Why was the cohort set up?
The population worldwide is ageing. In the USA, the large baby-boom cohorts born 1946–64 are now reaching the ages at which risks of disability and use of long-term services and supports are substantial. There is also growing recognition that daily life for older adults depends not only on their physical, cognitive and sensory reserves but also the environments in which they live.
The National Health and Aging Trends Study (NHATS) was initiated by the U.S. National Institute on Aging (NIA) in 2008 to guide efforts to reduce disability, maximize health and independent functioning and enhance quality of life at older ages. The panel study is designed to answer new questions about how population-level disability trends change and how individual-level dynamics in late-life functioning unfold as the U.S. population ages. Additionally, the study facilitates investigation of differences in trends and trajectories for various at-risk subgroups and deeper understanding of the consequences of disability from age 65 through to the end of life.
NHATS conducts annual in-home interviews with over 8000 older adults living in the USA. For individuals who die, an interview about the last month of life (LML) is conducted with a knowledgeable informant. NHATS also generates the National Study of Caregiving (NSOC) sample, which characterizes caregiving experiences of family and unpaid caregivers of NHATS participants.
NHATS is funded through a cooperative agreement with NIA. The study has been led by faculty from the Johns Hopkins University Bloomberg School of Public Health and the Institute for Social Research at the University of Michigan, with scientific input from a multidisciplinary group of co-investigators and two advisory groups. Westat, a research firm with expertise in data collection and management, conducts the fieldwork.
Who is in the cohort?
Initial sample selection
The initial sample was drawn from the enrolment file for Medicare, which provides health insurance for approximately 96% of US adults aged 65 and older. The remaining 4% of older adults include those who opt to defer enrolment (often because they have employer-provided insurance) and individuals who do not meet programme eligibility criteria (often related to residency requirements).
Cases were sampled for Round 1 (2011) in three stages: (i) 95 counties (or groups of counties) were sampled from the contiguous USA; (ii) 655 ZIP codes were then sampled within selected counties; and (iii) 12 411 beneficiaries age 65 and older, enrolled as of 30 September 2010, were then sampled within selected ZIP codes and released to the field. For the last step, individuals at older ages and Black individuals were sampled at higher rates than other groups. Oversampling by age and race was incorporated into the design to provide ample statistical power to analyse trends by 5-year age groups and comparisons between Black and non-Black subgroups over time. Of the 8245 participants in 2011, over 40% were ages 80 or older and about 20% self-identified as Black or African American.1
Periodic replenishment
NHATS is replenished periodically to provide a refreshed nationally representative cohort of the Medicare population aged 65 and older at regular intervals. In Round 5 (2015), a new sample of beneficiaries, aged 65 and older as of 30 September 2014, was introduced (using the same sampling approach, including oversampling) to restore the panel to original sizes by age and race groups.2 When added to survivors from the original panel, these samples form the 2015 cohort (initial n = 8038).
How often have they been followed up?
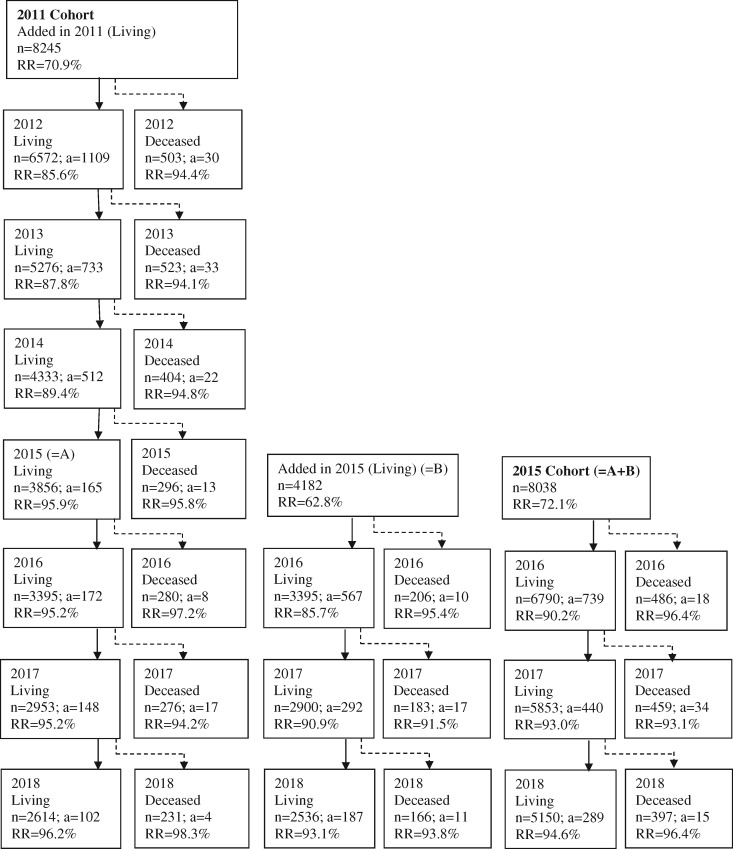
Interviews are conducted annually from approximately May/June-October/November. For the 2011 cohort, eight rounds (2011–18) have been collected thus far. For the 2015 cohort, four rounds (2015–18) have been collected. Figure 1 shows unweighted sample sizes, attrition and response rates through 2018 for the 2011 cohort, cases added in 2015 and the 2015 cohort.
Figure 1.
NHATS sample and response rates (RR) 2011018. N, completed interviews; a, attrited cases; RR Living, living respondents with a complete sample person or facility interview/respondents surviving since previous round; RR Deceased, deceased respondents with a complete last month of life interview/respondents dying since previous round. RR calculations exclude the small number of cases who became ineligible for follow-up each year (31 in 2012, seven in 2013, five in 2014, three in 2015, five in 2016, four in 2017, two in 2018).
Demographic characteristics of the cohorts
Sample weights and design variables are provided to users at each round for each cohort.3 Sample weights are necessary to adjust for differential probabilities of selection by age and race and for potential biases from differential initial response rates and attrition over time. Sample design variables are necessary to account for geographical clustering in the estimation of standard errors.4 When sample weights and design variables are used, resulting estimates are representative of successive cohorts of Medicare beneficiaries aged 65 and older (e.g. starting in 2011 and in 2015).
Weighted distributions of select demographic characteristics and unweighted sample sizes by round for each cohort are shown in Table 1. Comparisons with data from Medicare and the US Census Bureau confirm close agreement with NHATS by age groups and sex. Small differences in the youngest age group are attributable to the approximately 6-month gap between sampling and the start of field work.5
Table 1.
Distribution of demographic characteristics of 2011 and 2015 NHATS cohorts by round and of 2010 and 2014 medicare enrolment and census counts
| NHATS Round (year) |
Medicare |
Census |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cohort/characteristic | 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||||
| (2011) | (2012) | (2013) | (2014) | (2015) | (2016) | (2017) | 2010 | 2014 | 2010 | 2014 | |
| 2011 | |||||||||||
| n | 8245 | 6572 | 5276 | 4333 | 3856 | 3395 | 2953 | ||||
| Ages represented | 65+ | 66+ | 67+ | 68+ | 69+ | 70+ | 71+ | 65+ | 65+ | 65+ | 65+ |
| Age group | |||||||||||
| 65–69 | 27.2 | 22.0 | 14.4 | 6.7 | 1.4 | 0.0 | 0.0 | 30.4 | 30.9 | ||
| 70–74 | 24.6 | 25.8 | 30.6 | 34.1 | 35.7 | 32.2 | 27.5 | 23.2 | 23.0 | ||
| 75–79 | 18.9 | 20.5 | 21.5 | 22.8 | 25.4 | 27.7 | 28.8 | 18.1 | 18.1 | ||
| 80–84 | 14.8 | 15.7 | 16.5 | 17.9 | 18.3 | 19.1 | 20.9 | 14.2 | 14.3 | ||
| 85–89 | 9.6 | 10.5 | 10.7 | 11.6 | 12.0 | 12.7 | 13.8 | 9.0 | 13.7 | ||
| 90+ | 4.9 | 5.6 | 6.3 | 6.9 | 7.2 | 8.3 | 9.0 | 5.0 | – | ||
| Sex | |||||||||||
| Male | 42.9 | 43.0 | 43.0 | 42.9 | 43.0 | 42.5 | 42.6 | 43.2 | 43.1 | ||
| Female | 57.1 | 57.0 | 57.0 | 57.1 | 57.1 | 57.5 | 57.4 | 56.8 | 56.9 | ||
| Race/ethnicity | |||||||||||
| White non-Hispanic | 80.5 | 81.0 | 80.8 | 81.2 | 81.4 | 81.4 | 81.2 | ||||
| Black non-Hispanic | 8.2 | 8.4 | 8.4 | 8.2 | 8.2 | 8.2 | 8.2 | ||||
| Other, non-Hispanic | 6.7 | 6.4 | 6.5 | 6.2 | 6.2 | 6.3 | 6.5 | ||||
| Hispanic | 4.6 | 4.2 | 4.3 | 4.4 | 4.3 | 4.0 | 4.1 | ||||
| 2015 | |||||||||||
| n | 8038 | 6790 | 5853 | ||||||||
| Ages represented | 65+ | 66+ | 67+ | ||||||||
| Age group | |||||||||||
| 65–69 | 28.9 | 25.2 | 15.5 | 33.0 | 33.2 | ||||||
| 70–74 | 26.2 | 26.8 | 34.1 | 24.3 | 24.0 | ||||||
| 75–79 | 18.5 | 20.2 | 20.8 | 17.2 | 17.1 | ||||||
| 80–84 | 12.8 | 13.2 | 14.4 | 12.4 | 12.5 | ||||||
| 85–89 | 8.4 | 9.1 | 9.2 | 8.1 | 13.3 | ||||||
| 90+ | 5.2 | 5.6 | 6.1 | 5.1 | – | ||||||
| Sex | |||||||||||
| Male | 44.2 | 44.1 | 44.1 | 44.2 | 44.0 | ||||||
| Female | 55.8 | 55.9 | 55.9 | 55.8 | 56.0 | ||||||
| Race/ethnicity | |||||||||||
| White non-Hispanic | 77.8 | 78.1 | 78.3 | ||||||||
| Black non-Hispanic | 8.2 | 8.2 | 8.1 | ||||||||
| Other non-Hispanic | 7.0 | 6.7 | 6.4 | ||||||||
| Hispanic | 7.0 | 7.1 | 7.2 | ||||||||
Estimates are weighted to account for differential probabilities of selection, non-response, and attrition. Top age group for Census is age 85+.
What has been measured?
Overview of instruments
NHATS interviews participants in their homes. At each round a Sample Person (SP) interview is conducted, except for those initially residing in nursing homes. The initial SP interview takes about 2 h to complete; subsequent rounds take about 90 min. Most sample persons respond to the SP interview for themselves. A proxy who is familiar with the sampled person’s routine, typically a family member, is interviewed in instances where the sample person cannot respond on their own.
When the sample person lives in a residential care setting (nursing home, assisted living facility or other supportive living environment with services), a Facility Questionnaire (FQ) is also administered to a staff person. The FQ identifies type of place, care level, available services and sources and amounts of payment. The FQ is triggered through questions in the SP interview.
When a sample person is confirmed as deceased, typically by a family member, the Last Month of Life (LML) portion of the SP interview is administered. LML interviews are typically conducted with a close family member and focus on quality of the end of life experience.6
Overview of annual disability measures in the SP instrument
The NHATS disability protocol includes validated measures of the disablement process.7–10 Here we provide a brief overview of measures collected annually (see Table 2).
Table 2.
Overview of content in the National Health and Aging Trends Study, 2011–18
| Sample Person Interview | |
| Baseline onlya content | Personal Factors & Demographic Characteristics: date of birth, gender, early-life circumstances, race/ethnicity, veteran’s status, completed education, lifetime occupation |
| Baseline & annual follow-up content | Health Conditions & Treatments: self-rated health, self-report of common diseases and chronic conditions, common clinical concerns (falls, depression, anxiety, sleep), height and weight, hospital stays, surgeries, rehabilitation use and outcomes (added in 2015) |
| Impairments & Symptoms: problems with pain, breathing, strength or movement upper body, strength or movement lower body, low energy/exhaustion, balance/coordination, difficulty with hearing, vision, chewing, swallowing, speaking/being understood | |
| Cognition: Self-respondents: self-rated memory, date (month/day/year) and day of week, naming President and Vice President, 10-word immediate and delayed recall, clock-drawing test; Proxy-respondents: overall memory rating, 8 items on changes in thinking/memory, behavioural problems | |
| Physical Capacity: physical performance tests (balance, rapid chair stands, usual walking speed, grip strength, peak air flow), self-reports of ability to walk six blocks/walk three blocks, climb 20 stairs/climb 10 stairs, lift and carry 20 lb/10 lb, kneel down/bend over, heavy object overhead/reach overhead, open sealed jar/grasp small objects | |
| Activity Limitations & Participation Restrictions: device use, difficulty by oneself, change in frequency, help with self-care and mobility activities, help because of health or functioning, difficulty by oneself, change in frequency of household and medical activities, duration of self-care and mobility accommodations, restricted participation in valued activities due to health or functioning | |
| Unmet Need: negative consequences related to unmet needs in self-care, mobility and household activities | |
| Social Environment: household members, marital status, biological and step-children, social network members, whether mother/father still living, number of living siblings, social capital in surrounding community | |
| Physical Environment: type of housing, features of the home environment, home modifications, interviewer observations inside/outside home | |
| Technological Environment: use of internet in daily activities and forms of communication (e.g. e-mail, texting and socializing online) | |
| Service Environment: type of residential care setting, location within facility, services available and used | |
| Transportation: driving habits, how participants get to places, whether transportation problem limits participation | |
| Helpers: hours assisted in past month, whether paid and amount, sources | |
| Well-being: frequency of positive/negative emotions, agreement with statements reflecting flourishing, age participant feels, adaptability to change | |
| Economic Status: labour force participation, home ownership, insurance coverage, credit card debt, exchange of financial transfers with family, receipt of public programme assistance, food insecurity, problems paying bills | |
| Rotating content | Detailed income and assets: annual income and amounts by source, value of assets |
| Other content | Supplemental modules (select years): dried blood spot assays (C-reactive protein, interleukin-6, glycosylated haemoglobin and anti-cytomegalovirus, 2017), Stroop test (2012), National Study of Caregiving (NSOC, 2011, 2015, 2017) |
| Facility Questionnaire: Baseline & annual follow-up content | Place type, services available to the resident, payment sources and amounts, and demographic information |
| Last Month of Life interview content | Place of death, quality of last month of life, residence type, cognitive impairment, help with mobility and self-care, mobility device use, duration of mobility and self-care assistance, and participation in favourite activity |
Baseline only refers to 2011 for the 2011 cohort or added in 2015 for the 2015 cohort.
Health Conditions covers self-rated health, self-reports of diagnosed diseases and chronic conditions, hospital stays and surgeries and a number of common clinical concerns in later life including falls, depressive and anxiety-related symptoms and sleep quality. In 2015 questions about rehabilitation were added.
Impairments and Symptoms asks about impairments in several body systems (breathing, upper and lower body strength and movement, balance/coordination), pain and fatigue, vision and hearing impairments, ability to chew/swallow and speak/be understood.
Physical capacity measures in NHATS include both performance-based and self-reported measures. Performance-based measures include: balance tests; rapid chair stands; usual walking speed; grip strength; and peak air flow.11 Self-reports of ability by oneself, and if relevant without devices, to carry out less and more challenging tasks (e.g. bending over and kneeling down) are also obtained.
To assess cognitive capacity, participants first rate their memory and then perform a memory-related activity (immediate and delayed 10-word recall), respond to items related to orientation and perform a clock drawing test to assess executive function. For proxy interviews, an eight-item informant screener for dementia called the AD8 is administered.12,13 Items on previous diagnosis, a score of two or more on the AD8 and performance on orientation, memory and clock drawing tests have been combined to form an indicator distinguishing probable and possible dementia.14
Details about activity limitations and participation restrictions are also assessed. For self-care and mobility activities, respondents are asked whether in the past month they used specific assistive devices (e.g. grab bar, walker) while doing a particular activity, whether they had difficulty doing the activity by themselves when using named devices, frequencies compared with a year ago and whether they received help. For household and medical activities, NHATS asks how the activity was carried out in the past month (e.g. alone, with others, by others etc.) and frequency compared with a year ago. If someone else was involved, whether help was received for health and functioning reasons is assessed. For eight social and productive activities (e.g. visiting with friends, going out for enjoyment), sampled persons are asked whether they participated in the past month, whether their health or functioning limited their participation and how important it was to be able to participate.
NHATS also collects details about the environments in which older adults live. The social environment is captured through household members, marital status, living children and social network members, a count of living siblings and items about the broader community. The physical environment includes characteristics of the home (e.g. floors, stairs), modifications to the home (e.g. addition of grab bars) and observations by the interviewer (e.g. clutter). The technological environment is reflected in use of the internet in daily activities and forms of communication such as e-mail, texting and socializing online. The service environment is captured through questions about the type of housing and, in residential care (and starting in 2015, retirement settings), the services offered and used.
Transportation measures include driving habits, how participants get to places and whether a transportation problem limits their participation in various activities.15
For each helper identified in the interview (other than residential care staff), NHATS collects hours assisted in the past month, whether paid and amounts and sources of payment.
Other content
NHATS obtains demographic characteristics and several items about early life (e.g. family structure, economic status, location) during the baseline interview. Brief supplemental modules are included at the end of the SP interview. In Rounds 1 and 5, the module consisted of items from the National Long Term Care Survey Screener, which allows long-term trends to be assessed. In other rounds, modules are invited from the research community and have included end-of-life preferences, pain, sleep quality, personality, medication attitudes and sedentary time.
In Round 7 (2017) NHATS included a dried blood spot collection. Assays to be made available include: C-reactive protein, interleukin-6, glycosylated haemoglobin and anti-cytomegalovirus. Planning for genotyping of material is also under way.
Unpaid and family caregivers are occasionally interviewed as part of the National Study of Caregiving (NSOC), which provides information on family members and friends who are providing assistance to older adults.16
Linkages
Linkage to Medicare beneficiary files, which includes monthly enrolment information, is available for 100% of the sample. In addition, linkage is available to claims (e.g. hospital, physician, durable medical equipment, hospice) for those enrolled in fee-for-service plans, to prescribed medicine claims for those enrolled in Medicare’s prescription drug benefit (Part D) and to assessment files for those with nursing home, inpatient rehabilitation or home health utilization. Common chronic conditions constructed from claims histories are also available. For further information on Medicare linkages, see [www.ccwdata.org].
Linkage to the 1940 Census will provide historical information on household and family composition for individuals living in the USA in that year.
What has been found?
Here we illustrate several thematic areas that take advantage of NHATS’ unique design and measurements. See [www.nhats.org] for a full list of publications.
NHATS offers researchers the unique ability to examine a spectrum of behavioural adaptations to activity limitations—that is, how older adults carry out their daily activities. A five-stage hierarchy of late-life mobility and self-care limitations that captures behavioural adaptations has been proposed.17 In this schema, one-third of the population aged 65 years and older are fully able to carry out all self-care and mobility activities, one-fourth are able to manage without assistance by successfully accommodating with devices or environmental features and about one in 10 have reduced their activity level but report no difficulty. Other researchers have found support for the five-category scale over several alternative scales for predicting onset of help and a collapsed four-category scale for predicting mortality.18
Using NHATS, researchers have demonstrated that coping strategies matter to older adults’ well-being. Well-being levels for those successfully accommodating are similar to and participation restrictions only slightly below those of persons who are fully able to carry out mobility and self-care activities.19 Similarly, among persons with self-care limitations, use of assistive devices is associated with greater well-being, whereas personal help is negatively related.20
With its annual design and last month of life interview, NHATS is also exceptionally well suited for studying quality of end of life and functioning in the last year of life. For instance, researchers have found that reports of unmet need for end-of-life pain management are more common in 2011 than in 2000, and that the overall rating of quality of end-of-life care has decreased over this period.21 Others find that one in eight respondents report care in the last month of life was inconsistent with the patients' wishes and that inconsistent care is more likely to occur in a hospital or nursing home setting.22 Analysis of NHATS also finds that 40% of older adults have not discussed their end-of-life preferences.23
NHATS has also been used to explore the quality of life of vulnerable groups of older adults, such as those unable to leave their home. In 2011, about 2 million people aged 65 and older (5.6% of the older population) were considered homebound (400 000 completely homebound and 1.6 million mostly homebound) and only 12% of individuals who were classified as completely homebound reported receiving primary care services at home.24 The rate of depressive symptoms among those considered homebound is 44% and 2-year mortality is 40%.25,26
Researchers have also used NHATS with NSOC to document the status of family caregivers.27 In 2011, nearly 12 million caregivers had provided help for 2 to 10 years and another 2.5 million for more than 10 years. Over their lifetime, a typical adult can expect to care for an older family member or friend for 6 years. NSOC has also provided new national information on caregiver involvement in health care activities and its impact on care providers.28,29
Researchers have also studied dementia and related care issues with NHATS. Findings highlight the disproportionate share of care hours that are provided to individuals with dementia: although only 10% of older adults in the US have dementia, one-third of caregivers assist people with dementia and account for 41% of the hours of help provided.30 NHATS has also contributed to a growing literature demonstrating declines in the prevalence of late-life cognitive impairment in recent years.31 Other researchers have demonstrated that those who have probable dementia without a reported dementia diagnosis are more likely to engage in potentially unsafe behaviours (e.g. drive, make hot meals, handle finances and medications, and attend medical visits alone) than those with a reported diagnosis.32
Researchers have used NHATS to document the substantial prevalence of unmet need among older adults. Of those who had difficulty or received help in settings other than nursing homes, 32% had an adverse consequence in the past month related to an unmet need; for community residents with a paid caregiver, the figure was nearly 60%.33 Others have documented that individuals dually eligible for Medicare and Medicaid and those with caregivers experiencing high levels of burden and stress have greater unmet needs.34,35
NHATS is a unique resource for understanding long-term disability and care trends. Comparing active life expectancy in 1982 with 2011, researchers have documented that older women no longer live more active years than men, despite their longer lives, and that older Black women are especially disadvantaged in terms of the proportion of years expected to be lived without disability.36,37 Researchers have also found that, contrary to prevailing concerns, family caregivers’ circumstances have generally improved since 1999.38
What are the main strengths and weaknesses?
NHATS has several strengths for studying late-life disability trends and trajectories in the context of an ageing society.
NHATS is a probability-based sample. That means, with sampling weights, estimates are representative of Medicare beneficiaries aged 65 and older.
NHATS offers large sample sizes particularly at very old ages. Nearly half the sample is over age 80 and individuals aged 90 and over were sampled at a higher than average rate. NHATS also offers an oversample of Black, non-Hispanic persons.
NHATS has a comprehensive, validated disability protocol that is administered annually. A high degree of attention is given to the identification of residential care settings, including descriptions of services offered and costs associated with living in such places. In addition, NHATS offers monthly measures of assistance with self-care and mobility activities. The study is also fully linkable to Medicare claims and assessment files.
NHATS is a unique resource for studying end of life. Interviews take place on average approximately 6 months before and after death and focus on the quality of the end-of-life care experience.
NHATS serves as the foundation for NSOC, and together the two studies are the only national platform for studying caregiving from the perspective of both older adults and their caregivers.
Long-term trends can be assessed by comparing NHATS with its predecessor survey, the National Long Term Care Study.
Like all surveys, NHATS is subject to survey errors, including random and non-random errors in sampling and measurement. Non-response adjusted weights protect against non-random non-response and attrition; however, if there are additional factors related to response and disability that are not addressed by the weights, estimates may be biased. In addition, although generalizable to the older Medicare population, analyses of subgroups of interest may be limited because of sample size constraints. Moreover, because all participants are at least aged 65, content from earlier in life is limited to retrospective responses and (forthcoming) linkages to the 1940 Census.
How can I access the data? Where can I find out more?
NHATS public use data files can be obtained after registration (including agreement to NHATS’ conditions of use) at [www.NHATS.org]. Sensitive data, including NSOC data, are available after completion of a brief Sensitive Data Agreement and verification of research credentials. Access to restricted data—including Medicare linkages and geographical files—requires a Data Use Agreement with NHATS and data protection plan. Details about the application process are available at [www.NHATS.org]. For additional details, contact [nhatsdata@westat.com] or Judith Kasper at [jkasper1@jhu.edu] or Vicki Freedman at [vfreedma@umich.edu].
National Health and Aging Trends Study profile in a nutshell
The National Health and Aging Trends Study (NHATS) is designed to study population-level trends and individual-level dynamics in late-life functioning in the USA. NHATS also facilitates investigation of differences in disablement for various at-risk subgroups and of the economic and social consequences of disability from aged 65 through to the end of life.
Adults aged 65 and older were sampled from the Medicare enrolment file and first interviewed in 2011 (n = 8245); the panel was refreshed in 2015 (n = 8334). Weighted estimates are representative of Medicare beneficiaries aged 65 and older nationally.
Participants are interviewed annually in their homes. A facility interview is also completed for those in residential care settings. A last month of life interview collects details on quality of end-of-life care for decedents. Caregivers are also interviewed periodically.
A comprehensive validated protocol measures the components of disablement: self-reported and performance-based measures of physical and cognitive capacity, activities (mobility, self-care, household) and participation, accommodations (help, devices and modifications, behaviour changes) and the environment (physical, social, technological, services). Other topics cover rehabilitation service use, transportation, helper characteristics, well-being, economic status and baseline demographic characteristics. Interview data may be supplemented by restricted geographical information and linkages to Medicare data.
Data are available from www.NHATS.org.
Funding
This work was supported by the National Institute on Aging of the National Institutes of Health [U01-AG032947].
Conflict of interest: None declared.
References
- 1. Montaquila J, Freedman VA, Edwards B, Kasper JD.. National Health and Aging Trends Study Round 1 Sample Design and Selection. NHATS Technical Paper #1. Baltimore, MD: Johns Hopkins University School of Public Health, 2012. [Google Scholar]
- 2. DeMatteis J, Freedman VA, Kasper JD.. National Health and Aging Trends Study Round 5 Sample Design and Selection. NHATS Technical Paper #16. Baltimore, MD: Johns Hopkins University School of Public Health, 2016. [Google Scholar]
- 3. Montaquila J, Freedman VA, Spillman BC, Kasper JD.. National Health and Aging Trends Study Development of Round 1 Survey Weights. NHATS Technical Paper #2. Baltimore, MD: Johns Hopkins University School of Public Health, 2012. [Google Scholar]
- 4. DeMatteis J, Freedman VA, Kasper JD.. National Health and Aging Trends Study Development of round 5 Survey Weights. NHATS Technical Paper #14. Baltimore, MD: Johns Hopkins University School of Public Health, 2016. [Google Scholar]
- 5. Freedman VA, Spillman BC, Kasper JD.. Making National Estimates with the National Health and Aging Trends Study. NHATS Technical Paper #17. Baltimore, MD: Johns Hopkins University School of Public Health, 2016. [Google Scholar]
- 6. Teno JM, Clarridge B, Casey V. et al. Validation of toolkit after-death bereaved family member interview. J Pain Symptom Manage 2001;22:752–58. [DOI] [PubMed] [Google Scholar]
- 7. Freedman VA, Kasper JD, Cornman JC. et al. Validation of new measures of disability and functioning in the National Health and Aging Trends Study. J Gerontol A Biol Sci Med Sci 2011;66:1013–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Freedman VA, Agree EM, Cornman JC, Spillman BC, Kasper JD.. Reliability and validity of self-care and mobility accommodations measures in the National Health and Aging Trends Study. Gerontologist 2014;54:944–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kasper JD, Chan KS, Freedman VA.. Measuring physical capacity: an assessment of a composite measure using self-report and performance-based items. J Aging Health 2017;29:289–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kasper JD, Freedman VA.. National Health and Aging Trends Study User Guide. Baltimore, MD: Johns Hopkins University School of Public Health, 2018. [Google Scholar]
- 11. Kasper JD, Freedman VA, Niefeld MR.. Construction of Performance-based Summary Measures of Physical Capacity in the National Health and Aging Trends Study. NHATS Technical Paper #4. Baltimore, MD: Johns Hopkins University School of Public Health, 2012. [Google Scholar]
- 12. Galvin JE, Roe CM, Powlishta KK. et al. The AD8: a brief informant interview to detect dementia. Neurology 2005;65:559–64. [DOI] [PubMed] [Google Scholar]
- 13. Galvin JE, Roe CM, Xiong C, Morris JC.. Validity and reliability of the AD8 informant interview in dementia. Neurology 2006;67:1942–48. [DOI] [PubMed] [Google Scholar]
- 14. Kasper JD, Freedman VA, Spillman BC.. Classification of Persons by Dementia Status in the National Health and Aging Trends Study. Technical Paper #5. Baltimore, MD: Johns Hopkins University School of Public Health, 2013. [Google Scholar]
- 15. Skehan ME, Kasper JD, Freedman VA.. Driving and Transportation Measures in the National Health and Aging Trends Study. NHATS Technical Paper #8. Baltimore, MD: Johns Hopkins University School of Public Health, 2014. [Google Scholar]
- 16. Kasper JD, Freedman VA, Spillman BC.. National Study of Caregiving User Guide. Baltimore, MD: Johns Hopkins University School of Public Health, 2016. [Google Scholar]
- 17. Freedman VA, Kasper JD, Spillman BC. et al. Behavioral adaptation and late-life disability: a new spectrum for assessing public health impacts. Am J Public Health 2014;104:e88–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gill TM, Williams CS.. Evaluating distinctions in the assessment of late-life disability. J Gerontol A Biol Sci Med Sci 2017;72:1538–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Freedman VA, Kasper JD, Spillman BC.. Successful aging through successful accommodation with assistive devices. J Gerontol B Psychol Sci Soc Sci 2016;72:300–09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lin I-F, Wu H-S.. Activity limitations, use of assistive devices or personal help, and well-being: variation by education. J Gerontol B Psychol Sci Soc Sci 2014;69: S16–S25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Teno JM, Freedman VA, Kasper JD, Gozalo P, Mor V.. Is care for the dying improving in the United States? J Palliat Med 2015;18:662–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Khandelwal N, Curtis JR, Freedman VA. et al. How often is end-of-life care in the United States inconsistent with patients' goals of care? J Palliat Med 2017;20:1400–04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kale MS, Ornstein KA, Smith CB, Kelley AS.. End-of-life discussions with older adults. J Am Geriatr Soc 2016;64:1962–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ornstein KA, Leff B, Covinsky KE. et al. Epidemiology of the homebound population in the United States. JAMA Intern Med 2015;175:1180–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Xiang X, Brooks J.. Correlates of depressive symptoms among homebound and semi-homebound older adults. J Gerontol Soc Work 2017;60:201–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Soones T, Federman A, Leff B, Siu AL, Ornstein K.. Two-year mortality in homebound older adults: an analysis of the national health and aging trends study. J Am Geriatr Soc 2017;65:123–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Academies of Sciences, Engineering and Medicine. Families Caring for an Aging America. Washington, DC: National Academies Press, 2016. [PubMed] [Google Scholar]
- 28. Wolff JL, Spillman BC, Freedman VA, Kasper JD.. A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Intern Med 2016;176:372–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wolff JL, Spillman BC.. Older adults receiving assistance with physician visits and prescribed medications and their family caregivers: prevalence, characteristics, and hours of care. J Gerontol B Psychol Sci Soc Sci 2014;69: S65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kasper JD, Freedman VA, Spillman BC, Wolff JL.. The disproportionate impact of dementia on family and unpaid caregiving to older adults. Health Aff (Millwood) 2015;34:1642–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Freedman VA, Kasper JD, Spillman BC, Plassman BL.. Short-term changes in the prevalence of probable dementia: an analysis of the 2011-2015 National Health and Aging Trends Study. J Gerontol B Psychol Sci Soc Sci 2018;73:S48–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Amjad H, Roth DL, Samus QM, Yasar S, Wolff JL.. Potentially unsafe activities and living conditions of older adults with dementia. J Am Geriatr Soc 2016;64:1223–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Freedman VA, Spillman BC.. Disability and care needs among older Americans. Milbank Q 2014;92:509–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Allen SM, Piette E, Mor V.. The adverse consequences of unmet need among older persons living in the community: dual-eligible versus medicare-only beneficiaries. J Gerontol B Psychol Sci Soc Sci 2014;69: S51–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Beach SR, Schulz R.. Family caregiver factors associated with unmet needs for care of older adults. J Am Geriatr Soc 2017;65:560–66. [DOI] [PubMed] [Google Scholar]
- 36. Freedman VA, Wolf DA, Spillman BC.. Disability-free life expectancy over 30 years: a growing female disadvantage in the US population. Am J Public Health 2016;106:1079–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Freedman VA, Spillman BC.. Active life expectancy in the older US Population, 1982-2011: differences between blacks and whites persisted. Health Aff (Millwood) 2016;35:1351–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wolff JL, Mulcahy J, Huang J, Roth DL, Covinsky K, Kasper JD.. Family caregivers of older adults, 1999-2015: trends in characteristics, circumstances, and role-related appraisal. Gerontologist 2018;58:1021–32. [DOI] [PMC free article] [PubMed] [Google Scholar]