that were generated and prevented the reporting of detailed information regarding circumstances of death. To date, there have been no detailed investigations of death from suicide among veterinary students, and our experience revealed that the NVDRS is not an optimal source for these data. Specifically, there were numerous decedents identified as students in our initial screening efforts, but in many cases we were unable to ascertain whether these were veterinary students, as the field of study or type of school did not appear to be recorded systematically on death certificates. Colleges of veterinary medicine are better positioned to collect and record information about student suicides, which can be investigated in future research. To our knowledge, this information is not being systematically collected at present, and we therefore encourage colleges of veterinary medicine to consider doing so in the future.
Despite its strengths, the present study had a number of limitations. First, we used suicide rates for white, non-Hispanic people to calculate the number of expected suicides for each veterinary professional occupational group. It is well-established that white, non-Hispanic individuals have a higher suicide rate in the US general population than most other racial and ethnic groups.10 Thus, this decision might have yielded underestimates of the SMRs, particularly for the veterinary assistant or laboratory animal caretakers group, which was more diverse than the other 2 occupational groups. Second, the NVDRS relies on partnerships between states and local agencies to obtain the information recorded in the database; the degree of completeness might vary among and within states, and it also depends on the degree of knowledge available to family, friends, and other informants in an investigation, which might vary. Other limitations of the NVDRS have been described elsewhere.16 Third, related to the previous point, information regarding whether a decedent was employed in a particular occupation at the time of death was not always available. When there was sufficient information to indicate a decedent was not employed at the time of death, we used it to exclude that individual from certain analyses, resulting in more conservative estimates than values that would have resulted if we included everyone who was ever employed in that occupation. We also calculated SMRs with various inclusion criteria, and there were only minor differences depending on whether we excluded decedents who were not employed at the time of death. Thus, although we might have mistakenly included some unemployed decedents in the analyses of those who were employed at the time of suicide, we were confident this did not substantively impact our results. Fourth, the proportion of male and female veterinary professionals in each occupational group was estimated on the basis of data from multiple surveys. Biases in the original surveys could have resulted in overestimation or underestimation of the sex-specific suicide rates reported in our study. Moreover, the estimation procedures for occupational groups did not account for variation in the sex distribution across states over time, except for veterinarians, for whom there were annual estimates from 2006 through 2014. Fifth, the BLS does not collect information on self-employed people for its occupational employment statistics program,j which could have resulted in an underestimation of the denominators for veterinarians and an overestimation of the respective SMRs. Finally, to our knowledge, the present study was the most comprehensive investigation of suicide among veterinary professionals in the United States to date; however, the sample was still relatively small, limiting power to detect differences across occupational groups, and it might not have been representative of all veterinary professionals who died by suicide because the NVDRS was not yet nationally representative. However, the NVDRS has recently been expanded to include all 50 states, Puerto Rico, and Washington, DC.37 Thus, a replication of the present study with information available in the expanded NVDRS database would have additional statistical power and yield results that might be more representative of these groups.
Notwithstanding the limitations in our approach, the results of the present study had clear implications for suicide prevention for the veterinary industry. We found increased SMRs for suicide among veterinarians and veterinary technicians or technologists, and the study yielded evidence that access to pentobarbital may account for the high rate of death by suicide among veterinarians, compared with that for the general population. As discussed at a recent AVMA roundtable meeting,38 establishing an accurate baseline suicide rate for US veterinary professionals will allow for follow-up comparisons to evaluate the effectiveness of future prevention activities.
Supplementary Material
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the CDC National Institute for Occupational Safety and Health or the National Center for Injury Prevention and Control.
Research in the present report relied on data from the NVDRS, a surveillance system administered by the CDC’s National Center for Injury Prevention and Control. The findings were partly based on the contributions of 18 funded states that collected data on violent deaths during the study period and the contributions of the states’ partners, including personnel from law enforcement, vital records, medical examiners or coroners, and crime laboratories.
The authors thank Gerald Hobbs, Department of Statistics, West Virginia University, for assistance with calculating the SMRs; Caitlin Williams, Department of Psychology, Auburn University, for assistance in coding the occupations of decedents; and Audrey Reichard, Division of Safety Research, National Institute for Occupational Safety and Health, CDC, for assistance with occupational employment statistics.
ABBREVIATIONS
- BLS
Bureau of Labor Statistics
- CI
Confidence interval
- GRA
Graduate research assistant
- NVDRS
National Violent Death Reporting System
- PMR
Proportionate mortality ratio
- SMR
Standardized mortality ratio
- SOC
Standard occupational codes
Footnotes
Microsoft Excel, version 16.16.2, Microsoft Corp, Redmond, Wash.
Occupational Employment Statistics [database online]. Washington, DC: BLS. Available at: www.bls.gov/oes/. Accessed Mar 6, 2019.
Veterinary assistants and laboratory animal caretakers. Data USA [database online]. Available at: datausa.io/profile/soc/319096/#demographics. Accessed Oct 16, 2018.
Greenhill LM, Association of American Veterinary Medical Colleges, Washington, DC: Personal communication, 2018.
Underlying cause of death, 1999–2014. CDC WONDER [database online]. Atlanta, Ga: CDC, National Center for Health Statistics, 2015. Available at: wonder.cdc.gov/ucd-icd10.html. Accessed Oct 11, 2016.
SAS PROC STDRATE, version 9.4, SAS Institute Inc, Cary, NC.
SPSS, version 24, IBM Corp, Armonk, NY.
Tomasi SE, Epidemic Intelligence Service Center for Surveillance, Epidemiology and Laboratory Services, CDC, Atlanta, Ga: Personal communication, 2018.
Web-based injury statistics query and reporting system (WISQARS) [database online]. Atlanta, Ga: CDC, 2005. Available at: www.cdc.gov/injury/wisqars. Accessed Dec 20, 2018.
Occupational employment statistics overview [database online]. Washington, DC: BLS. Available at: www.bls.gov/oes/oes_emp.htm. Accessed Mar 6, 2019.
References
- 1.Bartram DJ, Baldwin DS. Veterinary surgeons and suicide: a structured review of possible influences on increased risk. Vet Rec 2010;166:388–397. [DOI] [PubMed] [Google Scholar]
- 2.Blair A, Hayes HM Jr. Mortality patterns among US veterinarians, 1947–1977: an expanded study. Int J Epidemiol 1982;11:391–397. [DOI] [PubMed] [Google Scholar]
- 3.Hem E, Haldorsen T, Aasland OG, et al. Suicide rates according to education with a particular focus on physicians in Norway 1960–2000. Psychol Med 2005;35:873–880. [DOI] [PubMed] [Google Scholar]
- 4.Jones-Fairnie H, Ferroni P, Silburn S, et al. Suicide in Australian veterinarians. Aust Vet J 2008;86:114–116. [DOI] [PubMed] [Google Scholar]
- 5.Miller JM, Beaumont JJ. Suicide, cancer, and other causes of death among California veterinarians, 1960–1992. Am J Ind Med 1995;27:37–49. [DOI] [PubMed] [Google Scholar]
- 6.Milner AJ, Niven H, Page K, et al. Suicide in veterinarians and veterinary nurses in Australia: 2001–2012. Aust Vet J 2015;93:308–310. [DOI] [PubMed] [Google Scholar]
- 7.Platt B, Hawton K, Simkin S, et al. Suicidal behavior and psychosocial problems in veterinary surgeons: a systematic review. Soc Psychiatry Psychiatr Epidemiol 2012;47:223–240. [DOI] [PubMed] [Google Scholar]
- 8.Tomasi SE, Fechter-Leggett ED, Edwards NT, et al. Suicide among veterinarians in the United States from 1979 through 2015. J Am Vet Med Assoc 2019;254:104–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Association of American Veterinary Medical Colleges. Annual data report 2016–2017. Available at: www.aavmc.org/data/files/data/2017%20aavmc%20public%20data-%20final.pdf. Accessed Oct 16, 2018.
- 10.Drapeau CW, McIntosh JL, American Association of Suicidology. U.S.A. suicide 2016: official final data. Available at: www.suicidology.org/Portals/14/docs/Resources/FactSheets/2016/2016datapgsv1b.pdf?ver=2018-01-15-211057-387. Accessed Oct 16, 2018.
- 11.Nett RJ, Witte TK, Holzbauer SM, et al. Risk factors for suicide, attitudes toward mental illness, and practice-related stressors among US veterinarians. J Am Vet Med Assoc 2015;247:945–955. [DOI] [PubMed] [Google Scholar]
- 12.Milner A, Witt K, Maheen H, et al. Access to means of suicide, occupation and the risk of suicide: a national study over 12 years of coronial data. BMC Psychiatry 2017;17:125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gold KJ, Sen A, Schwenk TL. Details on suicide among US physicians: data from the National Violent Death Reporting System. Gen Hosp Psychiatry 2013;35:45–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fowler HN, Holzbauer SM, Smith KE, et al. Survey of occupational hazards in Minnesota veterinary practices in 2012. J Am Vet Med Assoc 2016;248:207–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stallones L, Doenges T, Dik BJ, et al. Occupation and suicide: Colorado, 2004–2006. Am J Ind Med 2013;56:1290–1295. [DOI] [PubMed] [Google Scholar]
- 16.Jack SP, Petrosky E, Lyons BH, et al. Surveillance for violent deaths—National Violent Death Reporting System, 27 states, 2015. MMWR Surveill Summ 2018;67:1–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stone DM, Simon TR, Fowler KA, et al. Vital signs: trends in state suicide rates—United States, 1999–2016 and circumstances contributing to suicide—27 states, 2015. MMWR Morb Mortal Wkly Rep 2018;67:617–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hempstead KA, Phillips JA. Rising suicide among adults aged 40–64 years: the role of job and financial circumstances. Am J Prev Med 2015;48:491–500. [DOI] [PubMed] [Google Scholar]
- 19.Elkins AD, Kearney M. Professional burnout among female veterinarians in the United States. J Am Vet Med Assoc 1992;200:604–608. [PubMed] [Google Scholar]
- 20.Skipper GE, Williams JB. Failure to acknowledge high suicide risk among veterinarians. J Vet Med Educ 2012;39:79–82. [DOI] [PubMed] [Google Scholar]
- 21.National Association of Veterinary Technicians in America. NAVTA survey. Available at: c.ymcdn.com/sites/www.navta.net/resource/resmgr/NAVTA_SeptOct12_Survey.pdf. Accessed Oct 16, 2018.
- 22.CDC National Center for Injury Prevention and Control. National Violent Death Reporting System 2017. Available at: www.cdc.gov/violenceprevention/nvdrs/index.html. Accessed Oct 16, 2018.
- 23.CDC National Center for Injury Prevention and Control. National Violent Death Reporting System (NVDRS): guidelines for data users. Atlanta: CDC National Center for Injury Prevention and Control, 2017. [Google Scholar]
- 24.CDC National Center for Injury Prevention and Control. National Violent Death Reporting System web coding manual, version 5.2. Available at: https://cdc.gov/violenceprevention/pdf/nvdrs/NVDRS-WebCodingManual.pdf. Accessed Jul 19, 2019.
- 25.World Health Organization. International statistical classification of diseases and related health problems. 10th revision. Geneva: World Health Organization, 2014. [Google Scholar]
- 26.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–174. [PubMed] [Google Scholar]
- 27.AVMA. Market research statistics. Available at: www.avma.org/KB/Resources/Statistics/Pages/default.aspx. Accessed Oct 16, 2018.
- 28.Association of American Medical Colleges. Table A-6: age of applicants to US medical schools at anticipated matriculation by sex and race/ethnicity, 2014–2015 through 2017–2018. Available at: www.aamc.org/download/321468/data/factstablea6.pdf. Accessed Oct 16, 2018.
- 29.Roberts SE, Jaremin B, Lloyd K. High-risk occupations for suicide. Psychol Med 2013;43:1231–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yip PS, Caine E, Yousuf S, et al. Means restriction for suicide prevention. Lancet 2012;379:2393–2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stone DM, Holland KM, Bartholow B, et al. Preventing suicide: a technical package of policies, programs, and practices. Atlanta: CDC National Center for Injury Prevention and Control, 2017. [Google Scholar]
- 32.Hawton K Restricting access to methods of suicide: rationale and evaluation of this approach to suicide prevention. Crisis 2007;28(suppl 1):4–9. [DOI] [PubMed] [Google Scholar]
- 33.Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm. Systematic review. Br J Psychiatry 2002;181:193–199. [DOI] [PubMed] [Google Scholar]
- 34.National Institute for Occupational Safety and Health. Hierarchy of controls. Available at: www.cdc.gov/niosh/topics/hierarchy/default.html. Accessed Oct 16, 2018.
- 35.Yip PS, Law CK, Fu KW, et al. Restricting the means of suicide by charcoal burning. Br J Psychiatry 2010;196:241–242. [DOI] [PubMed] [Google Scholar]
- 36.Chan KP, Yip PS, Au J, et al. Charcoal-burning suicide in post-transition Hong Kong. Br J Psychiatry 2005;186:67–73. [DOI] [PubMed] [Google Scholar]
- 37.CDC National Center for Injury Prevention and Control. CDC’s National Violent Death Reporting System now includes all 50 states. Available at: www.cdc.gov/media/releases/2018/p0905-national-violent-reporting-system.html. Accessed Dec 19, 2018.
- 38.Larkin M Veterinary wellness roundtable advances conversation. J Am Vet Med Assoc 2016;248:970–971. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.