Abstract
Background
Hyperprolinemia type 2 (HPII) is a rare autosomal recessive disorder of the proline metabolism, that affects the ALDH4A1 gene. So far only four different pathogenic mutations are known. The manifestation is mostly in neonatal age, in early infancy or early childhood.
Case presentation
The 64-years female patient had a long history of abdominal pain, and episode of an acute neuritis. Ten years later she was admitted into the neurological intensive-care-unit with acute abdominal pain, multiple generalized epileptic seizures, a vertical gaze palsy accompanied by extensive lactic acidosis in serum 26.0 mmol/l (reference: 0.55–2.2 mmol/l) and CSF 12.01 mmol/l (reference: 1.12–2.47 mmol/l). Due to repeated epileptic seizures and secondary complications a long-term sedation with a ventilation therapy over 20 days was administered. A diagnostic work-up revealed up to 400-times increased prolin-level in urine CSF and blood. Furthermore, a low vitamin-B6 serum value was found, consistent with a HPII causing secondary pyridoxine deficiency and seizures. The ALDH4A1 gene sequencing confirmed two previously unknown compound heterozygous variants (ALDH4A1 gene (NM_003748.3) Intron 1: c.62 + 1G > A - heterozygous and ALDH4A1 gene (NM_003748.3) Exon 5 c.349G > C, p.(Asp117His) - heterozygous). Under high-dose vitamin-B6 therapy no further seizures occurred.
Conclusion
We describe two novel ALDH4A1-variants in an adult patient with hyperprolinemia type II causing secondary pyridoxine deficiency and seizures. Severe and potentially life-threatening course of this treatable disease emphasizes the importance of diagnostic vigilance and thorough laboratory work-up including gene analysis even in cases with atypical late manifestation.
Keywords: Hyperprolinemia type II, ALDH4A1 gene, Epilepsy, Vitamin B6 metabolism, Proline
Background
Hyperprolinemia type 2 (HPII) is an autosomal recessive disorder of the proline metabolism that is caused by a deficiency in pyrolin-5-carboxylate (P5C) dehydrogenase, which leads to an accumulation of P5C. In human, the protein is encoded by the ALDH4A1 gene and only four different pathogenic mutations are known so far (HGMD® Professional 2019.1) [1]. Pyridoxal phosphate (PLP) (active vitamin-B6 coenzyme) is de-activated by P5C acid [2], and PLP-depended enzymatic reactions in amino acid and neurotransmitter metabolism are disturbed. Consequently, PLP utilization is increased [2]. Neither prevalence nor incidence of HPII are exactly known. A 18-years long screening of 20,991 urinary organic acid profiles from an academic referral center in the Netherlands estimated a cumulative incidence of HPII of approximately 1 in 700,000 newborns [3]. Manifestation of previously reported patients was mostly in neonatal age, in early infancy or early childhood [4]. Patients suffered from generalized epileptic seizures and intellectual disability [4, 5].
Case presentation
In 2006, a 52-year old female patient was admitted to a neurological department due to sudden difficulties with swallowing and speech, ophthalmoparesis with a vertical and horizontal eye movement disorder, dysesthesia of the hands with a quality of “pins and needles” and a glove-like distribution, as well as generalized areflexia. Muscle strength was normal. A Miller Fisher syndrome was diagnosed. Under treatment with 150 g intravenous immunoglobulins the symptoms completely remitted within a few days. In the following years, the patient consulted the general practitioner and several gastroenterologists because of unspecific abdominal pain, from which she has been suffering since childhood. Diagnostics including computer tomography (CT), magnetic resonance imaging (MRI) and gastroscopy were normal.
In October 2017 the meanwhile 63-year old patient was hospitalized with generalized epileptic seizures with prolonged postictal confusion. Cerebral MRI showed no pathological findings, and therapy with levetiracetam was started.
In December 2017 the patient was admitted to our clinic for internal medicine because of persisting diarrhea, abdominal pain, renal failure and a reduced general state of health. Again, the patient had generalized epileptic seizures with postictal confusion and significantly reduced vigilance, accompanied from a lactic acidosis (serum-lactate 26.0 mmol/l (reference 0.55–2.2 mmol/l), pH 6.863), leading to admission to the neurological intensive care unit. Moreover, a slight, presumably residual ophthalmoparesis as vertical gaze palsy with conjugate, bilateral limitation of the eye movements in upgaze was evident. The anticonvulsive therapy with levetiracetam (3 g/day) was extended by lacosamide (400 mg/day). A mechanical ventilation was necessary due to the sudden and massive metabolic acidosis as well as a respiratory failure during an epileptic seizure (serum-lactat 14.7; 10.6; 16.0 mmol/l). In CSF, lactate (12.01 mmol/l (reference 1.12–2.47 mmol/l) and protein level (67 mg/dl (reference 15–45 mg/dl) were significantly increased. There were no signs for an infectious origin in CSF (polymerase chain reaction for neurotrophic germs, including Tropheryma whippelii). CT and MRI of the brain as well as abdominal- and thorax-CT were normal. The electroneurography revealed a slight mixed axonal-demyelinating polyneuropathy, the electromyography was normal. Besides a sinus-tachycardia with 140 bpm and a mild pericardial effusion, no signs of a Wolff–Parkinson–White syndrome, that would be common in mitochondriopathies, were present.
Attempted extubation failed as another severe epileptic seizure occurred with life-threatening lactic acidosis and hyperkalemia (lactate 26.0 mmol/l; pH 6.925; potassium 7.8 mmol/l (referece 3.6–5.2 mmol/l). EEG showed an alpha rhythm, with intermittent slow waves and tendency to generalize. In cerebral follow-up MRI, multiple fat embolies were detected. CT-angiography of the lung revealed a pulmonary embolism. As a reason for the fat embolies, multiple vertebral fractures were verified in CT, presumably as a result of severe epileptic seizures. A surgical fixation of vertebral fractures was performed. Intensive care therapy including ventilation was necessary for more than eight weeks. Weaning was successful after dilatative tracheostomy and nutrition via percutaneous endoscopic gastrostomy (PEG) tube. Vitamin-B6 was supplemented. Subsequently, a rehabilitative therapy was performed. After five months, the patient returned to her normal life. Tracheostomy and PEG were removed.
Taking into account all the symptoms (abdominal pain, relapsing remitting course, neurological deficits, epileptic seizures, peripheral neuropathy, lactic acidosis, cardiac disturbance), two main differential diagnosis were discussed: porphyria and a mitochondrial disease (MERRF syndrome). None of both diagnoses could be verified: Laboratory test revealed no hints of porphyria (Porphyria Specialist Center of the European Porphyria Network University Hospital Düsseldorf, Germany). A muscle biopsy gave no hint of a mitochondrial disease and revealed only a slight unspecific atrophy that was very likely due to immobility (Institute of Neuropathology of the University Hospital Essen, Germany). In terms of differential diagnosis, other metabolic diseases came into consideration. Comprehensive diagnostic for diseases of copper metabolism, lead poisoning or adrenoleukodystrophy remained inconspicuous. Finally, the analysis of the amino acids in the urine, CSF and serum showed a strong abnormality with ubiquitously increased amino acids, especially proline (proline in serum 3085 μmol/l (reference 90-342 μmol/l), in urine 46,531 μmol/g Crea (reference < 100 μmol/g Crea), in CSF 104 mg/dl (reference < 6 mg/dl), Hydroxyproline in urine 1395 μmol/g Crea (reference <100) Table 1). Furthermore, vitamin-B6 was decreased with 3.3 μg/l (reference > 4.9 μg/l). We supplemented vitamin B6 with 200 mg/d.
Table 1.
Amino acids in blood, urine and CSF
| Amino acid | blood μmol/l | reference μmol/l | urine μmol/g Crea | reference μmol/g Crea | CSF mg/dl | Reference mg/dl |
|---|---|---|---|---|---|---|
| Alanine | 685 | 205–508 | 929.0 | < 700 | 32 | 19–60 |
| Arginine | 113 | 40–140 | < 9.0 | < 150 | 18 | 11–32 |
| Asparagine | 90 | 39–79 | 59.0 | < 500 | 10 | 5–20 |
| Aspartic acid | 51 | < 35 | 352.0 | < 100 | < 3 | < 3 |
| Cysteine | 31 | < 200 | 4 | < 3 | ||
| Glutamine | 284 | 470–758 | 383.0 | < 800 | 466 | 380–1348 |
| Glutamine acid | 420 | 28–92 | 25. | < 200 | < 3 | < 4 |
| Glycine | 710 | 120–387 | 19,664.0 | < 2500 | 12 | < 35 |
| Histidine | 118 | 30–120 | 781.0 | < 1600 | 16 | 9–28 |
| Hydroxyproline | – | – | 1395 | < 100 | – | – |
| Isoleucine | 68 | 35–100 | 19.0 | < 100 | < 3 | < 17 |
| Lysine | 217 | 82–260 | 401.0 | < 250 | 21 | 13–42 |
| Methionine | 23 | 6–40 | 56.0 | < 100 | < 3 | < 10 |
| Phenylalanine | 120 | 37–115 | 160 | < 150 | 7 | 7–21 |
| Proline | 3085 | 90–342 | 46,531 | < 100 | 104 | < 6 |
| Serine | 226 | 67–193 | 12.0 | < 800 | 31 | 19–40 |
| Threonine | 152 | 75–194 | 25 | < 500 | 36 | 23–57 |
| Tryptophan | 50.0 | 34–90 | 15.0 | < 150 | < 3 | < 6 |
| Tyrosine | 86.0 | 21–107 | 386.0 | < 200 | 13 | 5–17 |
| Valine | 198 | 116–317 | 77.0 | < 120 | 9 | 11–40 |
Values were obtained in a fasted state in the morning.
Significant data are set in Bold
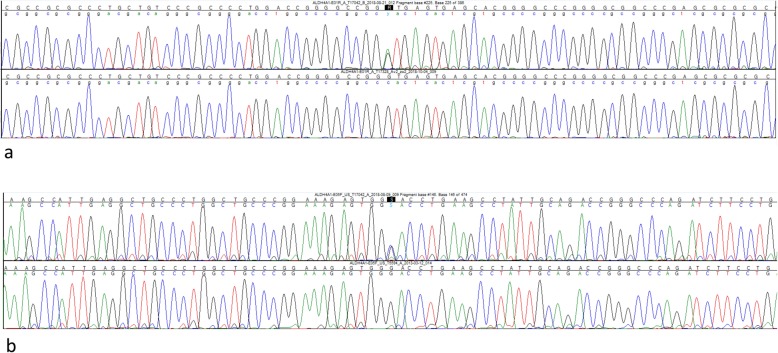
Therefore, a hyperprolinemia type I or type II was most likely. The targeted genetic analyses by Sanger sequencing revealed no pathogenic variant within the PRODH-gene (hyperprolinemia type I) but identified two novel variants within the ALDH4A1-gene (Fig. 1). In combination, both heterozygous variants within the ALDH4A1 gene could lead to a compound heterozygosity (variants in trans), that would cause the described disease phenotype. Since the patient’s son had only one of the two heterozygous variants of his mother, the compound heterozygous state of both variants in our patient was proven.
Fig. 1.
First variant (a): ALDH4A1 gene (NM_003748.3) Intron 1: c.62 + 1G > A heterozygous. This variant affects a canonical nucleotide of the splice donor site of intron 1 and is therefore thought to lead to aberrant splicing. Second variant (b): ALDH4A1 gene (NM_003748.3) Exon 5 c.349G > C, p.(Asp117His) heterozygous. This missense variant affects a highly conserved residue in the dehydrogenase domain of the protein. Furthermore, three out of four in silico predictions applied (SIFT, MutationTaster, Polyphen-2) support the role of this sequence alteration as a pathogenic variant
Discussion and conclusions
We describe a case of HPII with two novel ALDH4A1-variants in a compound heterozygous state. The first variant within the ALDH4A1 gene affects a canonical nucleotide of the splice donor site of intron 1 and is therefore thought to lead to aberrant splicing. The first variant is according to the Plon 5-step classification a class 4 variant (probably pathogenic).
The second variant within the ALDH4A1 gene is a missense variation and affects a highly conserved residue in the dehydrogenase domain of the protein. Furthermore, three out of four in silico predictions applied (SIFT, MutationTaster, Polyphen-2) support the role of this sequence alteration as a pathogenic variation. This variant is according to the Plon 5-step classification a class 3 variant (possibly pathogenic). In summary, it is highly probable that the two identified trans-ALDH4A1 variants are causally responsible for the disease.
The unique of this case is the rareness of HPII and the novel variants within the ALDH4A1 gene, with an adult and fulminant disease onset. In the late 1980s, Flynn et al. [6]. showed a cohort of 312 Irish travelers in which 14 HPII patients were reported. There were 7 healthy adult patients with HPII, the oldest with an age of 36 years.
Despite evidence of the genetic alterations, the exact pathomechanism remains unclear. Malnutrition and liver diseases can be a cause of hyperprolinaemia, however this patient did not show any signs of it.
The sudden critical deterioration of the patient’s condition seems to be the result of a massive acidosis. A lactic acidosis can lead to secondary hyperprolinemia [7]. and thus be a potential trigger for deterioration. Vice versa, the mutated P5C dehydrogenase is a mitochondrial enzyme and a lactic acidosis could be result of the gene defect [8]. Our suggestion however is, that the heterozygote patient’s gene variations lead to a latent hyperprolinaemia. Because of abdominal pain and a general deterioration of condition the patient developed an increase of lactate and an increase of proline. Proline accumulation results in oxidative stress and reduced Na++K+-ATPase activity which led to a circulus virtuoso with further lead to mitochondrial stress and resulted in increasing lactate levels.
P5C is a unique endogenous vitamin-B6 antagonist. The inactivation of vitamin-B6 by P5C may contribute to seizures in HPII [7]. In rat brain acute and chronic hyperprolinemia reduced glutamate uptake, Na+- K+-ATPase activity and ATP levels [9], which could be a reason for seizures. Long-term vitamin B6 supplementation may prevent these seizures [2]. However, in a Dutch cohort the clinical course of HPII was non-progressive and independent from the B6 concentration and B6 therapy [3]. Whether the vitamin B6 deficiency, detected in our patient was ultimately responsible for the seizures remains unclear. However, the previous case reports suggest such a pathomechanism, and the supplementation with vitamin B6 led to a seizure-free period.
According to previous publications, individuals with hyperprolinemia should be monitored intensively [3]. If acute manifestations of hyperprolinemia such as epileptic seizures are controlled, the prognosis for these disorders is quite good [7].
In conclusion, to our knowledge this is the first description of an adult patient showing two novel heterozygous variants within the ALDH41 gene in a compound heterozygous state. The late onset relapsing-remitting, potentially life-threatening course of this treatable disease emphasizes the importance of diagnostic caution and thorough laboratory work-up in cases with atypical clinical presentations. Metabolic diseases are often a chameleon and must always be considered in the differential diseases of the nervous system. Especially in therapy refractory seizures, not only in children, a hyperprolinemia causing secondary pyridoxine deficiency and seizures should be considered.
Acknowledgements
Not applicable.
Finacial disclosures
Jeremias Motte: received travel grants from Biogen idec, Novartis AG, Teva and Eisai GmbH, his research is funded by Klaus Tschira Foundation and Ruhr-University, Bochum (FoRUM-program); none related to this work.
Anna Lena Fisse: received research funding by Georgius Agricola Stiftung Ruhr, received honoraria and travel grants from Novartis AG, Sanofi and Eisai GmbH, none related to this work. Owns shares of Fresenius SE & Co., Gilead Sciences, Medtronic PLC and Novartis AG.
Thomas Grüter: received travel reimbursement from Sanofi Genzyme and Biogen Idec, none related to this manuscript.
Ruth Schneider: received consulting and speakers honoraria from Biogen Idec GmBH and Roche Pharma AG & has received research scientific grant support from Novartis Pharma.
Thomas Breuer: none.
Thomas Lücke: serves on scientific advisory boards for Novatis, Bial, MArS; has received speaker honoraria from Nutrica, Shire, Amicus, Meisinger/Straumann-Group, Sonofi-Genzyme; none related to this manuscript.
Stefan Krueger: none.
Huu Phuc Nguyen: none.
Ralf Gold: serves on scientific advisory boards for Teva Pharmaceutical Industries Ltd., Biogen Idec, Bayer Schering Pharma, and Novartis; has received speaker honoraria from Biogen Idec, Teva Pharmaceutical Industries Ltd., Bayer Schering Pharma, and Novartis; serves as editor for Therapeutic Advances in Neurological Diseases and on the editorial boards of Experimental Neurology and the Journal of Neuroimmunology; and receives research support from Teva Pharmaceutical Industries Ltd., Biogen Idec, Bayer Schering Pharma, Genzyme, Merck Serono, and Novartis, none related to this manuscript.
Ilya Ayzenberg: serves on scientific advisory boards for Roche, Alexion, received travel grants from Biogen Idec and scientific grant from Chugai Pharma.
Gisa Ellrichmann: Gisa Ellrichmann received speakers or scientific grant support from Biogen Idec, TEVA Pharma, Bayer Healthcare, Roche, Almirall and Novartis Pharma.
Abbreviations
- ALDH4A1-gene
Aldehyde dehydrogenase 4 family, member A1 - gene
- Asp
Aspartic acid
- CSF
Cerebrospinal fluid
- CT
Computer tomography
- EEG
Electroencephalography
- G > A
Guanine to Adenine
- G > C
Guanine to Cytosine
- HGMD
Human Gene Mutation Database
- His
Histidine
- HPII
Hyperprolinemia type 2
- MERRF-syndrome
Myoclonic epilepsy with ragged red fiber syndrome
- MRI
Magnetic resonance imaging
- P5C
Pyrolin-5-carboxylate
- PEG
Percutaneous endoscopic gastrostomy
- pH
Potentia Hydrogenii
- PLP
Pyridoxal phosphate
- PRODH-gene
Proline Dehydrogenase 1 – gene
- SIFT
Sorting Intolerant From Tolerant (Database)
Authors’ contributions
All authors have read and approved the manuscript. JM: Intensive care unit treatment, data collection, drafting and revising the manuscript. ALF: Data collection and revising the manuscript. TG: Data collection and revising the manuscript. RS: Data collection and revising the manuscript. TB: Data collection concerning internal medicine and revising the manuscript. TL: Critical comments during data collection, drafting and manuscript revision. SK: Geneanalyses and interpretation of genetic results, revision of the manuscript. HPN: Gene-analyses and interpretation of genetic results, revision of the manuscript. RG: Critical comments during data collection, drafting and manuscript revision. IA: Basic idea, assumption of hyperprolinemia type II and coordination of genetic tests, critical comments during data collection, drafting and manuscript revision. GE: First idea analyzing amin acids, intensive care unit treatment, initiation of tests concerning differential diagnoses, data collection, critical comments during data collection, drafting and manuscript revision. All authors read and approved the final manuscript.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
All procedures performed in studies involving humans participants were in accordance with the ethical standard of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendment or comparable ethical standards.
Consent for publication
The patients gave spoken and written consent prior to participation to the study as well as a written consent for the publication of the results.
Competing interests
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ilya Ayzenberg and Gisa Ellrichmann contributed equally to this work.
Contributor Information
Jeremias Motte, Email: Jeremias.Motte@rub.de, Email: jeremias.motte@rub.de.
Anna Lena Fisse, Email: anna.fisse@rub.de.
Thomas Grüter, Email: thomas.grueter@rub.de.
Ruth Schneider, Email: ruth.schneider@rub.de.
Thomas Breuer, Email: thomas.breuer@rub.de.
Thomas Lücke, Email: luecke.thomas@ruhr-uni-bochum.de.
Stefan Krueger, Email: st.krueger@medizinische-genetik-dresden.de.
Huu Phuc Nguyen, Email: Huu.Nguyen-r7w@ruhr-uni-bochum.de.
Ralf Gold, Email: ralf.gold@rub.de.
Ilya Ayzenberg, Email: ilya.ayzenberg@rub.de.
Gisa Ellrichmann, Email: gisa.ellrichmann@rub.de.
References
- 1.Geraghty M. Mutations in the Delta1-pyrroline 5-carboxylate dehydrogenase gene cause type II hyperprolinemia. Hum Mol Genet. 1998;7:1411–1415. doi: 10.1093/hmg/7.9.1411. [DOI] [PubMed] [Google Scholar]
- 2.Farrant R, Walker V, Mills G, Mellor J, Langley G. Pyridoxal phosphate de-activation by pyrroline-5-carboxylic acid. Increased risk of vitamin B6 deficiency and seizures in hyperprolinemia type II. J Biol Chem. 2001;276:15107–15116. doi: 10.1074/jbc.M010860200. [DOI] [PubMed] [Google Scholar]
- 3.van de Ven S, Gardeitchik T, Kouwenberg D, Kluijtmans L, Wevers R, Morava E. Long-term clinical outcome, therapy and mild mitochondrial dysfunction in hyperprolinemia. J Inherit Metab Dis. 2013;131:139–390. doi: 10.1007/s10545-013-9660-9. [DOI] [PubMed] [Google Scholar]
- 4.Millichap GJ. Seizures, pyridoxine, and Hyperprolinemia type II. Pediatr Neurol Briefs. 2000;14:27. [Google Scholar]
- 5.Plecko B. Pyridoxine and pyridoxalphosphate-dependent epilepsies. Handb Clin Neurology. 2013;113:1811–1817. doi: 10.1016/B978-0-444-59565-2.00050-2. [DOI] [PubMed] [Google Scholar]
- 6.Flynn M, Martin M, Moore P, Stafford J, Fleming G, Phang J. Type II hyperprolinaemia in a pedigree of Irish travellers (nomads) Arch Dis Child. 1989;64:1699–1707. doi: 10.1136/adc.64.12.1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mitsubuchi H, Nakamura K, Matsumoto S, Endo F. Biochemical and clinical features of hereditary hyperprolinemia. Pediatr Int. 2014;56:492–496. doi: 10.1111/ped.12420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wyse AT, Netto C. Behavioral and neurochemical effects of proline. Metab Brain Dis. 2011;26:159–172. doi: 10.1007/s11011-011-9246-x. [DOI] [PubMed] [Google Scholar]
- 9.Ferreira AG, da Cunha AA, Scherer EB, Machado FR, da Cunha MJ, Braga A, et al. Evidence that Hyperprolinemia alters Glutamatergic homeostasis in rat brain: Neuroprotector effect of Guanosine. Neurochem Res. 2001;37:205–213. doi: 10.1007/s11064-011-0604-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.