Abstract
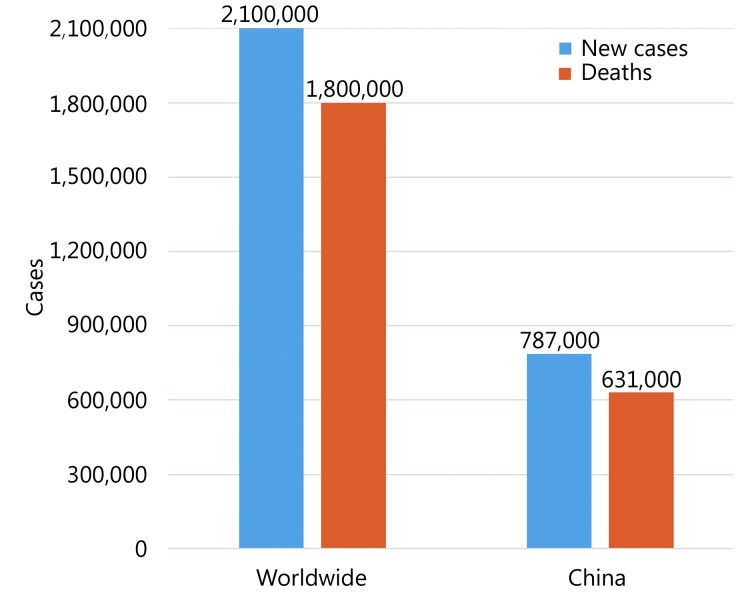
Each year there will be an estimated 2.1 million new lung cancer cases and 1.8 million lung cancer deaths worldwide. Tobacco smoke is the No.1 risk factors of lung cancer, accounting for > 85% lung cancer deaths. Air pollution, or haze, comprises ambient air pollution and household air pollution, which are reported to cause 252,000 and 304,000 lung cancer deaths each year, respectively. Tobacco smoke and haze (hereafter, smohaze) contain fine particles originated from insufficient combustion of biomass or coal, have quite similar carcinogens, and cause similar diseases. Smohaze exert hazardous effects on exposed populations, including induction of a large amount of mutations in the genome, alternative splicing of mRNAs, abnormalities in epigenomics, initiation of tumor-promoting chronic inflammation, and facilitating immune escape of transformed cells. Tackling smohaze and development of multi-targets-based preventive and therapeutic approaches targeting smohaze-induced carcinogenesis are the key to conquer lung cancer in the future.
Keywords: Lung cancer, tobacco smoke, air pollution, smohaze, carcinogenesis
Introduction
Lung cancer is the most common cause of cancer death worldwide, with 2.1 million new cases and 1.8 million deaths predicted in 20181. Lung cancer is also No. 1 cancer killer in China2 (Figure 1). Lung cancer is categorized by cell type into small-cell lung cancer (SCLC; accounting for 15% of all lung cancer cases) and non-small-cell lung cancer (NSCLC; 85%), whereas NSCLC can be divided into lung adenocarcinoma (LUAD; 40%), lung squamous cell carcinoma (LUSC; 30%), and large cell lung cancer (LCLC; 15%). The past two decades have witnessed enormous progress in development of targeted and immune therapies, which significantly improve the clinical outcome of the patients3. Targeted therapies include inhibitors of tyrosine kinases EGFR4, MET5, HER26, and BRAF V6007, inhibitors of fusion proteins involved ALK8, ROS19, RET10,11, and TRK12, antibodies against VEGF13, and others. Immune therapies include antibodies against cytotoxic T-cell lymphocyte-4 (CTLA-4)14, programmed cell death 1 (PD-1) receptor15, and PD-1 ligand 1 (PD-L1)16.
1.
Estimated new lung cancer cases and lung cancer deaths worldwide1 and in China2 in 2018.
However, drug resistance will eventually occur in patients treated with these therapies17, leading to treatment failure of the patients. Currently, the 5-year overall survival of lung cancer of all stage combined is only 18.6%18 and 7%19, respectively. Therefore, new strategies remain urgent needs to conquer lung cancer. It is well-known that a large majority of patients suffering from lung cancer have their roots in unhealthy life style and exposure to environmental factors, hence much more attentions should be paid to the causes of lung cancer and related lung carcinogenesis when considering curative approaches for this deadly disease.
Tobacco smoke: the No. 1 risk factor of lung cancer
Tobacco smoke is the single biggest public health threat the world is currently facing. It is estimated that there are 1.1 billion smokers worldwide, and around 8 million people are killed by tobacco smoke each year globally. Among these deaths, more than 7 million are the result of direct tobacco use while around 1.2 million are the result of non-smokers being exposed to second-hand smoke20-22. Tobacco use is responsible for approximately 22% of cancer deaths worldwide23. Recent studies show that approximately 15% to 24% of lifetime smokers will get lung cancer24, and tobacco smoking accounts for more than 85% of lung cancer worldwide25.
During smoking, tobacco is heated to 880°C or higher, and more than 8,000 compounds have been identified in tobacco and tobacco smoke. More than 70 carcinogens and more than 20 lung carcinogens have been identified, which fall into group 1 (carcinogenic to humans), group 2A (probably carcinogenic to humans), and group 2B (possibly carcinogenic to humans) of carcinogen classifications of the International Agency for Research on Cancer (IARC) of the World Health Organization (WHO). Group 1 carcinogens found in tobacco smoke include polycyclic aromatic hydrocarbons [PAHs; e.g., benzo (a) pyrene, BaP], N-nitrosamines [e.g., N’-nitrosonornicotine; 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone, NNK], aromatic amines (e.g., 2-naphthylamine, 4-aminobiphenyl), heterocyclic aromatic amines [e.g., 2-amino-3-methylimidazo (4,5-f) quinoline], aldehydes (e.g., formaldehyde), volatile hydrocarbons (e.g., benzene), miscellaneous organic compounds (e.g., vinyl chloride, ethylene oxide), heavy metals and inorganic compounds [e.g., arsenic, beryllium, nickel, chromium (hexavalent), cadmium, radioisotope polonium-210], and others24,26.
Cigarette smoking was linked to lung cancer in 1964 by the Surgeon General of U.S. Department of Health and Human Service in the first Surgeon General’s Report. This linking has had an enormous positive effect on public health, in that in U.S. male smoking prevalence has decreased from 51.1% to the current 21.6%, whereas prevalence in females diminished from 33.3% to 16.5%24. In China, male and female smoking prevalence has also began to decrease27. Due to reduced tobacco use, lung cancer death rates in U.S. declined 45% from 1990 to 2015 among males and 19% from 2002 to 2015 among females1. However, there will be an estimated 228,150 new lung cancer cases and 142,670 lung cancer deaths in 2019 in U.S.28, and there will be an estimated 2,540,842 new lung cancer cases and 2,145,215 lung cancer deaths worldwide in 202529. Of note, no therapeutics so far are designed to target tobacco smoke-induced lung carcinogenesis, which remains to be elucidated.
Air pollution represents the second risk factor of lung cancer
Clean air is a basic requirement of life. Air pollution, or haze, is a diverse mixture of pollutants that originated from anthropogenic and natural sources, is comprised of particulate matters (PM), gases (e.g., sulfur oxides, carbon monoxide, ozone), organic compounds (e.g., PAHs; resin acids; anhydrous sugars; lignin pyrolysis products; hopanes), metals (e.g., lead, vanadium, and nickel), microbes, and others30-32. The main PM in the environment are PM smaller than 10 μm in diameter (PM10) and PM smaller than 2.5 μm in diameter (PM2.5), and air pollution can be divided into ambient air pollution (AAP) and household air pollution (HAP), and is a global environmental health risk that affects the populations in developed and developing countries alike, and 91% of the world population is living in places where the WHO air quality guidelines levels (i.e. annual mean values of 20 μg/m3 for PM10 and 10 μg /m3 for PM2.5)33 are not met34. WHO also sets guidelines for the protection of public health from risks due to a number of chemicals commonly present in indoor air {i.e. benzene, carbon monoxide, formaldehyde, naphthalene, nitrogen dioxide, polycyclic aromatic hydrocarbons [especially benzo (a) pyrene], radon, trichloroethylene and tetrachloroethylene}35. AAP in both cities and rural areas is estimated to cause 4.2 million premature deaths worldwide each year34, and 3.8 million people a year die prematurely from illness attributable to the HAP caused by the inefficient combustion of solid fuels and kerosene for cooking36. It is estimated that there are 304,00037 and 252,00034 lung cancer deaths that are attributed to HAP and AAP each year worldwide, respectively.
Xuanwei (XW) City in Yunnan Province of China provides an example of the epidemiological association between PM10, PM2.5 and lung cancer38-40. This city has a large deposit of smoky coal and until the 1970s, local residents used smoky coal in unvented indoor firepits for domestic cooking and heating, all processes that release high concentrations of PM10 and PM2.5. These airborne particles contain high concentrations of PAHs including BaP and polar compounds that are highly mutagenic40. Lung cancer incidence in XW is among the highest in China38,40, and a reduction in lung cancer morbidity was noted in the 1990s after stove improvement in central XW, supporting the association between air pollution and lung cancer41. These findings had been cited in the IARC monograph classifying HAP as “carcinogenic to humans (group 1)”42. On the other hand, Raaschou-Nielsen et al.43 showed that the risk of lung cancer rises by 18% for every increase of 5 μg/m3 of PM2.5 in the environment, and the risk increases by 22% for every increase of 10 μg/m3 in PM10. AAP has also been classified as group 1 carcinogen in humans by IARC43. LUAD, LUSC, SCLC, and bronchiolo-alveolar carcinoma (BAC) represent the most frequently seen lung cancer subtypes in air pollution regions38,44.
Tobacco smoke and haze (smohaze) are responsible for more than 90% of lung cancer
Tobacco smoke and haze bear many common characteristics in causing lung cancer (Table 1). For example, the fine particles in the two factors are PM2.5, which are mainly originated from insufficient combustion of biomass or coal. Though they may contain different chemical components, tobacco smoke and haze have quite similar main carcinogens, e.g., PAHs, heterocyclic compounds, N-nitrosamines, aromatic amines, heterocyclic aromatic amines, aldehydes, phenolic compounds, volatile hydrocarbons, nitrohydrocarbons, miscellaneous organic compounds, metals, and others (Table 1). PM2.5 are inhaled, and cause diseases such as respiratory infections, cardiovascular disease, chronic obstructive pulmonary disease (COPD), and cancers20,21,34,37. Tobacco smoke and haze can cause all types of lung cancer (Table 1). Furthermore, these two factors are responsible more than 90% of lung cancer. Therefore, to elucidate the environmental lung carcinogenesis and to develop effective chemopreventive and therapeutic approaches to conquer lung cancer, tobacco smoke and haze should be treated as a single risk factor, smohaze (for tobacco smoke and haze).
1.
Comparison of tobacco smoke and haze
| PM | Origin of pollutants | Chemistry | Main carcinogens* | Exposure methods | Related diseases | Types of lung cancer | |
| *For each class, only the group 1 carcinogens are listed in parentheses. As, arsenic; Be, beryllium; Ni, nickel; Pb, plumbum; NNK, 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone; Cr, chromium; Cd, cadmium; 210Po, radioisotope polonium-210. | |||||||
| Tobacco smoke | PM2.5 | Burning of tobacco | Nicotine, N-Nitrosamines, PAHs, volatile compounds, heavy metals, aromatic amines, heterocyclic amines, etc. | PAHs (BaP), heterocyclic compounds, N-nitrosamines (N’-nitrosonornicotine, NNK), aromatic amines (2-naphthylamine, 4-aminobiphenyl), heterocyclic aromatic amines, aldehydes (formaldehyde), phenolic compounds, volatile hydrocarbons (benzene), nitrohydrocarbons, miscellaneous organic compounds (vinyl chloride, ethylene oxide), metals (As, Be, Ni, Cr, Cd, 210Po), etc.26 | Inhalation | Cancers, cardiovascular disease, diabetes, COPD, pneumonia, and others21,22 | All types of lung cancer, in particular small cell lung and squamous cell carcinoma |
| Haze | PM2.5 | Burning of coal, fossil fuel, biomass, etc | Organic matter, nitrate, sulphate, ammonium, chloride, heavy metals, elemental carbon, etc. | PAHs (BaP), heterocyclic compounds, N-nitrosamines, aromatic amines, heterocyclic aromatic amines, aldehydes (formaldehyde), phenolic compounds, volatile hydrocarbons (benzene), nitrohydrocarbons, miscellaneous organic compounds (vinyl chloride, ethylene oxide), metals (As, Be, Cr, Cd, Ni, Pb), etc.30-32 | Inhalation | Respiratory infections, cancers, cardiovascular disease, COPD, asthma, and others34,36 | LUAD, LUSC, SCLC, BAC38,44 |
Why smohaze
Treating the two risk factors as one, smohaze, may result in some positive effects in prevention and treatment of related disease. First, the health hazards of tobacco smoke and haze are currently separately assessed, which may lead to inconsistent results. For example, it is estimated that > 85% (1,530,000) of the 1.8 million lung cancer deaths are attributed to tobacco smoke, and other reports show that 252,000 and 304,000 patients may die from AAP- and HAP-caused lung cancer, respectively. Obviously, deaths from these factors exceed the total lung cancer deaths worldwide. Under the concept of smohaze, the more accurate data will be obtained from the related agencies. Second, when considering preventive medicine, the two factors should be tackled simultaneously. Combination of the two would be helpful for the public health domain to develop more effective strategies to tackle the public health problems, in that anti-tobacco campaign and anti-haze efforts could be propagated simultaneously. Third, the emerging concept of smohaze may create additional opportunities for the elucidation of environmental lung carcinogenesis and development of effective preventive and therapeutic approaches to conquer lung cancer.
Smohaze-induced lung carcinogenesis
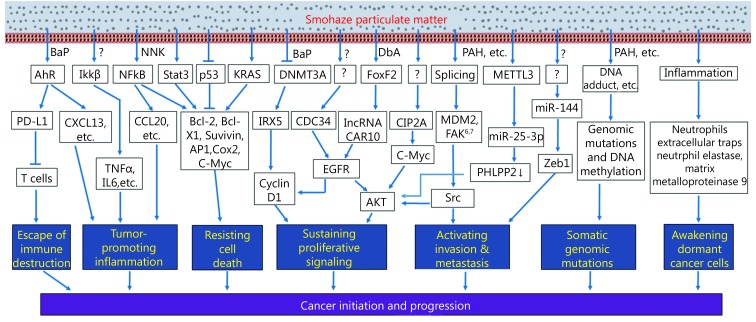
Efforts have been made to dissect tobacco smoke-induced tumorigenesis and air pollution in promoting lung cancer. These works show that smohaze exerts comprehensive effects on humans to trigger and promote lung cancer (Figure 2).
2.
Schematic representation of the complicated smohaze-induced lung carcinogenesis.
Genomic mutations
Carcinogens and nucleotide substitutions
As compared with counterpart normal controls, cancer genomes usually have six types of nucleotide changes, C→T/G→A, C→A/G→T, C→G/G→C, A→G/T→C, A→T/T→A, and A→C/T→G. Smohaze carcinogens can cause characteristic mutations (or signature) in the genome. For example, the G to T transversions have been described as a mutational fingerprint of tobacco smoke mutagens in smoking-associated lung cancers, and smokers more frequently show G→T transversions, whereas never-smokers have more G→A transitions45-48. PAHs are the main carcinogens that produce G→T mutations25,49. NNK may induce both G→T and G→A mutations50, and 4-aminobiphenyl and 1,3-butadiene cause the A→T transversions51-53. Other smohaze carcinogens also induce characteristic nucleotide substitutions in the genome54. These mutations were firstly reported in genes such as TP53, RAS, and others25,49,51-53. However, attentions should be paid to the fact that one type of nucleotide changes can be induced by different environmental factors or carcinogens, therefore the so-called “signature” is not stringently specific to one mutagen54,55.
Mutations in specific genes
Husgafvel-Pursiainen et al.56 showed that patients who smoke have a three-fold greater risk of TP53 mutations compared to those who do not smoke. Le Calvez et al.57 showed that the rate of TP53 mutations increased from 47.5% in never-smokers to 77.4% in active smokers, and the risk of having a TP53 mutation was significantly proportional to the amount of tobacco consumed. KRAS mutations are much more frequent in smokers, in that in active smokers and never-smokers the KRAS mutation rates were 34% and 5%, respectively58,59. BRAF mutations are significantly more frequent in smokers (active or former)60. On the contrary, EGFR mutations and ALK rearrangements are much more frequent in never-smokers compared to active smokers58,59,61,62. Barlesi et al.63 further reported significant differences between smokers and never-smokers for mutations in EGFR (4.5% vs. 36.3%), ALK (3.5% vs. 9.7%), KRAS (31.7% vs. 9.6%), BRAF (1.6% vs. 1.8%), and HER2 (0.2% vs. 3.8%), respectively (Table 2).
2.
Mutation rates of selected genes (10% or more) in NSCLCs associated with smohaze or not
| Genes | Smohaze | Non-smohaze | P | Reference |
| ALK | 3.5 | 9.7 | 63 | |
| CACNA1E | 19 | 1.2 | 0.0001 | 67 |
| EGFR | 4.5 | 36 | 63 | |
| 38 | 27 | 0.135 | 67 | |
| KRAS | 34 | 5 | 58,59 | |
| 24 | 12 | 0.039 | 67 | |
| MYH3 | 15.2 | 0.0 | 0.0002 | 67 |
| NRXN2 | 13.9 | 0.0 | 0.0004 | 67 |
| RB1CC1 | 13.9 | 1.2 | 0.0017 | 67 |
| RTL1 | 13.9 | 1.2 | 0.0017 | 67 |
| RYR2 | 29.1 | 8.2 | 0.0005 | 67 |
| TP53 | 77 | 47 | < 0.0001 | 57 |
| 58 | 40 | 0.02 | 67 | |
| XIRP2 | 19 | 3.5 | 0.0016 | 67 |
Genomic mutations
Alexandrov et al.64 analyzed somatic mutations and DNA methylation in 5,243 cancers of 17 types (including LUAD, LUSC, and SCLC) for which tobacco smoking confers an elevated risk. They showed that smoking is associated with increased mutation burdens of multiple distinct mutational signatures, which contribute to different extents in different cancers. One of these signatures, mainly found in cancers derived from tissues directly exposed to tobacco smoke, is attributable to misreplication of DNA damage caused by tobacco carcinogens. Others likely reflect indirect activation of DNA editing by APOBEC cytidine deaminases and of an endogenous clocklike mutational process. Smoking is associated with limited differences in methylation. Govindon et al.65 report the results of whole-genome and transcriptome sequencing of tumor and adjacent normal tissue samples from 17 NSCLCs. They identified 3,726 point mutations and more than 90 small insertions and deletions (indels) in the coding sequence, with an average mutation frequency more than 10-fold higher in smokers than in never-smokers. Deep digital sequencing revealed diverse clonality patterns in both never-smokers and smokers.
Only one work so far has looked at somatic genomic profiles in association with air pollution66. In that work67, we analyzed the somatic mutations of 164 NSCLCs from XW and control regions (CR) where smoky coal was not used. Whole genome sequencing revealed a mean of 289 somatic exonic mutations per tumor and the C:G→A:T nucleotide substitutions in XW NSCLCs. Exome sequencing of 2010 genes showed that XW and CR NSCLCs had a mean of 68 and 22 mutated genes per tumor, respectively (P<0.0001). We found 167 genes (includingCACNA1E, KRAS, MYH3, NRXN2, RB1CC1, RTL1, RYR2, TP53, XIRP2) which had significantly higher mutation frequencies in HPR than CR patients (Table 2), and mutations in most genes in XW NSCLCs differed from those in CR cases. The mutation rates of 70 genes (e.g., RYR2, MYH3, GPR144, CACNA1E) were associated with patients’ lifetime BaP exposure. This study uncovers the mutation spectrum of air pollution-related lung cancers, and provides evidence for pollution exposure-genomic mutation relationship at a large scale.
Very few studies systematically dissect genomic mutations specifically occurred in “normal” tissues68,69 and their roles in lung carcinogenesis. We analyzed the genome of normal lung tissues and paired tumors of patients with LUAD70 and LUSC71, and found genomic alterations in the “normal” lung tissues that can be verified by Sanger capillary sequencing. The C:G→T:A transitions, a signature of tobacco carcinogen N-methyl-N-nitro-N-nitrosoguanidine, were the predominant nucleotide changes in counterpart normal controls (CNCs) of LUAD and LUSC. The significance of these variations remains unclear. One possibility was that some of the mutated genes were pro-oncogenes (e.g., MUC472 and CDC2773) or tumor suppressors (e.g., NCOR174), cells harboring these variations were in a “precancerous” stage, and accumulation of other mutations would result in transformation and development of malignant neoplasms. Secondly, many of the CNC altered genes were associated with immune response, DNA-damage response system, or other important signal pathways, which may facilitate avoiding immune destruction and other hallmarks to facilitate lung cancer70,71. These possibilities warrant further investigation.
Alternative splicing
Alternative splicing, the process by which splice sites are differentially utilized to produce different mRNA isoforms, contributes to oncogenic activation in several types of cancers75,76. Emerging evidence demonstrates that smohaze can induce alternative splicing of some critical genes to facilitate lung carcinogenesis. Weng et al.77 showed that of the 117 lung cancer tissue samples analyzed, 31 (26.5%) had splice variants for the MDM2 gene, with 26 samples bearing a splice variant lacking exons 3–11. Significant association was found between the frequency of alternative splicing and the smoking habits of the patients. 44.2% of the smoker patients had alternative MDM2 splice forms versus 16.2% of nonsmokers (P = 0.003). BaP and BPDE induced generation of MDM2 splicing products in H1355 LUAD cells. BPDE-induced MDM2 mRNA alternative splicing in H1355 cells may occur through the PI3K or MAPK pathway. We recently reported a splicing variant of Focal adhesion kinase (FAK), FAK6,7 that contains alternatively spliced exons of 18 bp (Box 6) and 21 bp (Box 7) on either side of codon for Y397 in 4 (4.4%) of 91 patients with NSCLC78. Smokers had more FAK abnormalities than non-smokers. In TCGA RNA-seq data, Box 6/7-containing FAK variants were positive in 42 (8.3%) of 508 LUADs and 37 (7.4%) of 501 LUSCs, and current smokers had higher expression of Box 6/7 (+) FAK than reformed and never smokers. FAK6,7 promoted cell proliferation and migration, and exhibited increased autophosphorylation and was more sensitive to FAK inhibitor compared to wild type FAK78. The effects of smohaze on mRNA splicing and splicing factors warrant further investigation.
Less mutated genes that are critical to environmental lung carcinogenesis
Cancer has been considered as a disease of the genome, and genomic mutations have been shown to be critical to tumorigenesis and served as targets for drug development79. Some genes that are usually wild type also play crucial roles in smohaze-induced lung carcinogenesis.
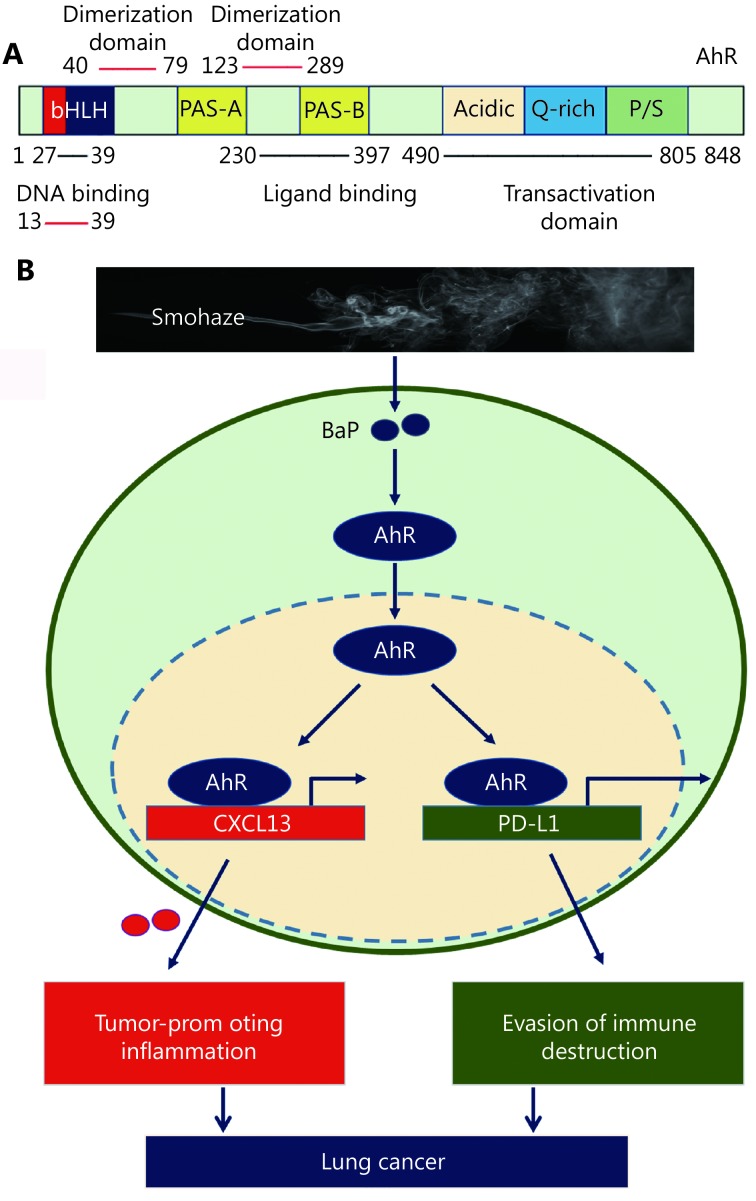
Aryl hydrocarbon receptor (AhR)
AhR (Figure 3A) is a member of the basic helix–loop–helix–PER– ARNT–SIM (bHLH–PAS) subgroup of the bHLH superfamily of transcription factors. AhR is an environmental sensor integrating immune responses in health and disease80. It can be activated by agonists such as 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD, dioxin) and BaP81, and plays a critical role in endogenous ligand kynurenine-promoted82- and environmental carcinogens-induced tumorigenesis83. A constitutively active AhR promotes hepatocarcinogenesis84 and induces stomach tumors85 in mice. Shimizu et al.83 investigated the response of AhR-deficient mice to BaP, and found that BaP induced subcutaneous tumors in AhR+/+ and AhR+/− mice. In contrast, no tumors were apparent in any of the AhR-deficient mice. We recently found that AhR mediated smohaze-induced PD-L1 expression on lung epithelial cells, and deficiency in AhR significantly suppresses BaP-induced lung cancer. AhR inhibitors alpha-naphthoflavone (ANF) and CH223191 exert significant antitumor activity in lung cancer mouse models86. These results indicate that AhR is critical to smohaze-induced lung carcinogenesis, and represents an attractive therapeutic target.
3.
AhR in lung carcinogenesis. (A) Schematic representation of AhR protein. bHLH, basic helix–loop–helix; PAS, period [Per]-aryl hydrocarbon receptor nuclear translocator [ARNT]-single minded [SIM]; P/S, proline (P)/serine (S). (B) AhR mediates smohaze-induced CXCL13 production by PD-L1 expression lung epithelial cells.
Other genes
Smohaze may perturb the expression of some genes to facilitate lung carcinogenesis. NNK promotes migration and invasion of lung cancer cells through activation of c-Src/PKCi/FAK loop87. Oncoprotein cancerous inhibitor of PP2A (CIP2A) was dramatically elevated in tumor samples compared to paratumor normal tissues of patients with NSCLC88. CIP2A overexpression was associated with patients’ smoking status88, and chronic cigarette smoke exposure induced CIP2A expression in mice89. Silencing CIP2A inhibited the proliferation and clonogenic activity of lung cancer cells. Smohaze may regulate the expression of some genes in an unexpected way. For example, we conducted a large-scale lethality screening in NSCLC cells to silence all the 1530 transcription factors and 696 ubiquitin pathway genes, and found that transcription factor Iroquois Homeobox 5 (IRX5)90 and E2 conjugase CDC3490 were required for lung cancer cell proliferation. To our surprise, the expression of IRX5 was significantly higher in smoker patients than non-smoker cases, and BaP was able to upregulate IRX5 in lung epithelial cells. Silencing IRX5 significantly inhibited tumor growth in nude mice90. We showed that CDC34 bound EGFR and competed with E3 ligase c-Cbl to inhibit the polyubiquitination and subsequent degradation of EGFR. In EGFR-L858R and EGFR-T790M/Del(exon 19)-driven lung cancer in mice, knockdown of CDC34 significantly inhibited tumor formation. CDC34 was elevated in tumor tissues in 67 of 102 (65.7%) NSCLCs, and smokers had much higher CDC34 than nonsmokers90. These results indicate that further works should be done to identify critical genes induced or suppressed by smohaze to promote lung carcinogenesis.
Epigenetic abnormalities
DNA methylation
NNK induces DNA methyltransferase 1 (DNMT1) accumulation and tumor suppressor gene hypermethylation in mice and lung cancer patients91. An epigenome wide association study was conducted using peripheral-blood DNA of 464 individuals (22 current smokers and 263 ex-smokers), and the results suggest the existence of dynamic, reversible site-specific methylation changes in response to cigarette smoking, which may contribute to the extended health risks associated with cigarette smoking92. A meta-analyses of gene methylation and smoking behavior in NSCLCs showed that 7 hypermethylated genes (including CDKN2A, RASSF1, MGMT, RARB, DAPK, WIF1 and FHIT) were significantly associated with the smoking behavior in NSCLC patients. CDKN2A hypermethylation was significantly associated with cigarette smoking in Japanese, Chinese and Americans, whereas RARB hypermethylation was associated with smoking status in Chinese patients93. Jiang et al.94 analyzed genome-wide DNA methylation alterations in XW lung cancers, and obtained a comprehensive dataset of genome-wide CpG island methylation in air pollution-related lung cancers. BaP exposure induced multiple alterations in DNA methylation and in mRNA expressions of DNMTs and ten-11 translocation proteins; these alterations partially occurred in XW lung cancer. BaP-induced DKK2 and EN1 promoter hypermethylation and LPAR2 promoter hypomethylation led to down-regulation and up-regulation of the genes, respectively; the down-regulation of DKK2 and EN1 promoted cellular proliferation. Vitamin C and B6 reduced BaP-induced DNA methylation alterations.
microRNAs (miRNAs)
Schembri et al.95 examined whole-genome miRNA expression in bronchial airway epithelium from current and never smokers (n = 20) and found 28 miRNAs to be differentially expressed with the majority being down-regulated in smokers. These miRNAs contain potential binding sites for the differentially expressed mRNAs in their 3'-untranslated region (UTR). Among them, miR-218 expression was reduced in primary bronchial epithelium exposed to cigarette smoke condensate. Izzotti et al.96 analyzed the expression of 484 miRNAs in the lungs of rats exposed to environmental cigarette smoke (ECS), and found that ECS down-regulated 126 miRNAs (26.0%) at least 2-fold and 24 miRNAs more than 3-fold. The most remarkably down-regulated miRNAs belonged to the families of let-7, miR-10, miR-26, miR-30, miR-34, miR-99, miR-122, miR-123, miR-124, miR-125, miR-140, miR-145, miR-146, miR-191, miR-192, miR-219, miR-222, and miR-223, while miR-294 was up-regulated. They reported a strong parallelism in dysregulation of rodent microRNAs and their human homologues, which are often transcribed from genes localized in fragile sites deleted in lung cancer. Zhang et al.97 showed that cigarette smoke upregulates miR-25-3p maturation via N6-methyladenosine and inhibits PHLPP2 to activate AKT, leading to promotion of pancreatic cancer progression. We performed miRNA microarray analysis in NSCLCs from XW or CR, and found 13 down-regulated and 2 up-regulated miRNAs in XW NSCLCs. Among them, miR-144 was one of the most significantly down-regulated miRNAs. The expanded experiments showed that miR-144 was down-regulated in 45/51 (88.2%) XW NSCLCs and 34/54 (63%) CR NSCLCs (P = 0.016). MiR-144 interacted with the oncogene Zeb1 at 2 sites in its 3'-UTR, and a decrease in miR-144 resulted in increased Zeb1 expression and an epithelial mesenchymal transition phenotype. Ectopic expression of miR-144 suppressed NSCLCs in vitro and in vivo by targeting Zeb1. Smohaze can also perturb the expression of other miRNAs to activate oncogenes, suppress tumor suppressors, promote cell proliferation, angiogenesis, and cell cycle, and inhibit apoptosis, to facilitate carcinogenesis98,99.
Long noncoding RNAs (lncRNAs)
lncRNAs are a group of non-coding RNAs consisting of > 200 nucleotides and having no or low translational potential 100. Cigarette smoke or BaP can induce the expression of several lncRNAs, such as lncRNA–1 (SCAL1), DQ786227, and LOC728228, in cells101-104. We screened for abnormal lncRNAs in XW lung cancers and reported that XW patients had much more dysregulated lncRNAs than patients from CR. The lncRNA CAR intergenic 10 (CAR10) was up-regulated in 39/62 (62.9%) of the XW patients, which was much higher than in patients from CR (32/86, 37.2%; P = 0.002). PAH compound dibenz (a, h) anthracene (DbA) up-regulated CAR10 by increasing the expression of transcription factor FoxF2. CAR10 bound and stabilized transcription factor Y-box-binding protein 1 (YB-1), leading to up-regulation of EGFR and proliferation of lung cancer cells. Knockdown of CAR10 inhibited cell growth in vitro and tumor growth in vivo105. These results demonstrate the role of lncRNAs in environmental lung carcinogenesis.
Chronic cancer-promoting inflammation
Tobacco smoke induces pulmonary inflammation, which is believed to play a role in progressive lung destruction in COPD106,107. Tobacco smoke induces production of cytokines and chemokines, and chronic inflammation may contribute to tumor initiation/promotion through the production of reactive oxygen and nitrogen species that contribute to DNA damage and induction of oncogenic mutations106,108,109. Takahashi et al.110 demonstrated that repetitive exposure to tobacco smoke promotes tumor development both in carcinogen-treated mice and in transgenic mice undergoing sporadic K-ras activation in lung epithelial cells. Tumor promotion is due to induction of inflammation that results in enhanced pneumocyte proliferation and is abrogated by IKKβ ablation in myeloid cells or inactivation of JNK1110. We systematically screened for clinically relevant inflammatory factors that are critical for carcinogenesis, and reported that a chemokine CCL20 was significantly up-regulated by NNK. In 78/173 (45.1%) patients the expression of CCL20 was higher in tumor samples than their adjacent normal lung tissues; CCL20 was up-regulated in 48/92 (52.2%) smoker and 29/78 (37.2%) non-smoker patients (P = 0.05), and high CCL20 was associated with poor prognosis. Anti-inflammation drug dexamethasone inhibited NNK-induced CCL20 production and suppressed lung cancer in vitro and in vivo111. We screened for abnormal inflammatory factors in NSCLCs from XW and CR, and found that a chemokine CXCL13 was overexpressed in 63/70 (90%) of XW NSCLCs and 44/71 (62%) of smoker and 27/60 (45%) of non-smoker CR patients. CXCL13 overexpression was associated with the XW region and cigarette smoke. The smohaze carcinogen BaP induced AhR-mediated CXCL13 production in lung epithelial cells and in mice prior to development of detectable lung cancer (Figure 3B). Deficiency in Cxcl13 or its receptor, Cxcr5, attenuated BaP-induced lung cancer in mice, demonstrating CXCL13’s critical role in PAH-induced lung carcinogenesis112. In a nested case-control study (n = 526 lung cancer patients and n = 592 control subjects) measuring serum levels of 77 inflammation markers, CXCL13 and C-reactive protein (CRP), CCL22, and IL-1RA provided good separation in 10-year lung cancer cumulative risks among former smokers and current smokers even after adjustment for smoking113. Lung inflammation caused by tobacco smoke exposure also converted disseminated, dormant cancer cells to aggressively growing metastases114.
Immune escape
Whether tobacco carcinogens confer the exposed cells immune escape to initiate carcinogenesis, and why smoker patients response better to immunotherapies than non-smokers14,15,115, remain poorly understood. We reported that cigarette smoke and carcinogen BaP induced PD-L1 expression on lung epithelial cells in vitro and in vivo, which is mediated by AhR (Figure 3B). Anti-PD-L1 antibody or deficiency in AhR significantly suppresses BaP-induced lung cancer. In 37 patients treated with anti-PD-1 antibody pembrolizumab, 13/16 (81.3%) patients who achieve partial response or stable disease express high levels, whereas 12/16 (75%) patients with progression disease exhibit low levels, of AhR in tumor tissues. AhR inhibitors exert significant antitumor activity and synergize with anti-PD-L1 antibody in lung cancer mouse models. These results demonstrate that tobacco smoke induces lung epithelial cells escape from adaptive immunity to promote tumorigenesis, and AhR predicts responses to immunotherapy and represent an attractive therapeutic target. The expression of CTLA-4 was analyzed in 909 NSCLC patients, and the results showed that CTLA-4 expression was significantly higher in LUSC and current/former smokers116. Cigarette smoke also induces lung inflammation and formation of neutrophil extracellular traps, which awaken dormant cancer cells by the neutrophil elastase and matrix metalloproteinase 9114. A recent study showed that carcinogenesis in the lung involves a dynamic co-evolution of pre-invasive bronchial cells and the immune response/immune escape through immune checkpoints and suppressive interleukins from high-grade pre-invasive lesions117.
The anti-lung cancer strategies
To tame lung cancer, WHO20 and many countries have launched measures to monitor tobacco use and prevention policies, protect people from tobacco use, offer help to quit tobacco use, warn about the dangers of tobacco, enforce bans on tobacco advertising, promotion and sponsorship, and raise taxes on tobacco. China118 and other countries have been tackling the health effects of air pollution. Tremendous efforts have been made to develop preventive and therapeutic approaches. However, the cancer incidence is still high and the 5-year overall survival rate of lung cancer remains dismally low.
Rethinking of the current anti-lung cancer strategies may uncover the following limitations for further improvement. First, smohaze-induced lung carcinogenesis remains to be elucidated. Though numerous studies have been performed to dissect environmental tumorigenesis, many of the works were conducted at cellular and animal models, the clinical relevance of the results should be further tested. Second, no druggable target for smohaze-induced lung cancer was identified and no drug was developed to target smohaze-induced lung carcinogenesis. This represents a major limitation of lung cancer studies in the past 5 decades. Third, while great efforts have been made to characterize genomic mutations, those critical genes that rarely mutate should be unveiled. Thousands of lung cancer genomes have been sequenced in the past decade and a large amount of somatic abnormalities have been reported, but only a few mutated genes have been shown to be the “driver” mutations, suggesting that some less mutated genes should play critical roles in smohaze-induced lung carcinogenesis. AhR represents one of this kind of critical genes, and other critical genes should be uncovered by systematic studies. Of course, the less mutated genes usually play important roles in physiological settings, targeting these genes may possibly induce side effects in the patients. Hence, efforts should be made to scrutinize the requirement of the genes by cancerous and normal tissues, and molecules that are more critical to tumor cells than normal cells could be appropriate targets exemplified by proteasome in multiple myeloma119. Fourth, the current single target-oriented treatment regimens will eventually failed due to development of drug resistance. Inhibition of EGFR gain-of-function mutations marks a revolution in the history of lung cancer treatment, and while resistance occurred the second, third, and even fourth generations of EGFR inhibitors were developed120,121, though drug resistance may develop again. This single target-based passive strategy could be improved by combinatory treatment regimens comprised of different components targeting different targets, exemplified by the traditional Chinese medicine formulae that usually contain compounds of “Jun” (Emperor), “Chen” (Minister), “Zuo” (Assistant), and “Shi” (Delivering Servant) to reach synergistic anti-cancer effects122.
Perspectives
Up to 90% of cancer cases are caused by environmental factors or lifestyle123. The fact that > 90% of lung cancer deaths are caused by smohaze clearly demonstrates the smohaze-induced lung carcinogenesis as the key to develop effective preventive and therapeutic strategies to tame lung cancer, given that the hazardous health effects of smohaze will not be avoidable for billions of people in the near future. The discoveries that deficiency in AhR significantly inhibited BaP-induced lung 86 and skin83 cancers indicate that inhibition of AhR may exert beneficial effects in prevention and treatment of lung cancer. Moreover, deficiency in CXCL13112 or suppression of PD-L186, both of which are AhR target genes, inhibited BaP-induced lung cancer, further confirming the critical roles of AhR in smohaze-induced lung carcinogenesis. With uncovering of more and more critical molecules in smohaze-induced lung carcinogenesis, more targets will be provided to develop more effective preventive and therapeutic approaches. Based on these targets, vaccines and anti-lung cancer formulae can be developed, and early diagnosis and early treatment can be achieved. I believe that these efforts will eventually result in conquering of lung cancer in the future.
Acknowledgments
This work was supported by the National Key Research and Development Program of China (Grant No. 2016YFC0905501), the National Natural Science Funds for Distinguished Young Scholar (Grant No. 81425025), the Key Project of the National Natural Science Foundation of China (Grant No. 81830093), the CAMS Innovation Fund for Medical Sciences (Grant No. CIFMS; 2019-I2M-1-003), and the National Natural Science Foundation of China (Grant No. 81672765).
Conflict of interest statement
No potential conflicts of interest are disclosed.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A Global cancer statistics 2018: globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Zheng RS, Sun KX, Zhang SW, Zeng HM, Zou XN, Chen R, et al Report of cancer epidemiology in China, 2015. Chin J Oncol. 2019;41:19–28. doi: 10.3760/cma.j.issn.0253-3766.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 3.Herbst RS, Morgensztern D, Boshoff C The biology and management of non-small cell lung cancer. Nature. 2018;553:446–54. doi: 10.1038/nature25183. [DOI] [PubMed] [Google Scholar]
- 4.Mok TS, Wu YL, Thongprasert S, Yang CH, Chu DT, Saijo N, et al Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361:947–57. doi: 10.1056/NEJMoa0810699. [DOI] [PubMed] [Google Scholar]
- 5.Paik PK, Drilon A, Fan PD, Yu H, Rekhtman N, Ginsberg MS, et al Response to MET inhibitors in patients with stage IV lung adenocarcinomas harboring MET mutations causing exon 14 skipping . Cancer Discov. 2015;8:842–9. doi: 10.1158/2159-8290.CD-14-1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mazières J, Peters S, Lepage B, Cortot AB, Barlesi F, Beau-Faller M, et al Lung cancer that harbors an HER2 mutation: epidemiologic characteristics and therapeutic perspectives . J Clin Oncol. 2013;31:1997–2003. doi: 10.1200/JCO.2012.45.6095. [DOI] [PubMed] [Google Scholar]
- 7.Hyman DM, Puzanov I, Subbiah V, Faris JE, Chau I, Blay JY, et al Vemurafenib in multiple nonmelanoma cancers with BRAF V600 mutations . N Engl J Med. 2015;373:726–36. doi: 10.1056/NEJMoa1502309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kwak EL, Bang YJ, Camidge DR, Shaw AT, Solomon B, Maki RG, et al Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med. 2010;363:1693–703. doi: 10.1056/NEJMoa1006448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shaw AT, Ou SHI, Bang YJ, Camidge DR, Solomon BJ, Salgia R, et al Crizotinib in ROS1-rearranged non-small-cell lung cancer . N Engl J Med. 2014;371:1963–71. doi: 10.1056/NEJMoa1406766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Drilon A, Rekhtman N, Arcila M, Wang L, Ni A, Albano M, et al Cabozantinib in patients with advanced RET-rearranged non-small-cell lung cancer: an open-label, single-centre, phase 2, single-arm trial . Lancet Oncol. 2016;17:1653–60. doi: 10.1016/S1470-2045(16)30562-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kohno T, Ichikawa H, Totoki Y, Yasuda K, Hiramoto M, Nammo T, et al KIF5B-RET fusions in lung adenocarcinoma . Nat Med. 2012;18:375–7. doi: 10.1038/nm.2644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hyman DM, Laetsch TW, Kummar S, DuBois SG, Farago AF, Pappo AS, et al The efficacy of larotrectinib (LOXO-101), a selective tropomyosin receptor kinase (TRK) inhibitor, in adult and pediatric TRK fusion cancers. J Clin Oncol. 2017;35:LBA2501. doi: 10.1200/JCO.2017.35.15_suppl.LBA2501. [DOI] [Google Scholar]
- 13.Sandler A, Gray R, Perry MC, Brahmer J, Schiller JH, Dowlati A, et al Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med. 2006;355:2542–50. doi: 10.1056/NEJMoa061884. [DOI] [PubMed] [Google Scholar]
- 14.Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, et al Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med. 2015;373:1627–39. doi: 10.1056/NEJMoa1507643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garon EB, Rizvi NA, Hui RN, Leighl N, Balmanoukian AS, Eder JP, et al Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med. 2015;372:2018–28. doi: 10.1056/NEJMoa1501824. [DOI] [PubMed] [Google Scholar]
- 16.Horn L, Mansfield AS, Szczęsna A, Havel L, Krzakowski M, Hochmair MJ, et al First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med. 2018;379:2220–9. doi: 10.1056/NEJMoa1809064. [DOI] [PubMed] [Google Scholar]
- 17.Kobayashi S, Boggon TJ, Dayaram T, Jänne PA, Kocher O, Meyerson M, et al EGFR mutation and resistance of non-small-cell lung cancer to gefitinib . N Engl J Med. 2005;352:786–792. doi: 10.1056/NEJMoa044238. [DOI] [PubMed] [Google Scholar]
- 18.SEER Cancer Stat Facts. Lung and bronchus cancer. [Accessed November 29, 2018], Available from:<a href="https://seer.cancer.gov/statfacts/html/lungb.html">https://seer.cancer.gov/statfacts/html/lungb.html</a>.
- 19.Gazdar AF, Bunn PA, Minna JD. Small-cell lung cancer: what we know, what we need to know and the path forward. Nat Rev Cancer. 2017;17:725-37.
- 20.World Health Organization. Tobacco fact sheet 2017. Available from: <a href="https://www.smokefreeworld.org/">https://www.smokefreeworld.org/</a>. [Accessed Jul 29, 2019]
- 21.Carter BD, Abnet CC, Feskanich D, Freedman ND, Hartge P, Lewis CE, et al Smoking and mortality - beyond established causes. N Engl J Med. 2015;372:631–40. doi: 10.1056/NEJMsa1407211. [DOI] [PubMed] [Google Scholar]
- 22.Services USDoHaH. The health consequences of smoking-50 years of progress: a report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services; 2014.
- 23.World Health Organization. Cancer fact sheets 2019. Available from: <a href="http://gco.iarc.fr/today/fact-sheets-cancers">http://gco.iarc.fr/today/fact-sheets-cancers</a>. [Accessed May 8, 2019]
- 24.Hecht SS, Szabo E Fifty years of tobacco carcinogenesis research: from mechanisms to early detection and prevention of lung cancer. Cancer Prev Res. 2014;7:1–8. doi: 10.1158/1940-6207.CAPR-13-0371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hecht SS Lung carcinogenesis by tobacco smoke. Int J Cancer. 2012;131:2724–32. doi: 10.1002/ijc.27816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2010.
- 27.World Health Organization. Who global report on trends in prevalence of tobacco smoking 2000-2025. 2nd ed. Geneva, Switzerland: World Health Organization; 2018.
- 28.Siegel RL, Miller KD, Jemal A Cancer statistics, 2019. CA: A Cancer J Clin. 2019;69:7–34. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 29.International Agency for Research on Cancer of World Health Organization. Cancer tomorrow. [Accessed February 10, 2019], Available from: <a href="http://gco.Iarc.Fr/tomorrow/graphic-isotype">http://gco.Iarc.Fr/tomorrow/graphic-isotype</a>.
- 30.Akimoto H Global air quality and pollution. Science. 2003;302:1716–9. doi: 10.1126/science.1092666. [DOI] [PubMed] [Google Scholar]
- 31.Huang RJ, Zhang YL, Bozzetti C, Ho KF, Cao JJ, Han YM, et al High secondary aerosol contribution to particulate pollution during haze events in china. Nature. 2014;514:218–22. doi: 10.1038/nature13774. [DOI] [PubMed] [Google Scholar]
- 32.Ho KF, Ho SSH, Huang RJ, Chuang HC, Cao JJ, Han YM, et al Chemical composition and bioreactivity of PM2.5 during 2013 haze events in china. Atmos Environ. 2016;126:162–70. doi: 10.1016/j.atmosenv.2015.11.055. [DOI] [Google Scholar]
- 33.WHO Regional Office for Europe. Air quality guidelines. Global update 2005. Particulate matter, ozone, nitrogen dioxide and sulfur dioxide. Copenhagen 2006. [Accessed July 11, 2019], Available from: <a href="http://www.euro.who.int/en/health-topics/environment-and-health/air-quality/publications/pre2009/air-quality-guidelines.-global-update-2005.-particulate-matter,-ozone,-nitrogen-dioxide-and-sulfur-dioxide">http://www.euro.who.int/en/health-topics/environment-and-health/air-quality/publications/pre2009/air-quality-guidelines.-global-update-2005.-particulate-matter,-ozone,-nitrogen-dioxide-and-sulfur-dioxide</a>.
- 34.World Health Organization. Ambient (outdoor) air quality and health. [Accessed November 12, 2018], Available from: <a href="http://www.Who.Int/mediacentre/factsheets/fs313/en/">http://www.Who.Int/mediacentre/factsheets/fs313/en/</a>.
- 35.WHO Regional Office for Europe. Who guidelines for indoor air quality: selected pollutants. [Accessed July 11, 2019], Available from: <a href="http://www.euro.who.int/en/health-topics/environment-and-health/air-quality/publications/2010/who-guidelines-for-indoor-air-quality-selected-pollutants">http://www.euro.who.int/en/health-topics/environment-and-health/air-quality/publications/2010/who-guidelines-for-indoor-air-quality-selected-pollutants</a>.
- 36.World Health Organization. Household air pollution and health. [Accessed October 1, 2019], Available from: <a href="https://www.Who.Int/news-room/fact-sheets/detail/household-air-pollution-and-health">https://www.Who.Int/news-room/fact-sheets/detail/household-air-pollution-and-health</a>.
- 37.Schraufnagel DE, Balmes JR, Cowl CT, De Matteis S, Jung S-H, Mortimer K, et al. Air pollution and noncommunicable diseases: A review by the forum of international respiratory societies’ environmental committee, part 2: Air pollution and organ systems. Chest. 2019; 155:417-426.
- 38.Xiao YZ, Shao Y, Yu XJ, Zhou GB The epidemic status and risk factors of lung cancer in Xuanwei City, Yunnan Province, China. Front Med. 2012;6:388–4. doi: 10.1007/s11684-012-0233-3. [DOI] [PubMed] [Google Scholar]
- 39.Cao Y, Gao HP Prevalence and causes of air pollution and lung cancer in Xuanwei city and Fuyuan County, Yunnan Province, China. Front Med. 2012;6:217–20. doi: 10.1007/s11684-012-0192-8. [DOI] [PubMed] [Google Scholar]
- 40.Mumford JL, He XZ, Chapman RS, Cao SR, Harris DB, Li XM, et al Lung cancer and indoor air pollution in Xuan Wei, China. Science. 1987;235:217–20. doi: 10.1126/science.3798109. [DOI] [PubMed] [Google Scholar]
- 41.Lan Q, Chapman RS, Schreinemachers DM, Tian L, He X Household stove improvement and risk of lung cancer in Xuanwei, China. J Natl Cancer Inst. 2002;94:826–35. doi: 10.1093/jnci/94.11.826. [DOI] [PubMed] [Google Scholar]
- 42.Xu Y, Wang YH, Besnard V, Ikegami M, Wert SE, Heffner C, et al Transcriptional programs controlling perinatal lung maturation. PLoS One. 2012;7:e37046. doi: 10.1371/journal.pone.0037046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Raaschou-Nielsen O, Andersen ZJ, Beelen R, Samoli E, Stafoggia M, Weinmayr G, et al Air pollution and lung cancer incidence in 17 European cohorts: prospective analyses from the European study of cohorts for air pollution effects (ESCAPE) Lancet Oncol. 2013;14:813–22. doi: 10.1016/S1470-2045(13)70279-1. [DOI] [PubMed] [Google Scholar]
- 44.Li JH, Zhang YS, Li Y, Yin GQ, Li YB, Ning BF, et al Descriptive study on the epidemiology of lung cancer in coal-producing area in Eastern Yunnan, China. Chin J Lung Cancer. 2011;14:107–19. doi: 10.3779/j.issn.1009-3419.2011.02.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.The Cancer Genome Atlas Research Network Comprehensive molecular profiling of lung adenocarcinoma. Nature. 2014;511:543–50. doi: 10.1038/nature13385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.The Cancer Genome Atlas Research Network Comprehensive genomic characterization of squamous cell lung cancers. Nature. 2012;489:519–25. doi: 10.1038/nature11404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.George J, Lim JS, Jang SJ, Cun YP, Ozretić L, Kong G, et al Comprehensive genomic profiles of small cell lung cancer. Nature. 2015;524:47–53. doi: 10.1038/nature14664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Imielinski M, Berger AH, Hammerman PS, Hernandez B, Pugh TJ, et al Mapping the hallmarks of lung adenocarcinoma with massively parallel sequencing. Cell. 2012;150:1107–20. doi: 10.1016/j.cell.2012.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Eisenstadt E, Warren AJ, Porter J, Atkins D, Miller JH Carcinogenic epoxides of benzo[a]pyrene and cyclopenta[cd]pyrene induce base substitutions via specific transversions. Proc Natl Acad Sci USA. 1982;79:1945–9. doi: 10.1073/pnas.79.6.1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ronai ZA, Gradia S, Peterson LA, Hecht SS G to a transitions and g to t transversions in codon 12 of the Ki-ras oncogene isolated from mouse lung tumors induced by 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) and relati DNA methylating and pyridyloxobutylating agents. Carcinogenesis. 1993;14:2419–22. doi: 10.1093/carcin/14.11.2419. [DOI] [PubMed] [Google Scholar]
- 51.Chappell G, Pogribny IP, Guyton KZ, Rusyn I Epigenetic alterations induced by genotoxic occupational and environmental human chemical carcinogens: a systematic literature review. Mutat Res Rev Mutat Res. 2016;768:27–45. doi: 10.1016/j.mrrev.2016.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Manjanatha MG H- and K-ras mutational profiles in chemically induced liver tumors from B6C3F1 and Cd-1 mice. J Toxicol Environ Health. 1996;47:195–208. doi: 10.1080/009841096161898. [DOI] [PubMed] [Google Scholar]
- 53.Ma HB, Wood TG, Ammenheuser MM, Rosenblatt JI, Ward JB Jr Molecular analysis of hprt mutant lymphocytes from 1,3-butadiene-exposed workers . Environ Mol Mutagen. 2000;36:59–71. doi: 10.1002/1098-2280(2000)36:1<59::AID-EM9>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 54.Pfeifer GP, Denissenko MF, Olivier M, Tretyakova N, Hecht SS, Hainaut P Tobacco smoke carcinogens, DNA damage and p53 mutations in smoking-associated cancers. Oncogene. 2002;21:7435–51. doi: 10.1038/sj.onc.1205803. [DOI] [PubMed] [Google Scholar]
- 55.Zhou GB, Zhao XC Carcinogens that induce the A: T > T: A nucleotide substitutions in the genome. Front Med. 2018;12:236–8. doi: 10.1007/s11684-017-0611-y. [DOI] [PubMed] [Google Scholar]
- 56.Husgafvel-Pursiainen K, Boffetta P, Kannio A, Nyberg F, Pershagen G, Mukeria A, et al p53 mutations and exposure to environmental tobacco smoke in a multicenter study on lung cancer . Cancer Res. 2000;60:2906–11. [PubMed] [Google Scholar]
- 57.Le Calvez F, Mukeria A, Hunt JD, Kelm O, Hung RJ, Tanière P, et al TP53 and KRAS mutation load and types in lung cancers in relation to tobacco smoke: distinct patterns in never, former, and current smokers . Cancer Res. 2005;65:5076–83. doi: 10.1158/0008-5472.CAN-05-0551. [DOI] [PubMed] [Google Scholar]
- 58.Couraud S, Zalcman G, Milleron B, Morin F, Souquet PJ Lung cancer in never smokers - a review. Eur J Cancer. 2012;48:1299–311. doi: 10.1016/j.ejca.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 59.Couraud S, Souquet PJ, Paris C, Dô P, Doubre H, Pichon E, et al BioCAST/IFCT-1002: epidemiological and molecular features of lung cancer in never-smokers. Eur Resp J. 2015;45:1403–14. doi: 10.1183/09031936.00097214. [DOI] [PubMed] [Google Scholar]
- 60.Tissot C, Couraud S, Tanguy R, Bringuier PP, Girard N, Souquet PJ Clinical characteristics and outcome of patients with lung cancer harboring BRAF mutations. Lung Cancer. 2016;91:23–8. doi: 10.1016/j.lungcan.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 61.Shigematsu H, Gazdar AF Somatic mutations of epidermal growth factor receptor signaling pathway in lung cancers. Int J Cancer. 2006;118:257–62. doi: 10.1002/ijc.21496. [DOI] [PubMed] [Google Scholar]
- 62.Fukui T, Yatabe Y, Kobayashi Y, Tomizawa K, Ito S, Hatooka S, et al Clinicoradiologic characteristics of patients with lung adenocarcinoma harboring EML4-ALK fusion oncogene . Lung Cancer. 2012;77:319–25. doi: 10.1016/j.lungcan.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 63.Barlesi F, Mazieres J, Merlio JP, Debieuvre D, Mosser J, Lena H, et al Routine molecular profiling of patients with advanced non-small-cell lung cancer: results of a 1-year nationwide programme of the french cooperative thoracic intergroup (IFCT) Lancet. 2016;387:1415–26. doi: 10.1016/S0140-6736(16)00004-0. [DOI] [PubMed] [Google Scholar]
- 64.Alexandrov LB, Ju YS, Haase K, Van Loo P, Martincorena I, Nik-Zainal S, et al Mutational signatures associated with tobacco smoking in human cancer. Science. 2016;354:618–22. doi: 10.1126/science.aag0299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Govindan R, Ding L, Griffith M, Subramanian J, Dees ND, Kanchi KL, et al Genomic landscape of non-small cell lung cancer in smokers and never-smokers. Cell. 2012;150:1121–34. doi: 10.1016/j.cell.2012.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gibelin C, Couraud S Somatic alterations in lung cancer: do environmental factors matter? Lung Cancer. 2016;100:45–52. doi: 10.1016/j.lungcan.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 67.Yu XJ, Yang MJ, Zhou B, Wang GZ, Huang YC, Wu LC, et al Characterization of somatic mutations in air pollution-related lung cancer. EBioMedicine. 2015;2:583–90. doi: 10.1016/j.ebiom.2015.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Martincorena I, Campbell PJ Somatic mutation in cancer and normal cells. Science. 2015;349:1483–9. doi: 10.1126/science.aab4082. [DOI] [PubMed] [Google Scholar]
- 69.Martincorena I, Roshan A, Gerstung M, Ellis P, Van Loo P, McLaren S, et al High burden and pervasive positive selection of somatic mutations in normal human skin. Science. 2015;348:880–6. doi: 10.1126/science.aaa6806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Qu LW, Zhou B, Wang GZ, Chen Y, Zhou GB Genomic variations in paired normal controls for lung adenocarcinomas. Oncotarget. 2017;8:104113–22. doi: 10.18632/oncotarget.22020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhang DL, Qu LW, Zhou B, Wang GZ, Zhou GB Genomic variations in the counterpart normal controls of lung squamous cell carcinomas. Front Med. 2018;12:280–8. doi: 10.1007/s11684-017-0580-1. [DOI] [PubMed] [Google Scholar]
- 72.Kargı A, Dinç ZA, Başok O, Üçvet A MUC4 expression and its relation to ErbB2 expression, apoptosis, proliferation, differentiation, and tumor stage in non-small cell lung cancer (NSCLC) Pathol Res Pract. 2006;202:577–83. doi: 10.1016/j.prp.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 73.Qiu L, Wu J, Pan C, Tan X, Lin J, Liu R, et al Downregulation of CDC27 inhibits the proliferation of colorectal cancer cells via the accumulation of p21Cip1/Waf1. Cell Death Dis. 2016;7:e2074. doi: 10.1038/cddis.2015.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wang W, Song XW, Bu XM, Zhang N, Zhao CH PDCD2 and NCoR1 as putative tumor suppressors in gastric gastrointestinal stromal tumors. Cellular Oncol. 2016;39:129–137. doi: 10.1007/s13402-015-0258-0. [DOI] [PubMed] [Google Scholar]
- 75.Danan-Gotthold M, Golan-Gerstl R, Eisenberg E, Meir K, Karni R, Levanon EY Identification of recurrent regulated alternative splicing events across human solid tumors. Nucl Acid Res. 2015;43:5130–44. doi: 10.1093/nar/gkv210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wiesner T, Lee W, Obenauf AC, Ran LL, Murali R, Zhang QF, et al Alternative transcription initiation leads to expression of a novel ALK isoform in cancer. Nature. 2015;526:453–7. doi: 10.1038/nature15258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Weng MW, Lai JC, Hsu CP, Yu KY, Chen CY, Lin TS, et al Alternative splicing of MDM2 mrna in lung carcinomas and lung cell lines . Environ Mol Mutagen. 2005;46:1–11. doi: 10.1002/em.20118. [DOI] [PubMed] [Google Scholar]
- 78.Zhou B, Wang GZ, Wen ZS, Zhou YC, Huang YC, Chen Y, et al Somatic mutations and splicing variants of focal adhesion kinase in non-small cell lung cancer. J Natl Cancer Inst. 2018;110:195–204. doi: 10.1093/jnci/djx157. [DOI] [PubMed] [Google Scholar]
- 79.Hanahan D, Weinberg RA Hallmarks of cancer: the next generation. Cell. 2011;144:646–74. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 80.Rothhammer V, Quintana FJ The aryl hydrocarbon receptor: an environmental sensor integrating immune responses in health and disease. Nat Rev Immunol. 2019;19:184–97. doi: 10.1038/s41577-019-0125-8. [DOI] [PubMed] [Google Scholar]
- 81.Murray IA, Patterson AD, Perdew GH Aryl hydrocarbon receptor ligands in cancer: friend and foe. Nat Rev Cancer. 2014;14:801–14. doi: 10.1038/nrc3846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Opitz CA, Litzenburger UM, Sahm F, Ott M, Tritschler I, Trump S, et al An endogenous tumour-promoting ligand of the human aryl hydrocarbon receptor. Nature. 2011;478:197–203. doi: 10.1038/nature10491. [DOI] [PubMed] [Google Scholar]
- 83.Shimizu Y, Nakatsuru Y, Ichinose M, Takahashi Y, Kume H, Mimura J, et al Benzo[a]pyrene carcinogenicity is lost in mice lacking the aryl hydrocarbon receptor. Proc Natl Acad Sci USA. 2000;97:779–82. doi: 10.1073/pnas.97.2.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Moennikes O, Loeppen S, Buchmann A, Andersson P, Ittrich C, Poellinger L, et al A constitutively active Dioxin/Aryl hydrocarbon receptor promotes hepatocarcinogenesis in mice. Cancer Res. 2004;64:4707–10. doi: 10.1158/0008-5472.CAN-03-0875. [DOI] [PubMed] [Google Scholar]
- 85.Andersson P, McGuire J, Rubio C, Gradin K, Whitelaw ML, Pettersson S, et al A constitutively active dioxin/aryl hydrocarbon receptor induces stomach tumors. Proc Natl Acad Sci USA. 2002;99:9990–5. doi: 10.1073/pnas.152706299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wang GZ, Zhang L, Zhao XC, Gao SH, Qu LW, Yu H, et al The Aryl hydrocarbon receptor mediates tobacco-induced PD-L1 expression and is associated with response to immunotherapy. Nat Commun. 2019;10:1125. doi: 10.1038/s41467-019-08887-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Shen J, Xu LJ, Owonikoko TK, Sun SY, Khuri FR, Curran WJ, et al NNK promotes migration and invasion of lung cancer cells through activation of c-Src/PKCι/FAK loop. Cancer Lett. 2012;318:106–13. doi: 10.1016/j.canlet.2011.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ma L, Wen ZS, Liu Z, Hu Z, Ma J, Chen XQ, et al Overexpression and small molecule-triggered downregulation of CIP2A in lung cancer. PLoS One. 2011;6:e20159. doi: 10.1371/journal.pone.0020159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nath S, Ohlmeyer M, Salathe MA, Poon J, Baumlin N, Foronjy RF, et al Chronic cigarette smoke exposure subdues PP2A activity by enhancing expression of the oncogene CIP2A. Am J Respir Cell Mol Biol. 2018;59:695–705. doi: 10.1165/rcmb.2018-0173OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhao XC, Wang GZ, Zhou YC, Ma L, Liu J, Zhang C, et al. Genome-wide identification of CDC34 that stabilizes EGFR and promotes lung carcinogenesis. bioRxiv. 2018; doi: <a href="http://dx.doi.org/10.1101/255844">10.1101/255844</a>.
- 91.Lin RK, Hsieh YS, Lin PP, Hsu HS, Chen CY, Tang YA, et al The tobacco-specific carcinogen NNK induces DNA methyltransferase 1 accumulation and tumor suppressor gene hypermethylation in mice and lung cancer patients. J Clin Invest. 2010;120:521–32. doi: 10.1172/JCI40706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zhang RY, Chu MJ, Zhao Y, Wu C, Guo H, Shi YY, et al A genome-wide gene-environment interaction analysis for tobacco smoke and lung cancer susceptibility. Carcinogenesis. 2014;35:1528–35. doi: 10.1093/carcin/bgu076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Huang T, Chen XY, Hong QX, Deng ZC, Ma HY, Xin YF, et al Meta-analyses of gene methylation and smoking behavior in non-small cell lung cancer patients. Sci Rep. 2015;5:8897. doi: 10.1038/srep08897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Jiang CL, He SW, Zhang YD, Duan HX, Huang T, Huang YC, et al Air pollution and DNA methylation alterations in lung cancer: a systematic and comparative study. Oncotarget. 2017;8:1369–91. doi: 10.18632/oncotarget.13622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Schembri F, Sridhar S, Perdomo C, Gustafson AM, Zhang XL, Ergun A, et al MicroRNAs as modulators of smoking-induced gene expression changes in human airway epithelium. Proc Natl Acad Sci USA. 2009;106:2319–24. doi: 10.1073/pnas.0806383106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Izzotti A, Calin GA, Arrigo P, Steele VE, Croce CM, de Flora S Downregulation of microrna expression in the lungs of rats exposed to cigarette smoke. FASEB J. 2009;23:806–12. doi: 10.1096/fj.08-121384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhang JL, Bai RH, Li M, Ye HL, Wu C, Wang CF, et al Excessive miR-25-3p maturation via N6-methyladenosine stimulated by cigarette smoke promotes pancreatic cancer progression . Nat Commun. 2019;10:1858. doi: 10.1038/s41467-019-09712-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Maccani MA, Knopik VS Cigarette smoke exposure-associated alterations to non-coding RNA. Front Genet. 2012;3:53. doi: 10.3389/fgene.2012.00053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Russ R, Slack FJ Cigarette-smoke-induced dysregulation of MicroRNA expression and its role in lung carcinogenesis. Pulm Med. 2012;2012:791234. doi: 10.1155/2012/791234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Guttman M, Rinn JL Modular regulatory principles of large non-coding RNAs. Nature. 2012;482:339–46. doi: 10.1038/nature10887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gao LY, Mai A, Li X, Lai YD, Zheng JL, Yang QY, et al LncRNA-DQ786227-mediated cell malignant transformation induced by benzo(a)pyrene. Toxicol Lett. 2013;223:205–10. doi: 10.1016/j.toxlet.2013.09.015. [DOI] [PubMed] [Google Scholar]
- 102.Hu GC, Yang T, Zheng JL, Dai JB, Nan AR, Lai YD, et al Functional role and mechanism of lncrna loc728228 in malignant 16hbe cells transformed by anti-benzopyrene-trans-7,8-dihydrodiol-9,10-epoxide. Mol Carcinog. 2015;54 Suppl 1:E192–204. doi: 10.1002/mc.22314. [DOI] [PubMed] [Google Scholar]
- 103.Thai P, Statt S, Chen CH, Liang E, Campbell C, Wu RE Characterization of a novel long noncoding RNA, SCAL1, induced by cigarette smoke and elevated in lung cancer cell lines. Am J Respir Cell Mol Biol. 2013;49:204–11. doi: 10.1165/rcmb.2013-0159RC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wei MM, Zhou GB Long non-coding RNAs and their roles in non-small-cell lung cancer. Genomics Proteomics Bioinformatics. 2016;14:280–8. doi: 10.1016/j.gpb.2016.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wei MM, Zhou YC, Wen ZS, Zhou B, Huang YC, Wang GZ, et al Long non-coding RNA stabilizes the Y-box-binding protein 1 and regulates the epidermal growth factor receptor to promote lung carcinogenesis. Oncotarget. 2016;7:59556–71. doi: 10.18632/oncotarget.10006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Shaykhiev R, Sackrowitz R, Fukui T, Zuo WL, Chao IW, Strulovici-Barel Y, et al Smoking-induced CXCL14 expression in the human airway epithelium links chronic obstructive pulmonary disease to lung cancer. Am J Respir Cell Mol Biol. 2013;49:418–25. doi: 10.1165/rcmb.2012-0396OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Vlahos R, Bozinovski S, Jones JE, Powell J, Gras J, Lilja A, et al Differential protease, innate immunity, and NF-κB induction profiles during lung inflammation induced by subchronic cigarette smoke exposure in mice. Am J Physiol Lung Cell Mol Physiol. 2006;290:L931–5. doi: 10.1152/ajplung.00201.2005. [DOI] [PubMed] [Google Scholar]
- 108.Hussain SP, Hofseth LJ, Harris CC Radical causes of cancer. Nat Rev Cancer. 2003;3:276–85. doi: 10.1038/nrc1046. [DOI] [PubMed] [Google Scholar]
- 109.Karin M, Greten FR NF-κB: linking inflammation and immunity to cancer development and progression. Nat Rev Immunol. 2005;5:749–59. doi: 10.1038/nri1703. [DOI] [PubMed] [Google Scholar]
- 110.Takahashi H, Ogata H, Nishigaki R, Broide DH, Karin M Tobacco smoke promotes lung tumorigenesis by triggering IKKβ- and JNK1-dependent inflammation. Cancer Cell. 2010;17:89–97. doi: 10.1016/j.ccr.2009.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Wang GZ, Cheng X, Li XC, Liu YQ, Wang XQ, Shi X, et al Tobacco smoke induces production of chemokine CCL20 to promote lung cancer. Cancer Lett. 2015;363:60–70. doi: 10.1016/j.canlet.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 112.Wang GZ, Cheng X, Zhou B, Wen ZS, Huang YC, Chen HB, et al The chemokine CXCL13 in lung cancers associated with environmental polycyclic aromatic hydrocarbons pollution. eLife. 2015;4:e09419. doi: 10.7554/eLife.09419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Shiels MS, Pfeiffer RM, Hildesheim A, Engels EA, Kemp TJ, Park JH, et al Circulating inflammation markers and prospective risk for lung cancer. J Natl Cancer Inst. 2013;105:1871–80. doi: 10.1093/jnci/djt309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Albrengues J, Shields MA, Ng D, Park CG, Ambrico A, Poindexter ME, et al Neutrophil extracellular traps produced during inflammation awaken dormant cancer cells in mice. Science. 2018;361:eaao4227. doi: 10.1126/science.aao4227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Rizvi NA, Hellmann MD, Snyder A, Kvistborg P, Makarov V, Havel JJ, et al Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science. 2015;348:124–8. doi: 10.1126/science.aaa1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Deng L, Gyorffy B, Na FF, Chen BQ, Lan J, Xue JX, et al Association of PDCD1 and CTLA-4 gene expression with clinicopathological factors and survival in non-small-cell lung cancer: results from a large and pooled microarray database . J Thorac Oncol. 2015;10:1020–6. doi: 10.1097/JTO.0000000000000550. [DOI] [PubMed] [Google Scholar]
- 117.Mascaux C, Angelova M, Vasaturo A, Beane J, Hijazi K, Anthoine G, et al Immune evasion before tumour invasion in early lung squamous carcinogenesis. Nature. 2019;571:570–5. doi: 10.1038/s41586-019-1330-0. [DOI] [PubMed] [Google Scholar]
- 118.Chen Z, Wang JN, Ma GX, Zhang YS China tackles the health effects of air pollution. Lancet. 2013;382:1959–60. doi: 10.1016/S0140-6736(13)62064-4. [DOI] [PubMed] [Google Scholar]
- 119.Adams J The proteasome: a suitable antineoplastic target. Nat Rev Cancer. 2004;4:349–60. doi: 10.1038/nrc1361. [DOI] [PubMed] [Google Scholar]
- 120.Patel H, Pawara R, Ansari A, Surana S Recent updates on third generation EGFR inhibitors and emergence of fourth generation EGFR inhibitors to combat C797S resistance. Eur J Med Chem. 2017;142:32–47. doi: 10.1016/j.ejmech.2017.05.027. [DOI] [PubMed] [Google Scholar]
- 121.Wang SH, Song YP, Yan FF, Liu DL Mechanisms of resistance to third-generation egfr tyrosine kinase inhibitors. Front Med. 2016;10:383–8. doi: 10.1007/s11684-016-0488-1. [DOI] [PubMed] [Google Scholar]
- 122.Wang L, Zhou GB, Liu P, Song JH, Liang Y, Yan XJ, et al Dissection of mechanisms of Chinese medicinal formula realgar-Indigo naturalis as an effective treatment for promyelocytic leukemia . Proc Natl Acad Sci USA. 2008;105:4826–31. doi: 10.1073/pnas.0712365105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wu S, Powers S, Zhu W, Hannun YA Substantial contribution of extrinsic risk factors to cancer development. Nature. 2016;529:43–7. doi: 10.1038/nature16166. [DOI] [PMC free article] [PubMed] [Google Scholar]