Abstract
Alzheimer's disease is the leading cause of dementia. However, neither Alzheimer’s disease nor Alzheimer’s dementia are an inevitable consequence of aging. This review provides an overview of the issues involved in a diagnosis of Alzheimer’s disease before an individual meets the criteria for Alzheimer’s dementia. It examines how Alzheimer’s disease diagnosis rates can be improved, the implications of an early diagnosis for the individual, carer and society, and the importance of risk reduction to prevent or delay progression. Although no disease-modifying agents capable of reversing the initial pathological changes are currently available, it may be possible to prevent or delay the development of dementia in a proportion of the population by modifying exposure to common risk factors. In other individuals, diagnosing the disease or risk of disease early is still valuable so that the individual and their carers have time to make choices and plan for the future, and to allow access to treatments that can help manage symptoms. Primary healthcare professionals play a pivotal role in recognising individuals at risk, recommending lifestyle changes in mid-adult life that can prevent or slow down the disease, and in timely diagnosis. Early intervention is the optimal strategy, because the patient’s level of function is preserved for longer.
Keywords: Alzheimer’s disease, Alzheimer’s dementia, early diagnosis
Plain Language Summary
Alzheimer’s and other forms of dementia are not an inevitable consequence of aging.
In a proportion of the population it may be possible to prevent or delay the development of dementia by modifying exposure to common risk factors.
Early diagnosis and intervention to delay the onset of dementia are beneficial for patients and their carers and can result in substantial cost savings to healthcare systems.
Introduction
Dementia is a syndrome that may be caused by a number of different diseases the most prevalent of which is Alzheimer’s disease. An accurate estimate of the prevalence of Alzheimer’s dementia is difficult to determine as it is often difficult to identify the precise dementia subtype. However, it is generally accepted that Alzheimer’s is responsible for around two thirds of all dementia diagnoses.1,2
Studies that have used mathematical models to estimate future dementia prevalence, taking into account factors such as increased life expectancy, changes in mortality, and incidence of cardiovascular disease, suggest an increasing proportion of society will be affected.3 UK estimates indicate that there will be a 57% increase in the number of people with dementia in England and Wales between 2016 and 2040, with more than 1.2 million people with dementia by 2040, driven mainly by improved life expectancy.3 US forecasts indicate that the population of Americans with either Alzheimer’s dementia or mild cognitive impairment will reach 15 million in 2060, up from 6.08 million in 2017.4 On the other hand, recent data suggest that incidence rates of dementia may be declining in some countries including the UK.5,6 A two-decade comparison of individuals aged 65 years and older from three geographical areas of England has found evidence for a reduction in the age-specific incidence of dementia.5 These data are encouraging because they show that Alzheimer’s and other forms of dementia are not an inevitable consequence of aging and suggest that in a proportion of the population it may be possible to prevent or delay the development of dementia by modifying exposure to certain risk factors such as hypertension, smoking, obesity, and diabetes.5,7,8
With the realisation that urgent action must be taken to reduce the burden of Alzheimer’s disease, a condition with escalating costs and very limited treatment options, there has been a shift in focus to identify individuals much earlier in the disease process. Not all individuals with mild cognitive impairment will develop dementia and despite there being no current treatment to prevent or cure the disease, there is an urgent need to improve diagnosis rates so that those at greatest risk can be identified early and measures implemented to reduce or prevent further progression.
This review is targeted to primary healthcare professionals, as well as those working in more specialised areas of dementia care including psychiatrists and memory clinics. It has been conducted to provide an overview of the personal, economic and research benefits of diagnosing Alzheimer’s disease early before an individual meets the criteria for Alzheimer’s dementia. It includes evidence on the wider benefits to the health and social care system of an early diagnosis, as well as the personal and social benefits to people with Alzheimer’s disease, their carers and families. It also sets out the personal perspectives of people with Alzheimer’s dementia, providing a voice for those who have first-hand experience of what a diagnosis means. The scope of the review has been limited to the Alzheimer’s dementia subtype. Early onset familial Alzheimer’s disease, dementia associated with Down’s syndrome and learning disabilities have also been excluded.
Search Strategy and Selection Criteria
References for this review were identified by searches of PubMed and Google Scholar between 1969 and December 2018; references from relevant articles were also included. The following search terms were used: “pre-dementia Alzheimer’s disease”; “evidence for benefits of early diagnosis of Alzheimer’s disease”; “dementia early diagnosis”; “dementia early diagnosis financial”; “benefits of early diagnosis of Alzheimer’s disease cost effectiveness”; “benefits of early diagnosis of Alzheimer’s disease”; and “early diagnosis of Alzheimer’s disease”. Papers were restricted to those in English language journals. The final reference list was generated on the basis of relevance to the topics covered in this review.
Improving Alzheimer’s Disease Diagnosis Rates
The progression of Alzheimer’s disease can be broken down into three general stages: preclinical, mild cognitive impairment, and dementia, but can be more accurately described according to a 7-Stage model (Table 1).9 The progression of the disease may be different for each individual, but most people live between 4 and 8 years following diagnosis.
Table 1.
The 7-Stage Model of Alzheimer’s Dementia.
| Stage | Level of Impairment |
|---|---|
| 1 | No impairment |
| 2 | Very mild cognitive decline |
| 3 | Mild cognitive decline |
| 4 | Moderate cognitive decline (early-stage dementia) |
| 5 | Moderately severe cognitive decline (early mid-stage dementia) |
| 6 | Severe cognitive decline (late mid-stage dementia) |
| 7 | Very severe cognitive decline (late-stage dementia) |
Note: Data from Reisberg et al.9
Preclinical Alzheimer’s disease describes a person who has no cognitive symptoms, but has signs of pathology on brain imaging or blood/cerebrospinal fluid (CSF) biomarkers.10 It is generally accepted that biomarker abnormalities such as low CSF β-amyloid 42 (Aβ42) and cerebral amyloid deposits precede elevated CSF tau cerebral injury.11 Preclinical diagnosis would require population or targeted screening and is currently only recommended for research purposes.12
For this review, an early Alzheimer’s disease diagnosis is one made at a stage when an individual comes to the attention of their physician because of mild cognitive impairment (Stage 2 or 3 of the 7-stage model), but who is still functionally independent and free of dementia. This phase of Alzheimer’s disease can be detected well before the onset of dementia symptoms, up to 8 years in some cases13 with currently available tools.14,15
While there is currently debate amongst specialists as to whether mild cognitive impairment is truly a diagnosis,16 what is acknowledged is that people with mild cognitive impairment have a risk state that could in the future develop into dementia. It is estimated to increase the risk of developing dementia caused by Alzheimer’s disease or other neurological conditions in around 30% of individuals; a further 30% will remain with mild cognitive impairment, and 30% with symptoms of mild cognitive impairment will improve.17 Patients should be advised that the issue they have is not entirely normal and needs to be reviewed to determine if it remains the same or changes either for the better or the worse. If the latter, then this will require further assessment and review.
A number of medical conditions and lifestyle factors have been linked to an increased risk of mild cognitive impairment as well as Alzheimer’s dementia including: increasing age, diabetes, smoking, high blood pressure, elevated cholesterol, obesity, depression, lack of physical exercise, a low education level, infrequent participation in mentally or socially stimulating activities, and the presence of the APO-E4 gene variant.8,18 There is a greater likelihood of progression in those with more than one of these risk factors.
The existence of potentially modifiable risk factors means that prevention of cognitive impairment and dementia may be possible through a public health approach.8 Individuals with the above risk factors are often seen in primary care, providing an opportunity for healthcare providers to inquire about health concerns including memory problems.8 When performed as part of a routine healthcare visit, there is ample opportunity to identify patients with potential mild cognitive impairment in a cost-effective manner without raising undue anxiety and without the stigma associated with attending a specialised clinic.8
In the UK, the Department of Health has stated that two thirds of the estimated number of people with dementia in England should have a diagnosis with appropriate post-diagnostic support.19 While the mean dementia diagnosis rate in the UK was 66% in 2017/18, this rate varies widely from 54% to 80%.20 Part of this variation is due to communication issues between different healthcare specialists. There is also ongoing debate about how the prevalence is calculated, especially as there is often a lack of correction for local variations in risk factors, e,g. cardiovascular disease. Dementia is a clinical diagnosis that should consider all available information, but psychiatrists may often not have direct access to patient scans, and radiologists, rather than neuroradiologists, may be reviewing brain scans without access to a patient’s relevant clinical history. These issues may also contribute to variation in diagnosis rates, incorrect diagnoses as well as missed diagnoses.
With increasing efforts to improve diagnosis there must also be improved post-diagnostic support. To meet this need, an implementation plan known as the `Well Pathway for Dementia` has been developed which covers all aspects of dementia care from the moment a person consults their physician with concerns about symptoms such as the loss of short-term memory, to a diagnosis of dementia, through to the end of their life.21 As part of the plan, targeted screening to identify high-risk patients may be helpful.18,22
Issues Associated with Early Diagnosis of Alzheimer’s Disease for the Individual, Carer and Society
Impact on the Individual
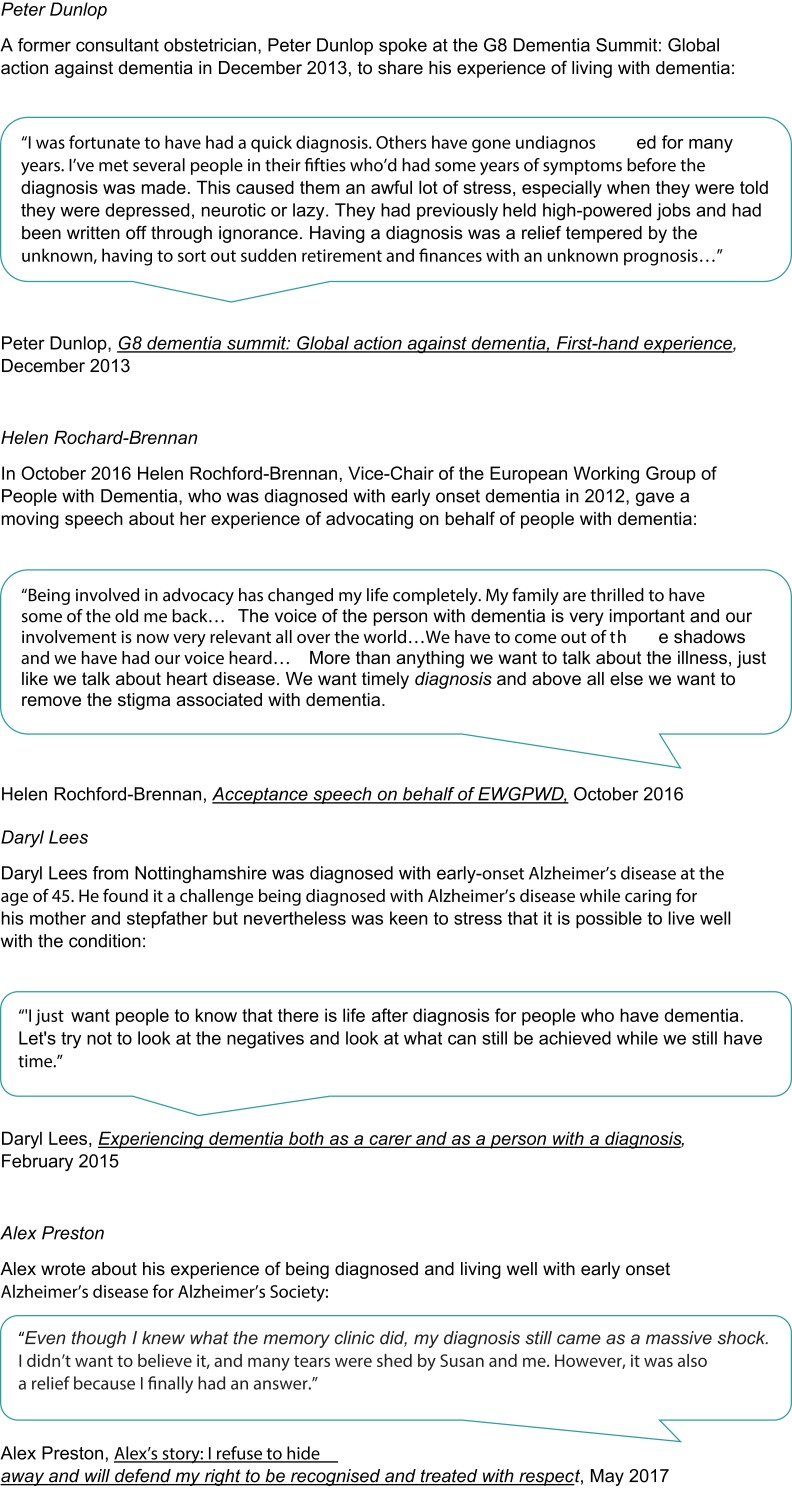
Alzheimer’s disease is one of the most feared diseases of old age.23 A diagnosis is often experienced with shock and feelings of disbelief, anger, fear, hopelessness, despair and grief. Some quotes from people describing their feelings on their original Alzheimer’s disease and Alzheimer’s dementia diagnosis are presented in Figure 1. Fear of the stigma surrounding Alzheimer’s disease, mainly as a result of misconceptions about the disease, may prevent people from: seeking medical treatment, receiving an early diagnosis or any diagnosis, living the best quality of life possible while they are able, making plans for their future, and benefiting from available treatments and support systems. In addition, patients may find the repeated assessments humiliating. From an ethical perspective, an early diagnosis could affect issues linked to privacy and confidentiality for example in relation to employment, the right to hold a driver’s licence, insurance premiums and financial management.24 It is therefore essential that individuals are not penalised by receiving an early diagnosis.
Figure 1.
Patient perspectives on diagnosis.
The positive benefits of receiving an early Alzheimer’s disease diagnosis to the patient are that it provides an explanation for the symptoms and signs they are experiencing and puts an end to their suspicions. An early diagnosis and subsequent access to the right services and support can help people take control of their condition, live independently in their own home for longer, and maintain a good quality of life for themselves, their family and carers.25 A good quality of life in the early phases of the illness can be maintained for several years. Forewarned, people can plan ahead while they still have the capacity and thus participate in their own legal, financial, and future support/care options and treatment and make their wishes known to family members.
It is only through receiving a diagnosis that patients can obtain access to available treatments that may improve their cognition and enhance their quality of life.26 Analysis of a US claims database identified 8995 newly-diagnosed Alzheimer’s disease patients aged 65–100 years and assigned them to treated and untreated cohorts.27 After controlling for comorbidities, the treated cohort had better survival and a 20% lower rate of institutionalisation.
A variety of studies suggest that most people would support targeted screening of those at risk of dementia and disclosure of dementia.28–32 In a Canadian study of community-living, older individuals without cognitive impairment, virtually all (98%) stated they would want to be informed of a diagnosis whether or not medication was available to treat it.29 A questionnaire survey conducted among 2678 randomly selected adults across the US and four European countries, which asked whether subjects would undergo a hypothetical early medical test for Alzheimer’s disease, found that potential demand was high with 67% reporting they would want to know if they were going to develop the disease.31
Impact on Carers
Most patients with Alzheimer’s dementia are cared for by a spouse or other family member. Given the long duration of Alzheimer’s disease, the strain on carers can be lengthy. A report from the Alzheimer’s Association indicates that in 2017, 16 million Americans provided an estimated 18.4 billion hours of unpaid care in the form of physical, emotional and financial support – a contribution to the nation valued at $232.1 billion.33
Early diagnosis allows carers time to adjust to the changes in function, mood and personality that can occur with Alzheimer’s dementia and their transition to a care giver role. It has been shown that carers who are better able to adapt, feel more competent to care, and experience less psychological problems such as anxiety and depression.34,35 Several enhanced support services for carers have demonstrated efficacy in delaying institutionalisation of the patient with dementia, including day care support programmes36 and memory clinics.37 In a cohort study of 970 patients with dementia (including 663 with Alzheimer’s dementia) attending a memory clinic in France, survival analysis showed that a shorter time between first symptoms and first visit was associated with longer survival regardless of diagnosis.38
Impact on Society
The high economic burden of Alzheimer’s dementia is spread across three main sectors: healthcare, social care and informal care, with the majority of costs falling on informal carers. In the UK, healthcare costs relate mainly to the NHS and are due to hospitalisation of people living with Alzheimer’s dementia. Social care costs relate to services such as nursing homes, homecare, and respite care. Informal care costs relate to family providing unpaid care for people living with Alzheimer’s dementia. Whilst a person with dementia is in the community, a great deal of the cost burden of care is informal, i.e. borne by family and carers. The total costs calculated for dementia, of which two thirds of cases are Alzheimer’s dementia are estimated to be over £26bn in the UK, with informal care accounting for £11.6bn (44.2%), social care £10.3bn (39.0%) and healthcare £4.3bn (16.4%).39
Although early diagnosis and intervention are likely to incur greater up-front costs,27,40 economic modelling suggests that these may be offset by subsequent savings, achieved primarily from a reduction in care needs and institutionalisation.41–45
Alzheimer’s Research UK and the Office of Health Economics have developed an economic model to examine the impact of delaying the onset of dementia.46 In the model, the intervention delays the onset by between 2 and 5 years and would become available in 2020. The results shows that if the onset of Alzheimer’s dementia was delayed by 2 years from 2020 then there would be 184,000 fewer people with dementia and 156,000 fewer family carers by 2030, with a related highly significant decrease in the costs of care. If the onset could be delayed by 5 years then there would be 469,000 (36%) fewer people with Alzheimer’s dementia and 399,000 (36%) fewer carers by 2030.46 Although this model assumes a disease-modifying treatment, any approach that delays the onset of dementia in a person diagnosed with Alzheimer’s disease would be beneficial.
Risk Reduction and Dementia Prevention
Recognition and management of risk for Alzheimer’s disease earlier in adult life is important to have the greatest impact.18 At this stage, lifestyle changes can be made that will slow or prevent the development of future disease.47 Vascular disease and dementia syndromes have many shared risk factors including hypertension, type 2 diabetes, smoking and poor diet and exercise habits. This has led the WHO to recommend combined implementation of their recent guidelines on risk reduction of cognitive decline and dementia with interventions related to the management of risk factors for cardiovascular disease and diabetes.8 While general screening is not recommended, individuals with these risk factors can be advised to improve lifestyle choices and control their modifiable risk factors to minimise their risk for future dementia as well as other chronic conditions. In addition, brain health should be protected throughout life by avoiding alcohol and substance abuse, supporting lifelong learning, and social interaction and stimulation in later life.
Primary care workers and other healthcare professionals in contact with people with a diagnosis of mild cognitive impairment or other established risk of dementia should routinely ask questions as part of their normal patient review to identify symptoms of Alzheimer’s dementia. Primary care providers are ideally positioned to monitor patients at risk of Alzheimer’s dementia as they have access to an individual’s medical and family history. However, recognition is not just the responsibility of general practitioners, but also other professionals who have regular contact with patients and may notice changes in cognitive functioning including community pharmacists, practice nurses, district nurses, social care, and nursing home staff.
Discussion
Summary
Alzheimer’s dementia places an immense burden on people with the condition, their families and carers, but also the health and social care system and society in general. With global increases in longevity, the prevalence of Alzheimer’s disease is escalating, and there is an urgent need for approaches to prevent or delay the onset of disease and subsequent dementia.
Although no disease-modifying agents capable of reversing the initial pathological changes associated with the disease have yet reached the market, a diagnosis early in the course of illness, allows time for all concerned to adjust whilst the patient can still actively engage, and offers access to advice, financial support and non-pharmacological and pharmacological treatments. Many patients with mild-to-moderate Alzheimer’s dementia can live with the disease for a number of years with a good quality of life with access to the optimal treatments and resources.
Strengths and Limitations
This review summarizes findings from multiple studies surrounding the research question “Why we need early diagnosis,” to provide the reader with information on the benefits to the patient, carer and society. Limitations are mostly related to the lack of randomized controlled trials with most data based on case reports and small case series. In addition, many of the advantages and disadvantages are subjective in nature and therefore subject to reporting bias.
Comparison with Existing Literature
While several reviews have considered the benefits and challenges of an early diagnosis of Alzheimer’s disease,45,48,49 a greater focus of the current review is placed on how early diagnosis can be used to identify those at risk for or with mild cognitive impairment to prevent or delay the onset of Alzheimer’s disease and subsequent dementia.
Implications for Research and/or Practice
Primary healthcare professionals will play a pivotal role in recognising individuals at risk, recommending lifestyle changes in mid-adult life that can prevent or slow down the disease, and in timely diagnosis by evaluating older patients for early cognitive signs and in initiating treatment that can significantly delay its progression. Early intervention is the optimal strategy, because the patient’s level of function is preserved for longer.
Ongoing research is examining how personalized therapeutic interventions, based on individual risk factors, can be achieved through clinical precision medicine.18 The precision medicine approach takes into account individual variability in genes, environment, and lifestyle. Individuals with Alzheimer’s disease are a heterogeneous group, but by breaking the population down into different genetic and biological subsets, precision medicine allows treatment algorithms to be developed that specify optimal treatments for an individual’s specific biological make-up.48 As part of this initiative, studies such as PREVENT49 and the European Prevention of Alzheimer’s Dementia (EPAD) Longitudinal Cohort Study50 are helping to provide information on the risks for developing dementia across a wide group of people. This strategy will form an essential component of the person-centred care approach advocated by the 2018 NICE guidelines for dementia care,15 and will require a multidimensional approach that combines collaboration between primary and secondary care, advances in research, and improved support for people with the disease and their carers.
Acknowledgments
The authors were supported by an independent medical writer, Jenny Grice, who was fully funded by MSD. The authors, including an author from MSD, had complete editorial control over the manuscript, which represents the views of the authors.
Author Contributions
JR and HL coordinated the overall process of manuscript production. JG performed literature searches, and JR and HL selected relevant papers. JR, HL and JG wrote the manuscript. JR and HL were involved in critically reading and editing the manuscript. All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Dr Rasmussen is the Clinical Representative for Dementia for the Royal College of General Practitioners; she is Director of her individual consultancy “Psi-napse”. In her consultancy role, she is a past Non-Executive Director for Cerestim and has received payment for consultancy/advisory boards/Speaker Bureaus from a number of Pharmaceutical Companies. She reports non-financial support from RCGP, personal fees from Psi-napse, personal fees from Cerestim, personal fees from NHS England – South East (Kent, Surrey, Sussex), personal fees from AHSN - Kent Surrey Sussex, non-financial support from Surrey Heartlands STP, outside the submitted work. Haya Langerman is an employee of MSD UK and reports personal fees from MSD Ltd, outside the submitted work.
References
- 1.Burns A, Iliffe S. Alzheimer’s disease. BMJ. 2009;338:b158. doi: 10.1136/bmj.b158 [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Dementia: Fact sheet, 2017. Available from: https://www.who.int/news-room/fact-sheets/detail/dementia. Accessed January4, 2018.
- 3.Ahmadi-Abhari S, Guzman-Castillo M, Bandosz P, et al. Temporal trend in dementia incidence since 2002 and projections for prevalence in England and Wales to 2040: modelling study. BMJ. 2017;358:j2856. doi: 10.1136/bmj.j2856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brookmeyer R, Abdalla N, Kawas CH, Corrada MM. Forecasting the prevalence of preclinical and clinical Alzheimer’s disease in the United States. Alzheimers Dement. 2018;14(2):121–129. doi: 10.1016/j.jalz.2017.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matthews FE, Stephan BC, Robinson L, et al. Cognitive Function and Ageing Studies (CFAS) collaboration. A two decade dementia incidence comparison from the Cognitive Function and Ageing Studies I and II. Nat Commun. 2016;7:11398. doi: 10.1038/ncomms11398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sullivan KJ, Dodge HH, Hughes TF, et al. Declining incident dementia rates across four population-based birth cohorts. J Gerontol A Biol Sci Med Sci. 2018. doi: 10.1093/gerona/gly236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Norton S, Matthews FE, Barnes DE, Yaffe K, Brayne C. Potential for primary prevention of Alzheimer’s disease: an analysis of population-based data. Lancet Neurol. 2014;13(8):788–794. doi: 10.1016/S1474-4422(14)70136-X [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. Risk Reduction of Cognitive Decline and Dementia. WHO Guidelines. World Health Organization; 2019. [PubMed] [Google Scholar]
- 9.Reisberg B, Ferris SH, de Leon MJ, Crook T. The global deterioration scale for assessment of primary degenerative dementia. Am J Psychiatr. 1982;139:1136–1139. [DOI] [PubMed] [Google Scholar]
- 10.Sperling RA, Aisen PS, Beckett LA, et al. Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):280–292. doi: 10.1016/j.jalz.2011.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bateman RJ, Aisen PS, De Strooper B, et al. Autosomal-dominant Alzheimer’s disease: a review and proposal for the prevention of Alzheimer’s disease. Alzheimers Res Ther. 2011;3(1):1. doi: 10.1186/alzrt59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jack CR, Bennett DA, Blennow K, et al. NIA-AA Research Framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018;14(4):535–562. doi: 10.1016/j.jalz.2018.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saxton J, Lopez OL, Ratcliff G, et al. Preclinical Alzheimer disease. Neuropsychological test performance 1.5 to 8 years prior to onset. Neurology. 2004;63:2341–2347. doi: 10.1212/01.WNL.0000147470.58328.50 [DOI] [PubMed] [Google Scholar]
- 14.Ballard C, Burns A, Corbett A, Livingston G, Rasmussen J. Helping You to Assess Cognition: A Practical Toolkit for Clinicians. London: Alzheimer’s Society; 2013. [Google Scholar]
- 15.NICE guideline [NG97]. Dementia: assessment, management and support for people living with dementia and their carers. June 2018. Available from: https://www.nice.org.uk/guidance/ng97/chapter/Recommendations. Accessed December11, 2019. [PubMed]
- 16.Zanetti O, Geroldi C, Frisoni GB. Mild cognitive impairment (MCI) is not a clinical entity. BMJ. 2009;338:b75. doi: 10.1136/bmj.b902 [DOI] [PubMed] [Google Scholar]
- 17.Mitchell AJ, Shiri-Feshki M. Rate of progression of mild cognitive impairment to dementia – meta-analysis of 41 robust inception cohort studies. Acta Psychiatr Scand. 2009;119:252–265. doi: 10.1111/acp.2009.119.issue-4 [DOI] [PubMed] [Google Scholar]
- 18.Isaacson RS, Ganzer CA, Hristov H, et al. The clinical practice of risk reduction for Alzheimer’s disease: a precision medicine approach. Alzheimers Dement. 2018;14(12):1663–1673. doi: 10.1016/j.jalz.2018.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Department of Health, UK. Dementia: a state of the nation report on dementia care and support in England. Department of Health, UK. 2013. November.
- 20.Alzheimers Research UK. Diagnoses in the UK. Available from: https://www.dementiastatistics.org/statistics/diagnoses-in-the-uk. Accessed December11, 2019.
- 21.NHS England. The Well Pathway for Dementia. Available from: https://www.england.nhs.uk/mentalhealth/wp-content/uploads/sites/29/2016/03/dementia-well-pathway.pdf. Accessed December11, 2019.
- 22.Barnes DE, Beiser AS, Lee A, et al. Development and validation of a brief dementia screening indicator for primary care. Alzheimers Dement. 2014;10(6):656–665.e1. doi: 10.1016/j.jalz.2013.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cantegreil-Kallen I, Pin S. Fear of Alzheimer’s disease in the French population: impact of age and proximity to the disease. Int Psychogeriatr. 2012;24(1):108–116. doi: 10.1017/S1041610211001529 [DOI] [PubMed] [Google Scholar]
- 24.Karlawish J. Addressing the ethical, policy, and social challenges of preclinical Alzheimer disease. Neurology. 2011;77(15):1487–1493. doi: 10.1212/WNL.0b013e318232ac1a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Social Care Institute for Excellence, Why early diagnosis of dementia is important; 2015. (UK study).
- 26.Prince M, Bryce R, Ferri C Alzheimer’s Disease International World Alzheimer report 2011. The benefits of early diagnosis and intervention. Available from: https://www.alz.co.uk/research/WorldAlzheimerReport2011.pdf. Accessed May28, 2018..
- 27.Black CM, Fillit H, Xie L, et al. Economic burden, mortality, and institutionalization in patients newly diagnosed with Alzheimer’s disease. J Alzheimers Dis. 2018;61(1):185–193. doi: 10.3233/JAD-170518 [DOI] [PubMed] [Google Scholar]
- 28.Turnbull Q, Wolf AM, Holroyd S. Attitudes of elderly subjects toward “truth telling” for the diagnosis of Alzheimer’s disease. J Geriatr Psychiatry Neurol. 2003;16(2):90–93. doi: 10.1177/0891988703016002005 [DOI] [PubMed] [Google Scholar]
- 29.Ouimet MA, Dendukuri N, Dion D, Beizile E, Elie M. Disclosure of Alzheimer’s disease. Senior citizens’ opinions. Can Fam Physician. 2004;50:1671–1677. [PMC free article] [PubMed] [Google Scholar]
- 30.Robinson SM, Canavan M, O’Keeffe ST. Preferences of older people for early diagnosis and disclosure of Alzheimer’s disease (AD) before and after considering potential risks and benefits. Arch Gerontol Geriatr. 2014;59(3):607–612. doi: 10.1016/j.archger.2014.07.010 [DOI] [PubMed] [Google Scholar]
- 31.Wikler EM, Blendon RJ, Benson JM. Would you want to know? Public attitudes on early diagnostic testing for Alzheimer’s disease. Alzheimers Res Ther. 2013;5(5):43. doi: 10.1186/alzrt206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sheffrin M, Stijacic Cenzer I, Steinman MA. Desire for predictive testing for Alzheimer’s disease and impact on advance care planning: a cross-sectional study. Alzheimers Res Ther. 2016;8(1):55. doi: 10.1186/s13195-016-0223-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alzheimer’s Association. 2018 Alzheimer’s disease facts and figures. Alzheimers Dement. 2018;14(3):367–429. doi: 10.1016/j.jalz.2018.02.001 [DOI] [PubMed] [Google Scholar]
- 34.de Vugt ME, Verhey FR. The impact of early dementia diagnosis and intervention on informal caregivers. Prog Neurobiol. 2013;110:54–62. doi: 10.1016/j.pneurobio.2013.04.005 [DOI] [PubMed] [Google Scholar]
- 35.Mittelman MS, Ferris SH, Shulman E, Steinberg G, Levin B. A family intervention to delay nursing home placement of patients with Alzheimer disease. A randomized controlled trial. JAMA. 1996;276(21):1725–1731. doi: 10.1001/jama.1996.03540210033030 [DOI] [PubMed] [Google Scholar]
- 36.Wimo A, Mattsson B, Adolfsson R, Eriksson T, Nelvig A. Dementia day care and its effects on symptoms and institutionalization–a controlled Swedish study. Scand J Prim Health Care. 1993;11(2):117–123. doi: 10.3109/02813439308994913 [DOI] [PubMed] [Google Scholar]
- 37.Littlewood C, Seymour J, Owen V. Does treating Alzheimer’s disease early, delay institutionalisation? Int J Geriatr Psychiatry. 2010;25(12):1307–1309. doi: 10.1002/gps.2446 [DOI] [PubMed] [Google Scholar]
- 38.Bruandet A, Richard F, Bombois S, et al. Alzheimer disease with cerebrovascular disease and vascular dementia: clinical features and course compared with Alzheimer disease. J Neurol Neurosurg Psychiatry. 2009;80:133–139. doi: 10.1136/jnnp.2007.137851 [DOI] [PubMed] [Google Scholar]
- 39.Prince M, Knapp M, Guerchet M, et al. King’s College London and the London School of Economics. Update’, second Dementia UK: Alzheimer’s Society 2014; Available fromhttps://www.alzheimers.org.uk/download/downloads/id/2323/dementia_uk_update.pdf.Accessed May, 252018. [Google Scholar]
- 40.Versijpt J. Effectiveness and cost-effectiveness of the pharmacological treatment of Alzheimer’s disease and vascular dementia. J Alzheimers Dis. 2014;42(Suppl 3):S19–25. doi: 10.3233/JAD-132639 [DOI] [PubMed] [Google Scholar]
- 41.Foldes SS, Moriarty JP, Farseth PH, Mittelman MS, Long KH. Medicaid savings from the New York University caregiver intervention for families with dementia. Gerontologist. 2018;58(2):e97–e106. doi: 10.1093/geront/gnx077 [DOI] [PubMed] [Google Scholar]
- 42.Banerjee S, Wittenberg R. Clinical and cost effectiveness of services for early diagnosis and intervention in dementia. Int J Geriatr Psychiatry. 2009;24:748–754. doi: 10.1002/gps.2191 [DOI] [PubMed] [Google Scholar]
- 43.Weimer DL, Sager MA. Early identification and treatment of Alzheimer’s disease: social and fiscal outcomes. Alzheimers Dement. 2009;5:215–226. doi: 10.1016/j.jalz.2009.01.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Getsios D, Blume S, Ishak KJ, Maclaine G, Hernandez L. An economic evaluation of early assessment for Alzheimer’s disease in the United Kingdom. Alzheimers Dement. 2012;8:22–30. doi: 10.1016/j.jalz.2010.07.001 [DOI] [PubMed] [Google Scholar]
- 45.Dubois B, Padovani A, Scheltens P, Rossi A, Dell’Agnello G. Timely diagnosis for Alzheimer’s disease: a literature review on benefits and challenges. J Alzheimers Dis. 2016;49(3):617–631. doi: 10.3233/JAD-150692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lewis F, Schaffer SK, Sussex J, O’Neill P, Cockcroft L. The Trajectory of Dementia in the UK - Making a Difference. London: Consulting Report, Office of Health Economics; 2014. [Google Scholar]
- 47.Barnes DE, Yaffe K. The projected effect of risk factor reduction on Alzheimer’s disease prevalence. Lancet Neurol. 2011;10(9):819–828. doi: 10.1016/S1474-4422(11)70072-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hampel H, Toschi N, Babiloni C, et al. Revolution of Alzheimer precision neurology: passageway of systems biology and neurophysiology. J Alzheimers Dis. 2018;64(Suppl 1):S47–S105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ritchie CW, Ritchie K. The PREVENT study: a prospective cohort study to identify mid-life biomarkers of late-onset Alzheimer’s disease. BMJ Open. 2012;2:e001893. doi: 10.1136/bmjopen-2012-001893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ritchie CW, Molinuevo JL, Truyen L, Satlin A, Van der Geyten S, Lovestone S, European Prevention of Alzheimer’s Dementia (EPAD) Consortium. Development of interventions for the secondary prevention of Alzheimer’s dementia: the European Prevention of Alzheimer’s Dementia (EPAD) project. Lancet Psychiatry. 2016;3(2):179–186. doi: 10.1016/S2215-0366(15)00454-X [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- World Health Organization. Dementia: Fact sheet, 2017. Available from: https://www.who.int/news-room/fact-sheets/detail/dementia. Accessed January4, 2018.