Abstract
In recent decades, attention has been directed toward the effects of bisphenol A (BPA) on human health. BPA has estrogenic activity and is regarded as a representative endocrine disruptor. In addition, mounting evidence indicates that BPA can disrupt thyroid hormone and its action. This review examined human epidemiological studies to investigate the association between BPA exposure and thyroid hormone levels, and analyzed in vivo and in vitro experiments to identify the causal relationship and its mechanism of action. BPA is involved in thyroid hormone action not only as a thyroid hormone receptor antagonist, but also through several other mechanisms. Since the use of bisphenols other than BPA has recently increased, we also reviewed the effects of other bisphenols on thyroid hormone action.
Keywords: Bisphenol A; Endocrine disruptors; Thyroid hormones; Receptors, thyroid hormone
INTRODUCTION
Bisphenol A (BPA, 4,4′-isopropylidenediphenol) is used to manufacture polycarbonate plastic and epoxy resins. BPA is widely used in a variety of applications, including baby bottles, food can lining, food packaging, and dental sealants [1]. Ingestion of BPA-containing food is thought to be the primary source of human exposure. BPA is a high-production-volume chemical, and the estimated production of BPA in the United States was approximately 1 million tons in 2004 [2]. As a result, human exposure to BPA is very extensive [3]. BPA is a well-known endocrine-disrupting chemical, and its estrogenic activity was documented in the early stages of its use (1960s). Considering its widespread use and potential harmful effects on human health, especially on reproduction, the use of BPA has been regulated. The United States Environmental Protection Agency has established a reference dose of 50 µg/kg/day and the European Food Safety Authority has set a temporary tolerable daily intake of 4 µg/kg/day [4]. In particular, BPA has been banned from baby bottles in many countries. As concerns about public health and regulations limiting BPA use have increased, the use of other bisphenols as BPA substitutes has become more widespread.
Recently, studies on BPA have increased exponentially, revealing that BPA has other endocrine-disrupting properties in addition to its estrogenic activity. This review focuses on the thyroid-disrupting effects of bisphenols, including BPA.
BPA AND THYROID FUNCTION
Thyroid hormone is essential for development, growth, and metabolism, and plays an especially important role in neurodevelopment. Therefore, alterations of thyroid hormone function can interfere with these vital functions. Thyroid hormones, such as thyroxine (T4), triiodothyronine (T3), and thyroid-stimulating hormone (TSH), can be easily measured in the blood. First, we reviewed the published literature on the association between BPA exposure and thyroid hormone.
Thyroid hormone in humans
BPA exposure in humans can be evaluated by measuring urinary BPA concentrations. Previous research has demonstrated that BPA is detected in most members of the population [3], and BPA exposure has been found to be associated with thyroid hormone levels [5,6,7,8]. Several large-scale epidemiological cross-sectional studies have been conducted (Table 1). Urinary BPA concentrations were negatively associated with total T4 in the United States National Health and Nutrition Examination Survey (NHANES) 2007 to 2008 [5]. Urinary BPA concentrations were negatively correlated with TSH levels in Korean National Environmental Health Survey 2012 to 2014 [6]. Serum BPA concentrations had a negative correlation with free T4 in men in the Thai National Health Examination Survey (NHES) 2009 [7]. Urinary BPA concentrations were related to increased free T3 and decreased TSH levels in Chinese adults [8]. Small-scale studies have also shown an association between BPA and TSH [9,10,11]. The leading cause of thyroid dysfunction is autoimmune disease, and the Thai NHES reported that serum BPA concentrations were positively associated with thyroid peroxidase (TPO) antibody positivity [12]. These findings suggest that BPA can induce thyroid autoimmunity, resulting in thyroid dysfunction. However, in the study conducted in China, there was no association between urinary BPA concentrations and thyroid autoantibodies [8].
Table 1. Previous Studies of BPA Exposure and Thyroid Measures in the General Population.
| Study | Country | Population | No. | Specimen | BPA concentration, ng/mL | Thyroid measures | Association |
|---|---|---|---|---|---|---|---|
| Meeker et al. (2011) [5] | USA | Aged ≥20 yr | 1,346 | Urine | GM 2.5 (95% CI, 2.3–2.7) | Total/free T4, total/ free T3, TSH | Total T4↓ |
| Park et al. (2017) [6] | Korea | Aged ≥20 yr | 6,003 | Urine | GM 1.13 (95% CI, 1.06–1.20) | Total T4, total T3, TSH | TSH↓ |
| Sriphrapradang et al. (2013) [7] | Thailand | Aged 18–94 yr | 2,340 | Serum | Median 0.33 (min 0–max 66.91) | Free T4, TSH | Free T4↓ (men) |
| Wang et al. (2013) [8] | China | Aged ≥40 yr | 3,394 | Urine | Median 0.81 (IQR, 0.47–1.43) | Free T4, free T3, TSH | Free T3↑ TSH↓ |
| Andrianou et al. (2016) [9] | Cyprus, Romania | Adult women | 212 | Urine | Median 2.258 (IQR, 1,100–4,611) | Free T4, TSH, thyroid nodules | TSH↑, thyroid nodule↓ |
| Geens et al. (2015) [10] | Belgium | Case-control (obese and lean) | 194 | Urine | Median 1.7 | Free T4, TSH | TSH↑ (lean) |
| Meeker et al. (2010) [11] | USA | Men (infertility clinic) | 167 | Urine | Median 1.3 (IQR, 0.7–2.4) | Free T4, total T3, TSH | TSH↑ |
| Zhou et al. (2017) [55] | China | Case-control | 178 | Urine | Median 4.18 (IQR, 1.74–7.01) | Thyroid cancer, nodular goiter | Thyroid cancer↑, nodular goiter↑ |
| Li et al. (2019) [56] | China | Case-control, women ≥18 yr | 1,416 | Urine | Median 1.35 (IQR, 0.83–2.34) | Thyroid nodule | Thyroid nodule↑ |
BPA, bisphenol A; GM, geometric mean; CI, confidence interval; T4, thyroxine; T3, triiodothyronine; TSH, thyroid-stimulating hormone; IQR, interquartile range.
In pregnant women, BPA exposure can affect thyroid hormone levels [13,14,15,16]. Because thyroid hormone plays a pivotal role in fetal neurodevelopment, maternal BPA exposure has a greater clinical significance than exposure in the general population. BPA exposure during pregnancy can affect thyroid hormone levels in newborns (Table 2). A prospective pregnancy and birth cohort study in the United States, reported that urinary BPA concentrations in pregnant women were inversely correlated with TSH levels in boys [16]. Another prospective study also showed an inverse association between maternal urinary BPA concentrations and TSH in girls [17]. Even after birth, maternal BPA exposure can affect children's thyroid hormone levels through breastfeeding [18]. However, some cross-sectional studies found no association between BPA exposure and thyroid hormone in cord blood samples [19,20,21].
Table 2. Previous Research on Maternal BPA Exposure and Thyroid Measures in Newborns.
| Study | Country | No. (newborn) | BPA specimen | BPA concentration | Thyroid specimen | Thyroid measures | Association |
|---|---|---|---|---|---|---|---|
| Chevrier et al. (2013) [16] | USA | 364 | Maternal urine in the first and second half of pregnancy | GM 1.3 μg/g Cr | Blood spots after birth | TSH | TSH↓ (boys) |
| Romano et al. (2015) [17] | USA | 249 | Maternal urine at 26 weeks of gestation | GM 2.3 μg/g Cr (95% CI, 2.1–2.5) | Cord blood | Total/free T4, total/free T3, TSH | TSH↓ (girls) |
| Minatoya et al. (2017) [19] | Japan | 283 | Cord blood | GM 0.051 ng/mL (IQR, <LOD–0.076) | Cord blood | Free T4, TSH | None |
| Sanlidag et al. (2018) [20] | Cyprus | 88 | Cord blood | Mean 4.934 ng/mL | Cord blood | Free T4, TSH | None |
| Brucker-Davis et al. (2011) [21] | France | 84 | Cord blood | Median 0.9 ng/mL | (IQR, 0.2–3.3) Cord blood | Free T4, free T3, TSH | None |
BPA, bisphenol A; GM, geometric mean; Cr, creatinine; TSH, thyroid-stimulating hormone; CI, confidence interval; T4, thyroxine; T3, triiodothyronine; IQR, interquartile range; LOD, limit of detection.
Human studies have some limitations. First, a single measurement of BPA in a spot urine sample may not be representative of overall BPA exposure. Because BPA has a short half-life, it leaves the body rapidly and does not bioaccumulate [22]. To assess BPA exposure properly, repeated BPA measurements are needed, but it is difficult to obtain serial BPA measurements in real-world circumstances. Second, the causal relationship between BPA exposure and thyroid hormone changes remains unclear, and is difficult to elucidate. Most of the studies were cross-sectional, and only two studies were longitudinal. Next, humans are exposed to numerous chemicals at once, and several chemicals share similar exposure sources [23], so the findings of those studies may reflect a mixed effect, rather than the effects of BPA alone, which could lead to false positive conclusions. Therefore, the association between BPA and thyroid function in humans reported in the literature is still inconclusive.
Thyroid hormone in animals
To supplement the limitations of human epidemiological studies, several animal experiments have been conducted. BPA was administered directly to animals, and thyroid hormone levels were measured. BPA exposure (40 mg/kg, 15 days, orally) in adult rats increased T4 levels [24]. Neonatal exposure to BPA (2.5 to 6.2 mg/kg, 10 days, subcutaneously) decreased T4 levels and increased TSH levels in adulthood [25]. Maternal exposure to BPA in rats can affect thyroid hormone in the offspring. Zoeller et al. [26] reported that maternal BPA exposure during pregnancy and lactation (1 to 50 mg/kg, orally) increased T4 levels in the offspring (postnatal day [PND] 15). Xu et al. [27] reported that maternal BPA exposure induced a transient increase in T4 levels (PND 7), followed by a decrease of T4 (PND 21) in male offspring. However, other researchers reported that perinatal exposure to BPA (0.0025 to 40 mg/kg, orally or subcutaneously) did not alter TSH and T4 levels in offspring [28,29,30,31]. The inconsistent results of rat experiments may be due to different doses, windows of exposure, and routes of exposure to BPA. BPA-induced thyroid hormone changes have also been observed in mice and zebrafish. BPA exposure during puberty decreased T4 levels in mice [32]. BPA exposure to zebrafish larvae increased T3 levels [33]. All these experiments indicate that BPA could affect thyroid function, but the effects might vary according to the route, dose, duration, or age at exposure.
MECHANISM OF BPA
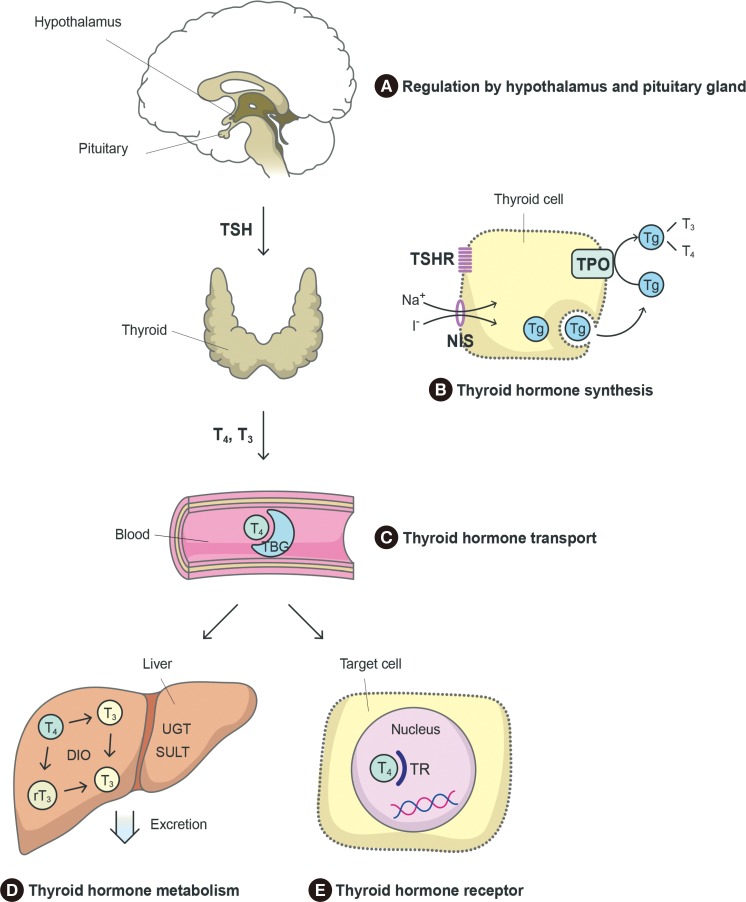
Thyroid hormone is synthesized in the thyroid gland under the regulation of TSH released from the pituitary gland. Synthesized thyroid hormone binds to proteins and circulates in the blood. At the target organ, thyroid hormone binds to the thyroid hormone receptor (TR) and stimulates thyroid hormone signaling pathways. Subsequently, thyroid hormone is metabolized to its inactive form in the liver. We explored the ways in which these processes are disrupted by BPA (Fig. 1) by reviewing the published mechanistic studies.
Fig. 1. Chemicals can interfere with thyroid hormone action at several points. (A) The pituitary gland and hypothalamus regulate thyroid hormone synthesis through thyroid-stimulating hormone (TSH) release. (B) Thyroid hormone is synthesized in the thyroid gland. If TSH stimulates thyrocytes, iodine uptake via the sodium iodide symporter (NIS), thyroglobulin (Tg) production, and oxidation by thyroid peroxidase (TPO) occur. (C) Thyroid hormone is carried on binding proteins such as thyroxine-binding globulin (TBG) and transthyretin (TTR). (D) Thyroid hormone is metabolized in the liver by deiodinase (DIO), UDP-glucuronosyltransferase (UGT), or sulfotransferase (SULT) and eliminated in bile. (E) Thyroid hormone binds to the thyroid hormone receptor (TR) in target cells and activates thyroid hormone signaling pathways. T4, thyroxine; T3, triiodothyronine.
Thyroid hormone synthesis
It is possible that BPA acts directly on the thyroid gland, as suggested by the finding that in humans, urinary BPA concentrations were inversely associated with thyroid volume in children [34]. In animal studies, BPA exposure, especially during pregnancy, has been found to alter thyroid gland weight or to change thyroid histology [35,36].
In thyroid hormone synthesis, iodine enters thyrocytes via the sodium iodide symporter (NIS), is oxidized by TPO, and is incorporated into tyrosyl residues of thyroglobulin (Tg). BPA exposure has been found to change the expression of genes involved in these processes, such as Slc5a5 (NIS), Tpo, and Tg. For example, BPA treatment increased Tg and Slc5a5 gene expression in zebrafish experiments [33,37,38] and Tshr, Slc5a5, Tpo, and Tg gene expression in FRTL5 cells [37,39,40]. BPA treatment decreased iodide uptake in FRTL5 cells and TPO activity in isolated rat thyroid microsomes [40]. In rats, BPA treatment decreased thyroid iodide uptake and TPO activity [36]. These findings suggest that BPA can inhibit thyroid hormone synthesis.
Regulation by the hypothalamus and pituitary gland
Little is known about BPA-associated changes in the hypothalamus and pituitary gland. BPA exposure (0.1 to 1 µM) did not change Crh or Tshβ gene expression in zebrafish experiments [33]. However, BPA treatment (10 µM) decreased Tshβ, Trα, Trβ, and deiodinase 2 (Dio2) expression in GH3 pituitary cells [39]. Dong and Wade [41] reported that BPA can inhibit thyroid hormone uptake via the thyroid hormone transporter monocarboxylate transporter 8 (MCT8) in the brain.
Thyroid hormone transport
In the blood, thyroid hormone is transported in conjunction with proteins such as thyroxine-binding globulin (TBG) and transthyretin (TTR). BPA can bind TTR [42]. Competitive binding with thyroid hormone transport proteins interferes with thyroid hormone. However, the affinity of BPA for TBG and TTR is weak. Instead, derivatives of BPA such as tetrachlorinate BPA (TCBPA) or tetrabrominated BPA (TBBPA) have a stronger affinity [43]. In addition, the BPA concentrations commonly found in humans are insufficient to interfere with thyroid hormone transport [42].
Thyroid hormone metabolism
Deiodination catalyzed by DIO is important in thyroid hormone metabolism. In rats, BPA treatment reduced hepatic DIO1 activity [24]. BPA exposure (0.1 to 1 µM) increased the expression of Dio1 gene and Ugt1ab gene encoding UDP glucuronosyltrasferase in zebrafish [33].
Thyroid hormone receptor
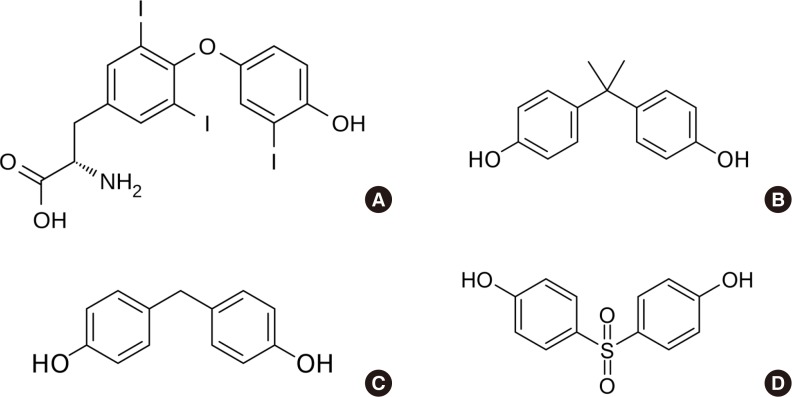
The structure of BPA and its analogues resembles that of T3 (Fig. 2). BPA can bind TR, particularly the beta isoform of TR (TRβ), and acts as an antagonist [26,44], as confirmed in a cell-based reporter gene assay [45,46]. TR was inhibited by BPA treatment (10 to 100 µM), where TRβ was at a lower concentration (0.001 to 0.1 µM). BPA was found to inhibit TR-mediated transcription of T3-response genes [47]. These findings suggest that BPA can disrupt the action of thyroid hormone. It is thought that the TR-antagonistic effect of BPA may be the main mechanism through which it disrupts thyroid function.
Fig. 2. Structure of thyroid hormone and bisphenols. (A) Triiodothyronine, (B) bisphenol A, (C) bisphenol F, and (D) bisphenol S.
OTHER BISPHENOLS AND THYROID FUNCTION
Since concerns have been raised regarding BPA from a public health perspective, several BPA substitutes, such as bisphenol F (BPF) and bisphenol S (BPS), have become used with increasing frequency. Because their structures are similar to that of BPA (Fig. 2), it is possible that these bisphenols disrupt thyroid function. However, since these bisphenols are only starting to be used, little research has been conducted on their role in thyroid disruption.
Like BPA, BPF and BPS can bind TRβ and exert antagonistic activity [48,49]. In zebrafish, BPF exposure altered T4, T3, and TSH levels and changed the expression of genes including Tg, Ttr, and Ugt1ab [33,50].
In zebrafish, BPS exposure decreased T4 and T3 levels and increased TSH levels [51,52]. Furthermore, in zebrafish, BPS treatment increased the expression of genes including Ttr and Ugt1ab [33,51].
In human, some epidemiological studies have investigated associations between non-BPA bisphenols and thyroid hormone levels, but only in pregnant women. Urinary BPF concentrations were associated with higher free T3 [13] or free T4 levels [53]. Aker et al. [53] reported that urinary BPS concentrations were associated with lower corticotropin-releasing hormone levels, but other studies found no association between BPS and thyroid hormone levels [13,54].
BPA AND THYROID NODULES
As BPA became known as a thyroid-disrupting chemical, the association between BPA and thyroid nodules or thyroid cancer emerged as a topic of interest. In case-control studies conducted in China, urinary BPA concentrations in patients with thyroid nodules or thyroid cancer were significantly higher than in the control groups (Table 1) [55,56]. However, Andrianou et al. [9] reported that BPA exposure was inversely associated with thyroid nodules. In animal experiments, BPA treatment in F344 rats did not induce thyroid cancer stimulated by N-bis(2-hydroxypropyl) nitrosamine (DHPN) [57]. However, BPA treatment enhanced the susceptibility of thyroid cancer stimulated by DHPN and iodine excess in rats [58]. BPA can induce the proliferation of thyroid cancer cells [59]. Taken together, a link may possibly exist between BPA and thyroid nodules or cancer, but there is a lack of evidence that BPA can induce thyroid nodules or thyroid cancer.
CONCLUSIONS
Here, we reviewed the associations between bisphenols and thyroid function. Several previous studies indicate that BPA affects thyroid hormone action. Considering the results of studies in pregnant women and experiments on perinatal exposure, the effects of BPA on thyroid hormone are thought to be more critical and harmful in the early stages of life. BPA may affect thyroid function through several possible mechanisms of action. First, the main mechanism of action is thought to be binding of BPA to TR and interference with thyroid hormone. However, this review also suggests that BPA can interfere with thyroid hormone synthesis, transport, and metabolism. Recently, this thyroid-disrupting effect was identified for other bisphenols, as well as BPA. Although they were not the primary focus of this review, BPA derivatives such as TCBPA and TBBPA resulting from BPA degradation processes have increasingly been investigated as thyroid-disrupting chemicals [60]. Therefore, attention should be paid to the effects of bisphenols, including BPA, on the thyroid.
ACKNOWLEDGMENTS
The authors would like to thank Jin Hyoung Pyo (Seoul National University Hospital Healthcare System Gangnam Center) for his assistance in drawing the figure. This research was supported by a grant (18182MFDS65) from Ministry of Food and Drug Safety in 2018.
Footnotes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Kang JH, Kondo F, Katayama Y. Human exposure to bisphenol A. Toxicology. 2006;226:79–89. doi: 10.1016/j.tox.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 2.Corrales J, Kristofco LA, Steele WB, Yates BS, Breed CS, Williams ES, et al. Global assessment of bisphenol a in the environment: review and analysis of its occurrence and bioaccumulation. Dose Response. 2015;13:1559325815598308. doi: 10.1177/1559325815598308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Calafat AM, Ye X, Wong LY, Reidy JA, Needham LL. Exposure of the U.S. population to bisphenol A and 4-tertiary-octylphenol: 2003-2004. Environ Health Perspect. 2008;116:39–44. doi: 10.1289/ehp.10753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gore AC, Chappell VA, Fenton SE, Flaws JA, Nadal A, Prins GS, et al. Executive summary to EDC-2: the Endocrine Society's Second Scientific Statement on Endocrine-Disrupting Chemicals. Endocr Rev. 2015;36:593–602. doi: 10.1210/er.2015-1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meeker JD, Ferguson KK. Relationship between urinary phthalate and bisphenol A concentrations and serum thyroid measures in U.S. adults and adolescents from the National Health and Nutrition Examination Survey (NHANES) 2007-2008. Environ Health Perspect. 2011;119:1396–1402. doi: 10.1289/ehp.1103582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park C, Choi W, Hwang M, Lee Y, Kim S, Yu S, et al. Associations between urinary phthalate metabolites and bisphenol A levels, and serum thyroid hormones among the Korean adult population: Korean National Environmental Health Survey (KoNEHS) 2012-2014. Sci Total Environ. 2017;584-585:950–957. doi: 10.1016/j.scitotenv.2017.01.144. [DOI] [PubMed] [Google Scholar]
- 7.Sriphrapradang C, Chailurkit LO, Aekplakorn W, Ongphiphadhanakul B. Association between bisphenol A and abnormal free thyroxine level in men. Endocrine. 2013;44:441–447. doi: 10.1007/s12020-013-9889-y. [DOI] [PubMed] [Google Scholar]
- 8.Wang T, Lu J, Xu M, Xu Y, Li M, Liu Y, et al. Urinary bisphenol a concentration and thyroid function in Chinese adults. Epidemiology. 2013;24:295–302. doi: 10.1097/EDE.0b013e318280e02f. [DOI] [PubMed] [Google Scholar]
- 9.Andrianou XD, Gangler S, Piciu A, Charisiadis P, Zira C, Aristidou K, et al. Human exposures to bisphenol A, bisphenol F and chlorinated bisphenol A derivatives and thyroid function. PLoS One. 2016;11:e0155237. doi: 10.1371/journal.pone.0155237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Geens T, Dirtu AC, Dirinck E, Malarvannan G, Van Gaal L, Jorens PG, et al. Daily intake of bisphenol A and triclosan and their association with anthropometric data, thyroid hormones and weight loss in overweight and obese individuals. Environ Int. 2015;76:98–105. doi: 10.1016/j.envint.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 11.Meeker JD, Calafat AM, Hauser R. Urinary bisphenol A concentrations in relation to serum thyroid and reproductive hormone levels in men from an infertility clinic. Environ Sci Technol. 2010;44:1458–1463. doi: 10.1021/es9028292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chailurkit LO, Aekplakorn W, Ongphiphadhanakul B. The association of serum bisphenol A with thyroid autoimmunity. Int J Environ Res Public Health. 2016;13:E1153. doi: 10.3390/ijerph13111153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Derakhshan A, Shu H, Peeters RP, Kortenkamp A, Lindh CH, Demeneix B, et al. Association of urinary bisphenols and triclosan with thyroid function during early pregnancy. Environ Int. 2019;133(Pt A):105123. doi: 10.1016/j.envint.2019.105123. [DOI] [PubMed] [Google Scholar]
- 14.Aung MT, Johns LE, Ferguson KK, Mukherjee B, McElrath TF, Meeker JD. Thyroid hormone parameters during pregnancy in relation to urinary bisphenol A concentrations: a repeated measures study. Environ Int. 2017;104:33–40. doi: 10.1016/j.envint.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aker AM, Watkins DJ, Johns LE, Ferguson KK, Soldin OP, Anzalota Del Toro LV, et al. Phenols and parabens in relation to reproductive and thyroid hormones in pregnant women. Environ Res. 2016;151:30–37. doi: 10.1016/j.envres.2016.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chevrier J, Gunier RB, Bradman A, Holland NT, Calafat AM, Eskenazi B, et al. Maternal urinary bisphenol a during pregnancy and maternal and neonatal thyroid function in the CHAMACOS study. Environ Health Perspect. 2013;121:138–144. doi: 10.1289/ehp.1205092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Romano ME, Webster GM, Vuong AM, Thomas Zoeller R, Chen A, Hoofnagle AN, et al. Gestational urinary bisphenol A and maternal and newborn thyroid hormone concentrations: the HOME Study. Environ Res. 2015;138:453–460. doi: 10.1016/j.envres.2015.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yi B, Kim C, Park M, Han Y, Park JY, Yang M. Association between endocrine disrupting phenols in colostrums and maternal and infant health. Int J Endocrinol. 2013;2013:282381. doi: 10.1155/2013/282381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Minatoya M, Sasaki S, Araki A, Miyashita C, Itoh S, Yamamoto J, et al. Cord blood bisphenol a levels and reproductive and thyroid hormone levels of neonates: the Hokkaido study on environment and childre's health. Epidemiology. 2017;28 Suppl 1:S3–S9. doi: 10.1097/EDE.0000000000000716. [DOI] [PubMed] [Google Scholar]
- 20.Sanlidag B, Dalkan C, Yetkin O, Bahceciler NN. Evaluation of dose dependent maternal exposure to bisphenol a on thyroid functions in newborns. J Clin Med. 2018;7:E119. doi: 10.3390/jcm7060119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brucker-Davis F, Ferrari P, Boda-Buccino M, Wagner-Mahler K, Pacini P, Gal J, et al. Cord blood thyroid tests in boys born with and without cryptorchidism: correlations with birth parameters and in utero xenobiotics exposure. Thyroid. 2011;21:1133–1141. doi: 10.1089/thy.2010.0459. [DOI] [PubMed] [Google Scholar]
- 22.Teeguarden JG, Waechter JM, Jr, Clewell HJ, 3rd, Covington TR, Barton HA. Evaluation of oral and intravenous route pharmacokinetics, plasma protein binding, and uterine tissue dose metrics of bisphenol A: a physiologically based pharmacokinetic approach. Toxicol Sci. 2005;85:823–838. doi: 10.1093/toxsci/kfi135. [DOI] [PubMed] [Google Scholar]
- 23.Kim S, Kim S, Won S, Choi K. Considering common sources of exposure in association studies: urinary benzophenone-3 and DEHP metabolites are associated with altered thyroid hormone balance in the NHANES 2007-2008. Environ Int. 2017;107:25–32. doi: 10.1016/j.envint.2017.06.013. [DOI] [PubMed] [Google Scholar]
- 24.da Silva MM, Goncalves CFL, Miranda-Alves L, Fortunato RS, Carvalho DP, Ferreira ACF. Inhibition of type 1 iodothyronine deiodinase by bisphenol A. Horm Metab Res. 2019;51:671–677. doi: 10.1055/a-0919-3879. [DOI] [PubMed] [Google Scholar]
- 25.Fernandez MO, Bourguignon NS, Arocena P, Rosa M, Libertun C, Lux-Lantos V. Neonatal exposure to bisphenol A alters the hypothalamic-pituitary-thyroid axis in female rats. Toxicol Lett. 2018;285:81–86. doi: 10.1016/j.toxlet.2017.12.029. [DOI] [PubMed] [Google Scholar]
- 26.Zoeller RT, Bansal R, Parris C. Bisphenol-A, an environmental contaminant that acts as a thyroid hormone receptor antagonist in vitro, increases serum thyroxine, and alters RC3/neurogranin expression in the developing rat brain. Endocrinology. 2005;146:607–612. doi: 10.1210/en.2004-1018. [DOI] [PubMed] [Google Scholar]
- 27.Xu X, Liu Y, Sadamatsu M, Tsutsumi S, Akaike M, Ushijima H, et al. Perinatal bisphenol A affects the behavior and SRC-1 expression of male pups but does not influence on the thyroid hormone receptors and its responsive gene. Neurosci Res. 2007;58:149–155. doi: 10.1016/j.neures.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 28.Sadowski RN, Park P, Neese SL, Ferguson DC, Schantz SL, Juraska JM. Effects of perinatal bisphenol A exposure during early development on radial arm maze behavior in adult male and female rats. Neurotoxicol Teratol. 2014;42:17–24. doi: 10.1016/j.ntt.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bansal R, Zoeller RT. CLARITY-BPA: bisphenol A or propylthiouracil on thyroid function and effects in the developing male and female rat brain. Endocrinology. 2019;160:1771–1785. doi: 10.1210/en.2019-00121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Santos-Silva AP, de Moura EG, Pinheiro CR, Oliveira E, Lisboa PC. Short-term and long-term effects of bisphenol A (BPA) exposure during breastfeeding on the biochemical and endocrine profiles in rats. Horm Metab Res. 2018;50:491–503. doi: 10.1055/a-0628-6708. [DOI] [PubMed] [Google Scholar]
- 31.Kobayashi K, Miyagawa M, Wang RS, Suda M, Sekiguchi S, Honma T. Effects of in utero and lactational exposure to bisphenol A on thyroid status in F1 rat offspring. Ind Health. 2005;43:685–690. doi: 10.2486/indhealth.43.685. [DOI] [PubMed] [Google Scholar]
- 32.Jiang W, Cao L, Wang F, Ge H, Wu PC, Li XW, et al. Accelerated reduction of serum thyroxine and hippocampal histone acetylation links to exacerbation of spatial memory impairment in aged CD-1 mice pubertally exposed to bisphenol-A. Age (Dordr) 2016;38:405–418. doi: 10.1007/s11357-016-9947-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee S, Kim C, Shin H, Kho Y, Choi K. Comparison of thyroid hormone disruption potentials by bisphenols A, S, F, and Z in embryo-larval zebrafish. Chemosphere. 2019;221:115–123. doi: 10.1016/j.chemosphere.2019.01.019. [DOI] [PubMed] [Google Scholar]
- 34.Wang N, Zhou Y, Fu C, Wang H, Huang P, Wang B, et al. Influence of bisphenol a on thyroid volume and structure independent of iodine in school children. PLoS One. 2015;10:e0141248. doi: 10.1371/journal.pone.0141248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ahmed RG. Maternal bisphenol A alters fetal endocrine system: thyroid adipokine dysfunction. Food Chem Toxicol. 2016;95:168–174. doi: 10.1016/j.fct.2016.06.017. [DOI] [PubMed] [Google Scholar]
- 36.Silva MMD, Xavier LLF, Goncalves CFL, Santos-Silva AP, Paiva-Melo FD, Freitas ML, et al. Bisphenol A increases hydrogen peroxide generation by thyrocytes both in vivo and in vitro. Endocr Connect. 2018;7:1196–1207. doi: 10.1530/EC-18-0348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gentilcore D, Porreca I, Rizzo F, Ganbaatar E, Carchia E, Mallardo M, et al. Bisphenol A interferes with thyroid specific gene expression. Toxicology. 2013;304:21–31. doi: 10.1016/j.tox.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 38.Berto-Junior C, Santos-Silva AP, Ferreira ACF, Graceli JB, de Carvalho DP, Soares P, et al. Unraveling molecular targets of bisphenol A and S in the thyroid gland. Environ Sci Pollut Res Int. 2018;25:26916–26926. doi: 10.1007/s11356-018-2419-y. [DOI] [PubMed] [Google Scholar]
- 39.Lee S, Kim C, Youn H, Choi K. Thyroid hormone disrupting potentials of bisphenol A and its analogues: in vitro comparison study employing rat pituitary (GH3) and thyroid follicular (FRTL-5) cells. Toxicol In Vitro. 2017;40:297–304. doi: 10.1016/j.tiv.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 40.Wu Y, Beland FA, Fang JL. Effect of triclosan, triclocarban, 2,2′,4,4′-tetrabromodiphenyl ether, and bisphenol A on the iodide uptake, thyroid peroxidase activity, and expression of genes involved in thyroid hormone synthesis. Toxicol In Vitro. 2016;32:310–319. doi: 10.1016/j.tiv.2016.01.014. [DOI] [PubMed] [Google Scholar]
- 41.Dong H, Wade MG. Application of a nonradioactive assay for high throughput screening for inhibition of thyroid hormone uptake via the transmembrane transporter MCT8. Toxicol In Vitro. 2017;40:234–242. doi: 10.1016/j.tiv.2017.01.014. [DOI] [PubMed] [Google Scholar]
- 42.Cao J, Guo LH, Wan B, Wei Y. In vitro fluorescence displacement investigation of thyroxine transport disruption by bisphenol A. J Environ Sci (China) 2011;23:315–321. doi: 10.1016/s1001-0742(10)60408-1. [DOI] [PubMed] [Google Scholar]
- 43.Marchesini GR, Meimaridou A, Haasnoot W, Meulenberg E, Albertus F, Mizuguchi M, et al. Biosensor discovery of thyroxine transport disrupting chemicals. Toxicol Appl Pharmacol. 2008;232:150–160. doi: 10.1016/j.taap.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 44.Moriyama K, Tagami T, Akamizu T, Usui T, Saijo M, Kanamoto N, et al. Thyroid hormone action is disrupted by bisphenol A as an antagonist. J Clin Endocrinol Metab. 2002;87:5185–5190. doi: 10.1210/jc.2002-020209. [DOI] [PubMed] [Google Scholar]
- 45.Freitas J, Cano P, Craig-Veit C, Goodson ML, Furlow JD, Murk AJ. Detection of thyroid hormone receptor disruptors by a novel stable in vitro reporter gene assay. Toxicol In Vitro. 2011;25:257–266. doi: 10.1016/j.tiv.2010.08.013. [DOI] [PubMed] [Google Scholar]
- 46.Sheng ZG, Tang Y, Liu YX, Yuan Y, Zhao BQ, Chao XJ, et al. Low concentrations of bisphenol a suppress thyroid hormone receptor transcription through a nongenomic mechanism. Toxicol Appl Pharmacol. 2012;259:133–142. doi: 10.1016/j.taap.2011.12.018. [DOI] [PubMed] [Google Scholar]
- 47.Heimeier RA, Das B, Buchholz DR, Shi YB. The xenoestrogen bisphenol A inhibits postembryonic vertebrate development by antagonizing gene regulation by thyroid hormone. Endocrinology. 2009;150:2964–2973. doi: 10.1210/en.2008-1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lu L, Zhan T, Ma M, Xu C, Wang J, Zhang C, et al. Thyroid disruption by bisphenol S Analogues via thyroid hormone receptor β: in vitro, in vivo, and molecular dynamics simulation study. Environ Sci Technol. 2018;52:6617–6625. doi: 10.1021/acs.est.8b00776. [DOI] [PubMed] [Google Scholar]
- 49.Zhang YF, Ren XM, Li YY, Yao XF, Li CH, Qin ZF, et al. Bisphenol A alternatives bisphenol S and bisphenol F interfere with thyroid hormone signaling pathway in vitro and in vivo. Environ Pollut. 2018;237:1072–1079. doi: 10.1016/j.envpol.2017.11.027. [DOI] [PubMed] [Google Scholar]
- 50.Huang GM, Tian XF, Fang XD, Ji FJ. Waterborne exposure to bisphenol F causes thyroid endocrine disruption in zebrafish larvae. Chemosphere. 2016;147:188–194. doi: 10.1016/j.chemosphere.2015.12.080. [DOI] [PubMed] [Google Scholar]
- 51.Zhang DH, Zhou EX, Yang ZL. Waterborne exposure to BPS causes thyroid endocrine disruption in zebrafish larvae. PLoS One. 2017;12:e0176927. doi: 10.1371/journal.pone.0176927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Naderi M, Wong MY, Gholami F. Developmental exposure of zebrafish (Danio rerio) to bisphenol-S impairs subsequent reproduction potential and hormonal balance in adults. Aquat Toxicol. 2014;148:195–203. doi: 10.1016/j.aquatox.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 53.Aker AM, Ferguson KK, Rosario ZY, Mukherjee B, Alshawabkeh AN, Calafat AM, et al. A repeated measures study of phenol, paraben and triclocarban urinary biomarkers and circulating maternal hormones during gestation in the Puerto Rico PROTECT cohort. Environ Health. 2019;18:28. doi: 10.1186/s12940-019-0459-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Aker AM, Johns L, McElrath TF, Cantonwine DE, Mukherjee B, Meeker JD. Associations between maternal phenol and paraben urinary biomarkers and maternal hormones during pregnancy: a repeated measures study. Environ Int. 2018;113:341–349. doi: 10.1016/j.envint.2018.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhou Z, Zhang J, Jiang F, Xie Y, Zhang X, Jiang L. Higher urinary bisphenol A concentration and excessive iodine intake are associated with nodular goiter and papillary thyroid carcinoma. Biosci Rep. 2017;37:BSR20170678. doi: 10.1042/BSR20170678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li L, Ying Y, Zhang C, Wang W, Li Y, Feng Y, et al. Bisphenol A exposure and risk of thyroid nodules in Chinese women: a case-control study. Environ Int. 2019;126:321–328. doi: 10.1016/j.envint.2019.02.026. [DOI] [PubMed] [Google Scholar]
- 57.Takagi H, Mitsumori K, Onodera H, Nasu M, Tamura T, Yasuhara K, et al. Improvement of a two-stage carcinogenesis model to detect modifying effects of endocrine disrupting chemicals on thyroid carcinogenesis in rats. Cancer Lett. 2002;178:1–9. doi: 10.1016/s0304-3835(01)00804-7. [DOI] [PubMed] [Google Scholar]
- 58.Zhang J, Zhang X, Li Y, Zhou Z, Wu C, Liu Z, et al. Low dose of bisphenol A enhance the susceptibility of thyroid carcinoma stimulated by DHPN and iodine excess in F344 rats. Oncotarget. 2017;8:69874–69887. doi: 10.18632/oncotarget.19434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang Y, Wei F, Zhang J, Hao L, Jiang J, Dang L, et al. Bisphenol A and estrogen induce proliferation of human thyroid tumor cells via an estrogen-receptor-dependent pathway. Arch Biochem Biophys. 2017;633:29–39. doi: 10.1016/j.abb.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 60.Pahigian JM, Zuo Y. Occurrence, endocrine-related bioeffects and fate of bisphenol A chemical degradation intermediates and impurities: a review. Chemosphere. 2018;207:469–480. doi: 10.1016/j.chemosphere.2018.05.117. [DOI] [PubMed] [Google Scholar]