Abstract
Objectives
This study aims to assess early changes in physical activity and function after total hip arthroplasty (THA) using both subjective and objective methods, and to identify predictors of outcomes of THA.
Patients and methods
Between October 2014 and October 2015, a total of 50 patients (14 males, 36 females; mean age 57.1±13.0 years; range, 31 to 75 years) with end-stage primary hip osteoarthritis who were scheduled for THA and 50 age- and sex-matched controls (10 males, 40 females; mean age 52.9±9.3 years; range, 36 to 75 years) were included in the study. Pain was evaluated using the Numeric Rating Scale (NRS), physical function using the Lequesne Index, physical capacity using the Six-Minute Walking Test (6MWT), and physical activity using both International Physical Activity Impact Questionnaire Short Form (IPAQ-SF) and step count monitor. Data at baseline and six weeks and six months were recorded.
Results
Pain severity was significantly lower after THA at six weeks and six months (NRS scores: 2.83 and 0.82, respectively; p<0.001), compared to baseline. Physical function, capacity, and activity significantly improved after THA at six weeks and six months with a mean Lequesne Index score of 2.62 and 1.02, respectively. The mean 6MWT distance was 272.62 at six weeks and 326.16 at six months. The mean IPAQ and 6MWT results were similar between the patient and control groups at six weeks and six months. Age, presence of comorbidities, and baseline Lequesne Index score were found to be effective on functional outcomes of THA. Age and baseline 6MWT scores were correlated with physical capacity after THA.
Conclusion
Our study showed a significant early improvement in pain severity and physical activity and function at six weeks and six months after THA, compared to baseline values. Baseline values and age were the positive predictors of improved postoperative function and physical capacity.
Keywords: Osteoarthritis, pain, physical activity, physical function, total hip arthroplasty, total hip replacement
Introduction
Osteoarthritis (OA) is the most common cause of arthritis. The 2016 Global Burden of Disease study ranked it as the second most rapidly rising cause of years lived with disability after diabetes mellitus and reported an OA incidence of 199/100,000 individuals.[1]
Single-joint OA may affect the lumbar spine and hand, hip, or knee joints. Hip OA is less common than knee OA and presents equally in men and women.[2] The main goals of OA management are to minimize pain, improve function, and modify the process of joint damage by targeting modifiable risk factors.[3] Conservative OA management requires non-pharmacological interventions such as exercise, weight loss, and walking aids. Pharmacological interventions include topical or oral non-steroidal anti-inflammatory drugs (NSAIDs), duloxetine, capsaicin, or intra-articular glucocorticoid injection.
Total hip arthroplasty (THA) is the gold-standard intervention in OA patients unresponsive to conservative treatment. It has been proven to be effective in reducing pain and improving joint function significantly.[4] However, 9% of patients undergoing THA still experience residual joint pain postoperatively.[5] The high rate of unfavorable outcomes after surgery may be associated with the presence of individual problems, such as pain at other joints and comorbidities.[6]
Evaluation of postoperative outcomes requires a quantitative assessment of several parameters. Self-reporting questionnaires are the most common method of physical function and activity assessment.[7] Also, devices such as accelerometers and pedometers have gained popularity in recent years owing to their easy-to-use design and the lack of recall bias associated with questionnaires.[8]
In the present study, we hypothesized that (i) patients with THA would benefit from surgery with similar physical activity and capacity with the age- and sex-matched controls at the postoperative sixth weeks, which is an earlier endpoint, compared to previous studies; (ii) preoperative physical function and capacity values and several socio-demographic factors such as age, sex, occupation, body mass index (BMI), comorbidities, and marriage would affect the outcomes of THA. Therefore, in this study, we aimed to assess early changes in physical activity and function after THA using both subjective and objective methods, and to identify predictors of outcomes of THA.
Patients and Methods
This single-center, prospective study was conducted at Ankara Numune Training and Research Hospital between October 2014 and October 2015. A total of 50 patients (14 males, 36 females; mean age 57.1±13.0 years; range, 31 to 75 years) with Grade 4 end-stage primary hip OA according to the Kellgren-Lawrence[9] classification who were unresponsive to conservative treatment and scheduled for THA and 50 age- and sex-matched controls (10 males, 40 females; mean age 52.9±9.3 years; range, 36 to 75 years) who had no arthroplasty and no pain in the lower extremity among the family members or attendants of hospitalized patients were included in the study. Patients aged above 75 years with accompanying joint diseases or advanced pulmonary and cardiovascular diseases which can affect mobilization, patients having prior contralateral hip surgery within the last 12 months, patients with mental problems that can affect participation in the study, and those inconvenient for follow-up due to far distance from the hospital were excluded. A written informed consent was obtained from each participant. The study protocol was approved by the Ankara Numune Training and Research Hospital Ethics Committee. The study was conducted in accordance with the principles of the Declaration of Helsinki.
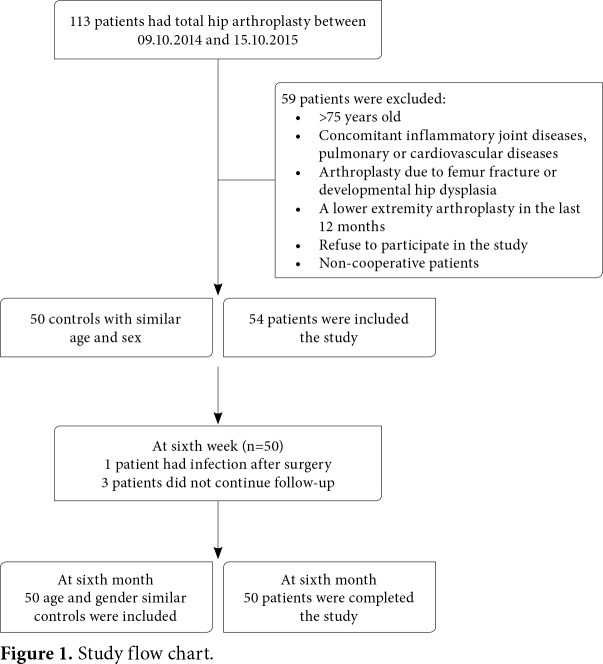
Data including baseline demographic and clinical characteristics of the patients and controls were recorded. Pain (Numeric Rating Scale [NRS]), physical function (Lequesne Index), physical capacity (Six-Minute Walking Test [6MWT]), and physical activity (International Physical Activity Questionnaire- Short Form [IPAQ-SF] and step count monitor) were recorded at baseline and at six weeks and six months in the patients with THA. Controls were evaluated with the 6MWT for physical capacity and IPAQ-SF for physical activity. The study flow chart is shown in Figure 1.
Figure 1. Study flow chart.
Interventions and follow-up measures
All THA surgeries were carried out by two orthopedic surgeons at a single center. All operations were performed via the anterolateral approach, and all patients received the uncemented prosthesis. All patients were evaluated for pain, physical function, capacity, and activity at one week before surgery and at six weeks and six months after surgery.
Postoperative treatment protocol
Postoperative pain was managed by tramadol and paracetamol as analgesics. However, in the late period following wound healing (after three weeks), the patients were allowed to take diclofenac 150 mg/day or its equivalent dose of NSAIDs. A postoperative rehabilitation program of weight-bearing exercises was performed by all patients.
Pain severity
Pain severity was evaluated using the NRS, a numeric scale on which 0 indicates no pain and 10 indicates the most severe pain the patient has ever experienced. Reliability and validation studies of the scale have been conducted in patients with chronic [10] pain.
Physical function
Lequesne Index is a valid and reliable index in the Turkish population and is a subjective 10-question survey to assess physical function in OA patients. It consists of five questions about pain or discomfort, one question about maximum distance walked, and four questions about activities of daily living. It is scored on a 0 to 24 scale. Lower scores indicate less functional impairment with values ≤7 considered as mild to moderate, 8 to 13 as severe, ≥14 as extremely severe impairment.[11,12]
Physical capacity
Physical capacity was assessed by the 6MWT, it is an objective method to evaluate exercise tolerance. It was performed on an unobstructed bare 30 meters (m) floor where every 3 meters were marked. The patients were allowed to complete the test by reducing their walking speed or stopping and getting some rest, if needed.[13] Maximum walking distance (meters) within six min was measured. An advantage of the 6MWT is that it allows the patients to exercise in the test model that they are familiar with. The 6MWT was previously used in studies evaluating patients with THA.[13,14] Previous studies showed that 6MWT distance in patients with lower extremity arthroplasty was found to be about 300 to 400 meters.[15,16]
Physical activity
Physical activity was assessed using the International IPAQ-SF and step count monitor. The IPAQ-SF which has been shown to be reliable and valid in the Turkish population is a subjective method of seven questions used to evaluate time spent in sitting, walking, and moderate-to-severe activities in the past seven days.[17] We used the metabolic equivalent of task (MET)-min score to calculate the energy required for the physical activities. Standard MET values are as follows: sitting= 1.5 MET, walking= 3.3 MET, moderate physical activity= 4.0 MET, and severe physical activity= 8.0 MET. Using these values, daily and weekly levels of physical activity were calculated. Values less than 600 MET-min/week were assessed as low, 600 to 3,000 MET-min/week as moderate physical activity, more than 3,000 MET-min/week as high physical activity. Step count monitor is a device used to count how many steps patients walk daily. Patients wore the step activity monitor (TKS1257/ BTM life) on the right wrist and were told to wear it from the time they woke up, until they went to bed. The mean steps per day were calculated for all patients. Basset et al.[18] indicated that step counts could be measured easily and definitely and this parameter has relations with physical health variables. Takenaga et al.[14] used the step activity monitor as a valid parameter for the patients after THA.
Statistical analysis
A power analysis was performed using the G* power version 3.0.10 program (Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany) to ensure the adequate sample size. To obtain a power of 0.90 [α (Type I error) was 0.05 and β (Type II error) was 0.10, and analysis of variance test with three repetitions], an appropriate total sample size was calculated as 50 for this study.
Statistical analysis was performed using the IBM SPSS version 21.0 software (IBM Corp., Armonk, NY, USA). Descriptive data were expressed in mean ± standard deviation (SD), median (min-max), or number and frequency. The Shapiro-Wilk test was used to test for the normality of the distribution of data. The Mann-Whitney U, Student’s t-, and chi-square or Fisher’s exact tests were used to compare continuous and nominal variables between groups. Analysis of pain, physical functioning, and physical capacity were conducted by repeated measured analysis of variance (ANOVA). The factors which would be effective on the physical function levels with the Lequesne Index scores and physical capacity with the 6MWT at six months after surgery were evaluated with the multivariate logistic regression analysis. The Lequesne Index scores and 6MWT results were evaluated in both groups. Using the Lequesne Index, the first group consisted of 0-point score which indicates no pain and no disability and the second group consisted of 1 to 7 points which indicate mild-to-moderate functional impairment. The 6MWT results were assessed in both groups according to a walking distance of <300 meters and ≥300 meters. Univariate analysis included variables and at least moderately significant variables (i.e., age, sex, comorbidities, and marriage) were selected for the multivariate logistic regression analysis. A p value of <0.05 was considered statistically significant.
Results
Demographic and clinical characteristics of the patients and controls are shown in Table 1. The mean NRS score at baseline was 7.7±0.3. The mean score at six weeks and six months postoperatively were 2.8±0.3 and 0.8±0.2, respectively. There was a statistically significant difference between the scores at baseline and at six weeks and six months (p<0.001).
Table 1. Demographic and clinical characteristics of study population Patients with THA (n=50).
| Patients with THA (n=50) | Controls (n=50) | ||||||
| n | % | Mean±SD | n | % | Mean±SD | p | |
| Age (year) | 57.1±13.0 | 52.9±9.3 | 0,077 | ||||
| Body mass index (kg/m2) | 29.2±5.2 | 28.1±5.0 | 0,497 | ||||
| Sex | 36 | 72 | 40 | 0,349 | |||
| Female | 36 | 72 | 20 | ||||
| Male | 14 | 28 | 10 | 20 | |||
| Body mass index | 12 | 0,112 | |||||
| Normal weight | 11 | 22 | 24 | ||||
| Overweight | 22 | 44 | 13 | 26 | |||
| Obese | 14 | 28 | 24 | 48 | |||
| Morbid obese | 3 | 6 | 1 | 2 | |||
| Marital status | 36 | 0,554 | |||||
| Living with a partner | 39 | 78 | 72 | ||||
| Living alone | 11 | 22 | 14 | 28 | |||
| Working status | 37 | 0,334 | |||||
| No | 41 | 82 | 74 | ||||
| Yes | 9 | 18 | 13 | 26 | |||
| Comorbidities | 24 | 0,313 | |||||
| No comorbidities | 19 | 38 | 48 | ||||
| Diabetes mellitus | 4 | 8 | 8 | 16 | |||
| Hypertension | 8 | 16 | 10 | 20 | |||
| Asthma-chronic bronchitis | 3 | 6 | 1 | 2 | |||
| Gastritis | 9 | 18 | 10 | 20 | |||
| Depression | 2 | 4 | 1 | 2 | |||
| Hypothyroidism | 3 | 6 | 2 | 4 | |||
| Urolithiasis | 1 | - | - | ||||
| THA: Total hip arthroplasty; SD: Standard deviation. | |||||||
The mean Lequesne Index scores at baseline and at six weeks and six months were 14.6±0.6, 2.6±0.2, and 1.0±0.2, respectively. There was a statistically significant difference between the mean scores at baseline and at six weeks and six months (p<0.001). At six months, data 25 patients showed no functional disability with 0 Lequesne Index score.
The mean walking distance at baseline and at six weeks and six months was 189.9±16.1 m, 272.6±11.2 m, and 326.2±12.4 m, respectively, indicating a statistically significant difference between the mean scores at baseline and at six weeks and six months (p<0.001).
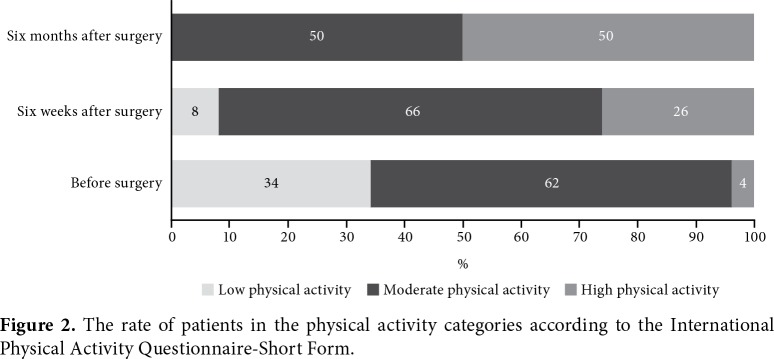
The mean IPAQ-SF scores at baseline and at six weeks and at six months were 953.2±139.0 MET-min/week, 2,125.6±165.6 MET-min/week, and 2,870.8±229.7 MET-min/week, respectively. There was a statistically significant difference between mean scores at baseline and at six weeks and six months (p<0.001). The patients were further classified according to the level of physical activity as low, moderate, and high. The rate of patients in each category at baseline and at six weeks and at six months are shown in Figure 2.
Figure 2. The rate of patients in the physical activity categories according to the International Physical Activity Questionnaire-Short Form.
The mean step count at baseline and at six weeks and six months were 4,091.5±235.9, 5,914.4±400.9, and 7,093.3±488.9, respectively. There was a statistically significant difference between the step counts at baseline and at six weeks and six months, respectively (p<0.001). Pain, physical function, capacity, and activity scores before, at six weeks and six months of surgery are summarized in Table 2.
Table 2. Clinical assessments before and after total hip arthroplasty.
| Mean±SD | Mean±SE | 95% CI | p | |
| Numeric Rating Scale | ||||
| Baseline | 7.7±0.3 | |||
| Six weeks after surgery | 2.8±0.3 | 4.9±0.2 | 3.89 - 5.04 | <0.001 |
| Six months after surgery | 0.8±0.2 | 2.0±0.1 | 1.86 - 2.17 | <0.001 |
| Lequesne Index | ||||
| Baseline | 14.6±0.6 | |||
| Six weeks after surgery | 2.6±0.2 | 11.9±0.4 | 11.15 - 12.56 | <0.001 |
| Six months after surgery | 1.0±0.2 | 1.6±0.1 | 1.17 - 2.02 | <0.001 |
| 6MWT (meter) | ||||
| Baseline | 189.9±16.1 | |||
| Six weeks after surgery | 272.6±11.2 | -82.7±9.2 | -101.15 - -64.24 | <0.001 |
| Six months after surgery | 326.2±12.4 | -53.5±4.8 | -63.15 - -43.92 | <0.001 |
| IPAQ-SF (MET-min/week) | ||||
| Baseline | 953.2±139.0 | |||
| Six weeks after surgery | 2,125.6±165.6 | -1,172.4±146.0 | -1,465.87 - -879.01 | <0.001 |
| Six months after surgery | 2,870.8±229.7 | -695.170±164.7 | -1,020.10 - -364.23 | <0.001 |
| Step counts | ||||
| Baseline | 4,091.5±235.9 | -2,600.02 - -1,045.65 | ||
| Six weeks after surgery | 5,914.4±400.9 | -1,822.8±386.7 | -1,579.14 - -778.73 | <0.001 |
| Six months after surgery | 7,093.3±488.9 | -1,178.9±199.2 | <0.001 | |
| SD: Standard deviation; SE: Standard error; CI: Confidence interval; 6MWT: Six-minute walking test; IPAQ-SF: International Physical Activity Questionnaire-Short Form; * p value for baseline and at six weeks after surgery; ** p value at six weeks and six months after surgery. | ||||
The physical activity using the IPAQ-SF and physical capacity using the 6MWT at three endpoint times were compared between the patient and control groups. Both baseline scores (IPAQ-SF and 6MWT) were lower in the patients compared to the controls, although there was no significant difference at six weeks and six months (Table 3).
Table 3. Physical activity and capacity difference between patients and controls.
| Patients with THA (n=50) | Controls (n=50) | p | |
| Mean±SD | Mean±SD | ||
| IPAQ-SF (MET-min/week) | |||
| Baseline | 953.2±139.0 | 2,507.2±142.9 | <0.001 |
| Sixth week | 2,125.6±165.6 | 0.115 | |
| Sixth month | 2,870.8±229.7 | 0.481 | |
| 6MWT (meter) | |||
| Baseline | 189.9±16.1 | 335.5±14.3 | <0.001 |
| Sixth week | 272.6±11.2 | 0.112 | |
| Sixth month | 326.2±12.4 | 0.589 | |
| THA: Total hip arthroplasty; SD: Standard deviation; IPAQ-SF: International Physical Activity Questionnaire-Short Form; MET: Metabolic equivalent of task; 6MWT: Six-minute walking test. | |||
In patients with THA, socio-demographic characteristics and baseline functional status which may affect the physical function and physical capacity at six months after surgery were evaluated using the multivariate logistic regression analysis. Physical function was assessed in two groups: (i) patients with no pain and no disability (Lequesne Index score was 0) and (ii) patients with mild-to- moderate functional impairment (Lequesne Index score was 1-7). Physical capacity was assessed in two groups according to the walking distance was <300 meters and ≥300 meters (6MWT results). Variables including age, sex, BMI, comorbidities, working status, living with a partner, baseline Lequesne Index scores, and walking distance were assessed using the univariate analysis and at least moderately significant variables were included in the multivariate analysis. A significant correlation was found between the Lequesne Index scores, and age, comorbidity, and baseline Lequesne scores, while age and baseline walking distance were found to be correlated with the 6MWT (Table 4).
Table 4. Multiple logistic regression analysis showing the association between Lequesne Index scores and 6MWT and risk factors.
| B | SE | p | 95% CI | |
|
Lequesne Index score 2* (Patients with mild to moderate functional impairment) |
||||
| Constant | -5.088 | 1.950 | 0.009 | 1.024-1.197 |
| Age | 0.102 | 0.040 | 0.011 | 1.151-1.936 |
| Baseline Lequesne | 0.401 | 0.133 | 0.003 | 0.831-1.082 |
| Body mass index | 0.053 | 0.067 | 0.428 | 1.094-19.522 |
| Presence of co-morbidity | 1.531 | 0.735 | 0.037 | |
| 6MWT | ||||
| 2** (walking distance was ≥300 meters) | ||||
| Constant | -0.183 | 2.872 | 0.039 | |
| Age | -0.066 | 0.033 | 0.048 | 0.877-0.999 |
| Baseline 6MWT | 0.018 | 0.005 | 0.001 | 1.007-1.029 |
| Body mass index | 0.133 | 0.081 | 0.100 | 0.975-1.339 |
| 6MWT: Six-minute walking test; SE: Standard error; CI: Confidence interval; * The reference category is: 1.00 (no pain and no disability, Lequesne Index score was 0); ** The reference category is: 1.00 (6MWT results <300 meters). | ||||
Discussion
The aim of the current study was to assess the improvement of physical activity and capacity with objective measurements and self-reported questionnaires after THA at an earlier endpoint, compared to previous studies. The results confirmed our first hypothesis that patients benefited from surgery and they had similar physical activity and capacity with the age- and sex-matched controls at the postoperative sixth week and month. In addition, our second hypothesis regarding that preoperative physical function/capacity values and several socio-demographic factors would be effective on the outcomes of THA was also supported. Multivariate logistic regression analysis revealed that baseline physical function/capacity values and age were effective on both physical function and capacity along with the presence of comorbid disease which increased the functional impairment.
Total hip arthroplasty is a frequently performed procedure in orthopedic surgery. Outcomes of THA have been assessed with pain, function, physical capacity, and health-related quality of life parameters.[19-21] Measurement of pain after THA is a challenging task, as all data about pain after surgery is dependent on the definition of the pain and when to measure it. Failure or complications of surgery is not necessarily the cause of postoperative pain experienced by THA patients. Many factors come into play and, thus, standardization of postoperative pain measurements regarding duration, frequency, character, and time of measurement is a necessary step in evaluating etiologies of pain and its management course. Most studies reporting pain after THA have demonstrated a significant reduction in pain levels. Fletcher et al.[22] reported moderate-to-severe chronic residual pain levels in less than 12% of patients. Wylde et al.[23] also reported severe persistent pain in only 6% of patients. This is consistent with our study showing a 63% reduction in the NRS after six weeks and this ratio was improved to 89.6% at six months.
Total hip arthroplasty provides older patients with the chance to be treated cost-effectively and improving physical function for the rest of their life. In a review by Jones et al.[20] reported that functional independence was a key factor in the postoperative recovery and added that functional gains appeared after than pain reduction. Similarly, Ritter et al.[24] reported the same conclusion regarding physical function at six months, one year, and two years. In contrast, some authors reported that physical function in THA patients did not improve after surgery, but even became worse. These authors who reached the same conclusion interpreted it as an effect of the other musculoskeletal comorbidities in these patients.[6,25-27] Another comment regarding the functional benefit of the patient after joint surgery is that functional improvement is associated with the patient's expectations. It was reported that expectations were not correlated with preoperative functional health status and expectation of complete pain relief after surgery was an independent predictor of improved physical function at six months after surgery.[28] In our study, all patients were assessed by the Lequesne Index as severely impaired before surgery; however, at six weeks, which is early compared to other studies, we found that all patients regressed to the mild impairment category. A total of 25 (50%) of the patients had no disability according to the Lequesne Index scores at six months, supporting more functional recovery over time. On the other hand, rapid improvement of functional status may depend on the fact that patients with more functional impairment refuse to participate in the study.
Physical activity after THA must be designed according to the patient’s need and lifestyle. Avoiding contact sports and high joint loading activities are necessary also in preventing postoperative complications.[29] In the present study, we assessed physical activity levels after surgery using the 6MWT, IPAQ-SF, and step count monitor. Our patients showed a significant increase in the distance walked, activity score, and steps per day as early as six weeks.
Expected daily step count in a healthy adult is 6,000 to 8,500.[30] Our patients’ preoperative daily step count was 4,090 which is less than expected. At six weeks, after THA step count increased to almost 5,900, but still below expected. At six months, the patients reached nearly 7,000 steps which are in the range of healthy older adults and above expected values for the disabled. This is consistent with previous studies by Fujita et al.[31] and Kinkel et al.[32] where they found an increase in the walking cycles at six months and one year.
The 6MWT measures the walking capacity objectively and gives information about walking speed endurance and ability to routinely walk. Previous studies indicated a significant improvement in the 6MWT after THA at three/six months and one year.[33-37] In accordance with the previous data, we found that 6MWT results had significant improvement at six months; however, we found that there was a significant increase in the results of the sixth week as an early measurement. Moreover, the 6MWT results were compared with age- and sex-matched controls and we found that the patients with THA were able to reach scores of controls even at six weeks. Pain, the main symptom of OA and the main indication of the operation, had also an effect on physical capacity and function. Therefore, pain relief after surgery was thought to be effective in early physical capacity increase.
Self-reported physical activity as well as objectively calculated step count or walking distance has presented considerable changes before and after the orthopedic surgery. In a similar way, Alvarez et al.[38] showed that the IPAQ score had a moderate positive correlation with accelerometers. A study from Japan also revealed that patients had improved light and moderate physical activities after THA at six and 12 months.[31] Their results supported that 12-month physical activity scores of patients which were similar with age-matched controls, while controls had higher physical activity levels at six months and before surgery. In our study, the patients’ total MET-min/week scores increased after surgery at six weeks and six months based on the results of objective physical activity parameters. Compared to the controls, we found no significant difference at six weeks and six months, although the patients’ values were worse at the beginning. Improvement in pain levels and increased walking capacity may have changed the patients’ perception and assured them to be more confident about performing different activities. The fact that patients who volunteered to participate in the study and relieved for pain would be motivated to increase the physical activity. As a consequence, this motivation may have affected the early increase in physical activity.
Despite improved technical procedures in THA surgery, some patients still complain of pain and functional deficits regarding the outcomes after THA. Therefore, predicting the indicators of good outcomes after the operation has come into prominence and has attracted the attention.[39] In this way, the appropriate patient selection for surgery may be facilitated. In a study investigating the type of surgery as a factor affecting postoperative outcomes, the results were similar between the direct anterior approach and the other surgical approaches.[36] In a study by Tilbury et al.,[40] which examined the factors affecting functional outcomes after THA, socio-demographic data, preoperative function, and preoperative patients’ expectancy were evaluated. The authors found that improved preoperative function and expectancy were associated with better outcomes, while BMI negatively affected the functional outcomes. However, Weber et al.[39] found no significant relationship between age, sex, BMI, and good response to THA, while they reported that preoperative patient-reported functional outcomes seemed to be a predictor for postoperative responses. In a similar study, preoperative functional status referred as an effective factor for postoperative outcomes.[27] In the present study, we assessed the predictors for postoperative function and physical capacity. Consistent with the literature, our results supported that preoperative measurements were associated with postoperative Lequesne Index scores and 6MWT results. Age, one of socio-demographic characteristics, was found to be effective on both function and physical capacity, while the presence of comorbid disease was associated with the Lequesne Index scores. Although it is expected that age and systemic comorbid diseases would decrease walking distance and increase functional disability, it would be useful to analyze our preliminary results in studies with a larger patient size.
To the best of our knowledge, this is the first study to evaluate changes in pain, physical function, capacity, and activity using both subjective and objective measures as early as six weeks after THA. However, our study has some limitations that need to be reported. The small sample size is main limitation. We excluded patients with advanced pulmonary and cardiovascular diseases which could have decreased the patients’ walking capacity. Short period use of the step count monitor was another limitation of this study. Some patients spent an extra-effort to walk more than their actual capacity, as they were motivated to meet their physicians’ expectations. Therefore, selection bias may have occurred in the present study.
In conclusion, patients with OA showed significantly decreased pain levels and improved physical function and activity as early as six weeks and up to six months after THA surgery and they had similar physical activity and capacity with the age- and sex-matched controls at the postoperative sixth month. Preoperative values and age were the positive predictors of improved postoperative function and physical capacity. However, further large-scale, prospective studies are needed to confirm these findings.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1.GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73:1323–1330. doi: 10.1136/annrheumdis-2013-204763. [DOI] [PubMed] [Google Scholar]
- 3.Hunter DJ. Focusing osteoarthritis management on modifiable risk factors and future therapeutic prospects. Ther Adv Musculoskelet Dis. 2009;1:35–47. doi: 10.1177/1759720X09342132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Skou ST, Roos EM, Laursen MB, Rathleff MS, Arendt-Nielsen L, Simonsen O, et al. A randomized, controlled trial of total knee replacement. N Engl J Med. 2015;373:1597–1606. doi: 10.1056/NEJMoa1505467. [DOI] [PubMed] [Google Scholar]
- 5.Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis. A systematic review of prospective studies in unselected patients. e000435BMJ Open. 2012;2 doi: 10.1136/bmjopen-2011-000435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nilsdotter AK, Isaksson F. Patient relevant outcome 7 years after total hip replacement for OA - a prospective study. BMC Musculoskelet Disord. 2010;11:47–47. doi: 10.1186/1471-2474-11-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sylvia LG, Bernstein EE, Hubbard JL, Keating L, Anderson EJ. Practical guide to measuring physical activity. J Acad Nutr Diet. 2014;114:199–208. doi: 10.1016/j.jand.2013.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silva M, McClung CD, Dela Rosa MA, Dorey FJ, Schmalzried TP. Activity sampling in the assessment of patients with total joint arthroplasty. J Arthroplasty. 2005;20:487–491. doi: 10.1016/j.arth.2004.08.013. [DOI] [PubMed] [Google Scholar]
- 9.Kohn MD, Sassoon AA, Fernando ND. Classifications in Brief: Kellgren-Lawrence classification of osteoarthritis. Clin Orthop Relat Res. 2016;474:1886–1893. doi: 10.1007/s11999-016-4732-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jensen MP, Turner JA, Romano JM, Fisher LD. Comparative reliability and validity of chronic pain intensity measures. Pain. 1999;83:157–162. doi: 10.1016/s0304-3959(99)00101-3. [DOI] [PubMed] [Google Scholar]
- 11.Lequesne MG, Samson M. Indices of severity in osteoarthritis for weight bearing joints. J Rheumatol Suppl. 1991;27:16–18. [PubMed] [Google Scholar]
- 12.Basaran S, Guzel R, Seydaoglu G, Guler-Uysal F. Validity, reliability, and comparison of the WOMAC osteoarthritis index and Lequesne algofunctional index in Turkish patients with hip or knee osteoarthritis. Clin Rheumatol. 2010;29:749–756. doi: 10.1007/s10067-010-1398-2. [DOI] [PubMed] [Google Scholar]
- 13.Kennedy DM, Stratford PW, Wessel J, Gollish JD, Penney D. Assessing stability and change of four performance measures: a longitudinal study evaluating outcome following total hip and knee arthroplasty. BMC Musculoskelet Disord. 2005;6:3–3. doi: 10.1186/1471-2474-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Takenaga RK, Callaghan JJ, Bedard NA, Liu SS, Gao Y. Which functional assessments predict long-term wear after total hip arthroplasty. Clin Orthop Relat Res. 2013;471:2586–2594. doi: 10.1007/s11999-013-2968-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ko V, Naylor JM, Harris IA, Crosbie J, Yeo AE. The six-minute walk test is an excellent predictor of functional ambulation after total knee arthroplasty. BMC Musculoskelet Disord. 2013;14:145–145. doi: 10.1186/1471-2474-14-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Naylor JM, Mills K, Buhagiar M, Fortunato R, Wright R. Minimal important improvement thresholds for the six-minute walk test in a knee arthroplasty cohort: triangulation of anchor- and distribution-based methods. BMC Musculoskelet Disord. 2016;17:390–390. doi: 10.1186/s12891-016-1249-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saglam M, Arikan H, Savci S, Inal-Ince D, Bosnak-Guclu M, Karabulut E, et al. International physical activity questionnaire: reliability and validity of the Turkish version. Percept Mot Skills. 2010;111:278–284. doi: 10.2466/06.08.PMS.111.4.278-284. [DOI] [PubMed] [Google Scholar]
- 18.Bassett DR Jr, Toth LP, LaMunion SR, Crouter SE. Step counting: A review of measurement considerations and health-related applications. Sports Med. 2017;47:1303–1315. doi: 10.1007/s40279-016-0663-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weber M, Craiovan B, Woerner ML, Schwarz T, Grifka J, Renkawitz TF. Predictors of outcome after primary total joint replacement. J Arthroplasty. 2018;33:431–435. doi: 10.1016/j.arth.2017.08.044. [DOI] [PubMed] [Google Scholar]
- 20.Jones CA, Beaupre LA, Johnston DW, Suarez-Almazor ME. Total joint arthroplasties: current concepts of patient outcomes after surgery. Rheum Dis Clin North Am. 2007;33:71–86. doi: 10.1016/j.rdc.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 21.Naili JE, Hedström M, Broström EW. Changes of and interrelationships between performance-based function and gait and patient-reported function 1 year after total hip arthroplasty. J Orthop Traumatol. 2019;20:14–14. doi: 10.1186/s10195-019-0521-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fletcher D, Stamer UM, Pogatzki-Zahn E, Zaslansky R, Tanase NV, Perruchoud C, et al. Chronic postsurgical pain in Europe: An observational study. Eur J Anaesthesiol. 2015;32:725–734. doi: 10.1097/EJA.0000000000000319. [DOI] [PubMed] [Google Scholar]
- 23.Wylde V, Hewlett S, Learmonth ID, Dieppe P. Persistent pain after joint replacement: prevalence, sensory qualities, and postoperative determinants. Pain. 2011;152:566–572. doi: 10.1016/j.pain.2010.11.023. [DOI] [PubMed] [Google Scholar]
- 24.Ritter MA, Albohm MJ, Keating EM, Faris PM, Meding JB. Comparative outcomes of total joint arthroplasty. J Arthroplasty. 1995;10:737–741. doi: 10.1016/s0883-5403(05)80068-3. [DOI] [PubMed] [Google Scholar]
- 25.Nilsdotter AK, Petersson IF, Roos EM, Lohmander LS. Predictors of patient relevant outcome after total hip replacement for osteoarthritis: a prospective study. Ann Rheum Dis. 2003;62:923–930. doi: 10.1136/ard.62.10.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fortin PR, Clarke AE, Joseph L, Liang MH, Tanzer M, Ferland D, et al. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999;42:1722–1728. doi: 10.1002/1529-0131(199908)42:8<1722::AID-ANR22>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 27.Röder C, Staub LP, Eggli S, Dietrich D, Busato A, Müller U. Influence of preoperative functional status on outcome after total hip arthroplasty. J Bone Joint Surg [Am] 2007;89:11–17. doi: 10.2106/JBJS.E.00012. [DOI] [PubMed] [Google Scholar]
- 28.Mahomed NN, Liang MH, Cook EF, Daltroy LH, Fortin PR, Fossel AH, et al. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. J Rheumatol. 2002;29:1273–1279. [PubMed] [Google Scholar]
- 29.Vogel LA, Carotenuto G, Basti JJ, Levine WN. Physical activity after total joint arthroplasty. Sports Health. 2011;3:441–450. doi: 10.1177/1941738111415826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hammett T, Simonian A, Austin M, Butler R, Allen KD, Ledbetter L, et al. Changes in physical activity after total hip or knee arthroplasty: A systematic review and meta- analysis of six- and twelve-month outcomes. Arthritis Care Res (Hoboken) 2018;70:892–901. doi: 10.1002/acr.23415. [DOI] [PubMed] [Google Scholar]
- 31.Fujita K, Makimoto K, Tanaka R, Mawatari M, Hotokebuchi T. Prospective study of physical activity and quality of life in Japanese women undergoing total hip arthroplasty. J Orthop Sci. 2013;18:45–53. doi: 10.1007/s00776-012-0318-5. [DOI] [PubMed] [Google Scholar]
- 32.Kinkel S, Wollmerstedt N, Kleinhans JA, Hendrich C, Heisel C. Patient activity after total hip arthroplasty declines with advancing age. Clin Orthop Relat Res. 2009;467:2053–2058. doi: 10.1007/s11999-009-0756-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.de Groot IB, Bussmann HJ, Stam HJ, Verhaar JA. Small increase of actual physical activity 6 months after total hip or knee arthroplasty. Clin Orthop Relat Res. 2008;466:2201–2208. doi: 10.1007/s11999-008-0315-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Laupacis A, Bourne R, Rorabeck C, Feeny D, Wong C, Tugwell P, et al. The effect of elective total hip replacement on health-related quality of life. J Bone Joint Surg [Am] 1993;75:1619–1626. doi: 10.2106/00004623-199311000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Heiberg KE, Ekeland A, Bruun-Olsen V, Mengshoel AM. Recovery and prediction of physical functioning outcomes during the first year after total hip arthroplasty. Arch Phys Med Rehabil. 2013;94:1352–1359. doi: 10.1016/j.apmr.2013.01.017. [DOI] [PubMed] [Google Scholar]
- 36.Jelsma J, Pijnenburg R, Boons HW, Eggen PJ, Kleijn LL, Lacroix H, et al. Limited benefits of the direct anterior approach in primary hip arthroplasty: A prospective single centre cohort study. J Orthop. 2016;14:53–58. doi: 10.1016/j.jor.2016.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jeldi AJ, Deakin AH, Allen DJ, Granat MH, Grant M, Stansfield BW. Total Hip Arthroplasty Improves Pain and Function but Not Physical Activity. J Arthroplasty. 2017;32:2191–2198. doi: 10.1016/j.arth.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 38.Alvarez A, Domenech J, Valverde-Mordt C, Lison JF. Correlation between the level of physical activity as measured by accelerometer and the Harris Hip Score. Hip Int. 2015;25:461–465. doi: 10.5301/hipint.5000245. [DOI] [PubMed] [Google Scholar]
- 39.Weber M, Zeman F, Craiovan B, Thieme M, Kaiser M, Woerner M, et al. Predicting Outcome after Total Hip Arthroplasty: The Role of Preoperative Patient-Reported Measures. Biomed Res Int. 2019;2019:4909561–4909561. doi: 10.1155/2019/4909561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tilbury C, Haanstra TM, Verdegaal SHM, Nelissen RGHH, de Vet HCW, Vliet Vlieland, et al. Patients' pre- operative general and specific outcome expectations predict postoperative pain and function after total knee and total hip arthroplasties. Scand J Pain. 2018;18:457–466. doi: 10.1515/sjpain-2018-0022. [DOI] [PubMed] [Google Scholar]