Abstract
Background:
The past decade has seen unprecedented shifts in the cannabis policy environment, and the public health impacts of these changes will hinge on how they affect patterns of cannabis use and the use and harms associated with other substances.
Objectives:
To review existing research on how state cannabis policy impacts substance use, emphasizing studies using methods for causal inference and highlighting gaps in our understanding of policy impacts on evolving cannabis markets.
Methods:
Narrative review of quasi-experimental studies for how medical cannabis laws (MCLs) and recreational cannabis laws (RCLs) affect cannabis use and use disorders, as well as the use of or harms from alcohol, opioids, and tobacco.
Results:
Research suggests MCLs increase adult but not adolescent cannabis use, and provisions of the laws associated with less regulated supply may increase adult cannabis use disorders. These laws may reduce some opioid-related harms, while their impacts on alcohol and tobacco use remain uncertain. Research on RCLs is just emerging, but findings suggest little impact on the prevalence of adolescent cannabis use, potential increases in college student use, and unknown effects on other substance use.
Conclusions:
Research on how MCLs influence cannabis use has advanced our understanding of the importance of heterogeneity in policies, populations, and market dynamics, but studies of how MCLs relate to other substance use often ignore these factors. Understanding effects of cannabis laws requires greater attention to differences in short-versus long-term effects of the laws, nuances of policies and patterns of consumption, and careful consideration of appropriate control groups.
Keywords: Cannabis, alcohol, opioids, substitution, drug policy, tobacco
Introduction
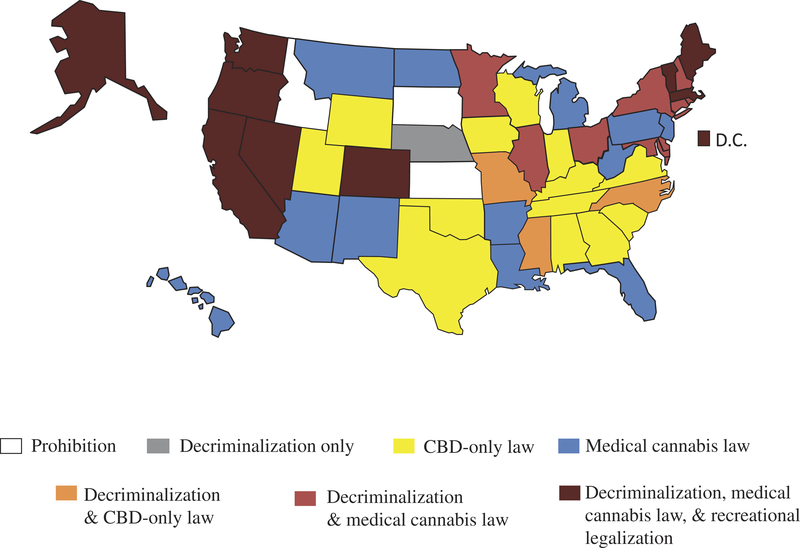
The past decade has seen unprecedented shifts in the cannabis policy environment. Canada and Uruguay became the first two countries to legalize the sale and use of cannabis for recreational purposes at the national level. Despite retaining its status as a strictly prohibited Schedule I substance at the federal level in the US, cannabis is currently (as of December 2018) legal for medicinal use in 33 states and the District of Columbia (policies hereafter referred to as “medical cannabis laws”); 10 states and D.C. have expanded their policies to also legalize cannabis use for recreational purposes (hereafter referred to as “legalization”) (1). If decriminalization (i.e., the removal of penalties associated with possession of cannabis, with no protection for supply) and high-cannabidiol (CBD) medical cannabis laws (MCLs) (i.e., “high-CBD-only laws”) are also considered, then all but three states have implemented some form of cannabis liberalization. This movement toward more liberal cannabis policies is mirrored by growing public support for legalization. In 2018, over 60% of US adults said use of cannabis should be legalized for recreational purposes, a considerable increase from the 32% in favor in 2006 (2).
Despite decades of policy experimentation, the current patchwork of state cannabis policies in the US (Figure 1) reflects ongoing disagreement about the potential benefits and harms of policies that regulate the production and consumption of cannabis. While some disagreements stem from limited scientific understanding of the potential harms and benefits of cannabis itself (3), often the discussions by policymakers regarding the impacts of legalization reflect mixed or uncertain evidence for how legalization policies influence key public health outcomes, including prevalence of cannabis use, risky cannabis use (e.g., cannabis use disorder [CUD]), and use of other substances.
Figure 1.
Cannabis policy in the United States, laws in effect as of January 1, 2018.
Decriminalization refers to policies that remove penalties associated with possession of small amounts of cannabis for personal use, with no protection for supply. Medical cannabis laws are laws that remove criminal penalties for medicinal cannabis use and some form of supply. CBD (cannabidiol)-only laws are medical cannabis laws that only permit certain low-delta9-tetrahydrocannabinol (THC) strains of cannabis to be used for medicinal purposes. Recreational legalization refers to laws that remove criminal and monetary penalties for the possession, use, and supply of cannabis for recreational purposes.
Recognizing there are a myriad of factors that characterize the interests of proponents and opponents of cannabis legalization (4), the present study focuses on one aspect of public health interest by reviewing the evidence for how medical and recreational cannabis laws (RCLs) impact cannabis use, as well as use of alcohol, opioids, and tobacco, three substances that generate substantial societal costs (5–8). We focus on evidence from scientifically rigorous policy evaluations that use methods for causal inference, i.e., those that (1) use time-series data, (2) verify that policies preceded their effects on outcomes, and (3) include a control or comparison group. By focusing on these empirical designs, we draw attention to the limited takeaways from these policy experiments so far and emphasize how challenging it is, even when using sophisticated econometric techniques, to draw firm conclusions from the current evidence.
Methods
We conducted searches in four databases (PubMed, Embase, EconLit, and PsycInfo) for peer-reviewed literature published between January 2005 and February 2019. Each database was searched on title, abstract, and keywords for policy-related terms such as “marijuana policy,” “marijuana law,” or “cannabis policy” as well as for outcome-related terms such as “alcohol,” “cannabis use,” and “opioid*.” Details of the search strategy are provided in the Supplementary material.
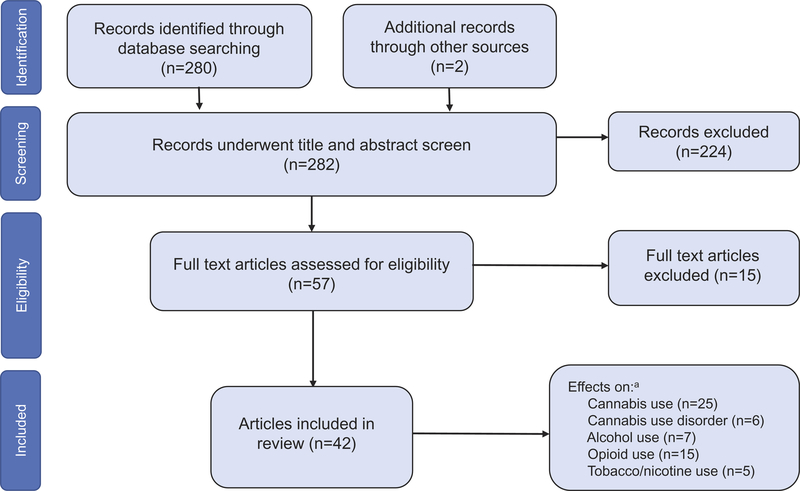
Our search yielded 280 distinct articles, and we identified two additional studies through hand-searching reference lists of relevant studies. After screening and full-text review, 42 studies met our inclusion criteria noted above and were included in this review (see Figure 2). MCLs were the most commonly evaluated policy (n = 37) with a smaller set of studies evaluating RCLs (n = 9). Most studies evaluated the effects of cannabis laws on cannabis use (n = 25) or opioid-related outcomes (n = 15), with fewer evaluating effects on alcohol use (n = 7), CUD (n = 7), and tobacco use (n = 5).
Figure 2.
Flow diagram of studies included in the review.
aCounts do not sum to 42 as many articles considered multiple outcomes within the same study.
Considering evidence for the effects of cannabis policy
Understanding how cannabis policies impact cannabis use is key to making subsequent causal claims about their effects on the use of other substances, but it is also an important question in and of itself. If liberalization does not impact cannabis use, but instead shifts some or all existing use (or potential use) from the illegal to legal market, then arguably such policies are welfare enhancing from a governmental perspective (e.g., increased tax revenues, reduced law enforcement expenditures) and from a consumer perspective (e.g., a safer and more consistent product). Even if liberalization increases cannabis use, the impact on risks or harms will depend on whether increased consumption occurs among populations whose use more strongly predicts subsequent harms (e.g., adolescents) or by leading to more problematic use patterns, such as persistent daily use (3).
Conceptually, cannabis liberalization, whether MCLs and RCLs, could influence consumption through several mechanisms, including changes in perceived harmfulness, social norms, prices, potential legal consequences, search costs of locating a supplier, and potential social stigma associated with participating in illegal activity (9–11). The extent to which particular mechanisms change in response to a policy and the timing of such changes depend on the specific provisions that comprise the law and how long it takes for particular provisions to influence cannabis markets. Laws that allow the proliferation of dispensaries or that grant legal cannabis access to a broader segment of the population, for example, are likely to have greater impacts on perceptions and norms (as well as access) than laws that are more restrictive. Similarly, while perceptions, social norms, and legal risks may change immediately upon passage of a law, changes in price and access depend more directly on the size and structure of the supply-side of the legal market. Thus, effects on access and price often take time to emerge, particularly if there are regulatory controls or legal risks that constrain supply (12–16). The implication of this is that studies that examine the impact of liberalization policies by focusing on when a law became effective or when the first store opens likely do not capture the full influence of when the market became “present” within the state and hence likely miss some of the more relevant impacts associated with norms, availability, and cost.
The effects of cannabis policy on cannabis use outcomes
Effects of medical cannabis laws on cannabis use
Several reviews summarizing the literature for the effects of MCLs on cannabis use and use disorders have drawn markedly similar conclusions (12,17–24), namely that the passage of MCLs has little or negative impact on the prevalence of cannabis use among adolescents but may increase use prevalence among adults aged 21 years and older.
Table 1 lists the 22 studies that met our inclusion criteria and estimated the effects of MCLs on cannabis use. All examined past-month or past-year cannabis use, with about half (n = 13) examining use frequency. Most studies (n = 16) evaluated effects on adolescent use, with fewer considering youths and young adults (n = 6) or adults (n = 7). Eight studies allowed for heterogeneous effects of cannabis policies depending on their specific provisions and five tested for lagged effects of MCLs on cannabis use.
Table 1.
Included studies of the effects of medical cannabis laws (MCLs) on cannabis use.
| Study (study year) | Data (years) | Population | Unit of analysis |
Policy provisions |
Lagged effects |
Use outcomes | Findings for any MCL, no lags |
Findings for effects of MCL provisions or lagged effects |
|---|---|---|---|---|---|---|---|---|
| Adolescents | ||||||||
| Keyes et al. (2016) | MTF (1992–2014) | Grades 8, 10, 12 | Individual | Yes | No | Past-month use Use frequency | (−) grade 8 (0) grades 10 and 12 | No difference whether dispensaries considered |
| Hasin et al. (2015) | MTF (1991–2014) | Grades 8, 10, 12 | Individual | Yes | Yes | Past-month use Past-year use Use frequency | (−) grade 8 (0) grades 10 and 12 | No difference whether dispensaries considered Similar findings whether treated MML as turning on one- or two-years post-passage |
| Cerdá et al. (2018) | MTF (1991–2015) | Grades 8, 10, 12 | Individual | No | Noa | Past-month use | (−) grade 8 (0) grades 10 and 12 | |
| Lynne-Landsman et al. (2013) | YRBSS (2003–2009) | Grades 9–12 | Individual | No | No | Past-month use Lifetime use Use frequency | (0) all use measures | |
| Choo et al. (2014) | YRBSS (1991–2011) | Grades 9–12 | Individual | No | No | Past-month use | (0) any use | |
| Johnson et al. (2017) | YRBSS (1991–2011) | Grades 9–12 | Individual | Yes | Yes | Past-month use Use frequency | (−) any use (0) heavy use | Allowance for 2.5 oz (+) any use; allowance of voluntary registry (+) any use and heavy use; (0) for dispensary provision index and home cultivation; stronger effects with lags |
| Johnson et al. (2018) | YRBSS (1991–2011) | Grades 9–12 | Individual | Yes | No | Past-month use Use frequency | (−) ale + cannabis (0) cannabis, no ale | No difference if consider “more restrictive” vs. “less restrictive” category |
| Anderson et al. (2015) | YRBSS (1993–2011) | Grades 9–12 | Individual | No | No | Past-month use Use frequency | (0) any or frequent use | |
| Coley et al. (2019) | YRBSS (1999–2015) | Grades 9–12 | Individual | No | Yes | Past-month use Use frequency | (−) any use (0) heavy use | Stronger effects when consider lags No difference from main effect for >2.5oz |
| Wall et al. (2016) | NSDUH (2002–2008) | Ages 12–17 | State | No | No | Past-month use | (0) any use | |
| Harper et al. (2012) | NSDUH (2002–2009) | Ages 12–17 | State | No | No | Past-month use | (0) any use | |
| Wall et al. (2011) | NSDUH (2002–2008) | Ages 12–17 | State | No | No | Past-month use | Higher use in MCL states pre and post | |
| Stolzenberg et al. (2016) | NSDUH (2002–2011) | Ages 12–17 | State | No | No | Past-month use | (+) any use | |
| Martins et al. (2016) | NSDUH (2004–2013) | Ages 12–17 | Individual | No | No | Past-month use | (0) any use | |
| Williams et al. (2017) | NSDUH (2004–2013) | Ages 12–17 | State | Yes | No | Past-month use Use frequency | (0) any use | (–) for heavy use only in “medicalized” states |
| Mauro et al. (2019) | NSDUH (2004–2013) | Ages 12–17 | Individual | No | No | Past-month use Use frequency | (0) any use or daily use | |
| Youth and young adults | ||||||||
| Wen et al. (2015) | NSDUH (2004–2012) | Ages 12–20 | Individual | Yes | Yes | Past-month use Use frequency Initiation | (0) any use or use frequency (+) initiation | Retail dispensaries have (+) effects on any use; tests for lagged effects on past-month use show (0) effect |
| Pacula et al. (2015) | NLSY (1997–2005) | Ages 12–20 | Individual | Yes | Nob | Past-month use Use frequency | (0) any use, heavy use (+) days use | Requiring registries (+) use, heavy use, days use Home cultivation (–) use, heavy use, days use |
| Pacula et al. (2015) | NLSY (1997–2011) | Ages 12–32 | Individual | Yes | Nob | Past-month use Use frequency | (0) any use and use frequency | Retail dispensaries have (+) effects on any use |
| Young adults | ||||||||
| Harper et al. (2012) | NSDUH (2002–2009) | Ages 18–25 | State | No | No | Past-month use | (0) any use | |
| Williams et al. (2017) | NSDUH (2004–2013) | Ages 18–25 | State | Yes | No | Past-month use Use frequency | (0) any use and heavy use | (0) for medicalized and for non-medical laws |
| Martins et al. (2016) | NSDUH (2004–2013) |
Ages 18–25 |
Individual | No | No | Past-month use | (0) any use | |
| Mauro et al. (2019) | NSDUH (2004–2013) |
Ages 18–25 |
Individual | No | No | Past-month use Use frequency |
(0) any use (+) daily use, men |
|
| Adults | ||||||||
| Hasin et al. (2017) | NLAES/NESARC (1991–1992; 2001/2002; 2012/2013) | Ages 18+ | Individual | Yes | No | Past-year use | (+) any use | Effects found for both early- and late-enacting MCLs, except California showed no effects and Colorado showed delayed effects |
| Choi et al. (2019) | NSDUH (2002–2015) | Ages 18+ | State | No | Yes | Past-month use | (+) any use | Some evidence of lagged effects, but pattern is non-monotonic |
| Wen et al. (2015) | NSDUH (2004–2012) | Ages 21 + | Individual | Yes | Yes | Past-month use Use frequency Initiation | (+) any use, daily use (0) use days | use (0) initiation | Nonspecific pain drives (+) use and daily use; evidence of 6-month lag after implementation for ages 21 + |
| Harper et al. (2012) | NSDUH (2002–2009) | Ages 26+ | State | No | No | Past-month use | (0) any use | |
| Williams et al. (2017) | NSDUH (2004–2013) | Ages 26+ | State | Yes | No | Past-month use Use frequency | (+) any use (0) heavy use | (+) any use only for “non-medical” laws; (0) for “medicalized” laws |
| Martins et al. (2016) | NSDUH (2004–2013) | Ages 26+ | Individual | No | No | Past-month use | (+) any use | |
| Kerr et al. (2018) | NAS (1984/1990/ 1995; 2000/2005/ 2010/2015) | Ages 18+ | Individual | Yes | No | Past-year use | (0) any use | No effect for allowing home cultivation or dispensaries (negative effects in some specifications) |
| Mauro et al. (2019) | NSDUH (2004–2013) | Ages 26+ | Individual | No | No | Past-month use Use frequency | (+) any use and daily use | |
Significant effects (p < 0.05) and direction indicated with (+) or (−), while (0) indicates insignificant effects. MTF: Monitoring the Future; YRBSS: Youth Risk Behavioral Surveillance System; NSDUH: National Survey of Drug Use and Health; NLSY: National Longitudinal Survey of Youth; NLAES: National Longitudinal Alcohol Epidemiologic Survey; NESARC: National Epidemiologic Survey on Alcohol and Related Conditions; NAS: National Alcohol Study.
Cerdá et al. (2018) do not model lagged effects of MCLs but test for whether MCL states experienced changes in use following the 2008/2009 change in federal enforcement policy. However, because they do not model this potential moderator of effects only for states with MCLs as of the time of the federal change, moderating effects are confounded with potential preexisting trends in states that passed MCLs subsequent to the federal change, and thus, it is difficult to interpret these effects as capturing either heterogeneous policy or time-varying effects.
While Pacula et al. (2015) present event study analyses that account for lagged effects; they do not provide inferential statistics for these lagged effects and are thus not counted as estimating lagged effects.
Based on current evidence, we largely concur with the conclusions of other reviews. Results for adolescents under age 18 are highly consistent in showing negative or insignificant effects of MCL enactment on the prevalence of use (25–39), with the exception of one study that found increases in use (40) but was later shown to have used a model that produced biased estimates (28). The relatively few studies that considered the specific provisions of MCLs, such as allowances for dispensaries, have also found little evidence that such provisions matter for adolescent use outcomes (25,30,35,38); only one study found that allowing higher possession limits for cannabis and voluntary versus mandatory registration of medical cannabis patients resulted in increased cannabis use among adolescents (31).
However, two studies that evaluated MCL effects on youth aged 12–20 suggest that MCLs may have impacted some aspects of youth cannabis use. Analyzing data from 2004 to 2012, Wen et al. (41) found that MCL passage was associated with significant increases in youth initiation of cannabis use. Another study evaluating an earlier timeframe (1997–2005) found that MCL passage significantly increased the number of days of cannabis use among youth aged 12–20 but did not increase the likelihood of past-month use (42). It may be that MCL passage results in short-term experimentation with cannabis use among youth or that early state adopters had laws with more salience for consumption among existing youth users.
Findings for adults are more consistent in showing increases in cannabis use following MCL enactment (34,35,39,41,43,44), with the exception of two studies that found insignificant effects: an early study (33), which only included data through 2009, and a recent study that used an age-period-cohort framework instead of methods better suited for causal inference (45). Of note, significant increases in cannabis use following MCL enactment have generally not been found in subgroup analyses of adults aged 18–25, although one study (39) found MCLs increase daily cannabis use among men aged 18–25. Additionally, studies that have considered specific provisions of MCLs indicate that increases in adult use are more pronounced for states that adopted laxer policies (35,41–43), such as by allowing retail dispensaries or including nonspecific pain as a qualifying condition.
Before discussing the literature on effects of RCLs on cannabis use, it is worth noting several key points about the MCL literature. First, while similar findings across 16 adolescent studies seem highly robust, these studies draw on evidence from the same three datasets – two school-based surveys and one household-based survey – evaluated over largely the same time periods. Studies of the effects on adult use have faced similar data limitations, with all but two studies (43,45) relying on evidence from a single household survey. Given the same datasets and timeframes evaluated, results across multiple studies cannot be treated as independent estimates.
Furthermore, most studies used a version of the difference-in-differences estimation technique, which implicitly assumes that the effects of MCL enactment are immediate and similar across states. Studies have begun to address the fact that the specific provisions of MCLs have varied substantially both across states and within states over time (12,16,42,46), although the use of different taxonomies to characterize variation in MCLs (15,16,47,48) complicates pooling findings across these newer studies. Still, studies have tended to find that “laxer” MCL provisions generate larger effects on adult cannabis use and daily use (35,41–43). Allowing dispensaries may also increase youth cannabis use (41,42), although these effects have not been found for school samples of adolescents (25,31,38).
Less attention has been given to the potential dynamic effects of MCLs. While the few studies (n = 5) that modeled lagged policy effects tend to show no evidence that including lags alters their overall conclusions (31,37,38,41,44), the common methods for operationalizing delayed policy effects (i.e., linear effects from time of enactment, a set of lagged indicators) assume that implementation delays are homogeneous across heterogeneous policy designs and that the time course of such delays is uncorrelated with both the local and federal context (49), yet time series of medical cannabis patient take-up suggest this is likely not the case (15,50).
Effects of recreational cannabis laws on cannabis use
Given how recently RCLs have been implemented, only a few studies have attempted to evaluate their impact on cannabis use. Five studies published within our review window assessed their effects on cannabis use among school samples of adolescents (51), college students (52–54), or adults (45). Findings are mixed, showing increased use prevalence among youth in some states (Washington and Oregon) but not in others (Colorado) and insignificant effects for adults. However, these early studies are subject to several limitations. First, they estimate the impact of RCLs using the effective date of the law, which will not account for the full impact of the policy as retail stores have consistently opened one or two years later. Relatedly, these studies rely on data that cover a relatively short period following RCL enactment, but short-run changes in cannabis consumption may not accurately reflect longer-run effects once markets stabilize. Indeed, studies have shown that RCLs result in short-term increases in cannabis prices and price volatility, followed by significant price declines as the market stabilizes (55,56). Finally, the three RCL states that inform most evidence to date (Washington, Colorado, and Oregon) all had robust medical markets in place, and the identification of a proper comparison group for these first movers is just as important as the length of time considered for evaluating their effects. It would be premature to assume that the effects of their laws will generalize to other states which might adopt different regulatory standards or that had less commercialized medical cannabis markets (i.e., those that only allowed for home cultivation or distribution by nonprofit organizations).
Effects of cannabis laws on cannabis use disorders
Seven studies that met our inclusion criteria evaluated how MCLs affect CUD, CUD treatment admissions, or CUD hospitalizations. These studies have generated mixed results depending on how the policies are operationalized, how the outcome is measured, and the time period analyzed. Early studies evaluating MCLs passed before 2010, and treatment admissions for CUD found mixed evidence, with insignificant, significant positive, or significant negative effects depending on the model specification or the exclusion of specific states (32,57). Later work that examined two later years of data and distinguished between provisions of state MCLs found that it was only states allowing dispensaries that experienced significantly higher rates of treatment admissions for CUD, both overall and specifically for youth (42). Other studies that have considered MCL effects using self-reported measures of CUD over a longer timeframe have supported that MCLs are associated with increased prevalence of CUD among adults, with some evidence of lagged effects and more pronounced effects in states that allowed dispensaries or collective cultivation (41,43). This relationship has not translated into increased risk of hospitalization for CUD (58) and appears to have weakened with the more recent “medicalized” policies (35). Overall, we are just beginning to understand the implications of cannabis liberalization on CUD and lifetime trajectories of cannabis use.
Effects of laws on products consumed
While most studies examining the impacts of cannabis policies focus on measures of use prevalence, a nascent literature is evaluating what gets used. Considerable evidence from the US supports that commercialization of cannabis has significantly impacted the types of cannabis available and the ways in which it is consumed. Cannabis potency, product variety, and methods of consumption have evolved as suppliers have innovated under the legal protections granted by MCLs and, more recently, RCLs. Consequently, cannabis users in liberalized states consume a different product mix than users in other states. Adults living in states with MCLs, particularly those with higher density of dispensaries, are significantly more likely to vaporize or ingest marijuana products compared to individuals in states without such laws (59). Adolescents in liberalizing states are also more likely to report lifetime use of vaporized and edible cannabis products, particularly in states where the laws had been in place for longer or where there was a higher density of dispensaries (60). Results from an Internet survey found nearly five times the odds of cannabis concentrate use among individuals living in states with RCLs and nearly twice the odds among individuals living in “laxer” (i.e., less medicalized) MCLs (61).
While the increased availability of alternative non-smoked routes of administration for cannabis could generate potential health benefits through reduced adverse respiratory symptoms (62,63) and lower expired carbon monoxide exposure (64), the types of products that are consumed orally or vaporized are often substantially more potent than smoked cannabis products. Cannabis concentrates, documented to have delta-9-tetrahydrocannabinol (THC) concentrations in excess of 70% (65), are the fastest growing share of the retail cannabis market in Washington (56). The use of higher potency products could offset the positive benefits associated with a move away from combustible use, as higher THC is more strongly associated with negative health impacts including acute cognitive effects and psycho-motor impairments (66,67), brain development and functioning (68), use disorders (69), and psychosis (70,71).
Evidence suggests that states that legally permit medical cannabis dispensaries experience significant increases in average THC levels (72), and the THC concentration of cannabis products sold through medical and recreational dispensaries greatly exceeds that previously seen in illegal markets (73,74). This evolution in the diversity of cannabis products and routes of administration under commercial cannabis regimes has implications for understanding the nature of the potential harms and benefits of these policies. It also provides new opportunities for establishing protections—particularly to naive users and children—that go beyond what states have considered thus far.
The effects of cannabis policy on other substance use
The overall public health benefits or harms of cannabis legalization may hinge critically on the extent to which cannabis is a substitute or complement for other substances that carry the risk of chronic or acute harm. Indeed, a series of reports describe how the cannabis-specific net benefit associated with legalization based on cannabis’ known health and productivity effects is likely to be dwarfed by the possible costs or benefits that would emerge if cannabis was either a complement or substitute, respectively, to alcohol (75,76). More recent attention has focused on the potential role of cannabis legalization for generating societal benefits by reducing opioid-related harms (77–79).
Below, we review the evidence from state policy evaluations for how cannabis liberalization has affected the use of alcohol, opioids, and tobacco or other nicotine products. However, it is important to keep in mind the limitations of the previously reviewed literature as they also apply here. Moreover, because the change in the legal status of cannabis has caused stark cannabis price declines (56,80–81), it is important that studies assessing the relationship between various substances and cannabis base conclusions on changes in relative prices of both goods and give proper consideration to likely income effects. We may not be able to presume incomes are held constant in several markets where substantial price declines for cannabis are occurring.
Cannabis policy and alcohol
Seven studies met our inclusion criteria, five of which evaluated MCLs (26,30,41,82,83) and two of which evaluated RCLs (52,53). All used data that considered some measures of self-reported alcohol use in the past month and most considered binge drinking (Table 2).
Table 2.
Included studies of the effects of medical cannabis laws (MCLs) and recreational cannabis laws (RCLs) on alcohol use.
| Study | Data (years) | Population | Unit of analysis |
Policy provisions |
Lagged effects |
Outcome measures | Findings for effects of MCL or RCL policy measures | Other state policies adjusted for |
|---|---|---|---|---|---|---|---|---|
| Medical cannabis laws | ||||||||
| Cerdá et al. (2018) | MTF (1991–2015) | Grades 8, 10, 12 | Individual | No | Noa | Binge drinking in past month | MCL (−) binge drinking among grade 8; (0) effect for grade 10 or grade 12 | Per gallon beer excise tax |
| Johnson et al. (2018) | YRBSS (1991–2011) | Grades 9–12 | Individual | Yes | No | Past-month alcohol use (overall, with or without past-month cannabis use); binge drinking past month | MCL (−) past-month alcohol use and use of both alcohol and cannabis; less restrictive MCL also saw (−) binge drinking and (−) alcohol use without cannabis | None mentioned |
| Wen et al. (2015) | NSDUH (2004–2012) | Ages 124– | Individual | Yes | Yes | # drinks in past month; # binge days past month; past-month cannabis use and binge drinking; simultaneous cannabis and alcohol use; alcohol use disorder | For ages 12–20, (0) effect of MCL or MCL provisions. For ages 21+, MCL (+) binge days, cannabis use plus binge drinking, and simultaneous use of cannabis and alcohol; effects driven by MCLs with provisions for nonspecific pain. (0) effect alcohol use disorder. | Beer excise tax; % ad valorem tax (on-premise); % ad-valorem tax (off-premise) |
| Anderson et al. (2013) | BRFSS (1993–2010) | Ages 18+ | Individual | No | No | Past-month alcohol use; number of drinks past month; binge drinking | MCL (0) overall effect on all alcohol use measures; some evidence of (−) effects on some use measures for 18–39 and 50–59 age group when stratify by age | BAC 0.08 law; decriminalization; beer tax; zero tolerance laws |
| Brewer’s Almanac (1990–2010) | All sales | State | No | No | Per capita beer sales, wine sales, and spirits sales | MCL (−) beer sales, (0) wine and spirits sales | ||
| FARS (1990–2010) | Ages 15+ | Individual | No | Yes | Traffic fatalities involving positive blood alcohol content (BAC) | MCL (−) traffic fatalities involving BAC >0.10; Three- year lagged (−) effects for BAC >0 and BAC >0.10. | ||
| Sabia et al. (2017) | BRFSS (1990–2012) |
Ages 18+ | Individual | Noa | Nob | Past-month alcohol use; past-month binge drinking | MCL (0) overall effect on past-month use but (−) effect for ages 18–24. MCL (−) overall effect on binge drinking, with larger effects for 18–24 and 35+ |
Beer tax, cigarette tax, cannabis decriminalization |
| Recreational cannabis laws | ||||||||
| Kerr et al. (2017) | HMS (2012–2016) | College students | Individual | No | No | Past-month alcohol use; heavy alcohol use in past two weeks | RCL had (0) effect heavy alcohol use. However, RCL (+) cannabis use only among those reporting heavy alcohol use |
None mentioned |
| Kerr et al. (2018) | NCHA (2008–2016) | College students | Individual | No | No | Past-month alcohol use | RCLS had (0) effect on alcohol use | None mentioned |
Significant effects (p < 0.05) and direction indicated with (+) or (−), while (0) indicates insignificant effects. MTF: Monitoring the Future; YRBSS: Youth Risk Behavioral Surveillance System; NSDUFI: National Survey of Drug Use and Health; NLSY: National Longitudinal Survey of Youth; NLAES: National Longitudinal Alcohol Epidemiologic Survey; BRFSS: Behavioral Risk Factor Surveillance System; HMS: Healthy Minds Study; NCHA: National College Health Assessment.
Cerdá et al. (2018) test for whether MCL states experienced changes in use following the 2008/2009 change in federal enforcement policy but did not model this potential moderator of effects only for states with MCLs as of the time of the federal change; thus, moderating effects are confounded with potential preexisting trends in states that passed MCLs subsequent to the federal change, and we cannot interpret these effects as capturing either heterogeneous policy or time-varying effects.
Sabia et al. (2017) consider policy provisions and lagged effects for their primary analyses on body weight but not for the alcohol use models.
Two studies evaluated the impact of MCLs on middle- and high-school students and found that MCL law passage had either a negative or no significant association with past-month alcohol use and binge drinking (26,30). Another study examining youth under age 21 also found no statistical association between MCLs or laxer MCL provisions and self-reported drinking prevalence, binge drinking, or number of drinks consumed in the past month (41). It is challenging to draw conclusions about substitution or complementarity of alcohol with cannabis among adolescents from this body of research. Studies that find negative effects of MCLs on alcohol use among adolescents also find negative effects on cannabis use, which would suggest complementarity; however, estimated declines in adolescent drinking among both cannabis users and abstainers suggest that seeming negative effects of MCLs on underage drinking may actually be unrelated to the law.
Findings regarding the association between MCLs and alcohol use among adults are similarly inconclusive. Two studies examining overlapping time periods from the same dataset show that MCLs have no association with drinking prevalence among adults overall (18 years and older) but may significantly reduce binge drinking, at least among certain age groups (82,83). One study using data from 1990 to 2010 also supported evidence of reductions in self-reported alcohol use by showing significant declines in per capita beer sales (but not wine or spirit sales) and declines in traffic fatalities where a driver had a positive blood alcohol content; changes in traffic fatalities occurred with a three-year lag post-MCL implementation. However, this evidence of a reduced alcohol use following MCL adoption is inconsistent with findings from Wen et al. (41), which conducted the most comprehensive assessment of the impact of MCLs on alcohol consumption. Using individual-level data from 2004 to 2012, they find that dichotomous measures of MCLs are not associated with past-month prevalence or quantity consumed among adults but that frequency of binge drinking and simultaneous use of alcohol with cannabis were positively associated with less restrictive MCLs.
With respect to RCLs, we identified two studies, both of which examine how Oregon college students’ use of cannabis and alcohol changed after RCL enactment, relative to students in non-legalizing states (52,53). The studies found no direct impact of RCL enactment on drinking overall but suggest a significant interaction between RCL and binge drinking, with binge drinking students in Oregon being 73% more likely to report past-month cannabis use than their counterparts in non-RCL states. The authors evaluated outcomes before and after July 2015 when RCL was implemented in Oregon; since cannabis sales began in October 2015, they were unable to differentiate the effect of retail availability from RCL enactment.
There are several reasons why one cannot draw conclusions from these two RCL studies. First, they examine legalization in only one state, and these findings may not generalize to other RCL contexts. Second, while both studies had adequate pre-policy data, they had only one year of post-policy data. The long-run effects of policy changes may or may not be the same as the short-run effects, particularly if increased competition among legal cannabis retailers or producers leads to further price declines. Additionally, because the authors did not have state identifiers for the non-RCL institutions, they were unable to control for other alchol policies that might have differed across the states.
This latter concern applies to the entire literature evaluating impacts of cannabis liberalization on alcohol consumption. The literature has yet to develop a consistent way of accounting for the broader alcohol policy environment, let alone alcohol policy changes that may be occurring at the same time as cannabis liberalization. With some exceptions (82), studies only include a measure of the beer tax to control for variation in the alcohol policy environment. However, as shown in other work (84), beer taxes are but one aspect of the overall alcohol policy environment, and they are not necessarily a good indicator of how restrictive a given state is in its regulation of alcohol, particularly given how little they have changed during the time periods being examined here. Future work needs to do a better job of representing the restrictiveness of both the alcohol and cannabis environment in order to draw clearer conclusions.
Cannabis policy and opioids
Alongside exponential growth in opioid mortality over the past two decades, there has been increased interest in the therapeutic potential of cannabinoids as an alternative to opioid analgesics for the treatment of chronic pain. The potential for cannabis to reduce opioid-related harms depends critically on its ability to effectively manage pain, an issue that is far from settled by the current state of clinical and epidemiological research (3,85–87). While surveys of medical cannabis patients show many reports using cannabis as an alternative or adjunctive approach to prescription pain medications (88–90), recent analyses of a nationally representative household survey indicate that medical cannabis users are significantly more likely to report medical and nonmedical use of prescription pain relievers than individuals who are not using cannabis medicinally (91). Combined with limitations of the few existing clinical studies (85), it remains unclear whether increased availability of cannabis will reduce the misuse of and harms from opioids.
Several state policy evaluations have sought to provide insight on this issue (Table 3) by assessing the effects of MCLs or RCLs on opioid-related mortality (n = 3), adverse events (n = 4), misuse (n = 2), and prescribing (n = 7).
Table 3.
Included studies of the effects of medical cannabis laws (MCLs) and recreational cannabis laws (RCLs) on opioid use and related outcomes.
| Study | Data (years) | Population | Unit of analysis |
Policy provisions |
Lagged effects |
Outcome measures | Findings for effects of MCL or RCL policy measures |
Other cannabis or opioid policies included |
|---|---|---|---|---|---|---|---|---|
| Medical cannabis laws and opioid mortality | ||||||||
| Bachhuber et al. (2014) | WONDER (1999–2010) | All ages | State | No | Yes | Age-adjusted opioid analgesic overdose mortality rate | (−) mortality, effects strengthened over time | PDMP, patient ID laws, pain clinic laws |
| Phillips & Gazmararian (2017) | WONDER (2011–2014) | All ages | State | No | Yes | Age-adjusted opioid-related overdose mortality rate capita | (+) mortality, effects strengthened over time; high-CBD laws had (0) effect; MCL and PDMP interacted to (−) mortality | Must-access PDMP, high-CBD laws |
| Powell et al. (2018) | NVSS (1999–2013) | All ages | State | Yes | Yes | Prescription opioid involved mortality rate | (0) effect of MCLs; but active and legal dispensaries (−) mortality | Must-access PDMP, pill mill laws |
| Medical cannabis laws and opioid adverese events | ||||||||
| Powell et al. (2018) | TEDS (1999–2012) | All ages | State | Yes | Yes | Treatment admissions for prescription opioids or heroin | (0) effect of MCLs; but active and legal dispensaries (−) treatment admissions | Must-access PDMP, pill mill laws |
| Shi (2017) | SID (1997–2014) | All ages | State | Yes | Yes | Rates of hospital discharge for opioid use disorder, overdose | (−) effect of MCLs, effects strengthened over time. No additional impact of dispensaries. | Decriminalization, PDMP, pain clinic regulations |
| Kim et al. (2016) | FARS (1999–2013) | Ages 15+ | State | Yes | No | Fatally injured drivers testing positive for opioids | Operational MCL had (0) association overall, but (−) for drivers aged 21–40 | Multiple PDMP provisions |
| Chu (2015) | UCR (1992–2011) | Ages 18+, men | Incident or State | Yes | Yes | Arrests for cocaine and heroin in cities with >25,000 pop, as well as state rates | MCLs and allowing dispensaries have (0) effect. Lagged policy indicators show delayed (−) effect that grows with time. | Decriminalization |
| Chu (2015) | TEDS (1992–2011) | Ages 18+, men | Incident or State | No | No | Treatment admission rates for heroin use disorder | MCLs (−) heroin-related primary treatment admissions | Decriminalization |
| Medical cannabis laws and opioid misuse | ||||||||
| Wen et al. (2015) | NSDUH (2004–2012) | Ages 12 + | Individual | Yes | Yes | Past year nonmedical use of pain reliever medication | (0) effect of MCLs or MCL provisions. 1-year lags and 2-year lags are not significant. | Decriminalization |
| Cerdá et al. (2017) | MTF (1991–2015) | Grades 8, 10, and 12 | Individual | No | No | Past-month nonmedical use of prescription opioid | (−) grade 8; (0) grade 10; (+) grade 12 | None mentioned |
| Medical cannabis laws and opioid prescribing and distribution | ||||||||
| Bradford & Bradford (2016) | Medicare Part D (2010–2013) | Eligible Medicare enrollees | Physician | Yes | No | Average number daily doses filled for Rx drugs for pain per physician | (−) effect of MCLs on drugs used to treat pain | None mentioned |
| Bradford et al. (2018) | Medicare Part D (2010–2015) | Eligible Medicare enrollees | State | Yes | No | Number of daily doses for any opioid prescription | (0) effect of any MCL. Large (−) effect of MCL with open dispensaries, smaller but (−) impact for only home cultivation. Largest effect for morphine. | RCL, presence of an electronic PDMP |
| Liang et al. (2018) | SDUD (1993–2014) | Eligible Medicaid enrollees | State | Yes | No | Number filled opioid Rx, dosage of filled opioid Rx, and Medicaid spending on opioid Rx | MCLs (−) number of Rx opioids, dosage, and Medicaid spending related to Schedule III opioids only. (0) effect on Schedule II opioids. Also (0) effect of dispensaries | Presence of an electronic PDMP, RCL, ACA Medicaid expansion, decriminalization |
| Bradford & Bradford (2017) | SDUD (2007–2014) | Eligible Medicaid enrollees | State | Yes | No | Average number of daily doses of prescription drug dispensed per enrollee | (−) effect for drugs to treat nausea, seizures, depression, pain, psychosis. (0) effects for drugs to treat anxiety, glaucoma, sleep disorders, spasticity. | Any PDMP, RCL, ACA Medicaid expansion |
| Wen & Hockenberry (2018) | SDUD (2011−2016) | Eligible Medicaid enrollees | State | No | No | Opioid prescribing rate per-Medicaid enrollees | (−) opioid prescribing, with largest effects on Schedule III—V vs. Schedule II opioids. | # of buprenorphine-waivered physicians, any PDMP, pain clinic regulations, ACA Medicaid expansion, RCL |
| Shah et al. (2019) | IMS Lifelink+ (2006−2014) | Eligible enrollees | Individual | Yes | No | Use of at least one opioid Rx in a year; 90+ days use within past 180 days; high-risk use | (−) all use measures; similar effects if define MCL as opening date of dispensaries for states banning home cultivation | Any PDMP, pain clinic laws |
| Powell et al. (2018) | ARCOS (1999–2013) | All ages | State | Yes | Yes | # of opioids distributed to the state for medical purposes | Neither MCL or active & legal dispensaries influence distribution of opioids. | Must access PDMP, pill mill laws |
| Recreational cannabis laws and opioid prescribing | ||||||||
| Bradford et al. (2018) | Medicare Part D (2010–2015) | Eligible Medicare enrollees | State | Yes | No | Number of daily doses for any opioid Rx, by opioid type | RCL had (−) effect overall, driven by reduced fentanyl doses | MCL, presence of an electronic PDMP |
| Liang et al. (2018) | SDUD (1993–2014) | Eligible Medicaid enrollees | State | Yes | No | Opioids: # filled prescriptions, dosage, Medicaid spending | (0) effect of RCL laws on all outcomes | Electronic PDMP, ACA Medicaid expansion, MCL, decriminalization |
| Bradford & Bradford (2017) | SDUD (2007–2014) |
Eligible Medicaid enrollees | State | Yes | No | Average # daily doses of prescription drug dispensed per Medicaid enrollee | RCLs (−) drugs to treat pain as well as all other drugs, including those used in falsification test | Any PDMP, MCL, ACA Medicaid expansion |
| Wen & Hockenberry (2018) | SDUD (2011–2016) | Eligible Medicaid enrollees | State | No | No | Opioid prescribing rate per-1000 Medicaid enrollees | RCL (−) opioid prescribing, driven by Schedule II; also (−) nonopioid pain medications | # of buprenorphine-waivered physicians, any PDMP, pain clinic regulations, ACA Medicaid expansion, MCL |
| Shi et al. (2019) | SDUD (2010–2017) | Eligible Medicaid enrollees | State | No | No | Number of opioid Rx per 100 Medicaid enrollees | RCLs (−) Schedule III opioids in some specifications but (0) effect on Schedule II. When compared to just states with MCLs, RCLs had (0) effect on Schedule III opioids. | MCL, any PDMP, ACA Medicaid expansion |
Significant effects (p < 0.05) and direction indicated with (+) or (−), while (0) indicates insignificant effects. WONDER: CDC’s Wide-ranging Online Data for Epidemiological Research interface to the multiple causes of death (MCOD) data; NVSS: National Vital Statistics System; TEDS: Treatment Episode Data System, produced by the Substance Abuse Mental Health Services Administration (SAMHSA); SID: State Inpatient Database; FARS: Fatal Accident Reporting System; UCR: Uniform Crime Reports, produced by the Federal Bureau of Investigation; MTF: Monitoring the Future; ARCOS: Automation of Reports and Consolidated Orders System; SDUD: Centers for Medicare & Medicaid Services (CMS) State Drug Utilization Data; NSDUH: National Survey on Drug Use or Health, produced by SAMHSA; Medicare Part D: CMS Medicare Part D Prescription Drug Event Analytic File; PDMP: Prescription Drug Monitoring Program.
While a 2014 study showing a large, negative association between MCLs enacted from 1999 to 2010 and opioid analgesic mortality (78) received substantial media attention, two subsequent papers raise doubts regarding the robustness of these findings. Powell et al. (79) showed that extending the analysis period through 2013 removed the statistical significance of the MCL policy variable; cannabis dispensaries remained negatively and statistically associated with opioid overdose deaths but that effect too was mitigated over time. Another study using data from a later time period (2011–2014) found a positive association of MCLs with opioid mortality (92). The switch in signs is not simply a function of the short time period being examined as another paper (released after our literature search was completed) showed a similar reversal in the relationship between MCLs and opioid mortality over the full period covering 1999–2017 (93), suggesting that omitted variable bias may be causing spurious correlation.
Studies examining impacts of cannabis liberalization policies on other opioid-related harms—opioid-related hospital inpatient stays (58), treatment episodes for opioid use disorder (79,94), and opioid positivity among fatally injured drivers (95)—have all shown negative associations. None of these adverse event studies extend ana- lyses past 2014, however, and they likely suffer from the same omitted variable biases as none of these studies fully adjust for the wide range of state opioid policies adopted during this period. Furthermore, studies evaluating the direct effects of MCLs on self-reported opioid misuse have not generated strong evidence to support an interpretation that MCLs reduce nonmedical use of prescription opioids (26,41).
Perhaps, the greatest evidence suggesting a reduction in opioid misuse associated with cannabis liberalization policies comes from studies examining opioid prescribing in Medicare (n = 2), Medicaid (n = 4), and the commercially insured (n = 1). Of the seven studies examining this outcome, all find a negative correlation between either MCLs or RCLs and various measures of opioid prescribing (see Table 3) (96–102). However, the association between MCLs and various prescribing measures appears to decline in magnitude as additional years of data past 2014 are included in analyses, particularly when the Medicaid data are used. Furthermore, examination of the few RCL evaluations suggests that estimates of RCLs on opioids may be picking up some other aspect of states with these laws that relates to lower prescribing of nonopioid medications.
There are at least two additional concerns with this literature. First, Powell et al. (79) show no impact of MCLs on the distribution of opioid medication, raising questions on how to reconcile these disparate results. If patients are switching to medical cannabis, then both prescribing and distribution should decrease. Second, evaluations of the impact of cannabis laws on opioid prescribing, in particular, may not adequately consider private- or public-sector strategies aimed at reducing inappropriate opioid prescribing, overprescribing to new patients, and doctor shopping (103–105). These factors, which may be difficult to capture but are unlikely to be time persistent, may confound evidence observed in the claims data.
Cannabis policy and tobacco
There is a substantial and varied literature examining interactions between cannabis and tobacco or nicotine. Neurobiological research has indicated that the endocannabinoid system is a factor in the development of tobacco use disorder, and several studies support the role of nicotine in facilitating both pharmacological and behavioral effects of THC (106,107). Epidemiological studies consistently demonstrate a high prevalence of co-occurring cannabis and tobacco use (108), and evidence shows an upward trend in the co-use and co-administration of cannabis and tobacco products (109,110). While further research is needed to disentangle the mechanisms driving the relationship between cannabis and tobacco use, it is generally agreed that there is a link between the use of both substances (111).
Thus, it is surprising that the question of whether cannabis and tobacco are complements or substitutes has received little attention in the cannabis policy evaluation literature. Our search identified five studies that met our inclusion criteria and evaluated how MCLs (n = 3) or RCLs (n = 2) influence the use of tobacco products (Table 4). Using school survey data, Cerdá et al. (26) find puzzling results for the effect of MCLs on past-month cigarette use among adolescents. MCLs were associated with significant declines in both cigarette and cannabis use among eighth graders, suggestive of a complementary relationship; for older adolescents, however, MCLs significantly increase cigarette use but have no effect on cannabis use, suggesting that the estimated models are not picking up substitution or complementarity behavior but rather some other confounder. Another study of adolescents shows a significant negative relationship between MCLs and past-month cigarette use from 2009 to 2014 (112), but their models do not control for state fixed or random effects and thus likely reflect between-state differences rather than the causal effect of the laws within states.
Table 4.
Included studies of the effects of medical cannabis laws (MCLs) or recreational cannabis laws (RCLs) on tobacco use.
| Study | Data (years) | Population | Unit of analysis |
Policy provisions |
Lagged effects |
Findings for effects of MCL or RCL policy measures |
outcome measures | Other substance use policies included |
|---|---|---|---|---|---|---|---|---|
| Medical cannabis laws | ||||||||
| Cerdá et al. (2018) | MTF (1991–2015) | Grades 8, 10, 12 | Individual | No | Noa | Past-month use of cigarettes | (−) grade 8, (0) grade 10, (+) grade 12 | Per-pack state excise taxes on cigarettes |
| Dutra et al. (2018) | NYTS (2009–2014) | Grades 6–12 | Individual | No | Yes | Past-month use of cigarettes | (−) for MCL, but becomes insignificant when lag one year | Mandatory legal sales age for e-cigarettes; % population covered by smoke-free workplace laws; % population covered by smoke-free bar laws; average state per-pack cigarette tax |
| Choi et al. (2019) | NSDUH (2002–2015) | Ages 18+ | State | No | Yes | Past-month use of cigarettes | (0) effect of MCL except for evidence of (−) effect starting two years after implementation | Cigarette tax; beer tax; zero tolerance law; BAC 0.08 law; detailed clean indoor air law variables; cannabis decriminalization; RCL law |
| BRFSS (1990–2015) | Ages 18+ | Individual | Yes | Yes | Past-month cigarette use; daily use | (−) effect of MCL on past-month use; (0) effect daily use | ||
| CPS-TUS (1992–2015) | Ages 18+ | Individual | Yes | Yes | Past-month cigarette use; cigarettes used per day; days smoking | (−) effect of MCL on any use and cigarettes per day; (0) effect on days of smoking | ||
| Recreational cannabis laws | ||||||||
| Kerr et al. (2017) | HMS (2012–2016) | College students | Individual | No | No | Past-month cigarette use | (0) effect of Oregon’s RCL | None mentioned |
| Kerr et al. (2018) | NCHA | College students | Individual | No | No | Past-month composite tobacco use; use frequency | (−) effect of Oregon’s RCL, driven by decreases in less frequent tobacco use patterns (i.e., no effect on daily use) | None mentioned |
Significant effects (p < 0.05) and direction indicated with (+) or (−), while (0) indicates insignificant effects. MTF: Monitoring the Future; NYTS: National Youth Tobacco Survey; NSDUH: National Survey of Drug Use and Health; BRFSS: Behavioral Risk Factor Surveillance System; CPS-TUS: Current Population Survey Tobacco Use Supplements; HMS: Healthy Minds Study; NCHA: National College Health Assessment.
Cerdá et al. (2018) test for whether MCL states experienced changes in use following the 2008/2009 change in federal enforcement policy but did not model this potential moderator of effects only for states with MCLs as of the time of the federal change; thus, moderating effects are confounded with potential preexisting trends in states that passed MCLs subsequent to the federal change, and we cannot interpret these effects as capturing either heterogeneous policy or time-varying effects.
Choi et al. (44) instead evaluate the relationship between MCL enactment and cigarette smoking among adults using several survey datasets. Overall, their results suggest that MCL enactment is associated with a small but significant decrease in the prevalence of cigarette smoking among adults as well as declines in smoking intensity among daily smokers; they find no evidence that negative effects on cigarette smoking depend on specific MCL provisions. Combined with their finding that MCL enactment significantly increases cannabis use prevalence among adults, they conclude that cannabis and cigarettes are substitutes. Finally, two assessments of Oregon’s RCL suggest insignificant impacts on cigarette use among college students (53) but a significant decrease in tobacco use rates (52).
While these preliminary findings are reassuring (113), several factors complicate drawing firm conclusions for the relationship between cannabis and tobacco. First, recent increases in the prevalence of tobacco and cannabis co-use have been entirely driven by increased cannabis use among past-month tobacco users; tobacco use among past-month cannabis users actually declined (109). With declining tobacco use in the overall population, increased cannabis use among the small segment of the tobacco-using population can be easily dwarfed by a decline in the overall tobacco-using population unless co-use is specifically considered. Second, it is unclear whether studies evaluating the impact of cannabis laws sufficiently control for the overall state tobacco environment, in particular policies regulating e-cigarettes and vaping devices (see Table 4). Third, most studies to date have focused on how cannabis policies impact the use of tobacco cigarettes. However, there has been a large shift in nicotine consumption from cigarettes to e-cigarettes and vaping since 2013 (114), concurrent with a near-doubling in rates of nicotine and cannabis vaping among adolescents (115). Given the dramatic expansion in markets for electronic nicotine-delivery system devices (116,117), a consideration of these alternative nicotine-delivery devices is warranted.
Discussion
As cannabis policies have evolved, so too has the literature examining the impact of these policies on substance use. While recent evaluations of the effects of MCLs have begun to pay better attention to variability in specific policy provisions, issues remain due to lack of consideration of the length of time it takes for mature markets to emerge and fully influence perceptions, norms, prices, and product choice. The outcomes evaluated thus far have also been relatively limited; while we have a relatively large number of studies examining cannabis use prevalence or days of use on average, we know far less about how liberalization policies may impact specific patterns of cannabis use or co-use of various substances with cannabis.
Some of these limitations may be challenging to address. We have few large-scale representative systematic data collection efforts that capture information on cannabis use in its various forms, and those we do have often only provide crude measures of use. These systems, established prior to the rise of commercialized cannabis regimes, were not equipped to provide detail on the variety of consumption patterns that exist today. They also provide only limited information on polysubstance use, particularly with respect to simultaneous substance use. Similarly, we have limited data to assess the implementation and evolution of policies “on the ground.” For instance, the conclusions drawn from most previous studies—particularly those that claim operating dispensaries provide evidence on substitution or complementarity—rely on the assumption that the opening of the first cannabis dispensary serves as a sufficient indicator for cannabis access. In the absence of data to inform the time course of MCL implementation, such indicators have often been the best that researchers had to work with, yet we now know from the experience of both MCLs and RCLs that cannabis prices and availability evolve dramatically as more suppliers and retailers enter these legal markets over time (50,56,80–82).
The rise of legal cannabis markets under RCLs may help reduce some of these challenges. Legalization has brought with it large-scale administrative datasets with more detailed information on retail outlets, product purchases, potency, and price. These data bring their own set of challenges, but they may provide greater insights into how markets for cannabis evolve and how consumer behavior in the legal market changes alongside policy. Furthermore, with more detail on monetary prices of cannabis, future research may be able to more adequately assess how changes in the price for cannabis relate to changes in other substance use, offering greater insight into economic substitution or complementarity of cannabis with other substances.
However, evaluations of RCLs face some additional methodological complexity. Currently, all states with RCLs had preexisting MCLs, and many already had fairly robust cannabis distribution through medical dispensaries. Both the preexisting and co-occurring policy environments in RCL states are important to consider, as estimating RCL effects relative to the existing MCL environment may conflate heterogeneity in the “control” group of non-RCL states. Serious consideration needs to be given to what makes a state a reasonable control group, given that no state has moved from strict prohibition to RCL. Additionally, since the literature suggests MCLs (and some provisions of them) increase adult cannabis use, models of RCL effects need to account for this potential differential trend when constructing an appropriate comparison group; including dummy variables for MCL or MCL provisions may not be an adequate enough adjustment if MCLs lead to a shift in cannabis use trends and not just levels.
Finally, while this review was restricted to studies that use methods most appropriate to identifying causal effects of MCLs and RCLs, a fundamental limitation of the state policy evaluations meeting this criterion is that they are largely estimating population-level associations using information from multiple years of cross-sectional data. Thus, it is unknown whether observed population-level changes in alcohol, opioid, or tobacco use were driven by individuals whose cannabis use actually changed. The mechanisms underlying some of these associations remain unclear, and the models may be highly susceptible to confounding. In the case of MCL evaluations in particular, nationally representative survey data suggest that less than 10% of past-year cannabis users report use for medicinal purposes (118). As such, MCLs target a group that is far too small to drive the large effects we are seeing in many of these population studies. In order to advance our understanding of how the use of cannabis and other substances interact, evidence from clinical and prospective cohort studies would greatly bolster any findings from evaluations of state policy effects.
Conclusions
Despite the growing attention of researchers, the evidence related to the public health impacts of MCLs or RCLs is inconclusive regarding many of the most important considerations. We have learned that states adopting MCLs tend to experience increased use of cannabis among adults, although it is unclear whether that leads to greater CUD and risky cannabis use behavior. Adolescents do not appear to be responsive to changes in MCL, but we have yet to learn whether they will respond differently to RCLs, whether the effects of liberalization policies may be more related to changes in price or exposure rather than changes in laws, or whether their cannabis use is changing in ways not well captured in the commonly used datasets.
Evidence of the impact of cannabis liberalization on the use of other substances is inconclusive. We have limited evidence of how alcohol or tobacco use has been impacted, and despite a broader literature evaluating the impact of cannabis laws on opioid-related outcomes, the findings from this literature are puzzling. Studies assessing impacts on self-reported misuse and distribution of opioids show no impact of MCLs, yet studies evaluating opioid-related adverse events and opioid prescribing show reductions. Opioid-related mortality, which early studies suggested was reduced by MCLs, now appears to be positively correlated with these policies and the adoption of RCLs. The significant policy action being taken to combat the opioid crisis as well as the evolution of the types of opioids driving opioid-related harm likely contributes to the lack of robust findings for this outcome.
Moving forward, it is important to consider heterogeneity in MCLs and RCLs and capture ways in which these policies may be more or less restrictive (e.g., taxation, marketing restrictions, licensing for on-premise use). Greater attention to the time course of RCL implementation, which may be correlated with this policy variation, will also be important for modeling potential time-varying effects of policy. Finally, legalization has fundamentally changed cannabis products and routes of administration, and greater attention to heterogeneous cannabis consumption behaviors, including polysubstance use, will likely be far more important to consider than the measures of use prevalence most commonly examined.
Supplementary Material
Acknowledgments
We would like to acknowledge several of our colleagues who we have worked with over the years and who have shaped our thinking on these topics, including Jonathan Caulkins, Mireille Jacobson, Beau Kilmer, Mark Kleiman, Greg Midgette, David Powell, Annie Boustead, and Eric Sevigny.
Funding
This work was supported by the National Institute on Alcohol Abuse and Alcoholism under grant 1R01AA026268.
Footnotes
Supplementary data for this article can be accessed here.
References
- 1.National Conference of State Legislatures. Marijuana deep dive. Washington, DC: National Conference of State Legislatures; 2018. Retrieved from: http://www.ncsl.org/bookstore/state-legislatures-magazine/marijuana-deep-dive.aspx. [Google Scholar]
- 2.Hartig H, Geiger A. About six-in-ten Americans support marijuana legalization. Washington, DC: Pew Research Center; 2018. Retrieved from: http://www.pewresearch.org/fact-tank/2018/10/08/americans-support-marijuana-legalization/. [Google Scholar]
- 3.National Academies of Sciences Engineering and Medicine. The health effects of cannabis and cannabinoids: the current state of evidence and recommendations for research. Washington, DC: The National Academies Press; 2017. [PubMed] [Google Scholar]
- 4.Jones JM. In U.S., medical aid top reason why legal marijuana favored. Gallup; 2019. Retrieved from: https://news.gallup.com/poll/258149/medical-aid-top-reason-why-legal-marijuana-favored.aspx [last accessed 12 June 2019]. [Google Scholar]
- 5.Johnson NB, Hayes LD, Brown K, Hoo EC, Ethier KA. CDC National Health Report: leading causes of morbidity and mortality and associated behavioral risk and protective factors—United States, 2005–2013; 2014. [PubMed] [Google Scholar]
- 6.Sacks JJ, Gonzales KR, Bouchery EE, Tomedi LE, Brewer RD. 2010 national and state costs of excessive alcohol consumption. Am J Prev Med. 2015;49:e73–e9. doi: 10.1016/j.amepre.2015.05.031. [DOI] [PubMed] [Google Scholar]
- 7.Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. The Lancet. 2014;384:45–52. doi: 10.1016/S0140-6736(14)60648-6. [DOI] [PubMed] [Google Scholar]
- 8.Florence CS, Zhou C, Luo F, Xu L. The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med Care. 2016;54:901–06. doi: 10.1097/MLR.0000000000000625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pacula RL, Grossman M, Chaloupka FJ, O’Malley PM, Johnston L, Farrelly MC. Marijuana and youth In: Gruber J, editor. Risky behavior among youths: an economic analysis. Chicago, IL: University of Chicago Press; 2001. p. 271–326. [Google Scholar]
- 10.Pacula RL, Kilmer B, Grossman M, Chaloupka FJ. Risks and prices: the role of user sanctions in marijuana markets. B E J Econom Anal Policy. 2010;10. Article 11. doi: 10.2202/1935-1682.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rhodes T. Risk environments and drug harms: a social science for harm reduction approach. Int J Drug Policy. 2009;20:193–201. doi: 10.1016/j.drugpo.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 12.Pacula RL, Smart R. Medical marijuana and marijuana legalization. Annu Rev Clin Psychol. 2017;13:397–419. doi: 10.1146/annurev-clinpsy-032816-045128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pacula RL, Sevigny EL. Marijuana liberalization policies: why we can’t learn much from policy still in motion. J Pol Anal Manage. 2014;33:212–21. doi: 10.1002/pam.21726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anderson DM, Rees DI. The role of dispensaries: the devil is in the details. J Pol Anal Manage. 2014;33:235–40. doi: 10.1002/pam.21733. [DOI] [PubMed] [Google Scholar]
- 15.Williams AR, Olfson M, Kim JH, Martins SS, Kleber HD, Older L. Regulated medical marijuana programs have much greater enrollment rates than newer `medicalized’ programs. Health Aff (Millwood). 2016;35:480–88. doi: 10.1377/hlthaff.2015.0528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pacula RL, Boustead AE, Hunt P. Words can be deceiving: a review of variation among legally effective medical marijuana laws in the United States. J Drug Policy Anal. 2014;7:1–19. doi: 10.1515/jdpa-2014-0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leung J, Chiu CYV, Stjepanović D, Hall W. Has the legalisation of medical and recreational cannabis use in the USA affected the prevalence of cannabis use and cannabis use disorders?. Curr Addict Rep. 2018;5:403–17. [Google Scholar]
- 18.Chadi N, Weitzman ER, Levy S. Understanding the impact of national and state medical marijuana policies on adolescents. Curr Addict Rep. 2018;5:93–101. [Google Scholar]
- 19.Sarvet AL, Wall MM, Fink DS, Greene E, Le A, Boustead AE, Pacula RL, Keyes KM, Cerdá M, Galea S, et al. Medical marijuana laws and adolescent marijuana use in the United States: a systematic review and meta-analysis. Addiction. 2018;113:1003–16. doi: 10.1111/add.14136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kilmer B, MacCoun RJ. How medical marijuana smoothed the transition to marijuana legalization in the United States. Annu Rev Law Social Sci. 2017;13:181–202. doi: 10.1146/annurev-lawsocsci-110615-084851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carliner H, Brown QL, Sarvet AL, Hasin DS. Cannabis use, attitudes, and legal status in the US: a review. Prev Med. 2017;104:13–23. doi: 10.1016/j.ypmed.2017.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sznitman SR, Zolotov Y. Cannabis for therapeutic purposes and public health and safety: a systematic and critical review. Int J Drug Policy. 2015;26:20–29. doi: 10.1016/j.drugpo.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 23.Choo EK, Emery SL. Clearing the haze: the complexities and challenges of research on state marijuana laws. Ann N Y Acad Sci. 2016;1394:55–73. doi: 10.1111/nyas.13093. [DOI] [PubMed] [Google Scholar]
- 24.Melchior M, Nakamura A, Bolze C, Hausfater F, El Khoury F, Mary-Krause M, Da Silva MA. Does liberalisation of cannabis policy influence levels of use in adolescents and young adults? A systematic review and meta-analysis. BMJ Open. 2019;9:e025880. doi: 10.1136/bmjopen-2018-025880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Keyes KM, Wall M, Cerdá M, Schulenberg J, O’Malley PM, Galea S, Feng T, Hasin DS. How does state marijuana policy affect US youth? Medical marijuana laws, marijuana use and perceived harmfulness: 1991–2014. Addiction. 2016;111:2187–95. doi: 10.1111/add.13523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cerdá M, Sarvet AL, Wall M, Feng T, Keyes KM, Galea S, Hasin DS . Medical marijuana laws and adolescent use of marijuana and other substances: alcohol, cigarettes, prescription drugs, and other illicit drugs. Drug Alcohol Depend. 2018;183:62–68. doi: 10.1016/j.drugalcdep.2017.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lynne-Landsman SD, Livingston MD, Wagenaar AC. Effects of state medical marijuana laws on adolescent marijuana use. Am J Public Health. 2013;103:1500–06. doi: 10.2105/AJPH.2012.301117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wall MM, Mauro C, Hasin DS, Keyes KM, Cerdá M, Martins SS, Feng T. Prevalence of marijuana use does not differentially increase among youth after states pass medical marijuana laws: commentary on and reanalysis of US national survey on drug use in households data 2002–2011. Int J Drug Policy. 2016;29:9–13. doi: 10.1016/j.drugpo.2016.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Choo EK, Benz M, Zaller N, Warren O, Rising KL, McConnell KJ. The impact of state medical marijuana legislation on adolescent marijuana use. J Adolesc Health. 2014;55:160–66. doi: 10.1016/j.jadohealth.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 30.Johnson JK, Johnson RM, Hodgkin D, Jones AA, Matteucci AM, Harris SK. Heterogeneity of state medical marijuana laws and adolescent recent use of alcohol and marijuana: analysis of 45 states, 1991–2011. Subst Abus. 2018;39:247–54. doi: 10.1080/08897077.2017.1389801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johnson J, Hodgkin D, Harris SK. The design of medical marijuana laws and adolescent use and heavy use of marijuana: analysis of 45 states from 1991 to 2011. Drug Alcohol Depend. 2017;170:1–8. doi: 10.1016/j.drugalcdep.2016.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Anderson DM, Hansen B, Rees DI. Medical marijuana laws and teen marijuana use. Amer Law Econ Rev. 2015;17:495–528. doi: 10.1093/aler/ahv002. [DOI] [Google Scholar]
- 33.Harper S, Strumpf EC, Kaufman JS. Do medical marijuana laws increase marijuana use? Replication study and extension. Ann Epidemiol. 2012;22:207–12. doi: 10.1016/j.annepidem.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 34.Martins SS, Mauro CM, Santaella-Tenorio J, Kim JH, Cerdá M, Keyes KM, Hasin DS, Galea S, Wall M. State-level medical marijuana laws, marijuana use and perceived availability of marijuana among the general U.S. population. Drug Alcohol Depend. 2016;169:26–32. doi: 10.1016/j.drugalcdep.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Williams AR, Santaella-Tenorio J, Mauro CM, Levin FR, Martins SS. Loose regulation of medical marijuana programs associated with higher rates of adult marijuana use but not cannabis use disorder. Addiction. 2017;112:1985–91. doi: 10.1111/add.13904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wall MM, Poh E, Cerdá M, Keyes KM, Galea S, Hasin DS. Adolescent marijuana use from 2002 to 2008: higher in states with medical marijuana laws, cause still unclear. Ann Epidemiol. 2011;21:714–16. doi: 10.1016/j.annepidem.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Coley RL, Hawkins SS, Ghiani M, Kruzik C, Baum CF. A quasi-experimental evaluation of marijuana policies and youth marijuana use. Am J Drug Alcohol Abuse. 2019;45:292–303. doi: 10.1080/00952990.2018.1559847. [DOI] [PubMed] [Google Scholar]
- 38.Hasin DS, Wall M, Keyes KM, Cerdá M, Schulenberg J, O’Malley PM, Galea S, Pacula R, Feng T. Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: results from annual, repeated cross-sectional surveys. Lancet Psychiatry. 2015;2:601–08. doi: 10.1016/S2215-0366(15)00217-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mauro CM, Newswanger P, Santaella-Tenorio J, Mauro PM, Carliner H, Martins SS. Impact of medical marijuana laws on state-level marijuana use by age and gender, 2004–2013. Prev Sci. 2019;20:205–14. doi: 10.1007/s11121-017-0848-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stolzenberg L, D’Alessio SJ, Dariano D. The effect of medical cannabis laws on juvenile cannabis use. Int J Drug Policy. 2016;27:82–88. doi: 10.1016/j.drugpo.2015.05.018. [DOI] [PubMed] [Google Scholar]
- 41.Wen H, Hockenberry JM, Cummings JR. The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. J Health Econ. 2015;42:64–80. doi: 10.1016/j.jhealeco.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 42.Pacula RL, Powell D, Heaton P, Sevigny EL. Assessing the effects of medical marijuana laws on marijuana use: the devil is in the details. J Pol Anal Manage. 2015;34:7–31. doi: 10.1002/pam.2015.34.issue-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hasin DS, Sarvet AL, Cerdá M, Keyes KM, Stohl M, Galea S, Wall MM. US adult illicit cannabis use, cannabis use disorder, and medical marijuana laws: 1991–1992 to 2012–2013. JAMA Psychiatry. 2017;74:579–88. doi: 10.1001/jamapsychiatry.2017.0724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Choi A, Dave D, Sabia JJ. Smoke gets in your eyes: medical marijuana laws and tobacco cigarette use. Am J Health Econ. 2018;5:303–33. [Google Scholar]
- 45.Kerr WC, Lui C, Ye Y. Trends and age, period and cohort effects for marijuana use prevalence in the 1984–2015 US national alcohol surveys. Addiction. 2018;113:473–81. doi: 10.1111/add.14031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Smart R. Essays on the effects of medical marijuana laws [PhD Dissertation]. Los Angeles: University of California, Los Angeles; 2016. [Google Scholar]
- 47.Chapman SA, Spetz J, Lin J, Chan K, Schmidt LA. Capturing heterogeneity in medical marijuana policies: a taxonomy of regulatory regimes across the United States. Subst Use Misuse. 2016;51:1174–84. doi: 10.3109/10826084.2016.1160932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hunt P, Miles JNV, Boustead A. Understanding patterns in medical marijuana laws: a latent class and transition analysis. Santa Monica, CA: RAND Health and RAND Justice, Infrastructure and Environment, RAND Corporation; 2013. [Google Scholar]
- 49.King EM, Behrman JR. Timing and duration of exposure in evaluations of social programs. World Bank Res Obs. 2009;24:55–82. doi: 10.1093/wbro/lkn009. [DOI] [Google Scholar]
- 50.Smart RG. Essays on the effects of medical marijuana laws [Doctoral Dissertation]. Los Angeles: University of California; 2016. [Google Scholar]
- 51.Cerdá M, Wall M, Feng T, Keyes KM, Sarvet A, Schulenberg J, O’malley PM, Pacula RL, Galea S, Hasin DS. Association of state recreational marijuana laws with adolescent marijuana use. JAMA Pediatr. 2017;171:142–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kerr DCR, Bae H, Koval AL. Oregon recreational marijuana legalization: changes in undergraduates’ marijuana use rates from 2008 to 2016. Psychol Addict Behav. 2018;32:670–78. doi: 10.1037/adb0000385. [DOI] [PubMed] [Google Scholar]
- 53.Kerr DC, Bae H, Phibbs S, Kern AC. Changes in undergraduates’ marijuana, heavy alcohol and cigarette use following legalization of recreational marijuana use in Oregon. Addiction. 2017;112:1992–2001. doi: 10.1111/add.13906. [DOI] [PubMed] [Google Scholar]
- 54.Miller AM, Rosenman R, Cowan BW. Recreational marijuana legalization and college student use: early evidence. SSM-Popul Health. 2017;3:649–57. doi: 10.1016/j.ssmph.2017.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hunt P, Pacula RL. Early impacts of marijuana legalization: an evaluation of prices in Colorado and Washington. J Prim Prev. 2017;38:221–48. doi: 10.1007/s10935-017-0471-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Smart R, Caulkins JP, Kilmer B, Davenport SS, Midgette G. Variation in cannabis potency and prices in a newly-legal market: evidence from 30 million cannabis sales in Washington State. Addiction. 2017;112:2167–77. doi: 10.1111/add.13886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chu Y-WL. The effects of medical marijuana laws on illegal marijuana use. J Health Econ. 2014;38:43–61. doi: 10.1016/j.jhealeco.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 58.Shi Y. Medical marijuana policies and hospitalizations related to marijuana and opioid pain reliever. Drug Alcohol Depend. 2017;173:144–50. doi: 10.1016/j.drugalcdep.2017.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Borodovsky JT, Crosier BS, Lee DC, Sargent JD, Budney AJ. Smoking, vaping, eating: is legalization impacting the way people use cannabis? Int J Drug Policy. 2016;36:141–47. doi: 10.1016/j.drugpo.2016.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Borodovsky JT, Lee DC, Crosier BS, Gabrielli JL, Sargent JD, Budney AJ. US cannabis legalization and use of vaping and edible products among youth. Drug Alcohol Depend. 2017;177:299–306. doi: 10.1016/j.drugalcdep.2017.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Daniulaityte R, Lamy FR, Barratt M, Nahhas RW, Martins SS, Boyer EW, Sheth A, Carlson RG. Characterizing marijuana concentrate users: a web-based survey. Drug Alcohol Depend. 2017;178:399–407. doi: 10.1016/j.drugalcdep.2017.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Earleywine M, Barnwell SS. Decreased respiratory symptoms in cannabis users who vaporize. Harm Reduct J. 2007;4:11. doi: 10.1186/1477-7517-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Russell C, Rueda S, Room R, Tyndall M, Fischer B. Routes of administration for cannabis use – basic prevalence and related health outcomes: a scoping review and synthesis. Int J Drug Policy. 2018;52:87–96. doi: 10.1016/j.drugpo.2017.11.008. [DOI] [PubMed] [Google Scholar]
- 64.Newmeyer MN, Swortwood MJ, Abulseoud OA, Huestis MA. Subjective and physiological effects, and expired carbon monoxide concentrations in frequent and occasional cannabis smokers following smoked, vaporized, and oral cannabis administration. Drug Alcohol Depend. 2017;175:67–76. doi: 10.1016/j.drugalcdep.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 65.Raber JC, Elzinga S, Kaplan C. Understanding dabs: contamination concerns of cannabis concentrates and cannabinoid transfer during the act of dabbing. J Toxicol Sci. 2015;40:797–803. doi: 10.2131/jts.40.797. [DOI] [PubMed] [Google Scholar]
- 66.Ramaekers JG, Kauert G, van Ruitenbeek P, Theunissen EL, Schneider E, Moeller MR. High-potency marijuana impairs executive function and inhibitory motor control. Neuropsychopharmacology. 2006;31:2296–303. doi: 10.1038/sj.npp.1301068. [DOI] [PubMed] [Google Scholar]
- 67.Hartman RL, Huestis MA. Cannabis effects on driving skills. Clin Chem. 2013;59:478–92. doi: 10.1373/clinchem.2012.194381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Volkow ND, Swanson JM, Evins AE, DeLisi LE, Meier MH, Gonzalez R, Bloomfield MA, Curran HV, Baler R. Effects of cannabis use on human behavior, including cognition, motivation, and psychosis: a review. JAMA Psychiatry. 2016;73:292–97. doi: 10.1001/jamapsychiatry.2015.3278. [DOI] [PubMed] [Google Scholar]
- 69.Loflin M, Earleywine M. A new method of cannabis ingestion: the dangers of dabs? Addict Behav. 2014;39:1430–33. doi: 10.1016/j.addbeh.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 70.D’Souza DC, Perry E, MacDougall L, Ammerman Y, Cooper T, Wu Y-T, Braley G, Gueorguieva R, Krystal JH. The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology. 2004;29:1558. doi: 10.1038/sj.npp.1300496. [DOI] [PubMed] [Google Scholar]
- 71.Di Forti M, Morgan C, Dazzan P, Pariante C, Mondelli V, Marques TR, Handley R, Luzi S, Russo M, Paparelli A, et al. High-potency cannabis and the risk of psychosis. Br J Psychiatry. 2009;195:488–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sevigny EL, Pacula RL, Heaton P. The effects of medical marijuana laws on potency. Int J Drug Policy. 2014;25:308–19. doi: 10.1016/j.drugpo.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Vandrey R, Raber JC, Raber ME, Douglass B, Miller C, Bonn-Miller MO. Cannabinoid dose and label accuracy in edible medical cannabis products. JAMA. 2015;313:2491–93. doi: 10.1001/jama.2015.6613. [DOI] [PubMed] [Google Scholar]
- 74.Carlini BH, Garrett SB, Harwick RM. Beyond joints and brownies: marijuana concentrates in the legal land- scape of WA State. Int J Drug Policy. 2017;42:26–29. doi: 10.1016/j.drugpo.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 75.Caulkins JP, Kilmer B, Kleiman MAR, MacCoun RJ, Midgette G, Oglesby P, Pacula RL, Reuter PH. Considering marijuana legalization: insights for vermont and other jurisdictions. Rand, editor. Santa Monica, CA: Rand Corporation; 2015. [Google Scholar]
- 76.Kilmer B, Caulkins JP, Pacula RL, MacCoun RJ, Reuter P. Altered state? Assessing how marijuana legalization in California could influence marijuana consumption and public budgets. Santa Monica, CA: The RAND Corporation; 2010. [Google Scholar]
- 77.Wen H, Hockenberry JM. Association of medical and adult-use marijuana laws with opioid prescribing for medicaid enrollees. JAMA Intern Med. 2018; 178:673–79. doi: 10.1001/jamainternmed.2018.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bachhuber MA, Saloner B, Cunningham CO, Barry CL. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999–2010. JAMA Intern Med. 2014;174:1668–73. doi: 10.1001/jamainternmed.2014.4005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Powell D, Pacula RL, Jacobson M. Do medical marijuana laws reduce addictions and deaths related to pain killers? J Health Econ. 2018;58:29–42. doi: 10.1016/j.jhealeco.2017.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kleiman MA. Legal commercial cannabis sales in Colorado and Washington: what can we learn?. J Drug Policy Anal. 2016;10:1–16. doi: 10.1515/jdpa-2015-0020 [DOI] [Google Scholar]
- 81.Hansen B, Miller K, Weber C. The taxation of recreational marijuana: evidence from Washington state. Cambridge, MA: National Bureau of Economic Research; 2017. Contract No.: 23632. [Google Scholar]
- 82.Anderson DM, Hansen B, Rees DI. Medical marijuana laws, traffic fatalities, and alcohol consumption. J Law Econ. 2013;56:333–69. doi: 10.1086/668812. [DOI] [Google Scholar]
- 83.Sabia JJ, Swigert J, Young T. The effect of medical marijuana laws on body weight. Health Econ. 2017;26:6–34. doi: 10.1002/hec.3267. [DOI] [PubMed] [Google Scholar]
- 84.Xuan Z, Blanchette J, Nelson TF, Heeren T, Oussayef N, Naimi TS. The alcohol policy environment and policy subgroups as predictors of binge drinking measures among US adults. Am J Public Health. 2015;105:816–22. doi: 10.2105/AJPH.2014.302112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nielsen S, Sabioni P, Trigo JM, Ware MA, Betz-Stablein BD, Murnion B, Lintzeris N, Khor KE, Farrell M, Smith A, et al. Opioid-sparing effect of cannabinoids: a systematic review and meta-analysis. Neuropsychopharmacology. 2017;42:1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Whiting PF, Wolff RF, Deshpande S, Di Nisio M, Duffy S, Hernandez AV, Keurentjes JC, Lang S, Misso K, Ryder S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313:2456–73. doi: 10.1001/jama.2015.6358. [DOI] [PubMed] [Google Scholar]
- 87.Stockings E, Campbell G, Hall WD, Nielsen S, Zagic D, Rahman R, Murnion B, Farrell M, Weier M, Degenhardt L. Cannabis and cannabinoids for the treatment of people with chronic noncancer pain conditions: a systematic review and meta-analysis of controlled and observational studies. Pain. 2018;159:1932–54. doi: 10.1097/j.pain.0000000000001293. [DOI] [PubMed] [Google Scholar]
- 88.Reiman A. Cannabis as a substitute for alcohol and other drugs. Harm Reduct J. 2009;6:1. doi: 10.1186/1477-7517-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lucas P, Walsh Z. Medical cannabis access, use, and substitution for prescription opioids and other substances: a survey of authorized medical cannabis patients. Int J Drug Policy. 2017;42:30–35. doi: 10.1016/j.drugpo.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 90.Reiman A, Welty M, Solomon P. Cannabis as a substitute for opioid-based pain medication: patient self-report. Cannabis Cannabinoid Res. 2017;2:160–66. doi: 10.1089/can.2017.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Caputi TL, Humphreys K. Medical marijuana users are more likely to use prescription drugs medically and nonmedically. J Addict Med. 2018;12:295–99. doi: 10.1097/ADM.0000000000000405. [DOI] [PubMed] [Google Scholar]
- 92.Phillips E, Gazmararian J . Implications of prescription drug monitoring and medical cannabis legislation on opioid overdose mortality. J Opioid Manag. 2017;13:229–39. doi: 10.5055/jom.2017.0391. [DOI] [PubMed] [Google Scholar]
- 93.Shover CL, Davis CS, Gordon SC, Humphreys K. Association between medical cannabis laws and opioid overdose mortality has reversed over time. P Natl Acad Sci USA. 2019;116:12624–26. doi: 10.1073/pnas.1903434116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chu Y-WL. Do medical marijuana laws increase hard-drug use? J Law Econ. 2015;58:481–517. doi: 10.1086/684043. [DOI] [Google Scholar]
- 95.Kim JH, Santaella-Tenorio J, Mauro C, Wrobel J, Cerdá M, Keyes KM, Hasin D, Martins SS, Li G. State medical marijuana laws and the prevalence of opioids detected among fatally injured drivers. Am J Public Health. 2016;106:2032–37. doi: 10.2105/AJPH.2016.303426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bradford AC, Bradford WD. Medical marijuana laws reduce prescription medication use in Medicare Part D. Health Aff. 2016;35:1230–36. doi: 10.1377/hlthaff.2015.1661. [DOI] [PubMed] [Google Scholar]
- 97.Shah A, Hayes CJ, Lakkad M, Martin BC. Impact of medical marijuana legalization on opioid use, chronic opioid use, and high-risk opioid use. J Gen Intern Med. 2019;34:1419–26. doi: 10.1007/s11606-018-4782-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wen H, Hockenberry JM, Druss BG. The effect of medical marijuana laws on marijuana-related attitude and perception among us adolescents and young adults. Prev Sci. 2019;20:215–23. doi: 10.1007/s11121-018-0903-8. [DOI] [PubMed] [Google Scholar]
- 99.Shi Y, Liang D, Bao Y, An R, Wallace MS, Grant I. Recreational marijuana legalization and prescription opioids received by medicaid enrollees. Drug Alcohol Depend. 2019;194:13–19. doi: 10.1016/j.drugalcdep.2018.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Liang D, Bao Y, Wallace M, Grant I, Shi Y. Medical cannabis legalization and opioid prescriptions: evidence on US Medicaid enrollees during 1993–2014. Addiction. 2018;113:2060–70. doi: 10.1111/add.14382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bradford AC, Bradford WD. Factors driving the diffusion of medical marijuana legalisation in the United States. Drugs. 2017;24:75–84. [Google Scholar]
- 102.Bradford AC, Bradford WD, Abraham A, Bagwell Adams G. Association between US State medical cannabis laws and opioid prescribing in the medicare part D population. JAMA Intern Med. 2018;178:667–72. doi: 10.1001/jamainternmed.2018.0266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Doctor JN, Nguyen A, Lev R, Lucas J, Knight T, Zhao H, Menchine M. Opioid prescribing decreases after learning of a patient’s fatal overdose. Science. 2018;361:588–90. doi: 10.1126/science.aat4595. [DOI] [PubMed] [Google Scholar]
- 104.Haegerich TM, Paulozzi LJ, Manns BJ, Jones CM. What we know, and don’t know, about the impact of state policy and systems-level interventions on prescription drug overdose. Drug Alcohol Depend. 2014;145:34–47. doi: 10.1016/j.drugalcdep.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Franklin G, Sabel J, Jones CM, Mai J, Baumgartner C, Banta-Green CJ, Neven D, Tauben DJ. A comprehensive approach to address the prescription opioid epidemic in Washington State: milestones and lessons learned. Am J Public Health. 2015;105:463–69. doi: 10.2105/AJPH.2014.302367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Scherma M, Muntoni AL, Melis M, Fattore L, Fadda P, Fratta W, Pistis M. Interactions between the endocannabinoid and nicotinic cholinergic systems: preclinical evi- dence and therapeutic perspectives. Psychopharmacology (Berl). 2016;233:1765–77. doi: 10.1007/s00213-015-4196-3. [DOI] [PubMed] [Google Scholar]
- 107.Kohut SJ. Interactions between nicotine and drugs of abuse: a review of preclinical findings. Am J Drug Alcohol Ab. 2017;43:155–70. doi: 10.1080/00952990.2016.1209513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Agrawal A, Budney AJ, Lynskey MT. The co-occurring use and misuse of cannabis and tobacco: a review. Addiction. 2012;107:1221–33. doi: 10.1111/j.1360-0443.2012.03837.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Schauer GL, Berg CJ, Kegler MC, Donovan DM, Windle M. Assessing the overlap between tobacco and marijuana: trends in patterns of co-use of tobacco and marijuana in adults from 2003–2012. Addict Behav. 2015;49:26–32. doi: 10.1016/j.addbeh.2015.05.012. [DOI] [PubMed] [Google Scholar]
- 110.Schauer GL, Rosenberry ZR, Peters EN. Marijuana and tobacco co-administration in blunts, spliffs, and mulled cigarettes: a systematic literature review. Addict Behav. 2017;64:200–11. doi: 10.1016/j.addbeh.2016.09.001. [DOI] [PubMed] [Google Scholar]
- 111.Rabin RA, George TP. A review of co-morbid tobacco and cannabis use disorders: possible mechanisms to explain high rates of co-use. Am J Addict. 2015;24:105–16. doi: 10.1111/ajad.12186. [DOI] [PubMed] [Google Scholar]
- 112.Dutra LM, Glantz SA, Arrazola RA, King BA. Impact of E-cigarette minimum legal sale age laws on current cigarette smoking. J Adolesc Health. 2018;62:532–38. doi: 10.1016/j.jadohealth.2017.11.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.US Department of Health Human Services. The health consequences of smoking – 50 years of progress: a report of the surgeon general. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 114.Levy DT, Warner KE, Cummings KM, Hammond D, Kuo C, Fong GT, Thrasher JF, Goniewicz ML, Borland R. Examining the relationship of vaping to smoking initiation among US youth and young adults: a reality check. Tob Control. 2018;1–7. doi: 10.1136/tobaccocontrol-2018-054446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Miech RA, Schulenberg JE, Johnston LD, Bachman JG, O’Malley PM, Patrick ME.National adolescent drug trends in 2018 [press release]. Ann Arbor, MI: Monitoring the Future; 2018. Available at: http://www.monitoringthefuture.org [Google Scholar]
- 116.Huang J, Duan Z, Kwok J, Binns S, Vera LE, Kim Y, Szczypka G, Emery SL. Vaping versus JUULing: how the extraordinary growth and marketing of JUUL transformed the US retail e-cigarette market. Tob Control. 2019;28(2):146–51. doi: 10.1136/tobaccocontrol-2018-054382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Zhu S-H, Sun JY, Bonnevie E, Cummins SE, Gamst A, Yin L, Lee M. Four hundred and sixty brands of e-cigarettes and counting: implications for product regulation. Tob Control. 2014;23:iii3–iii9. doi: 10.1136/tobaccocontrol-2014-051670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Compton WM, Han B, Hughes A, Jones CM, Blanco C. Use of marijuana for medical purposes among adults in the United States. JAMA. 2017;317:209–11. doi: 10.1001/jama.2016.18900. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.