Abstract
Objective:
Femoral nerve blocks (FNBs) for fragility hip fractures have benefits in improving pain relief and early mobilization while decreasing opioid use and rates of pneumonia. However, no study has looked at 1-year mortality outcomes for this intervention. This study aims to provide insight into 1-year outcomes.
Methods:
A single-site retrospective case–control study from 2007 to 2016 in primary fragility hip fractures compared 665 patients who received an emergency department FNB to 326 patients who did not receive an FNB. The primary outcome was 1-year mortality. Secondary outcomes included mortality, mobility, and residence at discharge, 6 months, and 1-year intervals.
Results:
There were no significant differences in preoperative characteristics. Although there was no statistically significant difference in 1-year mortality, patients who did not receive an FNB were more likely to be nonambulant at 1 year (odds ratio 1.71, 95% confidence interval, 1.14-2.57, P = .005). There were no other significant differences in mobility, residence, or mortality.
Conclusion:
There was no statistically significant difference in 1-year mortality, although individuals who did not receive an FNB were more likely to be nonambulant at 1 year.
Keywords: emergency department, hip fracture, mobility, residency, mortality, 1 year, outcomes, femoral nerve blocks
Introduction
Fragility hip fractures are catastrophic injuries for frail Australians. One-fifth of those who sustain this injury die within 1 year, one-half of them will become permanently disabled, and one-tenth of them will require new long-term care in a skilled nursing facility.1 Multimodal analgesia with femoral nerve blocks (FNBs) are included in Australian guidelines to decrease pain, opioid use, rates of pneumonia, and aid in earlier mobilization.2,3 Although FNB are suggested as a promising intervention to prevent mortality there is no literature to our knowledge on 1-year outcomes.4 Since FNB have been shown to decrease morbidity we hypothesize that FNB given in the emergency department will decrease 1-year mortality.
Methods
Ethics
Low negligible risk ethics exemption was provided by Metro South Human Research Ethics Committee in Brisbane, Australia, to undertake a retrospective population-matched case–control study.
Patient Population
This study was conducted at the Princess Alexandra Hospital in Brisbane, Australia, and complies with the Strengthening The Reporting of Observational studies in Epidemiology guidelines for case–control studies.5 Princess Alexandra Hospital introduced an orthogeriatric model of care for the management of patients presenting with hip fractures in 2006.
Inclusion criteria for this study were individuals who had a primary fragility hip fracture. Exclusion criteria were any patient who was younger than 50 years or had time to surgery greater than 48 hours.
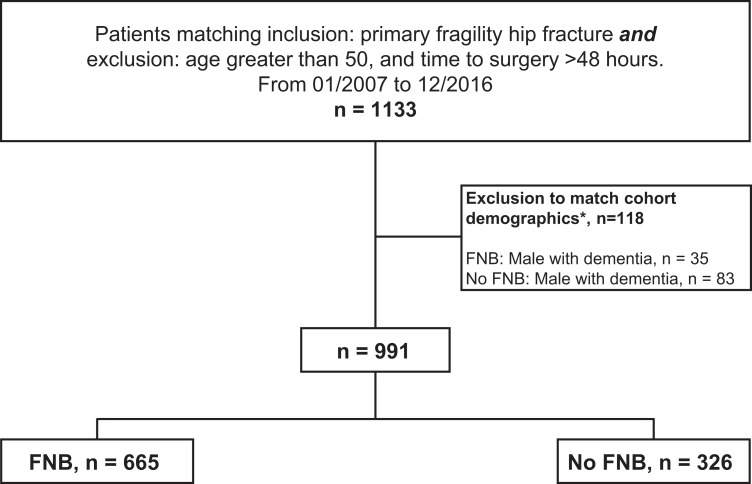
In all, 1133 patients were identified who matched the inclusion and exclusion criteria. Descriptive and frequency analysis was conducted to describe participant characteristics. Exclusion of 118 male patients with dementia was undertaken to match cohort demographics with the Australia New Zealand Hip Fracture Registry.2 Thirty-five males with dementia were excluded from the FNB group, and 83 males with dementia were excluded from the no FNB group. In all, 991 patients were then included, with 665 in the FNB group and 326 in the no FNB group (Figure 1).
Figure 1.
Study flowchart for patients who received an emergency department femoral nerve block versus patients who did not in fragility hip fractures. * Exclusion of these patients-matched cohort demographic proportions from the Australia New Zealand Hip Fracture Registry 2018.
Data Collection
Data were prospectively collected by clinical nurse consultants from 2007 to 2016 and augmented with retrospective chart reviews. The data collected included the use of an FNB in the emergency department as well as mortality, mobility, and residence data at intervals up to 1 year (on admission, at discharge, at 6 months, and at 1 year). Mobility data were recorded as independent, requiring an aid, or nonambulant. Residence data were recorded as private home, rehabilitation unit, or care facility.
Preoperative patient demographics (age, gender, American Society of Anesthesiologists [ASA] score, preexisting dementia), surgical considerations (time to surgery, surgeon experience), and postoperative complications (urinary tract infections, deep vein thrombosis, pulmonary embolisms, pneumonia, cerebral vascular accidents, myocardial infarcts, and resuscitation codes) were recorded.
Intervention
The FNB intervention was performed by emergency staff physicians and resident physicians using 20 mL of 0.5% bupivacaine inserted adjacent to the femoral nerve. Specific technique for performing the block was not reliably recorded in patient charts. Interventions were based on clinician availability and departmental constraints.
Outcome Measures
The primary outcome was 1-year mortality. Secondary outcomes were in-hospital and 6-month mortality, as well as residency and mobility at discharge, 6 months, and 1-year intervals.
Sample Size Estimation
No published data on 1-year mortality in patients who received an FNB was available to calculate a sample size. Sample size estimates for 6-month mortality with nerve blocks ranged from 443 to 3228 patients.3,6 G*Power 3.1 stats program7 was used to calculate our sample size with a range of effect sizes (0.1-0.25). Given an α of .01 and a power of 0.95, the sample size ranged from 256 to 1580 patients. Our convenience sample of 991 was then collected.
Statistical Analysis
Where data were missing, multiple imputations for chained equivalence (MICE) was used in consultation with a biostatistician. Statistical analysis of the data was undertaken using Statistical Package for Social Sciences version 22 software (IBM, Chicago, Illinois). All ordinal and continuous values were assessed using Mann-Whitney U median testing, and nonordinal values were evaluated using χ2 with odds ratio (OR) calculations for statistically significant variables. A P value less than .01 was considered statistically significant.
Results
Six-month and 1-year follow-up was recorded in 87% and 75% of individuals, respectively. The remaining data were imputed using MICE with biostatistical support.
There was no statistical difference in preoperative characteristics (Table 1) or 1-year mortality (Table 2). Patients who did not receive an FNB were more likely to be nonambulant at 1 year (OR 1.71, 95% confidence interval, 1.14-2.57; Table 3). There was no other statistically significant difference in mobility, residence, postoperative complications, and mortality outcomes (Tables 2 –4, Appendix A). Additional subgroup analysis between FNB and no FNB for age, ASA, time to surgery, type of fracture, and type of anesthetic showed no significant difference in mortality outcomes at 1 year (data not shown).
Table 1.
Demographics of Patients Who Received an Emergency Femoral Nerve Block Versus Patients Who Did Not in Fragility Hip Fractures From 2007 to 2016.a
| Demographics | FNB, n = 665 | No FNB, n = 326 | P |
|---|---|---|---|
| Age, median (IQR) | 83 (76-88) | 82 (74-87) | .02 |
| Female, n (%) | 487 (73) | 243 (75) | .19 |
| ASA, median (IQR) | 3 (3-3) | 3 (3-3) | .36 |
| Preexisting dementia, n (%) | 205 (31) | 103 (32) | .06 |
| Time to surgery in hours, median (IQR) | 29 (21-39) | 32 (20-30) | .23 |
| Surgeon experience staff versus trainee, n (% staff) | 255 (38) | 111 (34) | .19 |
Abbreviations: ASA, American Society of Anesthesiologists; FNB, femoral nerve block; IQR, interquartile range.
a P < .01 is considered significant.
Table 2.
Mortality Outcomes From Patients Who Received an Emergency Department Femoral Nerve Block Versus Patients Who Did Not in Fragility Hip Fractures From 2007 to 2016.a
| Mortality, n (%) | FNB, n = 665 | No FNB, n = 326 | P |
|---|---|---|---|
| In-hospital | 39 (6) | 17 (5) | .57 |
| 6 months | 106 (16) | 52 (16) | .99 |
| 1 year | 155 (23) | 72 (22) | .49 |
Abbreviation: FNB, femoral nerve block.
a P < .01 is considered significant.
Table 3.
Mobility Outcomes From Patients Who Received an Emergency Department Femoral Nerve Block Versus Patients Who Did Not in Fragility Hip Fractures From 2007 to 2016.a
| FNB, n = 665 | No FNB, n = 326 | P | Odds Ratio | |
|---|---|---|---|---|
| Preadmission mobility, n (%) | ||||
| Independent | 335 (50) | 169 (52) | .66 | – |
| Walking aid | 314 (47) | 150 (46) | .72 | – |
| Nonambulant | 10 (2) | 7 (2) | .46 | – |
| Discharge mobility, n (%) | ||||
| Independent | 2 (0) | 2 (1) | .47 | – |
| Walking aid | 600 (90) | 286 (88) | .23 | – |
| Nonambulant | 32 (5) | 22 (7) | .21 | – |
| 6 months, n (%) | ||||
| Independent | 101 (15) | 50 (15) | .94 | – |
| Walking aid | 400 (60) | 181 (56) | .16 | – |
| Nonambulant | 58 (9) | 43 (13) | .03 | – |
| 1 year, n (%) | ||||
| Independent | 140 (21) | 63 (19) | .52 | – |
| Walking aid | 313 (47) | 143 (44) | .34 | – |
| Nonambulant | 59 (9) | 48 (15) | .005 | 1.71 (1.14-2.59) |
Abbreviation: FNB, femoral nerve block.
a P < .01 is considered significant.
Table 4.
Residence Outcomes From Patients Who Received an Emergency Department Femoral Nerve Block Versus Patients Who Did Not in Fragility Hip Fractures From 2007 to 2016.a
| FNB, n = 665 | No FNB, n = 326 | P | |
|---|---|---|---|
| Preadmission residence, n (%) | |||
| Private | 470 (71) | 229 (70) | .89 |
| Care facility | 192 (29) | 91 (28) | .75 |
| Discharge location, n (%) | |||
| Private residence | 79 (12) | 55 (17) | .03 |
| Rehabilitation | 397 (60) | 193 (59) | .88 |
| Care facility | 159 (24) | 68 (21) | .28 |
| 6 months, n (%) | |||
| Private | 354 (53) | 163 (50) | .34 |
| Care facility | 197 (30) | 95 (29) | .88 |
| 1 year, n (%) | |||
| Private | 325 (49) | 156 (48) | .76 |
| Care facility | 179 (27) | 87 (27) | .94 |
Abbreviation: FNB, femoral nerve block.
a P < .01 is considered significant.
Discussion
To the best of our knowledge, this is the first study comparing FNB administered in the emergency department and 1-year mortality in patients with fragility hip fractures. Femoral nerve block may not reduce 1-year mortality but may prevent permanent immobilization. We postulate that FNB does this by decreasing pain, opioid use, and subsequent delirium. Patients who are less delirious then mobilize earlier, resulting in more sustained long-term mobility.
When resources and expertise are available, nerve blocks targeting the femoral nerve should be included in hip fracture management. These interventions can easily be performed in the emergency department and be repeated every 12 hours to ensure prolonged effects where possible.8 Although femoral blocks in hip fractures should be the minimum, new alternatives may include fascia iliaca catheters, transversus abdominis plane quadratus lumborum blocks, and pericapsular nerve group blocks.9-11 These peripheral anesthesia methods are exciting options that may offer better analgesia or broader coverage of the obturator nerve along with the femoral and lateral cutaneous nerves. They remain an open area for future research.
This case–control study accounted for known mortality risk factors, which include time to surgery, surgeon experience, age, gender, ASA classification, and premorbid mobility.4 The limitations include missing data regarding nerve block techniques and intervention selection. Prospective randomized trials in future studies may help address these limitations.
Conclusion
In summary, this study was unable to show a difference in 1-year mortality; however, it suggested an association between emergency department FNB and increased mobility at 1 year. Methodology should be considered in interpreting this study.
Acknowledgments
The authors thank Charles Yates, Emma List, Catherine Harmon, Braden Cuppit, Annabella Jacques, Jacqui Chui, David Yoon, Dong Yu, Dougal Middleton, Dr Kalonji Tony Nzembela, Dr An Xuan Ang, Dr Adrian Wan, Dr William Song, Dr Adrianne Corbette, Naomi O’Rourke, the staff at the PAH Medical Records, Dr Luke Visscher, Dr Vinay Gangathimmaiah, and Dr Chris Jeffrey.
Appendix A
Postoperative outcomes from patients who received an emergency department femoral nerve block versus patients who did not in fragility hip fractures from 2007 to 2016. P < .01 is considered significant.
| FNB, n = 665 | No FNB, n = 326 | P | |
|---|---|---|---|
| Postoperative complications, n (%) | |||
| Urinary tract infection | 200 (30) | 106 (33) | .61 |
| Pneumonia | 63 (9) | 28 (9) | .21 |
| Deep vein thrombosis | 8 (1) | 7 (2) | .25 |
| Pulmonary embolism | 6 (1) | 3 (1) | .98 |
| Stroke | 8 (1) | 7 (2) | .25 |
| Myocardial infarct | 16 (2) | 2 (1) | .05 |
| Resuscitation code | 16 (2) | 7 (2) | .06 |
Authors’ Note: All authors contributions keep with the ICJME authorship with substantial contributions to design/acquisition or analysis of data, drafting/revising, final approval of published versions, and agreement to be accountable for integrity and accuracy of the work.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding was provided by departmental resources for nurse lead database collections.
ORCID iDs: Michael Darren Polischuk  https://orcid.org/0000-0002-9958-2893
https://orcid.org/0000-0002-9958-2893
Nrusheel Kattar  https://orcid.org/0000-0002-3884-4597
https://orcid.org/0000-0002-3884-4597
Sajan Sriselvakumar  https://orcid.org/0000-0001-9117-867X
https://orcid.org/0000-0001-9117-867X
References
- 1. ANZHFR Bi-National Annual Report for Hip Fracture Care 2017. Australian and New Zealand Hip Fracture Registry 2017; July 2017. [Google Scholar]
- 2. Australian and New Zealand Hip Fracture Registry (ANZHFR) Steering Group. Australian and New Zealand Guideline for Hip Fracture Care: Improving Outcomes in Hip Fracture Management of Adults. Sydney: Australian and New Zealand Hip Fracture Registry Steering Group; 2014. www.anzhfr.org. [Google Scholar]
- 3. Guay J, Parker MJ, Griffiths R, Kopp S. Peripheral nerve blocks for hip fractures. Cochrane Database Syst Rev. 2017;(5):CD001159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Parker MJ. Reducing morbidity and mortality in the hip fracture patient group. Orthopaed Trauma. 2016;30(2):153–158. [Google Scholar]
- 5. Von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening The Reporting of OBservational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–1457. PMID: 18064739. [DOI] [PubMed] [Google Scholar]
- 6. Lees D, Harrison WD, Ankers T, et al. Fascia iliaca compartment block for hip fractures: experience of integrating a new protocol across two hospital sites. Eur J Emerg Med. 2016;23(1):12–18. [DOI] [PubMed] [Google Scholar]
- 7. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Meth. 2007;39:175–219. [DOI] [PubMed] [Google Scholar]
- 8. Agency for Clinical Innovation Pain Management Network Clinical Guideline. Fascia Iliaca Block: A Method of Preoperative Pain Management in Older People With Acute Hip Fractures; 2015. Chatswood, Australia: Version 1. [Google Scholar]
- 9. Polischuk M. Neck of Femur Fracture Pain Management With Ultrasound-Guided Single Bolus versus repeated bolus Fascia Iliaca CatheterS in the Emergency Department: A Double-Blind, Randomized Controlled Trial. (NOF-FICSED); Nov 11, 2018. Australian New Zealand Clinical Trials Registry: Sydney (NSW): NHMRC Clinical Trials Centre, University of Sydney (Australia); 2019. ACTRN12618001884291. [Google Scholar]
- 10. Parras T, Blanco R. Randomised trial comparing the transversus abdominis plane block posterior approach or quadratus lumborum block type I with femoral block for postoperative analgesia in femoral neck fracture, both ultrasound-guided. Rev Esp Anestesiol Reanim. 2016;63(3):141–148. [DOI] [PubMed] [Google Scholar]
- 11. Girón-Arango L, Peng PWH, Chin KJ, Brull R, Perlas A. Pericapsular Nerve Group (PENG) block for hip fracture. Reg Anesth Pain Med. 2018;43(8):859–863. [DOI] [PubMed] [Google Scholar]