Abstract
Few studies have examined the longitudinal association between sluggish cognitive tempo (SCT) symptoms and internalizing symptoms, and no study has examined the potentially bidirectional associations between SCT and internalizing symptoms. The present study used a short-term longitudinal design to examine the directionality of the associations between SCT, depressive, and anxious symptoms in children. Teachers of 188 children in 1st-6th grades (ages 6–13 years; 47% boys) provided ratings of children’s SCT, anxiety, and depressive symptoms in the fall school semester (T1) and again six months later (T2). Children in 3rd-6th grades (n=133) provided ratings of anxiety and depressive symptoms at both timepoints. Cross-lagged panel models examining the longitudinal associations between SCT, anxiety, and depressive symptoms were conducted controlling for sex and grade, with separate models for teacher- and child-reported internalizing symptoms. SCT symptoms at T1 predicted increased depressive symptoms at T2, with findings consistent across teacher-rated depression and child-rated depression. Depression at T1 did not predict SCT at T2. SCT symptoms at T1 also predicted increased teacher-rated anxiety at T2, but not child-rated anxiety. Finally, child-rated anxiety at T1 predicted increased SCT at T2. Findings from this study provide the first evidence that SCT symptoms predict subsequent depressive symptoms and not the reverse. Associations between SCT and anxiety are more nuanced, with results differing based on the informant. Additional studies are needed to replicate and extend these findings across longer developmental periods with more timepoints and to examine mechanisms of the associations between SCT and internalizing symptoms in children.
Keywords: anxiety, comorbidity, co-occurrence, depression, longitudinal, sluggish cognitive tempo
Until recently, it was unknown whether sluggish cognitive tempo (SCT) symptoms, characterized by excessive daydreaming, slowed behavior/thinking, and mental confusion and fogginess, were distinct from internalizing symptoms of anxiety and depression. A rapidly accumulating body of research demonstrates that SCT symptoms are in fact empirically distinct from internalizing symptoms (Becker, Burns, Garner, et al., 2018; Becker, Luebbe, Fite, Stoppelbein, & Greening, 2014; Becker, Luebbe, & Joyce, 2015; Lee, Burns, Snell, & McBurnett, 2014; McBurnett et al., 2014; Smith, Eadeh, Breaux, & Langberg, 2019; Willcutt et al., 2014). Importantly, the differentiation between SCT and internalizing symptoms has been shown across different developmental periods (children, adolescents, and adults), sample types (community and clinical), and informants (parent, teacher, and self-report).
Despite their differentiation, SCT and internalizing symptoms are also strongly associated (for reviews, see Barkley, 2014; Becker et al., 2016). In fact, although SCT was initially identified in the area of attention-deficit/hyperactivity disorder (ADHD), increasing evidence suggests that SCT may fall under the umbrella of internalizing psychopathology (Becker & Willcutt, 2019). For instance, SCT is associated with increased punishment sensitivity and behavior inhibition system (BIS) sensitivity (Becker et al., 2013; Becker, Schmitt, et al., 2018), conflicted shyness (Becker, Burns, Leopold, Olson, & Willcutt, 2018; Sáez, Servera, Burns, & Becker, 2019), and social isolation and withdrawal (Becker, Garner, Tamm, Antonini, & Epstein, 2019; Marshall, Evans, Eiraldi, Becker, & Power, 2014; Willcutt et al., 2014). These findings underscore the importance of better understanding the interrelations between SCT and internalizing symptoms.
Considering Longitudinal Co-occurrence between SCT and Internalizing Symptoms
Only a handful of longitudinal studies have examined the relations between SCT and internalizing symptoms (Becker, Burns, Leopold, et al., 2018; Bernad, Servera, Becker, & Burns, 2016; Bernad, Servera, Grases, Collado, & Burns, 2014; Servera, Bernad, Carrillo, Collado, & Burns, 2016), and no study to date has examined possible bidirectional co-occurrence between SCT and internalizing dimensions. Rather, the extant longitudinal studies have only examined SCT as a predictor of later internalizing symptoms. It is possible that there is a unidirectional association between SCT and internalizing symptoms, whereby SCT symptoms confer risk for subsequent internalizing symptoms, perhaps via SCT-related impairments such as academic difficulties and poorer social skills. In line with this hypothesis, studies that have examined SCT as a predictor of later internalizing symptoms across a period of one to ten years have consistently found SCT to predict subsequent depressive symptoms and, to a somewhat lesser extent, anxiety symptoms (Becker, Burns, Leopold, et al., 2018; Bernad et al., 2016; Bernad et al., 2014; Servera et al., 2016). However, these studies did not examine whether SCT predicted subsequent internalizing symptoms when also controlling for initial levels of internalizing, which is a crucial test for determining whether associations are unidirectional or bidirectional.
It is also possible that SCT and internalizing symptoms interrelate bidirectionally over time. That is, SCT may confer risk for subsequent internalizing symptoms, while at the same time internalizing symptoms confer risk for subsequent SCT symptoms. It has been hypothesized that SCT may fit as a first-order dimension on a higher order internalizing factor that also includes anxiety and depressive symptoms (Becker & Willcutt, 2019). Relatedly, negative affect and neuroticism are linked to both internalizing and SCT symptoms (Becker, Schmitt, et al., 2018). Internal thought processes, when excessive and negatively valenced, may maintain a feedback loop whereby internalizing and SCT symptoms influence each other over time. In line with this possibility, studies examining task unrelated thought (mind wandering) have documented a possible bidirectional link between excessive or absorbed daydreaming – which is a core feature of SCT – and depressive symptoms (Giambra & Traynor, 1978; Meyer, Finucane, & Jordan, 2011; Stawarczyk, Majerus, Van der Linden, & D’Argembeau, 2012). However, no study to date has examined whether internalizing symptoms predict later SCT symptoms or whether internalizing and SCT are bidirectionally related over time.
The Current Study
The current study builds on previous research by using longitudinal cross-lagged panel models to examine the potentially bidirectional associations between SCT and internalizing symptoms. Data were collected as part of a school-based study examining the validity of SCT in elementary school-aged children (Becker, 2014). Specifically, using a short-term longitudinal design with two timepoints in the fall and spring semesters of the school year, we examined separate anxiety and depression dimensions using both teacher and child self-report ratings. Separate anxiety and depression dimensions were used since some studies have found SCT symptoms to be more clearly associated with depression than with anxiety (Becker et al., 2014; Fenollar Cortés, Servera, Becker, & Burns, 2017; Jacobson et al., 2012), including in longitudinal research using teacher-reported internalizing symptoms specifically (Bernad et al., 2016). Since sex, grade, and socio-economic status may all be associated with internalizing and SCT symptoms (Becker et al., 2016), these were included as covariates in all analyses. Based on extant research (Becker, Burns, Leopold, et al., 2018; Bernad et al., 2016; Bernad et al., 2014; Servera et al., 2016), we hypothesized that SCT would predict increases in both teacher- and child-rated anxiety and depressive symptoms. We tentatively expected findings to be clearer for SCT predicting increases in depression rather than anxiety symptoms (Bernad et al., 2016). We did not make a priori hypotheses regarding anxiety and depressive symptoms predicting increases in teacher-rated SCT symptoms, as examination of these paths are novel to the present study.
Methods
Participants
The current study included teacher ratings of 188 students attending an elementary school in the Midwestern United States. Students included in this study were in first through sixth grades (ages 6–13 at the fall timepoint, M = 9.14, SD = 1.85). The sample was approximately equally split between boys (n = 89; 47%) and girls (n = 99; 53%). Most participants in this study were White (n = 175; 93%) with remaining participants Black (n = 10; 5%) or Asian (n = 3; 2%). Fifty-four percent (n = 101) of the students received free/reduced lunch, which was used in the present study as a marker of socioeconomic status. According to the 2010 Census, 28.4% of the city population was below the federal poverty level (median household income = $30,299).
Procedures
All study procedures were approved by the university Institutional Review Board and are described in more detail elsewhere (Becker, 2014; Becker et al., 2015). All grades (1st−6th grades) at the school were invited to participate, and students in each grade had only one primary teacher for all subjects (no students had multiple teachers). One month into the school year, the principal investigator described the study to teachers of 1st−6th grades. All 12 eligible mainstream classroom teachers provided signed informed consent to participate. After teachers provided consent, research staff described the study to the students in each teacher’s classroom. After answering any questions, students were given informed consent forms to take home to their parents. In consultation with the school principal, it was determined infeasible to collect parent ratings, though parents were required to provide consent. Of the 280 total students in 1st−6th grades in October (T1), 218 returned consent forms, 189 parents provided consent for participation (29 parents did not consent), and teachers completed ratings for 188 of these students who were included in the current analyses. Each teacher rated between 11 and 23 students (median = 15 students). 176 of the students were still attending the school in April and had data at the second timepoint (T2). Students who were missing data at T2 did not differ from those with complete data at both timepoints on demographic characteristics (i.e., sex, grade, race, free/reduced lunch status) or T1 SCT/internalizing symptoms (all ps > .05).
Measures
Child demographic variables
School records were used to gather demographic information (i.e., age, sex, race, free/reduced lunch status) for each participating student.
Teacher-rated SCT
The Sluggish Cognitive Tempo Scale (SCTS) (Penny, Waschbusch, Klein, Corkum, & Eskes, 2009) was completed by teachers to assess children’s SCT symptoms. Teachers completed the SCT measure at both T1 and T2. The SCTS consists of 14 items rated on a four-point scale (0 = not at all, 3 = very much). The psychometric properties of the SCTS were initially examined in a school-based sample of 335 children (ages 4–13 years), including strong associations between SCT symptoms and internalizing symptoms. In addition, a subset of parents completed the scale at two timepoints to establish test-retest reliability over an average of 12 weeks (r = .87; test-retest was not collected for teacher ratings) (Penny et al., 2009). As in previous research (Becker et al., 2019; Holdaway & Becker, 2018; Yung, Lai, Chan, Ng, & Chan, 2019), 10 items from the SCTS were used as a measure of SCT in the present study (T1 α = 0.91, T2 α = 0.95). These 10 items were selected based on recent meta-analytic findings of SCT items that were identified as consistently loading on a SCT factor (and not cross-loading with ADHD inattention) (Becker et al., 2016). The 10 items used to measure SCT in the present study are: (1) is apathetic; shows little interest in things or activities, (2) is unmotivated, (3) appears to be sluggish, (4) seems drowsy, (5) daydreams, (6), appears tired; lethargic, (7) gets lost in his or her own thoughts, (8) seems to be in a world of his or her own, (9) has a yawning, stretching, sleepy-eyed appearance, and (10) is underactive, slow moving, or lacks energy. The four excluded items (is slow or delayed in completing tasks, lacks initiative to complete work, effort on tasks fades quickly, needs extra time for assignments) did not demonstrate discriminant validity from ADHD inattention in initial validation studies of the SCTS (Penny et al., 2009) or in the subsequent meta-analysis (Becker et al., 2016). In addition, previous exploratory factor analyses from this dataset indicated that the 10 SCT items used in this study are best represented as a single dimension (Holdaway & Becker, 2018).
Teacher-rated internalizing symptoms
At T1 and T2, teachers completed the Vanderbilt ADHD Teacher Rating Scale (VATRS) (Wolraich, Bard, Neas, Doffing, & Beck, 2013), a well-validated teacher-report measure of child mental health symptoms. The VATRS includes three items assessing anxiety (i.e., is fearful, anxious or worried; is self-conscious or easily embarrassed; is afraid to try new things for fear of making mistakes) and four items assessing depression (i.e., feels worthless or inferior; feels lonely, unwanted, or unloved; is sad, unhappy, or depressed; blames self for problems, feels guilty). Each item is rated on a four-point scale (0 = never, 1 = occasionally, 2 = often, 3 = very often). In the present study, internal consistencies of the mean scale scores were acceptable at T1 (and T2): anxiety α = 0.83 (0.81) and depression α = 0.80 (0.70).
Child-rated internalizing symptoms
Since younger children may not have the language and insight to provide reliable and valid reports of their own internalizing states, the Revised Child Anxiety and Depression Scales (RCADS) has been validated for children in 3rd−12th grades (Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000; Ebesutani et al., 2012). As such, at T1 and T2, only students in third through sixth grades (n = 133) completed the RCADS (Chorpita et al., 2000). A short version (Ebesutani et al., 2012) was used in this study, consisting of 15 anxiety items (e.g., I worry what other people think of me; I worry that something bad will happen to me; I worry when I think I have done poorly at something) and 10 depression items (e.g., I feel sad or empty; nothing is much fun anymore; I feel worthless). Each item is rated on a four-point scale (0 = never, 1 = sometimes, 2 = often, 3 = always). In the present study, internal consistencies of the sum scale scores were acceptable at T1 (and T2): anxiety α = 0.84 (0.86) and depression α = 0.77 (0.81).
Statistical analyses
First, zero-order correlations were examined to test the hypothesis that SCT and internalizing symptoms would be associated with each other from T1 to T2. Next, longitudinal cross-lagged panel models (Curran & Bollen, 2001) were conducted in Mplus Version 8.2 to examine the associations between SCT, anxiety, and depressive symptoms. Separate models were conducted for teacher-reported and child-reported internalizing symptoms1. Within a structural equation model framework, these two models were conducted to examine the directional influence of SCT with teacher- and child-rated depressive and anxiety symptoms, controlling for prior levels of SCT and internalizing symptoms (i.e., autoregressive paths) and adjusting for covariates (i.e., sex, grade, and free/reduced lunch status). At T1, the residual correlations were specified to examine the concurrent correlations between SCT and anxiety and depressive symptoms, unexplained by the effects of the covariates. Similarly at T2, the concurrent correlations are also among the residuals to examine the variance in SCT, anxiety, and depressive symptoms not accounted for by the covariates, autoregressive, and cross-lagged paths. Missing data was minimal (5.85% and 5.26% of participants on the teacher and self-report ratings, respectively, were missing at T2) and were handled through use of full information maximum likelihood estimation with robust standard errors (MLR), which is recommended for small and medium sample sizes (Muthén & Muthén, 1998–2018)2. This estimator addresses missing data by using all available data (i.e., students with at least one wave of data were retained) to maximize the information available for data analysis. Model fit was assessed with the Comparative Fit Index (CFI) and the Root Mean Square Error of Approximation (RMSEA) given that χ2 is known to be sensitive to sample size (McDonald & Ho, 2002). CFI values ≥ 0.90–0.95 and RMSEA values ≤ 0.08 indicate adequate model fit (Wang & Wang, 2012). Squared semi-partial correlations (i.e., the percent of variance accounted for by the auto-regressive and cross-lag paths) were used as an index of effect size.
Results
Correlation Analyses
Intercorrelations among study variables and descriptive statistics are provided in Table 1. All psychopathology dimensions were significantly intercorrelated at T1 and T2 (ps < .05), with the exception of teacher-reported anxiety and depressive symptoms at T1 being unassociated with child-rated anxiety symptoms at T2 (ps > .05). T1 SCT symptoms were significantly associated with teacher-rated and child-rated internalizing symptoms (ps<.01), and Steiger’s z-test for dependent correlations indicated that the magnitude of T1 SCT with teacher-rated depressive (r = .37) and anxiety symptoms (r = .47) at T2 were similar (z = 1.71, p = .09). However, Steiger’s z-test indicated that teacher-rated SCT at T1 was more strongly associated with T2 child-rated depressive symptoms (r = .37) than anxiety symptoms (r = .21, z = 2.30, p = .02).
Table 1.
Intercorrelations and Descriptive Statistics of Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Lunch Status | -- | ||||||||||||
| 2. Sex | .092 | -- | |||||||||||
| 3. Grade | −.057 | .078 | -- | ||||||||||
| 4. T1 TR SCT | .186* | −.260*** | .128 | -- | |||||||||
| 5. T1 TR Anxiety | .038 | −.056 | .177* | .415*** | -- | ||||||||
| 6. T1 TR Depression | .043 | −.119 | .148* | .405*** | .630** | -- | |||||||
| 7. T1 SR Anxiety | −.032 | .057 | −.068 | .172* | .271** | .219* | -- | ||||||
| 8. T1 SR Depression | .051 | −.091 | −.249** | .199* | .331*** | .261** | .705*** | -- | |||||
| 9. T2 TR SCT | .196** | −.181* | .129 | .756*** | .307*** | .330*** | .283** | .210* | -- | ||||
| 10. T2 TR Anxiety | .100 | −.098 | .223** | .473*** | .512*** | .386*** | .280** | .304** | .513*** | -- | |||
| 11. T2 TR Depression | .126 | −.014 | .153* | .372*** | .429*** | .542*** | .287** | .307*** | .421*** | .614*** | -- | ||
| 12. T2 SR Anxiety | .094 | −.063 | −.093 | .211* | .160 | .069 | .540*** | .456*** | .295** | .365*** | .287** | -- | |
| 13. T2 SR Depression | .016 | −.286** | −.174 | .366*** | .246** | .207* | .461*** | .558*** | .384*** | .431*** | .333*** | .688*** | -- |
| Mean | -- | -- | 3.66 | .40 | .34 | .17 | 11.38 | 7.23 | .45 | .51 | .18 | 9.03 | 5.44 |
| Standard Deviation | -- | -- | 1.67 | .51 | .51 | .41 | 7.42 | 5.01 | .62 | .56 | .36 | 7.13 | 4.57 |
Note. For lunch status, 0 = paid lunch, 1 = free/reduced lunch. For sex, 0 = male, 1 = female. SCT = sluggish cognitive tempo. SR = child self-report. TR = teacher report. T1 = fall timepoint. T2 = spring timepoint (approximately 6 months after T1).
p < .05.
p < .01.
p < .001
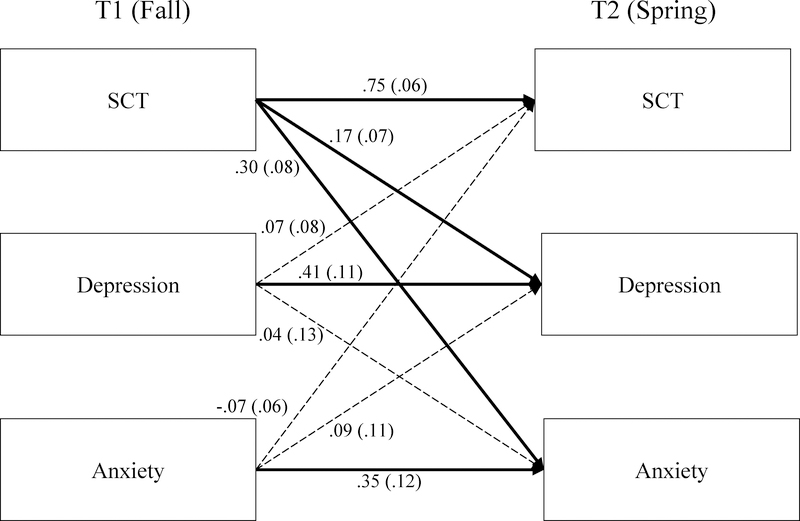
Cross-Lagged Model of SCT and Teacher-Reported Internalizing Symptoms
The model examining SCT and teacher-rated internalizing symptoms demonstrated excellent fit, χ2(9) = 9.568, p = .387, CFI = .998, RMSEA = .018 (see Figure 1). As expected, stability paths were all significant from T1 to T2 (SCT β = .75, SE = .06, p < .001; depression β = .41, SE = .11, p = .001; anxiety β = .35, SE = .12, p = .003). SCT symptoms at T1 predicted residual increases in depressive symptoms (β = .17, SE = .07, p = .016) and anxiety symptoms (β = .30, SE = .08, p < .001) at T2. Neither teacher-reported anxiety nor depressive symptoms at T1 predicted residual increases in SCT symptoms or each other at T2 (ps > .05; Figure 1). The model accounts for approximately one third of the variance in anxiety symptoms at T2 (R2 = .33), with prior levels of anxiety accounting for 12% of the variance, and SCT at T1 accounting for just over 9%. Similarly, the model also accounts for one third of the variance in depressive symptoms at T2 (R2 = .32), with prior levels of depressive symptoms accounting for 17%, and prior levels of SCT at T1 accounting for 3%. Finally, the model accounts for over half of the variance in SCT (R2 = .57) with prior levels of SCT accounting for 56% of the variance, and anxiety and depressive symptoms accounting for just over 1%.
Figure 1.
Cross-lag model for SCT and teacher-rated internalizing symptoms.
Note. SCT = Sluggish cognitive tempo. T1 = fall timepoint. T2 = spring timepoint (approximately 6 months after T1). Statistically significant standardized path coefficients (and standard errors) are shown with solid lines and dotted lines represent a non-significant path (p > .05). Covariates and cross-sectional correlations were included in the model but are omitted from the figure to reduce complexity. χ2(9) = 9.57, p = .39. RMSEA = .02. CFI = .998.
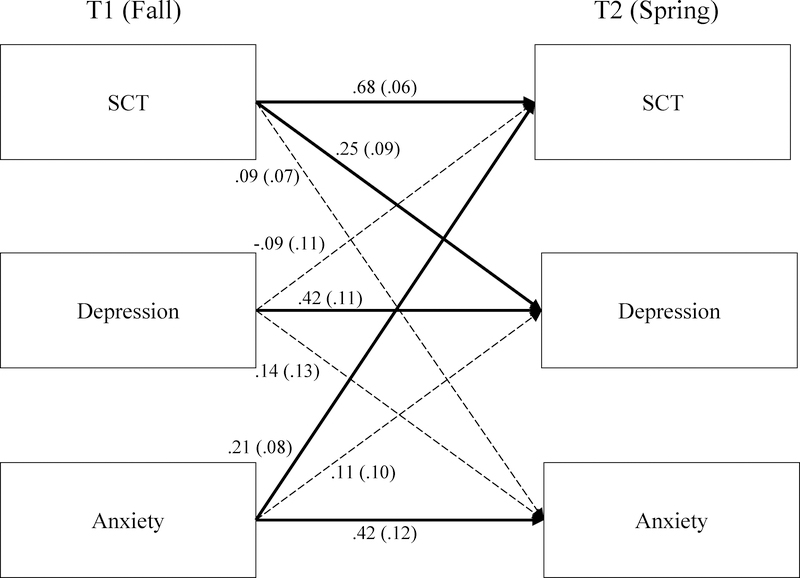
Cross-Lagged Model of SCT and Child-Reported Internalizing Symptoms
The model examining SCT and child-rated internalizing symptoms demonstrated adequate fit, χ2(9) = 15.567, p = .077, CFI = .979, RMSEA = .074 (see Figure 2). Stability paths were all significant from T1 to T2 (SCT β = .68 SE = .06; depression β = .42, SE = .11; anxiety β = .42, SE = .12; all ps = .001). SCT symptoms at T1 predicted residual increases in child-reported depressive symptoms at T2 (β = .25, SE = .09, p = .006), but not increased anxiety symptoms (β = .09, SE = .07, p = .171) at T2. In contrast, child-reported anxiety symptoms at T1 predicted residual increases in teacher-reported SCT symptoms at T2 (β = .21, SE = .08, p = .011). Child-reported depressive symptoms at T1 did not predict residual increases in SCT or anxiety symptoms at T2 (ps > .05; Figure 2). The model accounts for over a third of the variance in depressive symptoms at T2 (R2 = .37), with prior levels of depressive symptoms accounting for 17%, and prior levels of SCT at T1 accounting for over 6%. The model also accounts for approximately one third of the variance in anxiety symptoms at T2 (R2 = .31), with prior levels of anxiety accounting for 18% of the variance, and SCT at T1 accounting for just under 1%. Finally, the model accounts for approximately half of the variance in SCT (R2 = .51) with prior levels of SCT account for 45% of the variance and anxiety symptoms accounting for 5% and depressive symptoms accounting for just under 1%.
Figure 2.
Cross-lag model for SCT and child-rated internalizing symptoms.
Note. SCT = Sluggish cognitive tempo. T1 = fall timepoint. T2 = spring timepoint (approximately 6 months after T1). Statistically significant standardized path coefficients (and standard errors) are shown with solid lines and dotted lines represent a non-significant path (p > .05). Covariates and cross-sectional correlations were included in the model but are omitted from the figure to reduce complexity. χ2(9) = 15.57, p = .08. RMSEA = .07. CFI = .979.
Discussion
Despite strong associations between SCT and internalizing symptoms (Barkley, 2014; Becker et al., 2016), very few longitudinal studies have been conducted and this is the first study to examine possible bidirectional associations between these psychopathologies. Using a school-based sample and both teacher and child ratings of internalizing symptoms at two occasions across a school year, the current study provides a preliminary test of possible unidirectional and bidirectional relations between SCT and internalizing symptoms. SCT, anxiety, and depressive symptoms were each stable across the time interval examined in this study and underscores the importance of adjusting for autoregressive (stability) effects when examining the complex associations between SCT and internalizing symptoms. In addition, the pattern of findings differed for anxiety and depression, underscoring the importance of examining these internalizing dimensions separately, and these findings are discussed in turn.
SCT symptoms predicted residual increases in depressive symptoms across both teacher and child ratings. This finding supports a developmental precursor hypothesis whereby SCT symptoms may confer risk for subsequent depressive symptoms, rather than the reverse. Previous studies have found a prospective association between SCT and depressive symptoms (Becker, Burns, Leopold, et al., 2018_; Bernad et al., 2016; Bernad et al., 2014; Servera et al., 2016). However, this is the first study to demonstrate that this association is robust when controlling for initial levels of depressive symptoms and to also simultaneously examine the possible reverse association of depression predicting SCT symptoms. In addition to replicating our findings, the next step will be to examine possible mechanisms underlying the link between SCT and increased depressive symptoms. For instance, SCT is associated with increased social withdrawal (Becker et al., 2019; Marshall et al., 2014; Willcutt et al., 2014), and it has also been hypothesized (though not yet empirically tested) that the daydreaming nature of SCT may be associated with rumination (Becker & Willcutt, 2019). SCT symptoms may lead to increased ruminative thinking and withdrawal, as well as poorer functioning across various domains (e.g., academics, sleep), which may individually or jointly contribute to increased depression. In line with this possibility, a study examining self-generated thoughts found an indirect effect of ruminative thought to partly account for the association between daydreaming frequency and depressive symptoms (Marchetti, Van de Putte, & Koster, 2014).
Findings for anxiety were more nuanced and differed when examining teacher- and child-rated anxiety symptoms. SCT symptoms at T1 predicted residual increases in teacher-rated anxiety symptoms at T2, whereas child-rated anxiety symptoms at T1 predicted residual increases in SCT symptoms at T2. As this study was confined to two timepoints, it is impossible to test whether SCT and anxiety symptoms bidirectionally relate to each other over time, though this is certainly a possibly that should be examined in future studies with additional timepoints. Children with SCT symptoms may be especially prone to having a ruminative thinking style that leads to increases in anxiety. Further, given the fast-paced and complex nature of peer groups (e.g., involving sarcasm and the ability to pick up on subtle social cues), children with SCT may also find social situations to be overwhelming (Willcutt et al., 2014). Social and academic difficulties may contribute to greater worries and anxiety. It is intriguing that child-rated anxiety predicted increases in teacher-reported SCT symptoms, whereas teacher-reported SCT predicted increases in teacher-reported anxiety symptoms. It is not immediately clear why these differential associations emerged across child and teacher informants of anxiety. It may be that children who are anxious at the beginning of the year have increases in daydreaming and mental confusion behaviors that are readily observed by teachers. Conversely, children who begin the school year demonstrating SCT symptoms may be perceived by teachers as showing more anxiety-related behaviors, such as worry and social reticence, by the end of the school year. Additional research is needed to test these possibilities, as well as to replicate our study findings and examine whether anxiety and SCT symptoms are intertwined over time in a mutually-reinforcing ways.
Given the mixed findings for anxiety specifically, it would be beneficial for future research to consider specific anxiety dimensions (e.g., social anxiety, panic, and generalized anxiety symptoms) as well as related constructs of worry and obsessive-compulsive thinking. Considering the reverse association, attentional control theory posits that anxiety impairs attentional control, including working memory and processing efficiency (Eysenck, Derakshan, Santos, & Calvo, 2007), which may also lead to SCT behaviors including increased mental confusion, fogginess, and slower behaviors/thinking. Relatedly, youth with anxiety may have a negative anxiety response style that includes a tendency to have negative and persistent cognitions about anxiety symptoms (Starr, Stroud, & Li, 2016) that may contribute to increases in SCT symptoms characterized by excessive internal thought and negative affect.
Thought not the focus of the present study, is it worth noting that the test-retest correlation for SCT (r = .76) was notably larger than the test-retest for internalizing dimensions per teacher-report (rs = .51 and .54, for anxiety and depression, respectively) or child-report (rs = .54 and.46, for anxiety and depression, respectively). Similar findings were present for the stability paths in the cross-lagged panel models. There is emerging evidence that, after preschool, SCT is more trait-like than state-like (Burns, Becker, Geiser, Leopold, & Willcutt, 2019; Preszler et al., 2019). Internalizing symptoms may have more substantial occasion-specific variance (Dumenci & Windle, 1996; Olatunji & Cole, 2009), and so it is possible that there is greater possibility for SCT symptoms to influence internalizing symptoms over time rather than the reverse. We recognize that our finding that child-reported anxiety symptoms predicted increases in teacher-reported SCT conflicts with this possibility. In any event, it is important for future studies to consider construct stability when examining and interpreting cross-lagged associations.
Several limitations are important to acknowledge. In particular, our data were from a sample of convenience rather than a study specifically designed to examine possible unidirectional and bidirectional associations between SCT and internalizing symptoms. As such, this study included only two timepoints and could therefore only provide a preliminary test of possible bidirectional effects and was unable to directly test developmental precursor or developmental cascade hypotheses. Relatedly, studies with additional timepoints can examine developmental processes (e.g., SCT predicting impairment which in turn predicts depression) and cascading effects among these processes. We were also limited to only teacher-report of SCT, and it would be beneficial for subsequent research to incorporate a multi-informant assessment of SCT that also includes parent and self-report ratings. Our sample size was modest and included primarily non-Hispanic White children; larger studies with greater diversity will be needed to establish generalizability of our findings and to test whether sex or race moderate associations found in the present study. It will also be important for future studies to extend our findings to clinical samples and other developmental periods, including adolescence when both SCT (Leopold et al., 2016) and internalizing symptoms (Merikangas et al., 2010) may increase. Finally, for conceptual reasons, coupled with a limited sample size, it was determined a priori to not include ADHD symptoms in the models. That is, our interest was to provide an initial examination of whether SCT and internalizing symptoms were bidirectionally associated. Understanding whether ADHD symptoms are unidirectionally or bidirectionally associated with SCT and internalizing symptoms is also important, and additional studies are needed with larger samples and additional timepoints to further investigate the longitudinal associations between SCT and other psychopathology dimensions.
Despite these limitations, findings from the present study make an important contribution to the field’s current knowledge of the interrelations and co-occurrence of SCT and internalizing symptoms. SCT symptoms may be important to include in developmental psychopathology models of internalizing symptoms, though to date SCT has not been studied in youth at-risk for depression or anxiety. Findings further indicate the importance of distinguishing between anxiety and depression when examining associations with SCT. These findings, although preliminary, provide an important first step towards evaluating developmental precursor and developmental cascade hypotheses and mechanisms that may account for the strong associations between SCT and internalizing symptoms.
Acknowledgements
This research was supported in part by a scholarship to Stephen Becker from the American Psychological Foundation (APF) and the Council of Graduate Departments of Psychology (COGDOP). Stephen Becker is currently supported by award K23MH108603 from the National Institute of Mental Health (NIMH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the APF, COGDOP, or the National Institutes of Health (NIH).
Footnotes
Disclosure Statement: The authors declare no potential conflicts of interest with respect to the research, authorship, or publication of this article.
Students were nested within classrooms. However, the number of clusters (n=12) and number of students within cluster (median=15) is below the recommended number for using the Type=Complex command in Mplus (Muthén, 2013; Subramanian, Jones, & Duncan, 2003). When the Type=Complex option was used, results were unchanged though there was a warning regarding the number of parameters compared to the number of clusters. For this reason, findings without the clustering command are reported in the text.
A post-hoc Monte Carlo simulation power analysis was conducted with 5,000 replications. The population model was tested with N=188 and conservative estimates of .15 for cross-lagged effects and .35 for stability effects based on the actual results. Power was above .82 for all cross-variable path coefficients (M = .84; range = .83-.84) and above .94 for all stability path coefficients (M = .95; range = .94-.96). There were acceptably low levels of parameter and standard error bias and good coverage (94–95%). Note that .15 is the size of the smallest cross-lagged coefficient and .35 is the size of the smallest stability coefficient found in the current study. Overall, the analysis suggested acceptable power given found results.
References
- Barkley RA (2014). Sluggish cognitive tempo (concentration deficit disorder?): Current status, future directions, and a plea to change the name. Journal of Abnormal Child Psychology, 42, 117–125. doi: 10.1007/s10802-013-9824-y [DOI] [PubMed] [Google Scholar]
- Becker SP (2014). Sluggish cognitive tempo and peer functioning in school-aged children: A six-month longitudinal study. Psychiatry Research, 217, 72–78. doi: 10.1016/j.psychres.2014.02.007 [DOI] [PubMed] [Google Scholar]
- Becker SP, Burns GL, Garner AA, Jarrett MA, Luebbe AM, Epstein JN, & Willcutt EG (2018). Sluggish cognitive tempo in adults: Psychometric validation of the Adult Concentration Inventory. Psychological Assessment, 30, 296–310. doi: 10.1037/pas0000476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, Burns GL, Leopold DR, Olson RK, & Willcutt EG (2018). Differential impact of trait sluggish cognitive tempo and ADHD inattention in early childhood on adolescent functioning. Journal of Child Psychology and Psychiatry, 59, 1094–1104. doi: 10.1111/jcpp.12946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, Fite PJ, Garner AA, Greening L, Stoppelbein L, & Luebbe AM (2013). Reward and punishment sensitivity are differentially associated with ADHD and sluggish cognitive tempo symptoms in children. Journal of Research in Personality, 47, 719–727. doi: 10.1016/j.jrp.2013.07.001 [DOI] [Google Scholar]
- Becker SP, Garner AA, Tamm L, Antonini TN, & Epstein JN (2019). Honing in on the social difficulties associated with sluggish cognitive tempo in children: Withdrawal, peer ignoring, and low engagement. Journal of Clinical Child and Adolescent Psychology, 48, 228–237. doi: 10.1080/15374416.2017.1286595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, Leopold DR, Burns GL, Jarrett MA, Langberg JM, Marshall SA, … Willcutt EG (2016). The internal, external, and diagnostic validity of sluggish cognitive tempo: A meta-analysis and critical review. Journal of the American Academy of Child and Adolescent Psychiatry, 55, 163–178. doi: 10.1016/j.jaac.2015.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, Luebbe AM, Fite PJ, Stoppelbein L, & Greening L (2014). Sluggish cognitive tempo in psychiatrically hospitalized children: Factor structure and relations to internalizing symptoms, social problems, and observed behavioral dysregulation. Journal of Abnormal Child Psychology, 42, 49–62. doi: 10.1007/s10802-013-9719-y [DOI] [PubMed] [Google Scholar]
- Becker SP, Luebbe AM, & Joyce AM (2015). The Child Concentration Inventory (CCI): Initial validation of a child self-report measure of sluggish cognitive tempo. Psychological Assessment, 27, 1037–1052. doi: 10.1037/pas0000083 [DOI] [PubMed] [Google Scholar]
- Becker SP, Schmitt AP, Jarrett MA, Luebbe AM, Garner AA, Epstein JN, & Burns GL (2018). Sluggish cognitive tempo and personality: Links to BIS/BAS sensitivity and the five factor model. Journal of Research in Personality, 75, 103–112. doi: 10.1016/j.jrp.2018.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, & Willcutt EG (2019). Advancing the study of sluggish cognitive tempo via DSM, RDoC, and hierarchical models of psychopathology. European Child and Adolescent Psychiatry, 28, 603–613. doi: 10.1007/s00787-018-1136-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernad MD, Servera M, Becker SP, & Burns GL (2016). Sluggish cognitive tempo and ADHD inattention as predictors of externalizing, internalizing, and impairment domains: A 2-year longitudinal study. Journal of Abnormal Child Psychology, 44, 771–785. doi: 10.1007/s10802-015-0066-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernad MD, Servera M, Grases G, Collado S, & Burns GL (2014). A cross-sectional and longitudinal investigation of the external correlates of sluggish cognitive tempo and ADHD-inattention symptoms dimensions. Journal of Abnormal Child Psychology, 42, 1225–1236. doi: 10.1007/s10802-014-9866-9 [DOI] [PubMed] [Google Scholar]
- Burns GL, Becker SP, Geiser C, Leopold DR, & Willcutt EG (2019). Are sluggish cognitive tempo, ADHD, and oppositional defiant disorder trait- or state-like constructs from prekindergarten to fourth grade? Journal of Clinical Child and Adolescent Psychology. Advance online publication. doi: 10.1080/15374416.2019.1567348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, & Francis SE (2000). Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behaviour Research and Therapy, 38, 835–855. [DOI] [PubMed] [Google Scholar]
- Curran PJ, & Bollen KA (2001). The best of both worlds: Combining autoregressive and latent curve models. In Collins LM & Sayer AG (Eds.), Decade of behavior. New methods for the analysis of change (pp. 107–135). Washington, DC: American Psychological Association. [Google Scholar]
- Dumenci L, & Windle M (1996). A latent trait-state model of adolescent depression using the Center for Epidemiologic Studies-Depression Scale. Multivariate Behavioral Research, 31, 313–330. doi: 10.1207/s15327906mbr3103_3 [DOI] [PubMed] [Google Scholar]
- Ebesutani C, Reise SP, Chorpita BF, Ale C, Regan J, Young J, … Weisz JR (2012). The Revised Child Anxiety and Depression Scale-Short Version: scale reduction via exploratory bifactor modeling of the broad anxiety factor. Psychological Assessment, 24, 833–845. doi: 10.1037/a0027283 [DOI] [PubMed] [Google Scholar]
- Eysenck MW, Derakshan N, Santos R, & Calvo MG (2007). Anxiety and cognitive performance: attentional control theory. Emotion, 7, 336–353. doi: 10.1037/1528-3542.7.2.336 [DOI] [PubMed] [Google Scholar]
- Fenollar Cortés J, Servera M, Becker SP, & Burns GL (2017). External validity of ADHD inattention and sluggish cognitive tempo dimensions in Spanish children with ADHD. Journal of Attention Disorders, 21, 655–666. doi: 10.1177/1087054714548033 [DOI] [PubMed] [Google Scholar]
- Giambra LM, & Traynor TD (1978). Depression and daydreaming: An analysis based on self-ratings. Journal of Clinical Psychology, 34, 14–25. [PubMed] [Google Scholar]
- Holdaway AS, & Becker SP (2018). Sluggish cognitive tempo and student-teacher relationship quality: Short-term longitudinal and concurrent associations. School Psychology Quarterly, 33, 537–546. doi: 10.1037/spq0000245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson LA, Murphy-Bowman SC, Pritchard AE, Tart-Zelvin A, Zabel TA, & Mahone EM (2012). Factor structure of a sluggish cognitive tempo scale in clinically-referred children. Journal of Abnormal Child Psychology, 40, 1327–1337. doi: 10.1007/s10802-012-9643-6 [DOI] [PubMed] [Google Scholar]
- Lee S, Burns GL, Snell J, & McBurnett K (2014). Validity of the sluggish cognitive tempo symptom dimension in children: Sluggish cognitive tempo and ADHD-inattention as distinct symptom dimensions. Journal of Abnormal Child Psychology, 42, 7–19. doi: 10.1007/s10802-013-9714-3 [DOI] [PubMed] [Google Scholar]
- Leopold DR, Christopher ME, Burns GL, Becker SP, Olson RK, & Willcutt EG (2016). Attention-deficit/hyperactivity disorder and sluggish cognitive tempo throughout childhood: Temporal invariance and stability from preschool through ninth grade. Journal of Child Psychology and Psychiatry, 57, 1066–1074. doi: 10.1111/jcpp.12505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchetti I, Van de Putte E, & Koster EH (2014). Self-generated thoughts and depression: from daydreaming to depressive symptoms. Frontiers in Human Neuroscience, 8, 131. doi: 10.3389/fnhum.2014.00131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall SA, Evans SW, Eiraldi RB, Becker SP, & Power TJ (2014). Social and academic impairment in youth with ADHD, predominately inattentive type and sluggish cognitive tempo. Journal of Abnormal Child Psychology, 42, 77–90. doi: 10.1007/s10802-013-9758-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBurnett K, Villodas M, Burns GL, Hinshaw SP, Beaulieu A, & Pfiffner LJ (2014). Structure and validity of sluggish cognitive tempo using an expanded item pool in children with attention-deficit/hyperactivity disorder. Journal of Abnormal Child Psychology, 42, 37–48. doi: 10.1007/s10802-013-9801-5 [DOI] [PubMed] [Google Scholar]
- McDonald RP, & Ho MH (2002). Principles and practice in reporting structural equation analyses. Psychological Methods, 7, 64–82. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, … Swendsen J (2010). Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry, 49, 980–989. doi: 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer TD, Finucane L, & Jordan G (2011). Is risk for mania associated with increased daydreaming as a form of mental imagery? Journal of Affective Disorders, 135, 380–383. doi: 10.1016/j.jad.2011.06.002 [DOI] [PubMed] [Google Scholar]
- Muthén LK (2013). Example for type=complex. Retrieved from http://www.statmodel.com/discussion/messages/12/776.html?1491090688
- Muthén LK, & Muthén BO (1998–2018). Mplus user’s guide (Eigth ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Olatunji BO, & Cole DA (2009). The longitudinal structure of general and specific anxiety dimensions in children: testing a latent trait-state-occasion model. Psychological Assessment, 21, 412–424. doi: 10.1037/a0016206 [DOI] [PubMed] [Google Scholar]
- Penny AM, Waschbusch DA, Klein RM, Corkum P, & Eskes G (2009). Developing a measure of sluggish cognitive tempo for children: content validity, factor structure, and reliability. Psychological Assessment, 21, 380–389. doi: 10.1037/a0016600 [DOI] [PubMed] [Google Scholar]
- Preszler J, Burns GL, Litson K, Geiser C, Servera M, & Becker SP (2019). How consistent is sluggish cognitive tempo across occasions, sources, and settings? Evidence from latent state-trait modeling. Assessment, 26, 99–110. doi: 10.1177/1073191116686178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sáez B, Servera M, Burns GL, & Becker SP (2019). Advancing the multi-informant assessment of sluggish cognitive tempo: Child self-report in relation to parent and teacher ratings of SCT and impairment. Journal of Abnormal Child Psychology, 47, 35–46. doi: 10.1007/s10802-018-0436-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Servera M, Bernad MD, Carrillo JM, Collado S, & Burns GL (2016). Longitudinal correlates of sluggish cognitive tempo and ADHD-inattention symptom dimensions with Spanish children. Journal of Clinical Child and Adolescent Psychology, 45, 632–641. doi: 10.1080/15374416.2015.1004680 [DOI] [PubMed] [Google Scholar]
- Smith ZR, Eadeh HM, Breaux RP, & Langberg JM (2019). Sleepy, sluggish, worried, or down? The distinction between self-reported sluggish cognitive tempo, daytime sleepiness, and internalizing symptoms in youth with attention-deficit/hyperactivity disorder. Psychological Assessment, 31, 365–375. doi: 10.1037/pas0000671 [DOI] [PubMed] [Google Scholar]
- Starr LR, Stroud CB, & Li YI (2016). Predicting the transition from anxiety to depressive symptoms in early adolescence: Negative anxiety response style as a moderator of sequential comorbidity. Journal of Affective Disorders, 190, 757–763. doi: 10.1016/j.jad.2015.10.065 [DOI] [PubMed] [Google Scholar]
- Stawarczyk D, Majerus S, Van der Linden M, & D’Argembeau A (2012). Using the daydreaming frequency scale to investigate the relationships between mind-wandering, psychological well-being, and present-moment awareness. Frontiers in Psychology, 3, 363. doi: 10.3389/fpsyg.2012.00363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian SV, Jones K, & Duncan C (2003). Multilevel methods for public health research. In Kawachi I & Berkman LF (Eds.), Neighborhoods and health (pp. 65–111). New York: Oxford University Press. [Google Scholar]
- Wang J, & Wang X (2012). Structural equation modeling: Applications using Mplus. West Sussex, United Kingdom: John Wiley & Sons. [Google Scholar]
- Willcutt EG, Chhabildas N, Kinnear M, DeFries JC, Olson RK, Leopold DR, … Pennington BF (2014). The internal and external validity of sluggish cognitive tempo and its relation with DSM-IV ADHD. Journal of Abnormal Child Psychology, 42, 21–35. doi: 10.1007/s10802-013-9800-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolraich ML, Bard DE, Neas B, Doffing M, & Beck L (2013). The psychometric properties of the Vanderbilt attention-deficit hyperactivity disorder diagnostic teacher rating scale in a community population. Journal of Developmental and Behavioral Pediatrics, 34, 83–93. doi: 10.1097/DBP.0b013e31827d55c3 [DOI] [PubMed] [Google Scholar]
- Yung TWK, Lai CYY, Chan JYC, Ng SSM, & Chan CCH (2019). Neuro-physiological correlates of sluggish cognitive tempo (SCT) symptoms in school-aged children. European Child and Adolescent Psychiatry. Advance online publication. doi: 10.1007/s00787-019-01353-1 [DOI] [PubMed] [Google Scholar]