Abstract
Objective:
The objective of this study was to estimate the prevalence of child sexual abuse in a representative sample of Quebec high school youths and document its associations with mental health problems and health-risk behaviors.
Method:
Data were drawn from the Quebec Youths’ Romantic Relationships Survey, which involved a one-stage stratified cluster sampling of 34 Quebec high schools from Grades 10 to 12. A total of 8,194 youths (mean age = 15.35) were recruited. The survey assessed child sexual abuse, mental health problems (psychological distress, post-traumatic stress symptoms, suicidality), health services utilization, and health-risk behaviors (alcohol, drug, and cannabis use). Gender-stratified multivariate analyses were used to assess associations between child sexual abuse and mental health problems and health-risk behaviors while controlling for confounding demographic variables and other forms of child maltreatment experienced in childhood.
Results:
A total of 14.9% of girls and 3.9% of boys reported having experienced child sexual abuse. Child sexual abuse was independently associated with an increased risk of psychological distress, greater health services utilization, and increased health-risk behaviors, after controlling for other forms of childhood maltreatment experienced.
Conclusions:
Child sexual abuse is prevalent among youths in Quebec and is associated with an increased risk of a host of negative consequences. Continued efforts in the development of early detection strategies as well as prevention and intervention programs are warranted.
Keywords: child sexual abuse, mental health, suicidal ideation, post-traumatic stress disorder, health-risk behaviors, health services utilization
Abstract
Objectif :
L’objectif de la présente étude était d’estimer la prévalence de l’agression sexuelle pendant l’enfance dans un échantillon représentatif d'adolescentes et d'adolescents des écoles secondaires du Québec et d’en documenter les associations avec les problèmes de santé mentale et les comportements à risque.
Méthode :
Les données ont été tirées de l’enquête Parcours amoureux des jeunes (PAJ), qui comportait un échantillonnage par grappes stratifiées à un degré de 34 écoles secondaires du Québec de la 10e à la 12e année. Au total, 8 194 adolescents (âge moyen = 15,35) ont été recrutés. L’enquête a évalué l’agression sexuelle pendant l’enfance, les problèmes de santé mentale (détresse psychologique, symptômes de stress post-traumatique, suicidalité), l’utilisation de services de santé et les comportements à risque pour la santé (alcool, drogues et cannabis). Les analyses multivariées stratifiées selon le sexe ont évalué les associations entre l’agression sexuelle pendant l’enfance, les problèmes de santé mentale et les comportements à risque pour la santé tout en contrôlant pour les variables socio-démographiques et d’autres formes de maltraitance.
Résultats :
En tout, 14,9% des filles et 3,9% des garçons ont déclaré avoir vécu une agression sexuelle durant l’enfance. L’agression sexuelle durant l’enfance était indépendamment associée à un risque accru de détresse psychologique, à une plus grande utilisation des services de santé et à des comportements à risque, après avoir contrôlé pour d’autres formes de maltraitance.
Conclusions :
L’agression sexuelle pendant l’enfance est prévalente chez les adolescentes et les adolescents du Québec et est associée à un risque accru d’une panoplie de conséquences négatives. Des initiatives continues d’élaboration de stratégies de détection précoce, ainsi que des programmes de prévention et d’intervention sont à privilégier.
Child sexual abuse is a major public health issue with global prevalence estimates revealing that between 8% to 31% of girls and 3% to 17% of boys have been victims of child sexual abuse before the age of 18.1 A bulk of studies have examined negative outcomes associated with child sexual abuse relying on cross-sectional studies of adult samples. Findings highlight that child sexual abuse is associated with deleterious consequences affecting both the mental and physical health of victims in adulthood.2
In Canada, there is a paucity of information about the extent of this problem and its negative outcomes in representative samples. A Canadian study using representative data showed that 14.4% of women and 5.8% of men have experienced sexual abuse during childhood.3 This study reported that adult victims of child sexual abuse were 3 times more likely to self-report poor physical health than the general population. Adult victims were also found to be more likely to suffer from chronic pain, digestive and cardiac problems, as well as cancer.4 Child sexual abuse is also found to be associated with a heightened risk of mental health problems including suicidal thoughts and suicide attempts.3
While these studies provide a wealth of data regarding the devastating consequences associated with child sexual abuse in adulthood, to date, little research has offered prevalence rates of child sexual abuse and its correlates in Canadian adolescent samples. A cross-sectional study conducted in Ontario found 12.4% of girls and 4.3% of boys have been victims of sexual abuse before the age of 16.5 Child sexual abuse was found to be associated with several mental health disorders (anxiety, depression, alcohol abuse, drug abuse, antisocial behavior, and other psychiatric disorders) in women, but for men, only alcohol abuse was associated to child sexual abuse. However, this study included only adolescents aged 15 and above and did not report the more immediate consequences of sexual abuse related to mental and physical health in adolescence. Yet adolescence is a crucial developmental period, in which youths face several challenges and are susceptible to engage in health-risk behaviors such as alcohol and drug use.6 Thus, studying the potential impact of child sexual abuse among this age group is essential.
Authors have also underscored the importance of taking into consideration the fact that all too often traumatic events tend to co-occur. For example, in a study conducted in the United States, evaluating victimization and adverse life events among youths, 66% of participants have been victims of at least two forms of trauma.7 Moreover, 50% of youths who sustained an episode of sexual abuse also experienced more than 10 other forms of victimization. As such, it is essential to consider the possible influence of other forms of childhood maltreatment experiences when investigating correlates of child sexual abuse in order to ascertain its independent effects. Past studies have suggested that child sexual abuse may constitute a specific form of trauma associated with specific effects in survivors.8
Against this backdrop, the present study aimed to document the prevalence of child sexual abuse in a representative sample of Quebec high school youths and assess associations of child sexual abuse with mental health problems and health-risk behaviors. Given that past studies have suggested gender differences in possible outcomes related to child sexual abuse,9 analyses were stratified by gender.
Methods
Sample and Study Design
Data collected in the Quebec Youths’ Romantic Relationships Survey were used for this study. The goals of the survey were to identify the prevalence of interpersonal violence and explore associated mental health outcomes in high school adolescents aged 14 to 18 years. The target population included all students in Grades 10 to 12 attending public and private schools in Quebec. The survey was completed through a one-stage stratified cluster sampling of high schools in 2011 to 2012. Schools were randomly selected from an eligible pool from the Quebec Ministry of Education for the 2010 to 2011 school year. Given schools in the whole population are stratified according to metropolitan geographical area, status of schools (public or private schools), teaching language (French or English), and social economic deprivation index, surveyed schools were classified into eight strata giving the aforementioned characteristics in order to obtain a representative sample of students in Grades 10 to 12. A total of 34 high schools (of 131 solicited) participated. Following school directors’ approval, within the same school, students in the three grades were invited to participate in the study. Class response rates and the overall student response rate were determined as the ratio between the number of students who accepted to participate (students from whom written consent was obtained) and the number of solicited students. Response rate was 100% of students solicited for the majority (320 of 329) of classes, while for the remaining, the response rate ranged from 90% to 98% of students solicited. Overall, 99% of the students agreed to participate. The rate of partial nonresponse was less than 3.5% for most variables, and no additional adjustment was made for nonresponse, as bias and loss of power are likely to be inconsequential.10 In addition, analyses of the partial nonresponse did not reveal any specific pattern. A total of 8,230 teenagers (Grades 10, 11, and 12) responded to the self-reported questionnaire. After data verification, 36 participants were excluded for invalid or completely missing data for a final sample of 8,194 students.
The research ethic boards of the Université du Québec à Montréal approved the project. Participants agreed to participate on a voluntary basis by signing an informed consent form. Members of the research team were in direct contact with school personnel (psychologist, sexologist, psycho-educator, nurse) in all schools involved during the data collection and had established a procedure to offer support to teenagers if needed. In addition, students were provided a list of resources (including telephone help lines, websites, community organizations, health services, etc.).
Depending on the teaching language of the school, the survey was completed by students either in English or in French. A back-translation technique11 was used to translate English measures into French. Sociodemographic characteristics of the sample were as follows: 57.8% of participants were girls and 42.2% were boys, and the mean age of teenagers was 15.35 years. Participants were equally distributed for each grade level (37.0% in Grade 10, 31.4% in Grade 11, and 31.6% in Grade 12). Close to two-thirds of participants (63.1%) lived with both parents, 21.9% lived in single-parent families, while 12.8% were in shared custody arrangements and 2.2% described other living arrangements (foster care, living with a member of the extended family). A total of 78% of participants were offspring of Canadian-born parents. Participants were mostly French speaking as a total of 75.4% reported speaking only French at home, 3.6% only English, 5.1% both French and English, and 15.9% other languages.
Measures
Participants were asked to report on lifetime child sexual abuse and lifetime experiences of other forms of child maltreatment.
Child sexual abuse
Two items were adapted from previous studies to assess child sexual abuse.12,13 One item referred to unwanted touching (“Have you ever been touched sexually when you did not want to, or have you ever been manipulated, blackmailed, or physically forced to touch sexually”?) and other item referred to unwanted sexual activities involving penetration (“Has anyone ever used manipulation, blackmail, or physical force, to force or obligate you to have sex [including all sexual activities involving oral, vaginal, or anal penetration]”?) A dichotomized score was created based on the absence (0) or presence (1) of child sexual abuse, and the Spearman–Brown coefficient for the 2 items was .68.
Forms of child maltreatment
Physical abuse and exposure to physical violence were measured by using two questions from the Early Trauma Inventory Self-Report–Short Form.14 The questions were as follows: “Have you ever been physically hit by a member of your family?” and “Have you ever witnessed violence against someone, including a member of your family?” Emotional abuse was assessed with 2 items from the Inventory of Parent and Peer Attachment 15: “My mother tells me hurtful things and/or insulting things” and “My father tells me hurtful things and/or insulting things.” Exposure to interparental violence was assessed using an adapted version of the Revised Conflict Tactics Scales (CTS2)16 composed of 8 items. The frequency of exposure to interparental psychological (i.e., “insult, swear, shout, yell”) and physical violence (“push, shove, slap, throw something that could hurt”) was assessed. The internal consistency of the scale was high (α = .77). Participants were asked for each item “In my lifetime, I’ve seen my father/mother do this to my mother/father.”
Mental health problems
The following mental health problems were evaluated. The Abbreviated University of California at Los Angeles PTSD Reaction Index was used to measure post-traumatic stress disorder (PTSD) with 9 items evaluated on a frequency scale ranging from 0 (none) to 4 (always).17 Participants were first probed about a series of adverse life events and then asked to complete the items (e.g., “I have bad dreams about what happened,” “I get upset, afraid, or sad when something reminds me of what happened”) while thinking of the most difficult event experienced. A dichotomized score was used based on the cutoff of 20 provided by Steinberg et al.18 The scale showed a high internal consistency (α = .89) in the present study.
The 10-item Kessler Psychological Distress Scale assessed psychological distress over the past week.19 Items were rated on a 5-point frequency scale: 1 (never) to 5 (always), with a total score ranging from 10 to 50. A score of 22 and higher was used to identify clinical psychological distress.20,21 The scale showed a high internal consistency (α = .88) in the present study.
Suicidal ideation and suicide attempt were assessed using 2 items: “Have you seriously thought to kill yourself?” and “Have you seriously tried to kill yourself?” The short version of Self-Description Questionnaire was used to measure participants’ self-esteem.22,23 This scale included 5 items (i.e., “I have a lot of qualities”) with a response scale ranging from 0 (false) to 4 (true). A score varying from 0 to 20 was then computed. A score below 10 was considered to reflect low self-esteem.24 The internal consistency in this study was high (α = .86).
Health service utilization
A questionnaire adapted from the Ontario Student Drug Use and Health Survey 25 and the National Longitudinal Study of Adolescent Health 26 was used to assess health service utilization in the past 12 months. Four items evaluated whether the teenager had consulted a counselor, participated in group meetings, was prescribed medication for a psychological or emotional problem or seen a doctor or nurse. A dichotomized score was used with the score of 1 reflecting the use of at least one service.
Health-risk behaviors
Alcohol and drug consumption was measured using the Problematic Consumption of Alcohol and Drugs for Adolescents Scale. 27 Youths were asked about their consumption of alcohol, cannabis, and other drugs in the past year. Alcohol abuse was defined as reporting consuming five drinks or more in one occasion at least 3 times in the past year. Delinquent behaviors were assessed using a 6-item questionnaire from the National Longitudinal Survey of Children. 23 Sample items were “In the past 12 months have you stolen something?” and “Did you fight with someone with the idea of seriously hurting them?” Internal consistency of the scale was satisfactory (α = .70).
Sociodemographic variables
Information on gender, age, family structure (living with two parents under the same household, living with two parents in different households, shared custody, living with one parent, and other family structure arrangements), language most spoken at home (French, English, or other), and ethnicity of parents were collected.
Statistical Analysis
Participants were given a sample weight to correct biases in the nonproportionality of the school sample compared to the target population, ensuring that the estimates reflected the Quebec high school population (Grades 10 to 12). The weight was defined as the inverse of the probability of selecting the given grade in the respondent’s stratum in the sample multiplied by the probability of selecting the same grade in the same stratum in the population.
First, descriptive statistics were used to compute the overall and gender-specific prevalence of child sexual abuse. Second, prevalence estimates were computed for the mental health problem variables, and multivariable logistic regression models were used to test for possible Gender × Child Sexual Abuse Status interactions. Third, odds ratios (ORs) were calculated to quantify the associations between child sexual abuse, and mental health and health-risk indicators. Multivariable logistic regression models were used to estimate adjusted ORs for outcomes in two models. Regression models were first (adjusted OR1) computed while controlling for sociodemographic covariates (grade level, family structure, ethnicity). The second models (adjusted OR2) were then further adjusted for other forms of childhood maltreatment (physical and emotional abuse, exposure to violence, exposure to interparental violence), all variables being entered simultaneously. Significant models were determined with 95% confidence intervals (CIs) or P < .05. All analyses were conducted using the Complex Samples module in SPSS 25 to account for the cluster-stratified sampling design (students nested within 34 schools, within the eight design strata) and respondents’ unequal probability of selection (weighted data).
Results
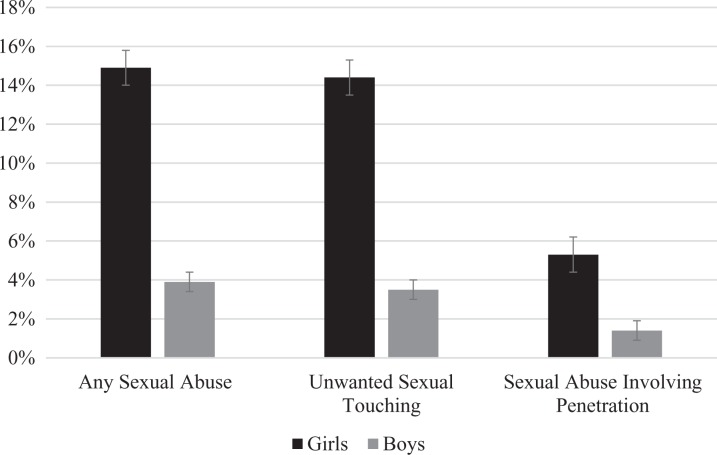
Figure 1 displays the prevalence of child sexual abuse by gender. In the sample, 14.4% (95% CI: 12.6 to 16.3) of girls and 3.5% (95% CI: 2.7 to 4.5) of boys reported unwanted sexual activities involving touching, while 5.3% (95% CI: 4.4 to 6.4) of girls and 1.4% (95% CI: 0.9 to 2.1) of boys reported forced sexual relations involving penetration, for an overall prevalence of 14.9% (95% CI: 13.1 to 16.9) for teenage girls and 3.9% (95% CI: 3.0 to 5.1) for teenage boys. Both unwanted touching (χ2 = 261.75, P < .001) and abuse involving penetration (χ2 = 83.03, P < .001) were reported more frequently by girls compared to boys. Table 1 presents the prevalence of mental health problems, health services utilization, and health-risk behaviors among girls and boys with and without experience of child sexual abuse. Main effects of child sexual abuse status were found for all variables. Gender effects revealed that overall, girls were more likely to report psychological distress, PTSD, suicidal ideation and attempts, and health service utilization than boys, while boys were more likely to report delinquent behaviors compared to girls. Significant Gender × Child Sexual Abuse Status interactions were found for alcohol, Wald F(1, 26) = 17.09, P < .001; cannabis use, Wald F(1, 26) = 8.80, P < .01; and for self-esteem, Wald F(1, 26) = 11.41, P < .01. Results indicate that the association between child sexual abuse and cannabis use was greater for girls compared to boys, while the association between child sexual abuse and low levels of self-esteem was greater for teenage boys compared to teenage girls. Finally, while girls with a history of child sexual abuse were more likely to report problematic consumption of alcohol compared to nonabused girls, there was no difference for boys.
Figure 1.
Prevalence of child sexual abuse by gender.
Table 1.
Prevalence of Mental Health Problems, Health Services Utilization, and Health-Risk Behaviors.
| Girls | Boys | |||
|---|---|---|---|---|
| Non-CSA % (95% CI) | CSA % (95% CI) | Non-CSA % (95% CI) | CSA % (95% CI) | |
| PTSD | 12.2 (11.0 to 13.4) | 30.0 (25.5 to 34.9) | 4.6 (3.7 to 5.6) | 17.0 (11.2 to 24.9) |
| Psychological distress | 38.8 (36.7 to 41.0) | 61.3 (57.6 to 64.9) | 17.2 (15.3 to 19.3) | 41.6 (33.3 to 50.5) |
| Suicidal ideation | 26.7 (24.4 to 29.2) | 55.2 (51.0 to 59.4) | 18.9 (17.0 to 21.0) | 46.5 (37.0 to 56.2) |
| Suicidal attempt | 8.7 (7.5 to 10.0) | 30.3 (25.8 to 35.1) | 4.3 (3.4 to 5.4) | 19.6 (13.1 to 28.2) |
| Low self-esteem | 38.2 (35.9 to 40.7) | 49.7 (45.7 to 53.7) | 23.5 (21.6 to 25.6) | 47.9 (38.6 to 57.4) |
| Health services utilization | 30.0 (26.7 to 33.6) | 52.5 (47.6 to 57.3) | 20.6 (18.6 to 22.8) | 38.7 (30.5 to 47.6) |
| Alcohol abuse | 33.7 (28.4 to 39.4) | 51.6 (45.6 to 57.6) | 43.2 (38.5 to 48.1) | 46.0 (38.2 to 54.1) |
| Cannabis abuse | 24.0 (19.5 to 29.1) | 45.6 (39.9 to 51.3) | 31.7 (27.9 to 35.7) | 43.3 (33.7 to 53.4) |
| Other drugs | 7.6 (5.7 to 10.0) | 21.5 (17.4 to 26.2) | 8.1 (6.6 to 9.9) | 22.4 (13.4 to 35.1) |
| Delinquency | 39.1 (36.7 to 41.6) | 66.9 (62.1 to 71.4) | 57.0 (53.0 to 60.8) | 84.1 (74.3 to 90.7) |
Note. CSA = child sexual abuse; PTSD = post-traumatic stress disorder; CI = confidence interval.
Multiple logistic regression models were then used to explore the association between child sexual abuse and mental health, health service utilization, and health-risk indicators while first controlling for sociodemographic covariates (OR1), then while further controlling for other forms of childhood maltreatment (OR2). The results are reported in Table 2.
Table 2.
Odds Ratios (and 95% Confidence Intervals) from Logistic Regression Analyses Assessing Associations between Child Sexual Abuse and Outcomes.
| Mental health problems and health-risk behaviors | Girls | Boys |
|---|---|---|
| PTSD | ||
| Adjusted OR1 (95% CI) | 2.94*** (2.43 to 3.56) | 3.84*** (2.11 to 7.01) |
| Adjusted OR2 (95% CI) | 2.54*** (1.98 to 3.24) | 2.73** (1.58 to 4.70) |
| Psychological distress | ||
| Adjusted OR1 (95% CI) | 2.16*** (1.87 to 2.49) | 2.82*** (1.98 to 4.02) |
| Adjusted OR2 (95% CI) | 1.88*** (1.62 to 2.18) | 2.22*** (1.57 to 3.14) |
| Suicidal ideation | ||
| Adjusted OR1 (95% CI) | 3.20*** (2.79 to 3.67) | 3.31*** (2.24 to 4.89) |
| Adjusted OR2 (95% CI) | 2.50*** (2.07 to 3.02) | 2.64*** (1.58 to 4.41) |
| Suicidal attempt | ||
| Adjusted OR1 (95% CI) | 4.35*** (3.63 to 5.21) | 4.69*** (2.67 to 8.23) |
| Adjusted OR2 (95% CI) | 3.35*** (2.74 to 4.10) | 3.64*** (1.96 to 6.75) |
| Low self-esteem | ||
| Adjusted OR1 (95% CI) | 1.56*** (1.33 to 1.83) | 2.86*** (1.96 to 4.18) |
| Adjusted OR2 (95% CI) | 1.30** (1.10 to 1.54) | 2.01** (1.23 to 3.28) |
| Health services utilization | ||
| Adjusted OR1 (95% CI) | 2.48*** (2.04 to 3.01) | 2.23*** (1.49 to 3.35) |
| Adjusted OR2 (95% CI) | 2.15*** (1.76 to 2.63) | 1.84* (1.15 to 2.96) |
| Alcohol abuse | ||
| Adjusted OR1 (95% CI) | 2.06*** (1.74 to 2.44) | 1.14 (0.84 to 1.55) |
| Adjusted OR2 (95% CI) | 1.87*** (1.57 to 2.22) | 1.03 (0.73 to 1.46) |
| Cannabis abuse | ||
| Adjusted OR1 (95% CI) | 2.54*** (2.13 to 3.02) | 1.59* (1.11 to 2.27) |
| Adjusted OR2 (95% CI) | 2.18*** (1.84 to 2.59) | 1.28 (0.88 to 1.84) |
| Other drugs | ||
| Adjusted OR1 (95% CI) | 3.18*** (2.16 to 4.70) | 2.91*** (1.66 to 5.11) |
| Adjusted OR2 (95% CI) | 2.58*** (1.77 to 3.77) | 2.13* (1.21 to 3.73) |
| Delinquency | ||
| Adjusted OR1 (95% CI) | 2.98*** (2.46 to 3.61) | 3.55*** (2.25 to 5.59) |
| Adjusted OR2 (95% CI) | 2.21*** (1.76 to 2.78) | 2.26** (1.27 to 4.03) |
Note. PTSD = post-traumatic stress disorder; adjusted OR1 = odds ratio adjusted for sociodemographic variables (grade level, family structure, ethnicity); adjusted OR2 = odds ratio adjusted for sociodemographic variables listed above and other forms of child maltreatment; CI = confidence interval.
*P < .05. **P < .01. ***P < .001.
Findings showed that for girls, after accounting for sociodemographic characteristics, child sexual abuse was significantly associated with greater odds of presenting psychological distress and lower self-esteem. Girls with a history of child sexual abuse were at close to a 3-fold risk of PTSD and suicidal ideations. They were also at 4-fold risk of suicidal attempts and 2-fold risk of psychological distress. Adjusting for other forms of childhood maltreatment had little appreciable impact on the strength of the associations between child sexual abuse and outcomes for girls. Similar results were found for health services utilization, with sexually abused girls twice as likely to report using health services for psychological problems. Girls with a history of sexual abuse were also more likely to display health-risk behaviors with ORs varying from 1.87 to 2.58 for alcohol and drug abuse and delinquency.
A similar picture emerged for boys. Sexually abused boys were close to twice as likely to report low self-esteem and clinical levels of psychological distress, suicidal ideations, and more than three times more likely to report suicidal attempts even after adjusting for other forms of child maltreatment experienced. Child sexual abuse was also associated with greater odds of post-traumatic stress symptoms (OR = 2.73; 95% CI, 1.58 to 4.70) and of health services utilization (OR = 1.84; 95% CI, 1.15 to 2.96). Regarding health-risk behaviors among boys, child sexual abuse was linked to drug abuse and delinquency in models accounting for sociodemographic variables. Yet, when other forms of childhood maltreatment experiences were added to the model, a history of child sexual abuse no longer predicted cannabis use but was still associated with a heightened risk of delinquency and use of other drugs.
Discussion
The purpose of the present study was to document the prevalence of child sexual abuse in a sample of Quebec High School youth and examine the association between mental health problems and such trauma. Results revealed that within this sample of teenagers aged 15.35 years on average, 14.9% of girls and 3.9% of boys reported having experienced child sexual abuse. Direct comparisons with past studies remain hazardous given sample differences in age groups, and definitional issues, as some surveys only took into account sexual abuse perpetrated by an adult. Nonetheless, the rates approximate those found in the 2018 BC Adolescent Health Survey conducted with a representative sample of adolescents aged 12 to 19 in British Colombia, in which 17% of girls and 5% of boys reported having been sexually abused.28 The prevalence rates are also comparable to sexual assault lifetime estimates (17.4% of girls and 4.2% of boys) found in a sample of youth aged 14 to 17 years reported in a national survey conducted in the United States.29 Our findings also showed that both sexual abuse involving unwanted touch and abuse involving penetration were more prevalent among girls than boys. These results are consistent with past studies reporting prevalence of child sexual abuse 2 to 3 times higher for girls than boys.1
As per past findings mainly derived from clinical or convenience samples, our results revealed that child sexual abuse is associated with multiple negative correlates for both girls and boys. Close to half of teenagers with a history of sexual abuse presented with clinical levels of psychological distress, low self-esteem, and suicidal ideations. About one in three girls and one in five sexually abused boys reported attempting suicide. Even after controlling for other forms of childhood maltreatment, child sexual abuse is linked to a 2-fold to more than 3-fold risk of significant distress including post-traumatic stress symptoms, delinquency, suicidal ideations and attempts. As for the prevalence of child sexual abuse, our results on the plurality of difficulties associated with child sexual abuse are consistent with past studies involving populations of high school teenagers. For example, in the BC Adolescent Health Survey, sexual violence was linked to a heightened risk of suicide attempts for both boys and girls.30
Our results suggest few gender differences in the association between child sexual abuse and the correlates examined while controlling for other forms of maltreatment. Our findings thus concur with past studies conducted with clinical samples of minor victims of sexual abuse and failed to identify gender differences in the severity of internalized, externalized, and trauma symptoms.31,32
Yet, despite the similarities in the association between child sexual abuse and health problems in teenage girls and boys, some specificities were identified. Indeed, for girls, while child sexual abuse appears to exert an independent effect on all variables considered even after controlling for other forms of childhood maltreatment, no effects were found for boys in regard to problematic alcohol consumption and cannabis use. Past studies have suggested that motives for alcohol consumption may be different for men and women.33 Heightened consumption of alcohol or cannabis following trauma may reflect a coping mechanism to deal with negative affect in teenage girls, while for boys, it may be more socially acceptable and represent a salient coping strategy to deal with a number of stressors in adolescence and not specifically for dealing with negative emotions associated with child sexual abuse. Finally, the difference in the proportion of teenagers presenting with low levels of self-esteem according a history of child sexual abuse is particularly salient for boys. These findings suggest that child sexual abuse may exert a more important impact on the sense of self of boys, as being abused and feeling powerless might be particularly threatening for boys as it contradicts masculinity norms which prescribe being aggressive, powerful and dominant.34
In sum, our findings highlight that experiencing child sexual abuse independently carries a higher risk of negative mental health outcomes for both teenage boys and girls. Our results also reveal that child sexual abuse is associated with an increased economic burden with victims twice as likely to report health services utilization. Although a direct comparison cannot be made, the results are in line with a study showing that adult victims of sexual abuse were at 3 times higher risk to rate their health as poor.4 Another study among youths aged 8 to 21 in foster care showed that sexual abuse was an independent predictor of health service utilization after accounting for the effect of chronic illness.35
Although our analyses provided pertinent information on the correlates of child sexual abuse in teenagers, the study has limitations. Within the cross-sectional design, exposure to child sexual abuse and the different outcomes were measured at the same time. In addition, given the nature of some of the questions (e.g., evaluating lifetime suicidal ideations), the outcome may have occurred before the exposure to child sexual abuse. Future studies would benefit from relying on a longitudinal design and including multiple assessments over time to assess the trajectories of mental health outcomes. Given the secrecy and taboos surrounding child sexual abuse, underreporting is an issue to be considered, especially for boys often facing additional barriers to disclosure.36 While the sample is representative of Quebec high school students, it did not include youth who might have been particularly vulnerable to sexual abuse such as school dropouts. In addition, the delay between child sexual abuse and the correlates was not evaluated; the delay might impact on the strength of the associations found. However, despite these limitations, our study has a number of strengths including being based on a large representative sample of high school youth, which offered the possibility of ascertaining negative outcomes associated with child sexual abuse for both adolescent girls and adolescent boys. We examined associations between child sexual abuse and several indicators of mental health problems and health-risk behaviors as well as health services utilization. Moreover, our analysis controlled for other forms of childhood maltreatment experienced to isolate correlates associated with child sexual abuse. In addition, past research findings are often based on samples that involve insufficient number of boys and the extent to which findings generalize to teenage boys remained unclear.8,31 Our findings suggest that CSA is associated with psychological health issues not only for girls but for boys as well.
Conclusion
Unfortunately, a significant number of youths are sexually victimized in their childhood. Our findings concur with past studies suggesting the child sexual abuse is associated with mental health issues and health-risk behaviors. The prevalence of child sexual abuse and its negative correlates clearly call for policies and prevention programs aiming to reduce the occurrence of child sexual abuse. Early sex education and prevention programs are clearly warranted. Training for all practitioners across the health sector to foster early detection of cases of child sexual abuse is also an avenue to prioritize. Given that boys may be less likely to disclose,13,37 exploring and addressing the many barriers to their help-seeking is also an objective to aim for. Furthermore, it is essential that policy makers and health professionals adopt a trauma-informed approach recognizing both the impact of trauma and the vast array of symptoms associated with trauma, while promoting practices fostering recovery in vulnerable youth. Evidence-based treatment models such as trauma-focused cognitive behavioral therapy that can foster recovery in youth survivors of child sexual abuse38 need to be widely implemented. In addition, systematic and repeated surveys would allow to track trends over time and monitor possible changes in the prevalence of child sexual abuse, given evolution of social norms as well as public policies implemented to tackle this important public health issue.
Acknowledgments
The authors wish to thank all the teenagers who participated in the study. Their thanks also extend to Catherine Moreau for project coordination and Manon Robichaud for management of the database.
Footnotes
Data Access: Data are not publicly available due to confidentiality reasons in accordance with ethics approval given by the ethics board from the participating university. Interested investigators may submit inquiries to the corresponding author.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by a grant (103944) from the Canadian Institutes of Health Research awarded to the first author.
ORCID iD: Martine Hébert, PhD  https://orcid.org/0000-0002-4531-5124
https://orcid.org/0000-0002-4531-5124
References
- 1. Barth J, Bermetz L, Heim E, Trelle S, Tonia T. The current prevalence of child sexual abuse worldwide: a systematic review and meta-analysis. Int J Public Health. 2013;58(3):469–483. [DOI] [PubMed] [Google Scholar]
- 2. Maniglio R. The impact of child sexual abuse on health: a systematic review of reviews. Clin Psychol Rev. 2009;29(7):647–657. [DOI] [PubMed] [Google Scholar]
- 3. Afifi TO, MacMillan HL, Boyle M, et al. Child abuse and mental disorders in Canada. CMAJ. 2014;186(9):E324–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Afifi TO, MacMillan HL, Boyle M, Taillieu T, Cheung K, Sareen J. La maltraitance à l’égard des enfants et la santé physique à l’âge adulte [Child abuse and physical health in adulthood]. Rapports Sur la Santé [Heatlh Reports]. 2016;27(3):11–20. [PubMed] [Google Scholar]
- 5. MacMillan HL, Fleming JE, Streiner DL, et al. Childhood abuse and lifetime psychopathology in a community sample. Am J Psychiatry. 2001;158(11):1878–1883. [DOI] [PubMed] [Google Scholar]
- 6. Duell N, Steinberg L, Icenogle G, et al. Age patterns in risk taking across the world. J Youth Adolesc. 2018;47(5):1052–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Turner HA, Finkelhor D, Ormrod R. Poly-victimization in a national sample of children and youth. Am J Prev Med. 2010;38(3):323–330. [DOI] [PubMed] [Google Scholar]
- 8. Lewis T, McElroy E, Harlaar N, Runyan D. Does the impact of child sexual abuse differ from maltreated but non-sexually abused children? A prospective examination of the impact of child sexual abuse on internalizing and externalizing behavior problems. Child Abuse Negl. 2016;51:31–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kozak RS, Gushwa M, Cadet TJ. Victimization and violence: an exploration of the relationship between child sexual abuse, violence, and delinquency. J Child Sex Abuse. 2018;27(6):699–717. [DOI] [PubMed] [Google Scholar]
- 10. Tabachnick BG, Fidell LS. Using multivariate statistics. 6th ed Harlow: Pearson Education Limited; 2013. p. 1072. [Google Scholar]
- 11. Brislin RW. Back-translation for cross-cultural research. J Cross Cult Psychol. 1970;1(3):185–216. [Google Scholar]
- 12. Finkelhor D, Hotaling G, Lewis IA, Smith C. Sexual abuse in a national survey of adult men and women: prevalence, characteristics, and risk factors. Child Abuse Negl. 1990;14(1):19–28. [DOI] [PubMed] [Google Scholar]
- 13. Hébert M, Tourigny M, Cyr M, McDuff P, Joly J. Prevalence of childhood sexual abuse and timing of disclosure in a representative sample of adults from Quebec. Can J Psychiatry. 2009;54(9):631–636. [DOI] [PubMed] [Google Scholar]
- 14. Bremner JD, Bolus R, Mayer EA. Psychometric properties of the Early Trauma Inventory–Self report. J Nerv Ment Dis. 2007;195(3):211–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Armsden GC, Greenberg MT. The inventory of parent and peer attachment: individual differences and their relationship to psychological well-being in adolescence. J Youth Adolesc. 1987;16(5):427–454. [DOI] [PubMed] [Google Scholar]
- 16. Straus MA, Hamby SL, Boney-McCoy S, David BS. The Revised Conflict Tactics Scales (CTS2): development and preliminary psychometric data. J Fam Issues. 1996;17(3):283–316. [Google Scholar]
- 17. Cohen JA, Issues TW, AACAP Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with posttraumatic stress disorder. J Am Acad Child Adolesc Psychiatry. 2010;49(4):414–430. [PubMed] [Google Scholar]
- 18. Steinberg AM, Brymer MJ, Decker KB, Pynoos RS. The University of California at Los Angeles post-traumatic stress disorder reaction index. Curr Psychiatry Rep. 2004;6(2):96–100. [DOI] [PubMed] [Google Scholar]
- 19. Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–976. [DOI] [PubMed] [Google Scholar]
- 20. Boak A, Hamilton HA, Adlaf EM, et al. The mental health and well-being of Ontario students, 1991–2013: detailed OSDUHS findings. Toronto (ON): Centre for Addiction and Mental Health; 2014. CAMH Research Document Series No. 38. [Google Scholar]
- 21. Sampasa-Kanyinga H, Willmore J. Relationships between bullying victimization psychological distress and breakfast skipping among boys and girls. Appetite. 2015;89:41–46. [DOI] [PubMed] [Google Scholar]
- 22. Marsh HW, O’Neill RO. Self-description questionnaire III: the construct validity of multidimensional self-concept ratings by late adolescents. J Educ Meas. 1984;21(2):153–174. [Google Scholar]
- 23. Statistique Canada. Matériel d’enquête 2006–2007—Cycle 7—Livre 2—Questionnaire du jeune. Ottawa: Statistique Canada, Enquête longitudinale nationale sur les enfants et les jeunes; 2007. [Google Scholar]
- 24. Garriguet D. Early sexual intercourse. Health Rep. 2005;16(3):9–18. [PubMed] [Google Scholar]
- 25. Centre for Addiction and Mental Health [CAMH]. Ontario Student Drug Use and Health Survey (OSDUHS), 1977-2011: Questionnaire. Toronto (ON): Centre for Addiction and Mental Health; 2011. [Google Scholar]
- 26. Harris KM, Halpern CT, Entzel P, et al. The national longitudinal study of adolescent health: research design. 2009; Available from: http://www.cpc.unc.edu/projects/addhealth/design.
- 27. Landry M, Tremblay J, Guyon L, Bergeron J, Brunelle N. La grille de dépistage de la consommation problématique d’alcool et de drogues chez les adolescents et les adolescentes (DEP-ADO): développement et qualités psychométriques. Drogues, Santé et Société. 2004;3(1):20–37. [Google Scholar]
- 28. Smith A, Forsyth K, Poon C, Peled M. Balance and connection in BC: the health and well-being of our youth. Vancouver (BC): McCreary Centre Society; 2019. [Google Scholar]
- 29. Finkelhor D, Turner HA, Shattuck A, Hamby SL. Violence, crime, and abuse exposure in a national sample of children and youth: an update.JAMA Pediatr. 2013;167(7):614–621. [DOI] [PubMed] [Google Scholar]
- 30. Saewyc EM, Chen W. To what extent can adolescent suicide attempts be attributed to violence exposure? A population-based study from Western Canada. Can J Commun Ment Health. 2013;32(1):79–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Maikovich-Fong AK, Jaffee SR. Sex differences in childhood sexual abuse characteristics and victims’ emotional and behavioral problems: Findings from a national sample of youth. Child Abus Negl. 2010;34(6):429–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Soylu N, Ayaz M, Gökten ES, et al. Gender differences in sexually abused children and adolescents: a multicenter study in Turkey. J Child Sex Abuse. 2016;25(4):415–427. [DOI] [PubMed] [Google Scholar]
- 33. Goldstein AL, Flett GL, Wekerle C. Child maltreatment, alcohol use and drinking consequences among male and female college students: an examination of drinking motives as mediators. Addic Behav. 2010;35(6):636–639. [DOI] [PubMed] [Google Scholar]
- 34. Price-Roberston R. Child sexual abuse, masculinity and fatherhood. J Fam Stud. 2012;18(2–3):130–142. [Google Scholar]
- 35. Jackson Y, Cushing CC, Gabrielli J, Fleming K, O’Connor BM, Huffhines L. Child maltreatment, trauma, and physical health outcomes: the role of abuse type and placement moves on health conditions and service use for youth in foster care. J. Pediatr Psychol 2015;41(1):28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gagnier C, Collin-Vézina D. The disclosure experiences of male child sexual abuse survivors. J Child Sex Abuse. 2016;25(2);221–241. [DOI] [PubMed] [Google Scholar]
- 37. Okur P, van der Knaap LM, Bogaerts S. A quantitative study on gender differences in disclosing child sexual abuse and reasons for nondisclosure. J Interpers Violence. 2017. Advanced online publication. [DOI] [PubMed] [Google Scholar]
- 38. Cohen JA, Deblinger E, Mannarino AP. Trauma-focused cognitive behavioral therapy for children and families. Psychother Res. 2018;28(1):47–57. [DOI] [PubMed] [Google Scholar]