Abstract
Introduction
Patients with severe visceral abdominal or pelvic pain are sometimes candidates for celiac or superior hypogastric block. These blocks are performed in the prone position that is usually very painful for these patients. We introduce another position for these blocks that can be better tolerated.
Case Presentation
We performed the superior hypogastric plexus block in the lateral position in a patient who was suffering from severe abdominal and pelvic pain. The procedure was done under the guide of C-Arm fluoroscopy. After the procedure, the pain score reduced to 2 out of 10 on the 11-point Numeric Rating Scale and the patient was discharged without any complication.
Conclusions
Superior hypogastric plexus block in the lateral position was safe and effective for a patient with severe abdominal and pelvic pain.
Keywords: Pain, Cancer, Pelvic Pain, Hypogastric Plexus, Block, Lateral Position, Intra-Abdominal
1. Introduction
Patients with pelvic visceral malignancies have severe pain that is sometimes refractory to oral and parenteral analgesics. Oncologic pelvic pain can have visceral, somatic, or neuropathic origins (1). About 75% of cancer patients suffer from pain at any time during the course of their disease. Half of these patients will have moderate to severe pain and up to 30% will suffer from very severe pain (2, 3). Superior hypogastric plexus block has been proposed as an effective treatment for visceral pelvic pain syndromes. However, the prone position is sometimes very painful for patients suffering from abdominal and pelvic pain. Moreover, there is always some concern to sedate a patient in the prone position while the airway is not secured and the position is not suitable for immediate airway management if indicated (4, 5).
2. Case Presentation
A 42-year-old woman with a severe lower abdominal and pelvic pain due to advanced cervical uterine cancer was referred to our pain clinic. Cancer had been diagnosed five months ago. The patient had used many pain killers and the pain was intractable to many analgesic modalities. She was a candidate for a superior hypogastric plexus block. In a uterine cervix biopsy, moderately differentiated non-keratinizing squamous cell carcinoma was reported. She had five sessions of chemotherapy and 25 sessions of radiotherapy in the past three months. She was receiving methadone 5 - 7.5 mg every eight hours, gabapentin, and acetaminophen for pain management during these three months. This medical treatment was administered by the palliative care service but in spite of this medical management, she was suffering from severe pain in lower abdominal and pelvic areas. Then, she was referred to our pain clinic. The pain was evaluated by the Brief Pain Inventory and the overall pain intensity was 8 out of 10 on the 11-point NRS scale (6).
In an MRI study, a heterogenous enhancing lobulated mass (9 × 8.5 cm) was reported involving lower uterine cervix and upper vagina suggestive for a cervical tumoral lesion. There were numerous enhancing masses (adenopathies) in both iliac and para-aortic regions, as well. Moreover, enhancing adnexal masses (4 - 5 cm) were observed in the right and left sides. The liver, spleen, pancreas, and both kidneys did not show any mass or abnormality.
On the physical exam, she had severe deep tenderness and pain in the lower abdominal and pelvic areas. Organomegaly was felt in the lower abdomen. She did not have any abdominal rebound tenderness; therefore, peritonitis was ruled out. There were radiotherapy-induced blisters on the lumbar skin. A dermatological consultation was requested. No infection or important lesion was reported over the skin of the lumbar area.
The origin of the pain was a pelvic malignancy. Consequently, we decided to perform the superior hypogastric plexus block to relieve the pain of the patient. The most disturbing position for this patient was the prone position due to severe abdominal and pelvic pain. The patient could not tolerate this position even for a few moments.
2.1. Technical Discussion
The patient was unable to tolerate the prone position. Therefore, we decided to perform the block in the left lateral position (Figure 1). After positioning the patient and applying vital sign monitoring (SPO2, NIBP, ECG, RR, and HR), midazolam 1 mg and fentanyl 50 µg were administered for sedation. The skin was prepped with povidone-iodine and then draped. Then, 10 mL of lidocaine 0.5% was infiltrated for skin local anesthesia. Two Chiba needles (15 cm, 20 G) were bilaterally placed 6 cm lateral to the midline at the level of the L5 vertebra. Then, the needles were advanced from the lateral to midline direction based on the tunneling technique and oblique views (Figure 2A and B) obtained by the guide of the C-arm fluoroscopy. The target point was the anterolateral surface of the L5-S1 junction. We placed the right needle first and subsequently put the left needle (Figure 1). All steps of the procedure were done under the guidance of the multiple fluoroscopic images (oblique, lateral and anteroposterior views).
Figure 1. Both needles placed in the left lateral decubitus position.
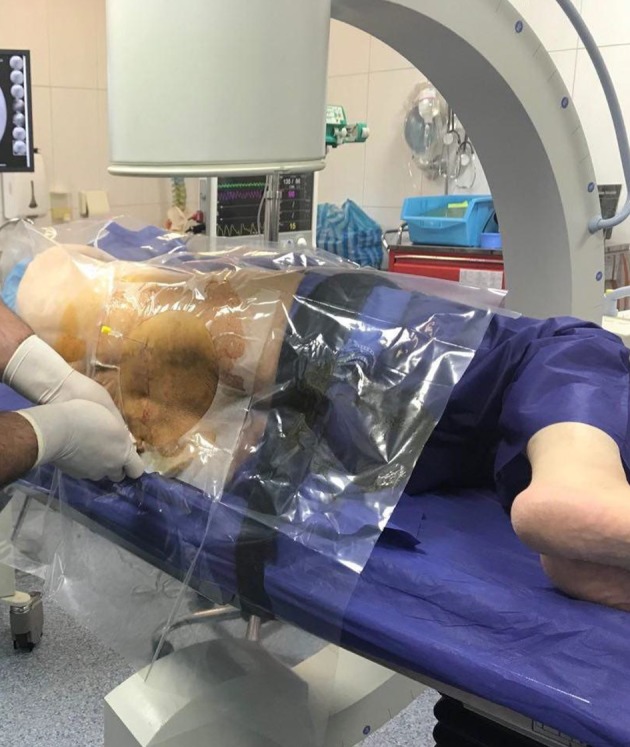
Figure 2. Fluoroscopic views from the needle insertion while the patient was in the left lateral decubitus position. Image A shows the right needle insertion almost in the tunnel (oblique) view. Image B shows the left needle insertion in the oblique view. Image C is the anteroposterior view after the dye injection through the right needle. Images D and E show the lateral views after contrast injection through the right and left needles.
After the injection of the contrast, the right position of the tip of the needles was confirmed. The contrast was not adequately distributed toward the anterior surface of the S1 and did not perfectly cover the L5 - S1 junction. Bilateral superior hypogastric plexus was blocked in the lateral position with 10 ml of bupivacaine 0.25% and 40 milligrams methylprednisolone on each side (Figure 2C - E).
The patient was comfortable in the lateral position during the procedure. The images were accurate and the block was performed straight forward without any technical problem. The pain score reduced to 2 out of 10 on the 11-point NRS scale after the end of the procedure.
3. Discussion
Cervical cancer is one of the most common causes of women’s death all over the world. The unresectable recurrent disease may be associated with moderate to severe pelvic pain resistant to medical therapy. Therefore, interventional pain management is needed to relieve the pain and improve the quality of life (7). Superior hypogastric plexus contains afferent pain fibers from the organs located in the lower abdomen and pelvic area. Blocking of this plexus can potentially relieve the pain originating from the above-mentioned regions (7). A superior hypogastric plexus block is one of the procedures proposed for the management of patients with pelvic visceral pain (8). This procedure is usually performed in the prone position with a pillow under the abdomen to achieve a better view while advancing the needles toward the anterolateral surface of the junction of the L5 - S1 (9).
In this case, we had to use another position that was not routinely mentioned in the pain literature. The patient was positioned in left lateral decubitus because of severe abdominal and pelvic pain. She was fixed with a safety belt below the pelvic area. The right-side (upward) procedure was done easier than the left-side procedure. The contrast did not adequately distribute toward the pelvis. The patient had received radiotherapy for 25 sessions. Radiotherapy may produce significant fibrosis in the pelvic area. Therefore, the fibrosis could impede the caudal distribution of the dye over the anterior surface of the S1 (Figure 2). We believe that this position can be used for the celiac block, as well. We did the celiac block in the lateral position previously without any technical problem.
3.1. Conclusions
Superior hypogastric plexus block in the lateral position was safe and effective for a patient with severe abdominal and pelvic pain due to a pelvic malignancy. Therefore, we propose that the patients suffering from severe abdominal or pelvic pain that are candidates for celiac or superior hypogastric plexus block can be put in the lateral position during the procedure.
Footnotes
Conflict of Interests:There is no conflict of interest in this study.
Ethical Approval:The ethics committee of our institution approved our study.
Funding/Support:There was no funding support for this study.
Patient Consent:Informed consent was obtained from the patient.
Contributor Information
Farhad Tavakoli, Email: fahatv@yahoo.com.
Fardin Yousefshahi, Email: yousefshahi@tums.ac.ir.
Arman Dabir, Email: dabirarman@gmail.com.
Hossein Majedi, Email: hossein_majedi@yahoo.com.
References
- 1.Plancarte R, de Leon-Casasola OA, El-Helaly M, Allende S, Lema MJ. Neurolytic superior hypogastric plexus block for chronic pelvic pain associated with cancer. Reg Anesth. 1997;22(6):562–8. [PubMed] [Google Scholar]
- 2.Portenoy RK. Cancer pain. Epidemiology and syndromes. Cancer. 1989;63(11 Suppl):2298–307. doi: 10.1002/1097-0142(19890601)63:11<2298::aid-cncr2820631140>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 3.Levy MH. Pharmacologic treatment of cancer pain. N Engl J Med. 1996;335(15):1124–32. doi: 10.1056/NEJM199610103351507. [DOI] [PubMed] [Google Scholar]
- 4.Bonica JJ. The management of pain of malignant disease with nerve blocks. Anesthesiology. 1954;15(3):280–91. doi: 10.1097/00000542-195405000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Wechsler RJ, Maurer PM, Halpern EJ, Frank ED. Superior hypogastric plexus block for chronic pelvic pain in the presence of endometriosis: CT techniques and results. Radiology. 1995;196(1):103–6. doi: 10.1148/radiology.196.1.7784552. [DOI] [PubMed] [Google Scholar]
- 6.Majedi H, Dehghani SS, Soleyman-Jahi S, Emami Meibodi SA, Mireskandari SM, Hajiaghababaei M, et al. Validation of the Persian version of the brief pain inventory (BPI-P) in chronic pain patients. J Pain Symptom Manage. 2017;54(1):132–138 e2. doi: 10.1016/j.jpainsymman.2017.02.017. [DOI] [PubMed] [Google Scholar]
- 7.Bharti N, Singla N, Batra Y. Radiofrequency ablation of superior hypogastric plexus for the management of pelvic cancer pain. India J Pain. 2016;30(1):58. doi: 10.4103/0970-5333.173481. [DOI] [Google Scholar]
- 8.Plancarte R, Amescua C, Patt RB, Aldrete JA. Superior hypogastric plexus block for pelvic cancer pain. Anesthesiology. 1990;73(2):236–9. doi: 10.1097/00000542-199008000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Kamel MA, Ahmed ASR, Shaaban MH, Hashem RH. Comparison between fluoroscopic posterior versus ultrasound-guided anterior approach for superior hypogastric plexus neurolysis: A prospective, randomized, comparative study. Res Opin Anesth Intensiv Care. 2016;3(4):151. doi: 10.4103/2356-9115.195882. [DOI] [Google Scholar]



