Abstract
Multifocal fibromatosis is a rare entity. We report on two cases where multifocal disease developed after surgical resection. Chronic inflammation and repetitive trauma may be considered a risk factor for developing multifocal disease.
Keywords: desmoid, extra‐abdominal, fibromatosis, multifocal, surgery
Multifocal fibromatosis is a rare entity. We report on two cases where multifocal disease developed after surgical resection. Chronic inflammation and repetitive trauma may be considered a risk factor for developing multifocal disease.
![]()
1. INTRODUCTION
Multifocal extra‐abdominal desmoid fibromatosis is a rare entity. Both sporadic and hereditary entities have been described. We report on two cases where multifocal disease developed after surgical resection due to lymphedema and irritation from a prosthesis. Chronic inflammation and repetitive trauma may be a risk factor for developing multifocal disease.
Extra‐abdominal desmoid fibromatosis, also known as desmoid tumor or fibromatosis, is a benign and locally aggressive fibroblastic tumor with an unpredictable natural history.1 It is a rare clinical entity with approximately 900 new cases diagnosed each year in the United States, or 3‐4 cases per million people. It usually presents between the ages of 15 and 60 years, is more common in young adulthood, and has a twofold to threefold female predominance.2 The majority of extra‐abdominal cases are sporadic and can occur anywhere in the body, with the most common sites being the shoulder, chest wall, back, and thigh.1 Intra‐abdominal desmoid tumors tend to be associated with a diagnosis of Familial adenomatous polyposis (FAP), whereas abdominal wall desmoid tumors are often associated with scar tissue. In approximately 10% of cases, the disease is multifocal.3 Most patients will present with a painless enlarging mass, but the clinical presentation can vary depending on the size and location of the tumor.
Desmoid fibromatosis has been broadly categorized into two groups, with approximately 90% being sporadic and the remaining 10% being hereditary.4 The most common mutation in sporadic cases involves an activating mutation in CTNNB1, the gene encoding β‐catenin. The APC tumor suppressor gene has been implicated in hereditary cases as a result of Gardner syndrome, which is a form of FAP, as well as the remainder of sporadic cases. In both groups, abnormal regulation of the WNT signaling pathway results in accumulation of β‐catenin in affected cells and is thought to play a role in driving development of desmoid fibromatosis.[5]
Multiple risk factors for development of desmoid fibromatosis have been suggested including FAP, prior surgery or scars, trauma, and increased estrogen levels. Antecedent trauma has been noted in up to 30% of patients with desmoid tumors, most commonly from surgical intervention in patients with FAP.6, 7 However, a similar relationship in sporadically occurring desmoid tumors has been noted. In one series, 28% of sporadic desmoid tumors had a history of antecedent trauma.8 Although incompletely understood, there is evidence that dysregulation of wound healing is involved in the pathogenesis of desmoid tumors.9 We report on two cases of solitary, sporadic fibromatosis that developed multifocal disease after surgery and suggest that chronic inflammation and repetitive trauma may be considered a risk factor for developing multifocal disease.
2. CASE REPORTS
The first patient is a 21‐year‐old woman who presented to a local Emergency Department with complaints of right leg and right lower quadrant abdominal pain. The patient had a history of two prior C‐sections, with the most recent being 6 months prior to presentation. Clinical exam revealed a mass in the region of the right hemipelvis. CT imaging identified a large tumor in the right hemipelvis with regional mass effect on the bladder and uterus, and involvement of the right external iliac and common femoral veins. A thrombus of the right common femoral vein was identified on ultrasound.
She was subsequently referred to Surgical Oncology for further evaluation and management of the pelvic mass. There was no history of FAP or colorectal cancer. A colonoscopy was performed with no evidence of colon cancer or polyps. Laboratory workup was noncontributory. An ultrasound‐guided biopsy of the mass was performed and was consistent with desmoid tumor. An MRI of the abdomen and pelvis was obtained and revealed a large, heterogeneously enhancing tumor occupying the right side of the pelvis without visible invasion of the pelvic organs (Figure 1).
Figure 1.
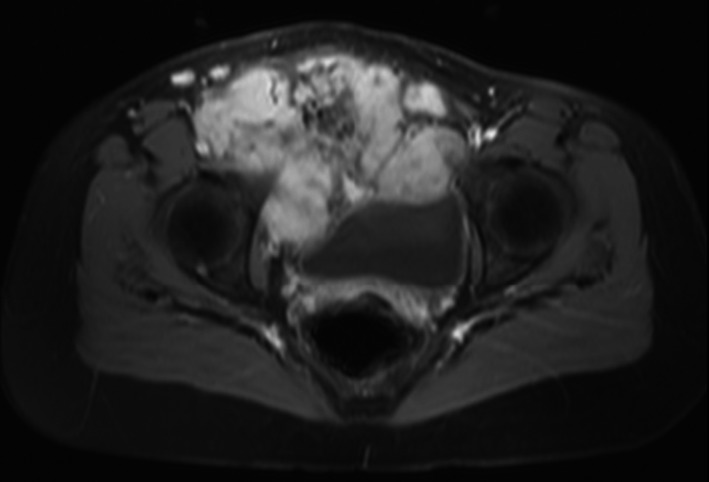
Representative axial image of a gadolinium‐enhanced MRI of the pelvis in a 21‐y‐old woman with desmoid fibromatosis of the right hemipelvis. The tumor displaced the bladder and uterus and involved the superior pubic ramus, lymphatics, and common femoral and external iliac veins
Resection of the tumor and reconstruction of the abdominal wall was performed by a multidisciplinary team including Surgical Oncology, General Surgery, Orthopaedic Oncology, and Urology. The tumor had eroded into the right pubic rami and pubic symphysis, which were partially excised along with the main tumor. The lymphatics were involved and resected along with the tumor. The right femoral vein and external iliac vein were thrombosed and were ligated, further contributing to the subsequent lymphedema in the right leg. Final pathology was consistent with desmoid tumor with positive margins and measured 17 × 13 × 10 cm in size.
Postoperatively, the patient developed significant lymphedema of her right leg (Figure 2). She underwent treatment for lymphedema including compression stockings, massage, lymphedema pumps, and physical therapy. A repeat MRI of the abdomen and pelvis as well as of bilateral lower extremities was obtained 10 months postoperatively and demonstrated two soft tissue lesions in the right groin which were suspicious for recurrence of extra‐abdominal desmoid tumor. There was no involvement of the lower extremities on MRI. After a discussion with the patient and due to concern for high risk of wound complications and the expected morbidity of further surgery, consideration was given to more conservative treatment options. Treatment with sulindac was started, and serial advanced imaging showed no significant progression of disease in the pelvis.
Figure 2.

Clinical photograph of a 21‐y‐old woman who developed significant lymphedema after surgery resection of desmoid fibromatosis from her right hemipelvis
Five years after resection of her original tumor, the patient complained of a new masses in the right ankle and right upper calf region. MRI's demonstrated a new 7 cm mass at the right ankle and 10 cm mass at the right upper calf (Figure 3). There was no evidence of other distant metastasis on PET‐CT. Separate biopsies of the right calf and ankle masses were performed, and pathology was consistent with desmoid fibromatosis. Treatment options were discussed with the patient including surgical resection, chemotherapy, and radiation. The patient elected to proceed with nonsurgical treatment and underwent radiation therapy and continued treatment with sulindac. She did not tolerate radiation well and did not complete therapy. Nine years after resection of her initial abdominal tumor, the patient's multifocal disease is stable.
Figure 3.
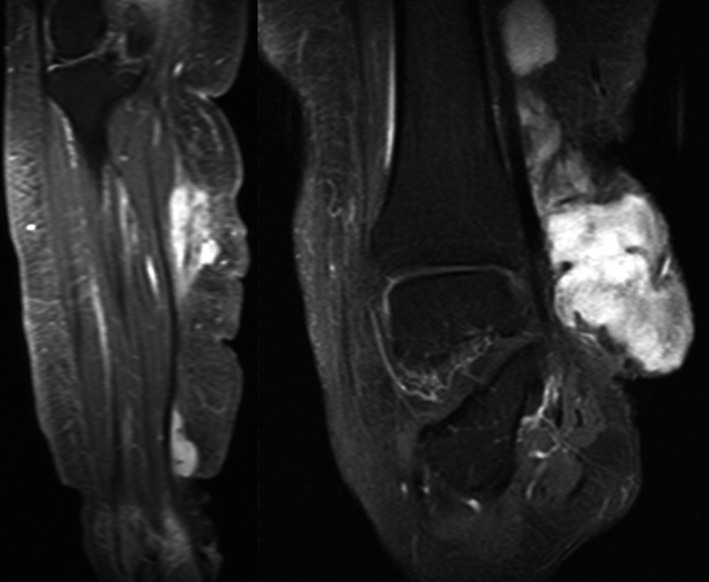
Representative coronal images of a gadolinium‐enhanced MRI of the lower leg and ankle in a 21‐y‐old woman who developed multifocal fibromatosis. Separate tumors are noted within the calf and ankle region
The second patient is a 20‐year‐old man who presented to our Emergency Department with a history of fibromatosis at the right foot and ankle status post four previous resections at an outside institution, each time with more aggressive recurrence. He was referred to Orthopaedic Oncology where his clinical exam revealed a fungating wound with tumor exposed over the lateral aspect of his foot. An MRI of the lower extremity demonstrated a large mass at the lateral aspect of the ankle and foot measuring 11 × 11 × 6 cm (Figure 4A). Laboratory findings were noncontributory. History was negative for FAP or colorectal cancer and a colonoscopy demonstrated no abnormalities. A biopsy performed in the office was consistent with recurrent fibromatosis. Resection of the tumor was performed with negative margins. The final pathology was consist with fibromatosis.
Figure 4.
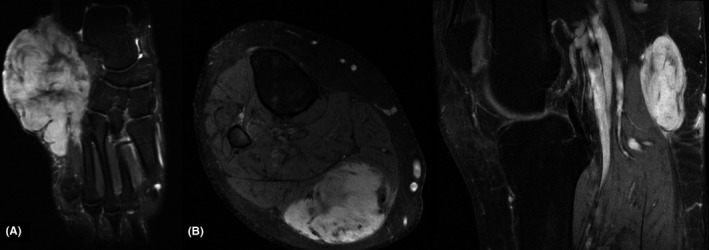
Representative gadolinium‐enhanced MRI images of a 20‐y‐old man who developed multifocal fibromatosis. A, An axial view of the foot demonstrating the patient's initial tumor that involved the lateral foot and ankle region and had resulted in a fungating wound. B, After amputation, and axial view of the leg at the distal stump and a sagittal view of the popliteal fossa demonstrates multifocal disease
Sixteen months after the resection, the patient developed a recurrence over the posterior ankle and a repeat resection was performed, again with negative margins. The patient had difficulty with wound healing and developed another recurrence of the tumor. Three years after his initial resection at our facility, the patient elected to undergo a below the knee amputation for a nonhealing wound at the right ankle with concurrent recurrence of the fibromatosis. The amputation healed well and he went on to wearing a prosthesis and returned to work. The following year he began to develop multiple episodes of folliculitis under the prosthesis due to sweating while working. This resulted in intermittent skin breakdown and was treated with rest, antibiotics, and local wound care.
Thirty‐two months after amputation, he developed a mass at the posterior stump that was painful while wearing his prosthesis. MRI of the lower extremity was obtained showing a 6 cm mass at the popliteal fossa area as well as a separate mass within the distal posterior calf musculature (Figure 4B). This was consistent with PET‐CT findings, which demonstrated no other areas of disease and a repeat colonoscopy was normal. Biopsies of the two separate tumors were performed confirming multifocal fibromatosis. Treatment options were discussed including surgical resection and conservative treatments. The patient subsequently underwent systemic treatment with vinblastine and methotrexate. The patient was intermittently compliant with treatment. The disease resolved while on treatment but would recur when he stopped his chemotherapy.
3. DISCUSSION
Desmoid fibromatosis is rare with an incidence of 3‐4 per million.1 The majority of these are intra‐abdominal and arise from the abdominal viscera, with extra‐abdominal tumors occurring in 43% of cases.10, 11 Multifocal desmoid fibromatosis is even less common. In one series of 234 cases of extra‐abdominal desmoid tumors, only 11% had more than one site involved.10
While it is difficult to prove the relationship between trauma and development of this disease, the incidence of trauma preceding the development of desmoid fibromatosis is greater than that reported for other soft tissue tumors.12, 13 Further, dysregulation of wound healing has been implicated in the development of fibromatosis. This has been demonstrated in mouse models where β‐catenin was shown to be an important part of normal cutaneous wound healing and that stabilization of β‐catenin alone is sufficient to cause aggressive fibromatosis.9 The WNT/β‐catenin signaling pathway has been implicated in a variety of inflammatory conditions including neuroinflammatory syndromes, such as Alzheimer's disease, autoimmune disease, cancer, and the inflammatory response to bacterial infection.14 While research is limited due to the rare nature of this disease, it appears that chronic inflammation and repetitive trauma may be considered a risk factor for developing multifocal disease.
The mainstay of treatment for desmoid tumor has traditionally been surgical resection as well as radiation.15 More recently, nonsurgical management including hormone therapy, cytotoxic chemotherapy, nonsteroidal anti‐inflammatory medications, and observation have proven to be effective.16, 17, 18 In the cases described, surgical management was initially chosen as this was the typical treatment of these tumors at the time of presentation. In the case of the pelvic resection, significant morbidity resulted in the form of severe lymphedema of the right leg. The patient with the ankle tumor developed multiple recurrences with wound breakdown that finally resulted in amputation. Subsequently, both patients underwent nonsurgical management with stabilization and intermittent resolution of their multifocal disease, respectively.
4. CONCLUSION
We believe that this is the first report of the development of multifocal, distant disease after the surgical resection of desmoid fibromatosis. The morbidity of further surgical management and the possibility of development of both recurrence and development of new tumors, even with amputation, are concerning in both these patients. As the treatment of desmoid fibromatosis has evolved, so has the understanding that surgical resection can result in significant morbidity and decreased function compared with other treatments.19 In the cases described, the surgical morbidity subsequently resulted in the development of multifocal disease. These findings suggest that chronic inflammation, and repetitive trauma are a risk factor for the development of multifocal disease in patients with solitary, sporadic desmoid fibromatosis.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTION
LMZ: was responsible for study design, literature review, composition and editing of the manuscript, and editing the figures. BMB: was responsible for the literature review, composition of the manuscript, and editing of the figures. NLW: was responsible for reviewing and editing the manuscript.
Bauer BM, Williams NL, Zuckerman LM. Development of multifocal extra‐abdominal desmoid fibromatosis after surgical resection. Clin Case Rep. 2019;7:2515–2519. 10.1002/ccr3.2551
REFERENCES
- 1. Hosalkar HS, Torbert JT, Fox EJ, et al. Musculoskeletal desmoid tumors. J Am Acad Orthop Surg. 2008;16:188‐198. [DOI] [PubMed] [Google Scholar]
- 2. Shih HA, Hornicek FJ, DeLaney TF, et al. Fibromatosis: current strategies for treatment. Curr Opin Orthop. 2003;14:405‐412. [Google Scholar]
- 3. Wagstaff MJD, Raurell A, Perks AGB. Multicentric extra‐abdominal desmoid tumours. Br J Plast Surg. 2004;57:362‐365. [DOI] [PubMed] [Google Scholar]
- 4. Penel N, Chibon F, Salas S. Adult desmoid tumors: biology, management and ongoing trials. Curr Opin Oncol. 2017;29:268‐274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Eastley N, Mcculloch T, Esler C, et al. Extra‐abdominal desmoid fibromatosis: a review of management, current guidance and unanswered questions. Eur J Surg Oncol. 2016;42:1071‐1083. [DOI] [PubMed] [Google Scholar]
- 6. Schlemmer M. Desmoid tumors and deep fibromatoses. Hematol Oncol Clin North Am. 2005;19:565‐571. [DOI] [PubMed] [Google Scholar]
- 7. Lopez R, Kemalyan N, Moseley HS, et al. Problems in diagnosis and management of desmoid tumors. Am J Surg. 1990;159:450‐453. [DOI] [PubMed] [Google Scholar]
- 8. Enzinger FM, Weiss SW, Enzinger FM, et al. Soft Tissue Tumours, 3rd edn St. Louis, MO: Mosby‐Yearbook Inc; 1995:201. [Google Scholar]
- 9. Cheon SS, Cheah AY, Turley S, et al. beta‐Catenin stabilization dysregulates mesenchymal cell proliferation, motility, and invasiveness and causes aggressive fibromatosis and hyperplastic cutaneous wounds. Proc Natl Acad Sci USA. 2002;99:6973‐6978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mankin HJ, Hornicek FJ, Springfield DS. Extra‐abdominal desmoid tumors: a report of 234 cases. J Surg Oncol. 2010;102:380‐384. [DOI] [PubMed] [Google Scholar]
- 11. Reitamo JJ, Häyry P, Nykyri E, et al. The desmoid tumor. I. Incidence, sex‐, age‐ and anatomical distribution in the Finnish population. Am J Clin Pathol. 1982;77:665‐673. [DOI] [PubMed] [Google Scholar]
- 12. Enzinger FM, Shiraki M. Musculo‐aponeurotic fibromatosis of the shoulder girdle (extra‐abdominal desmoid). Analysis of thirty cases followed up for ten or more years. Cancer. 1967;20:1131‐1140. [DOI] [PubMed] [Google Scholar]
- 13. Reitamo JJ, Scheinin TM, Häyry P. The desmoid syndrome. New aspects in the cause, pathogenesis and treatment of the desmoid tumor. Am J Surg. 1986;151:230‐237. [DOI] [PubMed] [Google Scholar]
- 14. Baizabal‐aguirre VM. Editorial: cross‐talk mechanisms of Wnt/beta‐catenin signaling components with TLR‐activated signaling molecules in the inflammatory response. Front Immunol. 2017;8:1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fiore M, MacNeill A, Gronchi A, et al. Desmoid‐type fibromatosis: evolving treatment standards. Surg Oncol Clin N Am. 2016;25:803‐826. [DOI] [PubMed] [Google Scholar]
- 16. Ingley KM, Burtenshaw SM, Theobalds NC, et al. Clinical benefit of methotrexate plus vinorelbine chemotherapy for desmoid fibromatosis (DF) and correlation of treatment response with MRI. Cancer Med. 2019;00:1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mastoraki A, Schizas D, Vergadis C, et al. Recurrent aggressive mesenteric desmoid tumor successfully treated with sorafenib: a case report and literature review. World J Clin Oncol. 2019;10:183‐191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Turner B, Alghamdi M, Henning JW, et al. Surgical excision versus observation as initial management of desmoid tumors: a population based study. Eur J Surg Oncol. 2019;45:699‐703. [DOI] [PubMed] [Google Scholar]
- 19. Newman ET, Lans J, Kim J, et al. PROMIS function scores are lower in patients who underwent more aggressive local treatment for desmoid tumors. Clin Orthop Relat Res. 2019; Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]


