Abstract
Background:
Recently, oral and maxillofacial surgeons are favoring three-dimensional (3D) miniplates to treat mandibular fractures.
Aims:
The aim of the study is to evaluate the efficacy of 3D-miniplates over standard miniplates in the management of mandibular parasymphysis fracture.
Materials and Methods:
Forty patients with mandibular parasymphysis fractures were divided into two groups of 20 patients each. Group I patients underwent osteosynthesis of mandibular fracture by noncompression, unicortical, and stainless steel 3D miniplates, and Group II patients underwent osteosynthesis by noncompression, unicortical, and stainless steel Champy's miniplates. All the patients were followed up 6 months’ postoperatively, evaluating occlusion, mobility of fracture segment, pain, wound dehiscence, neurological deficit, and infection.
Statistical Analysis Used:
The data were analyzed by SPSS for windows (version 17) statistical package (SPSS Inc., Chicago, IL, USA). Chi-square test was carried out to determine the statistical difference between the groups.
Results:
Mobility of the fractured site was evaluated postoperatively after 2 weeks, and it was found that mobility was absent in all the cases of Group I and 36 (80%) cases in Group II. There was significant difference in the mean visual analog scale scores among the Group I and II when compared from preoperative to 4-week follow-up. In Group II, two patients showed wound dehiscence. After 2 weeks, infection was seen in two patients of Group II.
Conclusion:
3D plates in mandibular parasymphysis fractures give dimensional stability and carry low morbidity and infection rates.
Keywords: Champy's miniplate, infection, mandibular fracture, osteosynthesis, three-dimensional miniplate
INTRODUCTION
The presence of teeth makes jaw fractures different from other bones. The major goal of treating jaw fractures is to stabilize the fractured segments, thus attaining functional occlusion. The introduction of recent biomaterials has modified surgical approach in the direction of bone plating and restoring lost function as early as possible.[1]
The most common etiology of maxillofacial fractures is road traffic accidents (RTA), with mandibular fractures being the second most commonly fractures after nasal fractures.[1,2,3]
With the advent of inert metals and broad-spectrum antibiotics, there was a shift in the treatment options toward open method using bone plates rather than by old closed methods of fixation. Chee NS et al. (2014) used self-compressing plate to stabilize the fractured segments of edentulous mandible.[2] Uhthoff HK et al. (2006) introduced dynamic compression plate in the field of maxillofacial trauma.[3]
Usually, mandibular fractures are treated by two methods of surgical treatment, rigid or semi-rigid fixation, with different concepts of mandibular osteosynthesis. The basic principles of the Association for the study of Osteosynthesis/Association for the Study of Internal Fixation are used in rigid fixation. Here, forces of functional loading are counterbalanced by thick solid plates fixed by bicortical screws.[4]
Champy's method of semi-rigid fixation uses straightforwardly adaptable monocortical miniplate along with an “ideal osteosynthesis line.” The developing forces are neutralized by masticatory forces developing forces.[5]
Goyal M et al. (2011) used small miniplates through Transbuccal approach for mandibular fixation.[6] Later, Sadhwani BS et al. (2013) finally developed the technique with practicality. According to them, the site of bone plate fixation must offer the most stable way of fixation corresponding to the line of tension at the base of alveolar process. Usually, two plates are used if the fractures are anterior to mental foramen and one plate for fractures posterior to foramen.[5,6]
Recent studies have shown advances in plating techniques, and thus giving more options to the maxillofacial surgeons. Prasad R et al. (2013) introduced the concept of three-dimensional (3D) miniplates or strut plates with the basic principle of quadrangle as a geometrically stable configuration for support.[7] According to them, the fracture fragments are held rigidly by plates with minimum thickness which resist the 3D forces, i.e., shearing, torsional, and bending forces. The fundamental shape of 3D plate is 2 × 2 hole plate with square or horizontal segments, fixed to mandible according to Champy's principles, secured with monocortical screws.[7,8]
We carried out this study to assess the effectiveness of 3D fixation over miniplate fixation for treating mandibular parasymphysis fractures.
MATERIALS AND METHODS
Source of data
This study was carried out in the Department of oral and maxillofacial surgery.
Method of collection of sample
Forty patients with mandibular parasymphysis fractures who reported to the department from January 2012 to August 2013 were included in the study. After obtaining consent, clinical examination and radiographs were taken [Figures 1 and 2]. The patients were divided into two groups, which included 20 patients each. Group I patients underwent osteosynthesis of the mandibular fracture by noncompression, unicortical, and stainless steel 3D miniplates, and Group II patients underwent osteosynthesis by noncompression, unicortical, and stainless steel Champy's miniplates. The patients were followed up 6 months’ postoperatively, evaluating occlusion, mobility of fracture segment, pain, wound dehiscence, neurological deficit, and infection.
Figure 1.
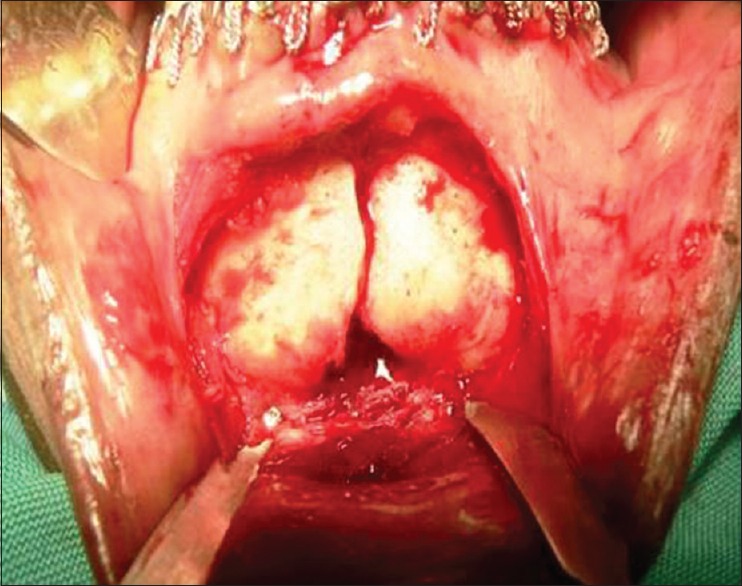
Fracture site
Figure 2.

Preoperative orthopantomogram
Inclusion criteria
Patients with parasymphysis fracture of the mandible with or without associated fractures
Patients reporting to the department within 7 days of trauma.
Exclusion criteria
Patients not willing to return for follow-up
Medically compromised patients
Patients with gross infection at the site of fracture
Patients with associated bone pathology
Patients with comminuted fracture.
Investigations
Surgical profile including hematological investigations, viral screening, serum creatinine, blood urea levels, random blood sugar level, electrocardiogram, and chest X-ray were done preoperatively.
Three-dimensional miniplates
3D plates were formed by joining two miniplates with interconnecting vertical crossbars, to minimize bending. An increase in stability was achieved by the geometric shape of the quadrangular plate and not by its thickness or length (thickness 1 mm, length 20 mm, and width 12 mm). The main forces of concern to a surgeon are bending, vertical displacement, and shearing. However, in the 3D miniplate, as the entire plate acts as a single unit, and due to its shape, the vertical displacement and shearing of bone are reduced to minimal, thereby holding the bone fragment in three dimensions. Four holes 3D-stainless steel miniplates were used in this study, with 2 mm × 8 mm screws.
Miniplates
A two holes (superiorly) and four holes (inferiorly) with gap, stainless steel miniplates were used in this study, with 2 mm × 8 mm monocortical screws with round head, with a drill bit of 1.5 mm diameter was used.
The patients were divided into two groups
Group I: Twenty patients who underwent osteosynthesis of the mandibular fracture by noncompression, unicortical, and stainless steel 3D miniplates
Group II: Twenty patients who underwent osteosynthesis of the mandibular fracture by noncompression, unicortical, and stainless steel Champy's miniplates.
Operative technique
Erich's arch bars were placed preoperatively in all the patients in both the groups, procedures were carried out either under general anesthesia or local anesthesia with diazepam 5 mg/ml and local anesthetic injection of 2% lignocaine with adrenaline 1:80,000 for hemostasis. A standard transoral surgical technique was followed in both the groups to expose and reduce the fractures. A degloving intraoral incision was made on oral mucosa 5 mm below the level of attached gingiva. It was extended parallel to the alveolar process and was slightly superiorly placed near the premolar region to prevent injury to the mental nerve. The incision was made so as to provide adequate exposure of the fracture site. Mucoperiosteal flap was raised. Mental nerve was isolated through blunt dissection in the vicinity of mental foramina. Fracture site was exposed, and curetted with the help of curette to remove granulation tissue and blood clots. The fracture site was irrigated with 5% povidone-iodine followed by normal saline. The fragments were reduced manually in correct anatomical position, and radiographs were taken [Figures 3 and 4]. Occlusion was checked and temporary intermaxillary fixation done.
Figure 3.
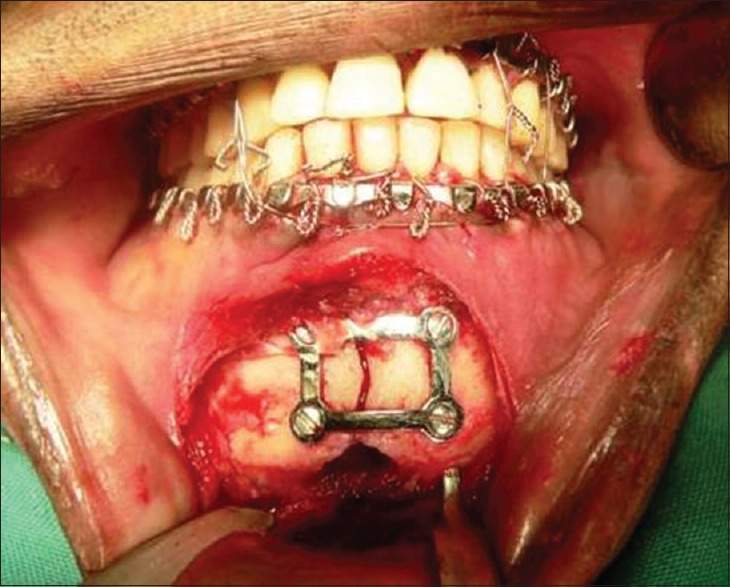
Plate fixation
Figure 4.

Postoperative orthopantomogram
Adaptation and fixation of plate
Group I: The four holes 2-mm stainless steel 3D plates were adapted across the fracture line in such a fashion that, the horizontal crossbars were positioned perpendicular to the fracture line, and vertical struts were placed parallel to fracture line. In cases with oblique fracture, the plates were placed parallel to the lower border of mandible. In parasymphyseal fractures, the upper crossbar was placed in the subapical position; the screw holes were made with 1.5-mm stainless steel drill bit, perpendicular to the surface of bone under copious saline irrigation. Plates were fixed with 2 mm × 8 mm stainless steel screws
Group II: Following reduction, 2.0-mm stainless steel miniplates were applied along the osteosynthesis line as described by Champy. In parasymphyseal fractures, two plates were placed to overcome the torsional forces. In the parasymphysis fracture site, both the plates were positioned lower than the mental foramina. The lower plate was placed first, followed by the plate above, to prevent development of diathesis at the lower border due to action of masticatory muscles. During drilling, the adapted plate was held firmly against the bone with the plate holding forceps. The screw holes were then performed by 1.5-mm stainless steel drill bit perpendicular to the surface of bone under copious saline irrigation. Immobilization of the fracture fragments done with 2.0 mm four holes with gap plates and 2 mm × 8 mm stainless steel screws.
Irrigation and closure
After plate fixation, surgical site was copiously irrigated with 5% povidone-iodine and followed by normal saline. Temporary intermaxillary fixation was released to check the passive occlusion. Hemostasis was achieved, and suturing was done in layers with 3–0. Pressure dressing was applied, and patients were prescribed antibiotics and analgesics for 5 days. Patients were advised to maintain the oral hygiene and to perform oral rinses with betadine solution. Patients were prescribed soft diet for the 1st week. The patients was followed up on weekly interval for a month and then at 2 months, 3 months, and 6 months [Figure 5].
Figure 5.

Occlusion postoperatively
RESULTS AND OBSERVATIONS
The most common etiology was (RTA-24 cases), assault and fall were the etiology in six cases each, and four had occupational trauma [Table 1].
Table 1.
Distribution of cases based on etiology
| Etiology | Number of cases (%) |
|---|---|
| RTA | 24 (60) |
| Assault | 6 (15) |
| Fall | 6 (15) |
| Occupational trauma | 4 (10) |
RTA: Road traffic accidents
The age group of the patients ranged from 20 to 65 years of age, the mean age of the patient being 30.3 years. Maximum number of cases were noted between 20–40 years, as RTA is usually seen in this age group [Table 2]
Thirty-eight patients were male and two were female
Twenty-two patients had associated fractures, sixteen had condylar fractures, angle, body, and ramus fractures were seen in two patients each
Occlusion evaluated preoperatively showed that 26 patients had minor occlusal disturbance and 14 patients had major occlusal disturbance [Table 3]. Chi-square test revealed statistically insignificant difference between the groups (P = 1). Similarly, postoperative occlusion was evaluated [Table 4]. It was found that occlusion was normal in 36 out of total 40 patients (90%). Chi-square test revealed statistically insignificant difference between the groups (P = 0.474)
Mobility of the fractured site was evaluated postoperatively after 2 weeks, and it was found that mobility was absent in 36 out of total 40 patients (90%)
Pain was recorded based on the visual analog scale (VAS) for patients preoperatively and postoperatively on the 1st day, at 2 weeks, 4 weeks, and 3 months at parasymphysis region of the mandible [Table 5]. There was significant difference in the mean VAS scores among the Group I and II when compared from preoperative to 4-week follow-up. Post hoc analysis showed that the VAS was significantly higher at preoperative followed by the 1st day, 2 weeks, and 4 weeks in both Groups I and II. After 3 months, there was not any significant difference between the two groups
In Group II, two patients showed wound dehiscence, as both the patients had preoperative soft-tissue loss due to laceration on buccal and lingual vestibular mucosa at parasymphysis region of the mandible
Neurological defects were not noticed in any of the patients. Patients were evaluated for signs of infection. As infection was said to be present locally in the presence of any swelling, local rise in temperature, inflammation, and pus discharge; preoperatively, patients with gross infection at the site of fracture were excluded from the study. Postoperatively, infection was checked after 2 weeks till 6 months. After 2 weeks, infection was seen in two patients of Group II.
Table 2.
Distribution of parasymphysis fracture according to age
| Age group | Number of cases (%) |
|---|---|
| <20 | 4 (10) |
| 21-30 | 26 (65) |
| 31-40 | 6 (15) |
| 41-50 | 2 (5) |
| >50 | 2 (5) |
| Total | 40 (100) |
Table 3.
Preoperative occlusion evaluation
| Occlusion | Group 1 | Group 2 | Total number of cases |
|---|---|---|---|
| No occlusal disturbance | 0 | 0 | 0 |
| Minor occlusal disturbance | 14 | 12 | 26 |
| Major occlusal disturbance | 6 | 8 | 14 |
Table 4.
Postoperative occlusion evaluation
| Occlusion | Group 1 | Group 2 | Total number of cases |
|---|---|---|---|
| No occlusal disturbance | 20 | 16 | 36 |
| Occlusal disturbance | 0 | 4 | 4 |
Table 5.
Comparison of pain in both the groups
| Pain | Group 1 | Group 2 |
|---|---|---|
| Preoperative | 6.90 | 6.80 |
| 1 day postoperative | 3.30 | 3.60 |
| 2 weeks’ postoperative | 1.1 | 1.5 |
| 4 weeks’ postoperative | 0.3 | 0.4 |
| 3 months’ postoperative | 0.00 | 0.00 |
DISCUSSION
Even though mandible is a large and strong bone of the facial region, it commonly gets fractured in cases of maxillofacial traumas. Parasymphysis consists of outer and inner cortical layers with a central spongiosa. The outer cortex is particularly strong; its thickness in the parasymphysis region is 2.3–2.5 mm and is reinforced laterally by the oblique line which runs caudally from the coronoid process and fans out in the region of cheek teeth to form a strong projection. This provides osteosynthesis screws with good anchorage by virtue of a compact bony structure. In parasymphysis region, the cross-section of the mandible shows a stronger cortex inferiorly at the lower border with a thickness of 8–10 mm, but the anatomy of the roots of the teeth, especially canines measuring around 16–17 mm, the presence of mental nerve and the structure of the bone do not allow easy screw fixation in this region as the distance between the root apex and the outer cortex is 3.2–4 mm.[3,4,5]
The management of parasymphysis fractures always poses challenge to the maxillofacial surgeons, due to its unique anatomy, blood supply, muscular attachments, curvature, and thickness of cortical plates. The aim of parasymphysis fracture treatment is reestablishment of anatomy and also restoring occlusion. Earlier wiring techniques were used in the management of these fractures. These techniques had complications such as more time, damage to soft tissues, feeding, and speech problems. However, in the recent years, diverse methods of open reduction and internal fixation have been in use and with good outcome, fewer complications, and increased patient satisfaction. However, even now, the choice of treatment is controversy, as many parameters should be taken into considerations such as site of fracture and number of fractures. A surgeon should have adequate knowledge of the anatomy as well as about the basic aspects of bone healing to prevent complications after fracture management.[5,6,8]
Parasymphysis region is parabola in shape. The management of fractures of this region is problematic due to various factors such as the forces created by mouth opening muscles (digastric, mylohyoid, and geniohyoid) and the presence of point of weakness associated with the canine root.[9]
Restoration of occlusion is also one of the main aims in fracture in parasymphysis area, as a malunion of fractured segments may lead to improper occlusion, thereby compromising function and may cause temporomandibular joint problems. Substances used for fracture fixation should be biologically well tolerated, smaller in size as possible, and adaptable and should be sufficiently strong to resist the bending and torsional forces of about 60–100 DaN. Champy's lines of osteosynthesis suggests that two plates applied in parallel with a gap of 4–5 mm are needed to resist torsion forces of up to 220 DaN.[9,10]
In 1970s, surgeons developed dynamic compression plating systems with screws for the mandible as means of rigid fixation, thereby obtaining more stability than that obtained with the use of plate alone. The main disadvantages include large plates, complex adaptation, scar, operation time, and possibility of nerve injury.[11,12,13]
Champy and Pape modified Michelet et al. method of fixation using two small, easily flexible, and noncompression plates anchored by monocortical screws. According to them, the advantages of miniplates are small size, ease of placement, intraoral approach, and adaptability.[9,14]
Mustafa[15] was first to introduce 3D miniplates. 3D plates contain thin 1 mm connecting arms, for easy adaptation to the bone without any deformation, and owing to the presence of free spaces between the arms allow good blood supply to the bone. The advantages of 3D-plate matrix plates or strut plates are that it allows more number of screws which give stability in 3D and resist torque forces. As symphysis and parasymphysis fractures are under higher torsional strain than other areas of the mandible; therefore, 3D plates are used in this area to provide superior stability.[12,13,14,15]
This study was designed with an aim of evaluating the efficacy of 3D-miniplate fixation in the management of mandibular parasymphysis fracture. Of 40 patients, 38 were male and two were female patients. This male predominance might be due to the fact that men are commonly exposed to RTA and other trauma.[9]
RTA was the main etiology with 24 (60%) cases. This finding is in accordance with Schuchardt et al.[16] who found RTA in 35.6% cases. They suggested that strict formulation and implementation of traffic rules may reduce trauma due to RTA.
We found parasymphysis fracture with associated fractures in 22 cases. About 16 (40%) patients had associated condyle fractures. Our findings were similar to Schuchardt et al.[16] and in contrast to Haug et al.[17] who found more cases of fractured body of mandible as associated fractures.
When occlusion was examined postoperatively, we found all the 20 cases in Group I to have no occlusal disturbance, and 4 patients in Group II were having occlusal disturbance. Chi-square test revealed statistically insignificant difference between the groups (P = 0.474).
Mobility of fractured segments was examined postoperatively, we found all the 20 cases in Group I to have no mobility, and 4 patients in Group II were having mobility. Chi-square test revealed statistically insignificant difference between the groups (P = 0.474). Our findings were similar to that of Gear et al.[18] and Alkan et al.[19] who showed that 3D struts plates to have superior resistance to compression load than the Champy's technique. The preoperative pain score in Group I was moderate in eight patients and severe in twelve patients, whereas in Group II, eight patients had moderate pain and two patients had severe pain. On the 1st postoperative day, pain was higher in Group II patients. This might be due to the wide surgical exposure and more time required for the placement of Champy's miniplate.[11,20]
At the end of 2 weeks, pain was mild in all the patients, except in two patients of Group II in whom pain was moderate. This might be due to higher incidence of infection and mobility at the fractured segments. However, no significant difference was noticed after 3 months in both groups. No neurological deficits were recorded in both Group I and Group II patients preoperatively and various follow-up stages postoperatively.
Pain and other postoperative complications may be due to other reasons, but the other parameters used for the study apart from pain are as follows:
Clinical parameters
Occlusion
Mobility of the fracture
Wound dehiscence
Neurological deficit
Infection.
Radiological parameter (orthopantomogram)
Approximation of the fracture segment
Screw loosening
Plate fracture
Six-month follow-up.
In our study, patients were evaluated preoperatively and postoperatively at 2 weeks, 4 weeks, 2 months, and 3 months after surgery for the signs of infection. As such, there was no incidence of infection noticed in Group I; whereas the incidence of infection for Group II was seen in four patients at 2 weeks and two patients at 4 weeks. All the patients were kept under antibiotic coverage and daily oral irrigation with betadine solution.
In 3D plates due to the extra vertical bars incorporated for countering the torque forces, in cases where fracture line passing through the mental foramina region, the lower bar of the plate was bent and placed above the mental nerve.
After using 3D plates, Guimond et al., Feledy et al., and Zix et al. reported infection rates of 5.4%, 9%, and 0%, respectively. In our study, infection rate reported was 0% in Group I and 20% in Group II. This infection might be due to mobility of fractured segments.[11,12,20] Guimond et al. showed a low incidence of wound dehiscence and plate exposure with 3D plate in comparison to Champy's miniplate.[20]
We found that 3D plates were indeed easy and simple to use. The placement of 3D plate was also found to be more comfortable without distortion or displacement due to the presence of connecting arms or vertical struts, and there were no major postoperative complications such as malocclusion, nonunion, or hardware failure. The quadrangular geometry of plate assures a 3D stability of the fracture sites as it offers good resistance against torque forces, thereby avoiding the need for maxillomandibular fixation and ensures the early restoration of parasymphysis function. Patients treated by 3D plates did show a less incidence of occlusal discrepancy than Champy's miniplates though the comparison between groups showed the results as statistically nonsignificant.
The only probable limitation of 3D plates is the placement of plate over oblique fractures and comminuted fractures. Hence, in these situations, Champy's miniplates have advantage over the 3D plates. The results of the present study were put to comparison with previous studies on fracture mandible and were found to be in accordance with them. All patients in the present study appreciated early recovery of normal jaw function, primary healing, and good union at fracture. The free areas between the arms of 3D-plate permit good blood supply to the bone which indirectly prevents infection and necrosis in our cases.
Henceforth, during the study, we conclude that the 3D plate was found to be standard in profile, strong yet malleable, facilitating reduction, and stabilization at both the superior and inferior borders giving 3D stability at fracture site. They seem to be an easy to use, shortens working time as an alternative to conventional miniplates for providing satisfactory osteosynthesis.[18,19,20]
CONCLUSION
Patients treated with 3D plates showed better results in terms of occlusion, infection, and other complications than with Champy's plates. The small sample size and limited follow-up could be considered as the limitations of our study. It is hence recommended to have a multicenter study with large number of patients and correlation among these studies would give definitive results.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Barde DH, Mudhol A, Ali FM, Madan RS, Kar S, Ustaad F. Efficacy of 3-dimensional plates over champys miniplates in mandibular anterior fractures. J Int Oral Health. 2014;6:20–6. [PMC free article] [PubMed] [Google Scholar]
- 2.Chee NS, Park SJ, Son MH, Lee EJ, Lee SW. Surgical management of edentulous atrophic mandible fractures in the elderly. Maxillofac Plast Reconstr Surg. 2014;36:207–13. doi: 10.14402/jkamprs.2014.36.5.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Uhthoff HK, Poitras P, Backman DS. Internal plate fixation of fractures: Short history and recent developments. J Orthop Sci. 2006;11:118–26. doi: 10.1007/s00776-005-0984-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Joshi U, Kurakar M. Comparison of stability of fracture segments in mandible fracture treated with different designs of mini-plates using FEM analysis. J Maxillofac Oral Surg. 2014;13:310–9. doi: 10.1007/s12663-013-0510-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sadhwani BS, Anchlia S. Conventional 2.0 mm miniplates versus 3-D plates in mandibular fractures. Ann Maxillofac Surg. 2013;3:154–9. doi: 10.4103/2231-0746.119231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goyal M, Marya K, Chawla S, Pandey R. Mandibular osteosynthesis: A Comparative evaluation of two different fixation systems using 2.0 mm titanium miniplates & 3-D locking plates. J Maxillofac Oral Surg. 2011;10:316–20. doi: 10.1007/s12663-011-0242-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prasad R, Thangavelu K, John R. The role of three dimensional plating system in mandibular fractures: A prospective study. J Pharm Bioallied Sci. 2013;5(Suppl 1):S10–3. doi: 10.4103/0975-7406.113280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gokkulakrishnan S, Singh S, Sharma A, Shahi AK. An analysis of postoperative complications and efficacy of 3-D miniplates in fixation of mandibular fractures. Dent Res J (Isfahan) 2012;9:414–21. [PMC free article] [PubMed] [Google Scholar]
- 9.Champy M, Pape HD. Chicago, USA: Quintessence; 1986. The Strasbourg Miniplate Osteosynthesis; pp. 19–43. [Google Scholar]
- 10.Jain MK, Manjunath KS, Bhagwan BK, Shah DK. Comparison of 3-dimensional and standard miniplate fixation in the management of mandibular fractures. J Oral Maxillofac Surg. 2010;68:1568–72. doi: 10.1016/j.joms.2009.07.083. [DOI] [PubMed] [Google Scholar]
- 11.Guimond C, Johnson JV, Marchena JM. Fixation of mandibular angle fractures with a 2.0-mm 3-dimensional curved angle strut plate. J Oral Maxillofac Surg. 2005;63:209–14. doi: 10.1016/j.joms.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 12.Zix J, Lieger O, Iizuka T. Use of straight and curved 3-dimensional titanium miniplates for fracture fixation at the mandibular angle. J Oral Maxillofac Surg. 2007;65:1758–63. doi: 10.1016/j.joms.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 13.Szabó G, Kovács A, Pulay G. Champy plates in mandibular surgery. Int J Oral Surg. 1984;13:290–3. doi: 10.1016/s0300-9785(84)80035-6. [DOI] [PubMed] [Google Scholar]
- 14.Kuriakose MA, Fardy M, Sirikumara M, Patton DW, Sugar AW. A comparative review of 266 mandibular fractures with internal fixation using rigid (AO/ASIF) plates or mini-plates. Br J Oral Maxillofac Surg. 1996;34:315–21. doi: 10.1016/s0266-4356(96)90010-8. [DOI] [PubMed] [Google Scholar]
- 15.Mustafa F. Three dimensional plate fixation of fractures and osteotomies. Facial Plast Surg Clin North Am. 1995;3:39–56. [Google Scholar]
- 16.Schuchardt K, Schwenzer N, Rottke B, Lentrodt J, Kruger E, Schilli W. Oral and Maxillofacial Traumatology. Vol. 1. Chicago. Quintessence: 1982. Ursachen, haufigkeit und lokalisation der frakturen des gesichtsschadels; p. 49. [Google Scholar]
- 17.Haug RH, Prather J, Indresano AT. An epidemiologic survey of facial fractures and concomitant injuries. J Oral Maxillofac Surg. 1990;48:926–32. doi: 10.1016/0278-2391(90)90004-l. [DOI] [PubMed] [Google Scholar]
- 18.Gear AJ, Apasova E, Schmitz JP, Schubert W. Treatment modalities for mandibular angle fractures. J Oral Maxillofac Surg. 2005;63:655–63. doi: 10.1016/j.joms.2004.02.016. [DOI] [PubMed] [Google Scholar]
- 19.Alkan A, Celebi N, Ozden B, Baş B, Inal S. Biomechanical comparison of different plating techniques in repair of mandibular angle fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:752–6. doi: 10.1016/j.tripleo.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 20.Feledy J, Caterson EJ, Steger S, Stal S, Hollier L. Treatment of mandibular angle fractures with a matrix miniplate: A preliminary report. Plast Reconstr Surg. 2004;114:1711–6. doi: 10.1097/01.prs.0000142477.77232.f7. [DOI] [PubMed] [Google Scholar]


