Abstract
An unhealthy body mass index (BMI) trajectory can exacerbate the burdens associated with child maltreatment. However, we have yet to explain why the relationship between maltreatment and BMI trajectories exists and what allows individuals to attain healthy BMI trajectories despite adversity. Guided by the Transactional Model of Stress and Coping, we evaluated (1) if peer friendship and adult mentors moderate, and (2) if impulsivity and depressive symptoms mediate, the relationship between maltreatment experiences and average excess BMI. We used data from four waves of the National Longitudinal Study of Adolescent to Adult Health (n = 17,696), following adolescents from ages 13-21 (Wave I) to 24-31 years (Wave IV). We did not find evidence of significant moderation or mediation of the maltreatment experience to average excess BMI relationship. However, models did demonstrate a relationship between peer friendship quality and average excess BMI, such that higher quality protected against higher average excess BMI (B = −0.073, s.e. = 0.02, p < 0.001). Age of maltreatment onset was also associated with average excess BMI, such that maltreatment onset in adolescence was associated with a higher average excess BMI (B = 0.275-0.284, s.e. = 0.11, p = 0.01). Although we found no evidence of moderation by social support or mediation by stress responses of the relationship between maltreatment experiences and average excess BMI, peer friendship appears to protect against higher average excess BMI from adolescence to young adulthood for all adolescents. Future public health interventions should consider how to leverage friendship in obesity prevention efforts.
Keywords: Child maltreatment, Body mass index, Longitudinal
1. Introduction1
Around one in 58 children in the United States experience maltreatment annually (Sedlak et al., 2010). Studies suggest the prevalence of obesity is significantly higher among these individuals compared to the general population (Burke, Hellman, Scott, Weems, & Carrion, 2011; Felitti et al., 1998). Although the link between maltreatment and BMI has been demonstrated in several studies, we have yet to (1) identify the factors allowing some individuals to attain healthy BMI trajectories despite experiencing child maltreatment (moderators), and (2) determine the mechanisms driving the relationship between maltreatment and unhealthy BMI trajectories (mediators). The overall objective of this study was to identify intervenable factors that drive this moderation and mediation to inform future interventions that improve BMI trajectories for those who have experienced child maltreatment. Identifying factors on the path from maltreatment to longitudinal weight outcomes may inform interventions that not only reduce obesity prevalence, but also improve quality of life for a vulnerable population.
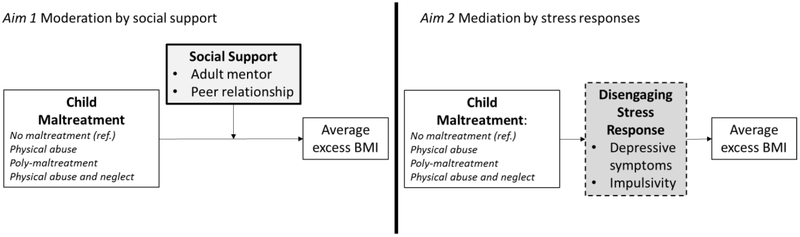
Guided by the Transactional Model of Stress and Coping (TMSC) theoretical framework, the present study aimed to (Figure 1):
Determine whether social supports moderate the relationship between child maltreatment and average excess BMI from adolescence to early adulthood; and
Evaluate whether stress responses mediate the relationship between child maltreatment and average excess BMI from adolescence to young adulthood.
Figure 1.
Conceptual models.
2. Theory
2.1. Transactional Model of Stress and Coping
The Transactional Model of Stress and Coping (TMSC) provides a rationale for investigating depressive symptoms, impulsivity, and social support, in the relationship between the stressor of child maltreatment and a longitudinal BMI measure—average excess BMI. According to Lazarus and Folkman’s TMSC, psychological stress is a relationship between a person and the environment that the person “[…] appraises as significant for his or her well-being and in which the demands tax or exceed available coping resource” (Lazarus & Folkman, 1986). Child maltreatment is a significant stressor that can have lasting effects on health via stress responses (i.e., maladaptive coping) that mediate the person-environment relationship, but the relationship between the child maltreatment stressor and health may also be buffered by social support. The present study investigates these processes.
Coping is a stress response that entails a person's efforts to manage stress (Folkman, 2013; Glanz & Schwartz, 2008). Coping can be maladaptive or adaptive: Adaptive coping promotes positive health outcomes, whereas maladaptive coping encourages poor health outcomes (Zeidner & Saklofske, 1996). Individuals exposed to maltreatment may have greater difficulty managing affective states, and thereby exhibit a higher intensity of maladaptive coping strategies, such as depressive and impulsive stress responses, compared to peers (Moore et al., 2015; Vachon, Krueger, Rogosch, & Cicchetti, 2015). In a meta-analysis of eight cohort studies, a history of child maltreatment was associated with an increased odds of major depressive disorder in adulthood [odds ratio (OR): 2.03; 1.37-3.01] (Li, D'Arcy, & Meng 2015). So what explains the link between child maltreatment and BMI? Research has linked the stress responses of depressive symptoms and impulsivity to poor weight outcomes in adolescence, as both depression and impulsivity are associated with weight-related disturbances (Korczak, Lipman, Morrison, & Szatmari, 2013; Thamotharan, Lange, Zale, Huffhines, & Fields, 2013). Using Add Health, Sacks and colleagues also found that depression mediated the relationship between physical abuse in childhood and BMI trajectories in girls (Sacks et al., 2017). These findings align with TMSC, which suggests stress responses can result in decreased functional health, including poor weight outcomes (Heatherton & Baumeister, 1991).
As evidenced by the resiliency of some children who experience child maltreatment (Afifi & MacMillan, 2011), the pathway from child maltreatment to unhealthy BMI trajectories through stress responses is not predetermined. Instead, this relationship is subject to influence by various intrapersonal, interpersonal, and environmental characteristics. Specifically, social support may break the link between maltreatment and poor health outcomes (Cohen & McKay, 1984). Previous research has well-established the stress-buffering role of social support for a variety of health outcomes (Cohen & McKay, 1984; Ditzen & Heinrichs, 2014; Meagher-Stewart, 1994; Short & Johnston, 1997). For individuals who have experienced child maltreatment, this social support may come in the form of peer friendships or mentorship from a non-parental adult—as the relationship with a parent would likely offer no (or potentially harmful) social support for individuals in these unique circumstances (Ahrens, DuBois, Richardson, Fan, & Lozano, 2008).
3. Methods
3.1. Data Source
This study used data from Add Health (P01-HD31921), a longitudinal study of a nationally representative sample of 20,745 adolescents in grades 7-12 in the U.S. during 1994-95.(K. Harris et al., 2016). We used data from Wave I (ages 13-21), Wave II (ages 13-21), Wave III (ages 18-28), and Wave IV (ages 24-31). The University of North Carolina Institutional Review Board granted exemption from human subjects’ research approval.
For all analyses, we restricted the sample to respondents aged 13-31 years with valid Wave I sampling weights and BMI measured at Wave II, III, or IV. We dropped data for time point(s) when the respondent was pregnant and for respondents who were underweight for the entire age range. This resulted in a final sample of 17,696.
3.2. Measures
3.2.1. Average excess BMI.
Average excess BMI from adolescence to young adulthood, developed and validated in previous work (R. L. Sokol, Gottfredson, Poti, et al., 2018), served as the focal outcome. This measure represents a person’s average deviance above a healthy BMI, healthy according to the Centers for Disease Control and Prevention, over a specified period. For example, as the upper limit of a healthy BMI range for adults is 25 kg/m2, a person with a BMI of 28 kg/m2 at age 25 years would have an excess BMI of 3 kg/m2. With longitudinal data containing multiple BMI measurements, we modeled a person’s latent BMI trajectory and averaged their model-implied excess BMI over time to arrive at a single numerical value for their average excess BMI.
3.2.2. Child maltreatment.
We operationalized child maltreatment experiences in a manner that does not require the mutual exclusion of maltreatment types, in line with previous research supporting the high co-occurrence of child maltreatment types (Kim & Cicchetti, 2010; Manly, Kim, Rogosch, & Cicchetti, 2001). A previous study using Add Health data employed a latent class analysis (LCA) that uncovered patterns of childhood maltreatment experiences, and we used these classes as the focal predictor in the present study (R. L. Sokol, Gottfredson, Shanahan, & Halpem, 2018). This operationalization of child maltreatment embodied overall patterns of maltreatment that simultaneously captured maltreatment timing, frequency, type(s), and type co-occurrence, to create a more accurate representation of an individual’s lived experience.
Methods for obtaining classes of child maltreatment via LCA are described in detail in Sokol et al., 2018. Briefly, study authors used indicators of child maltreatment assessed retrospectively at Waves III and IV to inform maltreatment experience classes. Questions at both waves asked respondents about the frequency of maltreatment types (physical abuse, sexual abuse, and neglect) perpetrated by a primary caregiver, with responses ranging from never to ten or more times. To account for maltreatment timing, we only considered maltreatment indicators prior to age 12 years to inform maltreatment class assignment, and we added an indicator for adolescent-onset maltreatment (i.e., post 12 years) in all analyses. The recovered child maltreatment experience classes included: 1) a poly-maltreatment class with high frequency of sexual abuse and co-occurring physical abuse and neglect (n = 1,025); 2) a physical abuse class with high frequency of physical abuse (n = 3,799); 3) a physical abuse and neglect class with high frequency of neglect and co-occurring physical abuse (n = 901); and 4) a no childhood maltreatment class (n = 11,944). We represented these classes by a series of indicator variables in analyses, with the no childhood maltreatment class serving as the reference group.
3.2.3. Social support moderators.
Following previous studies on the general and child maltreatment samples of Add Health, the presence of a mentor was captured by asking respondents if a non-parental adult made an “important positive difference in your life” (DuBois & Silverthorn, 2005). Peer friendship quality was a latent variable resulting from several items: Wave I questionnaires asked respondents if they had met a friend after school to hang out, spent time over the weekend, discussed a problem, or talked on the phone. Following previous analyses, we created a latent variable of peer friendship quality reflecting respondents’ answers for their best friend (Deutsch, Chernyavskiy, Steinley, & Slutske, 2015).
3.2.4. Stress response mediators.
Depressive symptoms was a latent variable comprised of 5 items from the Center for Epidemiologic Studies Depression Scale assessed at Wave I, as previous analyses have found these five items have stronger reliability and measurement invariance across racial/ethnic groups compared to the full 19 items (K. M. Harris, Deeb-Sossa, Perreira, & Bollen, 2003). These items included: 1) You felt your life what not worth living; 2) It was hard to get started doing things; 3) You felt like you could not shake off the blues; 4) You felt happy (reverse coded); and 5) You felt depressed. Impulsivity was a latent variable informed by five items from Wave I: 1) When making decisions, you usually go with your gut feeling; 2) When you have a problem to solve, one of the first things you do is get as many facts about the problem (reverse coded); 3) When you are attempting to find a solution to a problem, you usually try to think of as many different ways to approach the problem as possible (reverse coded); 4) When making decisions, you generally use a systematic method for judging and comparing alternatives (reverse coded); 5) After carrying out a solution to a problem, you usually try to analyze what went right and what went wrong (reverse coded).
3.2.5. Covariates.
We used our previously developed Directed Acyclic Graph (DAG) that depicted the casual relationship between child maltreatment and longitudinal weight outcomes to inform covariate selection (R. L. Sokol; Shanahan, ME; Gottfredson, NC; Poti, JM; Halpern, CT; Fisher, EB, 2019 (under review)). All covariates were assessed at Wave I and included biological sex (male or female), race/ethnicity (non-Hispanic Black, non-Hispanic White, Hispanic, other), parent education (less than high school, high school, some college, college graduate), parent employment (employed or unemployed), child birth weight (in ounces, mean-centered), if the child was exclusively breastfed for 6+ months, if the child was born in the United States, and if the biological mother or father was obese (ascertained from parent self-report) (Kathleen Mullan Harris, Perreira, & Lee, 2009; Owen, Martin, Whincup, Smith, & Cook, 2005; Parsons, Power, Logan, & Summerbelt, 1999).
3.3. Analytic Approach
To evaluate Aims 1 and 2 we estimated (1) a moderation structural equation model (SEM) to evaluate the roles of peer friendship and non-parental adult mentors, and (2) a mediation SEM to evaluate the roles of impulsivity and depression in the relationship between child maltreatment experience and average excess BMI. SEMs are particularly useful for evaluating relationships involving latent variables, a quality of several of the key mediating and moderating variables (Hayes, 2013). We used Stata 13© for data management, and we estimated Confirmatory Factor Analysis (CFA) models and SEMs using Mplus version 7.4.© To account for missing data, we conducted 20 imputations with chained equations to impute values for all covariates, and we conducted analyses over these imputed datasets (Graham, Olchowski, & Gilreath, 2007). Due to Add Health’s complex survey design, analyses adjusted variance estimates to account for clustering and include sampling weights (Lumley, 2004).
We first conducted CFAs to develop measurement models for the latent mediating and moderating variables (depressive symptoms, impulsivity, and peer friendship quality) using their indicators. From CFAs, we evaluated model fit (RMSEA <.05, TLI/CFI > .95). With well-specified measurement models, we advanced to SEM models
3.3.1. Aim 1: Moderation by social support.
We hypothesized that the presence of an adult mentor would attenuate the relationship between child maltreatment characterized by (a) physical abuse, (b) physical abuse and neglect, or (c) poly-maltreatment (relative to individuals who experienced no child maltreatment) and average excess BMI from adolescence to early adulthood. We additionally hypothesized that this relationship would be weaker for individuals with higher peer friendship. We estimated a SEM model using maximum likelihood with robust standard errors (MLR) with all focal predictors, moderators, interactions between predictors and moderators, and covariates entered simultaneously. We specified our covariates in the SEM as predictors in a regression explaining average excess BMI The presence of moderation was supported if the 95% confidence interval for an interaction parameter estimate did not contain zero.
3.3.2. Aim 2: Mediation by stress responses.
We hypothesized that adolescents who experienced child maltreatment characterized by (a) physical abuse, (b) physical abuse and neglect, or (c) poly-maltreatment would exhibit greater depressive symptoms and impulsivity compared to those who did not experience maltreatment, which in turn would be associated with higher average excess BMI from adolescence to early adulthood. We estimated a SEM model using an MLR estimator with all focal predictors, mediators, and covariates entered simultaneously, estimating both direct and indirect effects. We specified our covariates in the SEM as predictors in a regression explaining average excess BMI. We followed Hayes’ process for evaluating multiple mediation models with parallel mediators, which involves determining the indirect effects and evaluating their significance (Hayes, 2013). To make statistical inferences about indirect effects, we obtained 95% confidence intervals for the indirect effects.
4. Results
The final analytic sample size was 17,696. Of the original 20,744 Add Health respondents, 117 did not fall into the specified age range at any collection wave, 1,826 did not have sampling weights, 1,133 had no recorded BMI measurements at any wave, 27 were underweight at all time points, and 2 had no information on biological sex.
The overall sample was evenly divided on biological sex (male = 50.5%), and was primarily non-Hispanic white (65.5%), born in the United States (93.7%), normal birthweight (118.8 ounces), and not breastfed exclusively for six months (80.4%). The average excess BMI of respondents was 2.80 kg/m2. Among the primary caregivers of respondents, most respondents had at least one parent who was college educated (30.2%) and employed (69.0%), and neither parent was likely to be obese (77.3%) (Table 1).
Table 1.
Descriptive statistics of the analytic sample from the National Longitudinal Study of Adolescent to Adult Health (n = 17 696).
| Variable | Total, Mean (SD) or % |
|---|---|
| Average excess BMI | 2.80 (4.19) |
| Maltreatment class | |
| No maltreatment class | 67.6% |
| Physical abuse class | 21.5% |
| Physical abuse + neglect class | 5.1% |
| Poly-maltreatment class | 5.8% |
| Adolescent onset maltreatment | 26.4% |
| Male | 50.5% |
| Parental obesity | 23.7% |
| Birthweight | 1.58 (19.9) |
| Breastfed, 6+ months | 19.6% |
| US born | 93.7% |
| Parent employment | 69.0% |
| Race/ethnicity | |
| White | 65.5% |
| Hispanic | 12.0% |
| Black | 15.8% |
| Other | 6.8% |
| Parent education | |
| < High school | 12.7% |
| High school | 27.7% |
| Some college | 29.5% |
| College graduate | 30.2% |
| N | 17 696 |
Note: Descriptive statistics are averaged over 20 imputed datasets and account for survey weighting and clustering. Adolescent onset maltreatment, parental obesity, breastfed, US born, and parent employment are dichotomous indicator variables. Birthweight is mean-centered from the Add Health sample.
4.1. Confirmatory Factor Analysis
Model fit was very good for all measurement models (Table 2), including that for peer friendship quality (χ2[2] = 1.71, p = 0.43; CFI = 1.00; TLI = 1.00; RMSEA = 0.000 [95% CI: 0.000, 0.014]), depressive symptoms (χ2[5] = 63.2, p < 0.001; CFI = 0.996; TLI = 0.992; RMSEA = 0.026 [95% CI: 0.020, 0.031]), and impulsivity (χ2[5] = 160.0, p < 0.001; CFI = 0.99; TLI = 0.98; RMSEA = 0.042 [95% CI: 0.036, 0.048]).
Table 2.
Factor loadings from measurement models for peer friendship, depressive symptoms, and impulsivity (n = 17 696).
| Factor Loadings | λ (SE) | R2 | 95% CI |
|---|---|---|---|
| Peer friendship quality | |||
| House | 1.00 (--) | 0.80 | -- |
| After school | 0.89 (0.02) | 0.60 | 0.844, 0.924*** |
| Weekend | 0.92 (0.02) | 0.67 | 0.895, 0.974*** |
| Phone | 0.53 (0.02) | 0.21 | 0.481, 0.569*** |
| Depressive symptoms | |||
| Blue | 1.00 (--) | 0.69 | -- |
| Happy | 0.38 (0.01) | 0.10 | 0.361, 0.406*** |
| Motivated | 0.53 (0.01) | 0.19 | 0.501, 0.552*** |
| Reason to live | 0.84 (0.02) | 0.48 | 0.802, 0.869*** |
| Feel depressed | 1.08 (0.01) | 0.80 | 1.053, 1.107*** |
| Impulsivity | |||
| Decision | 1.00 (--) | 0.02 | -- |
| Facts | 5.80 (0.65) | 0.55 | 4.521, 7.085*** |
| Approach | 6.19 (0.67) | 0.62 | 4.865, 7.508*** |
| System | 5.45 (0.62) | 0.48 | 4.237, 6.658*** |
| Analyze | 5.08 (0.57) | 0.42 | 3.968, 6.196*** |
Note: Model fit was good for all measurement models. Peer friendship quality: χ2(2) = 1.71, p = 0.43; CFI = 1.00; TLI = 1.00; RMSEA = 0.000 (95% CI: 0.000, 0.014). Depressive symptoms: χ2(5) = 63.2, p < 0.001; CFI = 0.996; TLI = 0.992; RMSEA = 0.026 (95% CI: 0.020, 0.031). Impulsivity: χ2(5) = 160.0, p < 0.001; CFI = 0.99; TLI = 0.98; RMSEA = 0.042 (95% CI: 0.036, 0.048).
p < .05.
p < .01.
p < .001.
4.2. Aim 1: Moderation by Social Support
Adolescent-onset maltreatment was significantly and positively associated with average excess BMI (B = 0.275, s.e. = 0.11, p = 0.01). The moderation model did not find evidence of significant moderation of the maltreatment experience to average excess BMI relationship by social support factors (Table 3). However, the model did demonstrate evidence of a relationship between peer friendship quality and average excess BMI, such that higher peer friendship quality protects against higher average excess BMI (B = −0.073, s.e. = 0.02, p < 0.001).
Table 3.
Parameter estimates from moderation model predicting average excess BMI (n = 17696).
| Variable | B (SE) | 95% CI |
|---|---|---|
| Focal variables | ||
| Physical abuse | 0.089 (0.22) | −0.335, 0.513 |
| Physical abuse + neglect | −0.091 (0.42) | −0.910, 0.728 |
| Poly-maltreatment | −0.259 (0.34) | −0.920, 0.402 |
| Peer friendship | −0.073 (0.02) | −0.113, −0.033*** |
| Mentor | 0.225 (0.12) | −0.015, 0.465 |
| Conditional relationships | ||
| Physical abuse*peer friendship | −0.010 (0.05) | −0.099, 0.079 |
| Physical abuse/neglect*peer friendship | 0.017 (0.10) | −0.182, 0.217 |
| Poly-maltreatment*peer friendship | 0.146 (0.10) | −0.055, 0.347 |
| Physical abuse*mentor | 0.086 (0.25) | −0.408, 0.579 |
| Physical abuse/neglect*mentor | 0.154 (0.46) | −0.753, 1.061 |
| Poly-maltreatment* mentor | 0.633 (0.41) | −0.170, 1.436 |
| Covariates | ||
| Adolescent onset maltreatment | 0.275 (0.11) | 0.061, 0.488* |
| Male | −0.305 (0.11) | −0.515, −0.095* |
| Parental obesity | 2.316 (0.15) | 2.014, 2.618*** |
| Birthweight | 0.009 (0.00) | 0.005, 0.013** |
| Breastfed, 6+ months | −0.249 (0.10) | −0.446, −0.053* |
| US born | 0.891 (0.19) | 0.518, 1.263*** |
| Parental employment | −0.042 (0.10) | −0.239, 0.155 |
| Hispanic (ref. white) | 0.608 (0.15) | 0.314, 0.902*** |
| Black (ref. white) | 0.984 (0.12) | 0.759, 1.209*** |
| Other (ref. white) | 0.125 (0.28) | −0.421, 0.671 |
| Less than high school (ref. college graduate) | 0.978 (0.16) | 0.661, 1.295*** |
| High school (ref. college graduate) | 0.929 (0.16) | 0.621, 1.237*** |
| Some college (ref. college graduate) | 0.461 (0.12) | 0.228, 0.694*** |
Note: Adolescent onset maltreatment, parental obesity, breastfed, US born, and parent employment are dichotomous indicator variables.
p < .05.
p < .01.
p < .001.
4.3. Aim 2: Mediation by Stress Reponses
The mediation model did not find evidence of significant mediation of the child maltreatment experience to average excess BMI relationship through stress responses. However, the model demonstrated evidence of a direct relationship between maltreatment experiences and depressive symptoms, such that individuals who belonged to the child physical abuse (B = 0.511, s.e. = 0.09, p < 0.001), child physical abuse/neglect (B = 0.854, s.e. = 0.16, p < 0.001), and child poly-maltreatment (B = 1.020, s.e. = 0.15, p < 0.001) classes experienced higher depressive symptoms compared to individuals in the no child maltreatment class. As in the moderation model, while we did not observe any significant relationships between membership in a child maltreatment class and average excess BMI, adolescent-onset maltreatment was significantly and positively associated with average excess BMI (B = 0.284, s.e. = 0.11, p = 0.01).
5. Discussion
The present analyses did not find significant moderation by social support or mediation by stress responses of the relationship between child maltreatment experiences and average excess BMI. Instead, results suggest the importance of maltreatment timing in investigating these relationships.
The present study’s lack of evidence for mediation and moderation runs counter to our TSMC theoretically-driven hypotheses and previous empirical work (Lazarus & Folkman, 1987; Sacks et al., 2017). This difference could in part be due to the measurement timing of maltreatment, depressive symptoms, impulsivity, and social supports. For example, Sacks and colleagues found that the trajectory of depressive symptoms moderated the relationships between physical abuse and BMI trajectories among girls (Sacks et al., 2017). In the present analyses, we assessed depressive symptoms, impulsivity, and social supports at Wave I in order to establish proper temporal ordering of the predictors (which captured events prior to Wave I), mediators and moderators (which captured events contemporaneous with Wave I), and the outcome (which occurred from Wave I to IV). Because depressive symptoms, impulsivity, and social support may have effects on body weight throughout adolescence and early adulthood, future studies may benefit from evaluating the dynamic nature of these constructs as they relate to body weight over time.
Moreover, our study suggests the timing of maltreatment may be an important factor in these mediation and moderation models. The present analyses found that adolescent-onset maltreatment was significantly associated with average excess BMI compared to individuals who never experienced maltreatment, and this effect persisted in both the moderation and mediation models. Future analyses should explore how models can include developmental timing of maltreatment, and how such timing may interact with social supports—or work through stress responses—to predict longitudinal weight outcomes.
Despite our lack of evidence for the moderating role of social support, we did find that peer friendship protected against higher average excess BMI from adolescence to young adulthood for all individuals. This finding suggests that developing such ties could be beneficial to all adolescents in an effort to prevent poor weight outcomes later in life. Adolescence is a period of increased stress (Galvan & Rahdar, 2013), and peer friendship could buffer against the relationship between stress and poor weight outcomes for all individuals. Peer friendship can provide assistance and resources, and these resources can be emotional, instrumental, appraisal, or informational (House, 1987). The moderation of the stress-health relationship by social support could occur at various points. For example, social support could bolster beliefs about one’s ability to cope with situations, moderating the relationship between the stressor and appraisal (Cohen & McKay, 1984). Social support could also influence health behaviors and outcomes through the direct influence of social networks (e.g., being surrounded by a network who regularly exercises can increase a person’s physical activity) (Beasley et al., 2010).
The present results did not confirm the expected relationship between membership in child maltreatment classes and longitudinal BMI found in prior studies (R. L. Sokol, Gottfredson, Shanahan, et al., 2018). As described above, this may be due to the developmental timing of variables. Additionally, operationalization of the outcome (i.e., average excess BMI) and predictors (i.e., child maltreatment latent classes) in the present study varies from previous work. As such, child maltreatment may be associated with higher linear growth in BMI across adolescent development, but if the trajectory eventually levels off in early adulthood, maltreatment may pose no greater risk for increased average excess BMI over this developmental period.
As noted, a limitation of the present study involves the inability to consider developmental timing of variables. Our analyses assessed child maltreatment prior to Wave I, mediators and moderators at Wave I, and average excess BMI from Wave I-IV in order to establish proper temporal ordering of variables. While it is important that analyses establish temporality, given the suggested importance of adolescent-onset maltreatment, future research should explore the developmental timing of maltreatment, social support, and stress responses, in these mediation and moderation analyses. Although we designed the present analyses to follow proper temporal ordering of variables, we cannot guarantee this; given the heritability of psychopathology (including depressive symptoms and impulsivity), stress responses could have appeared before maltreatment experiences. Our primary aims were not concerned with the fundamental sources of depressive symptoms and impulsivity, however, but rather their role in the path from maltreatment to weight outcomes—regardless of the psychopathology source. Moreover, although a DAG informed our analyses to mitigate potential confounding, it is possible that an external variable could both increase the likelihood of having close friends and decrease risk for average excess BMI. This study also contains a number of strengths, including the large and nationally representative school-based sample, a strong theoretical framework, a longitudinal weight outcome, person-centered operationalization of child maltreatment experience, and adjusting for potential confounders.
6. Conclusions
While we found no evidence of moderation by social support or mediation by stress responses of the relationship between child maltreatment experiences and average excess BMI from adolescence to young adulthood, peer friendship appears to protect against higher average excess BMI from adolescence to young adulthood for all adolescents. Future public health interventions should consider how to leverage this phenomenon in obesity prevention efforts.
Table 4.
Parameter estimates from mediation model predicting average excess BMI (n = 17 696).
| Relationship | B (SE) | 95% CI |
|---|---|---|
| Direct associations | ||
| Physical abuse → Depression | 0.511 (0.09) | 0.337, 0.685*** |
| Physical abuse → Impulsivity | 0.006 (0.01) | −0.010, 0.022 |
| Physical abuse → Average excess BMI | 0.180 (0.12) | −0.063, 0.423 |
| Physical abuse/neglect → Depression | 0.854 (0.16) | 0.537, 1.172*** |
| Physical abuse/neglect → Impulsivity | 0.011 (0.02) | −0.018, 0.040 |
| Physical abuse/neglect → Average excess BMI | 0.043 (0.24) | −0.430, 0.516 |
| Poly-maltreatment → Depression | 1.020 (0.15) | 0.720, 1.320*** |
| Poly-maltreatment → Impulsivity | 0.012 (0.01) | −0.015, 0.039 |
| Poly-maltreatment → Average excess BMI | 0.214 (0.20) | −0.170, 0.597 |
| Depression → Average excess BMI | −0.020 (0.02) | −0.058, 0.018 |
| Impulsivity → Average excess BMI | −0.117 (0.19) | −0.481, 0.248 |
| Indirect Associations (α*β) | ||
| Physical abuse → Depression → Average excess BMI | −0.010 (0.01) | −0.030, 0.009 |
| Physical abuse → Impulsivity → Average excess BMI | −0.001 (0.00) | −0.004, 0.002 |
| Physical abuse/neglect → Depression → Average excess BMI | −0.017 (0.02) | −0.050, 0.016 |
| Physical abuse/neglect → Impulsivity → Average excess BMI | −0.001 (0.00) | −0.007, 0.004 |
| Poly-maltreatment → Depression → Average excess BMI | −0.020 (0.02) | −0.060, 0.019 |
| Poly-maltreatment → Impulsivity → Average excess BMI | −0.001 (0.00) | −0.007, 0.004 |
| Covariates | ||
| Adolescent onset maltreatment | 0.284 (0.11) | 0.070, 0.497** |
| Male | −0.336 (0.11) | −0.549, −0.123* |
| Parental obesity | 2.324 (0.15) | 2.021, 2.627*** |
| Birthweight | 0.009 (0.00) | 0.005, 0.013*** |
| Breastfed, 6+ months | −0.248 (0.10) | −0.446, −0.051* |
| US born | 0.876 (0.19) | 0.508, 1.244*** |
| Parental employment | −0.051 (0.10) | −0.249, 0.147 |
| Hispanic (ref white) | 0.614 (0.15) | 0.317, 0.912*** |
| Black (ref white) | 0.987 (0.12) | 0.757, 1.218*** |
| Other (ref white) | 0.135 (0.28) | −0.407, 0.678 |
| Less than high school (ref college graduate) | 0.961 (0.16) | 0.643, 1.280*** |
| High school (ref college graduate) | 0.915 (0.16) | 0.603, 1.227 *** |
| Some college (ref. college graduate) | 0.454 (0.12) | 0.220, 0.687*** |
Note: Adolescent onset maltreatment, parental obesity, breastfed, US born, and parent employment are dichotomous indicator variables.
p < .05.
p < .01.
p < .001.
Highlights.
Maltreatment in adolescence increases risk for excess BMI
Friendship may protect against excess BMI regardless of maltreatment status
Future work may consider how to leverage friendships in obesity prevention
Acknowledgments:
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis.
Funding source: This work was supported by the National Institute of Child Health and Human Development (T32-HD07376), and by the National Institute on Drug Abuse of the National Institutes of Health (K01 DA035153). The funding sources had no involvement in the study design, data collection, analysis, interpretation, or writing of the report.
Footnotes
Declarations of interest: none.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Abbreviations: Body mass index (BMI); confirmatory factor analysis (CFA); latent class analysis (LCA); structural equation modeling (SEM); Transactional Model of Stress and Coping (TMSC)
References
- Afifi TO, & MacMillan HL (2011). Resilience following child maltreatment: A review of protective factors. The Canadian Journal of Psychiatry, 56(5), 266–272. [DOI] [PubMed] [Google Scholar]
- Ahrens KR, DuBois DL, Richardson LP, Fan M-Y, & Lozano P (2008). Youth in foster care with adult mentors during adolescence have improved adult outcomes. Pediatrics, 121(2), e246–e252. [DOI] [PubMed] [Google Scholar]
- Beasley JM, Newcomb PA, Trentham-Dietz A, Hampton JM, Ceballos RM, Titus-Ernstoff L, … Holmes MD (2010). Social networks and survival after breast cancer diagnosis. Journal of Cancer Survivorship, 4(4), 372–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke NJ, Hellman JL, Scott BG, Weems CF, & Carrion VG (2011). The impact of adverse childhood experiences on an urban pediatric population. Child Abuse Negl, 35(6), 408–413. doi: 10.1016/j.chiabu.2011.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, & McKay G (1984). Social support, stress and the buffering hypothesis: A theoretical analysis Handbook of psychology and health, 4, 253–267. [Google Scholar]
- Deutsch AR, Chernyavskiy P, Steinley D, & Slutske WS (2015). Measuring peer socialization for adolescent substance use: a comparison of perceived and actual friends' substance use effects. J Stud Alcohol Drugs, 76(2), 267–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ditzen B, & Heinrichs M (2014). Psychobiology of social support: the social dimension of stress buffering. Restor Neurol Neurosci, 32(1), 149–162. doi: 10.3233/rnn-139008 [DOI] [PubMed] [Google Scholar]
- DuBois DL, & Silverthorn N (2005). Natural mentoring relationships and adolescent health: Evidence from a national study. American Journal of Public Health, 95(3), 518–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, … Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American journal of preventive medicine, 14(4), 245–258. [DOI] [PubMed] [Google Scholar]
- Folkman S (2013). Stress: appraisal and coping Encyclopedia of behavioral medicine (pp. 1913–1915): Springer. [Google Scholar]
- Galvan A, & Rahdar A (2013). The neurobiological effects of stress on adolescent decision making. Neuroscience, 249, 223–231. doi: 10.1016/j.neuroscience.2012.09.074 [DOI] [PubMed] [Google Scholar]
- Glanz K, & Schwartz MD (2008). Stress, coping, and health behavior. Health behavior and health education: Theory, research, and practice, 4, 211–236. [Google Scholar]
- Graham JW, Olchowski AE, & Gilreath TD (2007). How many imputations are really needed? Some practical clarifications of multiple imputation theory. Prevention Science, 8(3), 206–213. [DOI] [PubMed] [Google Scholar]
- Harris K, Halpern C, Whitsel E, Hussey J, Tabor J, Entzel P, & Udry J (2016). The National Longitudinal Study of Adolescent to Adult Health: Research Desig. 2009. URL: http://www.cpc.unc.edu/projects/addhealth/design. Accessed, 5.
- Harris KM, Deeb-Sossa N, Perreira K, & Bollen K (2003). What Are We Measuring? An Evaluation of the CES-D Across Race, Ethnicity, and Immigrant Generation. Paper presented at the Add Health Users Conference, Bethesda, MD. [Google Scholar]
- Harris KM, Perreira KM, & Lee D (2009). Obesity in the transition to adulthood: predictions across race/ethnicity, immigrant generation, and sex. Archives of pediatrics & adolescent medicine, 163(11), 1022–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach: Guilford Press. [Google Scholar]
- Heatherton TF, & Baumeister RF (1991). Binge eating as escape from self-awareness. Psychological bulletin, 110(1), 86. [DOI] [PubMed] [Google Scholar]
- House JS (1987). Social support and social structure. Paper presented at the Sociological forum. [Google Scholar]
- Kim J, & Cicchetti D (2010). Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 51(6), 706–716. doi: 10.1111/j.1469-7610.2009.02202.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korczak DJ, Lipman E, Morrison K, & Szatmari P (2013). Are children and adolescents with psychiatric illness at risk for increased future body weight? A systematic review. Dev Med Child Neurol, 55(11), 980–987. doi: 10.1111/dmcn.12168 [DOI] [PubMed] [Google Scholar]
- Lazarus RS (1991). Emotion and adaptation: Oxford University Press on Demand. [Google Scholar]
- Lazarus RS, & Folkman S (1986). Cognitive theories of stress and the issue of circularity. Dynamics of stress: Physiological, psychological, and social perspectives, 63–80. [Google Scholar]
- Lazarus RS, & Folkman S (1987). Transactional theory and research on emotions and coping. European Journal of personality, 1 (3), 141–169. [Google Scholar]
- Li M, D'Arcy C, & Meng X (2015). Maltreatment in childhood substantially increases the risk of adult depression and anxiety in prospective cohort studies: systematic review, meta-analysis, and proportional attributable fractions. Psychological Medicine, 46(4), 717–730. doi: 10.1017/S0033291715002743 [DOI] [PubMed] [Google Scholar]
- Lumley T (2004). Analysis of complex survey samples. Journal of Statistical Software, 9(1), 1–19. [Google Scholar]
- Manly JT, Kim JE, Rogosch FA, & Cicchetti D (2001). Dimensions of child maltreatment and children's adjustment: contributions of developmental timing and subtype. Dev Psychopathol, 13(4), 759–782. [PubMed] [Google Scholar]
- Meagher-Stewart D (1994). The role of social support in recovery from cardiovascular illness. Can J Cardiovasc Nurs, 5(2), 19–29. [PubMed] [Google Scholar]
- Moore SE, Scott JG, Ferrari AJ, Mills R, Dunne MP, Erskine HE, … Norman RE (2015). Burden attributable to child maltreatment in Australia. Child Abuse Negl, 48, 208–220. doi: 10.1016/j.chiabu.2015.05.006 [DOI] [PubMed] [Google Scholar]
- Owen CG, Martin RM, Whincup PH, Smith GD, & Cook DG (2005). Effect of infant feeding on the risk of obesity across the life course: a quantitative review of published evidence. Pediatrics, 115(5), 1367–1377. [DOI] [PubMed] [Google Scholar]
- Parsons TJ, Power C, Logan S, & Summerbelt C (1999). Childhood predictors of adult obesity: a systematic review. International journal of obesity, 23. [PubMed] [Google Scholar]
- Sacks RM, Takemoto E, Andrea S, Dieckmann NF, Bauer KW, & Boone-Heinonen J (2017). Childhood Maltreatment and BMI Trajectory: The Mediating Role of Depression. Am J Prev Med, 53(5), 625–633. doi: 10.1016/j.amepre.2017.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedlak AJ, Mettenburg J, Basena M, Peta I, McPherson K, & Greene A (2010). Fourth national incidence study of child abuse and neglect (NIS-4). Washington, DC: US Department of Health and Human Services. Retrieved on July, 9, 2010. [Google Scholar]
- Short KH, & Johnston C (1997). Stress, maternal distress, and children's adjustment following immigration: the buffering role of social support. J Consult Clin Psychol, 65(3), 494–503. [DOI] [PubMed] [Google Scholar]
- Sokol RL; Shanahan ME; Gottfredson NC; Poti JM; Halpern CT; Fisher EB (2019. (under review)). Maltreatment experience in childhood and average excess body mass from adolescence to young adulthood. Child abuse & neglect. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokol RL, Gottfredson NC, Poti JM, Halpern CT, Shanahan ME, Fisher EB, & Ennett ST (2018). Does a parsimonious measure of complex body mass index trajectories exist? International journal of obesity. doi: 10.1038/s41366-018-0194-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokol RL, Gottfredson NC, Shanahan ME, & Halpern CT (2018). Relationship between child maltreatment and adolescent body mass index trajectories. Children and Youth Services Review, 93, 196–202. doi: 10.1016/j.childyouth.2018.07.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thamotharan S, Lange K, Zale EL, Huffhines L, & Fields S (2013). The role of impulsivity in pediatric obesity and weight status: a meta-analytic review. Clin Psychol Rev, 33(2), 253–262. doi: 10.1016/j.cpr.2012.12.001 [DOI] [PubMed] [Google Scholar]
- Vachon DD, Krueger RF, Rogosch FA, & Cicchetti D (2015). Assessment of the Harmful Psychiatric and Behavioral Effects of Different Forms of Child Maltreatment. JAMA Psychiatry, 72(11), 1135–1142. doi: 10.1001/jamapsychiatry.2015.1792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeidner M, & Saklofske D (1996). Adaptive and maladaptive coping. [Google Scholar]