Abstract
A 41‐year‐old man with abdominal enlargement, as a result of large retroperitoneal Schwannoma, was reported to our center. It was seen to have caused the displacement of the colon and was attached to the presacral region of the spine. Following the diagnosis, successful resection of Schwannoma was achieved.
Keywords: pelvic, Schwannomas, surgery
A 41‐year‐old man with abdominal enlargement, as a result of large retroperitoneal Schwannoma, was reported to our center. It was seen to have caused the displacement of the colon and was attached to the presacral region of the spine. Following the diagnosis, successful resection of Schwannoma was achieved.

1. INTRODUCTION
Schwannomas, also known as neurilemmoma, are rare and benign neurogenic tumors that have their origin from well‐differentiated Schwann cells (that make up the nerve sheath). The majority of these tumors are found in the head and neck region, which might also affect the oral cavity. In exception to the olfactory and cranial nerves, they can affect all other cranial, peripheral, and autonomic nerves in the majority of the cases.1, 2
Sporadic cases of pelvic Schwannomas (1%‐3%), arising from sacral nerve or hypogastric plexus, are also reported; however, due to inconsistencies in clinical symptoms, they can be misdiagnosed as pelvic lesions. Schwannomas are removed surgically, with effective and long‐term therapeutic outcomes.3 They are usually found in the form of a large solid cyst; nonetheless, cystic degeneration can cause necrosis.4
2. CASE PRESENTATION
A 41‐year‐old man was referred to our center with the abdominal enlargement and stiffening due to the masses (Figure 1). Workup showed no other symptoms, and the routine laboratory tests were as follows:
Figure 1.

A view of the patient's swollen abdomen due to the presence of mass
WBC: 4.2 (Neutrophils: % 67), RBC: 3.86 (Lymphocyte: % 29 [Low]), HGB: 11.2 (Monocytes: % 3 [Low]), HCT: 33.2 (Eosinophil: % 1 [Low]), MCV: 86, MCH: 29, MCHC: 33.7, Platelets: 166, RDW‐CV: 13.5, ESR (1h): 11, Blood Glucose: 105, CRP: Positive, CEA: 0.85, CA 19‐9:21.9, and TSH: 5.9.
Pelvis MRI with and without gadolinium injection revealed the absence of avascular necrosis, dislocation, and bursitis. Bladder showed normal wall thickness whereas left hydronephrosis was seen. There was a large 187 *120 *752 mm well‐defined heterogeneous enhancing mass with the necrotic and cystic component in the pelvic cavity left to the urinary bidder extending to aortic bifurcation with pressure effect to the bowel loops and urinary bladder that appeared to be in the retroperitoneal region. It was suspected to be a soft tissue sarcoma. Fat pain around the mass was intact, and biopsy was recommended.
Helical spiral CT of the abdomen and pelvis with and without gadolinium contrast showed the homogenous density of the liver and spleen without any space mass; the vessels and bile ducts were also normal. In para‐aortic regions, no significant lesions were observed and no signs of a valuable lesion of the abdominal aorta were observed. The adrenal glands and pancreas had a normal appearance, and there was no lesion in the small intestine.
Patellar lobes of the pelvic region seemed normal, and the kidneys had normal secretion too. No symptoms were reported in favor of parenchymal spastic lesions. In no‐contrast images, there were no symptoms in favor of the stone in the kidney and ureter's pyelocaliceal system. The bladder had a normal appearance, and the hematuronic mass 155 mm × 122 mm inside the pelvic and lower abdominal cavity with a compressive effect on adjacent organs was found with severe renal hydronephrosis.
The right urethral catheter was inserted in the bladder and the right urethra. The pathological outcomes confirmed the existence of Schwannoma.
Patient echocardiography for mitral valve, aortic valve, tricuspid valve, pump valve, and mitral valve were reported as normal.
The patient underwent the surgery for the removal of the mass (Figure 2). After opening the abdomen, a mass of about 25 cm in diameter was detected in retroperitoneum that had displaced the sigmoid colon to the right. The sigmoid and mesosigmoid were gradually separated from the mass and the peritoneum was opened to access the mass, which was released from the surrounding area.
Figure 2.
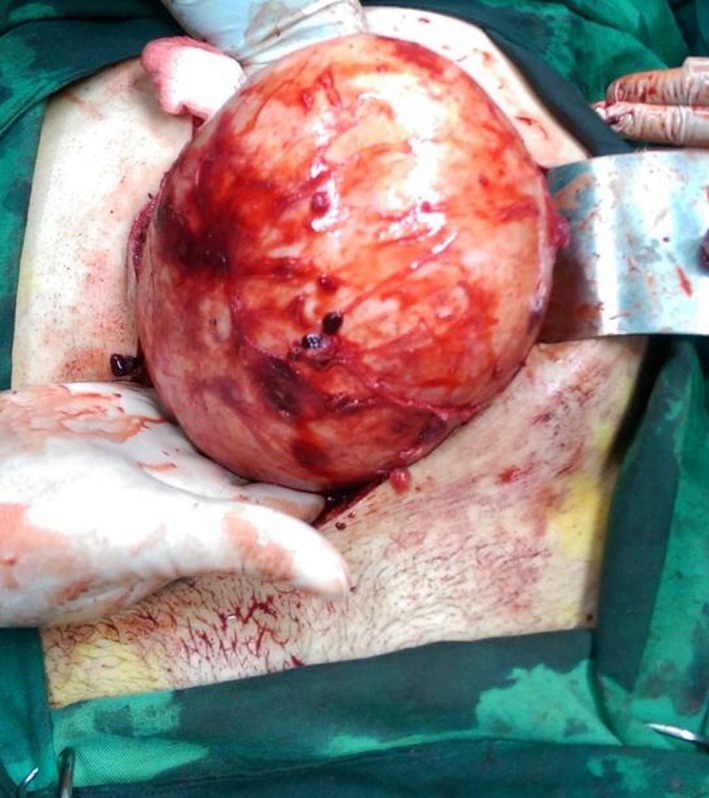
View of the mass out of the patient's abdomen
The ureter of the two sides, due to preoperative stenting, was explored and separated from the mass.
The mass at the posterior had a severe adhesion to the spine, especially in the presacral region, which was gradually released by the preservation of the hypogastric nerves without any damage to the rectum. Ultimately, the mass was completely removed and was kept hemostatic with the wall. After the surgery, the general condition of the patient was well, and the vital signs were stable, and evidence of bleeding was tolerated. After 24 hours, making sure that Ileus was not present, the patient was discharged. During the admission, he was administered antibiotics only. Following the surgery, he did not show any complications such as urinary and stool incontinency, and impotency. To date, the patient did not report the recurrence of the mass.
3. DISCUSSION
Pelvic Schwannomas originate from sacral nerve or hypogastric plexus; nonetheless, only a small amount of these cases is reported.5 Mainly they are benign, whereas in von Recklinghausen's disease, they are found in the malignant state. Enlargement of these tumors, causing pain and compressions of the surrounding viscera, aids the diagnosis of Schwannomas while left unnoticed otherwise. The radiological examination can help clinicians and surgeons to define the morphology and histology of the tumor such as hematoma, cystic or connective tissue tumor.6 Occasionally, imaging results can be misleading; therefore, the biopsy is recommended.7 Furthermore, histological findings by complete or fractional tumor resection can aid to analyze the type and the nature and also to attain surgical accuracy depending on the benignness or the malignancy of the mass, for malignant tumors are associated with the greater rate of recurrence perhaps, due to their resistance to chemoradiotherapies.8, 9 Several case studies have suggested that these tumors can be accidentally identified, particularly in benign cases.10
Molecular studies have revealed that certain tumor suppressor genes like SMARCB1 and LZTR1 are likely to be associated with the pathogenesis of the Schwannomas.11
Fewer previous case reports have marked the clinical significance and timely management of Schwannomas. Xu, Sha3 reported a successful resection of 16 cm diameter retroperitoneal Schwannoma in an elderly patient; however, excessive bleeding was seen in this case. Retroperitoneal schwannoma accounts for 6% retroperitoneal. Similarly, in a recent report by Wang, Yu12 a pediatric case of a painless Schwannoma near the right lumbar region. After successful removal of the tumor, one month later, recurrence was seen. Tumorectomy of conducted due to the aggressive recurrence of the mass thrice. Advancements in surgical techniques have allowed surgeons to perform laparoscopic resection of the tumor. Di Furia, Salvatorelli13 in a recent case study reported the laparoscopic resection of pelvic schwannoma originating from hypogastric plexus. They suggested that the method offers a better field of view with greater surgical advantages in obese patients. Nonetheless, owing to its neurological origin, blunt dissections are likely to give rise to neurological damage.
4. CONCLUSION
In this case, we report a resection of the giant malignant pelvic Schwannoma, which was located in the retroperitoneal region. Owing to the size of the tumor, displacement of the viscera such as sigmoid colon was seen in this case. However, successful surgical correction and resection of the Schwannoma were achieved without any perioperative and postoperative complications. Timely management of Schwannoma can save patients from the loss of sensory functions and motor weakness. Moreover, follow‐up is required to inspect the recurrence of the tumor.
CONFLICT OF INTEREST
The authors deny any conflict of interest in any terms or by any means during the study. All the fees provided by research center fund and deployed accordingly.
AUTHOR CONTRIBUTIONS
HP: conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript. LHM: designed the data collection instruments, collected data, carried out the initial analyses, reviewed and revised the manuscript, coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Pak H, Haji Maghsoudi L. Pelvic Schwannoma: In light of a case report. Clin Case Rep. 2019;7:2488–2490. 10.1002/ccr3.2542
REFERENCES
- 1. Lira RB, Gonçalves Filho J, Carvalho GB, Pinto CA, Kowalski LP. Lingual schwannoma: case report and review of the literature. Acta Otorhinolaryngol Ital. 2013;33(2):137‐140. [PMC free article] [PubMed] [Google Scholar]
- 2. Aswath N, Manigandan T, Sankari SL, Yogesh L. A rare case of palatal schwannoma with literature review. J Oral Maxillofac Pathol. 2019;23(Suppl 1):36‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Xu H, Sha N, Li HW, et al. A giant pelvic malignant schwannoma: a case report and literature review. Int J Clin Exp Pathol. 2015;8(11):15363‐15368. [PMC free article] [PubMed] [Google Scholar]
- 4. Padmanaban N, Chandrabose PS, Esakki M, Kirubamani H, Srinivasan C. Gynaecological perspective of Schwannoma: a rare pelvic tumour. J Clin Diagn Res. 2016;10(4): QD03‐QD05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chan PT, Tripathi S, Low SE, Robinson LQ. Case report–ancient schwannoma of the scrotum. BMC Urol. 2007;7:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jindal T,Mukherjee S, Kamal MR,, et al. Cystic schwannoma of the pelvis. Ann R Coll Surg Engl. 2013;95(1):e1‐e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Walczak DA, Jaguścik R, Olborski B, Fałek W, Trzeciak PW. Retroperitoneal "ancient" Schwannoma ‐ a rare case of rare location: case report and literature review. Pol Przegl Chir. 2012;84(12):646‐650. [DOI] [PubMed] [Google Scholar]
- 8. Cury J, Coelho RF, Srougi M. Retroperitoneal schwannoma: case series and literature review. Clinics (Sao Paulo). 2007;62(3):359‐362. [DOI] [PubMed] [Google Scholar]
- 9. Choudry HA, Nikfarjam M, Liang JJ, et al. Diagnosis and management of retroperitoneal ancient schwannomas. World J Surg Oncol. 2009;7:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jones A, Doepker M, Kellermier H. Incidental pelvic Schwannoma: a case report. Oncol Cancer Case Rep. 2018;4:146. [Google Scholar]
- 11. Kehrer‐Sawatzki H, Farschtschi S, Mautner VF, Cooper DN. The molecular pathogenesis of schwannomatosis, a paradigm for the co‐involvement of multiple tumour suppressor genes in tumorigenesis. Hum Genet. 2017;136(2):129‐148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wang J, Yu M, Zhu H, et al. Retroperitoneal malignant schwannoma in a child. J Int Med Res. 2018;46(10):4315‐4322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Di Furia M,Salvatorelli A, Della Penna A, et al. Advantage of laparoscopic resection for pelvic Schwannoma: case report and review of the literature. Int J Surg Case Rep. 2018;45:38‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]


