Abstract
Objectives
The aim of this study was to investigate the effect of virtual reality (VR) therapy on motor and functional development in children with cerebral palsy (CP).
Patients and methods
In this single-blind, prospective, randomized-controlled study, a total of 41 patients (28 males, 13 females; mean age 8.49 years; range, 5 to 15 years) receiving inpatient treatment for CP were included between April 2009 and September 2009. The patients were randomly divided into two groups as the study group (n=21) and control group (n=20). Neurophysiological and conventional treatment methods, and occupational therapy were applied to all patients. In addition, a total of 12 VR therapy sessions for one hour were administered three days a week for four weeks to the study group. Before and after treatment, the Bimanual Fine Motor Function (BFMF) test was performed to measure hand functioning, Gross Motor Function Classification System (GMFCS) for functional levels, and Functional Mobility Scale (FMS) for mobility.
Results
There was a significant increase in the BFMF, GMFCS, and FMS scores after treatment, compared to baseline values in the study group (p<0.05). There was a statistically significant results in favor of the study group for all parameters after treatment compared to pre-treatment values (p<0.05).
Conclusion
Our study results indicate that VR therapy is a useful treatment method which can be used in rehabilitation of CP with improved motor function. The addition of this method to conventional rehabilitation techniques may have a significant impact on treatment success.
Keywords: Cerebral palsy, motor function, rehabilitation, virtual reality therapy
Introduction
Motor disorders in cerebral palsy (CP) are usually accompanied by sensory and perceptual problems, cognitive disorders, communication and behavioral problems, epilepsy, and secondary musculoskeletal system problems.[1] Fine motor development in CP includes skills requiring the use of the hands, while gross motor development includes skills requiring gross movements. Fine motor development advances from the ulnar side of the hand to the radial side, while gross motor development follows a cephalocaudal direction, from proximal to distal and from the center to the periphery of the body.[2] A delay in motor development steps is the main finding of CP.
The main goals of rehabilitation in CP are to correct abnormal posture and patterns, to prevent any deformities, to improve existing skills, to gain new skills, to enable functional use of the upper extremities, to provide gait training, and to gain comprehensible speech.[3] Rehabilitation methods in children with CP have mostly focused on the lower extremity and ambulation; however, new treatment approaches are needed to improve upper extremity functions. Therefore, virtual reality (VR) therapy has been recently used in children with CP to improve motor performance.[4,5] It is a computer technology which allows the user to create conditions and objects in a virtual environment.[6,7] It creates an exercise environment which can be applied through positive visual and sensory feedback and can be used fully and systematically for individual study during motor learning in many environments that seem almost natural.[8,9] The VR also provides three-dimensional spatial consistency between the degree of movement in the real world setting and the degree of movement seen on the computer screen. Such spatial presentation enables visual feedback related to performance and guidance information which is critical for motor learning in children with CP.[7,8]
The VR provides significant gains in functional motor skills by increasing cortical reorganization and neuroplastic changes.[9] The biofeedback during VR therapy is multimodal, as it uses sensory and cognitive functions simultaneously, and it is also entertaining, interesting, motivating, and easy to understand.[10] Virtual reality therapy has a high rehabilitation potential. It enables adaptation to the real world. Computers have endless patience and consistency, and many things which seem to be impossible to perform in the real world can be performed in a computer environment.[11]
Eligible patients for VR therapy are those having lack of any visual or auditory problems, adequate cognitive function, adequate cooperation and motivation, lack of any significant joint contracture that would prevent the exercises, and lack of severe spasticity.[9] Virtual reality therapy can be used in many fields such as posture and balance rehabilitation, motor rehabilitation in hemiplegia and CP, rehabilitation of spinal cord injuries, cognitive rehabilitation, autism, panic attack and phobia treatment, attention deficit syndrome and pain treatment, fetal alcohol syndrome, and the treatment of visual disorders such as amblyopia and sensory auditory disturbances.[11,12]
In the present study, we aimed to evaluate the effect of VR therapy on functional development in children with CP.
Patients and Methods
This single-blind, prospective, randomized- controlled study was conducted at Ankara Physical Therapy and Rehabilitation Training and Research Hospital between April 2009 and September 2009. Initially, a total of 60 CP patients who were under inpatient treatment in the rehabilitation program were screened for eligibility. Inclusion criteria were as follows: (i) age between 5 and 15 years, (ii) being able to cooperate and being motivated, and (iii) having sitting balance and normal upper extremity passive range of motion (PROM) (i.e., patients without limitation of shoulder, elbow and wrist range of motion). Exclusion criteria were as follows: (i) having visual or auditory problems, (ii) having severe spasticity (an Ashworth spasticity score of 4 in any upper or lower extremities), (iii) having severe mental retardation, (iv) having prior surgery for spasticity within the past three months, (v) having botulinum toxin injection within the past three months. Among 46 eligible patients, a total of 41 patients (28 males, 13 females; mean age 8.49 years; range, 5 to 15 years) who completed the study were included. A written informed consent was obtained from each parent. The study protocol was approved by the Ankara Physical Therapy and Rehabilitation Training and Research Hospital Local Ethics Committee. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Data including age, sex, and etiological factors (prenatal, natal, postnatal) were recorded for all patients on admission. A detailed physical and neurological examination was performed, and the type of CP was identified. The Ashworth scale[13] was used to evaluate spasticity in the upper and lower extremities. The manual functions were evaluated using the Bimanual Fine Motor Function (BFMF) test,[14] functional level by the Gross Motor Function Classification System (GMFCS),[15] and mobility by the Functional Mobility Scale (FMS)[16] before and after treatment.
Randomization
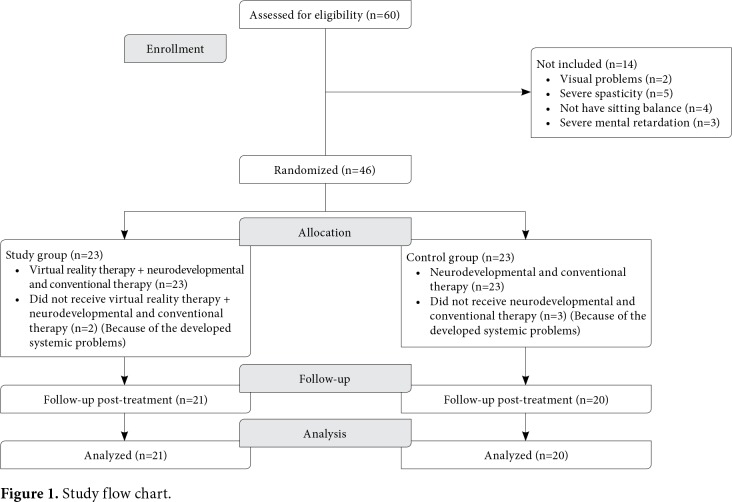
The patients were randomly divided into two groups using a random number table. Group 1 (study group, n=21) received neurophysiological, conventional treatment methods, occupational therapy, and VT therapy. Group 2 (control group) (n=20) received neurophysiological, conventional treatment methods, and occupational therapy. The study flow chart is shown in Figure 1.
Figure 1. Study flow chart.
Interventions
All patients received neurophysiological and conventional treatment methods five times a day by a physiotherapist. Occupational therapy was administered to all patients by the hospital's occupational therapist. In addition to these treatments, the study group also played with the Sony PlayStation 2 EyeToy for an hour three days a week for four weeks for a total of 12 sessions (1-hour sessions).
The EyeToy Game System: The commercial EyeToy Game VT System (Sony Computer Entertainment Inc., London, UK) consists of a camera, a 37-inch TV, EyeToy Game CD and PlayStation 2. The children are able to see themselves on the television screen with this system thanks to the camera and therefore to interact more easily with the virtual objects and events. The games are presented in a random manner without any particular order. In our study, patients attempted to play sports games (basketball, swimming, tennis, etc.) in the EyeToy game system by watching themselves on the television screen and moving their hands and feet in the sitting position in front of the television (Figures 2 and 3).
Figure 2. An image of application of virtual reality system from the side view.
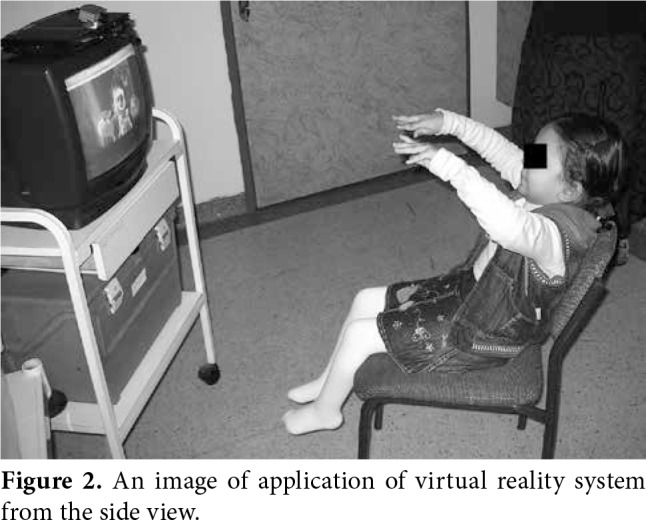
Figure 3. An image of application of virtual reality system from the back view.
Statistical analysis The post-hoc power analysis was performed using the G*Power version 3.1.9.2 software (Heinrich-Heine- Universität Düsseldorf, Düsseldorf, Germany). The GMFCS post-treatment values were found to have an effect size of 1.195. The study power was calculated as 0.96 for α=0.05 with a sample size of 21 in the study group and of 20 in the control group.
Statistical analysis was performed using the SPSS version 15.0 software (SPSS Inc., Chicago, IL, USA). Descriptive data were expressed in mean ± standard deviation (SD), median (min-max), or number and frequency. Categorical comparisons were performed using the chi-square and Fisherʹs exact tests. Normal distribution of the data was analyzed using the Shapiro-Wilk test. For normally distributed data, independent samples t-test was used for inter-group comparisons and paired sample test was used for intra-group comparisons. Non-parametric tests were used to examine parameters (Wilcoxon test for intra- group analysis and Mann-Whitney U test for inter- group analysis). A p value of 0.05 was considered statistically significant.
Results
Demographic and clinical characteristics of the patients and controls including age, sex, inpatient treatment duration, upper and lower extremity spasticity, and type of CP according to the muscle tone disorder and the affected part of the body are shown in Table 1. There was no statistically significant difference in the demographic and clinical characteristics between the two groups (p>0.05) (Table 1).
Table 1. Demographic and clinical characteristics of patients.
| Study group (n=21) | Control group (n=20) | p | |||||
| n | % | Mean±SD | n | % | Mean±SD | ||
| Age (year) | 8.8±2.5 | 8.2±1.8 | 0.342 | ||||
| Sex | 0.824 | ||||||
| Male | 14 | 14 | |||||
| Female | 7 | 6 | |||||
| Inpatient treatment duration (days) | 49.9±13.4 | 49.2±12.7 | 0.863 | ||||
| Upper extremity | 0.574 | ||||||
| Normal | 9 | 42.9 | 10 | 50 | |||
| Ashworth 1 | 8 | 38.1 | 6 | 50 | |||
| Ashworth 2 | 2 | 9.5 | 4 | 20 | |||
| Ashworth 3 | 2 | 9.5 | 0 | 0 | |||
| Lower extremity | 0.165 | ||||||
| Normal | 5 | 23.8 | 5 | 25 | |||
| Ashworth 1 | 6 | 28.6 | 9 | 45 | |||
| Ashworth 2 | 5 | 23.8 | 6 | 30 | |||
| Ashworth 3 | 5 | 23.8 | 0 | 0 | |||
| CP type according to muscle tone | 0.367 | ||||||
| Spastic | 20 | 95.2 | 19 | 95.0 | |||
| Dyskinetic athetoid | 1 | 4.8 | - | 0 | |||
| Mixed | - | 0 | 1 | 5 | |||
| CP type according to affected part of the body | 0.143 | ||||||
| Diplegia | 15 | 71.4 | 12 | 60 | |||
| Quadriplegia | 5 | 23.8 | 4 | 20 | |||
| Triplegia | 1 | 4.8 | - | 0 | |||
| Hemiplegia | - | 0 | 4 | 20 | |||
| SD: Standard deviation; CP: Cerebral palsy; Independent samples t-test, chi-square test, and Fisher’s exact test were used; p<0.05 statistically significant. | |||||||
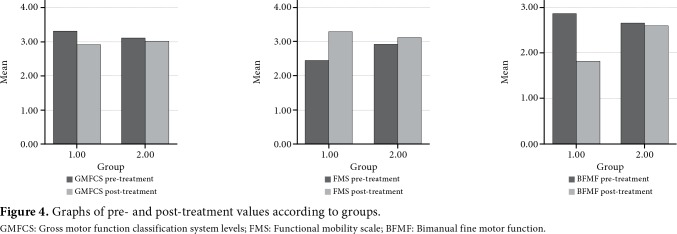
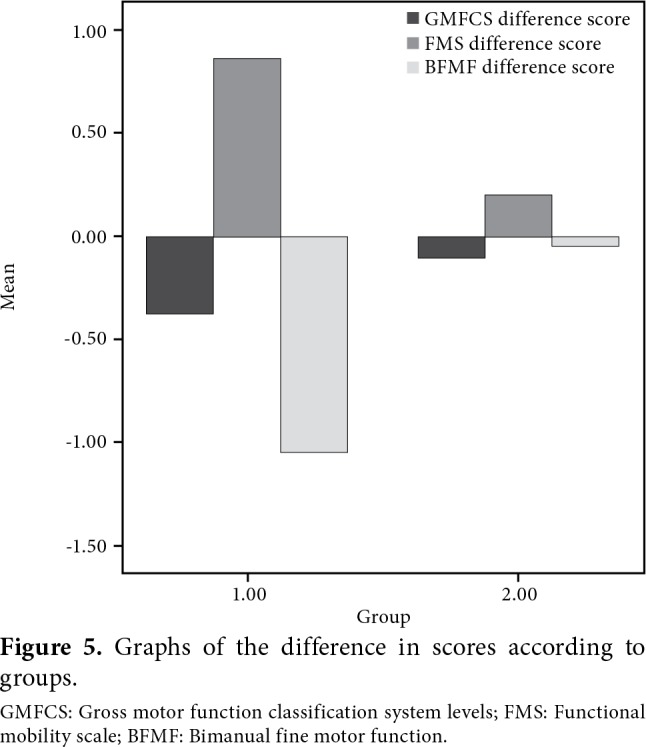
In addition, there was no statistically significant difference between the study and control groups in terms of the BFMF, GMFCS and FMS scores (p>0.05) before treatment. However, we found a statistically significant increase in the post-treatment BFMF, GMFCS, and FMS scores, compared to the pre-treatment values, in the study group (p<0.05) (Table 2; Figure 4). On the other hand, there was no statistically significant difference in the post-treatment values compared to the pre-treatment values in the control group (p>0.05) (Table 2). For the comparison of post-treatment values between the groups, there was a statistically significant difference in the BFMF scores in favor of the study group (p<0.05), while there was no statistically significant difference in the other variables (p>0.05) (Table 2). Inter-group comparison showed statistically significant superior results in the study group for all variables after treatment (p<0.05) (Table 3; Figure 5).
Table 2. Comparison of pre- and post-treatment values within the groups and between the groups.
| Study group (n=21) | Control group (n=20) | p | |||
| Median | Min-Max | Median | Min-Max | ||
| BFMF pre-treatment | 3 | 2-4 | 2,5 | 2-4 | 0,236 |
| BFMF post-treatment | 2 | 1-3 | 2,5 | 2-4 | 0.001* |
| p | <0.001* | 0,317 | |||
| GMFCS pre-treatment | 3 | 2-4 | 3 | 2-4 | 0,434 |
| GMFCS post-treatment | 3 | 2-4 | 3 | 2-4 | 0,673 |
| p | 0.005* | 0,157 | |||
| FMS pre-treatment | 2 | 1-5 | 3 | 1-5 | 0,395 |
| FMS post-treatment | 2,5 | 1-5 | 3 | 1-5 | 0,676 |
| p | 0.002* | 0,336 | |||
| Min-Minimum; Max: Maximum; BFMF: Bimanual fine motor function; GMFCS: Gross motor function classification system levels; FMS: Functional mobility scale; Wilcoxon test was used for intragroup analysis and Mann Whitney U test was used for intergroup analysis (shown in bold); * p<0.05 was assumed to be significant. | |||||
Table 3. Comparison of the differences in scores between the groups.
| W2-W0 | |||
| n | Median | Min-Max | |
| BFMF | |||
| Study group | 21 | -1 | -2 / -1 |
| Control group | 20 | 0 | -1 / 0 |
| p | <0.001* | ||
| GMFCS | |||
| Study group | 21 | 0 | -1 / 0 |
| Control group | 20 | 0 | -1 / 0 |
| p | 0.039* | ||
| FMS | |||
| Study group | 21 | 1 | 0 / 2 |
| Control group | 20 | 0 | -2 / 3 |
| p | 0.020* | ||
| Min-Minimum; Max: Maximum; BFMF: Bimanual fine motor function; GMFCS: Gross motor function classification system levels; FMS: Functional mobility scale; Mann Whitney U test was used for intergroup analysis; * p<0.05 statistically significant. | |||
Figure 4. Graphs of pre- and post-treatment values according to groups. GMFCS: Gross motor function classification system levels; FMS: Functional mobility scale; BFMF: Bimanual fine motor function.
Figure 5. Graphs of the difference in scores according to groups. GMFCS: Gross motor function classification system levels; FMS: Functional mobility scale; BFMF: Bimanual fine motor function.
Discussion
In the present study, we investigated the effect of VR therapy on functional development in children with CP. Our study results showed that there was a significant improvement in the function and mobility in the CP patients receiving VR therapy.
Virtual reality therapy is a rehabilitation technique which has been attempted in recent years and mostly targets the upper extremity. It has been postulated to have the potential to improve hand-eye coordination and skill-requiring daily living activities, by increasing sensory and cognitive performance and enabling the functional use of the upper extremities for the child.[9] In a case report, You et al.[9] reported that VR therapy was associated with significant gains in motor skills by increasing cortical reorganization and neuroplastic changes in an eight-year-old child with hemiparetic CP. Children can be encouraged to exercise, while having fun in VT with this treatment, and more prominent results can be obtained.
There are few studies in the literature evaluating the effect of VR therapy on upper extremity function in children with CP.[10,17-20] Chen et al.[17] used VR therapy in their study in four spastic children with CP. The evaluation was performed with reaching for objects and the Peabody Developmental Motor Scales-Second Edition tests. They observed a favorable functional development in children with normal cognition and good cooperation and reported that effectiveness of this treatment was also maintained afterwards. Reid[10] also applied VR playing-based intervention therapy in three children in 90-min sessions twice a week for four weeks. They evaluated the patients using the Canadian Occupational Performance Measure (COPM). Group scores on the COPM indicated clinically significant changes in self-efficacy for all children. Two of the patients demonstrated the highest changes in both perceived performance abilities and satisfaction with performance in terms of the task-specific domains. Qualitative comments from the patients revealed a high degree of motivation, interest, and pleasure. The results of our study are consistent with those reported by Chen et al.[17] and Reid.[10] As one of the advantages, our study has a larger sample size with a control group.
In their study, Frascarelli et al.[18] used a robot- mediated therapy similar to the method we used in our study and found robotic treatment to be a beneficial treatment using the Melbourne and Fugl-Meyer scales in 12 children with upper extremity problems aged three to 15 years. Fasoli et al.[19] also used upper extremity robotic therapy for 13 hemiplegic children aged eight to 12 years. They used the Quality of Upper Extremity Skills Test and Fugl-Meyer scales for the evaluation and found that robotic treatment may provide new opportunities in children with CP in terms of improvement of upper extremity coordination and functioning. Qiu et al.[20] also evaluated two children with CP aged seven and 10 years using the Melbourne Assessment of Unilateral Upper Limb Function after the administration of robot-assisted virtual rehabilitation during one-hour session three days a week for a total of three weeks. The authors found improved upper extremity functions and concluded that the combination of robotic treatment- enhanced VR therapy was a useful and practical method. Although not as comprehensive as our study, all these studies demonstrate that similar treatment methods applied to upper extremities are beneficial, as assessed by different measurement methods. These studies also show that combined treatment methods would be on the agenda in the near future. In our study, we found an improvement in the BFMF scores in both groups. We also observed a statistically significant improvement in the post-treatment values compared to baseline values in the study group. Of note, we are unable to find any study in the literature evaluating the effect of VR therapy on the upper extremities with BFMF.
Although the aim of our study was to improve the upper extremity motor function, we used the GMFCS test to identify whether VT therapy had a positive effect on the patient and whether it affected gross motor functions including sitting and holding a handheld accessory support or body- supporting walking aids, and changing location. In a review including 34 studies, Clutterbuck et al.[21] evaluated the effects of active exercise on children with CP and concluded that active, performance- focused exercise with variable practice opportunities improved gross motor function in CP. In another study, de Paula et al.[22] investigated the effects of VT therapy on motor function in 25 children with CP using mobile phone games. The authors found a statistically significant improvement in motor development in the study group, compared to the control group, and reported that such games would present new possibilities in the field of rehabilitation. In addition, Massetti et al.[23] reviewed 10 studies to examine the effects of VT therapy on motor function and they concluded that VR therapy provided benefits in motor function and improvements in motor learning with skill transfer to real-life setting by means of VT in children with CP. Similarly, we found statistically significant superior results in the study group in terms of motor function with GMFCS after treatment. We believe that VR therapy directed toward lower extremities would be beneficial in children with CP, as it enables children to exercise while having fun with increased patient compliance to the treatment.
To the best of our knowledge, the present study is the first largest-scale study including a control group to investigate the effect of VR therapy on motor and functional development in children with CP. We believe that VT therapy is a treatment method which can make a positive contribution to motor function in children with CP and that children with CP are able to be motivated and have fun with this method with voluntary exercises.
In a review of 11 studies on VR therapy, Snider and Majnemer[24] analyzed the quality of the study methods using suitable scales and concluded that VR had potential benefits for children with CP and that it particularly had a positive effect on personal factors such as motivation, volition, and interest. Golomb et al.[25] used VT video game tele- rehabilitation therapy via a glove with sensors and found improved hand function, better finger range of motion, increased radial BMD in the plegic arm, and widening activation in the brain motor circuitry in the post-treatment functional magnetic resonance imaging scans in three children with hemiplegic type CP aged 13 to 15 years, who suffered from severe hemiplegia and spasticity. The authors concluded that VR therapy could be effective even in difficult-to-treat patients who were often excluded from clinical studies. Furthermore, Levin et al.[26] reported that VR therapy was a very innovative and potentially effective technology which could be used for the evaluation and as a treatment method for the rehabilitation of adults and children, and that much better rehabilitation results could be obtained with the contribution of VR, compared to conventional approaches. Our results also support the conclusions of Levin et al.[26] who reported that future studies were required to identify whether motor gains and functional improvements obtained through VR could be transferred to the real-world setting. Based on the feedback we obtained from the family members of children with CP, we believe that these patients are able to transfer these gains to their daily lives. However, whether the functional improvement can be maintained in the long-term is still unclear. Further long-term studies would be valuable to evaluate the persistence of the effect of VR therapy. Of note, the PlayStation EyeToy game which we used in our study is inexpensive upon considering the treatment costs, and it is a tool that the families can readily obtain. Patients can also use this treatment method at their home which enables them to perform the exercises in a voluntary, regular, and systematic manner.
The lack of long-term follow-up results is the limitation of this study.
In conclusion, our study results suggest that VR therapy is a useful treatment method which can be used in rehabilitation of CP with improved motor function. The addition of this method to conventional rehabilitation techniques may have a significant impact on treatment success.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1.Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;109:8–14. [PubMed] [Google Scholar]
- 2.Pellegrino L, Dormans JP. Making the diagnosis of cerebral palsy. In: Dormans JP, Pellegrino L, editors. Caring for Children with Cerebral Palsy. Baltimore: Paul H. Brookes Publishing Co.; 1998. pp. 31–55. [Google Scholar]
- 3.Stempien LM, Gaebler-Spira D. Physical Medicine and Rehabilitation. 2. Philadelphia: WB Saunders; 2000. Rehabilitation of children an adults with cerebral palsy; pp. 1191–1212. [Google Scholar]
- 4.Reid D. The use of virtual reality to improve upper ekstremity efficiency skills in children with cerebral palsy: a pilot study. Tech Disabil. 2002;14:53–61. [Google Scholar]
- 5.Reid D. Virtual reality and the person-environment experience. Cyberpsychol Behav. 2002;5:559–564. doi: 10.1089/109493102321018204. [DOI] [PubMed] [Google Scholar]
- 6.Wilson PN, Foreman N, Stanton D. Virtual reality, disability and rehabilitation. Disabil Rehabil. 1997;19:213–220. doi: 10.3109/09638289709166530. [DOI] [PubMed] [Google Scholar]
- 7.Merians AS, Jack D, Boian R, Tremaine M, Burdea GC, Adamovich SV, et al. Virtual reality-augmented rehabilitation for patients following stroke. Phys Ther. 2002;82:898–915. [PubMed] [Google Scholar]
- 8.Sveistrup H, Thornton M, Bryanton C, McComas J, Marshall S, Finestone H, et al. Outcomes of intervention programs using flatscreen virtual reality. Conf Proc IEEE Eng Med Biol Soc. 2004;7:4856–4858. doi: 10.1109/IEMBS.2004.1404343. [DOI] [PubMed] [Google Scholar]
- 9.You SH, Jang SH, Kim YH, Kwon YH, Barrow I, Hallett M. Cortical reorganization induced by virtual reality therapy in a child with hemiparetic cerebral palsy. Dev Med Child Neurol. 2005;47:628–635. [PubMed] [Google Scholar]
- 10.Reid DT. Benefits of a virtual play rehabilitation environment for children with cerebral palsy on perceptions of self- efficacy: a pilot study. Pediatr Rehabil. 2002;5:141–148. doi: 10.1080/1363849021000039344. [DOI] [PubMed] [Google Scholar]
- 11.Parsons TD, Rizzo AA, Rogers S, York P. Virtual reality in paediatric rehabilitation: a review. Dev Neurorehabil. 2009;12:224–238. doi: 10.1080/17518420902991719. [DOI] [PubMed] [Google Scholar]
- 12.Rand D, Katz N, Weiss PL. Intervention using the VMall for improving motor and functional ability of the upper extremity in post stroke participants. Eur J Phys Rehabil Med. 2009;45:113–121. [PubMed] [Google Scholar]
- 13.Bohannon RW, Smith MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther. 1987;67:206–207. doi: 10.1093/ptj/67.2.206. [DOI] [PubMed] [Google Scholar]
- 14.Beckung E, Hagberg G. Neuroimpairments, activity limitations, and participation restrictions in children with cerebral palsy. Dev Med Child Neurol. 2002;44:309–316. doi: 10.1017/s0012162201002134. [DOI] [PubMed] [Google Scholar]
- 15.Palisano RJ, Cameron D, Rosenbaum PL, Walter SD, Russell D. Stability of the gross motor function classification system. Dev Med Child Neurol. 2006;48:424–428. doi: 10.1017/S0012162206000934. [DOI] [PubMed] [Google Scholar]
- 16.Graham HK, Harvey A, Rodda J, Nattrass GR, Pirpiris M. The Functional Mobility Scale (FMS) J Pediatr Orthop. 2004;24:514–520. doi: 10.1097/00004694-200409000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Chen YP, Kang LJ, Chuang TY, Doong JL, Lee SJ, Tsai MW, et al. Use of virtual reality to improve upper-extremity control in children with cerebral palsy: a single-subject design. Phys Ther. 2007;87:1441–1457. doi: 10.2522/ptj.20060062. [DOI] [PubMed] [Google Scholar]
- 18.Frascarelli F, Masia L, Di Rosa G, Cappa P, Petrarca M, Castelli E, et al. The impact of robotic rehabilitation in children with acquired or congenital movement disorders. Eur J Phys Rehabil Med. 2009;45:135–141. [PubMed] [Google Scholar]
- 19.Fasoli SE, Fragala-Pinkham M, Hughes R, Hogan N, Krebs HI, Stein J. Upper limb robotic therapy for children with hemiplegia. Am J Phys Med Rehabil. 2008;87:929–936. doi: 10.1097/PHM.0b013e31818a6aa4. [DOI] [PubMed] [Google Scholar]
- 20.Qiu Q, Ramirez DA, Saleh S, Fluet GG, Parikh HD, Kelly D, et al. The New Jersey Institute of Technology Robot- Assisted Virtual Rehabilitation (NJIT-RAVR) system for children with cerebral palsy: a feasibility study. J Neuroeng Rehabil. 2009;6:40–40. doi: 10.1186/1743-0003-6-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clutterbuck G, Auld M, Johnston L. Active exercise interventions improve gross motor function of ambulant/ semi-ambulant children with cerebral palsy: a systematic review. Disabil Rehabil. 2019;41:1131–1151. doi: 10.1080/09638288.2017.1422035. [DOI] [PubMed] [Google Scholar]
- 22.de Paula JN, de Mello Monteiro CB, da Silva TD, Capelini CM, de Menezes LDC, Massetti T, et al. Motor performance of individuals with cerebral palsy in a virtual game using a mobile phone. Disabil Rehabil Assist Technol. 2018;13:609–613. doi: 10.1080/17483107.2017.1392620. [DOI] [PubMed] [Google Scholar]
- 23.Massetti T, da Silva TD, Ribeiro DC, Malheiros SRP, Ré AHN, Favero FM, et al. Motor learning through virtual reality in cerebral palsy - a literature review. Medical Express. 2014;1:302–306. [Google Scholar]
- 24.Snider L, Majnemer A. Virtual reality: we are virtually there. Phys Occup Ther Pediatr. 2010;30:1–3. doi: 10.3109/01942630903476131. [DOI] [PubMed] [Google Scholar]
- 25.Golomb MR, McDonald BC, Warden SJ, Yonkman J, Saykin AJ, Shirley B, et al. In-home virtual reality videogame telerehabilitation in adolescents with hemiplegic cerebral palsy. Arch Phys Med Rehabil. 2010;91:1–8. doi: 10.1016/j.apmr.2009.08.153. [DOI] [PubMed] [Google Scholar]
- 26.Levin MF, Knaut LA, Magdalon EC, Subramanian S. Virtual reality environments to enhance upper limb functional recovery in patients with hemiparesis. Stud Health Technol Inform. 2009;145:94–108. [PubMed] [Google Scholar]