Abstract
Aims.
To examine differences in high-intensity drinking (HID) by parental status, parent age, and parent sex, including two- and three-way interaction effects of these parent demographic categories.
Methods.
The present study included individuals ages 18-50 from the National Epidemiologic Study of Alcohol and Related Conditions-III (2012-13), a sample of non-institutionalized adults in the US (N=22,278). We calculated weighted estimates of past-year HID (≥10/≥8 standard drinks for men/women on a single occasion) for each parental status group (parents of young children <5, parents of children 5-17, not parents of children <18) overall and stratified by sex and stratified by age. We then examined the overall association of parental status and HID and tested for interactions of parental status × sex, parental status × age, and parental status × age × sex, while controlling for other relevant sociodemographic characteristics.
Results.
Prevalence of HID varied considerably by parental status, with 14.84% of parents with kids under age 5, 12.72% of parents with kids 5 to 17, and 23.15% of non-parents reporting HID. The strength of the associations of parenthood and HID were strongest for females and for older parents.
Conclusions.
While parents engage in HID less than those who are not parents, a portion of parents of young and adolescent children do report heavy drinking. Younger parents and male parents, in particular, are at high risk for HID. Given the risks to children and parents, interventions focused on preventing HID among parents, especially fathers, could have significant public health impacts.
1. Introduction
Parental alcohol use confers risk to children’s physical and mental health. For example, infant mortality and sudden infant death syndrome (SIDS) are associated with maternal alcohol use and alcohol use disorder (1–4). Throughout childhood, parental alcohol use disorder is associated with an increased risk of abuse, neglect, and child welfare involvement (5,6). Children of parents with alcohol use disorder symptoms are at heightened risk for negative health outcomes, such as early initiation of substance use, conduct disorders, and mental illness (7–10). Even occasional parental alcohol use can pose risks to children: 24% of parents with young children say they are unlikely to plan drinking limits or next-day childcare when drinking alcohol for special events (11), leaving children vulnerable to insufficient care.
High-intensity drinking (HID) is a type of heavy drinking characterized by consuming twice the number of drinks traditionally associated with binge drinking. HID is associated with particular risks, including an increased risk of alcohol-related injuries, driving accidents, and blacking out (12–14). Previous research has not documented the extent to which parents of young and adolescent children engage in HID, or whether prevalence differs by child age, or parent age and sex. Parents of younger children are more likely to decrease their alcohol use than parents of older children (15). While young children under the age of 5 require more hands-on caregiving, school-aged children continue to require care and supervision and they are susceptible to the modeling of alcohol use by parents (16,17).
Despite the fact that parental HID is likely to have particularly negative consequences for children, only one previous study has examined the relationship between HID and parental status (18): parents at age 25/26 were less likely to engage in HID than non-parents. Understanding characteristics of parents most at risk for HID will identify children most at risk and inform the development of targeted interventions for parents.
Although parenthood is generally associated with a decrease in alcohol use (19–21) including HID (18), some studies showing no or reverse associations (22–24). Disparate findings may be because some parents are more likely to reduce drinking than others. For example, women are consistently found to decrease alcohol use in response to parenthood but findings related to men’s response are varied and often smaller than those for women (22,25–29). Additionally, in contrast to general decrease in alcohol use among parents, becoming a parent before age 25 is sometimes associated with increased alcohol and substance use (20,30,31). Compared to older mothers, mothers under 25 were most likely to binge drink in the first year of their child’s life; mothers over 36 years old when their child was born had the highest proportion of binge drinkers five years later (32–34). The current study is one of the first to compare the associations between parental status and HID for men and women, allowing direct comparisons of mothers’ and fathers’ drinking.
1.1. Research Aims
The purpose of this paper is to examine the relationship between parental status and HID. Building on findings from previous studies, we also examine sex and age differences in this relationship. Specific research aims were to examine: (1) differences in HID by parental status (i.e., parents of young children under age 5, parents of children ages 5 to 17, and adults with no children under age 18 living with them), (2) the association of parental status with HID, for women and men, and (3) the three-way interaction of parental status, age, and sex on HID.
2. Method
2.1. Sample
Data were drawn from the National Epidemiologic Study of Alcohol and Related Conditions-III (NESARC-III) collected in 2012-13. NESARC-III is a nationally representative survey of non-institutionalized civilian adults in the US 18 and older (N=36,309). NESARC-III had a household- and person-level response rate of 72% and 84%, respectively. Institutional Review Boards at National Institutes of Health and Westat approved the study. This study focused on those who were ages 18 to 50 and had data on parental status and drinking (n=22,278; 50.95% female; 59.52% White non-Hispanic, 13.12% Black non-Hispanic, 6.72% Asian non-Hispanic, and 18.96% Hispanic).
2.2. Measures
Individuals self-reported the largest number of drinks they had consumed in a single day in the last 12 months. High-intensity drinking (HID) was defined as one or more past-year occasions in which men consume 10 or more and women consume 8 or more standard drinks.
Parental status.
We contrasted those who were parents of children under 5 who lived with them, those who were parents of children age 5-17 who lived with them, and those who did not have any children under age 18 living with them. Those with multiple children were categorized based on their youngest child.
Age (18-24, 25-35, and 36-50 years) and sex (male, female) were used as predictors and moderators. Race/ethnicity (White non-Hispanic, Black non-Hispanic, American Indian/Alaska Native non-Hispanic, Asian non-Hispanic, and Hispanic), family income tertiles (<$25,000, $25,000-$59,999, and $60,000+), and marital status (married, living with someone as if married, widowed, divorced, separated, and never married) were included as controls.
2.3. Analysis
We first estimated the prevalence of HID by parental status (aim 1). We also examined HID prevalence by parental status and by age for adults 18-24, 25-35, and 36-50 years old, separately for men and women, using design-based Pearson chi-square to test for differences. Using multivariable logistic regression, we examined the overall associations of parental status and HID, separately for women and men, and tested for interactions of parental status × sex (aim 2) and parental status × age × sex (aim 3) while controlling for other relevant sociodemographic characteristics. NESARC-III survey weights were used to adjust for oversampling and nonresponse, and weight respondents to represent the US civilian population.
3. Results
3.1. Overall prevalence of HID by parental status
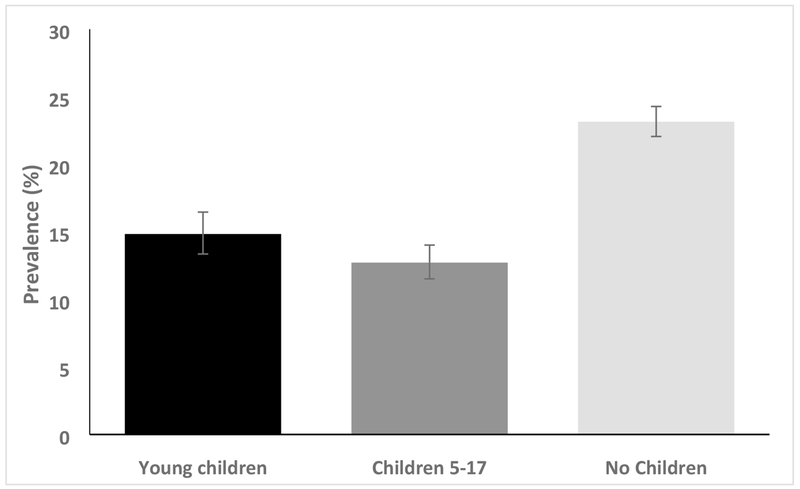
Overall, 19.15% of adults age 18 to 50 engaged in HID in the past year. In Figure 1 we present prevalence of HID by parental status. The prevalence of HID differed significantly by parental status (χ2(113)=101.05, p<0.001). Specifically, HID prevalence was greater for nonparents (23.15% [95% CI: 22.06%, 24.28%]) compared to parents of young children less than age 5 (14.84% [13.36%, 16.46%]) and parents with children 5-17 (12.72% [11.52%, 14.02%]). Parents with children under age 5 were significantly more likely to engage in HID compared to those with children age 5-17.
Figure 1. Weighted prevalence of high-intensity drinking in the past year by parental status among adults aged 18 to 50.
Note: error bars represent 95% confidence intervals.
3.2. Prevalence of HID by parental status and sex
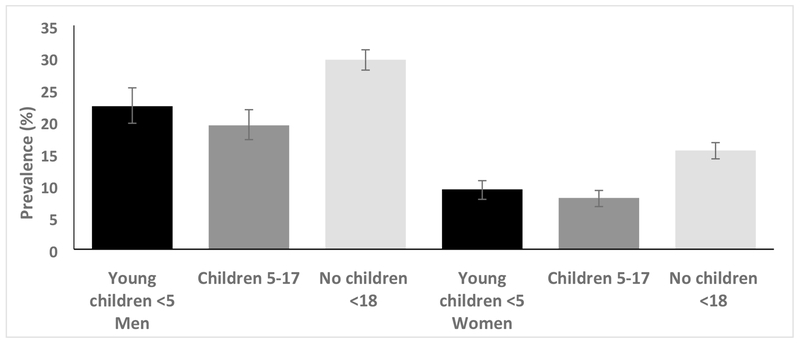
Shown in Figure 2, we examined prevalence of HID by parental status separately for men and women. Among men and women, HID prevalence differed significantly by parental status (χ2(113)=30.68, p<0.001 and χ2(113)=46.92, p<0.001, respectively). Both men and women who were parents (with children less than age 5 or children ages 5-17) had lower prevalence of HID (22.35% [19.70%, 25.24%] and 19.37% [17.14%, 21.82%] for men, and 9.36% [8.00%, 10.92%] and 8.02% [6.85%, 9.37%] for women, respectively) compared to those without children (29.63% [28.07%, 31.25%] for men and 15.44% [14.21%, 16.75%] for women).
Figure 2. Weighted prevalence of high-intensity drinking in the past year by parental status and sex among adults aged 18 to 50.
Note: error bars represent 95% confidence intervals.
3.3. Prevalence of HID by parental status and age
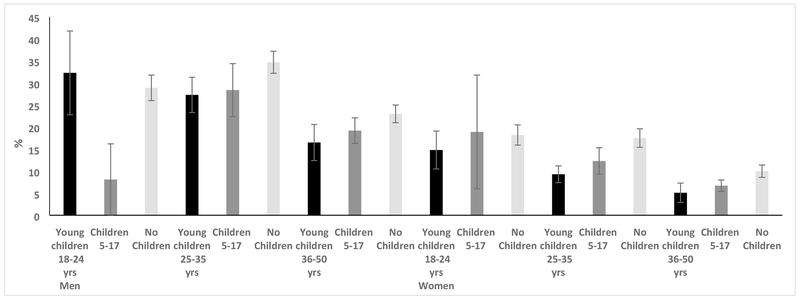
Shown in Figure 3, we examined prevalence of HID by parental status separately by age. In all three age groups (18-24, 25-35, and 36-50) HID differed significantly by parental status (χ2(113)=6.33, p=0.002; χ2(113)=40.62, p<0.001, χ2(113)=23.42, p<0.001, respectively) such that HID prevalence was significantly lower for both parental groups compared to non-parents. Among 18-24 year olds, 18.86% (15.01%, 23.42%) of parents with children under 5, 14.14% (7.73%, 24.47%) of parents with children 5-17, and 25.94% (23.90%, 28.08%) of those with no children reported HID. Among 25-35 year olds, comparable prevalence levels were 15.98% (14.03%, 18.13%) and 16.98% (14.35%, 19.99%) of parents with young and adolescent children, and 27.92% (26.31%, 29.60%) of non-parents. Finally, among 36-50 year olds, 9.94% (7.82%, 12.56%) and 11.38% (10.09%, 12.81%) of parents with young and adolescent children and 16.97% (15.63%, 18.41%) of non-parents reported HID.
Figure 3. Weighted prevalence of high-intensity drinking in the past year by parental status and age, separately for women and men, among adults aged 18 to 50.
Note: error bars represent 95% confidence intervals. Ages 18-24, 25-35, and 36-50 represent ages of adults in the sample and Young children, Children 5-17, No Children represent parental status categories.
3.4. Multivariable associations of parental status and HID for men and women
In multivariable regression, we first examined overall associations of parental status and HID while controlling for sociodemographic factors (i.e., age, marital status, race/ethnicity, and family income), separately for men and women. Both men and women who were parents of young children under age 5 and who were parents of older children aged 5-17 were significantly less likely to engage in HID, compared to those with no children under age 18 (Table 1 Main Effects Models). There was a significant parental status × sex interaction (not shown). The negative association of having young children <5 or children 5-17 (vs. no children <18) with HID was stronger for women compared to men.
Table 1.
Parental Status as a Predictor of HID among adults aged 18-50, separately for women and men
| MEN | WOMEN | |||||||
|---|---|---|---|---|---|---|---|---|
| Main Effects Model | Interactions Model | Main Effects Model | Interaction Model | |||||
| AORb | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Parental status | ||||||||
| Young children <5 years | 0.71 | 0.58, 0.87* | 1.01 | 0.64, 1.59 | 0.62 | 0.51, 0.75* | 0.80 | 0.56, 1.15 |
| Children 5-17 years old | 0.76 | 0.64, 0.91* | 0.19 | 0.05, 0.67* | 0.73 | 0.59, 0.91* | 1.07 | 0.45, 2.53 |
| No children <18 years old | REF. | REF. | REF. | REF. | ||||
| Age | ||||||||
| 18-24 | REF. | REF. | REF. | REF. | ||||
| 25-35 | 1.25 | 1.06, 1.47* | 1.27 | 1.07, 1.50* | 0.94 | 0.78, 1.14 | 1.01 | 0.81, 1.25 |
| 36-50 | 0.73 | 0.61, 0.87* | 0.73 | 0.61, 0.89* | 0.54 | 0.44, 0.67* | 0.52 | 0.42, 0.65* |
| Marital status | ||||||||
| Never married | REF. | REF. | REF. | REF. | ||||
| Married | 0.76 | 0.64, 0.90* | 0.74 | 0.62, 0.88* | 0.53 | 0.44, 0.64* | 0.53 | 0.44, 0.64* |
| Living with someone as if married | 1.29 | 1.06, 1.57* | 1.25 | 1.04, 1.52* | 1.16 | 0.90, 1.49 | 1.14 | 0.89, 1.46 |
| Widowed | 0.40 | 0.16, 0.98* | 0.39 | 0.16, 0.96* | 0.86 | 0.38, 1.95 | 0.85 | 0.37, 1.93 |
| Divorced | 0.97 | 0.79, 1.19 | 0.95 | 0.77, 1.71 | 0.87 | 0.67, 1.13 | 0.86 | 0.66, 1.12 |
| Separated | 1.22 | 0.85, 1.73 | 1.19 | 0.83, 1.71 | 1.12 | 0.77, 1.64 | 1.10 | 0.76, 1.60 |
| Race/ethnicity | ||||||||
| White non-Hispanic | REF. | REF. | REF. | REF. | ||||
| Black non-Hispanic | 0.40 | 0.33, 0.49* | 0.40 | 0.33, 0.49* | 0.37 | 0.30, 0.47* | 0.37 | 0.30, 0.47* |
| AI/ANa non-Hispanic | 1.28 | 0.77, 2.10 | 1.28 | 0.77, 2.12 | 1.92 | 1.13, 3.27* | 1.91 | 1.12, 3.25* |
| Asian non-Hispanic | 0.51 | 0.39, 0.65* | 0.51 | 0.39, 0.65* | 0.40 | 0.26, 0.62* | 0.40 | 0.26, 0.62* |
| Hispanic | 0.81 | 0.69, 0.95* | 0.81 | 0.69, 0.94* | 0.66 | 0.54, 0.81* | 0.66 | 0.54, 0.80* |
| Family income | ||||||||
| Low | REF. | REF. | REF. | REF. | ||||
| Medium | 0.90 | 0.77, 1.04 | 0.90 | 0.78, 1.05 | 0.85 | 0.72, 1.00 | 0.84 | 0.71, 0.99* |
| High | 0.92 | 0.77, 1.09 | 0.92 | 0.77, 1.10 | 0.84 | 0.69, 1.02 | 0.85 | 0.70, 1.03 |
| Parental status × Parental age | ||||||||
| Parenting young children×age 25-35 | 0.70 | 0.43, 1.13 | 0.68 | 0.43, 1.06 | ||||
| Parenting young children×age 36-50 | 0.64 | 0.38, 1.10 | 0.65 | 0.34, 1.24 | ||||
| Children 5-17×age 25-35 | 3.92 | 1.05, 14.66* | 0.65 | 0.26, 1.65 | ||||
| Children 5-17×age 36-50 | 4.23 | 1.16, 15.38* | 0.66 | 0.27, 1.57 | ||||
American Indian/Alaska Native
Adjusted odds ratio
p<0.05
3.5. Interactions of parental status by age for men and women
Next, we examined potential interactions of parental status with age. We found a significant interaction of parental status × age for men and women. Among men, the negative association of having young children with HID (vs. no children <18) was stronger for those aged 25-35 and for those aged 36-50 compared to those aged 18 to 24 (Table 1). There was no significant association among women (Table 1 Interaction Models).
The three-way interaction of parental status, parent age, and sex was significant (p<0.020). As seen in Table 1, for men the association of having children 5-17 with HID when a parent is 25-35 (aOR: 3.92) The 3-way interaction can also be visualized in Figure 3 where there is greater variability in prevalence between parental age categories for men than for women.
4. Discussion
There are no specific guidelines for parents’ alcohol use, even around their children, despite binge drinking and parental alcohol use disorder carrying present and future risks for children (35–37). This study is the first to document rates of HID among parents of children of various ages. Our findings highlight specific areas of public health concern. Although parenthood is associated with decreased drinking overall (18,19), many parents continue to engage in HID after having children. In particular, nearly 15% of parents of children under age 5, and nearly 13% of parents with children ages 5-17 have engaged in HID in the last year. Adults who continue to drink alcohol at high levels after transitioning to parenthood may represent a non-responder group. The interactions we analyzed showed that parents who are men or younger are less likely to have decreased levels of HID compared to parents who are women or older, respectively. The differences between mothers and fathers were largest when parenting young children, perhaps reflecting a time when sex differences in childrearing tend to be the greatest. Interventions for fathers, especially of fathers of infants and preschool-aged children, and for adults who become parents at younger ages should focus on reducing HID.
Prevalence of HID for those with young children were particularly low for older parents. This finding, along with the findings of Liu et al. (32–34), suggests that older parents may adjust their alcohol use in response to parenting more than younger parents. Younger parents (e.g., ages 18 to 24) may require more support to reduce their drinking, possibly to address factors relating to things such as unplanned parenthood, difficulties with financial or other resources, and greater social pressure to drink heavily as is normative among their peers.
The primary limitation of this study is that the relatively broad predictors necessarily obscure some heterogeneity within groups and do not differentiate HID that occurred while responsible for children or while children were being cared for by others. Furthermore, only data on children living with the adults were available, so people in the no children group may have been parents of children not residing with them. Future research should examine contexts of parent drinking, whether children were present, and parenting quality during and after drinking occasions.
In sum, parents are generally less likely to engage in HID than non-parents, but the significant portion of parents who engage in HID—particularly fathers and younger parents—represent a public health concern. Interventions should target parental HID and guidance should be given to parents on ways to recognize and minimize risks their drinking poses for their children.
Highlights.
Prevalence of high-intensity drinking (HID) varied by parental status and sex.
Parents reported HID less than non-parents; women less than men.
Parenting a young child was associated with a greater decrease for women than men.
Younger (aged 18 to 24) and male parents are at higher risk for HID.
Acknowledgements.
Development of this manuscript was supported by research grant R01AA023504 to M. Patrick from the National Institute on Alcohol Abuse and Alcoholism. The study sponsors had no role in the study design, collection, analysis or interpretation of the data, writing of the manuscript, or the decision to submit the paper for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the study sponsors.
Role of Funding Sources
Development of this manuscript was supported by research grant R01AA023504 from the National Institute on Alcohol Abuse and Alcoholism to M. Patrick. The study sponsors had no role in the study design, collection, analysis or interpretation of the data, writing of the manuscript, or the decision to submit the paper for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the study sponsor.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
All authors declare that they have no conflicts of interest.
References
- 1.Alm B, Wennergren G, Norvenius G, R Skjærven, N Øyen, K Helweg-Larsen, et al. Caffeine and alcohol as risk factors for sudden infant death syndrome. Arch Dis Child. 1999;81(2):107–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Friend KB, Goodwin MS, Lipsitt LP. Alcohol use and sudden infant death syndrome. Dev Rev. 2004;24(3):235–51. [Google Scholar]
- 3.O’Leary CM, Jacoby PJ, Bartu A, D’Antoine H, Bower C. Maternal alcohol use and Sudden Infant Death Syndrome and infant mortality excluding SIDS. Pediatrics. 2013;131(3):e770–8. [DOI] [PubMed] [Google Scholar]
- 4.Phillips DP, Brewer KM, Wadensweiler P. Alcohol as a risk factor for sudden infant death syndrome (SIDS). Addiction. 2011;106(3):516–25. [DOI] [PubMed] [Google Scholar]
- 5.Kelleher K, Chaffin M, Hollenberg J, Fischer E. Alcohol and drug disorders among physically abusive and neglectful parents in a community-based sample. Am J Public Health. 1994;84(10):1586–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Young NK, Boles SM, Otero C. Parental substance use disorders and child maltreatment: Overlap, gaps, and opportunities. Child Maltreat. 2007;12(2):137–49. [DOI] [PubMed] [Google Scholar]
- 7.Chassin L, Pitts SC, DeLucia C, Todd M. A longitudinal study of children of alcoholics: Predicting young adult substance use disorders, anxiety, and depression. J Abnorm Psychol. 1999;108(1):106–19. [DOI] [PubMed] [Google Scholar]
- 8.Hussong AM, Flora DB, Curran PJ, Chassin LA, Zucker RA. Defining risk heterogeneity for internalizing symptoms among children of alcoholic parents. Dev Psychopathol. 2008;20(1):165–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Latendresse SJ, Rose RJ, Viken RJ, Pulkkinen L, Kaprio J, Dick DM. Parenting Mechanisms in Links between Parents’ and Adolescents’ Alcohol Use Behaviors. Alcohol Clin Exp Res. 2008;32(5):322–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marmorstein NR, Iacono WG, McGue M. Alcohol and illicit drug dependence among parents: Associations with offspring externalizing disorders. Psychol Med. 2009;39(1):149–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.C.S. Mott Children’s Hospital. Mott Poll Report. Vol. 33 2018. [Google Scholar]
- 12.Evans-Polce RJ, Patrick ME, O’Malley PM. Prospective associations of 12th-grade drinking intensity and age 19/20 driving-related consequences. J Adolesc Heal. 2017. September;61(3):389–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Read JP, Beattie M, Chamberlain R, Merrill JE. Beyond the “Binge” threshold: Heavy drinking patterns and their association with alcohol involvement indices in college students. Addict Behav. 2008;33(2):225–34. [DOI] [PubMed] [Google Scholar]
- 14.Mundt MP, Zakletskaia LI, Fleming MF. Extreme College Drinking and Alcohol-Related Injury Risk. Alcohol Clin Exp Res. 2009;33(9):1532–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Staff J, Greene KM, Maggs JL, Schoon I. Family transitions and changes in drinking from adolescence through mid-life. Addiction. 2014;109(2):227–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ennett ST, Jackson C, Bowling JM, Dickinson DM. Parental Socialization and Children’s Susceptibility to Alcohol Use Initiation. J Stud Alcohol Drugs. 2013;74(5):694–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tildesley EA, Andrews JA. The Development of Children’s Intentions to Use Alcohol: Direct and Indirect Effects of Parent Alcohol Use and Parenting Behaviors. Psychol Addict Behav. 2008;22(3):326–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Terry-McElrath YM, Patrick ME. Intoxication and binge and high-intensity drinking among US young adults in their mid-20s. Subst Abus. 2016;37(4):597–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Condon JT, Boyce P, Corkindale CJ. The First-Time Fathers Study: a prospective study of the mental health and wellbeing of men during the transition to parenthood. Vol. 38, Australian and New Zealand Journal of Psychiatry. 2004. [DOI] [PubMed] [Google Scholar]
- 20.Little M, Handley E, Leuthe E, Chassin L. The impact of parenthood on alcohol consumption trajectories: Variations as a function of timing of parenthood, familial alcoholism, and gender. Dev Psychopathol. 2009;21(2):661–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wolfe JD. Age at first birth and alcohol use. J Health Soc Behav. 2009;50(4):395–409. [DOI] [PubMed] [Google Scholar]
- 22.Leonard KE, Eiden RD. Marital and Family Processes in the Context of Alcohol Use and Alcohol Disorders. Annu Rev Clin Psychol. 2007;3:285–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paradis C, Demers A, Nadeau L, Picard E. Parenthood , Alcohol Intake , and Drinking Contexts : Occasio Furem Facit *. J Stud Alcohol Drugs. 2011;72:259–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Richman JA, Rospenda KM, Kelley MA. Gender roles and alcohol abuse across the transition to parenthood. J Stud Alcohol. 1995;56(5):553–7. [DOI] [PubMed] [Google Scholar]
- 25.Christie-Mizell CA, Peralta RL. The Gender Gap in Alcohol Consumption during Late Adolescence and Young Adulthood: Gendered Attitudes and Adult Roles*. Vol. 50, Journal of Health and Social Behavior. 2009. [DOI] [PubMed] [Google Scholar]
- 26.Fergusson DM, Boden JM, John Horwood L. Transition to parenthood and substance use disorders: Findings from a 30-year longitudinal study. Drug Alcohol Depend. 2012;125(3):295–300. [DOI] [PubMed] [Google Scholar]
- 27.Neve RJM, Lemmens PH, Drop MJ. Changes in alcohol use and drinking problems in relation to role transitions in different stages of the life course. Subst Abus. 2000;21(3):163–78. [DOI] [PubMed] [Google Scholar]
- 28.Ahlström S, Bloomfield K, Knibbe R. Gender differences in drinking patterns in nine European countries: Descriptive findings. Subst Abus. 2001;22(l):69–85. [DOI] [PubMed] [Google Scholar]
- 29.Borschmann R, Becker D, Spry E, Youssef GJ, Olsson CA, Hutchinson DM, et al. Alcohol and parenthood: An integrative analysis of the effects of transition to parenthood in three Australasian cohorts. Drug Alcohol Depend. 2019;197(January):326–34. [DOI] [PubMed] [Google Scholar]
- 30.Kokko K, Pulkkinen L, Mesiäinen P. Timing of parenthood in relation to other life transitions and adult social functioning. Int J Behav Dev. 2009;33(4):356–65. [Google Scholar]
- 31.Krohn MD, Lizotte AJ, Perez CM. The Interrelationship Between Substance Use and Precocious Transitions to Adult Statuses. J Health Soc Behav. 1997;38(1):87–103. [PubMed] [Google Scholar]
- 32.Liu W, Mumford EA, Petras H. Maternal Patterns of Postpartum Alcohol Consumption by Age: A Longitudinal Analysis of Adult Urban Mothers. Prev Sci. 2015;16(3):353–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu W, Mumford EA, Petras H. Maternal Alcohol Consumption During the Perinatal and Early Parenting Period: A Longitudinal Analysis. Matern Child Health J. 2016;20(2):376–85. [DOI] [PubMed] [Google Scholar]
- 34.Liu W, Mumford EA. Concurrent Trajectories of Female Drinking and Smoking Behaviors Throughout Transitions to Pregnancy and Early Parenthood. Prev Sci. 2017;18(4):416–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Malone SM, Iacono WG, McGue M. Drinks of the Father: Father’s Maximum Number of Drinks Consumed Predicts Externalizing Disorders, Substance Use, and Substance Use Disorders in Preadolescent and Adolescent Offspring. Alcohol Clin Exp Res. 2002;26(12):1823–32. [DOI] [PubMed] [Google Scholar]
- 36.Malone SM, Mcgue M, Iacono WG. Mothers’ maximum drinks ever consumed in 24 hours predicts mental health problems in adolescent offspring. J Child Psych Psychiatry. 2010;51(9):1067–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Balsa AI, French MT. The impact of parental drinking on children’s use of health care. Subst Use Misuse. 2012;47(4):450–60. [DOI] [PubMed] [Google Scholar]