Abstract
There are increased reports of pill-induced esophagitis in the past 2 decades, with almost 100 different substances identified as the cause for more than 700 cases, and the overall incidence is estimated to be 0.004% per year. Antibiotics are one of the major contributors for these cases, especially tetracycline and doxycycline; other major contributors are bisphosphonates, nonsteroidal anti-inflammatory drugs, and iron pills. Clindamycin is commonly prescribed by physicians, yet side effect in the form of esophagitis is uncommon and mostly documented in case report. It is possible that these cases are mostly unnoticed due to initial consideration of common and more serious problems. Thus, patients may be assumed to be having a severe episode of acid reflux, and it is not routinely reported or recognized. In this case series, we presented 8 patients with clindamycin-induced esophagitis. The initial presentation of all patients was odynophagia, which appeared within the first day of taking the antibiotic. All patients were subjected to endoscopic examination and ulcer was found in all cases, in the form of localized solitary or multiple ulcers with sharply defined borders. Patients were treated with proton pump inhibitor and sucralfate, and the symptoms subside within 1 week. Patient education regarding the proper way of ingesting drug seems to be the key factor in the prevention of pill-induced esophagitis. The prevention of esophagitis is even more important with antibiotics as adverse effect would decrease the patient compliance in completing the regimen and would ultimately increase antibiotic resistance.
Keywords: Clindamycin, drug-induced, esophagitis, odynophagia
Introduction
Pill-induced esophagitis is often reported in the past 2 decades, with almost 100 different agents identified as the cause for more than 700 cases. The overall incidence is estimated to be 0.004% per year. However, some drug groups seem to be more commonly reported (eg, nonsteroidal anti-inflammatory drug [NSAID] as high as 20%).1,2 Broad categories of medication types may cause esophageal injury. These include antibiotics, nelfinavir, zidovudine, NSAIDs, quinidine, vitamins, and miscellaneous isolated drugs from various categories.3 Antibiotics are by far the major contributor of these cases, especially tetracycline and doxycycline, and the other contributors are bisphosphonates, NSAIDs, and iron pills. Both tetracycline and doxycycline had been reported to cause esophageal injuries almost as much as all other drugs combined.
Advanced age is considered a risk factor for pill-induced esophagitis due to decrease in esophageal motility, polypharmacy, and insufficient water while ingesting the pill.4,5 Nevertheless, esophageal injury from other antibiotics is uncommon and mostly only documented in case reports. Clindamycin is worth mentioning that the incidence is still exceedingly low given that this drug is commonly used. With the advance of gastrointestinal endoscopy, it is expected to detect pill-induced esophagitis more frequently and to have better understanding of the course of the disease.6,7 To the best of our knowledge, the latest pill-induced esophagitis report is by Zhang et al8 in 2018 that reported esophagitis as a rare side effect of ascorbic acid. The purpose of this study was to explore the clinical and endoscopic features, especially, of clindamycin-induced esophageal injury.
Patients and Methods
Endoscopy records of esophageal injury due to clindamycin for the period from January to June 2018 were collected. Afterward, the records of patients were evaluated. We identified a total of 8 patients with clindamycin-induced esophageal injury. Of the 8 patients, 2 (patients 4 and 8) took no other medications other than clindamycin for acne, whereas the other patients were given clindamycin with paracetamol for pharyngitis. There was no history of side effects associated with paracetamol.
Results
A total of 8 patients with clindamycin-induced esophageal injury were identified: 6 of whom were men and the rest were women, with the mean age of 59 (range = 26-76) years. All patients had symptoms of odynophagia. Within the first day of taking clindamycin, 6 patients had odynophagia, one of the patients was in the third day and one patient was in the fifth day of taking clindamycin (Table 1). In 3 of the patients, there were comorbidities: patient 2 has diabetes with maintenance medication of glibenclamide 2.5 mg and metformin 500 mg once daily; patient 3 has coronary artery disease maintained with bisoprolol 2.5 mg once daily; and patient 5 has hypertension that was managed with telmisartan 40 mg once a day. No other complications were found.
Table 1.
Data of patients with clindamycin-induced esophagitis.
| Patient | Sex | Age | Symptom | Onset (day) | Endoscopic finding |
|---|---|---|---|---|---|
| 1 | M | 68 | Odynophagia | 1 | Mucosal erosions at mid esophagus |
| 2 | F | 61 | Odynophagia | 1 | Multiple erosions, mid-distal esophagus |
| 3 | M | 43 | Odynophagia | 3 | Multiple ulcers, mid-distal esophagus |
| 4 | F | 26 | Odynophagia | 1 | Solitary ulcer, mid esophagus |
| 5 | M | 53 | Odynophagia | 1 | Discrete ulcers from mid-distal esophagus |
| 6 | M | 76 | Odynophagia | 1 | Superficial linear ulcers at mid esophagus |
| 7 | M | 42 | Odynophagia | 5 | Multiple ulcers at mid esophagus |
| 8 | M | 31 | Odynophagia | 1 | Multiple ulcers at distal esophagus |
The endoscopic findings in the esophagus were multiple erosions in 2 patients and multiple ulcers in 6 patients. None of them had bleeding lesions. The esophageal lesions were located at distal in 1 patient (12.5%), mid in 4 patients (50.0%), and mid-distal in 3 patients (37.5%). All of the patients were treated as outpatient with proton pump inhibitor (PPI) and sucralfate. In 1-week follow-up, all patients reported that their symptoms subsided.
Discussion
Pill-induced esophageal injury could be underdiagnosed in clinical setting for several reasons: (1) clinicians often considered the more usual and more serious problems such as an acute coronary syndrome or pulmonary embolism that often presented with severe chest pain, sometimes pleuritic in nature, which may also be associated with pill-induced esophagitis; (2) patients may be assumed to have severe episode of acid reflux or gastroesophageal reflux disease, a more common entity for the symptoms compared with pill-induced esophageal injury; (3) some of the medications that can cause pill-induced esophagitis are over-the-counter medications or medication which may have been taken safely for years (eg, tetracycline) without esophageal injury, and therefore they were not considered as contributors to their symptoms; and (4) pill-induced esophageal injury is considered an uncommon entity because it is not routinely reported or even recognized. Because of these factors, pill-induced esophageal injury may not even be considered. This is a problem because failure in recognition of the causative agent might result in late discontinuation of the offending agent or failure to give the patient proper instruction to avoid future injury. It can lead to unnecessary and erroneous evaluation that is targeted for other conditions, and this will ultimately increase morbidity and the cost of health care.6
The first known drug-induced esophageal injury was reported by Pemberton in 1970 in a patient taking oral potassium.9 To date, more than 1000 cases involving more than 100 different drugs have been reported in the literature. The true incidence is unknown and estimated to be much higher because the diagnosis is often overlooked and the cases with mild clinical symptoms may be not reported or misdiagnosed with reflux esophagitis.7,10
There are different factors that play a role in pill-induced esophagitis. First, it is the harmful effect of the drug on the wall of esophagus, especially after extended contact, and second, patient or personal factors. The most common identifiable cause is personal factor. Dag et al10 stated the most common personal factors are insufficient water while ingesting the drug (41.6%) and recumbent position while taking the medication (22.9%). The harmful effect of the drug on the wall of esophagus may be through one of the 4 known mechanisms: (1) production of acidic solution that is caustic (eg, ferrous sulfate and ascorbic acid); (2) production of a caustic alkaline (eg, alendronate); (3) hyperosmolar solution in contact with esophageal mucosa (eg, potassium chloride); and (4) direct toxicity to the mucosa (eg, tetracycline). For a lot of medicines, the mechanism of injury does not categorize into any of these known.6
There are reports stating that one of the risk factors for pill-induced esophagitis is older age (⩾65 years), because they spend more time in recumbent position and use multiple medicines (polypharmacy), and a decrease in esophageal motility and mid-esophagus compression from enlarged heart have also shown to cause pill-induced esophagitis in elderly.4,11,12 Another study stated that esophageal transit time in elderly is significantly lower.13 Interestingly, in our case series, we identified esophagitis case in a patient as young as 26 years and in patients with an average age of 59 years. The reason behind it is because our case series solely investigated esophagitis induced by clindamycin, which is an antibiotic that is frequently prescribed and used in younger age group, as compared with other medications such as NSAID, antihypertensive drugs, and bisphosphonates that are more frequently prescribed to older population.7,11
In contrast with other reports in which pill-induced esophagitis predominantly occurs in women,7,10,12 only 2 of our patients are women (25%). This predominance is attributed to women receiving more medications than men, such as emepronium bromide that is used to relieve urinary frequency that is more common in women,14 potassium chloride pills are also more commonly prescribed for rheumatic heart disease that is more common in women, and bisphosphonates for osteoporosis.12 In our case series that specifically look into clindamycin-induced esophagitis, there is male predominance that may be caused by adherence to proper medication intake.
Chest pain and odynophagia are the hallmarks of pill esophagitis. In all of our patients, the first presentation was odynophagia, in which the symptom mostly developed in the first day after taking clindamycin. A case series by Dag et al10 reported that the most prominent clinical symptoms for drug-induced ulcer was odynophagia (79.1%), with the next common symptom being retrosternal/chest pain (62.5%), followed by dysphagia (47.9%). Other authors stated that the most common symptom for drug-induced esophageal injury was retrosternal/chest pain (71.8%), followed by odynophagia (38.5%).7 Pain may increase when ingesting further doses of the offending drug, food, or fluid. Symptoms are usually acute and can often be related to ingestion of an offending drug. These symptoms may develop within hours and up to 10 days after medication onset. Dysphagia, which is less common than chest pain or odynophagia, is reported in 20% to 40% of cases and usually indicates severe inflammatory stenosis or stricture formation.2,9,15
To help diagnose esophagitis, endoscopy or radiography can be used. Endoscopy is considered to be more important, although trials comparing the 2 have not been performed. Endoscopy allows for direct inspection, biopsy-taking, cytology-sampling and microbiological tests.6,9 We performed endoscopy in all of our patients, and our data comprise a total of 8 patients, 4 has ulcer at mid-distal esophagus, 3 at mid esophagus, and 1 at distal esophagus. These findings are consistent with some studies which found out that most clindamycin-induced esophagitis located at distal or middle part of esophagus. Rivera Vaquerizo et al9 reported a case of clindamycin-induced esophageal ulcer which revealed the presence of 2 superficial ulcers at 30 cm and another 2 deep, friable-upon-friction ulcers at 28 cm. Sutton and Gosnold16 also reported esophageal ulceration after oral clindamycin (Dalacin C®) and found 2 necrotic ulcers with surrounding hyperemia on the anterior and posterior esophageal walls, 25 cm from the incisor teeth.
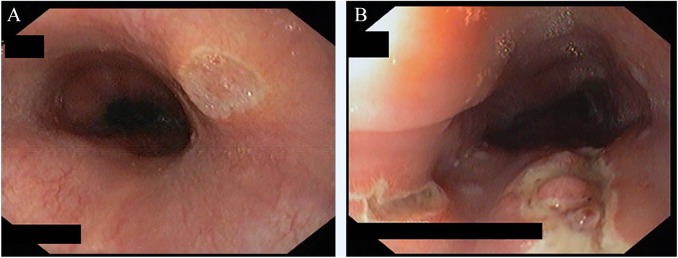
The ulcer that we found during endoscopy was mostly in the form of localized solitary or multiple ulcers with sharply defined borders (Figure 1). The mechanism by which clindamycin causes injury is that it has low acid pH when dissolved in solution. This property might cause injury to the esophageal wall, most commonly localized discrete ulcer. A study by Kim et al7 found that kissing ulcer (ulcers facing each other) is found in 43.6% of the cases. However, kissing ulcer was also found in cases other than pill-induced esophagitis.17 Therefore, kissing ulcer alone cannot confirm pill-induced esophagitis.
Figure 1.
Endoscopic finding of patients with clindamycin-induced esophagitis: (A) Localized solitary ulcer with sharply defined at mid esophagus. (B) Multiple ulcers at mid to distal esophagus.
No specific treatments have been shown to be beneficial in altering the disease progression of pill-induced injury. Management of these patients is aimed at controlling the symptoms, preventing superimposed injury from acid reflux, maintaining adequate hydration or water intake, and removing the offending drug.6 Symptoms usually subside within a week from the cessation of the offending drug, and it is accompanied by healing of the lesions, even without specific therapy.15 Our patients were treated with PPI and sucralfate and the symptoms subsided in a week. Thus, we did not perform follow-up endoscopy in this case series as the aim of the management is to control the symptoms. Furthermore, unnecessary endoscopy would result in increased morbidity and cost for the patient. If there is no clinical improvement in 8 days control, endoscopy should be considered.10
Proper administration of potentially injurious medications will help avoid occurrence of esophageal injury. When evaluating risks factors of pill-induced esophagitis, drugs per se and the patient factors should be evaluated separately. The following recommendations are made as prevention: (1) medications should be swallowed with at least 8 ounces of a clear liquid; (2) patients should remain upright for at least 30 min following ingestion of the medication; (3) in patients with potential underlying increased risk for pill-induced injury (eg, inability to follow the previous instructions, poor esophageal motility, anatomic compromise of the esophageal lumen), one should search for alternative safer medications or carefully weigh the risks and benefits of this medication against the disease for which this medication is necessary.6,18 For patients in decubitus position, the medicine should be taken in a sitting position; if sitting is not possible, reclining position of 30° can help by the means of gravity force.19
Conclusions
Clindamycin is a widely used antibiotic; however, clindamycin-induced esophagitis is uncommon or may be not recognized. Proper patient education before prescribing the drug is important, and taking enough water, ingesting the drug in upright position, early diagnosis of adverse drug reaction, and a high level of suspicion by the clinician are the necessary preventive measures. The symptoms and endoscopic finding of clindamycin-induced esophagitis are similar to that of other pill-induced esophagitis. The treatment by cessation of the offending antibiotic and administration of PPI and sucralfate is very effective.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: All authors contributed equally in the write-up and editing of the article.
Disclaimer: Abstract of this article has been published in American Journal of Gastroenterology on October 2018;113: S1539-S40. The full article has not been submitted/published elsewhere.
Informed Consent: The patients reported in these case series were informed of this publication and consent was obtained.
ORCID iD: Muhammad Begawan Bestari  https://orcid.org/0000-0002-6911-8213
https://orcid.org/0000-0002-6911-8213
References
- 1. Bestari M, Agustanti N, Abdurachman S. Clindamycin-induced esophageal injury: is it an under-diagnosed case? Am J Gastroenterol. 2018;113:S1539-S1540. [Google Scholar]
- 2. Dellon E, Shaheen N. Miscellaneous diseases of the esophagus: foreign bodies, physical injury, and systemic and dermatological diseases. In: Yamada T, ed. Textbook of Gastroenterology. 5th ed. Oxford, UK: Blackwell Publishing, Ltd.; 2009:871-888. [Google Scholar]
- 3. Amjad W, Qureshi W, Farooq A, et al. Gastrointestinal side effects of antiarrhythmic medications: a review of current literature. Cureus. 2017;9:e1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dumic I, Nordin T, Jecmenica M, Stojkovic Lalosevic M, Milosavljevic T, Milovanovic T. Gastrointestinal tract disorders in older age. Can J Gastroenterol Hepatol. 2019;2019:6757524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kikendall JW. Pill-induced esophagitis. Gastroenterol Hepatol (N Y). 2007;3: 275-276. [PMC free article] [PubMed] [Google Scholar]
- 6. Katzka D. Esophageal disorders caused by medications, trauma, and infection. In: Feldman M, Friedman L, Brandt L, eds. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease. 9th ed. Amsterdam, The Netherlands: Elsevier Inc; 2010:735-743. [Google Scholar]
- 7. Kim S, Jeong J, Kim J, et al. Clinical and endoscopic characteristics of drug-induced esophagitis. World J Gastroenterol. 2014;20:10994-10999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhang Y, Tong Y, Wang W, Xu L. Chest pain from pill-induced esophagitis: a rare side effect of ascorbic acid. SAGE Open Med Case Rep. 2018;6: 2050313X18775004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rivera Vaquerizo PA, Santisteban Lopez Y, Blasco Colmenarejo M, Vicente Gutierrez M, Garcia Garcia V, Perez-Flores R. Clindamycin-induced esophageal ulcer. Rev Esp Enferm Dig. 2004;96:143-145. [DOI] [PubMed] [Google Scholar]
- 10. Dag MS, Ozturk ZA, Akin I, Tutar E, Cikman O, Gulsen MT. Drug-induced esophageal ulcers: case series and the review of the literature. Turk J Gastroenterol. 2014;25:180-184. [DOI] [PubMed] [Google Scholar]
- 11. Boyce HW., Jr. Drug-induced esophageal damage: diseases of medical progress. Gastrointest Endosc. 1998;47:547-550. [DOI] [PubMed] [Google Scholar]
- 12. Zografos GN, Georgiadou D, Thomas D, Kaltsas G, Digalakis M. Drug-induced esophagitis. Dis Esophagus. 2009;22:633-637. [DOI] [PubMed] [Google Scholar]
- 13. Hey H, Jorgensen F, Sorensen K, Hasselbalch H, Wamberg T. Oesophageal transit of six commonly used tablets and capsules. Br Med J (Clin Res Ed). 1982;285:1717-1719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kikendall JW, Friedman AC, Oyewole MA, Fleischer D, Johnson LF. Pill-induced esophageal injury. Case reports and review of the medical literature. Dig Dis Sci. 1983;28:174-182. [DOI] [PubMed] [Google Scholar]
- 15. Bytzer P. Medication-induced esophageal disease. In: Talley N, Kenneth R, eds. Practical Gastroenterology and Hepatology: Esophagus and Stomach. Oxford, UK: Blackwell Publishing, Ltd.; 2010:287-290. [Google Scholar]
- 16. Sutton D, Gosnold J. Oesophageal ulceration due to clindamycin. Br Med J. 1977;1:1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kim GB, Jeong JJ, Park S, et al. A large symmetrical esophageal ulcer caused by thermal and compressive injury from a solid foodstuff known as “Song-Pyen.” Korean J Med. 2012;82:589-593. [Google Scholar]
- 18. Buyukberber M, Demirci F, Savas MC, Kis C, Gulsen MT, Koruk M. Pill esophagitis caused by telithromycin: a case report. Turk J Gastroenterol. 2006;17: 113-115. [PubMed] [Google Scholar]
- 19. Kagaya H, Inamoto Y, Okada S, Saitoh E. Body positions and functional training to reduce aspiration in patients with dysphagia. JMAJ. 2011;54:35-38. [Google Scholar]