Abstract
Objective:
To describe the settings of care in which antipsychotics that nursing home (NH) residents received were likely to have been initiated.
Design:
Cross-Sectional.
Setting:
Iowa NHs.
Participants:
Fee-for-service Medicare beneficiaries who had NH stays between January 1, 2011, and December 31, 2014, and had new use of antipsychotics during their NH stays, defined as no antipsychotic use in NHs in the last 6 months.
Measurements:
A linked dataset of Chronic Condition Data Warehouse Medicare Claims and Long Term Care Minimum Data Set 3.0 (MDS 3.0) was used to determine care settings of antipsychotic initiations.
Results:
Of 7,496 residents with new antipsychotic use in NHs, 4,794 (64.0%, 95% confidence interval (CI) = 62.9–65.0%) initiated them in NHs, 1,392 (18.6%, 95% CI = 17.7–19.5%) appeared to have had them initiated in hospitals, and 1,310 (17.5%, 95% CI = 16.6–18.3%) had antipsychotics first dispensed as outpatients. Antipsychotics were commonly prescribed during the early NH stays, and 3,026 (40.4%, 95% CI = 39.3–41.5%) of the entire sample received antipsychotic therapy within the first 7 days after NH admissions. Fifty-eight percent (n = 4,348) of the study residents initiating antipsychotics had potentially appropriate antipsychotic indications according to MDS records.
Conclusions:
Most residents initiated antipsychotic therapy in NHs, confirming that NH providers are appropriate primary target of interventions to reduce antipsychotic initiation in their residents. However, many antipsychotics were continued from other settings, indicating a need to evaluate the necessity of continued antipsychotic treatment after such transitions of care.
Keywords: antipsychotics, initiation, nursing home
INTRODUCTION
Antipsychotics are commonly used off label in nursing homes (NHs) to control behavioral and psychological symptoms of dementia (BPSD).1–5 Between 2009 and 2014, more than 20% of NH residents received antipsychotics each year, despite black-box warnings from the Food and Drug Administration (FDA) highlighting an increased risk of mortality with antipsychotic use with dementia.6–9 Although the effectiveness of antipsychotics for BPSD is modest, they are sometimes perceived as needed to manage BPSD.10, 11
Given the high prevalence of antipsychotic use in NHs, Centers for Medicare and Medicaid Services (CMS) launched a national partnership in May 2012 involving providers, caregivers, and patients to improve dementia care and ensure appropriate use of antipsychotics in NHs.12 The goal of this partnership was to reduce the use of antipsychotics by 15%, 25%, and 30% in NHs nationwide by the end of 2012, 2015, and 2016, respectively.12, 13 From the end of 2011 to the end of 2013, the prevalence of antipsychotic use in NHs across the country had decreased from 23.8% to 20.2%.13 By the third quarter of 2015, the national prevalence of antipsychotic utilization in long-stay NH residents had been reduced by 27%.14
Although a number of studies have evaluated the prevalence and predictors of antipsychotic use in NHs,1, 3, 15 there is little information on the settings in which antipsychotics that NH residents receive are first prescribed. Drug initiation, which is the first step of a drug use pattern, is helpful in understanding an individual’s drug use history and opportunities to intervene. NHs are in a position to advocate for initiation and discontinuation of antipsychotics, and interventions to reduce unnecessary drug initiation should primarily target NHs if antipsychotics are typically initiated in NHs. However, if antipsychotics are more often started before NH entry, such as in hospitals or the outpatient setting, interventions in these settings could be helpful in reducing unnecessary antipsychotic use in NHs. To fill this gap, the purpose of the present study was to describe the settings of care in which antipsychotics that NH residents received were likely to have been initiated.
METHODS
Study Population and Data Source
We conducted a descriptive study to characterize initiations of antipsychotics in NH residents in Iowa. A linked dataset of Chronic Condition Data Warehouse Medicare data and Long Term Care Minimum Data Set 3.0 (MDS 3.0) was used to obtain resident information, including demographic and clinical characteristics, medication use, health insurance coverage, and healthcare facility stays. Detailed information about the data sources can be found in Table S1.
Residents who had NH stays between January 1, 2011 and December 31, 2014 were identified as potentially eligible if they used antipsychotics in a NH during this study period. NH and skilled nursing facility (SNF) residents were included in the analysis. In Iowa, only 10 of 464 facilities are purely SNFs, and most facilities are dually certified. The index date for an included resident was defined as the date of his or her first antipsychotic use in a NH within the study period.
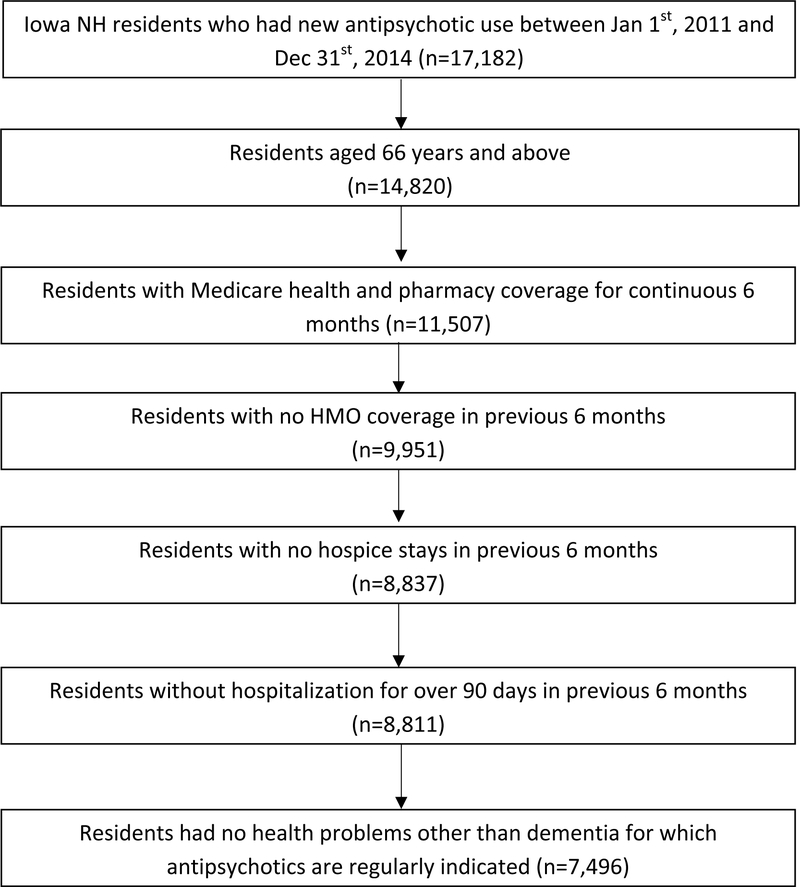
Eligible subjects were aged 66-years or older; were new antipsychotic users in NHs (no antipsychotic prescriptions during any NH stay within 6 months before their index dates); had a minimum of 6 months of continuous fee-for-service Medicare health and pharmacy insurance coverage before their index dates; had not been enrolled in or discharged from hospice within 6 months before the index dates, because the hospice benefit covers most medications used during hospice enrollment, which are not identifiable using Medicare Part D claims; were not members of any health maintenance organization (HMO) within 6 months before the index dates, because there is often inadequate information about medication use or medical encounters for individuals covered by HMO insurance; and were not hospitalized for more than 90 days in the 6 months before their index dates, because there was no information about antipsychotic use during hospitalization in these datasets. Figure S1 shows the inclusion criteria in this study.
We excluded residents if they had diagnoses of Down’s syndrome, autism, developmental disability, bipolar disorder, schizophrenia, schizoaffective disorder, schizophreniform disorder, Tourette syndrome, or Huntington’s disease at any time during the study period, based on their International Classification of Diseases, Ninth Revision diagnoses or MDS records. Diagnosis codes and MDS 3.0 variables used to define these exclusion conditions are in Table S2. Diagnoses after entry into the study sample were examined because of the limited look-back period to define some conditions for some individuals. Also these are generally not conditions with late-life onset so these diseases were assumed to have been present before the first occurrence of a diagnosis in the available data.
Measures
Antipsychotic use was identified using National Drug Codes on Medicare Part D claims and antipsychotic indicators from MDS records. First- (conventional) and second- (atypical) generation antipsychotics were included, except for prochlorperazine, which is typically used to treat other health problems (e.g. nausea and vomiting).16 Table S3 provides the full list of antipsychotics in this study. MDS assessments included an indicator about whether an antipsychotic was received in the last 7 days or since admission or reentry, although information about the specific medication received was not available. This indicator was important to define medication use during SNF stays, during which payment for medications is bundled and Part D claims should not be observed, but these assessment dates could not demonstrate the exact dates of antipsychotic initiation.
History of hospitalization, SNF stays, and history of antipsychotic prescribing in the outpatient setting were tracked for each eligible resident. Using Medicare data and MDS assessment data within 6 months before the index dates, transitions between settings of care before antipsychotic initiations were classified according to the following algorithm: If a resident received antipsychotics according to Medicare Part D claims in the 183 days before NH admission and had an index date within 7 days of NH admission, this resident was considered to have continued antipsychotic treatment given in the outpatient setting before NH admission. If a resident had not received any antipsychotic at home but had a hospitalization with a discharge date within 2 days before NH admission and had an index date within the first 7 days after NH admission, this resident was considered to have continued antipsychotic therapy from the hospital. If neither of these criteria was met, the antipsychotic was considered to have been started in a NH. The algorithm for classifying antipsychotic initiations is illustrated in Figure S2. Because this is not a validated algorithm, we conducted a sensitivity analysis to evaluate how using NH admission within 5 days instead of 2 days after discharge to classify hospital initiations affected the study results. In addition to the overall description of antipsychotic initiations attributed to each setting of care, we also compared the proportions of participants initiating antipsychotics in each setting during each year of the study period.
We also collected information about potentially appropriate BPSD indications for antipsychotic use from MDS assessments, and about dementia status from Medicare data and MDS assessments. We defined potentially appropriate BPSD indications as verbal or physical aggression, psychosis (hallucinations or delusions), and delirium. The definitions of these BPSD indications and dementia are listed in Table S4. If the first antipsychotic use in the NH was identified from MDS records, and items corresponding to these conditions and symptoms were included in the same MDS records, those values were used for analysis. Otherwise, the evaluation was based on the most recent MDS assessment before and the next MDS assessment after the index dates on which related information was available. If a symptom was present on either, it was considered present.
Statistical Analysis
Descriptive analysis was used to describe demographic and clinical characteristics of residents who had new use of antipsychotics in NHs during the study period. Proportions of residents who initiated antipsychotics in different healthcare settings were estimated. Multinomial logistic regression was used to evaluate the relationships between certain characteristics of residents and NHs with the settings of antipsychotic initiation. SAS version 9.4 (SAS Institute, Inc., Cary, NC) was used for data analysis. The University of Iowa Institutional Review Board approved this study.
RESULTS
We identified 17,182 new users of antipsychotics in NHs between January 1, 2011 and December 31, 2014, from Medicare Part D claims and MDS records. After applying exclusion criteria, 7,496 residents remained in the analytic sample. Figure 1 shows the flowchart of sample selection.
Figure 1.
Flowchart of sample selection
Of these 7,496 residents, 68.1% were female, 97.2% were white, and 53.9% were widowed. The median age was 86 (interquartile range of 80–91). Based on facility address, 62.7% of the study sample resided in rural areas; 93.6% had a diagnosis of dementia before antipsychotic initiations in NHs, and 58.0% had evidence of potentially appropriate antipsychotic indications from the MDS. Selected characteristics of study residents are summarized in Table 1. Of all the sampled residents, 40.4% were first dispensed antipsychotics within 7 days after NH admission, 11.4% between 8 and 30 days after admission, 10.4% after the first 30 days but within the first 90 days after admission, and 37.9% more than 90 days after NH admission.
Table 1.
Selected Characteristics of Study Residents
| Selected characteristics | Number of residents | Percentage (%) | |
|---|---|---|---|
| Gender | Male | 2392 | 31.9 |
| Female | 5104 | 68.1 | |
| Age (years) | 66 to 74 | 838 | 11.2 |
| 75 to 84 | 2494 | 33.3 | |
| 85 to 94 | 3485 | 46.5 | |
| 95 and above | 679 | 9.1 | |
| Race | White | 7287 | 97.2 |
| African American | 78 | 1.0 | |
| Other | 131 | 1.8 | |
| Marital status | Widowed | 4039 | 53.9 |
| Married | 2360 | 31.5 | |
| Divorced | 621 | 8.3 | |
| Never married | 360 | 4.8 | |
| Others | 116 | 1.6 | |
| Facility area | Urban | 2793 | 37.3 |
| Rural | 4703 | 62.7 | |
| Potentially appropriate indications for antipsychotic use | Verbal aggression | 2411 | 32.2 |
| Physical aggression | 1900 | 25.4 | |
| Delusion | 1850 | 24.7 | |
| Hallucination | 838 | 11.2 | |
| Delirium | 2198 | 29.3 | |
| Any indication | 4348 | 58.0 | |
| Had diagnosis of dementia before antipsychotic initiations | 7014 | 93.6 | |
Based on our algorithm, 64.0% of sampled residents initiated antipsychotics in NHs, 18.6% as outpatients, and 17.5% during hospitalizations. These proportions were relatively stable over the 4 years (Table 2). Sensitivity analysis shows that the change in time window after hospitalization had little impact on the results (Table S5). Of the 3,026 residents who had their first antipsychotics dispensed within the first 7 days after their NH admissions, 43.5% appeared to have initiated an antipsychotic in the outpatient settings and 43.3% in the hospital. Of those in NHs for at least 100 days after antipsychotic initiation, 79.4% had evidence of antipsychotic use between 61 and 100 days after initiation (Figure S3). Of those 4,794 residents who had an antipsychotic initiated in the NH, 59.1% received their first antipsychotic after at least 3 months in the NH.
Table 2.
Care settings where antipsychotics were initiated
| Year | Initiation settings | Number of residents | Percentage, 95% CI (%) | SE of percentage | Facility variations | Proportion (%) of residents who initiated antipsychoticsa | Prevalence (%) of antipsychotic use in NHsb | ||
|---|---|---|---|---|---|---|---|---|---|
| IQR 1 (%) | Median (%) | IQR 3 (%) | |||||||
| 2011 | Hospital | 339 | 15.9 (14.4, 17.5) |
0.8 | 0.0 | 0.0 | 40.0 | 11.1 (4843/43786) | 23.8 (10425/43786) |
| NH | 1377 | 64.6 (62.6, 66.7) |
1.0 | 40.0 | 66.7 | 87.5 | |||
| Outpatient | 415 | 19.5 (17.8, 21.2) |
0.9 | 0.0 | 9.6 | 30.0 | |||
| 2012 | Hospital | 324 | 17.0 (15.3, 18.7) |
0.9 | 0.0 | 0.0 | 25.0 | 10.0 (4415/43970) | 23.5 (10331/43970) |
| NH | 1236 | 64.8 (62.7, 67.0) |
1.1 | 40.0 | 66.7 | 86.6 | |||
| Outpatient | 347 | 18.2 (16.5, 19.9) |
0.9 | 0.0 | 0.0 | 28.6 | |||
| 2013 | Hospital | 332 | 18.9 (17.0, 20.7) |
0.9 | 0.0 | 0.0 | 27.9 | 9.2 (4127/44626) | 22.0 (9822/44626) |
| NH | 1130 | 64.2 (61.9, 66.4) |
1.1 | 36.4 | 66.7 | 1.0 | |||
| Outpatient | 299 | 17.0 (15.2, 18.7) |
0.9 | 0.0 | 0.0 | 25.0 | |||
| 2014 | Hospital | 315 | 18.6 (16.7, 20.4) |
0.9 | 0.0 | 0.0 | 25.0 | 8.6 (3797/44209) | 21.3 (9437/44209) |
| NH | 1051 | 61.9 (59.6, 64.3) |
1.2 | 33.3 | 64.0 | 87.9 | |||
| Outpatient | 331 | 19.5 (17.6, 21.4) |
1.0 | 0.0 | 0.0 | 33.3 | |||
| Total | Hospital | 1310 | 17.5 (16.6, 18.3) |
0.4 | 7.7 | 15.4 | 24.5 | 18.2 (17182/94172) | 23.9 (22509/94172) |
| NH | 4794 | 64.0 (62.9, 65.0) |
0.6 | 55.6 | 66.7 | 77.5 | |||
| Outpatient | 1392 | 18.8 (17.7, 19.5) |
0.6 | 7.5 | 16.1 | 25.0 | |||
IQR: interquartile range; NH: nursing home
Resident characteristics varied based on the care settings where their antipsychotics was newly dispensed (Table S6). After accounting for some potential confounders, certain demographic characteristics, health conditions, and facility features were found to be associated with antipsychotic initiations (Table 3). The odds ratios (OR) represent the odds of initiating in other care settings relative to the odds of initiating in a NH. Female residents were more likely to have received an antipsychotic in the outpatient setting but less likely to have initiation in a hospital. Residents aged 85 and older appeared to be less likely than those younger than 85 to have initiated an antipsychotic in a setting other than the NH. Similarly, married residents were less likely to first be prescribed an antipsychotic firstly outside the NH than residents with other marital status. Residents with dementia were more likely to have initiated an antipsychotic in the community but less likely in a hospital. Those who resided in rural facilities were less likely to have had an antipsychotic initiated in the hospital or in the outpatient setting. There was no difference in initiation setting according to year after adjusting for these other factors.
Table 3.
Odds of Having an Antipsychotic Initiated in the Hospital or in an Outpatient Setting Versus in a Nursing Home
| Selected characteristics | Hospital initiation | Outpatient initiation | P-value | |||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |||
| Gender | Male | (Ref) | (Ref) | <0.001 | ||
| Female | 0.83 | 0.72–0.95 | 1.19 | 1.04–1.38 | ||
| Age | 66 to 74 | (Ref) | (Ref) | <0.001 | ||
| 75 to 84 | 0.86 | 0.70–1.06 | 0.84 | 0.69–1.03 | ||
| 85 to 94 | 0.67 | 0.54–0.82 | 0.53 | 0.43–0.65 | ||
| 95 and above | 0.38 | 0.28–0.53 | 0.31 | 0.23–0.43 | ||
| Race | White | (Ref) | (Ref) | 0.403 | ||
| African American | 1.60 | 0.94–2.72 | 0.92 | 0.50–1.70 | ||
| Others | 0.96 | 0.59–1.55 | 1.10 | 0.71–1.71 | ||
| Marital status | Married | (Ref) | (Ref) | <0.001 | ||
| Widowed | 0.78 | 0.67–0.91 | 0.77 | 0.67–0.90 | ||
| Divorced | 0.75 | 0.59–0.96 | 0.74 | 0.58–0.93 | ||
| Never married | 0.60 | 0.44–0.82 | 0.57 | 0.42–0.78 | ||
| Others | 1.22 | 0.76–1.95 | 1.15 | 0.72–1.85 | ||
| Dementia | No | (Ref) | (Ref) | <0.001 | ||
| Yes | 0.68 | 0.54–0.86 | 1.28 | 0.98–1.68 | ||
| Facility area | Urban | (Ref) | (Ref) | <0.001 | ||
| Rural | 0.77 | 0.67–0.87 | 0.72 | 0.63–0.81 | ||
| Year | 2011 | (Ref) | (Ref) | 0.008 | ||
| 2012 | 1.05 | 0.89–1.25 | 0.92 | 0.78–1.08 | ||
| 2013 | 1.19 | 1.00–1.41 | 0.86 | 0.73–1.02 | ||
| 2014 | 1.19 | 1.00–1.42 | 0.99 | 0.84–1.17 | ||
NH: nursing home; Ref: reference, OR: odds ratio
DISCUSSION
This study assessed the care settings where antipsychotics were initiated for NH residents in Iowa. The study results show that a majority of residents who received antipsychotics newly started their antipsychotic treatments in NHs but that more than one-third appeared to have started antipsychotics in other settings. This confirms that NH providers should be a primary target for interventions focused on reducing antipsychotic initiation, although it also illustrates that care provided in other settings is an important contributor to antipsychotic use in NHs.
To our knowledge, this is the first study to evaluate the initial prescribing setting for antipsychotics that NH residents receive and to attempt to discern between hospital and outpatient initiation. A study in England reported that 45.3% of antipsychotic prescriptions were initiated prior to NH admission, with data collected from 1997 to 1998.17 Another study with hospitalization data in 2012 in the United States concluded that 6% of inpatients discharged to a NH received an antipsychotic initiated during hospitalization, although it was unclear whether these antipsychotics were continued in NHs.18
This study demonstrates that most residents who initiated antipsychotics in NHs first received antipsychotics after the first 3 months of their NH stay. This group of residents may not have had severe BPSD when admitted to the NH and may have been admitted for reasons other than BPSD. A previous study using data from 1998 to 2000 in Ontario, Canada found that approximately 70% of residents who newly initiated an antipsychotic in the first year of their NH stay started it in the first 100 days.19 In our study, approximately 87% of those who received an antipsychotic during the first week in NHs appeared likely to have started it in the outpatient or hospital setting, and the other 13% had no evidence suggesting that the antipsychotic was started before NH admission. The clinical context for these antipsychotic initiations occurring in the first week of the NH stay cannot be determined from these data. However, the speed with which antipsychotics were initiated in this subset of residents with no prior evidence of antipsychotic use raises questions about whether adequate attempts to manage these symptoms with nonpharmacological interventions were made and the extent to which these symptoms could be classified as persistent and in need of antipsychotic treatment.
Some demographic characteristics, including sex, age, marital status, and rural status of facilities, were associated with the settings of antipsychotic initiation. Prior work on individuals discharged from hospitals to NHs found that men were more likely to have an antipsychotic initiated in the hospital, although continuation in the NH was not evaluated.18 In our study, residents who had an antipsychotic initiated in the hospital were more likely to be male, younger, and married; live in an urban NH; and not have a dementia diagnosis than those initiating antipsychotics in the NH. Residents who had received an antipsychotic in the outpatient setting before admission were more likely to be female, younger, and married and live in an urban NH than those who initiated in a NH. These findings may relate to the characteristics of long-stay NH residents, who have more opportunities for antipsychotic initiation in the NH. A previous study indicated that long-stay residents were more likely than short-stay residents to be female, older, and widowed.20 The reason for the higher proportion of initiations attributable to NHs in rural settings is unclear but could be a factor of different proportions of long- vs. short-stay residents in rural settings.
The majority of included residents had evidence of symptoms that might justify antipsychotic use, although nearly 40% did not. We did not evaluate symptoms as predictors of the setting of care in which antipsychotics were initiated. Those who initiated antipsychotics before their NH stay may not have symptoms detected on the MDS if antipsychotics controlled the symptoms, so any differences between settings of care may have been artifacts of when the antipsychotics were initiated. The substantial minority with no symptoms detected on the MDS may be a group for whom antipsychotic dose reduction or discontinuation could be considered.21 We did not evaluate predictors of antipsychotic use duration or discontinuation in this study, so we cannot comment on whether the absence of symptoms predicted discontinuation in these residents.
Our study had three primary limitations. First, Medicare Part D data do not capture antipsychotic use in hospital or SNF settings. Since there is no information about medication use during hospitalization, we assumed that antipsychotics started shortly after a hospital discharge were started in the hospital. This may attribute some antipsychotic initiations to the hospital when they had occurred in NHs. Antipsychotic use in SNFs was captured using MDS assessment records. These records are completed fairly frequently during SNF stays but each assessment covers only the prior 7 days, so they do not capture all time periods from longer SNF stays. Thus, some antipsychotic use during SNF stays may have been missed.
Second, we had inadequate look-back periods for some residents to characterize past use of antipsychotics and past conditions, which led to exclusion of a fairly large number of residents. Ascertainment of the data 1 year at a time, with the exception of the 2013 and 2014 data, which were obtained at the same time and included residents eligible in any year through 2014, influenced this (Figure S4). The data for each year included information on anyone with a diagnosis of dementia in that year or in the past and anyone who had a NH stay in that year or since 2009. Subjects newly entering the cohort in a given year were most likely to be excluded if they initiated antipsychotics in the first half of the year because of the lack of a 6 month look-back period. For this reason, the proportion of residents who were prescribed antipsychotics shortly after NH admissions might have been underestimated, although we were able to include 2013 Medicare data for those who were first in a NH in 2014, and the findings about care settings of antipsychotic initiations in 2014 were similar to other years.
Third, this study analyzed the healthcare settings where antipsychotics were initiated for NH residents in Iowa. Although the prevalence of antipsychotic use of Iowa NH residents is near the average for the United States,14 additional research is needed to determine the extent to which the findings on antipsychotic initiations are generalizable.
In summary, the majority of antipsychotics prescribed in NHs in this study were started in the NH setting, but more than one-third appear to have been initiated in the hospital or outpatient setting. This confirms the importance of targeting NHs to reduce antipsychotic initiations. It also suggests interventions in other settings may affect antipsychotic use in NHs and illustrates the importance of evaluating the need for continued use of antipsychotics during transitions in care.
Supplementary Material
Figure S1. Inclusion criteria for study population
Figure S2. Algorithm for classifying antipsychotic initiation as having occurred in the outpatient (A), hospital (B), and nursing home (C) settings
Figure S3. Continued antipsychotic use between 61 and 100 days after index dates for residents who had antipsychotics initiated within 7 days of NH admission
Figure S4. Data ascertainment in the study
Table S1. Datasets included in the study analysis
Table S2. Diagnosis Codes and Minimum Data Set (MDS) 3.0 Variables Used to Define Medical Conditions Applied as Exclusion Criteria
Table S3. Antipsychotics included in the study analysis
Table S4. Minimum Data Set (MDS) 3.0 Variables used to define dementia and potentially appropriate BPSD indications for antipsychotic use
Table S5. Sensitivity Analysis of algorithm
Table S6. Selected characteristics of residents and facility locations by antipsychotic initiation settings
IMPACT STATEMENT:
We certify that this work is novel. This research provides new information about the settings of care in which antipsychotics received by nursing home residents were likely to have been initiated. Very little information is available on this topic. This information is useful in understanding patterns of antipsychotic utilization in nursing homes, which can inform interventions to address overuse of antipsychotics.
ACKNOWLEDGMENTS
Financial Disclosure: This work was supported through a Patient-Centered Outcomes Research Institute Program Award (1131). All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI) or its Board of Governors or Methodology Committee.
Footnotes
Publisher's Disclaimer: Disclaimer: All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology Committee.
The study was submitted to American Public Health Association (APHA) 2017 annual meeting.
Conflict of Interest: Dr. Carnahan has served as a consultant to the U.S. Department of Justice on medication use in nursing homes. Other authors have no conflicts of interest to declare.
References
- 1.Kamble P, Chen H, Sherer J et al. Antipsychotic drug use among elderly nursing home residents in the United States. Am J Geriatr Pharmacother. 2008;6: 187–197. [DOI] [PubMed] [Google Scholar]
- 2.Hersch EC, Falzgraf S. Management of the behavioral and psychological symptoms of dementia. Clin Interv Aging. 2007;2: 611–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stevenson DG, Decker SL, Dwyer LL et al. Antipsychotic and Benzodiazepine Use Among Nursing Home Residents: Findings From the 2004 National Nursing Home Survey. Am J Geriatr Psychiatry. 2010;18: 1078–1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jeste DV, Blazer D, Casey D et al. ACNP White Paper: Update on Use of Antipsychotic Drugs in Elderly Persons with Dementia. Neuropsychopharmacology. 2007;33: 957–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weiss E, Hummer M, Koller D et al. Off-Label Use of Antipsychotic Drugs. J Clin Psychopharmacol. 2000;20: 695–698. [DOI] [PubMed] [Google Scholar]
- 6.Briesacher BA, Tjia J, Field T et al. Antipsychotic use among nursing home residents. JAMA. 2013;309: 440–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Medicare & Medicaid Services (CMS) 2015. Nursing Home Data Compendium (online). Available at: https://www.cms.gov/medicare/provider-enrollment-and-certification/certificationandcomplianc/nhs.html. Accessed August 31, 2016.
- 8.U.S. Food and Drug Administration (FDA) 2005. Public Health Advisory: Deaths with Antipsychotics in Elderly Patients with Behavioral Disturbances. Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm053171.html. Accessed December 28, 2015.
- 9.U.S. Food and Drug Administration (FDA) 2008. Information for Healthcare Professionals: Conventional Antipsychotics. Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm124830.html. Accessed December 28, 2015.
- 10.Shekelle P, Maglione M, Bagley S et al. Efficacy and Comparative Effectiveness of Off-Label Use of Atypical Antipsychotics. Agency for Healthcare Research and Quality (US), 2007. Available at: https://www.effectivehealthcare.ahrq.gov/search-for-guides-reviews-and-reports/?pageaction=displayproduct&productID=63. Accessed December 28, 2015. [PubMed] [Google Scholar]
- 11.Huybrechts KF, Gerhard T, Crystal S, et al. Differential risk of death in older residents in nursing homes prescribed specific antipsychotic drugs: population based cohort study. BMJ. 2012;344: e977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Medicare & Medicaid Services (CMS) 2012. CMS annuounces partnership to improve dementia care in nursing homes. Available at: https://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-Releases/2012-Press-Releases-Items/2012-05-30.html. Accessed December 31, 2015
- 13.Centers for Medicare & Medicaid Services (CMS) 2014. National Partnership to Improve Dementia Care exceeds goal to reduce use of antipsychotic medications in nursing homes: CMS announces new goal. Available at: https://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-releases/2014-Press-releases-items/2014-09-19.html. Accessed December 31, 2015.
- 14.Tritz K, Laughman M, O’Donnell D. Update Report on the Centers for Medicare & Medicaid Services (CMS) National Partnership to Improve Dementia Care in Nursing Homes: 2014 Quarter 2 -- 2015 Quarter 3. Centers for Medicare & Medicaid Services (CMS), 2016. Available at: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/SC-Letter-16-28-Partnership-Update-Report.pdf. Accessed August 29, 2016.
- 15.Hughes CM, Lapane KL, Mor V. Influence of Facility Characteristics on Use of Antipsychotic Medications in Nursing Homes. Medical Care. 2000;38: 1164–1173. [DOI] [PubMed] [Google Scholar]
- 16.Longstreth GF. Approach to the adult with nausea and vomiting In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA: (Accessed on December 28, 2015.) [Google Scholar]
- 17.Oborne CA, Hooper R, Li KC et al. An indicator of appropriate neuroleptic prescribing in nursing homes. Age and ageing. 2002;31: 435–439. [DOI] [PubMed] [Google Scholar]
- 18.Lapane KL, Jesdale BM, Ulbricht CM et al. Correlates of In-Patient Initiation of Antipsychotics Among Elderly Patients Discharged to Nursing Homes [ISPE abstract 358]. Pharmacoepidemiol Drug Saf. 2016;25 (Suppl. 3): 209–210. [Google Scholar]
- 19.Bronskill SE, Anderson GM, Sykora K et al. Neuroleptic Drug Therapy in Older Adults Newly Admitted to Nursing Homes: Incidence, Dose, and Specialist Contact. J Am Geriatr Soc. 2004;52: 749–755. [DOI] [PubMed] [Google Scholar]
- 20.Kasper J. Who Stays and Who Goes Home: Using National Data on Nursing Home Discharges and Long-Stay Residents to Draw Implications for Nursing Home Transition Programs. Kaiser Family Foundation, 2005. Available at: http://kff.org/medicaid/report/who-stays-and-who-goes-home-using/. Accessed May 11, 2017. [Google Scholar]
- 21.Reus VI, Fochtmann LJ, Eyler AE, et al. The American Psychiatric Association practice guideline on the use of antipsychotics to treat agitation or psychosis in patients with dementia. Am J of Psychiatry. 2016. May 1;173(5):543–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Inclusion criteria for study population
Figure S2. Algorithm for classifying antipsychotic initiation as having occurred in the outpatient (A), hospital (B), and nursing home (C) settings
Figure S3. Continued antipsychotic use between 61 and 100 days after index dates for residents who had antipsychotics initiated within 7 days of NH admission
Figure S4. Data ascertainment in the study
Table S1. Datasets included in the study analysis
Table S2. Diagnosis Codes and Minimum Data Set (MDS) 3.0 Variables Used to Define Medical Conditions Applied as Exclusion Criteria
Table S3. Antipsychotics included in the study analysis
Table S4. Minimum Data Set (MDS) 3.0 Variables used to define dementia and potentially appropriate BPSD indications for antipsychotic use
Table S5. Sensitivity Analysis of algorithm
Table S6. Selected characteristics of residents and facility locations by antipsychotic initiation settings