Abstract
Two different treatment paradigms are most often used in multiple sclerosis (MS). An escalation or induction approach is considered when treating a patient early in the disease course. An escalator prioritizes safety, whereas an inducer would favor efficacy. Our understanding of MS pathophysiology has evolved with novel in vivo and in vitro observations. The treatment landscape has also shifted significantly with the approval of over 10 new medications over the past decade alone. Here, we re-examine the treatment approach in light of these recent developments. We believe that recent work suggests that early prediction of the disease course is fraught, the amount of damage to the brain that MS causes is underappreciated, and its impact on patient function oftentimes is underestimated. These concerns, coupled with the recent availability of agents that allow a better therapeutic effect without compromising safety, lead us to believe that initiating higher efficacy treatments early is the best way to achieve the best possible long-term outcomes for people with MS.
MS is a chronic autoimmune disorder resulting in accumulated damage to the brain, spinal cord, and optic nerves that can lead to significant neurologic disability. Two and a half decades after the first drug approval for MS, no consensus has been achieved regarding which treatments should be most often used with practices varying widely1 and recently published international consensus guidelines differing.2,3
Two potential treatment frameworks have been articulated. Some advocate an escalation approach, positing that a premium should be placed on safety. The argument continues that if during prospective monitoring a patient experiences breakthrough disease as evinced by relapses, MRI change, or disability, then strong consideration should be given to switching to an agent with increased efficacy. In this way, patients who do not require stronger medicines are spared potential side effects and safety concerns. A second model is an “induction” or, better named, a highly effective treatment early approach (HETA). Proponents of the HETA contend that a neurologist's current ability at initial presentation to predict the long-term outcome is limited. They also argue that a neurologist's ability to prospectively determine whether ongoing damage to the nervous system is occurring is limited. In addition, HETA advocates view the risk profile of some highly efficacious drugs as not materially worse than less efficacious treatments.
A number of thoughtful articles considering whether higher efficacy agents should be used early have been published. Nevertheless, we believe it is time to re-examine these frameworks in more detail, given the accumulating research on pathology, imaging, and disease course and in light of the evolving treatment landscape. Here, we elaborate on why we believe a HETA is warranted for most patients with MS early in disease (age <40 years old).
Our ability to predict disease course at onset is limited
Clinicians oftentimes discuss how they use factors that have been identified in the literature as carrying a poor prognosis to guide the choice of high- vs low-efficacy medication start. Commonly cited demographic factors for poorer outcomes include older age at onset, male sex, race, and motor or cerebellar presentation. In fact, the relationship between these factors and prognosis in longitudinal patient cohorts is fair at best. Weinshenker et al. 4 reported a significant effect of the above-cited factors on whether patients were liable to progress to an Expanded Disability Status Scale (EDSS) score of 6 (requires unilateral assistance). However, the reported absolute coefficients of magnitude for the effect are underwhelming with male sex increasing the chance of reaching a DSS of 6 by 0.17, age at onset of 0.03, motor symptoms at onset of 0.21, and limb ataxia/balance symptoms at onset of 0.29. In a separate cohort, Tremlett et al.5 reported similar weak effects with male sex contributing a 1.1 hazard relative to female sex and motor onset of symptoms with a hazard ratio of 1 to probability of reaching an EDSS of 6. Other large cohort studies do not present the effect on the overall risk of achieving EDSS in a readily applicable way. A study examining the effect of African American race on EDSS progression failed to show an effect.6 Cohort studies examining whether demographic factors influence the risk of developing progressive disease report similar weak effects. Another cohort reported that sex and symptom type at presentation do not influence the risk of conversion to secondary progressive MS (SPMS), whereas age at disease onset has little influence (hazard ratio 1.02) although statistically significant.7 A study of over 8,000 patients found that the type of attack (monofocal vs polyfocal) was not predictive of conversion to SPMS, whereas the magnitude of the effect for sex (−1.24 for women) and onset age (−0.93) was small although statistically significant.8
Conventional clinical imaging can miss or underestimate ongoing damage
When “normal-appearing white matter” is examined with immunohistochemical techniques, more damaged axons are seen in patients with MS than in normal controls.9 As the MRI magnet strength increases, better fit is obtained with clinical measures, and even at the highest available strengths, correlations are fair at best.10 Studies comparing 1.5T and 7T MRI for detecting white matter and cortical lesions identify a markedly increased yield at 7T.11 In addition, the above-referenced study by Sinnecker et al. reported that every T2 hyperintensity visualized in the brain was hypointense on magnetization prepared rapid acquisition with gradient echo at 7T, suggesting that all MS lesions are in fact “black holes.” Even then, 7T imaging is an imperfect tool. Pitt et al.12 reported that 7T MRI visualized 82%–93% of cortical lesions apparent at pathology. Measures of whole-brain atrophy and gray matter atrophy correlate cross-sectionally better with clinical disability than conventional measures such as T2 lesion volume, T1 hypointensities, and gadolinium enhancing lesions,13 but such measures are not available in routine clinical practice. Novel imaging techniques such as diffusion tensor imaging (DTI), magnetization transfer ratio (MTR), and 23Na MRI imaging all demonstrate that more damage is present than is visualized on conventional MRI. Imaging of diffusion of water along axonal tracts (DTI) with sophisticated processing has suggested that the contribution of white matter abnormalities to cognitive impairment is determined by damage in the otherwise normal-appearing white matter and that this association is in part independent of gray matter volume atrophy and lesion load.14 23Na MRI imaging allows direct visualization of ongoing cellular dysfunction and cell death. This is found to be abnormal in both lesioned areas of the brain and normal-appearing white matter.15 A study of 45 patients with newly diagnosed relapsing-remitting MS found a decrease of whole-brain cerebral viscoelasticity relative to matched healthy volunteers and suggested a more widespread disturbance of tissue integrity than expected from the few visible T2 lesions.16 A measure of macromolecular integrity, MTR is reduced in normal-appearing white and gray matter from patients even at the earliest clinical stages of the disease17 with reduced MTR correlated with disability18 and cognitive impairment.19
MS is rarely benign over the long term when dysfunction is carefully interrogated
Many MS clinicians will discuss patients who have been maintained off treatment or on low efficacy treatment that have done “well.” One might wonder, however, what qualifies as well? Would this patient be in the same condition if they did not have MS? As clinicians, how hard are we looking?
A recent report from Tallantyre et al.20 found that in a carefully examined untreated population with disease duration >15 years, 2.9% of patients had “benign” disease as defined by an EDSS <3, no significant fatigue, mood disturbance, cognitive impairment, or disrupted employment. Indeed, the absolute number of patients identified is instructive with only 9 patients in a cohort of 1,049 patients included for analysis classified as truly benign.
Recent patient survey work and disability claims reveal significant disability over time. In the North American Research Committee on Multiple Sclerosis (NARCOMS) database of patients mostly treated at 15 years after diagnosis, only 13% of patients reported no or mild symptoms. Moderate or greater disability was reported by >40% of patients in hand function, vision, cognition, bowel/bladder function, spasticity, pain, fatigue, and coordination. At 30 years, moderate or greater disability was reported for mobility in 69%, hand function in 60%, vision in 47%, cognition in 50%, bowel/bladder function in 70%, spasticity in 65%, pain in 64%, depression in 35%, fatigue in 72%, and tremor/coordination in 51%.21
A recent survey of NARCOMS participants with a mean age of 55 years found that 58% of patients were not working, with 48.5% of those surveyed received disability benefits. Of those employed, 27% reported missing 6 days or more of work a year. Moderate to severe cognitive impairment, fatigue, and hand function problems were associated with both disability and absenteeism.22
Of adults 65 years or older, 15% of patients without MS reported using an assistive device, whereas 81% of patients with MS required an assistive device in the NARCOMS cohort, a 6-fold difference.23,24
Long-term follow-up studies of patients on platform agents reveal the risks of undertreatment
An extension of the pivotal glatiramer acetate trial found that of patients who were maintained on treatment for an average of 13.6 years, 35% were likely to develop secondary progressive disease. When considering disability progression, 59% progressed to at least an EDSS of 4, with 18% worsening to an EDSS of 6, and 3% reaching an EDSS of 8.25 A follow-up study of patients enrolled in the interferon (IFN) β-1a subcutaneous (SC) pivotal trial26 reported that of those receiving IFN β-1a SC 44mcg regularly for at least 7 years, 23.9% progressed to an EDSS of 4, 19.7% to an EDSS of 6, 12% to an EDSS of 6.5, and 6.1% to an EDSS of 7, with a mean increase in EDSS in both treated groups (22 and 44 μg) of 1.1 and mean EDSS score of 3.5 at the last visit. When considering the long-term follow-up group as a whole (22 and 44 μg doses), 19.7% were found to have converted to SPMS. Of patients taking IFN β-1b assessed at the 16-year pivotal phase III follow-up,27 45.8% had reached an EDSS of 6. These lackluster results are despite these studies being subject to corruption by survivorship bias so that patients who are not doing well drop out of the treated group or might not be assessed in the follow-up, potentially leading these studies to report better outcomes than those that truly exist. Some would interpret these results as positive and that those included who have suffered from long-standing neurologic illness are “well enough,” given that they have had the disease for some time. We do not believe that this is acceptable and take as our goal that patients track in a similar way to individuals not diagnosed with MS. One might also question how accurately the EDSS reflects true disability, given only fair inter-rater and intra-rater reliability at lower levels of the scale and less sensitivity at higher levels with ambulatory dysfunction primarily determining the level in the upper ranges.28
More efficacious MS drugs, which better control inflammatory disease, are not a panacea. Studies of even the most effective agents available for MS indicate that no evidence of disease activity (NEDA) is achieved in only 47.7% of ocrelizumab-treated patients29 when followed up for 96 weeks and 29.5% of natalizumab-treated patients followed up for 2 years.30 So, even with best possible efficacy, an argument can be lodged that our treatments are not fully adequate.
Short-term comparison studies demonstrate superiority in reduction of relapses, MRI change, and disability progression for some agents
Good quality evidence suggests that ocrelizumab and alemtuzumab are more effective than IFN β-1a SC31–33 and fingolimod is more effective than IFN β-1a IM34 in a selected patient group. There is also MRI evidence that dimethyl fumarate better attenuates new MRI lesions than glatiramer acetate, although clinical outcomes over the 2-year trial were mixed.35 We have been cautioned by statisticians not to compare across trials, but these head-to-head comparisons are informative.
The reported safety profiles of some highly effective agents do not currently materially differ from lower efficacy agents
The risk of developing progressive multifocal leukoencephalopathy (PML) in a John Cunningham virus antibody-negative natalizumab-treated patient is estimated at 1:10,00036 and may be further reduced with extended interval dosing.37 Natalizumab is otherwise generally well tolerated with a paucity of other potential side effects. In a population with rheumatoid arthritis, the risk of rituximab with long-term use is estimated to be 1:30,000.38 Some groups have conducted retrospective analysis on the long-term safety of rituximab in their patients with MS and found few adverse events.39,40 The safety profile of ocrelizumab is being defined with time, but based on the molecular structure, one might expect a similar profile to that of rituximab. So far, a single case of PML has been reported that can be directly attributed to ocrelizumab monotherapy. The imbalance of breast cancer seen in trials requires further monitoring in the future, but a long-term cohort treated with ocrelizumab does not vary in cancer risk from risk estimates in a general population and MS non--ocrelizumab-treated group.41 Although ostensibly high-efficacy agents' safety may be in line with that seen in lower efficacy agents, further definition of the safety profile with time will be paramount. It seems short sighted, however, to allow greater CNS tissue loss now because of worry about drug side effects not currently manifest, especially given a lack of definite mechanistic rationale to support safety concerns.
The challenges of patient preference and adherence, therapeutic inertia, and insurance coverage
Other barriers exist to HETA implementation. Patient preference is a fundamental part of medication selection. The literature indicates that patient preferences may not be in line with an appropriate treatment approach. Patients with longer disease duration prefer more efficacious therapies42 and tend to underestimate therapy risks and overestimate benefits.43 This approach may be counter to disease biology, which likely benefits from the use of higher efficacy agents earlier in the disease.
In addition, adherence and persistence remain a challenge with a retrospective claims analysis finding that only between 52% and 62% of patients had injectable medication in their possession 80% of the time.44 Adherence is better but also not ideal with oral treatments with a claims database analysis finding that 80% medication possession was seen in 98.2% of patients on fingolimod and 87.8% on dimethyl fumarate.45 It is already a challenge to treat patients adequately even if a patient is fully adherent.
Health insurance is another potential hurdle. Over 6% of the patients do not receive treatment because of financial concerns and insurance barriers.46 Governmental and private insurers struggle to construct policies without consensus from the MS community regarding treatment. Developed policies can prevent patient access to highly effective therapies by requiring step edits before approval. These policies may do patients harm, leading to a delayed start of the most appropriate treatments. Recent understandings and trial data raise a concern that insurers that restrict patients with MS access to highly effective immunotherapies may not only be damaging their long-term financial interest but also acting unethically.
Early intervention might substantively alter disease course and prevent irreversible progression, whereas later treatment might not confer much benefit
Scalfari et al.47 reported that relapses which occur in the first 2 years influence the disease course, whereas relapses that occur after this do not. A nationwide Danish registry found that patients left untreated for 2 years after MS symptom onset reached an EDSS of 6 faster than those treated and trended toward experiencing an earlier death.48 A meta-analysis of MS clinical trials found a larger reduction in relapses and MRI damage in a younger patient group, with a lack of difference between treated and untreated patients seen in patients older than age 40.5 years.49 A population-based cohort in the United Kingdom found that patients (n = 104) treated initially with highly effective therapy had a lower mean change in EDSS at 5 years and a higher median time to sustained accumulation of disability than those treated with moderately effective therapies (n = 488). This effect persisted after adjustment for covariates including age and sex.50
Once inflammatory nervous system damage occurs, other downstream effects might be seen including mitochondrial dysfunction, oxidative damage from iron deposition, microglial activation, and glutamate toxicity, which might cause additional neuronal damage and propagate a feed-forward loop.51 Damage to the nervous system early in the disease is oftentimes well compensated for initially but becomes apparent after reserve is lost, typically decades after disease onset.52 Keegan et al.53 reported that progressive lower extremity weakness can be traced to critically placed lesions in the corticospinal tract, most often in the spinal cord. Once patients reach a DSS of 4, progression to cane dependence (DSS of 6) occurs independent of relapses.54
Indeed, a rational interpretation of the published literature might be to use a HETA in patients younger than 40 years of age with a de-escalation strategy used in an older patient group who experience immune senescence and who could be at more risk of infections and other potential complications.
If the working theories described above are correct, then, one would expect that more effectively preventing inflammation early would result in better protection from irreversible disability. This seems to be the case. The MSBase consortium recently analyzed a cohort of 1,555 patients with MS and found that individuals treated with higher efficacy agents developed secondary progressive disease later.55
The perils of escalation
Neurologists choosing an escalation path face challenges. Therapeutic inertia may contribute to the loss of brain tissue in patients with MS. Harding et al.50 found a median delay of 2.4 years in patients who escalated disease-modifying agents. Another issue is a period of vulnerability that may exist in treatment transitions. Drugs may be sequenced too closely together, temporally resulting in harmful effects. A more frequent harm is loss of nervous system tissue related to a therapeutic gap during treatment transitions, with potential relapses, MRI activity, or disability accrual as a result.56 Neurologists choosing more efficacious agents will less often need to transition medications and expose their patients less to these potential dangers.
In addition, a neurologist waiting for “efficacy failure” may be engaged in a frivolous exercise. Our current ability to monitor disease using clinical and radiologic measures is fair at best. Studies evaluating the prognostic value of NEDA find that it is poorly predictive of the outcome over the longer term.57,58 Ongoing brain structural damage (as measured by DTI) has been reported in patients who meet NEDA criteria.59 As such, a neurologist looking for overt signs of drug failure as manifest by clinical or MRI change may be ill advised. We believe a recent study helped expose the conceptual fallacy of switching after a patient experienced an “efficacy failure” on their current disease-modifying agent. De Flon et al.60 switched patients considered “stable” on their current injectable agent and found that after the switch, these patients developed fewer MRI lesions and had lower neurofilament light (NFL) levels.
The way forward
NFL holds promise as a potentially more sensitive way to monitor neuronal damage. As such, it might be used to illuminate the question of early use of high-efficacy therapies vs escalation approaches. Recently, the UCSF-Epic cohort reported that at the 5-year follow-up, those treated with highly effective therapies experienced greater decreases in serum NFL compared with those on platform therapies, with a significant interaction found between NFL and EDSS.61 This biomarker may also have utility in clinic as an adjunct to conventional MRI and may even have prognostic value at disease onset. However, further standardization and refinement of serum neurofilament testing is necessary before neurofilament can enter routine clinical use.62
Two Patient-Centered Outcomes Research Institute-sponsored prospective studies will further explore the benefit/risk profile of using more effective agents earlier vs an escalation approach. Both populations will be deeply characterized beyond their primary endpoint. On the other hand, blinding is limited and the populations are quite heterogeneous. As such, it might be difficult to know how these results might apply to a specific patient in clinic given limited subsets at different ages and ranges of disease activity. Assuming that enrollment goes as planned (a potential challenge given the current treatment landscape and fixed beliefs amongst clinicians), these studies are not scheduled to report results until 2022. One might reasonably question how much these studies will add to double-blinded randomized placebo-controlled trials, which employed more rigorous methodologies.
One might even ask, given the confluence of current evidence, whether we need additional trial evidence to begin a HETA initiation in younger patients. Rheumatologists as a group decided to begin more efficacious agents earlier based on a strong correlation between disease duration and chances of achieving remission or low disease activity. This adjustment improved the outcomes achieved in patients with rheumatoid arthritis.63
Conclusion
An examination of relevant pathology and MRI studies suggest that MS is a chronically progressive neurologic condition rather than one characterized by episodic disease. These lines of inquiry also suggest that we underappreciate the amount of brain and spinal cord damage our patients experience over time. We also lack the ability to effectively predict at initial presentation who will do well and who will not over the long term. Even careful early prospective monitoring of disease activity may not adequately predict the outcome. It should be our goal for patients that they adhere as closely to normal aging processes as possible. Current data suggest that we are oftentimes not meeting this goal. In addition, recent developments in the MS treatment landscape have left us with some medications that recast the balance so that the potential harm to an MS patient's nervous system outpaces by far potential concerns about serious side effects. Given these factors, we strongly believe neurologists and policy makers can better keep patients with MS on a course toward long-term healthy aging by using a HETA stratagem.
Acknowledgment
The authors would like to thank Nardine Moawde for editing the manuscript for nonintellectual content.
Glossary
- DTI
diffusion tensor imaging
- EDSS
Expanded Disability Status Scale
- HETA
highly effective treatment early approach
- IFN
interferon
- MTR
magnetization transfer ratio
- NARCOMS
North American Research Committee on Multiple Sclerosis
- NEDA
no evidence of disease activity
- NFL
neurofilament light
- PCORI
Patient-Centered Outcomes Research Institute
- PML
progressive multifocal leukoencephalopathy
- SC
subcutaneous
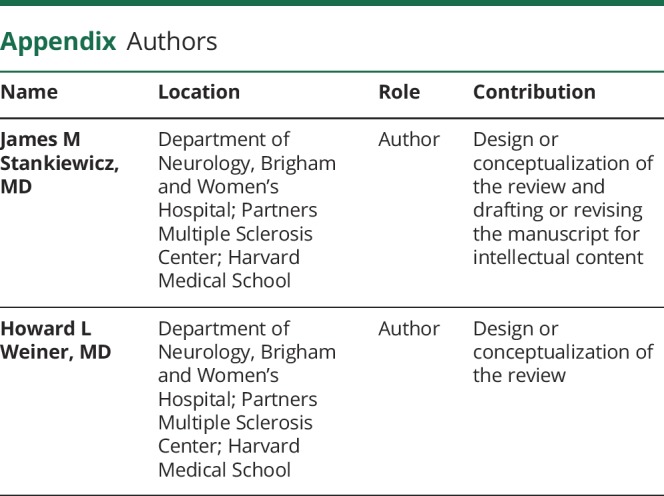
Appendix. Authors
Study funding
Supported in part by the National MS Society and the Water Cove Charitable Foundation.
Disclosure
J.M. Stankiewicz has received consulting fees from Biogen Idec, Novartis, EMD Serono, Hoffman-La Roche, Celgene, and Sanofi Genzyme. H.L. Weiner has served on the advisory boards of The Guthy-Jackson Charitable Foundation, Teva, Biogen, Novartis, Sanofi-Aventis, Tilos, C-Bridge Capital, Genentech, Genzyme, vTv Therapeutics, and MedDay; consulted for Biodextris, Biogen, Novartis, Serono, Teva, Sanofi Genzyme, Tilos, Tiziana Life Sciences, vTv Therapeutics, MedDay, Genentech, and CBridge Capital; and received research support from EMD Serono, Google Life Sciences, the NIH, and the NMSS. Go to Neurology.org/NN for full disclosures. Funding information is provided at the end of the article.
References
- 1.Marziniak M, Ghorab K, Kozubski W, et al. Variations in multiple sclerosis practice within Europe—is it time for a new treatment guideline? Mult Scler Relat Disord 2016;8:35–44. [DOI] [PubMed] [Google Scholar]
- 2.Rae-Grant A, Day GS, Marrie RA, et al. Comprehensive systematic review summary: disease-modifying therapies for adults with multiple sclerosis. Neurology 2018;90:789–800. [DOI] [PubMed] [Google Scholar]
- 3.Montalban X, Gold R, Thompson AJ, et al. ECTRIMS/EAN Guideline on the pharmacological treatment of people with multiple sclerosis. Mult Scler 2018;24:96–120. [DOI] [PubMed] [Google Scholar]
- 4.Weinshenker BG, Rice GP, Noseworthy JH, Carriere W, Baskerville J, Ebers GC. The natural history of multiple sclerosis: a geographically based study: 3. MULTIVARIATE analysis OF predictive FACTORS and MODELS of outcome. Brain 1991;114:1045–1056. [DOI] [PubMed] [Google Scholar]
- 5.Tremlett H, Paty D, Devonshire V. Disability progression in multiple sclerosis is slower than previously reported. Neurology 2006;66:172–177. [DOI] [PubMed] [Google Scholar]
- 6.Weinstock-Guttman B, Jacobs LD, Brownscheidle CM, et al. Multiple sclerosis characteristics in African American patients in the New York state multiple sclerosis consortium. Mult Scler 2003;9:293–298. [DOI] [PubMed] [Google Scholar]
- 7.Koch M, Uyttenboogaart M, van Harten A, De Keyser J. Factors associated with the risk of secondary progression in multiple sclerosis. Mult Scler 2008;14:799–803. Available at: ncbi.nlm.nih.gov/pubmed/18573840. Accessed July 24, 2019. [DOI] [PubMed] [Google Scholar]
- 8.Manouchehrinia A, Zhu F, Piani-Meier D, et al. Predicting risk of secondary progression in multiple sclerosis: a nomogram. Mult Scler 2019;25:1102–1112. [DOI] [PubMed] [Google Scholar]
- 9.Trapp BD, Peterson J, Ransohoff RM, Rudick R, Mörk S, Bö L. Axonal transection in the lesions of multiple sclerosis. N Engl J Med 1998;338: 278–285. [DOI] [PubMed] [Google Scholar]
- 10.Nielsen AS, Kinkel RP, Madigan N, Tinelli E, Benner T, Mainero C. Contribution of cortical lesion subtypes at 7T MRI to physical and cognitive performance in MS. Neurology 2013;81:641–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kollia K, Maderwald S, Putzki N, et al. First clinical study on ultra-high-field MR imaging in patients with multiple sclerosis: comparison of 1.5T and 7T. Am J Neuroradiol 2009;30:699–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pitt D, Boster A, Pei W, et al. Imaging cortical lesions in multiple sclerosis with ultra-high-field magnetic resonance imaging. Arch Neurol 2010;67:812–818. [DOI] [PubMed] [Google Scholar]
- 13.Bermel RA, Bakshi R. The measurement and clinical relevance of brain atrophy in multiple sclerosis. Lancet Neurol 2006;5:158–170. [DOI] [PubMed] [Google Scholar]
- 14.Bodini B, Cercignani M, Khaleeli Z, et al. Corpus callosum damage predicts disability progression and cognitive dysfunction in primary-progressive MS after five years. Hum Brain Mapp 2013;34:1163–1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Inglese M, Madelin G, Oesingmann N, et al. Brain tissue sodium concentration in multiple sclerosis: a sodium imaging study at 3 tesla. Brain 2010;133:847–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wuerfel J, Paul F, Beierbach B, et al. MR-elastography reveals degradation of tissue integrity in multiple sclerosis. Neuroimage 2010;49:2520–2525. [DOI] [PubMed] [Google Scholar]
- 17.Filippi M, Rocca MA. Magnetization transfer magnetic resonance imaging of the brain, spinal cord, and optic nerve. Neurotherapeutics 2007;4:401– 413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ranjeva JP, Audoin B, Au Duong MV, et al. Local tissue damage assessed with statistical mapping analysis of brain magnetization transfer ratio: relationship with functional status of patients in the earliest stage of multiple sclerosis. AJNR Am J Neuroradiol 2005;26:119–127. [PMC free article] [PubMed] [Google Scholar]
- 19.Amato MP, Portaccio E, Stromillo ML, et al. Cognitive assessment and quantitative magnetic resonance metrics can help to identify benign multiple sclerosis. Neurology 2008;71:632–638. [DOI] [PubMed] [Google Scholar]
- 20.Tallantyre EC, Major PC, Atherton MJ, et al. How common is truly benign MS in a UK population? J Neurol Neurosurg Psychiatry 2019;90:522–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kister I, Bacon TE, Chamot E, et al. Natural history of multiple sclerosis symptoms. Int J MS Care 2013;15:146–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salter A, Thomas N, Tyry T, Cutter G, Marrie RA. Employment and absenteeism in working-age persons with multiple sclerosis. J Med Econ 2017;20:493–502. [DOI] [PubMed] [Google Scholar]
- 23.Kister I, Chamot E, Salter AR, Cutter GR, Bacon TE, Herbert J. Disability in multiple sclerosis: a reference for patients and clinicians. Neurology 2013;80:1018–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stephen H. Mobility device use in the United States. Disability statistics report 14 MF01/PC03 Plus Postage [online]. Available at: dsc.ucsf.edu. Accessed August 1, 2019.
- 25.Ford C, Goodman AD, Johnson K, et al. Continuous long-term immunomodulatory therapy in relapsing multiple sclerosis: results from the 15-year analysis of the US prospective open-label study of glatiramer acetate. Mult Scler 2010;16:342–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kappos L, Traboulsee A, Constantinescu C, et al. Long-term subcutaneous interferon beta-1a therapy in patients with relapsing-remitting MS. Neurology 2006;67:944–953. [DOI] [PubMed] [Google Scholar]
- 27.Ebers GC, Traboulsee A, Li D, et al. Analysis of clinical outcomes according to original treatment groups 16 years after the pivotal IFNB-1b trial. J Neurol Neurosurg Psychiatry 2010;81:907–912. [DOI] [PubMed] [Google Scholar]
- 28.Meyer-Moock S, Feng YS, Maeurer M, Dippel FW, Kohlmann T. Systematic literature review and validity evaluation of the Expanded Disability Status Scale (EDSS) and the Multiple Sclerosis Functional Composite (MSFC) in patients with multiple sclerosis. BMC Neurol 2014;14:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Havrdová E, Arnold DL, Bar-Or A, et al. No evidence of disease activity (NEDA) analysis by epochs in patients with relapsing multiple sclerosis treated with ocrelizumab vs interferon beta-1a. Mult Scler J Exp Transl Clin 2018;4:2055217318760642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Havrdova E, Galetta S, Hutchinson M, et al. Effect of natalizumab on clinical and radiological disease activity in multiple sclerosis: a retrospective analysis of the natalizumab safety and efficacy in relapsing-remitting multiple sclerosis (AFFIRM) study. Lancet Neurol 2009;8:254–260. [DOI] [PubMed] [Google Scholar]
- 31.Hauser SL, Bar-Or A, Comi G, et al. Ocrelizumab versus interferon beta-1a in relapsing multiple sclerosis. N Engl J Med 2017;376:221–234. [DOI] [PubMed] [Google Scholar]
- 32.Coles AJ, Twyman CL, Arnold DL, et al. Alemtuzumab for patients with relapsing multiple sclerosis after disease-modifying therapy: a randomised controlled phase 3 trial. Lancet 2012;380:1829–1839. [DOI] [PubMed] [Google Scholar]
- 33.Cohen JA, Coles AJ, Arnold DL, et al. Alemtuzumab versus interferon beta 1a as first-line treatment for patients with relapsing-remitting multiple sclerosis: a randomised controlled phase 3 trial. Lancet 2012;380:1819–1828. [DOI] [PubMed] [Google Scholar]
- 34.Cohen JA, Barkhof F, Comi G, et al. Oral fingolimod or intramuscular interferon for relapsing multiple sclerosis. N Engl J Med.2010;362:402–415. [DOI] [PubMed] [Google Scholar]
- 35.Fox RJ, Miller DH, Phillips JT, et al. Placebo-controlled phase 3 study of oral BG-12 or glatiramer in multiple sclerosis. N Engl J Med 2012;367:1087–1097. [DOI] [PubMed] [Google Scholar]
- 36.Ho PR, Koendgen H, Campbell N, Haddock B, Richman S, Chang I. Risk of natalizumab-associated progressive multifocal leukoencephalopathy in patients with multiple sclerosis: a retrospective analysis of data from four clinical studies. Lancet Neurol 2017;16:925–933. [DOI] [PubMed] [Google Scholar]
- 37.Zhovtis Ryerson L, Frohman TC, Foley J, et al. Extended interval dosing of natalizumab in multiple sclerosis. J Neurol Neurosurg Psychiatry 2016;87:885–889. [DOI] [PubMed] [Google Scholar]
- 38.Berger JR, Malik V, Lacey S, Brunetta P, Lehane PB. Progressive multifocal leukoencephalopathy in rituximab-treated rheumatic diseases: a rare event. J Neurovirol 2018;24:323–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barra ME, Soni D, Vo KH, Chitnis T, Stankiewicz JM. Experience with long-term rituximab use in a multiple sclerosis clinic. Mult Scler J Exp Transl Clin 2016;2:2055217316672100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Salzer J, Svenningsson R, Alping P, et al. Rituximab in multiple sclerosis. A retrospective observational study on safety and efficacy. Neurology 2016;87:2074–2081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Juanatey A, Blanco-Garcia L, Tellez N. Ocrelizumab: its efficacy and safety in multiple sclerosis [in Spanish]. Rev Neurol 2018;66:423–433. Available at: ncbi.nlm.nih.gov/pubmed/29897610. Accessed July 24, 2019. [PubMed] [Google Scholar]
- 42.Bottomley C, Lloyd A, Bennett G, Adlard N. A discrete choice experiment to determine UK patient preference for attributes of disease modifying treatments in Multiple Sclerosis. J Med Econ 2017;20:863–870. [DOI] [PubMed] [Google Scholar]
- 43.Reen GK, Silber E, Langdon DW. Multiple sclerosis patients' understanding and preferences for risks and benefits of disease-modifying drugs: a systematic review. J Neurol Sci 2017;375:107–122. [DOI] [PubMed] [Google Scholar]
- 44.Halpern R, Agarwal S, Dembek C, Borton L, Lopez-Bresnahan M. Comparison of adherence and persistence among multiple sclerosis patients treated with disease-modifying therapies: a retrospective administrative claims analysis. Patient Prefer Adherence 2011;5:73–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Johnson KM, Zhou H, Lin F, Ko JJ, Herrera V. Real-world adherence and persistence to oral disease-modifying therapies in multiple sclerosis patients over 1 year. J Manag Care Spec Pharm 2017;23:844–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang G, Marrie RA, Salter AR, et al. Health insurance affects the use of disease-modifying therapy in multiple sclerosis. Neurology 2016;87:365–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Scalfari A, Neuhaus A, Daumer M, Muraro PA, Ebers GC. Onset of secondary progressive phase and long-term evolution of multiple sclerosis. J Neurol Neurosurg Psychiatry 2014;85:67–75. [DOI] [PubMed] [Google Scholar]
- 48.Chalmer TA, Baggesen LM, Nørgaard M, Koch-Henriksen N, Magyari M, Sorensen PS. Early versus later treatment start in multiple sclerosis: a register-based cohort study. Eur J Neurol 2018;25:1262–e110. [DOI] [PubMed] [Google Scholar]
- 49.Weideman AM, Tapia-Maltos MA, Johnson K, Greenwood M, Bielekova B. Meta-analysis of the age-dependent efficacy of multiple sclerosis treatments. Front Neurol 2017;8:577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Harding K, Williams O, Willis M, et al. Clinical outcomes of escalation vs early intensive disease-modifying therapy in patients with multiple sclerosis. JAMA Neurol 2019;76:536–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Correale J, Gaitán MI, Ysrraelit MC, Fiol MP. Progressive multiple sclerosis: from pathogenic mechanisms to treatment. Brain 2017;140:527–546. [DOI] [PubMed] [Google Scholar]
- 52.Krieger SC, Cook K, De Nino S, Fletcher M. The topographical model of multiple sclerosis. Neurol Neuroimmunol Neuroinflamm 2016;3:e279 doi:10.1212/NXI.0000000000000279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Keegan BM, Kaufmann TJ, Weinshenker BG, et al. Progressive motor impairment from a critically located lesion in highly restricted CNS-demyelinating disease. Mult Scler 2018;24:1445–1452. [DOI] [PubMed] [Google Scholar]
- 54.Confavreux C, Vukusic S, Moreau T, Adeleine P. Relapses and progression of disability in multiple sclerosis. N Engl J Med 2000;343:1430–1438. [DOI] [PubMed] [Google Scholar]
- 55.Brown JWL, Coles A, Horakova D, et al. Association of initial disease-modifying therapy with later conversion to secondary progressive multiple sclerosis. JAMA 2019;321:175–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cohen M, Maillart E, Tourbah A, et al. Switching from natalizumab to fingolimod in multiple sclerosis: a French prospective study. JAMA Neurol 2014;71:436–441. [DOI] [PubMed] [Google Scholar]
- 57.Cree BAC, Gourraud PA, Oksenberg JR, et al. Long-term evolution of multiple sclerosis disability in the treatment era. Ann Neurol 2016;80:499–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rotstein DL, Healy BC, Malik MT, Chitnis T, Weiner HL. Evaluation of no evidence of disease activity in a 7-year longitudinal multiple sclerosis cohort. JAMA Neurol 2015;72:152–158. [DOI] [PubMed] [Google Scholar]
- 59.Harel A, Sperling D, Petracca M, et al. Brain microstructural injury occurs in patients with RRMS despite “no evidence of disease activity”. J Neurol Neurosurg Psychiatry 2018;89:977–982. [DOI] [PubMed] [Google Scholar]
- 60.de Flon P, Gunnarsson M, Laurell K, et al. Reduced inflammation in relapsing-remitting multiple sclerosis after therapy switch to rituximab. Neurology 2016;87:141–147. [DOI] [PubMed] [Google Scholar]
- 61.Cantó E, Barro C, Zhao C, et al. Association between serum neurofilament light chain levels and long-term disease course among patients with multiple sclerosis followed up for 12 years. JAMA Neurol Epub 2019 Aug 12. [DOI] [PMC free article] [PubMed]
- 62.Leppert D, Kuhle J. Blood neurofilament light chain at the doorstep of clinical application. Neurol Neuroimmunol Neuroinflamm 2019;6:e599 doi: 10.1212/NXI.0000000000000599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Burmester GR, Pope JE. Novel treatment strategies in rheumatoid arthritis. Lancet 2017;389:2338–2348. [DOI] [PubMed] [Google Scholar]


