Abstract
Background
Acupuncture has been used for more than two thousand years as part of traditional Chinese medicine.
Objectives
This randomized prospective clinical trial aimed to compare the effect of acupuncture on K1 (Yongquan) and DU26 (Renghong) with acupuncture on K1 (Yongquan) and DU25 (Suliao), with sham acupuncture on the recovery time of general anesthesia.
Methods
The patients (51) were randomly assigned to three groups: (A) acupuncture on K1 and DU26, (B) acupuncture on K1 and DU25, and (C) sham acupuncture. In each group, at the end of surgery acupuncture was performed accordingly for twenty minutes and the Bispectral Index (BIS) values at end of surgery, 5th minute, 10th minute, 15th minute and 20th minute as well as time of extubation and time of eye opening after the end of surgery were evaluated.
Results
BIS study at 5th minute, 10th minute and 15th minute after the end of surgery in the groups revealed a significant difference between sham acupuncture group and both A and B acupuncture groups, which was higher in groups A and B in comparison with sham acupuncture group. Time of opening eyes and time of extubation after the end of surgery between group A and sham acupuncture group differed significantly, which was earlier in group A. There was no significant difference between group B and sham acupuncture group in terms of eye opening and extubation time.
Conclusions
Acupuncture on K1 and DU26 accelerates restoring of consciousness and shortens of eye opening and extubation after general anesthesia, but on K1 and DU25 only speeds up retrieving of consciousness without significant effect on time of eye opening or extubation after general anesthesia.
Keywords: Acupuncture, General Anesthesia, K1, DU26, DU25, Recovery Time
1. Background
Acupuncture is an important part of traditional Chinese medicine (1). Acupuncture application goes back to more than two thousand years ago (1, 2). Acupuncture in the field of anesthesia has been studied widely (3) which shows many benefits in this setting including sedative and anxiolytic effects (4), reducing hypnotics consumption and analgesic demand (5, 6), hemodynamic stability (7, 8), decreasing post-operative nausea and vomiting (9-11) and protective organ effects during anesthesia (12, 13).
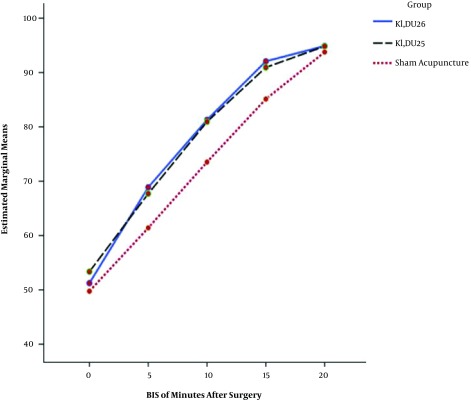
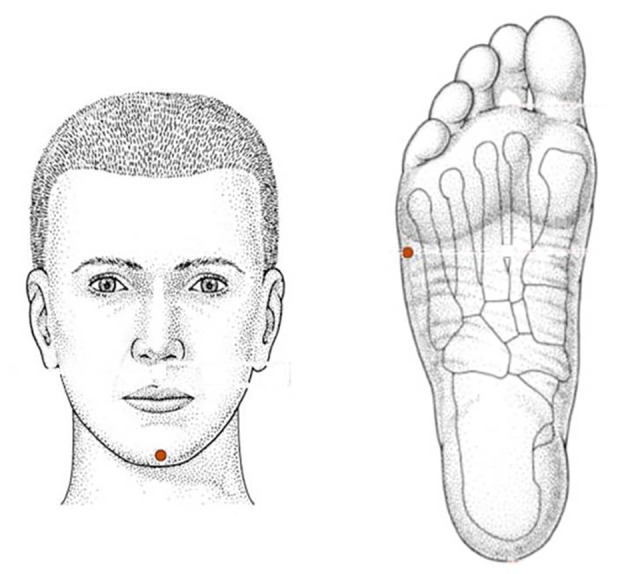
Regarding the effect of acupuncture in recovery time after general anesthesia there is a study showing acceleration in recovery time by using K1 (Yongquan) (Figure 1), and DU26 (Renghong), (Figure 2), acupoints. The study also revealed the synergism effect in reduction of recovery time by using those acupoints together in comparison with their solitary application (14). Both K1 (Yongquan) and DU26 (Renghong) are traditionally used as symptomatic treatment in loss of consciousness (15) another acupoint with similar property which is comparable with DU26 (Renghong) (16) and in somehow is more effective in the awakening of comatose patients is DU25 (Suliao) (17) (Figure 3).
Figure 1. K1 acupuncture point.
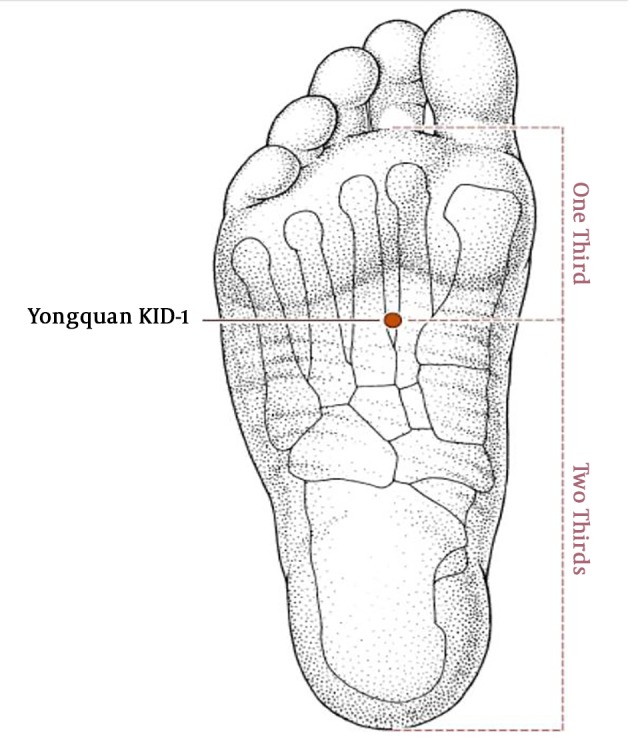
Figure 2. DU26 acupuncture point.
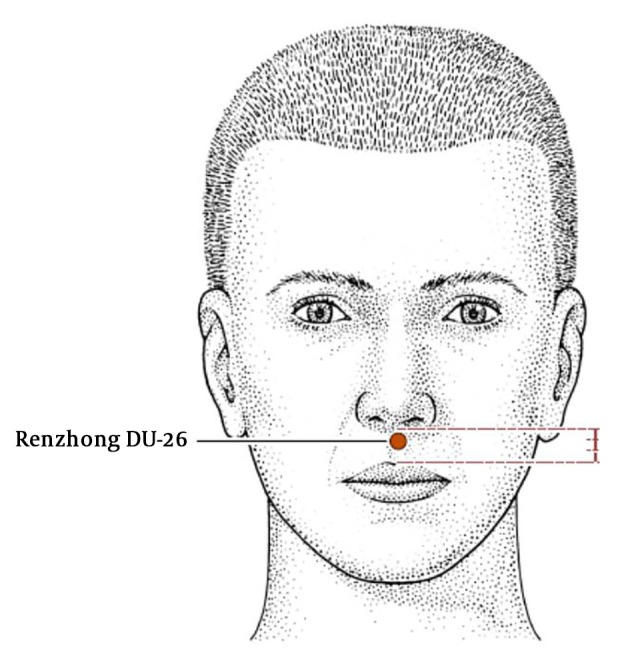
Figure 3. DU25 acupuncture point.
2. Objectives
In this study we compared the effect of acupuncture on K1 (Yongquan) and DU26 (Renghong) with acupuncture on K1 (Yongquan) and DU25 (Suliao) as well as with sham acupuncture on recovery time of patients who underwent general anesthesia in terms of the Bispectral Index (BIS), time of eye opening and time of extubation after the end of surgery.
3. Methods
This prospective randomized, double-blind, clinical trial was registered in the Iranian Registry of Clinical Trials (IRCT2017071710599N17) and approved by the ethics committee of Iran University of Medical Sciences in Tehran, Iran (18). The study was conducted on 51 adult (18 - 60 years old) participants who were scheduled for elective short (30 - 120 minutes) surgeries under general anesthesia from 2017-08-13 to 2018-02-19 in a training hospital, Tehran, Iran.
Inclusion criteria were defined as: consent to participate in the study; ASA score I and II; non neurosurgical surgeries; non pregnant; no anatomical abnormalities or infection in acupuncture sites; without history of neurological condition, psychiatric disorders, addiction, cardiac arrhythmia, hypertension, diabetes (type I and II), coagulopathy, allergy to propofol, and head trauma. Patients were excluded from study in case of hypotension more than 10 minutes during surgery; blood loss more than 250 cc during surgery; surgery time less than 30 minutes or more than 120 minutes.
After selecting patients according to inclusion criteria, informed consent was taken. Patients were transferred to operating room and monitored by heart rate, non-invasive blood pressure and pulse oximetry. End tidal CO2 (EtCO2) and BIS (BIS VISTA™ Monitoring System, Norwood, USA) were measured during and after surgery. BIS values were recorded every 5 minutes during surgery.
The same anesthesia protocol was applied to all patients (premedication: midazolam 0.01 mg/kg and fentanyl 2 μ/kg, induction: propofol 2 mg/kg, muscle relaxant: cisatracurium 0.2 mg/kg, maintenance of anesthesia with infusion of propofol and remifentanil to keep BIS value within 40 - 60). Mechanical ventilation was employed by tidal volume of 8 - 10 mL/kg and adjusting respiratory rate to maintain EtCO2 within 30 - 35 mmHg. Before the end of surgery, Apotel 1 gr/IV was administrated. At the end of surgery, residual neuromuscular block was reversed by neostigmine 0.04 mg/kg and atropine 0.02 mg/kg and anesthesia administration was stopped.
At the end of surgery, patients were assigned to one of three groups by block randomization according to a computer generated random list. First group (A) acupuncture on K1, DU26 acupoints, second group (B) acupuncture on K1, DU25 acupoints and third group (C) sham acupuncture on lateral margin of both feet in the level of K1 (perpendicular insertion,0.5 - 0.7 cm deep) and apex of chin (oblique transverse-up insertion, 0.2 - 0.5 cm deep) (Figure 4), and acupuncture was performed accordingly for twenty minutes.
Figure 4. Sham acupuncture points.
Disposable sterile acupuncture needles (Dongbang Medical Co., Korea) were used (0.25 × 25 mm for K1 and feet sham acupuncture and 0.18 × 15 mm for face). Needles were stimulated manually according to acupuncture practice by expert acupuncturist and patients did not receive any sensory or verbal stimulations.
BIS values at end of surgery, 5th minute, 10th minute, 15th minute and 20th minute after the end of surgery (BIS0, BIS5, BIS10, BIS15, and BIS20, respectively) were recorded as well as time of extubation and time of eye opening. Extubation was performed by the anesthesiologist in charge of patients who was not involved in the study and was not aware of acupuncture practice and study setting. Data collection was made by a resident in anesthesiology who was also not involved in the study and not aware of acupuncture practice and study setting. Needles were removed before transferring patient to post anesthesia care unit.
3.1. Statistical Analysis
The collected data was analyzed using SPSS for Windows 20.0 (IBM Corporation, Armonk, NY, USA). Continuous data are shown as mean ± standard deviation and categorical data are shown as number (%). Categorical data was analyzed by chi-square test. Data had normal distribution according to Kolmogorov-Smirnov test. The ANOVA one-way test or repeated measure ANOVA was performed to analyze continuous data as appropriate. Scheffe post hoc test were used for multiple comparisons between groups. The null hypothesis was rejected at alpha (P values) less than 0.05.
4. Results
A total number of 51 patients were enrolled in the study according to inclusion criteria; none of them met the exclusion criteria for hypotension during surgery, intraoperative bleeding or duration of surgery. At the end of surgery, participants were randomly assigned to the three groups, with 17 participants in each group.
There were no significant differences between three groups in terms of age, weight, gender, duration of surgery, total dose of propofol and remifentanil consumed during surgery, and BIS value at the end of surgery (Tables 1 and 2). Although ANOVA analysis showed difference in BIS20 in groups (Table 2, P = 0.047), there was no significant difference between groups by post hoc analysis.
Table 1. Patient Characteristics in the Three Groups.
| Groups | Group A (K1, DU26) | Group B (K1, DU25) | Sham Acupuncture | P Value |
|---|---|---|---|---|
| Age, y | 35.7 ± 9.3 | 34.5 ± 8.4 | 34.1 ± 8.4 | 0.863 |
| Weight, kg | 67.2 ± 8.6 | 65.7 ± 8.7 | 70.1 ± 7.0 | 0.298 |
| Gender | 0.784 | |||
| Male | 9 (53) | 11 (65) | 10 (59) | |
| Female | 8 (47) | 6 (35) | 7 (41) | |
| Duration of Surgery, min | 82.3 ± 13.8 | 79.7 ± 12.0 | 80.5 ± 14.6 | 0.846 |
| Total dose of propofol, mg | 582.9 ± 116.1 | 552.0 ± 103.0 | 568.8 ± 102.1 | 0.705 |
| Total dose of remifentanil, mg | 1.3 ± 0.4 | 1.1 ± 0.4 | 1.4 ± 0.3 | 0.337 |
| Time of eye opening, min | 12.1 ± 1.1 | 13.1 ± 1.2 | 14.0 ± 1.7 | 0.002b |
| Time of extubation, min | 10.8 ± 2.0 | 11.4 ± 2.0 | 13.1 ± 2.4 | 0.015b |
aValues are expressed as mean ± SD or No. (%).
bSignificant at P < 0.05.
Table 2. Bispectral Index Values in the Three Groups After the End of Surgerya.
| Groupsb | Group A (K1, DU26) | Group B (K1, DU25) | Sham Acupuncture | P Value |
|---|---|---|---|---|
| BIS 0, min | 51.2 ± 4.5 | 53.3 ± 5.1 | 49.7 ± 4.8 | 0.106 |
| BIS 5, min | 68.8 ± 6.0 | 67.7 ± 4.4 | 61.4 ± 5.1 | 0.000c |
| BIS 10, min | 81.2 ± 6.7 | 80.9 ± 4.7 | 73.5 ± 6.8 | 0.001c |
| BIS 15, min | 92.0 ± 4.8 | 90.9 ± 3.7 | 85.1 ± 5.6 | 0.000c |
| BIS 20, min | 94.8 ± 1.4 | 94.8 ± 1.2 | 93.7 ± 1.6 | 0.047c |
aValues are expressed as mean ± SD.
bBIS 0 represents BIS value at the end of surgery; BIS 5, BIS 10, BIS 15 and BIS 20 represent BIS values at 5, 10, 15 and 20 minute after the end of surgery, respectively.
cSignificant at P < 0.05.
Time of eye opening after the end of surgery differed among groups (Table 1, P = 0.002). Post hoc analysis indicated significant difference between group A (K1, DU26) and sham acupuncture group (Table 3, P = 0.002).
Table 3. Comparison of BIS Values, Time of Opening Eye After Surgery and Time of Extubation After Surgery Between the Three Groups by Post Hoc Analysis.
| Groupsa | P Values | ||
|---|---|---|---|
| Sham Acupuncture | Group A ( K1, DU26 | ||
| Group A ( K1, DU26) | Group B (K1, DU25) | Group B (K1, DU25) | |
| BIS 5 | 0.001b | 0.004b | 0.807 |
| BIS 10 | 0.003b | 0.004b | 0.986 |
| BIS 15 | 0.001b | 0.004b | 0.795 |
| BIS 20 | 0.077 | 0.123 | 0.973 |
| Time of extubation | 0.020b | 0.110 | 0.746 |
| Time of eye opening | 0.002b | 0.250 | 0.133 |
aBIS 5, BIS 10, BIS 15 and BIS 20 represent BIS values at 5, 10, 15 and 20 minute after the end of surgery, respectively.
bSignificant at P < 0.05.
Time of extubation after the end of surgery varied among groups (Table 1, P = 0.015). Post hoc analysis revealed significant difference between group A (K1, DU26) and sham acupuncture group (Table 3, P = 0.020).
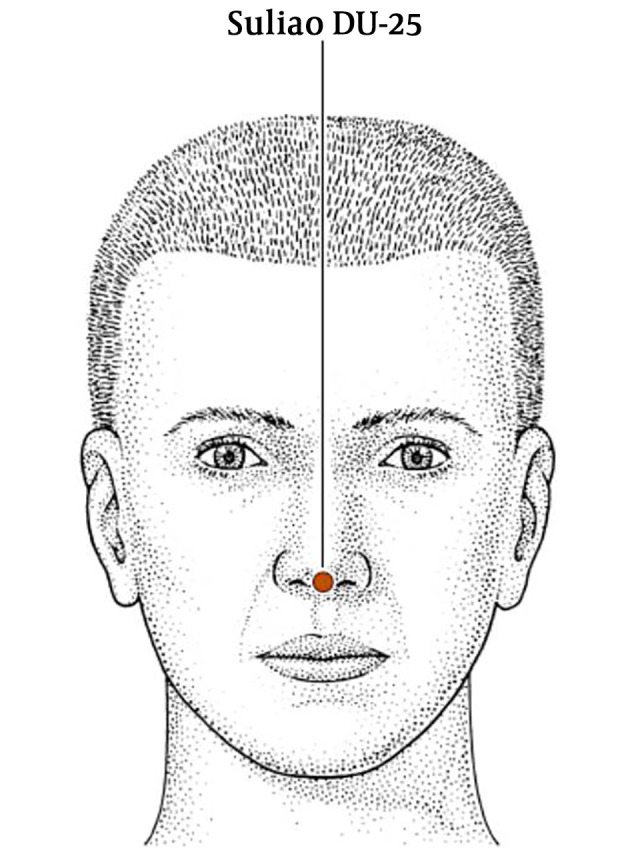
BIS5, BIS10 and BIS15 had significant difference in the three groups (Table 1, P = 0.000, P = 0.001 and P = 0.000, respectively). Post hoc analysis revealed significant difference between sham acupuncture group and group A (K1, DU26) in BIS5, BIS10 and BIS15 (Table 3, P = 0.001, P = 0.003 and P = 0.001, respectively) and also showed significant difference between sham acupuncture group and group B (K1, DU25) in BIS5, BIS10 and BIS15 (Table 3, P = 0.004 for all three of them).
Figure 5 shows means of BIS values in the three groups in different time courses; BIS0, BIS5, BIS10, BIS15 and BIS20. Repeated measure ANOVA analysis confirmed significant difference between sham acupuncture group and group A (K1, DU26) and group B (K1, DU25) (P = 0.002 and P = 0.003, respectively).
Figure 5. Means of BIS values at the end of surgery, 5th minute, 10th minute, 15th minute and 20th minute after surgery in the three study groups.
5. Discussion
Many studies have been performed to evaluate different aspects of acupuncture efficacy during perioperative period and anesthesia related issues including; sedative and anxiolytic effects (4), reducing hypnotics consumption and analgesic demand (5, 6), hemodynamic stability (7, 8), decreasing post-operative nausea and vomiting (9-11), protective organ effects during anesthesia (12, 13) and shortening recovery time after general anesthesia (14). Improving consciousness level by acupuncture after cardiac arrest and hypovolemic shock (19, 20) and in comatose patients (17) has also been reported.
According to TCM, K1 (Yongquan), DU26 (Renghong) and DU25 (Suliao) are effective acupoints in retrieving consciousness (15-17). Kidney channel plays an important role in consciousness, particularly K1 (Yongquan) as jing-well point of kidney meridian which can bubble up chi through the channel (20, 21). Therefore, in this study we employed K1 as a common acupoint in conjunction with two other acupoints, DU26 and DU25, separately.
In our clinical observation, there were no significant differences between three groups in terms of age, weight, gender, duration of surgery, total dose of propofol and remifentanil consumed during surgery, and BIS value at the end of surgery (Tables 1 and 2) as confounding or intervening factors.
BIS study in 5 minutes, 10 minutes and 15 minutes after the end of surgery in the three groups revealed significant difference between sham acupuncture group and both acupuncture groups A and B (Table 2). There was no significant difference in BIS values at 20 minutes after the end of surgery between the three groups, which can be justified by increasing level of consciousness due to passing the time and elimination of anesthetics. Pattern of BIS values in the three groups in different time courses after the end of surgery shows the similar accelerating upsurge in both group A and B in comparison with steady rise in sham acupuncture group (Figure 1).
Time of opening eyes and time of extubation after the end of surgery between group A and sham acupuncture group differed significantly (P = 0.002 and P = 0.020, respectively) which confirmed the Gemma et al. findings who in their study, evaluated effectiveness of K1 and DU26 acupuncture in recovery time after general anesthesia (14).
Although in our study acupuncture on K1 and DU25 compared with acupuncture on K1 and DU26 had similar properties in BIS values and regaining consciousness, but acupuncture on K1 and DU25 did not show matching results in eye opening and extubation time, possibly because of specific positive stimulation on respiratory neural pathway and phrenic nerve due to DU26 acupuncture (22).
5.1. Conclusions
Acupuncture on K1 and DU26 accelerates restoration of consciousness as well as shortening time of eye opening and extubation after general anesthesia, but acupuncture on K1 and DU25 only speeds up retrieval of consciousness without significant effect on the time of eye opening or extubation after general anesthesia.
5.2. Suggestions
In our project, we used manual toning stimulation on needles according to TCM practice. Alternatively, the stimulation can be applied by electro stimulation, moxibustion or laser. There are some other acupoints with proven effects in resuscitation and consciousness improvement such as PC-9 (Zhong Chong) (15, 21) which would be worth investigating in the recovery setting of anesthesia in future studies.
Acknowledgments
The authors wish to thank Rasoul Akram Hospital Clinical Research Development Center, Iran University of Medical Science for its editorial assistance.
Footnotes
Authors' Contribution: Study concept and design: Seyed Hamid Reza Faiz, Nasim Nikoubakht, and Farnad Imani; analysis and interpretation of data: Hossein Sadegh and Mohsen Ziyaeifard; drafting of the manuscript: Poupak Rahimzadeh, Mohsen Ziyaeifard, and Farnad Imani; critical revision of the manuscript for important intellectual content: Seyed Hamid Reza Faiz, Farnad Imani, and Poupak Rahimzadeh; statistical analysis: Hossein Sadegh, Nasim Nikoubakht, and Poupak Rahimzadeh.
Clinical Trial Registration Code: IRCT2017071710599N17.
Conflict of Interests: The authors have no conflict of interest to declare.
Ethical Approval: The study was approved by the ethics committee of Iran University of Medical Sciences in Tehran, Iran.
Funding/Support: It was not declared by the authors.
Patient Consent: Informed consent was obtained from all individuals.
Contributor Information
Seyed Hamid Reza Faiz, Email: hrfaiz@hotmail.com.
Nasim Nikoubakht, Email: nnikobakht@yahoo.com.
Farnad Imani, Email: farnadimani@yahoo.com.
Mohsen Ziyaeifard, Email: mziyaeifard@yahoo.com.
Hossein Sadegh, Email: hossein.sadegh@gmail.com.
Poupak Rahimzadeh, Email: p.rahimzadeh.anesthesiology@gmail.com.
References
- 1.Ma KW. The roots and development of Chinese acupuncture: From prehistory to early 20th century. Acupunct Med. 1992;10(1_suppl):92–9. doi: 10.1136/aim.10.Suppl.92. [DOI] [Google Scholar]
- 2.White A, Ernst E. A brief history of acupuncture. Rheumatology (Oxford). 2004;43(5):662–3. doi: 10.1093/rheumatology/keg005. [DOI] [PubMed] [Google Scholar]
- 3.Lu Z, Dong H, Wang Q, Xiong L. Perioperative acupuncture modulation: More than anaesthesia. Br J Anaesth. 2015;115(2):183–93. doi: 10.1093/bja/aev227. [DOI] [PubMed] [Google Scholar]
- 4.Gioia L, Cabrini L, Gemma M, Fiori R, Fasce F, Bolognesi G, et al. Sedative effect of acupuncture during cataract surgery: Prospective randomized double-blind study. J Cataract Refract Surg. 2006;32(11):1951–4. doi: 10.1016/j.jcrs.2006.06.027. [DOI] [PubMed] [Google Scholar]
- 5.Greif R, Laciny S, Mokhtarani M, Doufas AG, Bakhshandeh M, Dorfer L, et al. Transcutaneous electrical stimulation of an auricular acupuncture point decreases anesthetic requirement. Anesthesiology. 2002;96(2):306–12. doi: 10.1097/00000542-200202000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Dias M, Carneiro NM, Guerra LA, Velarde GC, de Souza PA, da Silva LL, et al. Effects of electroacupuncture on local anaesthesia for inguinal hernia repair: A randomised placebo-controlled trial. Acupunct Med. 2010;28(2):65–70. doi: 10.1136/aim.2009.000570. [DOI] [PubMed] [Google Scholar]
- 7.Syuu Y, Matsubara H, Hosogi S, Suga H. Pressor effect of electroacupuncture on hemorrhagic hypotension. Am J Physiol Regul Integr Comp Physiol. 2003;285(6):R1446–52. doi: 10.1152/ajpregu.00243.2003. [DOI] [PubMed] [Google Scholar]
- 8.Saghaei M, Ahmadi A, Rezvani M. Clinical trial of nitroglycerin-induced controlled hypotension with or without acupoint electrical stimulation in microscopic middle ear surgery under general anesthesia with halothane. Acta Anaesthesiol Taiwan. 2005;43(3):135–9. [PubMed] [Google Scholar]
- 9.World Health Organization . Acupuncture: review and analysis of reports on controlled clinical trials. World Health Organization; 2002. [Google Scholar]
- 10.Lee A, Fan LT. Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev. 2009;(2):CD003281. doi: 10.1002/14651858.CD003281.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheong KB, Zhang JP, Huang Y, Zhang ZJ. The effectiveness of acupuncture in prevention and treatment of postoperative nausea and vomiting--a systematic review and meta-analysis. PLoS One. 2013;8(12):e82474. doi: 10.1371/journal.pone.0082474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yan Q, Feng Y. [Acupuncture assisted anesthesia and its organ protective effects.]. Zhongguo Zhen Jiu. 2013;33(8):765–8. [PubMed] [Google Scholar]
- 13.Shen H, Chen YJ. [Effects of electro-acupuncture combined general anesthesia on myocardial injury of high blood sugar patients with coronary heart disease in the perioperative phase.]. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2012;32(12):1607–10. [PubMed] [Google Scholar]
- 14.Gemma M, Nicelli E, Gioia L, Moizo E, Beretta L, Calvi MR. Acupuncture accelerates recovery after general anesthesia: A prospective randomized controlled trial. J Integr Med. 2015;13(2):99–104. doi: 10.1016/S2095-4964(15)60159-5. [DOI] [PubMed] [Google Scholar]
- 15.Deadman P, Al-Khafaji M, Baker K. A manual of acupuncture. 2nd ed. UK: J Chin Med Publ East Sussex; 1998. [Google Scholar]
- 16.Lu M. [New explaination of mechanisms of indications of Suliao (GV 25) and Shuigou (GV 26).]. Zhongguo Zhen Jiu. 2006;26(7):487–8. [PubMed] [Google Scholar]
- 17.Xu KS, Song JH, Huang TH, Huang ZH, Yu LC, Zheng WP, et al. [Clinical efficacy observation of acupuncture at suliao (GV 25) on improving regain of consciousness from coma in severe craniocerebral injury.]. Zhongguo Zhen Jiu. 2014;34(6):529–33. [PubMed] [Google Scholar]
- 18.IRCT2017071710599N17, Iranian Registry of Clinical Trials. 2017 Available from: www.irct.ir.
- 19.Hsu CH, Hua Y, Jong GP, Chao CL, Liu JY, Hwang KC, et al. Shock resuscitation with acupuncture: Case report. Emerg Med J. 2006;23(3):e18. doi: 10.1136/emj.2004.023218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Inchauspe A. Traditional Chinese medicine K1 Yongquan and resuscitation: Another kind of "Lazarus phenomenon". Resuscitation. 2010;81(4):505–6. doi: 10.1016/j.resuscitation.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 21.Tseng YJ, Chao CY, Hung YC, Hsu SF, Hung IL, Hu WL. Efficacy of stimulation at the Jing-Well points of meridians. Int J Nurs Clin Pract. 2015;2(2) doi: 10.15344/2394-4978/2015/121. [DOI] [Google Scholar]
- 22.Zheng Y, Xu ML, Yang SR. [Mechanisms of effects of electrical stimulation of "Renzhong" (Du 26) on phrenic discharge in rabbits.]. Hua Xi Yi Ke Da Xue Xue Bao. 1989;20(4):384–8. [PubMed] [Google Scholar]