Abstract
Objectives:
Morbidity and mortality from intussusception, the leading cause of bowel obstruction in infants, is higher in Africa than in other regions of the world, but the reasons have not been well examined. We sought to identify risk and protective factors associated with death or intestinal resection following intussusception.
Methods:
Infants with intussusception from 7 sub-Saharan African countries (Ethiopia, Ghana, Kenya, Malawi, Tanzania, Zambia, and Zimbabwe) were enrolled through active, hospital-based surveillance from February 2012 to December 2016. We examined demographic, clinical, and socioeconomic factors associated with death or intestinal resection following intussusception, using multivariable logistic regression.
Results:
A total of 1017 infants <1 year of age with intussusception were enrolled. Overall, 13% of children (133/1017) died during the hospitalization, and 48% (467/966) required intestinal resection. In multivariable analyses, female sex (OR 1.8, 95% CI 1.2–3.3), longer duration of symptoms prior to presentation (OR 1.1; 95% CI 1.0–1.2), and undergoing intestinal resection (OR 3.4; 95% CI 1.9–6.1) were associated with death after intussusception. Diagnosis by ultrasound or enema (OR 0.4; 95% CI 0.3–0.7), and employment of a household member (OR 0.7; 95% CI 0.4–1.0) were protective against intestinal resection.
Conclusion:
Delays in hospital presentation and female sex were significantly associated with death, whereas higher socioeconomic status and availability of radiologic diagnosis reduced likelihood of undergoing resection. Efforts should be intensified to improve the awareness, diagnosis, and management of intussusception in sub-Saharan African countries to reduce morbidity and mortality from intussusception in these resource limited settings.
Keywords: bowel obstruction, death, intestinal resection
Introduction
Intussusception, or the invagination of one segment of the intestine within another segment, is the most common cause of bowel obstruction in infants.[1] It is a pediatric emergency and can result in intestinal ischemia and necrosis, potentially requiring intestinal resection.[2] Prompt diagnosis and treatment are essential as untreated intussusception may be fatal.[3] Regional variations in mortality and morbidity following intussusception exist; among children less than one year of age with intussusception, case-fatality is higher in Africa (9%) as compared to other regions (<1%).[4]. Diagnostic modality also differed substantially in Africa as compared to other regions of the world; while 95–100% of cases globally were diagnosed using a radiographic modality, 65% of cases from Africa were diagnosed clinically or surgically.[4] In a systematic review of 16 intussusception studies in Africa, 87% received surgical intervention.[5]
The reasons for the greater morbidity and mortality from intussusception in African infants are unclear. African country-specific studies report a high proportion of infants experience symptoms for more than 3 days prior to admission, suggesting that delay in diagnosis or a delay in seeking care may be a contributing factor.[5-7] Decreased availability of radiological diagnostics and non-invasive treatment modalities at healthcare facilities may also be delaying timely management.[8,9] However, examination of these risk factors has been limited due to low numbers of cases in country-specific studies. Furthermore, there is a paucity of data regarding the role of individual-level socioeconomic status (SES) factors, such as availability of household electricity, employment status in the household, and access to transportation in predicting poor outcomes following intussusception.
In this evaluation we describe the epidemiology of intussusception in infants across 7 sub-Saharan African countries, and examined demographic, clinical, and SES factors associated with death or intestinal resection.
Methods
Study aims
The primary aim of this evaluation was to examine the epidemiology and risk factors associated with death from intussusception in sub-Saharan African infants. The secondary aim was to examine risk factors associated with intestinal resection during hospitalization for intussusception.
Study design
Infants enrolled in the Rotarix (RV1) African intussusception surveillance network, an intussusception active surveillance network of 29 sentinel hospitals in seven sub-Saharan African countries that were early adopters of RV1 (Ethiopia, Ghana, Kenya, Malawi, Tanzania, Zambia, and Zimbabwe), were included in this evaluation. The participating sentinel hospitals and active surveillance protocol have been described elsewhere.[10] Briefly, infants were enrolled if they were younger than 12 months of age and met the Brighton Collaboration criteria for level 1 of diagnostic certainty for intussusception.[11] The year of vaccine introduction varied by country, and so countries joined the network and sentinel hospitals began enrollment on a rolling basis, beginning in February 2012 and ending for all participating countries in December 2016. Sentinel hospitals were regionally diverse within country, and major pediatric hospitals were included to identify the most cases of intussusception. Sentinel hospitals had surgical units and were able to provide surgical treatment for intussusception. Infants enrolled in intussusception active surveillance were included in this analysis if outcome of the hospitalization was available. Infants were excluded if intussusception spontaneously resolved and thus did not require radiological or surgical intervention.
Statistical analysis
Potential risk factors were screened in bivariate analyses for both the primary (death) and secondary (intestinal resection) outcomes.(Supplementary materials, Tables 1 and 2) All variables significantly associated with the outcome (p value < 0.15) in bivariate analyses were included in the initial multivariable model. An a priori decision was also made to include age, sex, country, and year of enrollment in the initial model. Risk factors were then identified by multivariable logistic regression using backward elimination, using a p value criteria of <0.05.
Results
Patient characteristics and demographics
A total of 1017 children under 12 months of age and diagnosed with intussusception were enrolled in surveillance in 29 sentinel hospitals. (Table 1)
Table 1:
Demographic and social patient characteristics
| Variables | n/N (%)a |
|---|---|
| Total | 1017 |
| Age in weeks at diagnosis (Median, 25, 75 IQR) | 27 (21, 33) |
| Female sex | 414/1016 (40.8) |
| Household employment statusb | 593/888 (66.8) |
| Household electricity statusb | |
| Present 24hours per day | 522/872 (59.9) |
| Present some hours | 109/872 (12.5) |
| Household transportation status | |
| Bicycleb | 317/907 (35.0) |
| Motorcycleb | 83/903 (9.2) |
| Carb | 193/902 (21.4) |
| Household electronics status | |
| Computerb | 154/899 (17.1) |
| Telephoneb | 714/910 (78.5) |
| Televisionb | 613/910 (67.4) |
| Radiob | 703/909 (77.3) |
| Household appliance status | |
| Refrigeratorb | 339/907 (37.4) |
Unless otherwise specified. Missing values excluded from the denominator.
Missing data for 10-15% of patients
Of the 1017 infants included in the analyses, the median age of admission for intussusception was 27 weeks (interquartile range, 21 to 33), with only 28 (3%) cases detected in infants less than 12 weeks of age. (Figure 1) The majority of infants (59%, 602/1017) were male. The median birthweight was 3.3 kilograms and 98% (906/927) were breastfed. Among the infants with information available, 67% (593/888) lived in a household in which at least one person was employed, and 72% (631/872) lived in a household with electricity at least part of the time.
Figure 1:
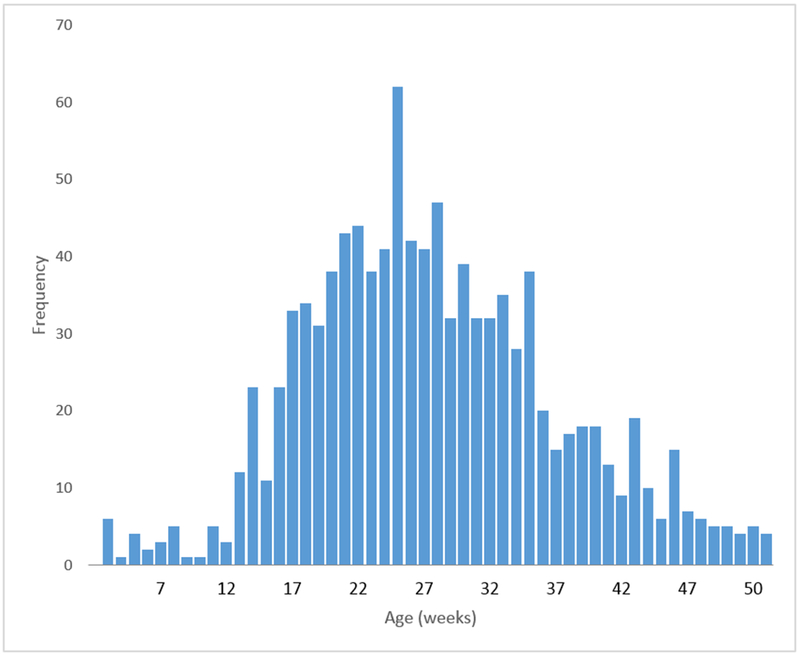
Distribution of infants by age in weeks
Characteristics of intussusception and clinical course
The median duration of symptoms prior to hospitalization at the sentinel hospital was 3 days (interquartile range 1 to 4), and the median duration of symptoms prior to hospitalization at any hospital was 2 days (IQR: 0–3).(Table 2) Of the 313 infants in which symptom onset began over 3 days prior to hospitalization at the treatment facility, 86% came from households without a car. In the majority of children, intussusception was diagnosed surgically (65%, 663/1017) and treated surgically (85%, 851/996). Overall, 13% of children (133/1017) died during the hospitalization. Intestinal resection was performed on 48% of children (467/966); of these children, 21% (97/467) died.
Table 2:
Features of intussusception and clinical course
| Variables | n/N (%)a |
|---|---|
| Total | 1017 |
| Clinical characteristics | |
| Child’s birthweight (kilograms) (Median, IQR) | 3.3 (2.9, 3.7) |
| Breastfed (yes) | 906/927 (97.7) |
| Days from symptom onset to IS admission at sentinel site hospital (median, IQR) | 3 (1, 4) |
| Days from symptom onset to IS admission at hospital where care first sought | 2 (0, 3) |
| Transferred from previous facilityb | 598/779 (76.8) |
| If transferred: days from first hospital admission to sentinel site hospital admission | 1 (0, 2) |
| If transferred: Days from symptom onset to IS admission at hospital where care first sought (median, IQR) | 1 (0, 3) |
| Method of IS diagnosis | |
| Clinical alone | 154/1015 (15.2) |
| US and/or enema (+/− clinical) | 215/1017 (21.1) |
| Surgery (+/− clinical, US, enema) | 663/1017 (65.2) |
| IS treatment | |
| Enema | 145/996 (14.6) |
| Surgery | 851/996 (85.4) |
| Outcome | |
| Resection performed (Yes) | 467/966 (48.3) |
| Of those that survived, % resection performed | 370/837 (44.2) |
| Of those that received surgery (diagnostic or treatment), % resection performed | 462/825 (56.0) |
| Of those that received resection, % died | 97/467 (20.8) |
| Death (Yes) | 133/1017 (13.1) |
Unless otherwise specified. Missing data excluded from the denominators.
Missing data for 20%-30% of patients
Abbreviations: IS = Intussusception, IQR = Interquartile range
Risk factors associated with death or intestinal resection after intussusception
In the adjusted primary analyses, female sex (OR 1.98, 95% CI 1.20–3.27), longer duration of symptoms (OR 1.08; 95% CI 1.01–1.15), and intestinal resection (3.43; 95% CI 1.90–6.15) were associated with death after intussusception. (Table 3)
Table 3:
Clinical and social risk factors that independently predict death or intestinal resection after intussusception
| Outcome | Variablesa | Death (n = 133)b | No death (n = 884) b |
cOR (95% UCL- LCL) |
aOR (95% UCL- LCL) |
|---|---|---|---|---|---|
| Death | Intestinal resection | 97 (75.19) | 370 (44.21) | 3.83 (2.51, 5.84) | 3.43 (1.9, 6.15) |
| Female sex | 54 (40.6) | 360 (40.77) | 0.99 (0.69, 1.44) | 1.98 (1.20, 3.27) | |
| Duration of symptoms | 4 (2, 6) | 2 (1, 4) | 1.05 (1.02, 1.08) | 1.08 (1.01, 1.15) | |
| Television | 43 (40.95) | 570 (70.81) | 0.29 (0.19, 0.43) | 0.51 (0.30, 0.87) | |
| Resection (n = 467) b |
No resection (n = 499) b |
||||
| Intestinal resection | Age (months) | 25 (19, 31) | 28 (22, 35) | 0.96 (0.95, 0.98) | 0.96 (0.95, 0.98) |
| Diagnostic US/enema | 51 (10.92) | 138 (27.66) | 0.32 (0.23, 0.46) | 0.42 (0.26, 0.68) | |
| Employment | 228 (56.58) | 333 (75.34) | 0.43 (0.32, 0.57) | 0.65 (0.43, 0.98) | |
| Television | 238 (56.0) | 348 (79.09) | 0.34 (0.25, 0.45) | 0.51 (0.35, 0.76) |
Abbreviations: cOR=crude Odds Ratio and aOR=adjusted Odds Ratio, UCL = Upper confidence limit, LCL = lower confidence limit
Missing data for outcome = death: Intestinal resection = 51, sex = 1, television = 107, electricity = 145, employment = 121
Missing data for outcome = resection: employment = 121, television = 101
Country-related findings not provided
Data are presented as n (%) or median (interquartile range)
In the adjusted secondary analyses, diagnosis by ultrasound or enema (OR 0.32; 95% CI 0.23–0.46), having a television at home (OR 0.51, 95% CI 0.35–0.76), and employment of a household member (OR 0.65; 95% CI 0.43–0.98) were protective against intestinal resection.
Discussion
In this evaluation of African infants with intussusception from 7 sub-Saharan African countries, we found that longer duration of symptoms prior to hospitalization was associated with death from intussusception; for every extra day that an infant experienced symptoms prior to admission at the sentinel hospital, risk of death increased by 8%. These findings indicate that delays in hospitalization for intussusception, whether due to distance from treatment facility, economic costs of transport and hospitalization, or misdiagnosis early on, is an important risk factor for death from intussusception in African infants. Adjusting for availability of car or motorcycle did not influence these findings.
Intestinal resection was strongly associated with mortality, which is consistent with the literature on mortality following emergency abdominal surgery.[12] The risk of mortality following emergency abdominal surgery is even higher in low-resource settings; in one study, after adjusting for differences in patient and hospital risk factors, the odds of death at 30 days after emergency abdominal surgery was seven times that of high-income countries (adjusted OR 7.14; 95% CI 2.52 to 20.23, p <0.001).[13] Poor access to timely and essential treatment has been identified as a significant contributing factor to these disparities.[14,15] Our findings support these hypotheses, demonstrating that lack of access to timely intervention for intussusception, leading to late presentation, is a risk factor for mortality.
Additionally, in adjusted analyses, girls were almost twice as likely to die from intussusception than boys. The reason for this finding is unclear, and is not explained by late presentation to the treatment hospital. Intussusception is described more often in males than in females,[5] but a mortality difference has not been described previously in the literature. However, gender differences in general care-seeking practices in low- and middle-income countries that have been described in the literature may play a role.[16,17]
Use of a radiologic method (ultrasound or enema) to diagnose intussusception decreased the likelihood of resection by approximately 60%, suggesting that access to diagnostic ultrasound allows for more timely diagnosis, and potential access to non-surgical treatment. However, independent of diagnostic method, economic barriers are also likely playing a role. Both presence of employment and having a television, proxies for household wealth, also significantly decreased the likelihood of resection, suggesting that household wealth improves access and affordability of timely treatment.
This analysis was subject to limitations. The data were initially collected for the purpose of monitoring for intussusception among early-introducing African countries, and SES-related data was not complete for all cases. Facility–specific information, such as the availability of diagnostic ultrasound, was not available, and so it is unclear whether infants did not obtain diagnostic ultrasound due to availability or provider training. The role of being transferred from a first facility to the treatment facility, and diagnostic resources available at the first facility were not collected. We were not able to account for location of residence (rural versus urban), distance from the nearest treatment facility, or time required to reach the nearest treatment facility from an infant’s place of residence. However, when access to a car or any motorized vehicle was included in the model, duration of symptoms remained significantly associated with death, indicating that other factors (such as provider misdiagnosis, social support, cost of transport) may be playing a role. We were not able to evaluate the role of other SES indicators, such as occupation, location of residence, and food insecurity, which may be better indicators of SES in some African countries. Finally, we were not able to evaluate the role of malnutrition prior to surgery, which is a risk factor for post-operative complications following surgery.[18,19]
Conclusions
The morbidity and mortality following intussusception was high in sub-Saharan African infants. Longer duration of symptoms and female sex were significantly associated with death following intussusception in African infants, even after accounting for demographic factors and socioeconomic status indicators. Indicators of household poverty were associated with intestinal resection following intussusception. Future studies should continue to explore drivers of delayed hospitalization, including those associated with direct medical and social costs and health seeking behaviors. Efforts to improve the awareness, diagnosis, and management of intussusception in sub-Saharan Africa should target these resource limited settings.
Supplementary Material
What is Known
Intussusception, or the invagination of one segment of the intestine within another segment, is a pediatric emergency and may be fatal.
Among children less than one year of age with intussusception, case-fatality is higher in Africa as compared to other regions of the world.
What is New
Delays in hospital presentation and female sex were associated with death following intussusception
Indicators of household poverty were associated with intestinal resection following intussusception.
Efforts should be intensified to improve the awareness, diagnosis, and management of intussusception in sub-Saharan African countries, especially in low resource settings.
Acknowledgments
Conflicts of Interest and Source of Funding: The African Intussusception Surveillance Network was funded by Gavi. No conflicts of interest disclosures to report.
Disclaimer: The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention or World Health Organization (WHO).
Footnotes
A list of additional members of the African Intussusception Surveillance Network is provided in the Supplementary Appendix.
Conflicts of interest: None
References
- 1.WHO. Acute intussusception in infants and children : incidence, clinical representation and management : a global perspective. (World Health Organization, Geneva, 2002) [Google Scholar]
- 2.Waseem M, Rosenberg HK. Intussusception. Pediatric emergency care, 24(11), 793–800 (2008). [DOI] [PubMed] [Google Scholar]
- 3.Stringer MD, Pablot SM, Brereton RJ . Pediatric Intussusception. Br J Surg, 79, 867–876 (1992). [DOI] [PubMed] [Google Scholar]
- 4.Jiang J, Jiang B, Parashar U, Nguyen T, Bines J, Patel MM. Childhood intussusception: a literature review. PLoS One, 8(7), e68482 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mpabalwani EM, Mwenda JM, Tate JE, Parashar UD. Review of Naturally Occurring Intussusception in Young Children in the WHO African Region prior to the Era of Rotavirus Vaccine Utilization in the Expanded Programme of Immunization. Journal of tropical pediatrics, 63(3), 221–228 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mpabalwani EM, Chitambala P, Chibumbya JN et al. Intussusception incidence rates in 9 Zambian hospitals, 2007–2011: prerotavirus vaccine introduction. Pediatr Infect Dis J, 33 Suppl 1, S94–98 (2014). [DOI] [PubMed] [Google Scholar]
- 7.Chalya PL, Kayange NM, Chandika AB. Childhood intussusceptions at a tertiary care hospital in northwestern Tanzania: a diagnostic and therapeutic challenge in resource-limited setting. Italian journal of pediatrics, 40(1), 28 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ekenze SO, Mgbor SO. Childhood intussusception: the implications of delayed presentation. African journal of paediatric surgery : AJPS, 8(1), 15–18 (2011). [DOI] [PubMed] [Google Scholar]
- 9.van Heek NT, Aronson DC, Halimun EM, Soewarno R, Molenaar JC, Vos A. Intussusception in a tropical country: comparison among patient populations in Jakarta, Jogyakarta, and Amsterdam. Journal of pediatric gastroenterology and nutrition, 29(4), 402–405 (1999). [DOI] [PubMed] [Google Scholar]
- 10.Tate JE, Mwenda JM, Armah G et al. Evaluation of Intussusception after Monovalent Rotavirus Vaccination in Africa. The New England journal of medicine, 378(16), 1521–1528 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bines JE, Kohl KS, Forster J et al. Acute intussusception in infants and children as an adverse event following immunization: case definition and guidelines of data collection, analysis, and presentation. Vaccine, 22(5–6), 569–574 (2004). [DOI] [PubMed] [Google Scholar]
- 12.Mortality of emergency abdominal surgery in high-, middle- and low-income countries. The British journal of surgery, 103(8), 971–988 (2016). [DOI] [PubMed] [Google Scholar]
- 13.Determinants of morbidity and mortality following emergency abdominal surgery in children in low-income and middle-income countries. BMJ global health, 1(4), e000091 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meara JG, Leather AJ, Hagander L et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet (London, England), 386(9993), 569–624 (2015). [DOI] [PubMed] [Google Scholar]
- 15.Weiser TG, Uribe-Leitz T, Fu R et al. Variability in mortality after caesarean delivery, appendectomy, and groin hernia repair in low-income and middle-income countries: implications for expanding surgical services. Lancet (London, England), 385 Suppl 2, S34 (2015). [DOI] [PubMed] [Google Scholar]
- 16.Calu Costa J, Wehrmeister FC, Barros AJ, Victora CG. Gender bias in careseeking practices in 57 low- and middle-income countries. Journal of global health, 7(1), 010418 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dachs JN, Ferrer M, Florez CE, Barros AJ, Narvaez R, Valdivia M. Inequalities in health in Latin America and the Caribbean: descriptive and exploratory results for self-reported health problems and health care in twelve countries. Revista panamericana de salud publica = Pan American journal of public health, 11(5–6), 335–355 (2002). [DOI] [PubMed] [Google Scholar]
- 18.Braga M, Ljungqvist O, Soeters P, Fearon K, Weimann A, Bozzetti F. ESPEN Guidelines on Parenteral Nutrition: surgery. Clinical nutrition (Edinburgh, Scotland), 28(4), 378–386 (2009). [DOI] [PubMed] [Google Scholar]
- 19.Schiesser M, Kirchhoff P, Muller MK, Schafer M, Clavien PA. The correlation of nutrition risk index, nutrition risk score, and bioimpedance analysis with postoperative complications in patients undergoing gastrointestinal surgery. Surgery, 145(5), 519–526 (2009). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


