Abstract
Increasingly, primary hypertension is being considered a syndrome and not a disease, with the individual causes (diseases) having a common sign—an elevated blood pressure. To determine these causes, genetic tools are increasingly employed. This review identified 62 proposed genes. However, only 21 of them met our inclusion criteria: (i) primary hypertension, (ii) two or more supporting cohorts from different publications or within a single publication or one supporting cohort with a confirmatory genetically modified animal study, and (iii) 600 or more subjects in the primary cohort; when including our exclusion criteria: (i) meta-analyses or reviews, (ii) secondary and monogenic hypertension, (iii) only hypertensive complications, (iv) genes related to blood pressure but not hypertension per se, (v) nonsupporting studies more common than supporting ones, and (vi) studies that did not perform a Bonferroni or similar multiassessment correction. These 21 genes were organized in a four-tiered structure: distant phenotype (hypertension); intermediate phenotype [salt-sensitive (18) or salt-resistant (0)]; subintermediate phenotypes under salt-sensitive hypertension [normal renin (4), low renin (8), and unclassified renin (6)]; and proximate phenotypes (specific genetically driven hypertensive subgroup). Many proximate hypertensive phenotypes had a substantial endocrine component. In conclusion, primary hypertension is a syndrome; many proposed genes are likely to be false positives; and deep phenotyping will be required to determine the utility of genetics in the treatment of hypertension. However, to date, the positive genes are associated with nearly 50% of primary hypertensives, suggesting that in the near term precise, mechanistically driven treatment and prevention strategies for the specific primary hypertension subgroups are feasible.
Essential Points.
Primary hypertension is not a disease but a syndrome whose individual diseases have a common sign—an elevated blood pressure
Substantial preclinical and clinical data have documented that increased blood pressure and its accompanying substantial cardiovascular risks are largely secondary to the interplay between genetics and environment
Sixty-two genes were identified as potential candidates for this review
Only 21 of the 62 candidate genes met the following criteria: two supporting cohorts from different publications or two different cohorts within a single publication or a single positive cohort with a confirmatory genetically modified animal study
In all but three genes, deeper phenotyping studies beyond hypertension had been performed
Of the 21 genes, 18 were associated with salt-sensitive hypertension: 4 with normal renin levels, 8 with lower renin levels, and 6 with undefined renin levels
These 18 genotype/phenotype groups are associated with nearly 50% of the primary hypertension population, suggesting that precise mechanistically driven treatment/prevention strategies for the individual primary hypertension phenotypes are feasible in the near term
Hypertension is the leading contributing factor to all-cause global mortality. It is the main risk factor for stroke (ischemic and hemorrhagic) and coronary artery disease. Furthermore, people with hypertension are predisposed to renal failure, heart failure, peripheral vascular disease, and other medical conditions (1). It is estimated that, worldwide, nearly 1.4 billion adults (20% of females and 25% of males age >18 years old) have hypertension (1). Successful treatment rates vary from modest to poor. An acknowledged substantial contributor to this low success rate is the lack of definitive data as to the mechanism(s) for the hypertension in the individual patient and, therefore, the lack of therapy to treat the specific underlying cause (“disease”) rather than the more distant sign—the blood pressure.
Hypertension as a syndrome
An increasing body of knowledge that had its origin decades ago suggests that hypertension is not a disease but a syndrome whose individual diseases have a common sign—an elevated blood pressure. By the mid-20th century it was known that there were secondary causes of hypertension. However, the hypothesis that nearly the entire “essential” population with hypertension is composed of “secondary” subsets is a phenomenon of the 21st century. Thus, currently there are at least six factors to consider when addressing the hypertension treatment dilemma described above.
First, for 85% to 90% of people with hypertension, there is no specific cause. These individuals are grouped together in a single category—essential (primary) hypertension.
Second, nearly all the secondary forms of hypertension are due to dysfunction in one or more of the endocrine systems (2).
Third, it has long been known that there is a strong heritable component to hypertension with heritability estimates ranging from 25% to 60% in the general populations (3–13).
Fourth, substantial preclinical and clinical data have documented that an increased blood pressure and its accompanying substantial cardiovascular risks are largely secondary to the interplay between genetics and environment (3–13).
Fifth, for the past dozen years genome-wide association studies (GWASs) and whole-exome sequencing techniques have revealed many potential blood pressure–related pathways, but consistent associations with hypertension are infrequent to rare (14, 15). These results are not unique to hypertension, as similar results (pathway gene variants but no consistent disease variants) have been reported for other complex chronic diseases, for example, anemia and diabetes mellitus (16, 17).
Sixth, it is evident that what are termed “chronic complex diseases” are not actually diseases but syndromes, with several underlying diseases or causes potentially with their separate phenotype/genotype relationships. Recently this has been documented even with “rare diseases.” Some new rare diseases may be composites of two, or potentially more, separate genetic disease entities (causes) present in a single subject (18).
These concepts have led to an increased emphasis on understanding the human phenome with the development during the past decade of tools to do so, for example, the human Phenotype Ontology, PhenoMiner, and Phenolyzer (19–21).
Linkage and association techniques
Genetics studies fundamentally build on the premise that Mendel first demonstrated in the latter half of the 19th century, namely, that a specific genetic locus (genotype) is associated with a trait (phenotype) and therefore causative of the trait. For many monogenic conditions, linkage analyses have been used.
Linkage analyses usually require multigenerational family data, although sometimes the approach uses data from affected sibling pairs (siblings both having the same trait, e.g., hypertension). The hypothesis being tested is based on Mendel’s second law of independent assortment: genetic traits should not be linked in different individuals; that is, variants in individual genes should not cosegregate (22). Thus, when variants in a gene do cosegregate with a trait in a family, this result provides strong evidence for linkage of the gene to the trait and likely in a causative relationship.
A much more common statistical approach is association analysis using a case control method. In this approach relatedness is not required, but a “matched” control group is. This approach is increasing used in large-scale genetic studies (e.g., GWAS, exome, or whole-genome sequencing) and often requires highly sophisticated analytical techniques. “Big data” is the latest example of this approach. The overriding challenge of these new approaches is not the quality of the genetic component of the genotype/phenotype association but the reliability of the phenotypic data. The major hurdle to overcome for big data is the quality of the clinical data used. This may be particularly challenging for conditions such as hypertension where the so-called “disease” is actually a syndrome but coded in the medical records as a disease. Other challenges include population stratification (namely, the separation of a study population into subgroups) and identification of an appropriate control group. The latter challenge has been a major issue in studies of the genetics of hypertension, because the control group needs to consist of individuals who will always be normotensive—a difficult goal to achieve. Statistical evidence for an association between polymorphic variants of a gene and a phenotype can occur because the variant itself is functional and directly affects the expression of the phenotype; or it is correlated with, or in linkage disequilibrium with, a closely associated causative allele; or it is attributable to chance, artifact, or selection bias. Determining which of these conditions were met in each study is often difficult. In this review, we have attempted to address these challenges by reviewing the details as to how the studied population was selected. Many published reports reviewed did not meet the appropriate standards. Those that did were carefully controlled and/or assessed the clinical state of their subjects, specifically in relationship to known environmental factors that can influence blood pressure.
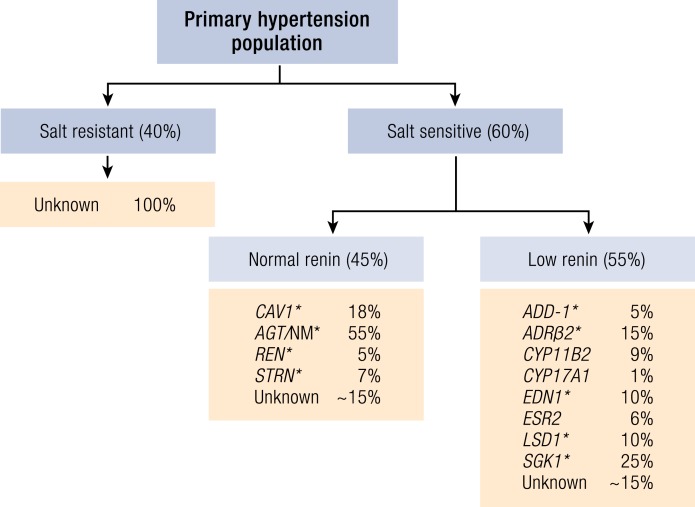
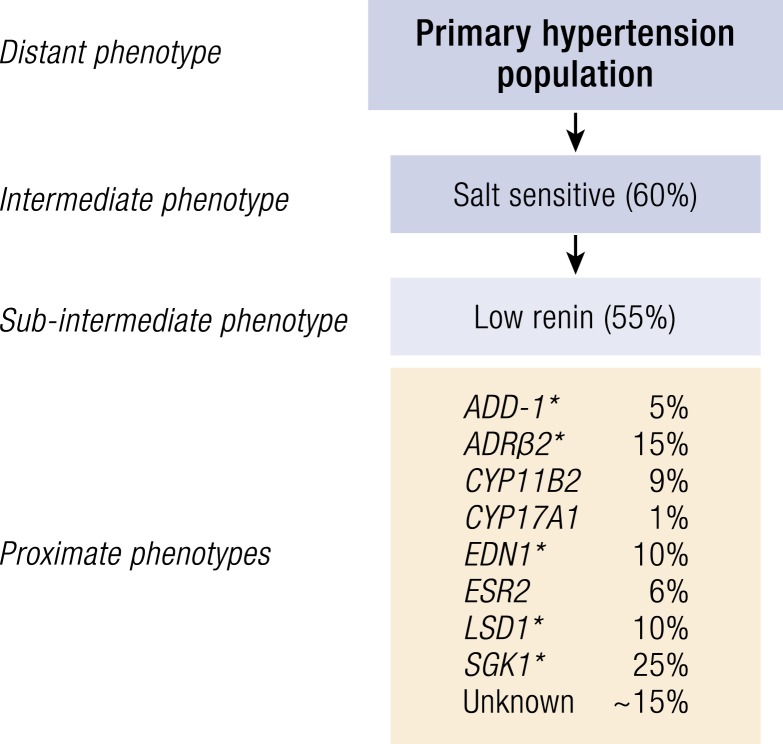
Rationale for Choosing Specific Genes/Phenotype Associations
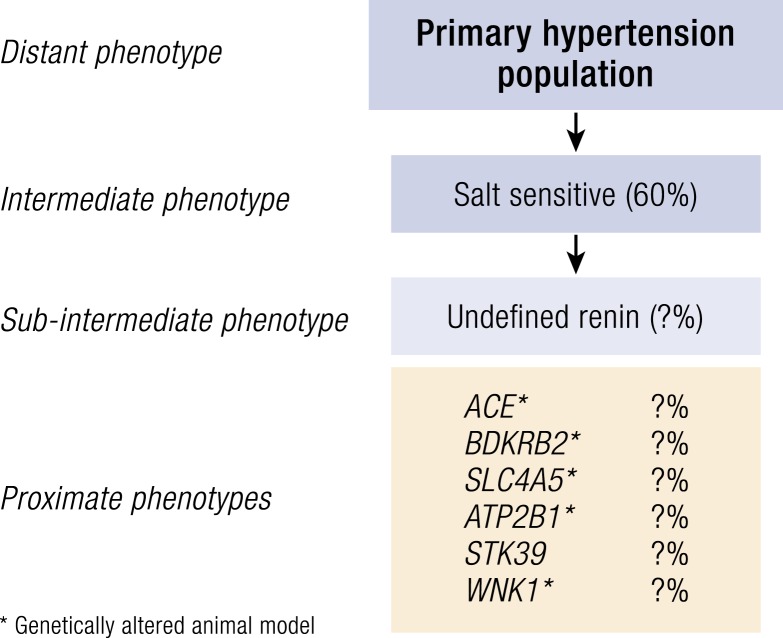
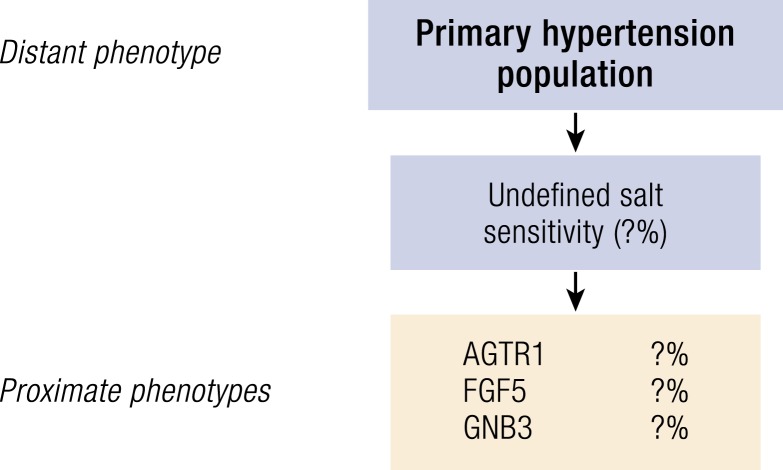
This genetics of hypertension review is focused on primary (essential) hypertension. The data are presented to emphasize that primary hypertension is a syndrome, not a disease. Thus, we have expanded the usual categorizing of hypertensive subgroups (2) into a traditional four-tiered genetic approach: (i) distant phenotype (hypertension); (ii) intermediate phenotype (salt-sensitive and salt-resistant hypertension); (iii) subintermediate phenotypes under salt-sensitive hypertension (normal renin and low renin); and (iv) proximate phenotypes (specific genotype–driven hypertensive subgroup) (Fig. 1). Thus, this approach first groups all hypertensive subjects into the most heterogeneous, distant phenotype (hypertension) and then successively subgroups them into increasingly more homogeneous groups, with the proximate phenotype groups being the most homogeneous and closest to the likely genetic mechanisms causing the hypertension. Of importance, each genetic subtype of primary hypertension has a substantial endocrine component, similar to what has been reported with secondary forms of hypertension. Finally, this review includes studies of genotype/phenotype relationships where either all or many of the subjects have hypertension. Studies where the phenotype assessed is only blood pressure per se and not hypertension are not included. Our reason to exclude these reports is that both animal and human studies have noted that genes involved with blood pressure control in the physiologic range may not always lead to hypertension. Therefore, we have used the more stringent phenotype—hypertension.
Figure 1.
Categorization of the genotype/phenotypes of primary (essential) hypertension. The entities are grouped into increasingly homogeneous physiological subgroups (distant, intermediate, subintermediate, and proximate phenotypes). The percentage, in parentheses indicates the faction of the subentity for each of the preceding primary entities; for example, 60% of the population with primary hypertension have salt-sensitive hypertension, and 55% of the group with salt sensitivity have low-renin hypertension.
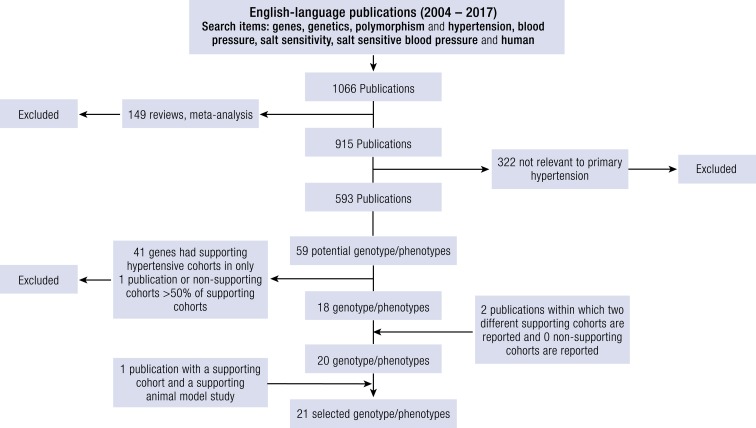
The data used in this review were acquired from an online search of the National Library of Medicine using the PubMed search engine from January 2004 through December 2017. Our approach is summarized in Fig. 2. Specifically, the search terms “genes,” “genetics,” “polymorphism with hypertension,” “blood pressure,” “salt sensitivity,” and “salt-sensitive blood pressure” were applied. The criteria used for a gene to be included in this review rested on three considerations. (i) Many genes have been reported to be associated with complex chronic phenotypes such as hypertension. With additional studies and analyses, often these associations are not replicated, for example, in hypertension (2). (ii) To reduce the number of potential false-positive associations, the criteria used herein are more restrictive than previous ones (2). We reasoned that ideally every gene should have replication of supporting studies in different cohorts, an association with deep phenotyping supporting the proposed mechanism(s) causing of the hypertension, and animal- and cell-based studies that confirm the linkage between altered gene function and the mechanistic pathway causing the hypertension. (iii) However, in our review of the published data, we became concerned that we may exclude some likely genes because data to support all of the criteria noted above were not available. Thus, we developed a restricted, but modified, set of criteria, and then ranked each gene selected on the strength of the available data. The following six inclusion criteria were applied:
English language publications
Primary hypertension
Hypertension as defined by the authors
For each candidate gene, at least two supporting cohorts from different publications or two different cohorts within a single publication or a single supporting cohort with a confirmatory genetically modified animal study
At least 600 individuals in the primary cohort
In some cases, use of data before January 2004, usually to put the current data into perspective
The following seven exclusion criteria were applied:
Results from meta-analyses or reviews
Secondary hypertension and monogenic hypertension
Hypertensive complications unless related to genes that met the primary inclusion criteria
Genes related to blood pressure but not hypertension per se
Genes where the number of supporting studies were less than twice the number of nonsupporting ones
Studies that did not perform a Bonferroni or similar multi-assessment correction to their statistics or that, when done, resulted in a nonsignificant P value
Only nonhuman studies
For some genes, the strength of evidence supporting a relationship to hypertension was minimal or poor, usually because the data available met only some but not all of our criteria. We have listed these genes but will not provide an assessment or references. For those genotype/phenotype groups where the strength of evidence was fair or greater (each one meeting all criteria), we have provided the following:
Phenotype characteristics
Genotype characteristics [in most cases, tagging single-nucleotide polymorphisms (SNPs)]
Number of supporting and nonsupporting studies
Characteristics of genetically modified animal models, if available
Pathophysiology linking the hypertension to the gene, if available
Therapeutic implications stemming from the genotype/phenotype association, if available
-
Strength of evidence:
◦ Very strong—six or more supporting studies; the number of nonsupporting studies was not >25% of the number of supporting studies; salt sensitivity of blood pressure was assessed in humans; and mechanistic human and/or animal studies were reported—that is, deep phenotyping or gene manipulation studies
◦ Strong—two or more supporting studies; the number of nonsupporting studies was not >35% of the number of supporting studies; salt sensitivity of blood pressure was assessed in humans; and mechanisms were suggested by human and/or animal studies
◦ Moderate—two or more supporting studies; the number of nonsupporting studies was not >35% of the number of supporting studies; and salt sensitivity of blood pressure was assessed in humans and/or animals
◦ Fair—one or more supporting studies; the number of nonsupporting studies was not >50% of the number of supporting studies; and no salt sensitivity of blood pressure or mechanistic studies were reported in humans or animals; when only one supporting study was reported, a confirmatory animal study was required
There was an extensive review of the genetics of hypertension published in 2005 where the information was obtained from online searches of the National Library of Medicine using the PubMed search engine from 1996 to November 2004 (2). This is the reason that this review consists of information published since then. Importantly, the inclusion criteria used in the previous review were not as stringent as those used in the current review. Where pertinent, the current review will include updated information on the 25 genes described in the previous review to provide an assessment of the long-term sustainability of genotype/phenotype associations in hypertension.
Figure 2.
Flow diagram of process used to select genes for assessment of their relationship with primary (essential) hypertension. See text for details.
Summary of Selected Genotypes/Phenotypes
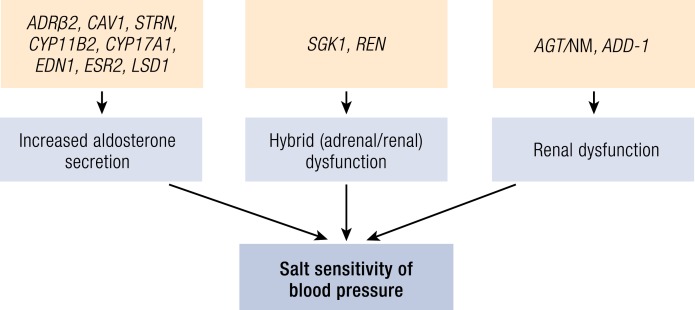
As stated above, we first review the 12 proximate, genotype/phenotype groups that met our criteria and were documented to have salt-sensitive, primary hypertension [normal-renin (4) and low-renin (8) proximate phenotypes] (Fig. 3). For each proximate phenotype, a figure has been included illustrating the potential mechanism. For two proximate phenotypes, where the evidence was the strongest, a specific figure is provided. For the other 10 proximate phenotypes, where the evidence was not as strong, a figure is provided illustrating three general mechanisms for each gene.
Figure 3.
Expansion of the categorization of the genotypes/phenotypes of primary (essential) hypertension. The primary (essential) hypertension population (distant phenotype) can be divided into two intermediate phenotypes (salt-resistant and salt-sensitive hypertension) based on their blood pressure response to changes in salt intake (liberal − restricted). Salt-sensitive hypertension can be divided into two subintermediate phenotypes based on their renin (PRA) response to upright posture and dietary salt restriction. Under each intermediate or subintermediate phenotype, the individual proximate phenotypes are listed by the code for the gene. The percentage, in parenthesis, indicates the fraction of the subentity for each of the next above primary entity; for example, 60% of the population with primary hypertension have salt-sensitive hypertension, 55% of the group with salt sensitivity have low-renin hypertension, and 5% of the group with salt sensitivity and low renin carry the risk allele for ADD-1. Asterisks indicate that a genetically altered animal model is available. NM, nonmodulation.
We then review two other groups: six genes associated with salt-sensitive blood pressure for which renin status was not reported, and three genes that met our criteria but for which data were not available to determine whether the gene was associated with salt-sensitive or salt-resistant hypertension. There were no gene/phenotype subgroups that met our criteria and were documented to have salt-resistant hypertension.
In each subsection, the genotype/phenotype groups are listed alphabetically. Finally, we list, but do not review, the 41 genes that did not meet all of our criteria. Each proximate genotype/phenotype group usually will be identified by the name of the gene but, in a few cases, by the name of the phenotype.
Salt-sensitive, intermediate phenotype primary hypertension
Salt-sensitive, intermediate phenotype primary hypertension has been the most commonly reported primary hypertension subset. Regardless of what method has been used to assess salt-sensitive hypertension, this intermediate phenotype comprises ∼50% to 60% of the primary hypertensive population, although its prevalence varies somewhat in different populations. Various mechanisms have been proposed to underlie salt-sensitive hypertension, but most involve renal dysfunction and/or dysfunction of an endocrine system, most commonly, the renin–angiotensin–aldosterone system (RAAS) (23–25). Because the RAAS is involved in a volume, negative feedback loop, it has been assumed that subjects with salt-sensitive hypertension will have a suppressed RAAS, usually identified by a low renin or plasma renin activity (PRA) level. However, a low PRA state is only associated with 25% to 30% of the primary population with hypertension. Therefore, an equally large salt-sensitive hypertension subgroup must have normal/high PRA levels. Thus, in this review, we divide the salt-sensitive hypertension intermediate phenotype group into two subintermediate phenotypes according to their renin-status: (i) normal/high renin and (ii) low renin.
Normal/high-renin, salt-sensitive, subintermediate phenotype primary hypertension
This group comprises individuals who have normal physiologic renin responses to sodium intake and upright posture. Their normal renin status in the presence of salt-sensitive hypertension suggests that these hypertensives have dysfunction not only in salt handling, but also in the normal RAAS physiologic response to inappropriate sodium retention. Approximately 45% of hypertensives with salt-sensitive blood pressure (SSBP) belong to this salt-sensitive, subintermediate phenotype hypertension group. Thus, ∼25% to 30% of primary hypertensives have normal/high-renin, salt-sensitive hypertension. To date, all but 10% to 15% of these individuals can be subgrouped into four proximate phenotype groups (Fig. 4).
Figure 4.
The hypertension subintermediate phenotype group with salt-sensitive blood pressure and normal renin status. All hypertensive subjects had substantial blood pressure responses to dietary salt intake but normal renin (PRA) responses to upright posture and dietary salt restriction. Asterisks indicate that a genetically altered animal model is available. NM, nonmodulation.
Caveolin-1 gene (CAV1).
Support for an association of polymorphic variants in CAV1 and hypertension has been moderate during the past dozen years. However, it has become increasingly evident that the association between variants in CAV1 and hypertension is most likely to occur in the context of the metabolic syndrome. Caveolins are a family of proteins that, as oligomers, associate with cholesterol and sphingolipids to form caveolae (26). Caveolae are specialized lipid rafts, located on the surface of nearly all cells. They are 50- to 100-nm hourglass invaginations that function as scaffolding proteins compartmentalizing and concentrating signaling molecules and their receptors and channels, thereby enhancing the efficiency of their interactions. Caveolae may also be involved in receptor-independent endocytosis. Importantly, caveolae are rapidly lost in cell lines. Their loss could contribute to the discrepancies in the time and dose response relationships often reported in studies using cell cultures vs those using acutely dispersed cells. In humans, there are three members of the caveolin family—caveolin-1 (CAV-1), caveolin-2, and caveolin-3. In vivo or acutely ex vivo, caveolin-3s are located on skeletal and cardiac muscle, whereas CAV-1s are located on all other cell types. Caveolin-2s are located on all cells and are usually physically associated with the other two caveolins. In cultured cell lines, these relationships have been reported to vary. CAV-1 has been the most extensively studied member of this family. It has been shown to interact with steroid, peptide, and adrenergic receptors. It also is known to bind to nitric oxide synthase, thereby inhibiting its enzymatic activity (26).
Phenotype characteristics: The hypertensive phenotype is driven as a component of the metabolic syndrome. In white and Hispanic hypertensive cohorts, there was an association between CAV-1 polymorphic variants and higher fasting insulin and homeostatic model assessment of insulin resistance levels, thereby linking hypertension and insulin resistance. However, there was an association between hypertension per se in Hispanics but not in whites (27). The hypertensive subjects carrying the CAV-1 risk allele had normal PRA levels. Hypertension alone also was found to be related to CAV-1 polymorphism in a Japanese cohort (28). PRA levels were not reported. In a hypertensive cohort, low high-density lipoprotein and metabolic syndrome were associated with a CAV-1 risk allele. Interestingly, although the association was supported in the entire population, it was largely driven by the nonobese subjects (29, 30). In in silico analyses, this risk allele was associated with decreased CAV-1 expression. Although no nonsupporting correlations between CAV-1 polymorphisms and hypertension have been reported, one study did report a supporting association between CAV-1 gene variants and hypertension associated with the metabolic syndrome but not in its absence (31). Thus, the clinical phenotype associated with the CAV-1 risk allele consists of hypertension in normal renin subjects who also have insulin resistance and the metabolic syndrome, but not obesity.
Genotype characteristics: Various SNPs of CAV1 have been studied regarding association with hypertension alone or in association with the metabolic syndrome. They include rs917664, rs3807989 (in complete linkage disequilibrium in some populations with rs917664), rs926198, and rs4730751 (27–31). In one study an insertion/deletion polymorphism was used (30).
Number of supporting and nonsupporting studies: There have been three supporting (27–30) and one nonsupporting (30) association studies between CAV1 and hypertension.
Availability and characteristics of genetically modified animal models: There have been extensive cardiovascular and metabolic studies in the CAV-1 knockout mouse. Disruption of the CAV-1/insulin receptor complex is associated with impairment of the insulin signaling pathway (32, 33). This disruption leads to insulin resistance, diabetes, increased triglyceride levels, and salt-sensitive hypertension (i.e., the metabolic syndrome). However, these mice are not fat, but are skinny, similar to the humans carrying the CAV-1 risk allele (32–35). The CAV-1 knockout mice also have dysregulated aldosterone secretion with increased endothelial nitric oxide synthase (eNOS) activity, presumably secondary to the absence of the inhibitory effect of CAV-1. Their hypertension likely is secondary to increased vasoconstrictor activity, assessed ex vivo, and the dysfunction in aldosterone secretion. Their hypertension is salt sensitive and normal renin. Both the hypertension and the vascular dysfunction are normalized by salt restriction or mineralocorticoid receptor (MR) blockade (35, 36). These mice also have histologic and molecular markers for cardiovascular and renal damage. It is postulated that the damage is secondary to pathologically increased nitric oxide activity resulting in increased production of reactive oxygen species.
Potential mechanisms linking hypertension to the gene: Based on the preclinical data, the association between decreased CAV-1 expression and the metabolic syndrome and hypertension, in part, is mediated by (i) insulin resistance, (ii) inappropriate aldosterone secretion, and (iii) enhanced vasoconstrictor activity (Fig. 5).
Therapeutic implications stemming from the genotype/phenotype association: Given the clinical and preclinical data, one would assume that the blood pressure in CAV-1 risk allele carriers (vs noncarriers) would be more responsive to insulin sensitizers (e.g., metformin), MR antagoinists (MRAs), and/or vasodilators. However, no clinical studies have been reported associating CAV-1 allele status and blood pressure response to treatment with these agents. Of importance, the CAV-1 risk allele is present in nearly 50% of whites, blacks, and Hispanics.
Strength of evidence: moderate
Figure 5.
Relationship of genotype/phenotype group to mechanism of hypertension. The genes are divided into three broad mechanistic categories—those associated with dysregulated aldosterone secretion, those primarily associated with renal or renovascular dysfunction, and those associated with both renal and adrenal dysfunction. NM, nonmodulation.
Nonmodulation (NM).
This subtype is one of the few that is identified by its proximate phenotype. It is also one of the earliest proximate phenotypes of primary hypertension identified (37, 38). Its characteristics have been confirmed around the world (39–43). Nonmodulation is a salt-sensitive hypertension phenotype (44) comprising 15% to 20% of hypertensives. Finally, it is one of the more complicated phenotypes to identify.
Phenotype characteristics: The term nonmodulation comes from the absence of a common physiologic trait documented in normal humans and animals. The level of salt intake changes the vascular and aldosterone responses to angiotensin II (ANGII) in a teleologically important way: when salt intake is reduced, the aldosterone response to ANGII is increased and the vascular response is reduced, whereas salt loading produces the opposite responses. This salt intake–mediated modulation of target tissues responses to ANGII is absent in nonmodulators. Thus, nonmodulators on a low-salt diet do not have the anticipated enhanced aldosterone response to ANGII (causing their normal renin status), and on a liberal salt diet the renovascular response to ANGII is not modified from the low-salt state, causing inappropriate renal vasoconstriction, sodium retention, and salt-sensitive hypertension. Thus, phenotypically, to distinguish nonmodulators from other individuals with salt-sensitive hypertension requires an assessment of aldosterone responses to ANGII on a low-salt diet or renal blood flow response to ANGII on a liberal salt diet. However, because antihypertensive medications need to be stopped, careful control of salt intake is required, and an infusion of ANGII must be given to identify nonmodulators clinically, which usually requires a clinical research unit. In such a facility and with the appropriate environmental controls, nonmodulators have the following phenotypic characteristics: blunted renovascular and aldosterone responses to Na+ intake and to AngII (45–49); a high degree of heritability (nearly 80% of nonmodulators have a family history of hypertension); increased circulating angiotensinogen (AGT) (49) levels; delayed Na+ excretion after salt loading; and insulin resistance (41, 50, 51). Importantly, in a clinical research center setting the defects underlying this subintermediate phenotype can be corrected by blocking the activity of the renin–angiotensin system (38, 52–54). Additional clinical characteristics associated with hypertensives that carry the AGT risk allele, but not necessarily associated with nonmodulation, include subarachnoid hemorrhage, renal cyst, coronary artery disease, and preeclampsia (55–58).
Genotype characteristics: The genetics of nonmodulation originally were identified by polymorphic variants in the AGT gene [the promoter A-6C (rs5051) and the coding 235T (4072C: rs699) SNPs] (5, 59). Several additional studies have associated these same AGT SNPs [and/or A-20C (rs5050)] with hypertension, but data regarding PRA status and salt-sensitive hypertension have not always been provided (60–65). To better understand the relationship between genetic variation of AGT and essential hypertension, two additional studies have been published. First, in white hypertensives, Kosachunhanun et al. (66) reported the influence of additional RAAS genes on aldosterone response to ANGII on a restricted salt intake. Not only was AGT (235T, rs699) associated with nonmodulators, but also this association was enriched when the subjects also carried risk alleles for both rs699 and angiotensin-converting enzyme (ACE: I/D) and even more so when hypertensives carried risk alleles for three RAAS genes: AGT plus ACE plus aldosterone synthase [cytochrome P450 family 11 subfamily B member 2 gene (CYP11B2): -344T, rs1799998] (66). However, alone neither variants in the ACE nor the CYP11B2 was associated with nonmodulation. Second, Watkins et al. (46) suggested that the genetic linkage of nonmodulators is not with a single AGT SNP, but with a haplotype. SNPs and AGT haplotypes were tested for association with plasma AGT levels, a phenotypic marker of nonmodulation (renal plasma flow), and primary hypertension (46). Associations were reported for alleles -1178G, 6066A, 6152A, 6233C, and 12822C in addition to previous associations for -1074T, -532T, -217A, -6A, and 235T. Most individually associated SNPs, including -6A and 235T, were found on a common complete AGT haplotype, H4 (frequency, 0.09). Individuals with haplotype H4 had significantly higher plasma AGT and reduced renal plasma flow (P < 0.003 and P < 0.0002, respectively), characteristics classical for nonmodulators. Other common haplotypes were not associated with characteristics of nonmodulators despite the presence of the rs5051 and rs699 risk alleles (-6A and 235T, respectively), suggesting that the AGT haplotype H4 is more predictive of nonmodulators than are the single SNPs -6A or 235T. Their findings may explain some of the discrepancies in clinical results using AGT SNPs to predict the response to therapy. Additionally, prior published data regarding AGT 235T and other SNPs assessed the association between this gene and primary hypertension without addressing the subjects’ renin status (67–71).
Number of supporting and nonsupporting studies: There were six supporting and one nonsupporting association studies between AGT and hypertension (65–71).
Availability and characteristics of genetically modified animal models: Deficiency of AGT in male mice results in substantial hypotension (72). Furthermore, two relevant preclinical studies have been reported where human AGT has been overexpressed. When the human AGT is overexpressed in the renal proximal tubule, salt-sensitive hypertension is produced. Transgenic mice with the human -6A haplotype have increased blood pressure compared with the human -6G haplotype (73, 74).
Potential mechanisms linking hypertension to the gene: The proposed mechanism leading to salt-sensitive hypertension in nonmodulators is the failure of the renal vascular to appropriately vasodilate on a liberal salt diet. Thus, sodium is retained, volume is expanded, and salt-sensitive hypertension develops. Although the response of aldosterone to salt restriction is also defective, this does not appear to contribute to salt-sensitive hypertension, but it does provide an explanation for the normal PRA (Fig. 6). [See Table 1 (37, 38, 41–49, 52–55, 66, 75–83) for nonmodulating phenotypic characteristics.]
Therapeutic implications: The AGT risk alleles associated with nonmodulators were assumed to be good biomarkers for individuals who preferentially would respond to ACE inhibitors. Risk vs nonrisk allele carriers of AGT-6A had a greater blood pressure response to atenolol in a Swedish population, to a thiazide diuretic in black women, and to an ACE inhibitor in a Chinese population. In an Indian population, risk vs nonrisk allele carriers of AGT 235T had a better blood pressure response to ACE inhibitors (54, 59, 68, 83). However, the results from other observational or post hoc analyses of hypertension clinical trials have been mixed (84–89), with one study suggesting that the AGT risk allele appeared to blunt the blood pressure response to an ACE inhibitor (58). The reasons for these discrepancies could be related to: (i) the reliability of observational/post hoc analyses; (ii) the uniqueness of AGT in mediating the nonmodulation phenotype; and/or (iii) the reliability of the genetic biomarker used as suggested by Watkins et al. (46). Furthermore, these results also raise a note of caution regarding the utility of data obtained from clinical trials where the subjects have not been randomized by genotype at the trial’s initiation.
Strength of evidence: very strong
Figure 6.
Pathophysiologic mechanism causing salt-sensitive hypertension in the AGT gene/NM subgroup.
Table 1.
Characteristics Associated with the Nonmodulating Phenotype
| • Decreased aldosterone response to ANGII when salt restricted (37, 42–48) |
| • Decreased renal plasma flow response to ANGII when salt loaded (37, 38, 44–48) |
| • Decreased renal plasma flow response to salt loading (44, 45) |
| • Decreased sodium excretion with acute and chronic salt loading (75, 76) |
| • Increased blood pressure response to chronic salt loading (75) |
| • Decreased PRA response to acute salt loading (77, 78) |
| • Correction of above conditions with ACE inhibitor administration (38, 52–55) |
| • Increased family history of coronary disease (41) |
| • Increased plasma and urine dopamine levels (79) |
| • Increased sodium–lithium countertransport levels (80) |
| • Associated with specific polymorphisms in AGT gene (45–49, 66) |
| • Increased PAI-1 levels (81) |
| • Insulin resistance and increased total, low-density lipoprotein cholesterol, and triglyceride levels (41, 82) |
| • Low frequency in premenopausal women (83) |
| • Increased plasma AGT (46) |
References are given in parentheses.
Renin gene (REN).
Renin is an enzyme primarily located and secreted from the juxtaglomerular apparatus of the kidney. Most of the circulating renin comes from this source. However, it is also synthesized and secreted in a paracrine and autocrine fashion from a variety of tissues, including, heart, fat, vasculature, and adrenal. Functionally its substrate is usually AGT to form the product angiotensin I (mostly inactive) that is rapidly converted into ANGII, with the active product of this cascade having several biologic effects, for example, vasoconstriction and aldosterone stimulation (90, 91).
Phenotype characteristics: Polymorphic variants in REN have been reported to be associated with SSBP (92). Furthermore, on a liberal salt diet the risk allele and a haplotype were associated with higher supine PRA and reduced blood pressure response to infused ANGII (92). Women who were postmenopausal with hypertension that carried the REN risk allele had significantly higher blood pressure than did noncarriers (93–95). PRA status and SSBP were not reported in these latter studies. However, a minimal association between REN and hypertension, as a state, also has been reported (96).
Genotype characteristics: Various REN SNPs have been used, including rs6682082, rs6693954, and rs5707 (92, 94–96). In one study an insertion/deletion polymorphism was used (93).
Number of supporting and nonsupporting studies: There have been four supporting (92, 94–96) and two nonsupporting (93, 97) association studies between REN and hypertension.
Availability and characteristics of genetically modified animal models: The ANGII-induced increase in blood pressure was attenuated in collecting duct-specific REN knockout mice (98). In a cell-based study, the REN risk allele promoter was associated with increased renin expression (94). These data suggest that rs6682082 is a functional variant. However, there have been no confirmations of this report.
Potential mechanism linking hypertension to the gene: Variance in REN expression could result in increased renin levels resulting in increased generation of ANGII, thereby increasing aldosterone secretion and vasoconstriction (specifically renal vasoconstriction), resulting in salt-sensitive hypertension (92). The presently available data support this hypothesis, as carriers of the REN risk allele do have reduced blood pressure response to infused ANGII, indicative of increased ANGII, at least at the level of the vasculature (98). However, increased ANGII and/or aldosterone levels have not been reported to be associated with REN risk allele status (Fig. 5).
Therapeutic implications stemming from the genotype/phenotype association: Given the clinical and preclinical data, one would assume that the blood pressure in carriers vs noncarriers of the REN risk allele would be more responsive to ACE inhibitors, angiotensin receptor blockers, or renin inhibitors. However, no studies have been reported associating REN allele status and blood pressure response to treatment.
Strength of evidence: moderate/fair
Striatin gene (STRN).
Striatin is a recently described protein initially reported to be involved in vesicular trafficking in neurons. It binds to CAV-1 and Ca2+ calmodulin, GαI, and phosphatase 2A and regulates eNOS and MAPK (99). It also has been documented that striatin mediates the rapid nongenomic effect of steroids, specifically the MR and estrogen receptor (ER)α (100–104). Striatin colocalizes with the MR and modulates its nongenomic activity in vascular endothelial cells, that is, it rapidly increases phosphorylation of ERK1/2 and AKT.
Phenotype characteristics: Studies assessing the association between polymorphisms in this gene and hypertension have been limited. Garza et al. (104) reported that there was a significant association of STRN polymorphisms and SSBP in a white population with hypertension. PRA levels were normal in carriers of the risk allele. A subsequent study documented SSBP in risk allele carriers in individuals of African descent, normotensives, and elderly subjects (105). Currently, there are no nonsupporting results regarding STRN polymorphism and hypertension.
Genotype characteristics: A haplotype analysis using STRN-tagging SNPs defined three haplotype blocks. The global block analysis was significantly associated with SSBP (Pglobal = 0.04). This association was entirely driven by one haplotype and specifically one SNP within that haplotype (rs2540923) (104, 105).
Number of supporting and nonsupporting studies: There have been two supporting (104, 105) and no nonsupporting association studies between STRN and hypertension.
Availability and characteristics of genetically modified animal models: SSBP was evaluated in heterozygote knockout mice (Strn+/−) (103, 106). Compared with wild-type mice, Strn+/− mice exhibited a significant increase in blood pressure when sodium intake was increased from restricted to liberal. Furthermore, serum aldosterone levels, renal expression of the MR and its genomic downstream targets serum/glucocorticoid-regulated kinase 1, and epithelial sodium channel were increased in Strn+/− vs wild-type mice on liberal sodium intake. In contrast, the pAkt/Akt ratio, a readout of the MR’s rapid, nongenomic pathway, was reduced. Furthermore, striatin deficiency was associated with enhanced vasoconstriction and decreased vascular relaxation, suggesting a critical role for striatin, through modulation of endothelial nitric oxide–cGMP, in the regulation of vascular function and blood pressure during changes in sodium intake. Finally, aldosterone, but not estradiol, increased striatin protein levels in endothelial cells (107).
Potential mechanisms linking hypertension to the gene: Both the carriers of the STRN risk allele and the Strn+/− mice have SSBP. From the studies in the Strn+/− mice at least two mechanisms may contribute to this SSBP. First, the increased aldosterone levels on a liberal salt intake would lead to increased sodium retention. Second, the decreased vasodilation, specifically in the renovasculature, on a liberal salt diet would increase sodium reabsorption. Both abnormalities could be secondary to a reduction in cyclic GMP (cGMP) levels on a liberal salt diet because cGMP inhibits aldosterone secretion and promotes vasodilation (Fig. 5).
Therapeutic implications stemming from the genotype/phenotype association: Given the clinical and preclinical data, one would assume that the blood pressure in carriers vs noncarriers of the STRN would be more responsive to MRAs or cGMP modulators. However, no studies have been reported that associate STRN allele status and blood pressure response to treatment with these agents.
Strength of evidence: moderate
Low-renin, salt-sensitive, subintermediate phenotype primary hypertension
The normal response of an individual to intravascular volume expansion is to suppress the RAAS. By this physiologic maneuver renal sodium absorption is reduced both in the proximal tubule (in part, by increased renal blood flow secondary to the reduced ANGII) and in the distal tubule/collecting duct (by the reduction in aldosterone secondary to the reduced ANGII). Thus, the low-renin subintermediate phenotype group comprises individuals who have had the anticipated physiologic renin response to SSBP. Approximately 55% of subjects with salt-sensitive hypertension are part of this subintermediate phenotype. Thus, ∼25% to 30% of all primary essential hypertensives have low-renin, salt-sensitive hypertension. To date, all but 10% to 15% of these individuals can be subgrouped into eight proximate phenotypes (Fig. 7).
Figure 7.
The hypertension subintermediate phenotype with salt-sensitive blood pressure and low-renin status. All hypertensive subjects had substantial blood pressure responses to dietary salt intake and low-renin (PRA) responses to upright posture and dietary salt restriction. Asterisks indicate that a genetically altered animal model is available.
Adducin-1 gene (ADD-1).
Polymorphic variants in ADD-1 was one of the earliest genetic factors associated with salt-sensitive primary hypertension. Support for it has remained strong for nearly the past two decades. Adducins are a family of cytoskeletal proteins first described by Bianchi and colleagues in the Milan hypertensive rat (108). Subsequently, Bianchi and colleagues (109) reported that polymorphic variants in ADD-1 are associated with salt-sensitive human hypertension. The adducin family consists of three proteins (α, β, and γ) that form heterodimers. The α and γ proteins are found in most cells whereas the β protein is expressed mainly in the brain and hematopoietic cells. Adducin binds to calmodulin and serves as a substrate for protein kinases A and C. Thus, in addition to the major role of adducins in maintaining the actin-based cytoskeleton, they are also involved in signal transduction, cell-to-cell contact information, and cell migration (110). Some studies suggest that α-adducin also interacts with α-Na/K ATPase and thereby the Na/K pump potentially in the kidney, heart, and brain (111, 112). Each adducin is produced by a different gene, although their structures are similar. For example, α-adducin is produced by ADD-1.
Phenotype characteristics: ADD-1 polymorphism is widely known as a candidate gene influencing blood pressure. In 1995, Casari et al. (113) first reported an association between ADD-1 polymorphism and hypertension. Two years later this same group reported that the association was with salt-sensitive hypertension (114). During the past 20 years, this group and others have expanded the description of this proximate hypertensive phenotype’s characteristics. ADD-1 polymorphism has been reported to be associated with low-renin hypertension in younger subjects (<60 years old) in Japan (115) and in whites in Europe and the United States (116, 117). These groups also have observed decreased intracellular erythrocyte sodium content and decreased sodium–lithium countertransport in hypertensives homozygous for the risk allele. Finally, a reduction in fractional excretion of sodium (the percentage of the sodium filtered by the kidney that is excreted in the urine) was observed in risk vs nonrisk allele carriers (116–118). Salt-sensitive hypertension without low PRA levels was reported in a Chinese population (119). Other phenotypic characteristics associated with carriers of the ADD-1 risk allele include impaired renal function, peripheral artery disease, coronary artery disease, increased blood pressure response to cold pressure test, and high low-density lipoprotein level (120–123). Finally, there also are several reports where no association with hypertension was found (124–128). However, in all nonsupporting studies, the characteristics of the populations analyzed were limited. With homozygosity in the minor allele being the driver of this association and its frequency being quite low, population characteristics, particularly of the control group, are of substantial importance.
Genotype characteristics: The most extensive studied ADD-1 SNP has been rs4961 (G460T). In general, because of the low frequency of the minor allele, allele carrier status has been used. However, where a genotype analysis was used, the strongest effect on blood pressure, particularly salt-sensitive hypertension, was associated with homozygosity of the minor allele. Individuals that fit this criterion comprise 2% to 3% of the hypertensive population or ∼5% of the low-renin subgroup. Haplotype assessment has been inconsistently reported. The combined effect of ADD-1 polymorphism and polymorphism in other genes that may be involved in salt intake–mediated blood pressure pathways has been reported. These included various combinations of the following: AGT, plasma membrane calcium-transporting ATPase 1 gene (ATP2B1), prostaglandin-endoperoxide synthase 2 (PTGS2), WNK1, and neural precursor cell–expressed developmentally downregulated gene 4-like (NEDD4L) (129). In each case the combination appeared to be additive. However, only a single publication supports each of these results.
Number of supporting and nonsupporting studies: There have been five supporting and two nonsupporting association studies between ADD-1 and hypertension (114, 116–118, 126–128).
Availability and characteristics of genetically modified animal models: The identification of this gene as a potential candidate for human hypertension originated from animal studies in the Milan hypertensive rat (108). In this rat, there is increased expression of α-Na/K ATPase (the Na/K pump) in the kidney, suggesting that the increased pump activity leads to salt-sensitive hypertension. The linkage to humans occurred when polymorphic variants in ADD-1 was associated with salt-sensitive hypertension in the Milan hypertensive rat vs normotensive littermates. A subsequent report identified that the G460T SNP in humans is associated with salt-sensitive hypertension (114). The group then performed a cross-over study between the Milan hypertensive and normotensive rats where they introgressed the α-, β-, and γ-adducin genes from one strain into the other. Their results strongly suggested that it was the α-adducin that confers the salt-sensitive hypertension phenotype (130).
Potential mechanism linking the hypertension to the gene: Given the salt-sensitive hypertension, the decreased renal fractional clearance of sodium, and the association between α-adducin and the Na/K pump, the most likely mechanism leading to SSBP is increased activity of the Na/K pump resulting in increased sodium reabsorption by the kidney, intravascular volume expansion, suppression of renin, and salt-sensitive hypertension (Fig. 8).
Therapeutic implications stemming from the genotype/phenotype association: Clinical studies suggest that greater blood pressure reductions with ramipril (likely by increasing renal blood flow) and hydrochlorothiazide occur in carriers vs noncarriers of the ADD-1 risk allele (131, 132).
Strength of evidence: strong.
Figure 8.
Pathophysiologic mechanism causing the salt-sensitive hypertension in the ADD-1 gene subgroup.
β 2-adrenergic receptor gene (ADRβ2).
Support for polymorphic variants in ADRβ2 associated with hypertension has been variable for almost the past two decades. The β2-adrenergic receptor is a member of the G protein–coupled receptor family. It is activated by epinephrine-type agonists that cause smooth muscle relaxation in the vasculature and bronchi and increased speed of contraction in skeletal and cardiac muscles. The receptor is a classical seven-loop one spanning the plasma membrane (133). Because of β2-adrenergic receptor’s effect on vascular smooth muscle, β2AR polymorphic variants and their association with hypertension have been extensively studied. However, the findings have been mixed. Relevant to hypertension, β2ARs are also located on the adrenal glomerulosa cell, and β2AR agonists can stimulate aldosterone secretion (134, 135).
Phenotype characteristics: β2AR has shown great promise as one of the genes affecting blood pressure via sympathetic nervous system–mediated effects on vascular tone and cardiac contractility. The gene has been widely investigated as a potential genetic factor associated with hypertension with inconsistent results (2). However, Pojoga et al. (25) used a different approach. Based on the studies by Svetkey et al. (136), they documented that the ADRβ2 locus was associated with salt-sensitive hypertension. This proximate phenotype not only had salt-sensitive hypertension, but also low PRA on a low-salt diet and increased aldosterone on a liberal salt diet (25). That aldosterone was the driver of this phenotype was supported by lower serum potassium on the liberal salt diet in carriers vs noncarriers of the risk diplotype (25). These findings were supported by a report of an association between the ADRβ2 locus and the blood pressure response to the Dietary Approaches to Stop Hypertension diet. Risk allele carriers vs noncarriers had a greater reduction in blood pressure and a reduced PRA level in response to the diet (137). Association with primary hypertension regardless of renin status has also been reported (138). Recently, Liu et al. (139) confirmed SSBP associated with the risk allele of this gene in a Chinese cohort. Changes in blood pressure associated with other phenotypes, for example, coronary artery disease, obesity (body mass index >30 kg/m2), and nocturnal nondipping of blood pressure, also have been described (138, 140–143). Nonsupporting association results have also been reported (144, 145).
Genotype characteristics: Although several ADRβ2 SNPs have been reported to be associated with hypertension, the most frequent ones have been G46A (rs1042713) and C79G (rs1042714). A haplotype has been reported between the homozygote for the minor allele of rs1042713 and the homozygote for the major allele of rs1042714. The haplotype identified the salt-sensitive hypertension group better than either SNP alone (25). One study reported that an interaction of ADRβ2 G46A and the 4a allele of NOS3 was associated with the risk of hypertension (146). However, no confirming studies were reported.
Number of supporting and nonsupporting studies: There have been five supporting and two nonsupporting association studies between ADRβ2 and hypertension (25, 136–139, 144, 145). However, all studies that assessed the relationship between genotype and SSBP were supporting.
Availability and characteristics of genetically modified animal models: No studies assessing blood pressure– or volume-mediated effects have been reported in genetically modified animals. However, several studies have documented that the β2AR is located on the glomerulosa cell and that activation and/or blockade will modulate aldosterone secretion (25, 134, 135).
Potential mechanism linking the hypertension to the gene: The salt-sensitive hypertension associated with variance at the ADRβ2 locus are likely secondary to an inappropriate level of aldosterone on a liberal salt diet (Fig. 5).
Therapeutic implications stemming from the genotype/phenotype association: The minor allele of Rs2053044 was reported to be associated with a better blood pressure response to ramipril (147). However, no confirmatory studies have been reported. No studies assessing the relationship of blood responses to MRAs have been reported.
Strength of evidence: moderate for hypertension; strong for salt-sensitive hypertension.
Cytochrome P450 family 11 subfamily B member 2 gene (CYP11B2).
CYP11B2 encodes aldosterone synthase, the last enzymatic step involved in aldosterone biosynthesis. The synthesis of this enzyme is regulated chronically by dietary sodium and potassium intakes. Decreased intake of sodium and increased intake of potassium result in increased aldosterone synthase levels and activity. The mechanisms responsible for the increased synthesis of the enzyme are unclear (148). Increased aldosterone production could lead to salt-sensitive hypertension. Alterations in aldosterone secretion could be secondary to variants of CYP11B2 (149, 150).
Phenotype characteristics: Rossi et al. (151) stated that the variants of CYP11B2 (-C344T, rs1799998) alleles were frequently found in those with low-renin hypertension. High plasma aldosterone concentration and a high aldosterone-to-renin ratio in hypertensives with CYP11B2 variants were reported in Indian and Chinese populations (152, 153). A report of CYP11B2 variants associated with hypertension without mentioning renin status was described in an Indian population (154). Salt-sensitive hypertension was demonstrated in a Japanese population regardless of renin status (150). In one study, salt-sensitive hypertension was associated with polymorphic variants in CYP11B2 but only in subjects who carried the risk alleles associated with hypertension for AGT and ACE (66). In addition to hypertension, polymorphic variants in this gene have been associated with characteristics often linked to excess aldosterone secretion: insulin resistance, metabolic syndrome, diabetes mellitus type II, ischemic stroke, left ventricular hypertrophy, and preeclampsia (155–159).
Genotype characteristics: The most frequently reported risk allele of CYP11B2 associated with hypertension was -C344T (rs1799998). Other variants reported in association with hypertension included rs4539 (62, 150–161). Finally, a recent report suggested that a rare variant rs542092383 also was associated with hypertension in a Chinese population (162)
Number of supporting and nonsupporting studies: Seven supporting studies and two nonsupporting studies have been reported (65, 149–153, 159, 160, 162).
Availability and characteristics of genetically modified animal models: CYP11B2-deficient mice have hypotension with a dependency on high salt intake to maintain a normal blood pressure (163, 164). Although deficiency is associated with poor pregnancy outcomes, it is not associated with preeclampsia (161). To date, no studies have been reported using an overexpressing rodent model.
Potential mechanism linking hypertension to the gene: One study reported that CYP11B2 risk allele carriers had higher aldosterone levels in response to salt intake that was not offset by lower renin levels. Therefore, inappropriate sodium retention occurred (151) (Fig. 5).
Therapeutic implications stemming from the genotype/phenotype association: One would assume the CYP11B2 risk allele carriers would be particularly responsive to MRAs. No specific clinical trial data have been reported, but in an observational study, risk allele carriers did have higher aldosterone levels, and both their blood pressure and aldosterone levels were more responsive to spironolactone (an MRA) (165).
Strength of evidence: strong/very strong.
Cytochrome P450 family 17 subfamily A member 1 gene (CYP17A1).
CYP17A1 codes for CYP17A1 an enzyme also known as 17α-hydroxylase and 17,20-lyase. Its 17α-hydroxylase activity is a major step in the production of steroids, specifically glucocorticoids by adding a hydroxyl group at carbon 17 of progesterone or pregnenolone. 17-OH progesterone then can be further converted to cortisol in a two-enzyme step process. By its lyase activity, both 17-OH pregnenolone and 17-OH progesterone can be further converted into androstenedione and dehydroepiandrostenedione with further conversions leading to testosterone and estradiol (166, 167). Substantial deficiency in CYP17A1 results in an infrequent form of congenital adrenal hyperplasia whose characteristics include deficiencies in cortisol and sex steroids and increases in mineralocorticoids, for example, 11-deoxycorticosterone and aldosterone, and hypertension.
Phenotype characteristics: Polymorphic variants in CYP17A1 (e.g., rs1458038) associated with hypertension were identified in one GWAS study (168) but not in another (169). Several additional studies have confirmed its association with hypertension (170, 171). In a Han Chinese population, the risk allele also was associated with decreased PRA and serum potassium levels (172), suggestive of increased mineralocorticoid effect, and SSBP. However, there were no published data in primary hypertensive patients where measurements of aldosterone, deoxycorticosterone, or sex steroids were provided.
Genotype characteristics: The following SNPs have been used in these reports: rs11191548, rs1004467, and rs11191416 (168, 170–174).
Number of supporting and nonsupporting studies: In this review, four supporting studies (168, 170–172), two nonsupporting studies in adults (169, 173), and one nonsupporting study in children (174) have been reported.
Availability and characteristics of genetically modified animal models: CYP17A1 is not required to make glucocorticoids in the mouse, but it is to make androgens and estrogens. Thus, genetically modified mice for this gene have been used to assess sex hormone effects but not mineralocorticoids or hypertension.
Potential mechanism linking hypertension to the gene: Based on the study cited above (172), it is likely that carriers of the CYP17A1 risk allele will have mineralocorticoid-dependent, salt-sensitive hypertension (Fig. 5).
Therapeutic implications stemming from the genotype/phenotype association: One would assume the CYP17A1 risk allele carriers would be particularly responsive to MRAs. However, there are no current trial data to support this hypothesis.
Strength of evidence: fair.
Endothelin-1 gene (EDN1).
Endothelin-1 protein encoded from EDN1, produced and released by vascular endothelial and smooth cells, is a potent vasoconstrictor (175). It also can stimulate aldosterone secretion and thus has many parallels to the renin–angiotensin system. Indeed, there are substantial interactions between the two systems (176). The secretion and mechanism of action of endothelin-1 have been reported to be involved in pulmonary vasculature, brain, ovary, and penile erectile functions. Dysregulation has been implicated in a variety of disease states, including cancers, lower urinary tract dysfunction, obesity, renal dysfunction, aging, preeclampsia, and several cardiovascular syndromes (177).
Phenotype characteristics: Subjects with high endothelin-1 levels have an increased risk of low-renin hypertension (178, 179). Polymorphic variants in EDN1 have been associated with low-renin hypertension and increased aldosterone/renin ratios in individuals of African descent, but not in whites (180). The association of variants in EDN1 with hypertension or blood pressure changes has been reported in individuals with other medical conditions, for example, rheumatoid arthritis and mild obesity (181, 182). EDN1 variants have been linked to preeclampsia in women living in India (183). An association of EDN1 and hypertension has been reported in a Chinese population (184, 185). Finally, variants in endothelin-converting enzyme-1 gene have been reported to be associated with hypertension in the Japanese population (186).
Genotype characteristics: Polymorphic variants of EDN1 have been extensively reported, with rs1800541 and rs5370 being the most frequent ones reported in association with hypertension (179–185).
Number of supporting and nonsupporting studies: Five supporting studies (178–180, 184, 185) and two nonsupporting studies have been published (183, 184)
Availability and characteristics of genetically modified animal models: Analogous to data in humans, animal studies demonstrated that rat models of SSBP had enhanced activity of endothelin-1 (187, 188). There are no studies of END1 total knockout, as this deletion is embryonically lethal. However, the endothelial-specific knockout is associated with low blood pressure (189). In our database search, there were no published studies involving EDN1 overexpression.
Potential mechanism linking the hypertension to the gene: Given the role of endothelin in the regulation of vascular tone and aldosterone secretion, the SSBP could be secondary to dysfunction in either the vasculature (particularly the renal blood flow) and/or the adrenal (aldosterone secretion) (Fig. 5).
Therapeutic implications stemming from the genotype/phenotype association: Tan et al. (180) suggested that individuals of African descent who carry the END1 risk allele may be particularly response to MRAs based on their increased aldosterone/renin ratio. However, there are no clinical trial data to support this hypothesis.
Strength of evidence: fair for hypertension in blacks.
Estrogen receptor β gene (ESR2).
Hypertension in young women is uncommon compared with men (young and old) and older women. Estrogen appears to protect most women against hypertension, with the incidence of hypertension increasing after menopause (estrogen deplete). Yet, genetic variations in the ER are associated with cardiovascular disease. Estrogen interacts with three receptors: ERα, ERβ, and G protein–coupled ER. ESR2 is the coding gene for ERβ. ERβ is predominantly expressed in the vasculature where the binding of estrogen usually results in vasodilatation (190, 191). Because some premenopausal women develop hypertension, estrogen may play a different role in these women.
Phenotype characteristics: Only a few studies have been reported on an association of ESR2 variants and hypertension, with controversial results. Two studies reported no association with blood pressure or the development of hypertension with polymorphic variants in ESR2 (191, 192). However, in a Chinese cohort, ESR2 variants contributed to hypertension, particularly in women with oral contraceptive use (193). A recent study in two cohorts provide support for the findings in the Chinese study (194). A candidate gene association study with ESR2 and SSBP was conducted in normotensive and hypertensive women (estrogen replete and estrogen deplete) and men. Multivariate analyses between variants of ESR2 and SSBP documented that risk allele carriers had a significantly supporting association with SSBP driven by estrogen-replete women in both cohorts with neither estrogen-deplete women or men having any genotype/phenotype association. Furthermore, these estrogen-replete risk allele carriers had increased aldosterone/renin ratios with lower PRA levels. Thus, inappropriately increased aldosterone levels on a liberal salt diet may mediate the SSBP. No associations with ESR1 were identified. A supporting association between ESR2 variants and hypertension regardless of sex has also been reported (28).
Genotype characteristics: Multiple variants of ESR2 linked to hypertension have been reported, including C1213T, rs4986938, rs1256044, rs10144225 and G1082A (28, 192–195).
Number of supporting and nonsupporting studies: There were three supporting studies with four cohorts (28, 192, 194) and two nonsupporting studies (192, 195).
Availability and characteristics of genetically modified animal models: No direct evidence from animal studies have been published. However, in rodents, activation of ESR2 can prevent the adverse cardiovascular effects of aldosterone (196, 197).
Potential mechanism linking hypertension to the gene: Manosroi et al. (194) documented that only in premenopausal women were ESR2 variants related to salt-sensitive hypertension and an elevated aldosterone/renin ratio on a liberal salt diet (Fig. 5).
Therapeutic implications stemming from the genotype/phenotype association: Manosroi et al. (194) proposed that the SSBP could be secondary to estrogen occupying an abnormal ERβ resulting in inappropriate aldosterone suppression. Thus, MR blockade may be a useful, precise way to treat these young women with hypertension.
Strength of evidence: fair for hypertension in women
“[LSD1] plays an important epigenetic role by regulating gene transcription via alteration in histone methylation.”
Lysine-specific demethylase 1 gene (LSD1 or KDM1A).
In 2004, Shi et al. (198) isolated the first histone demethylase, LSD1. It plays an important epigenetic role by regulating gene transcription via alteration in histone methylation (199). It acts specifically to demethylate two lysine sites on histone 3—K4 and K9. When it demethylates K4 this opens the histone structure and thereby promotes gene transcription. In contrast, histone structure is tightened when LSD1 acts on the K9 site. Thus, LSD1 can act as a coactivator or corepressor. Of interest, interaction with steroid receptors fosters LSD1 activation at the K9 site and thereby enhances its role as a corepressor. LSD1 is coded by the KDM1A gene.
Phenotype characteristics: Polymorphic variants in KDM1A (LSD1) are associated with low renin, SSHT in two populations—African descent and Hispanics—but not in whites (200). However, normotensive white risk allele carriers vs noncarriers of LSD1 do show a steeper rise in their age-associated increase in salt-mediated blood pressure (201). Also, decreased plasma aldosterone concentration and decreased renovascular response to salt loading were depicted only in blacks (200, 201).
Genotype characteristics: Two tagging SNPs have been identified to be associated with hypertension—rs587168 and rs671357 (200, 201). They are both intronic. No haplotype analyses have been reported. The minor allele frequency is 28% in blacks and 18% in whites. Thus, potentially nearly a quarter of black hypertensives may carry the LSD1 risk allele or most of this racial group’s low-renin hypertension subset.
Number of supporting and nonsupporting studies: There has been one supporting study with two different cohorts and no nonsupporting association studies between LSD1 and hypertension (200).
Availability and characteristics of genetically modified animal models: An LSD1 heterozygote knockout mouse has been developed. The total knockout is embryologically lethal. The LSD1 heterozygote knockout vs the wild-type mouse develops salt-sensitive hypertension at about 1 year of age with suppression of PRA, expanded intravascular volume on a liberal salt diet, and enhanced sodium excretion in response to a salt load. These characteristics are typical of what occurs in low-renin humans with hypertension (201, 202). Finally, ex vivo aortic vascular studies suggest that the LSD1 heterozygote knockout mice have enhanced vascular contraction and an altered nitric oxide–cGMP relaxation pathway in response to a high-salt diet (200). Importantly, all the animal studies were performed on male mice. Whether there is a similar response in female mice is unknown.
Potential mechanism linking hypertension to the gene:From the animal studies the defect in the vasculature could be the link to the salt-sensitive hypertension if the results observed in the aorta also occur in the renal vasculature. Normally when salt intake is increased, the renal vasculature dilates to increase flow and enhance sodium excretion. If this renal vascular response is impaired, salt-sensitive hypertension could occur (Fig. 5).
Therapeutic implications stemming from the genotype/phenotype association: Potentially, agents that can increased salt excretion would be more effective in the LSD1 risk allele carriers (e.g., diuretics, ACE inhibitors, or MRAs).
Strength of evidence: moderate.
Serum- and glucocorticoid-inducible kinase 1 gene (SGK1).
Serum- and glucocorticoid-inducible kinase 1 (SGK1) is an important regulator of epithelial Na+ channel (ENaC) activity. Thus, it is a proximate effector of aldosterone’s modulation of sodium reabsorption. SGK1’s expression is modified by mineralocorticoids, intravascular volume, glucocorticoids, and insulin (203–205).
Phenotype characteristics: Individuals with polymorphic variants in SGK1 are associated with SSBP (206–208). Furthermore, one study documented that SGK1 risk allele carriers with SSBP also had low PRA levels on a low-salt diet (206). Finally, one study suggested that polymorphic variants of SGK1 were associated with the development of hypertension during a 7.2-year follow-up (207).
Genotype characteristics: The following SGK1 SNPs were associated with hypertension: rs1763498 and rs114414980 (207). Associated with SSBP were rs2758151, rs9402571, rs9389154, rs1763509, and rs9376026 (206, 208) and to low renin levels rs2758151 and rs9402571 (206). Of interest, in some studies the risk allele associated with SSBP was present in close to 50% of the study cohort (206).
Number of supporting and nonsupporting studies: There have been three supporting and no nonsupporting association studies between the SGK1 and hypertension (206–208).
Availability and characteristics of genetically modified animal models: Mice lacking the SGK1 gene are unable to appropriately increase the expression and activity of ENaC, leading to impaired sodium reabsorption and mild hypotension on a sodium-restricted diet and resulting in sodium dependency to maintain blood pressure (209). No data have been reported using an SGK1-overexpressing rodent.
Potential mechanism linking hypertension to the gene: Given SGK1’s key role in modulating ENaC activity and sodium resorption, it is likely that overexpression of SGK1 would result in increased sodium retention and salt-sensitive, low-renin hypertension. However, data to support this hypothesis are limited (Fig. 5).
Therapeutic implications stemming from the genotype/phenotype association: Blockade of SGK1 could provide precise therapy for hypertensives who are SGK1 risk allele carriers. Such individuals may also be more sensitive to MRAs. However, no clinical trial data to support this hypothesis have been reported.
Strength of evidence: moderate.
Undefined renin, salt-sensitive, subintermediate phenotype primary hypertension
This group contains variants of genes associated with salt-sensitive hypertension where data are lacking concerning the renin status of the subjects. Thus, in several respects the phenotypes associated with these genes are less well characterized compared with those in subintermediate phenotypes 1.1 and 1.2 (Fig. 9).
Figure 9.
Groups with hypertension, salt-sensitive blood pressure intermediate phenotypes (without renin status). All subjects with hypertension had substantial blood pressure responses to dietary salt intake, but renin status was not provided. Asterisks indicate that a genetically altered animal model is available.
Angiotensin-converting enzyme gene (ACE).
ACE encodes an enzyme that converts angiotensin I to ANGII. It is one of the most studied genes related to hypertension because ANGII is a potent vasoconstrictor, particularly on the renal vasculature, and aldosterone secretagogue. Thus, the activity of ACE and the regulation of its expression have been substantially investigated in cardiovascular diseases (210). Additionally, variants in the ACE gene have been associated with cancer, sarcoidosis, and autoimmune diseases (211). Furthermore, antagonists of this enzyme have been extensively used to treat cardiovascular and renal diseases (212, 213). Of interest, ACE not only activates a potent vasoconstrictor, it also inactivates a potent vasodilator—bradykinin (214).
Phenotype characteristics: Most of the available data support an association between ACE polymorphism and hypertension or SSBP (67, 215, 216). However, in some cases the supporting data have not been with ACE alone but in combination with polymorphisms in other genes in the RAAS or related pathways (66, 217). For example, an association with the metabolic syndrome and/or insulin resistance has been documented in some studies, for example, with polymorphic variants of CAV1 (217). Finally, some studies have supported a relationship between ACE polymorphism and pregnancy-induced hypertension/mild preeclampsia or type 2 diabetes mellitus (218–220).
Genotype characteristics: Based on its involvement in RAAS, this gene has been one of the most substantially investigated for association with hypertension (221). Most studies have used the insertion/deletion polymorphism in intron 16.
Number of supporting and nonsupporting studies: Association of variants in this gene and hypertension was documented in four studies (67, 215–217). One study did not support this association (161).
Availability and characteristics of genetically modified animal models: He et al. (221) reported that compared with the wild-type rat, the ACE-silenced rat had a significantly reduced systolic blood pressure.
Potential mechanism linking the hypertension to the gene: ACE is a pivotal factor regulating vasoconstrictor and hormonal-mediated, volume-regulating factors. Kaplan et al. (67) have provided evidence documenting that the SSBP associated with ACE variants is secondary to incomplete suppression of the RAAS on a liberal salt intake. However, because of inconsistencies in the human studies, it is unclear how critical ACE variants are in mediating most of the pathophysiologic characteristics associated with cardiovascular and renal diseases.
Therapeutic implications stemming from the genotype/phenotype association: ACE polymorphism has been associated with greater blood pressure response to treatment with the ACE inhibitors enalapril and lisinopil (222).
Strength of evidence: fair.
Bradykinin receptor B2 gene (BDKRB2).
BDKRB2 encodes bradykinin receptor B2 protein, a G protein–coupled receptor involving in the kallikrein–kinin system (KKS). This receptor binds to bradykinin, which acts as a strong diuretic and potent vasodilator via promoting nitric oxide synthesis (223, 224).
Phenotype characteristics: There have been few studies assessing BDKRB2 polymorphisms in hypertensive cohorts. One study reported that the association was with salt-sensitive hypertension in Asians of both sexes (225). A second study reported an increase in the prevalence of the BDKRB2 risk allele in hypertensive blacks, but it did not assess SSBP (226). Another reported an association between the risk allele and Indian hypertensives that was largely driven by males (227). No additional phenotypic characteristics were reported in these studies.
Genotype characteristics: The following variants have been used in these studies: rs11847625, rs334, and an insertion/deletion in exon 1 (225–228). Of note, the frequency of the risk allele in blacks was much higher than in whites.
Number of supporting and nonsupporting studies: There were three supporting (225–227) and one nonsupporting (228) studies.
Availability and characteristics of genetically modified animal models: In a BDKRB2 knockout mouse, profound ANGII-induced hypertension occurred compared with wild-type littermates (229).
Potential mechanism linking hypertension to the gene: The presumed mechanism responsible for the hypertension is a loss of function of the diuretic/vasodilator properties associated with activation of this receptor. However, no specific studies have been performed to test this hypothesis.
Therapeutic implications stemming from the genotype/phenotype association: None reported to date.
Strength of evidence: fair.
Electrogenic sodium bicarbonate cotransporter 4 gene (SLC4A5).
SLC4A5 encodes Na+-HCO3− cotransporter expressed in the distal nephron. This transporter is involved in intracellular pH regulation and mediates Na+-HCO3− influx (230, 231). Recent evidence indicates that SLC4A5, which encodes NBCe2, is expressed and can act in the proximal tubule to modify sodium and bicarbonate transport (232)
Phenotype characteristics: Two studies and three cohorts have documented an association between polymorphic variants in SLC4A5 and hypertension (232, 233). One of the cohorts was black the other two were white. In the white cohorts, the association was with SSBP. In one cohort, gene variants of NBCe2 increased sodium and bicarbonate transport in human proximal tubule cells (232). No other phenotypic characteristics were provided in these studies.
Genotype characteristics: Two SNPs have been reported to date: rs7571842 and rs10177833 (232, 233). These two SNPs are in linkage disequilibrium.
Number of supporting and nonsupporting studies: There have been two supporting studies and three supporting cohorts reported (232, 233). No nonsupporting studies have been reported to date.
Availability and characteristics of genetically modified animal models: SLC4A5 acid-loaded knockout mice were linked to sodium retention and hypertension (234).
Potential mechanism linking hypertension to the gene: A loss-of-function mutation in SLC4A5 could reduce the synthesis of the sodium bicarbonate cotransporter, thereby increasing sodium retention, SSBP, and hypertension (234).
Therapeutic implications stemming from the genotype/phenotype association: None have been reported.
Strength of evidence: moderate.
Plasma membrane calcium-transporting ATPase 1 gene (ATP2B1).
ATP2B1 encodes plasma membrane calcium ATPase isoform 1, an enzyme that removes bivalent calcium from intracellular stores against a very high concentration gradient. Therefore, this enzyme plays an important role in calcium homeostasis (235).
Phenotype characteristics: Hypertension associated with variants of ATP2B1 has been documented in two large-scale GWASs (169, 170) and five cohort studies (174, 235–238). These studies also provided three additional phenotypic characteristics. (i) The hypertension phenotype was particular strong in females (237). (ii) A longitudinal Korean cohort study suggested that an increased sodium intake increases the risk of developing hypertension in risk allele carriers vs noncarriers (236). (iii) The risk allele is associated with hypertension in Chinese children (174).
Genotype characteristics: rs2681472 was the most commonly documented SNP of ATP2B1 associated with hypertension, with rs17249754, rs2621472, and rs2070759 also being used (168, 169, 174, 236–239).
Number of supporting and nonsupporting studies: Seven supporting (168–170, 174, 236–239) and no nonsupporting studies have been reported to date.
Availability and characteristics of genetically modified animal models: Silencing the ATP2B1 gene using siRNA increased blood pressure and vasoconstriction (240). Also, an ATP2B1 knockout mouse had substantially higher blood pressure than did wild-type littermates (241).
Potential mechanism linking hypertension to the gene: One study based on an animal model proposed that ATP2B1 may play a crucial role in blood pressure control by altering calcium handling in vascular smooth muscle cells and thereby vascular tone (242).
Therapeutic implications stemming from the genotype/phenotype association: None reported.
Strength of evidence: fair for SSBP; strong for hypertension.
Serine/threonine 39 gene (STK39).
STK39 encodes a serine/threonine kinase and is also known as a thiazide response gene. It has been shown to interact with WNK kinase to regulate the Na/Cl cotransporter. Thus, this kinase acts as a mediator of renal sodium and chloride reabsorption as well as a controller of salt transport in the regulation of osmotic cell volume (243–245).
Phenotype characteristics: A GWAS study reported a strong association of STK39’s common variants and hypertension in Amish subjects (243). A single study reported an association between STK39 polymorphisms and SSBP (246). All other studies were linked with hypertension per se (247–250). None of these studies commented on the renin status of the subjects. Finally, in three populations there was no association between hypertension and STK39 genotype, that is, Chinese children, Korean adults, and Chinese adults (174, 251, 252).
Genotype characteristics: rs3754777 is the most frequently reported SNP of STK39 in relationship to hypertension. However, other SNPs of STK39 also have been association with hypertension, for example, rs35929607, rs35929607, and rs6749447 (174, 242, 245–252).
Number of supporting and nonsupporting studies: Five supporting studies (246–250) and three nonsupporting studies (174, 251, 252) have been reported.
Availability and characteristics of genetically modified animal models: None.
Potential mechanism linking hypertension to the gene: Wang et al. (243) proposed that in individuals who carry the STK39 risk allele, a gain in function occurs. If so, in the renal tubule STK39 expression would increase, consequently reducing renal sodium excretion and thereby resulting in hypertension.
Therapeutic implications stemming from the genotype/phenotype association: Absence of a selective blood pressure response to thiazide diuretics (253) brings into question the clinical relevance of Wang et al.’s (242) hypothesis. However, intriguingly, hypertensive male carriers of the STK39 risk allele had a substantial blood pressure response to the angiotensin receptor blocker losartan (254).
Strength of evidence: fair.
WNK lysine-deficient protein kinase 1 gene (WNK1).
WNK1 encodes cytoplasmic serine-threonine kinase in the distal nephron. This kinase activates SGK1, resulting in the activation of ENaC and sodium retention (255). WNK1 mutation is known to be associated with the rare monogenic hypertension disease, Gordon hyperkalemia-hypertension syndrome (pseudohypoaldosteronism type II) (256).
Phenotype characteristics: WNK1 variants have been associated with hypertension in two studies (152, 247). Neither study reported any other phenotypic features (e.g., SSBP or hormone levels), although one suggested that positive findings varied with the population studied. WNK1 variants also were associated with the risk of developing hypertension with bevacizumab treatment (257). Bevacizumab, a monoclonal antibody to vascular endothelial growth factor, is used to treat gynecologic cancers. As many as a third of subjects treated with bevacizumab develop substantial hypertension.
Genotype characteristics: Four SNPs have been reported in these studies: rs1468324, rs3168640, rs11885, and rs11554421 (152, 247, 255, 257).
Number of supporting and nonsupporting studies: Two supporting (152, 247) and one nonsupporting (258) studies have been reported.
Availability and characteristics of genetically modified animal models: In WNK1 heterozygous knockout mice, a significant decreased in blood pressure was observed (259).
Potential mechanism linking hypertension to the gene: It is assumed that variation in WNK1 levels or activity will modify the individual’s ability to appropriately excrete sodium. Thus, WNK1 deficiency likely will be associated with SSBP.
Therapeutic implications stemming from the genotype/phenotype association: Different responses to a thiazide diuretic were documented to be related to WNK1 variants in hypertensive subjects (260). Two to four percent of the variation in blood pressure response to the diuretic could be attributable to the presence of a WNK1 risk allele. Finally, the risk of developing hypertension with bevacizumab is increase sixfold in carriers of the WNK1 risk allele.
Strength of evidence: fair.
Salt-resistant, intermediate phenotype hypertension
This intermediate phenotype includes individuals with no or minimal changes in blood pressure when salt intake is modified. Approximately 40% of hypertensives worldwide belong to this group. There are substantial racial and geographic differences in the number of subjects who have salt-resistant hypertension. There were no proximate phenotypes identified within this group that met our criteria for inclusion in this review (Fig. 3).
Undefined hypertension phenotype
This group comprises three genes whose phenotype was not specifically associated with either salt-sensitive or salt-resistant hypertension. It is likely that additional studies may further define the phenotypic characteristics associated with these genes (Fig. 10).
Figure 10.
Groups with hypertension with undefined salt-sensitive blood pressure and renin status.
Angiotensin receptor type I gene (AGTR1).
AGTR1 encodes angiotensin receptor type 1 (AT1R), a cell surface receptor. ANGII and some of its analogs bind to this receptor. This interaction triggers a cascade of events in targeted cells, resulting in, for example, vasoconstriction, increased aldosterone secretion, suppression of renin, modulation of renal sodium resorption, increased vasopressin secretion, altered cardiac function, and changes in immune function (261, 262). Given AT1R’s mechanism of action, one would anticipate that it would be associated with hypertension. However, support for this hypothesis has been mixed.
Phenotype characteristics: Polymorphic variants of AGTR1 were associated with hypertension in subjects from India and in blacks, but not in Latinos. In one study, circulating levels of the AT1R were greater in hypertensives than normal, but there were no differences in their levels by genotype. One study in a white cohort, using a haplotype approach, reported a modest relationship between polymorphic variants in the gene and hypertension. No study assessed SSBP or provided information on other potentially important factors (e.g., hormone levels, renal function) (263–265). Two nonsupporting studies have also been reported (266, 267).
Genotype characteristics: Most studies used the rs5186 SNP, although rs5535 also has been used (263–267).
Number of supporting and nonsupporting studies: Three supporting (264–266) and two nonsupporting (266, 267) studies have been reported.
Availability and characteristics of genetically modified animal models: A haplotype of AGTR1 in humans when inserted into a mouse’s genome causes an increase in blood pressured and an increase in AT1R mRNA levels in heart and kidney (268).
Potential mechanism linking hypertension to the gene: The most common mechanistic hypothesis is a gain of function of the AGTR1 gene, resulting in increased AT1R levels with consequent increased vasoconstriction and hypertension. There is less evidence for increased aldosterone production, particularly chronically (262).
Therapeutic implications stemming from the genotype/phenotype association: Given the gain-of-function mechanistic hypothesis, one would anticipate that subjects who carry the risk allele for hypertension would have greater reductions in blood pressure when given an angiotensin receptor blocker. Two studies, one in China and one in Sweden, did report this effect (269, 270).
Strength of evidence: fair/poor.
Fibroblast growth factor 5 gene (FGF5).
FGF5 encodes a protein (FGF5) that is a member of the fibroblast growth factor family. FGF5 possesses cell survival and mitogenic activities and is involved in multiple human biological processes, for example, cell growth, morphogenesis, tumor growth and invasion, and tissue repair (271). It is an oncogene, and therefore its mechanism of action has been intensively investigated in oncology. However, FGF5 may also be involved in a variety of other cellular processes, including inflammation. For example, FGF5 knockout mice, fed a high-fat diet, gained weight, had increased liver enzymes, and showed histologic evidence of marked inflammation that was similar to nonalcoholic steatohepatitis (272).
Phenotype characteristics: One large GWAS reported an association between FGF5 and hypertension (168). Additionally, three case control studies have shown this association. (174, 46, 273–275). One study suggested that FGF5 variants were associated with SSBP (246). This finding was not confirmed in another study (139). Another study reported that an increased body mass index increased the blood pressure difference between risk allele carriers and noncarriers (275).
Genotype characteristics: The most common SNPs used were rs16998073 and rs1458038 (139, 174, 247, 274–276).
Number of supporting and nonsupporting studies: Five supporting (168, 174, 246, 274–275) and one nonsupporting (276) studies are reported herein.
Genetically modified animal models: None reported.
Potential mechanism linking hypertension to the gene: No specific mechanism has been suggested.
Therapeutic implications stemming from the genotype/phenotype association: None reported.
Strength of evidence: fair.
G protein β3 subunit gene (GNB3).
GNB3 encodes the G protein β3 subunit that is a component of heterotrimeric G protein complexes. These complexes transduce signals from G protein–coupled receptors to intracellular effectors, thereby facilitating diverse physiological processes, including cardiovascular and/or metabolic functions (277, 278). Animal studies suggest that altered production of GNB3 could result in increased signal transduction, cell proliferation, and enhanced vascular reactivity. Association of this gene with hypertension is mixed.
Phenotype characteristics: Besides hypertension, other distinguishing characteristics included increased aldosterone levels associated with increased serum sodium, potassium, and creatinine levels; hyperreactivity to a cold pressor test; obesity; and, specifically, with hypertension in women who are postmenopausal (121, 279–281). In the study that reported higher aldosterone levels, it is unclear whether the increased levels were primary or secondary given the increased potassium and creatinine levels (280). There was a significant, twofold greater risk of cardiovascular events in a 7-year follow-up study in hypertensive Chinese subjects homozygous for the GNB3 risk allele vs nonrisk allele. Two studies did not support an association between GNB3 and hypertension.
Genotype characteristics: The following SNPs have been used: rs4963516, rs5441, rs5443, rs5446, and rs1129649 (121, 279–283).
Number of supporting and nonsupporting studies: Four supporting (121, 279–281) and two nonsupporting (282, 283) studies have been published.
Availability and characteristics of genetically modified animal models: No genetically altered animal model studies were reported.
Potential mechanism linking hypertension to the gene: No consistent mechanistic hypothesis has been proposed.
Therapeutic implications stemming from the genotype/phenotype association: A polymorphic variant in rs5443 was linked to hypertensive responders to diuretics (284).
Strength of evidence: fair.
Genes with insufficient evidence for association with hypertension phenotype
The following 41 genes had some evidence for association with hypertension but did not meet all our inclusion/exclusion criteria: ADD2 [adducin 2 (β)], ADRA1A (α adrenergic receptor), ADRB3 [β3 adrenergic receptor (β3 adrenoreceptor)], ANP (atrial natriuretic peptide), APOC3 (apoliprotein C III), CACNB2 (voltage-dependent L-type calcium channel subunit β2), CLCNKA (chloride voltage-gated channel Ka), CSK (C-terminal Src kinase), CYBA (cytochrome B-245 α chain), DRD1 (dopamine receptor D1), DRD2 (dopamine receptor D2), ECE1 (endothelin converting enzyme 1), EDNRA (endothelin receptor type A), EDNRB (endothelin receptor type B), ELN (elastin), eNOS (NOS3), ESR1 (ER1), GYS1 (glycogen synthase 1), HSD11B2 (11β-hydroxysteroid dehydrogenase type 2), INSR (insulin receptor), JAG1 (Jagged 1), KCNJ1 (potassium voltage-gated channel subfamily J member 1), KLKB1 (kallikrein B1), LPL (lipoprotein lipase), MOV10 (putative helicase), MTHFR (methylene tetrahydrofolate reductase), NPR1 (matriuretic peptide receptor A), NPR2 (natriuretic peptide receptor B), NEDD4L (neutral precursor cell expressed, developmentally downregulated 4-like), NOS2A (nitric oxide synthase 2A), NR3C2 (nuclear receptor subfamily 3 group C member 2), PLEKHA7 (pleckstrin homology domain containing A7), PRKG1 (cGMP-dependent protein kinase 1), PRRC2A (proline-rich coiled-coil 2A), SAH (S-adenosyl-l-homocysteine hydrolase), SCNN1A (sodium channel epithelial 1 α subunit), SCNN1G (sodium channel epithelial 1 γ subunit), SELE (selectin E), SH2B3 (SH2B adaptor protein 3), UMOD (uromodulin), WNK4 (WNK lysine-deficient protein kinase 4).
Discussion
During this century, the use of genetic techniques to uncover the mechanisms underlying hypertension has increased dramatically. In a 2005 review, polymorphic variants in 25 genes were identified as being associated with essential (primary) hypertension (2). Using similar criteria as used in the 2005 review, an additional 37 genes were identified in the literature published between 2004 and 2017. Thus, using PubMed data, as of 31 December 2017, 62 genes were associated with primary hypertension. However, only about a third of these genes (21) met the stricter criteria used for this review. Of note, only 9 of the 25 genotype/phenotype associations reported in the previous review are among the 21 genes reported herein. Several factors likely contribute to both the increase in the number of genes identified and the substantial dropout rate. First, the publication of GWASs since the previous report identified several loci associated with hypertension. Second, none of the loci identified in the GWAS reports covered areas where genes reported in the 2005 review are located. Third, there was a substantial increase in the number of publications designed to support or refute the findings from the GWASs. Many of these studies were negative. Fourth, to be included in the list of genes associated with hypertension, the current review required published results from at least two supporting cohorts (beyond a finding in a GWAS), and nonsupporting studies could not exceed supporting ones.
“…62 genes were associated with primary hypertension.…Only about a third of these genes (21) met the stricter criteria used for this review.”
The two GWAS reports were published in the same issue of Nature Genetics in 2009. Their results substantially accelerated the number of genes potentially associated with hypertension. Loci potentially covering 20 genes were identified. Interestingly, only one gene was identified in both GWASs. Of the 20 genes, five met the criteria used in the 2005 review (2), but only three of these five also met the stricter criteria used in this review (CYP17A1, FGF5, and ATP2B1). Thus, 8 years after publication of these pivotal GWASs, only 15% of the potential genes are included in the present review. The frequent failure of traditional candidate gene approaches to support GWAS findings is not surprising for several reasons. First, GWASs are sophisticated observational studies. Therefore, they are useful for nominating candidate genes, but they typically are unable to establish disease causality. In part, these two GWASs affirm this conclusion because only one of the genes identified in one GWAS was found in the other despite apparently similar populations, inclusion criteria, and statistical approaches. Furthermore, although new genetic loci potentially can be identified by GWASs, these loci often contain multiple candidate genes, with some, but not all, contributing to the susceptibility to a disease. Second, GWAS may not be able to identify a causative gene that is in linkage disequilibrium with some component of the loci identified by GWASs but not the actual gene. Thus, similar to microarrays, additional studies specifically designed to test the validity of a GWAS proposed candidate gene are required. Third, 8 years may be insufficient time to develop cohorts with the appropriate phenotypes to test the validity of the genetic hypotheses generated from the GWASs.
Of interest, there were no reported association studies using the more refined techniques of exome sequencing or whole-genome sequencing. These approaches are designed to provide a more precise structural view of an individual’s genome. However, it is unclear whether, by themselves, these newer genetic analytical techniques will provide a clearer pathway to personalized, precision medicine envisioned at the beginning of the genetics revolution 25 to 30 years ago. For most complex, chronic conditions such as diabetes, asthma, heart failure, and particularly hypertension, more detailed phenotyping data will be required.
In addition to the benefits of more personalized, precision medicine that genetics-based studies will provide, they also are likely to reduce overall health care costs. For the patient, these costs reductions will fall into three general areas. First, rather than using a population treatment focus with a multistep “see what happens” approach, a limited number of targeted steps will be used. Second, because of increased compliance and specific mechanism targeting, a reduction in organ damage secondary to more consistent control of blood pressure will occur. Third, with a treatment strategy based on targeting specific mechanisms, there will be a reduction in off-target side effects with their associated costs. The pharmaceutical industry will also experience cost savings. First, drug development costs will be reduced because a more responsive, genetically identified, clinical trial cohort can be used, thereby reducing the size and costs of randomized clinical trials. Second, knowing the mechanisms to target will reduce the preclinical development costs. Finally, both factors will reduce the time required to bring an agent to market, resulting in increased patent-protected marketing time.
What were the characteristics shared by the 21 genes in the proximate phenotype group beyond fulfilling the initial selection criteria? First, in all but three genes, deeper phenotyping studies, beyond hypertension, had been performed. Indeed, several of these 21 proximate phenotypes did not associate with hypertension per se, but only with an intermediate phenotype. Importantly, the phenotype/genotype associations in all nine genes from the 2005 review that also are included in this review had their associations supported by deep phenotyping data. For the other 16 genes previously reported, there were few additional association studies reported in the past dozen years and most of those reported were nonsupporting. Second, 18 of the 21 genes support the premise that polymorphic variants in a gene alone were insufficient to produce a level of blood pressure high enough to be called hypertension. Gene variants and an appropriate environment (usually liberal salt intake) were required. These 18 genes were associated with a proximate phenotype that included SSBP and, therefore, salt-sensitive hypertension. In the other three, salt sensitivity was not assessed. However, only a few of the studies documented SSBP in people who are normotensive, which would be anticipated in a gene linked to SSBP in people with hypertension.
No genotype/phenotype groups were associated with salt-resistant hypertension unless it was present in one or more of the three genetic groups where salt sensitivity was not tested. There were no published data assessing SSBP in any of the 41 genes that did not make the final list. Given that in general only ∼60% of people with hypertension have salt-sensitive blood pressure, these findings are puzzling. They suggest that (i) our estimate of salt-sensitive hypertension is too low, (ii) assessing salt-sensitive hypertension is easier to do than assessing salt-resistant hypertension, and/or (iii) salt-resistant hypertension does not have a genetic component. Third, 15 of the 21 genes had animal- and/or cell-based studies to support the mechanisms by which gene modification could lead to hypertension. All but one of these involved genes associated with salt-sensitive hypertension. Only occasionally did the 41 genes that we did not extensively review have animal- or cell-based studies. Fourth, volume-related biomarkers were used in most of the 21 proximate phenotype groups. For example, (i) renin status, assessed using controlled salt intake and posture protocols, was determined in studies associated with 12 of the 21 genes. For all but 3 of these 12 genes, animal- and/or cell-based studies also were performed. For one of these three, CYP17A1, the gene does not exist in rodents. Renin status was not assessed in any of the 41 genes not on the final list. (ii) Aldosterone levels in serum and/or urine were measured in 8 out of 12 of the renin-classified phenotype/genotype groups. All but one also had animal studies to support the mechanism of action resulting in hypertension. There were several other isolated deep phenotyping characteristics in a few of the 18 genotype/phenotype salt-sensitive hypertensive groups.
Previously identified secondary forms of hypertension have been associated with a change in structure either of an organ or the coding region of a gene. Intriguingly, both the genetic and the deep phenotyping data suggest that these new genetically identified secondary forms of hypertension are most likely associated with a change in a gene’s expression rather than a change in its structure. How common are these genetically identified secondary forms of hypertension? Based on the prevalence of the risk alleles of the 18 genes associated with SSBP and considering the likelihood that some individuals will carry a risk allele from more than one gene, it is likely that nearly half of the primary hypertension population will carry a risk allele from one or more of these 18 genes. Thus, when validated with clinical trial data, the known causes of hypertension may have increased from the 7% to 12% (the currently defined secondary hypertensives) to nearly 60% of the hypertensive population.
The active phenotype used in all GWASs and many candidate gene approaches reviewed herein has been hypertension with the control group consisting of individuals with “normotension.” There are several assumptions on which the validity of these approaches rests. First, hypertension is a consistently defined entity. This assumption seems unlikely. During the past 30 years, who has hypertension, and particularly at what blood pressure level treatment should be instituted, has varied by as much as 25/10 mm Hg. Furthermore, the level of blood pressure used to define hypertension varies in different parts of the world. Also, when treatment is stopped even for as long as a year, for some “hypertensives” blood pressure may not rise above the normal range. Thus, comparing results from studies from different years or areas of the world are likely flawed. Second, hypertension and normotension can clearly be distinguished. This assumption seems unlikely. Nearly all, if not all, studies that have assessed blood pressure levels in large populations have confirmed that blood pressure is a continuous, not dichotomous, variable. This fact likely explains the continuing change in the criteria used to define hypertension. It is not a specific blood pressure level that is unique, but rather cardiovascular events that are associated with an imprecise surrogate marker—blood pressure. Third, hypertension is a disease. This assumption also seems unlikely. Several lines of evidence, including the data in many of the articles reviewed herein, support the hypothesis that hypertension is a syndrome composed of several disease states, each associated with dysregulation of volume homeostatic and/or vasoconstrictor systems that results in a common sign—an increased blood pressure. The clinical expression of these dysregulations, that is, hypertension, takes time, usually years, to develop. Thus, in contrast to the 2005 review that organized the data by systems (2), the currently available data fit more logically in a blood pressure functional paradigm. For example, in this review, some people with salt-sensitive hypertension had low renin levels, whereas others did not. As would be anticipated, the mechanisms underlying their hypertensive states differed. More than half of the group with low renin had evidence of increased aldosterone, whereas the group with normal renin and salt sensitivity had more support for a vascular, particularly renovascular, mechanism for the salt sensitivity of their blood pressure.
What is required to test the hypothesis that hypertension is a syndrome composed of several disease states as suggested by the articles surveyed for this review? There are at least three major, current obstacles: first, defining the phenotypic characteristics of each hypertensive disease; second, determining each disease’s specific mechanisms; and third, identifying the specific individuals whose hypertension is caused by each unique mechanism. These obstacles are similar to those faced by other complex chronic conditions, for example, diabetes, asthma, congestive heart failure, and chronic anxiety states. Because of these obstacles, other “omics” in addition to genomics are being employed to identify potential mechanisms. Omics are powerful tools to accomplish this goal, but they will only take us so far for complex pathophysiological entities such as hypertension if we fail to seriously consider the intense phenotypic heterogeneity. Based on the articles reviewed herein, the most likely way to accomplish this goal is to study genotype/phenotype relationships in exquisitely “deeply” phenotyped cohorts. Some of the articles surveyed used such cohorts. These cohorts had the following two attributes: (i) individuals (with and without hypertension) enrolled in a protocol where most of the environmental factors that could influence the activity of volume and vasoconstrictor regulating systems had been controlled; and (ii) on this controlled background, interventions (“stress tests”) were performed to nearly maximally stimulate and nearly maximally suppress the activity of these regulating systems to uncover subtle mechanistic dysfunctions that, with time, could lead to hypertension.
“…hypertension is a syndrome composed of several disease states, each associated with dysregulation of volume homeostatic and/or vasoconstrictor systems….”
In the literature surveyed, however, there were at least four critical findings absent from most of the publications reviewed that limited our ability to more precisely address the above hypothesis. First, in nearly all studies, a causative gene variation was not identified. The studies used either tagging SNPs from haplotype candidate gene analyses or from GWASs. Second, only a few studies (LSD1, ESR2, EDN1, AGT, and STRN) assessed the effect of the risk allele on the intermediate and/or proximate phenotypes in a normotensive group. Because the genetic changes observed are in the germline, one would anticipate that people who are normotensive who carried the risk allele might also have the associated intermediate or proximate phenotype even though they did not have the distant phenotype (hypertension). Such information could provide clues to the mechanisms underlying the relationship between the risk allele and hypertension. Third, there were no controlled trials where the subjects were randomized to treatment groups by their genotype status. Some of the 21 proximate phenotype groups, particularly in those where there were extensive data from deeply phenotyped human studies and genetically modified animals, are reasonable candidates for such trials.
In this survey, the phenotypic findings were grouped by individual genes. However, it is likely that the subjects inherited risk alleles from several genes. However, there were only five studies where the effects of gene–gene interaction were reported (ACE/EDNRB, ADD1/ATP2B1, ADD/WNK1/NEDD4L, AGT/ACE, and AGT/ACE/CYP11B2). Of interest, in none of the five cases did the phenotypic characteristics change, except to make more pronounced the phenotype associated with polymorphic variants in the primary gene. For example, the AGT risk allele was associated with SSBP, normal PRA, and reduced aldosterone response to ANGII on a restricted salt intake. When the subject also possessed the risk allele for ACE, the aldosterone response was further reduced; and when the individual possessed the risk allele for AGT/ACE/ CYP11B2, the blunted aldosterone response was even greater (61). Of importance, in this cohort neither the ACE nor CYP11B2 alone was associated with altered aldosterone response to ANGII. This characteristic occurred only when they were combined with AGT. None of the other phenotypic characteristics changed appreciably. These results suggest that the fundamental mechanism underlying the pathophysiology in these subjects did not change even though the individuals possessed more risk alleles—the genetic driver was defined primarily by the principal genotype/phenotype association. However, none of these studies has been replicated.
There are several limitations to the conclusions drawn from this survey of the literature. First, only the PubMed search engine was used. Other data sources might have yield different results. Second, the key search words were limited to hypertension or variants on that word. As noted above, some of the genotype/phenotype groups reported an association with an intermediate phenotype of hypertension and not hypertension per se. We in part compensated for this potential issue by also including “salt sensitivity” and “salt-sensitive hypertension” in our search word list. Third, we excluded publications of known monogenic and secondary causes of hypertension. Thus, our list is not all encompassing of the genetics of hypertension. Finally, definitive exclusion of known secondary causes of hypertension was infrequently reported. Thus, whether only subjects with primary hypertension were included in these cohorts is uncertain.
In conclusion, during the past dozen years, substantial progress has been made in identifying potential genetic factors associated with the primary hypertension syndrome. This progress has been largely driven by considerable improvement in the tools needed to assess the human genome. Yet, the data obtained also support the conclusion that many of the proposed genes are likely false positives. Contrariwise, more consistent associations were reported because of refinements in phenotyping. However, improvements in phenotyping appear to be more difficult to implement than what has occurred with genotyping. Specifically, the availability of even modestly deep phenotyping data was the most common factor distinguishing the phenotype of the 21 genes that made the detailed review list from the 41 that did not. Yet, to date, intermediate or more proximate phenotypes have been used infrequently to identify genes associated with hypertension. The reasons likely are related to the lack of appropriate “clean” data sets given, at least, seven factors:
Determining who has hypertension, given its changing definition [compare recommendations in JNC7 and the 2017 American College of Cardiology/American Heart Association guidelines (285, 286)].
Criteria that are used to exclude secondary hypertension are limited at best and nonexistent at worst.
Usually hypertension per se is used as the phenotype, even though the term is describing a syndrome, not a disease.
Most genetic factors related to primary hypertension likely involve a change in the regulation of a gene’s transcription, not the structure of its product, thereby requiring more detailed phenotypic data.
Difficulty in determining who does not have primary hypertension makes determining who can serve as a control group also difficult.
Environmental factors, particularly salt intake, have a substantial impact on the primary hypertension phenotype expressed. Clinical data likely have limited utility to overcome this problem.
The complex array of systems that could be dysfunctional in people with hypertension results in a very heterogeneous cohort in the absence of deep phenotyping.
Thus, these challenges need to be addressed, likely by developing better deep phenotyping approaches. When accomplished, individualized, personalized therapy can be achieved by using a three-step paradigm: by determining the specific mechanisms of the individual diseases (causes) (usually with the assistance of genetically modified animal models); by identifying the specific person with the disease (using genotypes of the linked genes); and finally, by defining the precise mechanistically driven treatment and prevention strategies for the individual primary hypertension diseases, that is, proximate phenotypes.
Acknowledgments
We thank the students, fellows, and faculty of the Cardiovascular Endocrinology Section, Division of Endocrinology, Diabetes, and Hypertension, Brigham and Women’s Hospital, for inspiring and encouraging us to complete this project. We appreciate the administrative and editorial assistance of Haris Lefteri and the artistic assistance of Luminita Pojoga, Chee Sin Tay, and Jessica Lee.
Financial Support: This work was supported in part by the Division of Endocrinology, Diabetes and Hypertension, Brigham and Women’s Hospital, Boston, MA, as well as by a fellowship to W.M. from the Faculty of Medicine, Chiang Mai University (Chiang Mai, Thailand).
Author Contributions: W.M. and G.H.W. established the survey plan, independently screened the individual publications and then, by consensus, identified the publications to be assessed for inclusion/exclusion criteria. W.M. and G.H.W. wrote the manuscript. G.H.W. created the concept of the manuscript and provided the final editing of the manuscript.
Disclosure Summary: The authors have nothing to disclose.
Glossary
Abbreviations:
- ACE
angiotensin-converting enzyme
- ADD-1
adducin-1
- ADRβ2
β 2-adrenergic receptor
- AGT
angiotensinogen
- AGTR1
angiotensin receptor type I
- ANGII
angiotensin II
- ATP2B1
plasma membrane calcium-transporting ATPase 1
- AT1R
angiotensin receptor type 1
- BDKRB2
bradykinin receptor B2
- CAV1
caveolin-1
- cGMP
cyclic GMP
- CYP17A1
cytochrome P450 family 17 subfamily A member 1
- CYP11B2
cytochrome P450 family 11 subfamily B member 2
- EDN1
endothelin-1
- ENaC
epithelial Na+ channel
- eNOS
endothelial nitric oxide synthase
- ER
estrogen receptor
- ESR2
estrogen receptor β
- FGF5
fibroblast growth factor 5
- GNB3
G protein β3 subunit
- GWAS
genome-wide association study
- LSD1
lysine-specific demethylase 1
- MR
mineralocorticoid receptor
- MRA
MR antagonist
- NEDD4L
neural precursor cell expressed developmentally downregulated 4-like
- PRA
plasma renin activity
- RAAS
renin–angiotensin–aldosterone system
- REN
renin (gene)
- SGK1
serum- and glucocorticoid-inducible kinase 1
- SLC4A5
electrogenic sodium bicarbonate cotransporter 4
- SNP
single-nucleotide polymorphism
- SSBP
salt-sensitive blood pressure
- STK39
serine/threonine 39
- STRN
striatin (gene)
- WNK1
lysine-deficient protein kinase 1.
References
- 1. Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, Chen J, He J. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Agarwal A, Williams GH, Fisher ND. Genetics of human hypertension. Trends Endocrinol Metab. 2005;16(3):127–133. [DOI] [PubMed] [Google Scholar]
- 3. Robinson RF, Batisky DL, Hayes JR, Nahata MC, Mahan JD. Significance of heritability in primary and secondary pediatric hypertension. Am J Hypertens. 2005;18(7):917–921. [DOI] [PubMed] [Google Scholar]
- 4. Biino G, Parati G, Concas MP, Adamo M, Angius A, Vaccargiu S, Pirastu M. Environmental and genetic contribution to hypertension prevalence: data from an epidemiological survey on Sardinian genetic isolates. PLoS One. 2013;8(3):e59612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hollenberg NK. Genes, hypertension, and intermediate phenotypes. Curr Opin Cardiol. 1996;11(5):457–463. [DOI] [PubMed] [Google Scholar]
- 6. Hollenberg NK. A genome-wide search for susceptibility loci to human essential hypertension. Curr Hypertens Rep. 2001;3(1):7–8. [PubMed] [Google Scholar]
- 7. Dickson ME, Sigmund CD. Genetic basis of hypertension: revisiting angiotensinogen. Hypertension. 2006;48(1):14–20. [DOI] [PubMed] [Google Scholar]
- 8. Hottenga JJ, Boomsma DI, Kupper N, Posthuma D, Snieder H, Willemsen G, de Geus JC. Heritability and stability of resting blood pressure. Twin Res Hum Genet. 2005;8(5):499–508. [DOI] [PubMed] [Google Scholar]
- 9. Frohlich ED. Treating hypertension—what are we to believe? N Engl J Med. 2003;348(7):639–641. [DOI] [PubMed] [Google Scholar]
- 10. Williams GH, Fisher ND. Genetic approach to diagnostic and therapeutic decisions in human hypertension. Curr Opin Nephrol Hypertens. 1997;6(2):199–204. [DOI] [PubMed] [Google Scholar]
- 11. Kupper N, Ge D, Treiber FA, Snieder H. Emergence of novel genetic effects on blood pressure and hemodynamics in adolescence: the Georgia Cardiovascular Twin Study. Hypertension. 2006;47(5):948–954. [DOI] [PubMed] [Google Scholar]
- 12. Hedayati SS, Elsayed EF, Reilly RF. Non-pharmacological aspects of blood pressure management: what are the data? Kidney Int. 2011;79(10):1061–1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Knight BS, Sunn N, Pennell CE, Adamson SL, Lye SJ. Developmental regulation of cardiovascular function is dependent on both genotype and environment. Am J Physiol Heart Circ Physiol. 2009;297(6):H2234–H2241. [DOI] [PubMed] [Google Scholar]
- 14. Zheng J, Rao DC, Shi G. An update on genome-wide association studies of hypertension. Appl Inform (Berl). 2015;2(1):10. [Google Scholar]
- 15. Warren HR, Evangelou E, Cabrera CP, Gao H, Ren M, Mifsud B, Ntalla I, Surendran P, Liu C, Cook JP, Kraja AT, Drenos F, Loh M, Verweij N, Marten J, Karaman I, Lepe MP, O’Reilly PF, Knight J, Snieder H, Kato N, He J, Tai ES, Said MA, Porteous D, Alver M, Poulter N, Farrall M, Gansevoort RT, Padmanabhan S, Mägi R, Stanton A, Connell J, Bakker SJ, Metspalu A, Shields DC, Thom S, Brown M, Sever P, Esko T, Hayward C, van der Harst P, Saleheen D, Chowdhury R, Chambers JC, Chasman DI, Chakravarti A, Newton-Cheh C, Lindgren CM, Levy D, Kooner JS, Keavney B, Tomaszewski M, Samani NJ, Howson JM, Tobin MD, Munroe PB, Ehret GB, Wain LV; International Consortium of Blood Pressure (ICBP) 1000G Analyses; BIOS Consortium; Lifelines Cohort Study; Understanding Society Scientific group; CHD Exome+ Consortium; ExomeBP Consortium; T2D-GENES Consortium; GoT2DGenes Consortium; Cohorts for Heart and Ageing Research in Genome Epidemiology (CHARGE) BP Exome Consortium; International Genomics of Blood Pressure (iGEN-BP) Consortium; UK Biobank CardioMetabolic Consortium BP working group. Genome-wide association analysis identifies novel blood pressure loci and offers biological insights into cardiovascular risk. Nat Genet. 2017;49(3):403–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chami N, Lettre G. Lessons and implications from genome-wide association studies (GWAS) findings of blood cell phenotypes. Genes (Basel). 2014;5(1):51–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kodama S, Fujihara K, Ishiguro H, Horikawa C, Ohara N, Yachi Y, Tanaka S, Shimano H, Kato K, Hanyu O, Sone H. Quantitative relationship between cumulative risk alleles based on genome-wide association studies and type 2 diabetes mellitus: a systematic review and meta-analysis. J Epidemiol. 2018;28(1):3–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Posey JE, Harel T, Liu P, Rosenfeld JA, James RA, Coban Akdemir ZH, Walkiewicz M, Bi W, Xiao R, Ding Y, Xia F, Beaudet AL, Muzny DM, Gibbs RA, Boerwinkle E, Eng CM, Sutton VR, Shaw CA, Plon SE, Yang Y, Lupski JR. Resolution of disease phenotypes resulting from multilocus genomic variation. N Engl J Med. 2017;376(1):21–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Robinson PN, Köhler S, Bauer S, Seelow D, Horn D, Mundlos S. The Human Phenotype Ontology: a tool for annotating and analyzing human hereditary disease. Am J Hum Genet. 2008;83(5):610–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yang H, Robinson PN, Wang K. Phenolyzer: phenotype-based prioritization of candidate genes for human diseases. Nat Methods. 2015;12(9):841–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Collier N, Groza T, Smedley D, Robinson PN, Oellrich A, Rebholz-Schuhmann D. PhenoMiner: from text to a database of phenotypes associated with OMIM diseases. Database (Oxford). 2015;2015:bav104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mendel G. Experiments in Plant Hybridization (1865). New York: Cosimo, Inc., 2008. [Google Scholar]
- 23. Fisher ND, Hurwitz S, Ferri C, Jeunemaitre X, Hollenberg NK, Williams GH. Altered adrenal sensitivity to angiotensin II in low-renin essential hypertension. Hypertension. 1999;34(3):388–394. [DOI] [PubMed] [Google Scholar]
- 24. Chamarthi B, Williams JS, Williams GH. A mechanism for salt-sensitive hypertension: abnormal dietary sodium-mediated vascular response to angiotensin-II. J Hypertens. 2010;28(5):1020–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pojoga L, Kolatkar NS, Williams JS, Perlstein TS, Jeunemaitre X, Brown NJ, Hopkins PN, Raby BA, Williams GH. β-2 Adrenergic receptor diplotype defines a subset of salt-sensitive hypertension. Hypertension. 2006;48(5):892–900. [DOI] [PubMed] [Google Scholar]
- 26. Lamaze C, Tardif N, Dewulf M, Vassilopoulos S, Blouin CM. The caveolae dress code: structure and signaling. Curr Opin Cell Biol. 2017;47:117–125. [DOI] [PubMed] [Google Scholar]
- 27. Pojoga LH, Underwood PC, Goodarzi MO, Williams JS, Adler GK, Jeunemaitre X, Hopkins PN, Raby BA, Lasky-Su J, Sun B, Cui J, Guo X, Taylor KD, Chen YD, Xiang A, Raffel LJ, Buchanan TA, Rotter JI, Williams GH. Variants of the caveolin-1 gene: a translational investigation linking insulin resistance and hypertension. J Clin Endocrinol Metab. 2011;96(8):E1288–E1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yamada Y, Ando F, Shimokata H. Association of gene polymorphisms with blood pressure and the prevalence of hypertension in community-dwelling Japanese individuals. Int J Mol Med. 2007;19(4):675–683. [PubMed] [Google Scholar]
- 29. Baudrand R, Goodarzi MO, Vaidya A, Underwood PC, Williams JS, Jeunemaitre X, Hopkins PN, Brown N, Raby BA, Lasky-Su J, Adler GK, Cui J, Guo X, Taylor KD, Chen YD, Xiang A, Raffel LJ, Buchanan TA, Rotter JI, Williams GH, Pojoga LH. A prevalent caveolin-1 gene variant is associated with the metabolic syndrome in Caucasians and Hispanics. Metabolism. 2015;64(12):1674–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Baudrand R, Gupta N, Garza AE, Vaidya A, Leopold JA, Hopkins PN, Jeunemaitre X, Ferri C, Romero JR, Williams J, Loscalzo J, Adler GK, Williams GH, Pojoga LH. Caveolin 1 modulates aldosterone-mediated pathways of glucose and lipid homeostasis. J Am Heart Assoc. 2016;5(10):e003845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Grilo A, Fernandez ML, Beltrán M, Ramirez-Lorca R, González MA, Royo JL, Gutierrez-Tous R, Morón FJ, Couto C, Serrano-Rios M, Saez ME, Ruiz A, Real LM. Genetic analysis of CAV1 gene in hypertension and metabolic syndrome. Thromb Haemost. 2006;95(4):696–701. [PubMed] [Google Scholar]
- 32. Cohen AW, Razani B, Wang XB, Combs TP, Williams TM, Scherer PE, Lisanti MP. Caveolin-1-deficient mice show insulin resistance and defective insulin receptor protein expression in adipose tissue. Am J Physiol Cell Physiol. 2003;285(1):C222–C235. [DOI] [PubMed] [Google Scholar]
- 33. Kabayama K, Sato T, Saito K, Loberto N, Prinetti A, Sonnino S, Kinjo M, Igarashi Y, Inokuchi J. Dissociation of the insulin receptor and caveolin-1 complex by ganglioside GM3 in the state of insulin resistance. Proc Natl Acad Sci USA. 2007;104(34):13678–13683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Pojoga LH, Romero JR, Yao TM, Loutraris P, Ricchiuti V, Coutinho P, Guo C, Lapointe N, Stone JR, Adler GK, Williams GH. Caveolin-1 ablation reduces the adverse cardiovascular effects of N-ω-nitro-l-arginine methyl ester and angiotensin II. Endocrinology. 2010;151(3):1236–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Pojoga LH, Yao TM, Sinha S, Ross RL, Lin JC, Raffetto JD, Adler GK, Williams GH, Khalil RA. Effect of dietary sodium on vasoconstriction and eNOS-mediated vascular relaxation in caveolin-1-deficient mice. Am J Physiol Heart Circ Physiol. 2008;294(3):H1258–H1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Pojoga LH, Adamová Z, Kumar A, Stennett AK, Romero JR, Adler GK, Williams GH, Khalil RA. Sensitivity of NOS-dependent vascular relaxation pathway to mineralocorticoid receptor blockade in caveolin-1-deficient mice. Am J Physiol Heart Circ Physiol. 2010;298(6):H1776–H1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Shoback DM, Williams GH, Moore TJ, Dluhy RG, Podolsky S, Hollenberg NK. Defect in the sodium-modulated tissue responsiveness to angiotensin II in essential hypertension. J Clin Invest. 1983;72(6):2115–2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Redgrave J, Rabinowe S, Hollenberg NK, Williams GH. Correction of abnormal renal blood flow response to angiotensin II by converting enzyme inhibition in essential hypertensives. J Clin Invest. 1985;75(4):1285–1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Uneda S, Fujishima S, Fujiki Y, Tochikubo O, Oda H, Asahina S, Kaneko Y. Renal haemodynamics and the renin-angiotensin system in adolescents genetically predisposed to essential hypertension. J Hypertens Suppl. 1984;2(3):S437–S439. [PubMed] [Google Scholar]
- 40. Ramirez AJ, Migliorini M, Gilbert BH, Marco EJ, Sanchez RA. Non-modulating essential hypertension: renal hemodynamic effects of long-term angiotensin converting enzyme inhibition. J Hypertens Suppl. 1991;9(6):S396–S397. [PubMed] [Google Scholar]
- 41. Ferri C, Bellini C, Desideri G, Valenti M, De Mattia G, Santucci A, Hollenberg NK, Williams GH. Relationship between insulin resistance and nonmodulating hypertension: linkage of metabolic abnormalities and cardiovascular risk. Diabetes. 1999;48(8):1623–1630. [DOI] [PubMed] [Google Scholar]
- 42. van Hooft IM, Grobbee DE, Derkx FH, de Leeuw PW, Schalekamp MA, Hofman A. Renal hemodynamics and the renin-angiotensin-aldosterone system in normotensive subjects with hypertensive and normotensive parents. N Engl J Med. 1991;324(19):1305–1311. [DOI] [PubMed] [Google Scholar]
- 43. Beretta-Piccoli C, Pusterla C, Städler P, Weidmann P. Blunted aldosterone responsiveness to angiotensin II in normotensive subjects with familial predisposition to essential hypertension. J Hypertens. 1988;6(1):57–61. [PubMed] [Google Scholar]
- 44. Hollenberg NK, Williams GH. Abnormal renal function, sodium-volume homeostasis and renin system behavior in normal-renin essential hypertension: the evolution of the nonmodulator concept. In: Laragh JH, Brenner BM, eds. Hypertension: Pathophysiology, Diagnosis, and Management. 2nd ed. New York, NY: Raven; 1995:1837–1856. [Google Scholar]
- 45. Hopkins PN, Lifton RP, Hollenberg NK, Jeunemaitre X, Hallouin MC, Skuppin J, Williams CS, Dluhy RG, Lalouel JM, Williams RR, Williams GH. Blunted renal vascular response to angiotensin II is associated with a common variant of the angiotensinogen gene and obesity. J Hypertens. 1996;14(2):199–207. [DOI] [PubMed] [Google Scholar]
- 46. Watkins WS, Hunt SC, Williams GH, Tolpinrud W, Jeunemaitre X, Lalouel JM, Jorde LB. Genotype-phenotype analysis of angiotensinogen polymorphisms and essential hypertension: the importance of haplotypes. J Hypertens. 2010;28(1):65–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Patel TV, Williams GH, Fisher ND. Angiotensinogen genotype predicts abnormal renal hemodynamics in young hypertensive patients. J Hypertens. 2008;26(7):1353–1359. [DOI] [PubMed] [Google Scholar]
- 48. Hopkins PN, Hunt SC, Jeunemaitre X, Smith B, Solorio D, Fisher ND, Hollenberg NK, Williams GH. Angiotensinogen genotype affects renal and adrenal responses to angiotensin II in essential hypertension. Circulation. 2002;105(16):1921–1927. [DOI] [PubMed] [Google Scholar]
- 49. Jeunemaitre X, Soubrier F, Kotelevtsev YV, Lifton RP, Williams CS, Charru A, Hunt SC, Hopkins PN, Williams RR, Lalouel JM, Corvol P. Molecular basis of human hypertension: role of angiotensinogen. Cell. 1992;71(1):169–180. [DOI] [PubMed] [Google Scholar]
- 50. Underwood PC, Chamarthi B, Williams JS, Vaidya A, Garg R, Adler GK, Grotzke MP, Staskus G, Wadwekar D, Hopkins PN, Ferri C, McCall A, McClain D, Williams GH. Nonmodulation as the mechanism for salt sensitivity of blood pressure in individuals with hypertension and type 2 diabetes mellitus. J Clin Endocrinol Metab. 2012;97(10):3775–3782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Underwood PC, Sun B, Williams JS, Pojoga LH, Raby B, Lasky-Su J, Hunt S, Hopkins PN, Jeunemaitre X, Adler GK, Williams GH. The association of the angiotensinogen gene with insulin sensitivity in humans: a tagging single nucleotide polymorphism and haplotype approach. Metabolism. 2011;60(8):1150–1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Dluhy RG, Smith K, Taylor T, Hollenberg NK, Williams GH. Prolonged converting enzyme inhibition in non-modulating hypertension. Hypertension. 1989;13(4):371–377. [DOI] [PubMed] [Google Scholar]
- 53. Taylor T, Moore TJ, Hollenberg NK, Williams GH. Converting-enzyme inhibition corrects the altered adrenal response to angiotensin II in essential hypertension. Hypertension. 1984;6(1):92–99. [DOI] [PubMed] [Google Scholar]
- 54. Williams GH, Hollenberg NK. Non-modulating essential hypertension: a subset particularly responsive to converting enzyme inhibitors. J Hypertens Suppl. 1985;3(2):S81–S87. [PubMed] [Google Scholar]
- 55. Bonfim-Silva R, Guimarães LO, Souza Santos J, Pereira JF, Leal Barbosa AA, Souza Rios DL. Case-control association study of polymorphisms in the angiotensinogen and angiotensin-converting enzyme genes and coronary artery disease and systemic artery hypertension in African-Brazilians and Caucasian-Brazilians. J Genet. 2016;95(1):63–69. [DOI] [PubMed] [Google Scholar]
- 56. Tabei SM, Nariman A, Daliri K, Roozbeh J, Khezri A, Goodarzi HR, Lotfi M, Sefidbakht S, Entezam M. Simple renal cysts and hypertension are associated with angiotensinogen (AGT) gene variant in Shiraz population (Iran). J Renin Angiotensin Aldosterone Syst. 2015;16(2):409–414. [DOI] [PubMed] [Google Scholar]
- 57. Goldenberg I, Moss AJ, Ryan D, McNitt S, Eberly SW, Zareba W. Polymorphism in the angiotensinogen gene, hypertension, and ethnic differences in the risk of recurrent coronary events. Hypertension. 2006;48(4):693–699. [DOI] [PubMed] [Google Scholar]
- 58. Afshariani R, Roozbeh J, Sharifian M, Ghaedi M, Samsami Dehaghani A, Ghaderi A. Association between angiotensinogen M235T polymorphism and preeclampsia in Iranian pregnant women. J Family Reprod Health. 2014;8(4):169–173. [PMC free article] [PubMed] [Google Scholar]
- 59. Kurland L, Liljedahl U, Karlsson J, Kahan T, Malmqvist K, Melhus H, Syvänen AC, Lind L. Angiotensinogen gene polymorphisms: relationship to blood pressure response to antihypertensive treatment. Results from the Swedish Irbesartan Left Ventricular Hypertrophy Investigation vs Atenolol (SILVHIA) trial. Am J Hypertens. 2004;17(1):8–13. [DOI] [PubMed] [Google Scholar]
- 60. Yu H, Lin S, Zhong J, He M, Jin L, Zhang Y, Liu G. A core promoter variant of angiotensinogen gene and interindividual variation in response to angiotensin-converting enzyme inhibitors. J Renin Angiotensin Aldosterone Syst. 2014;15(4):540–546. [DOI] [PubMed] [Google Scholar]
- 61. Li Q, Sun L, Du J, Ran P, Gao T, Yuan Y, Xiao C. Risk given by AGT polymorphisms in inducing susceptibility to essential hypertension among isolated populations from a remote region of China: a case-control study among the isolated populations. J Renin Angiotensin Aldosterone Syst. 2015;16(4):1202–1217. [DOI] [PubMed] [Google Scholar]
- 62. Niu S, Zhang B, Zhang K, Zhu P, Li J, Sun Y, He N, Zhang M, Gao Z, Li X, Simayi A, Ge J, Cong M, Zhou W, Qiu C. Synergistic effects of gene polymorphisms of the renin–angiotensin–aldosterone system on essential hypertension in Kazakhs in Xinjiang. Clin Exp Hypertens. 2016;38(1):63–70. [DOI] [PubMed] [Google Scholar]
- 63. Purkait P, Halder K, Thakur S, Ghosh Roy A, Raychaudhuri P, Bhattacharya S, Sarkar BN, Naidu JM. Association of angiotensinogen gene SNPs and haplotypes with risk of hypertension in eastern Indian population. Clin Hypertens. 2017;23(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Zotova TY, Kubanova AP, Azova MM, Aissa AA, Gigani OO, Frolov VA. Analysis of polymorphism of angiotensin system genes (ACE, AGTR1, and AGT) and gene ITGB3 in patients with arterial hypertension in combination with metabolic syndrome. Bull Exp Biol Med. 2016;161(3):334–338. [DOI] [PubMed] [Google Scholar]
- 65. Tsezou A, Karayannis G, Giannatou E, Papanikolaou V, Triposkiadis F. Association of renin-angiotensin system and natriuretic peptide receptor A gene polymorphisms with hypertension in a Hellenic population. J Renin Angiotensin Aldosterone Syst. 2008;9(4):202–207. [DOI] [PubMed] [Google Scholar]
- 66. Kosachunhanun N, Hunt SC, Hopkins PN, Williams RR, Jeunemaitre X, Corvol P, Ferri C, Mortensen RM, Hollenberg NK, Williams GH. Genetic determinants of nonmodulating hypertension. Hypertension. 2003;42(5):901–908. [DOI] [PubMed] [Google Scholar]
- 67. Kaplan İ, Sancaktar E, Ece A, Şen V, Tekkeşin N, Basarali MK, Kelekci S, Evliyaoglu O. Gene polymorphisms of adducin GLY460TRP, ACE I/D, and AGT M235T in pediatric hypertension patients. Med Sci Monit. 2014;20:1745–1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Kolovou V, Lagou E, Mihas C, Vasiliki G, Katsiki N, Kollia A, Triposkiadis F, Degiannis D, Mavrogeni S, Kolovou G. Angiotensinogen (AGT) M235T, AGT T174M and angiotensin-1-converting enzyme (ACE) I/D gene polymorphisms in essential hypertension: effects on ramipril efficacy. Open Cardiovasc Med J. 2015;9(1):118–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Srivastava K, Chandra S, Bhatia J, Narang R, Saluja D. Association of angiotensinogen (M235T) gene polymorphism with blood pressure lowering response to angiotensin converting enzyme inhibitor (enalapril). J Pharm Pharm Sci. 2012;15(3):399–406. [DOI] [PubMed] [Google Scholar]
- 70. Ramachandran V, Ismail P, Stanslas J, Shamsudin N. Analysis of renin-angiotensin aldosterone system gene polymorphisms in Malaysian essential hypertensive and type 2 diabetic subjects. Cardiovasc Diabetol. 2009;8(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Liao X, Yang Z, Peng D, Dai H, Lei Y, Zhao Q, Han Y, Wang W. Association of T174M polymorphism of angiotensinogen gene with essential hypertension: a meta-analysis. Genet Mol Biol. 2014;37(3):473–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Yiannikouris F, Wang Y, Shoemaker R, Larian N, Thompson J, English VL, Charnigo R, Su W, Gong M, Cassis LA. Deficiency of angiotensinogen in hepatocytes markedly decreases blood pressure in lean and obese male mice. Hypertension. 2015;66(4):836–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Ying J, Stuart D, Hillas E, Gociman BR, Ramkumar N, Lalouel JM, Kohan DE. Overexpression of mouse angiotensinogen in renal proximal tubule causes salt-sensitive hypertension in mice. Am J Hypertens. 2012;25(6):684–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Jain S, Tillinger A, Mopidevi B, Pandey VG, Chauhan CK, Fiering SN, Warming S, Kumar A. Transgenic mice with –6A haplotype of the human angiotensinogen gene have increased blood pressure compared with –6G haplotype. J Biol Chem. 2010;285(52):41172–41186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Hollenberg NK, Moore T, Shoback D, Redgrave J, Rabinowe S, Williams GH. Abnormal renal sodium handling in essential hypertension. Relation to failure of renal and adrenal modulation of responses to angiotensin II. Am J Med. 1986;81(3):412–418. [DOI] [PubMed] [Google Scholar]
- 76. Rydstedt LL, Williams GH, Hollenberg NK. Renal and endocrine response to saline infusion in essential hypertension. Hypertension. 1986;8(3):217–222. [DOI] [PubMed] [Google Scholar]
- 77. Seely EW, Moore TJ, Rogacz S, Gordon MS, Gleason RE, Hollenberg NK, Williams GH. Angiotensin-mediated renin suppression is altered in non-modulating hypertension. Hypertension. 1989;13(1):31–37. [DOI] [PubMed] [Google Scholar]
- 78. Rabinowe SL, Redgrave JE, Shoback DM, Podolsky S, Hollenberg NK, Williams GH. Renin suppression by saline is blunted in nonmodulating essential hypertension. Hypertension. 1987;10(4):404–408. [DOI] [PubMed] [Google Scholar]
- 79. Gordon MS, Steunkel CA, Conlin PR, Hollenberg NK, Williams GH. The role of dopamine in nonmodulating hypertension. J Clin Endocrinol Metab. 1989;69(2):426–432. [DOI] [PubMed] [Google Scholar]
- 80. Redgrave J, Canessa M, Gleason R, Hollenberg NK, Williams GH. Red blood cell lithium-sodium countertransport in non-modulating essential hypertension. Hypertension. 1989;13(6 Pt 2):721–726. [DOI] [PubMed] [Google Scholar]
- 81. Srikumar N, Brown NJ, Hopkins PN, Jeunemaitre X, Hunt SC, Vaughan DE, Williams GH. PAI-1 in human hypertension: relation to hypertensive groups. Am J Hypertens. 2002;15(8):683–690. [DOI] [PubMed] [Google Scholar]
- 82. Raji A, Williams GH, Jeunemaitre X, Hopkins PN, Hunt SC, Hollenberg NK, Seely EW. Insulin resistance in hypertensives: effect of salt sensitivity, renin status and sodium intake. J Hypertens. 2001;19(1):99–105. [DOI] [PubMed] [Google Scholar]
- 83. Fisher ND, Ferri C, Bellini C, Santucci A, Gleason R, Williams GH, Hollenberg NK, Seely EW. Age, gender, and non-modulation. A sexual dimorphism in essential hypertension. Hypertension. 1997;29(4):980–985. [DOI] [PubMed] [Google Scholar]
- 84. Frazier L, Turner ST, Schwartz GL, Chapman AB, Boerwinkle E. Multilocus effects of the renin-angiotensin-aldosterone system genes on blood pressure response to a thiazide diuretic. Pharmacogenomics J. 2004;4(1):17–23. [DOI] [PubMed] [Google Scholar]
- 85. Hingorani AD, Jia H, Stevens PA, Hopper R, Dickerson JE, Brown MJ. Renin-angiotensin system gene polymorphisms influence blood pressure and the response to angiotensin converting enzyme inhibition. J Hypertens. 1995;13(12 Pt 2):1602–1609. [PubMed] [Google Scholar]
- 86. Dudley C, Keavney B, Casadei B, Conway J, Bird R, Ratcliffe P. Prediction of patient responses to antihypertensive drugs using genetic polymorphisms: investigation of renin-angiotensin system genes. J Hypertens. 1996;14(2):259–262. [DOI] [PubMed] [Google Scholar]
- 87. Heidari F, Vasudevan R, Mohd Ali SZ, Ismail P, Arkani M. RAS genetic variants in interaction with ACE inhibitors drugs influences essential hypertension control. Arch Med Res. 2017;48(1):88–95. [DOI] [PubMed] [Google Scholar]
- 88. Lynch AI, Arnett DK, Davis BR, Boerwinkle E, Ford CE, Eckfeldt JH, Leiendecker-Foster C. Sex-specific effects of AGT-6 and ACE I/D on pulse pressure after 6 months on antihypertensive treatment: the GenHAT study. Ann Hum Genet. 2007;71(Pt 6):735–745. [DOI] [PubMed] [Google Scholar]
- 89. Do AN, Irvin MR, Lynch AI, Claas SA, Boerwinkle E, Davis BR, Ford CE, Eckfeldt JH, Tiwari HK, Limdi NA, Arnett DK. The effects of angiotensinogen gene polymorphisms on cardiovascular disease outcomes during antihypertensive treatment in the GenHAT study. Front Pharmacol. 2014;5:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Catanzaro DF. Molecular biology of renin and regulation of its gene. In: Singh AK, Williams GH, eds. Textbook of Nephro-Endocrinology. San Diego, CA: Academic; 2017:389–400. [Google Scholar]
- 91. Carey MR, Padia SH. Physiology and regulation of the renin–angiotensin–aldosterone system. In: Singh AK, Williams GH, eds. Textbook of Nephro-Endocrinology, 2nd ed. San Diego, CA: Academic; 2017:1–23. [Google Scholar]
- 92. Sun B, Williams JS, Pojoga L, Chamarthi B, Lasky-Su J, Raby BA, Hopkins PN, Jeunemaitre X, Brown NJ, Ferri C, Williams GH. Renin gene polymorphism: its relationship to hypertension, renin levels and vascular responses. J Renin Angiotensin Aldosterone Syst. 2011;12(4):564–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Fu Y, Katsuya T, Asai T, Fukuda M, Inamoto N, Iwashima Y, Sugimoto K, Rakugi H, Higaki J, Ogihara T. Lack of correlation between Mbo I restriction fragment length polymorphism of renin gene and essential hypertension in Japanese. Hypertens Res. 2001;24(3):295–298. [DOI] [PubMed] [Google Scholar]
- 94. Park J, Song K, Jang Y, Kim Yoon S. A polymorphism of the renin gene rs6682082 is associated with essential hypertension risk and blood pressure levels in Korean women. Yonsei Med J. 2015;56(1):227–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Mansego ML, Redon J, Marin R, González-Albert V, Martin-Escudero JC, Fabia MJ, Martinez F, Chaves FJ. Renin polymorphisms and haplotypes are associated with blood pressure levels and hypertension risk in postmenopausal women. J Hypertens. 2008;26(2):230–237. [DOI] [PubMed] [Google Scholar]
- 96. Ying CQ, Wang YH, Wu ZL, Fang MW, Wang J, Li YS, Zhang YH, Qiu CC. Association of the renin gene polymorphism, three angiotensinogen gene polymorphisms and the haplotypes with essential hypertension in the Mongolian population. Clin Exp Hypertens. 2010;32(5):293–300. [DOI] [PubMed] [Google Scholar]
- 97. Afruza R, Islam LN, Banerjee S, Hassan MM, Suzuki F, Nabi AN. Renin gene polymorphisms in bangladeshi hypertensive population. J Genomics. 2014;2:45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Ramkumar N, Stuart D, Rees S, Hoek AV, Sigmund CD, Kohan DE. Collecting duct-specific knockout of renin attenuates angiotensin II-induced hypertension. Am J Physiol Renal Physiol. 2014;307(8):F931–F938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Castets F, Rakitina T, Gaillard S, Moqrich A, Mattei MG, Monneron A. Zinedin, SG2NA, and striatin are calmodulin-binding, WD repeat proteins principally expressed in the brain. J Biol Chem. 2000;275(26):19970–19977. [DOI] [PubMed] [Google Scholar]
- 100. Ueda K, Lu Q, Baur W, Aronovitz MJ, Karas RH. Rapid estrogen receptor signaling mediates estrogen-induced inhibition of vascular smooth muscle cell proliferation. Arterioscler Thromb Vasc Biol. 2013;33(8):1837–1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Lu Q, Pallas DC, Surks HK, Baur WE, Mendelsohn ME, Karas RH. Striatin assembles a membrane signaling complex necessary for rapid, nongenomic activation of endothelial NO synthase by estrogen receptor alpha. Proc Natl Acad Sci USA. 2004;101(49):17126–17131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Coutinho P, Vega C, Pojoga LH, Rivera A, Prado GN, Yao TM, Adler G, Torres-Grajales M, Maldonado ER, Ramos-Rivera A, Williams JS, Williams G, Romero JR. Aldosterone’s rapid, nongenomic effects are mediated by striatin: a modulator of aldosterone’s effect on estrogen action. Endocrinology. 2014;155(6):2233–2243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Baudrand R, Pojoga L, Romero JR. Aldosterone’s mechanism of action: genomic and nongenomic signaling. In: Singh AK, Williams GH, eds. Textbook of Nephro-Endocrinology, 2nd ed. San Diego, CA: Academic; 2017:173–186. [Google Scholar]
- 104. Garza AE, Rariy CM, Sun B, Williams J, Lasky-Su J, Baudrand R, Yao T, Moize B, Hafiz WM, Romero JR, Adler GK, Ferri C, Hopkins PN, Pojoga LH, Williams GH. Variants in striatin gene are associated with salt-sensitive blood pressure in mice and humans. Hypertension. 2015;65(1):211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Gupta T, Connors M, Tan JW, Manosroi W, Ahmed N, Ting PY, Garza AE, Romero JR, Hopkins PN, Williams JS, Williams GH. Striatin gene polymorphic variants are associated with salt sensitive blood pressure in normotensives and hypertensives. Am J Hypertens. 2017;31(1):124–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Garza AE, Pojoga LH, Moize B, Hafiz WM, Opsasnick LA, Siddiqui WT, Horenstein M, Adler GK, Williams GH, Khalil RA. Critical role of striatin in blood pressure and vascular responses to dietary sodium intake. Hypertension. 2015;66(3):674–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Pojoga LH, Coutinho P, Rivera A, Yao TM, Maldonado ER, Youte R, Adler GK, Williams J, Turchin A, Williams GH, Romero JR. Activation of the mineralocorticoid receptor increases striatin levels. Am J Hypertens. 2012;25(2):243–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Tripodi G, Piscone A, Borsani G, Tisminetzky S, Salardi S, Sidoli A, James P, Pongor S, Bianchi G, Baralle FE. Molecular cloning of an adducin-like protein: evidence of a polymorphism in the normotensive and hypertensive rats of the Milan strain. Biochem Biophys Res Commun. 1991;177(3):939–947. [DOI] [PubMed] [Google Scholar]
- 109. Bianchi G, Tripodi G, Casari G, Salardi S, Barber BR, Garcia R, Leoni P, Torielli L, Cusi D, Ferrandi M. Two point mutations within the adducin genes are involved in blood pressure variation. Proc Natl Acad Sci USA. 1994;91(9):3999–4003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Matsuoka Y, Li X, Bennett V. Adducin: structure, function and regulation. Cell Mol Life Sci. 2000;57(6):884–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Gallardo G, Barowski J, Ravits J, Siddique T, Lingrel JB, Robertson J, Steen H, Bonni A. An α2-Na/K ATPase/α-adducin complex in astrocytes triggers non-cell autonomous neurodegeneration. Nat Neurosci. 2014;17(12):1710–1719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Torielli L, Tivodar S, Montella RC, Iacone R, Padoani G, Tarsini P, Russo O, Sarnataro D, Strazzullo P, Ferrari P, Bianchi G, Zurzolo C α-Adducin mutations increase Na/K pump activity in renal cells by affecting constitutive endocytosis: implications for tubular Na reabsorption. Am J Physiol Renal Physiol. 2008;295(2):F478–F487. [DOI] [PubMed] [Google Scholar]
- 113. Casari G, Barlassina C, Cusi D, Zagato L, Muirhead R, Righetti M, Nembri P, Amar K, Gatti M, Macciardi F, Binelli G, Bianchi G. Association of the α-adducin locus with essential hypertension. Hypertension. 1995;25(3):320–326. [DOI] [PubMed] [Google Scholar]
- 114. Cusi D, Barlassina C, Azzani T, Casari G, Citterio L, Devoto M, Glorioso N, Lanzani C, Manunta P, Righetti M, Rivera R, Stella P, Troffa C, Zagato L, Bianchi G. Polymorphisms of α-adducin and salt sensitivity in patients with essential hypertension. Lancet. 1997;349(9062):1353–1357. [DOI] [PubMed] [Google Scholar]
- 115. Sugimoto K, Hozawa A, Katsuya T, Matsubara M, Ohkubo T, Tsuji I, Motone M, Higaki J, Hisamachi S, Imai Y, Ogihara T. Alpha-adducin Gly460Trp polymorphism is associated with low renin hypertension in younger subjects in the Ohasama study. J Hypertens. 2002;20(9):1779–1784. [DOI] [PubMed] [Google Scholar]
- 116. Manunta P, Cusi D, Barlassina C, Righetti M, Lanzani C, D’Amico M, Buzzi L, Citterio L, Stella P, Rivera R, Bianchi G α-Adducin polymorphisms and renal sodium handling in essential hypertensive patients. Kidney Int. 1998;53(6):1471–1478. [DOI] [PubMed] [Google Scholar]
- 117. Grant FD, Romero JR, Jeunemaitre X, Hunt SC, Hopkins PN, Hollenberg NH, Williams GH. Low-renin hypertension, altered sodium homeostasis, and an α-adducin polymorphism. Hypertension. 2002;39(2):191–196. [DOI] [PubMed] [Google Scholar]
- 118. Fisher ND, Hurwitz S, Jeunemaitre X, Hopkins PN, Hollenberg NK, Williams GH. Familial aggregation of low-renin hypertension. Hypertension. 2002;39(4):914–918. [DOI] [PubMed] [Google Scholar]
- 119. Zhang LN, Ji LD, Fei LJ, Yuan F, Zhang YM, Xu J. Association between polymorphisms of alpha-adducin gene and essential hypertension in Chinese population. BioMed Res Int. 2013;2013:451094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Beeks E, van der Klauw MM, Kroon AA, Spiering W, Fuss-Lejeune MJ, de Leeuw PW α-Adducin Gly460Trp polymorphism and renal hemodynamics in essential hypertension. Hypertension. 2004;44(4):419–423. [DOI] [PubMed] [Google Scholar]
- 121. Wang L, Chen S, Zhao Q, Hixson JE, Rao DC, Jaquish CE, Huang J, Lu X, Chen J, Cao J, Li J, Li H, He J, Liu DP, Gu D; GenSalt Collaborative Research Group. Association between genetic variants of the ADD1 and GNB3 genes and blood pressure response to the cold pressor test in a Chinese Han population: the GenSalt Study. Hypertens Res. 2012;35(8):805–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Morrison AC, Bray MS, Folsom AR, Boerwinkle E. ADD1 460W allele associated with cardiovascular disease in hypertensive individuals. Hypertension. 2002;39(6):1053–1057. [DOI] [PubMed] [Google Scholar]
- 123. Wang L, Zheng B, Zhao H, Du P, Sun A, Hua K, Gao Y. α-Adducin gene G614T polymorphisms in essential hypertension patients with high low density lipoprotein (LDL) levels. Indian J Med Res. 2014;139(2):273–278. [PMC free article] [PubMed] [Google Scholar]
- 124. Ishikawa K, Katsuya T, Sato N, Nakata Y, Takami S, Takiuchi S, Fu Y, Higaki J, Ogihara T. No association between α-adducin 460 polymorphism and essential hypertension in a Japanese population. Am J Hypertens. 1998;11(4 Pt 1):502–506. [DOI] [PubMed] [Google Scholar]
- 125. Kamitani A, Wong ZY, Fraser R, Davies DL, Connor JM, Foy CJ, Watt GC, Harrap SB. Human α-adducin gene, blood pressure, and sodium metabolism. Hypertension. 1998;32(1):138–143. [DOI] [PubMed] [Google Scholar]
- 126. Kato N, Sugiyama T, Nabika T, Morita H, Kurihara H, Yazaki Y, Yamori Y. Lack of association between the α-adducin locus and essential hypertension in the Japanese population. Hypertension. 1998;31(3):730–733. [DOI] [PubMed] [Google Scholar]
- 127. Ramu P, Umamaheswaran G, Shewade DG, Swaminathan RP, Balachander J, Adithan C. Gly460Trp polymorphism of the ADD1 gene and essential hypertension in an Indian population: a meta-analysis on hypertension risk. Indian J Hum Genet. 2010;16(1):8–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Niu WQ, Zhang Y, Ji KD, Gao PJ, Zhu DL. Lack of association between α-adducin G460W polymorphism and hypertension: evidence from a case-control study and a meta-analysis. J Hum Hypertens. 2010;24(7):467–474. [DOI] [PubMed] [Google Scholar]
- 129. Manunta P, Lavery G, Lanzani C, Braund PS, Simonini M, Bodycote C, Zagato L, Delli Carpini S, Tantardini C, Brioni E, Bianchi G, Samani NJ. Physiological interaction between α-adducin and WNK1-NEDD4L pathways on sodium-related blood pressure regulation. Hypertension. 2008;52(2):366–372. [DOI] [PubMed] [Google Scholar]
- 130. Tripodi G, Florio M, Ferrandi M, Modica R, Zimdahl H, Hubner N, Ferrari P, Bianchi G. Effect of Add1 gene transfer on blood pressure in reciprocal congenic strains of Milan rats. Biochem Biophys Res Commun. 2004;324(2):562–568. [DOI] [PubMed] [Google Scholar]
- 131. Gupta S, Chattopadhyaya I, Agrawal BK, Sehajpal PK, Goel RK. Correlation of renin angiotensin system (RAS) candidate gene polymorphisms with response to ramipril in patients with essential hypertension. J Postgrad Med. 2015;61(1):21–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Choi HD, Suh JH, Lee JY, Bae SK, Kang HE, Lee MG, Shin WG. Effects of ACE and ADD1 gene polymorphisms on blood pressure response to hydrochlorothiazide: a meta-analysis. Int J Clin Pharmacol Ther. 2013;51(9):718–724. [DOI] [PubMed] [Google Scholar]
- 133. Manglik A, Kobilka B. The role of protein dynamics in GPCR function: insights from the β2AR and rhodopsin. Curr Opin Cell Biol. 2014;27:136–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. De Léan A, Racz K, McNicoll N, Desrosiers ML. Direct β-adrenergic stimulation of aldosterone secretion in cultured bovine adrenal subcapsular cells. Endocrinology. 1984;115(2):485–492. [DOI] [PubMed] [Google Scholar]
- 135. Pratt JH, McAteer JA. Beta-adrenergic enhancement of angiotensin II-stimulated aldosterone secretion. Life Sci. 1989;44(26):2089–2095. [DOI] [PubMed] [Google Scholar]
- 136. Svetkey LP, Chen YT, McKeown SP, Preis L, Wilson AF. Preliminary evidence of linkage of salt sensitivity in black Americans at the β2-adrenergic receptor locus. Hypertension. 1997;29(4):918–922. [DOI] [PubMed] [Google Scholar]
- 137. Sun B, Williams JS, Svetkey LP, Kolatkar NS, Conlin PR β2-Adrenergic receptor genotype affects the renin-angiotensin-aldosterone system response to the Dietary Approaches to Stop Hypertension (DASH) dietary pattern. Am J Clin Nutr. 2010;92(2):444–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Komara M, Vasudevan R, Ismail P, Bakar SA, Pishva SR, Heidari F. Association of β2 adrenoceptor gene polymorphisms in Malaysian hypertensive subjects. Genet Mol Res. 2014;13(2):2939–2948. [DOI] [PubMed] [Google Scholar]
- 139. Liu Z, Qi H, Liu B, Liu K, Wu J, Cao H, Zhang J, Yan Y, He Y, Zhang L. Genetic susceptibility to salt-sensitive hypertension in a Han Chinese population: a validation study of candidate genes. Hypertens Res. 2017;40(10):876–884. [DOI] [PubMed] [Google Scholar]
- 140. Thomsen M, Dahl M, Tybjaerg-Hansen A, Nordestgaard BG. β2-Adrenergic receptor Thr164IIe polymorphism, blood pressure and ischaemic heart disease in 66 750 individuals. J Intern Med. 2012;271(3):305–314. [DOI] [PubMed] [Google Scholar]
- 141. Kawaguchi H, Masuo K, Katsuya T, Sugimoto K, Rakugi H, Ogihara T, Tuck ML. β2- and β3-Adrenoceptor polymorphisms relate to subsequent weight gain and blood pressure elevation in obese normotensive individuals. Hypertens Res. 2006;29(12):951–959. [DOI] [PubMed] [Google Scholar]
- 142. Masuo K, Katsuya T, Fu Y, Rakugi H, Ogihara T, Tuck ML β2- and β3-Adrenergic receptor polymorphisms are related to the onset of weight gain and blood pressure elevation over 5 years. Circulation. 2005;111(25):3429–3434. [DOI] [PubMed] [Google Scholar]
- 143. Vardeny O, Peppard PE, Finn LA, Faraco JH, Mignot E, Hla KM. β2 Adrenergic receptor polymorphisms and nocturnal blood pressure dipping status in the Wisconsin Sleep Cohort Study. J Am Soc Hypertens. 2011;5(2):114–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Hindorff LA, Heckbert SR, Psaty BM, Lumley T, Siscovick DS, Herrington DM, Edwards KL, Tracy RP β2-Adrenergic receptor polymorphisms and determinants of cardiovascular risk: the Cardiovascular Health Study. Am J Hypertens. 2005;18(3):392–397. [DOI] [PubMed] [Google Scholar]
- 145. Atia AE, Norsidah K, Nor Zamzila A, Rafidah Hanim M, Samsul D, Aznan MA, Rashidah AR, Norlelawati AT. Preliminary study on association of β2-adrenergic receptor polymorphism with hypertension in hypertensive subjects attending Balok Health Centre, Kuantan. Med J Malaysia. 2012;67(1):25–30. [PubMed] [Google Scholar]
- 146. Kumar R, Kohli S, Mishra A, Garg R, Alam P, Stobdan T, Nejatizadeh A, Gupta M, Tyagi S, Pasha MA. Interactions between the genes of vasodilatation pathways influence blood pressure and nitric oxide level in hypertension. Am J Hypertens. 2015;28(2):239–247. [DOI] [PubMed] [Google Scholar]
- 147. Anthony EG, Richard E, Lipkowitz MS, Bhatnagar V. Association of the ADRB2 (rs2053044) polymorphism and angiotensin-converting enzyme-inhibitor blood pressure response in the African American Study of Kidney Disease and Hypertension. Pharmacogenet Genomics. 2015;25(9):444–449. [DOI] [PubMed] [Google Scholar]
- 148. Baudrand R, Pojoga LH, Romero JR, Williams GH. Aldosterone’s mechanism of action: roles of lysine-specific demethylase 1, caveolin and striatin. Curr Opin Nephrol Hypertens. 2014;23(1):32–37. [DOI] [PubMed] [Google Scholar]
- 149. Konoshita T; Genomic Disease Outcome Consortium (G-DOC) Study Investigators. Do genetic variants of the renin-angiotensin system predict blood pressure response to renin-angiotensin system–blocking drugs?: a systematic review of pharmacogenomics in the renin-angiotensin system. Curr Hypertens Rep. 2011;13(5):356–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Iwai N, Kajimoto K, Tomoike H, Takashima N. Polymorphism of CYP11B2 determines salt sensitivity in Japanese. Hypertension. 2007;49(4):825–831. [DOI] [PubMed] [Google Scholar]
- 151. Rossi E, Regolisti G, Perazzoli F, Negro A, Davoli S, Nicoli D, Sani C, Casali B. -344C/T polymorphism of CYP11B2 gene in Italian patients with idiopathic low renin hypertension. Am J Hypertens. 2001;14(9 Pt 1):934–941. [DOI] [PubMed] [Google Scholar]
- 152. Cun Y, Li J, Tang W, Sheng X, Yu H, Zheng B, Xiao C. Association of WNK1 exon 1 polymorphisms with essential hypertension in Hani and Yi minorities of China. J Genet Genomics. 2011;38(4):165–171. [DOI] [PubMed] [Google Scholar]
- 153. Nejatizadeh A, Kumar R, Stobdan T, Goyal AK, Gupta M, Tyagi S, Jain SK, Pasha MA. CYP11B2 gene haplotypes independently and in concurrence with aldosterone and aldosterone to renin ratio increase the risk of hypertension. Clin Biochem. 2010;43(1–2):136–141. [DOI] [PubMed] [Google Scholar]
- 154. Vamsi UM, Swapna N, Padma G, Vishnupriya S, Padma T. Haplotype association and synergistic effect of human aldosterone synthase (CYP11B2) gene polymorphisms causing susceptibility to essential hypertension in Indian patients. Clin Exp Hypertens. 2016;38(8):659–665. [DOI] [PubMed] [Google Scholar]
- 155. Bogacz A, Bartkowiak-Wieczorek J, Procyk D, Seremak-Mrozikiewicz A, Majchrzycki M, Dziekan K, Bienert A, Czerny B. Analysis of the gene polymorphism of aldosterone synthase (CYP11B2) and atrial natriuretic peptide (ANP) in women with preeclampsia. Eur J Obstet Gynecol Reprod Biol. 2016;197:11–15. [DOI] [PubMed] [Google Scholar]
- 156. Hsiao CF, Sheu WW, Hung YJ, Lin MW, Curb D, Ranadex K, Quertermous T, Chen YM, Chen IY, Wu KD. The effects of the renin-angiotensin-aldosterone system gene polymorphisms on insulin resistance in hypertensive families. J Renin Angiotensin Aldosterone Syst. 2012;13(4):446–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Sia SK, Chiou HL, Chen SC, Tsai CF, Yang SF, Ueng KC. Distribution and phenotypic expression of mineralocorticoid receptor and CYP11B2 T-344C polymorphisms in a Taiwanese hypertensive population. Mol Biol Rep. 2013;40(5):3705–3711. [DOI] [PubMed] [Google Scholar]
- 158. Bellili NM, Foucan L, Fumeron F, Mohammedi K, Travert F, Roussel R, Balkau B, Tichet J, Marre M. Associations of the −344 T>C and the 3097 G>A polymorphisms of CYP11B2 gene with hypertension, type 2 diabetes, and metabolic syndrome in a French population. Am J Hypertens. 2010;23(6):660–667. [DOI] [PubMed] [Google Scholar]
- 159. Munshi A, Sharma V, Kaul S, Rajeshwar K, Babu MS, Shafi G, Anila AN, Balakrishna N, Alladi S, Jyothy A. Association of the −344C/T aldosterone synthase (CYP11B2) gene variant with hypertension and stroke. J Neurol Sci. 2010;296(1–2):34–38. [DOI] [PubMed] [Google Scholar]
- 160. Li X, Xie P, He J, Cai H, Yang R, Zhang Q, Li B, Qi W, Ma H. CYP11B2 gene polymorphism and essential hypertension among Tibetan, Dongxiang and Han populations from northwest of China. Clin Exp Hypertens. 2016;38(4):375–380. [DOI] [PubMed] [Google Scholar]
- 161. Sun J, Zhao M, Miao S, Xi B. Polymorphisms of three genes (ACE, AGT and CYP11B2) in the renin-angiotensin-aldosterone system are not associated with blood pressure salt sensitivity: a systematic meta-analysis. Blood Press. 2016;25(2):117–122. [DOI] [PubMed] [Google Scholar]
- 162. Zhang H, Li X, Zhou L, Zhang K, Zhang Q, Li J, Wang N, Jin M, Wu N, Cong M, Qiu C. A novel haplotype of low-frequency variants in the aldosterone synthase gene among northern Han Chinese with essential hypertension. Medicine (Baltimore). 2017;96(39):e8150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Todkar A, Di Chiara M, Loffing-Cueni D, Bettoni C, Mohaupt M, Loffing J, Wagner CA. Aldosterone deficiency adversely affects pregnancy outcome in mice. Pflugers Arch. 2012;464(4):331–343. [DOI] [PubMed] [Google Scholar]
- 164. Lee G, Makhanova N, Caron K, Lopez ML, Gomez RA, Smithies O, Kim HS. Homeostatic responses in the adrenal cortex to the absence of aldosterone in mice. Endocrinology. 2005;146(6):2650–2656. [DOI] [PubMed] [Google Scholar]
- 165. Fontana V, de Faria AP, Barbaro NR, Sabbatini AR, Modolo R, Lacchini R, Moreno H. Modulation of aldosterone levels by −344 C/T CYP11B2 polymorphism and spironolactone use in resistant hypertension. J Am Soc Hypertens. 2014;8(3):146–151. [DOI] [PubMed] [Google Scholar]
- 166. Rainey WE, Nakamura Y. Regulation of the adrenal androgen biosynthesis. J Steroid Biochem Mol Biol. 2008;108(3–5):281–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Baker ME, Nelson DR, Studer RA. Origin of the response to adrenal and sex steroids: roles of promiscuity and co-evolution of enzymes and steroid receptors. J Steroid Biochem Mol Biol. 2015;151:12–24. [DOI] [PubMed] [Google Scholar]
- 168. Newton-Cheh C, Johnson T, Gateva V, Tobin MD, Bochud M, Coin L, Najjar SS, Zhao JH, Heath SC, Eyheramendy S, Papadakis K, Voight BF, Scott LJ, Zhang F, Farrall M, Tanaka T, Wallace C, Chambers JC, Khaw KT, Nilsson P, van der Harst P, Polidoro S, Grobbee DE, Onland-Moret NC, Bots ML, Wain LV, Elliott KS, Teumer A, Luan J, Lucas G, Kuusisto J, Burton PR, Hadley D, McArdle WL, Brown M, Dominiczak A, Newhouse SJ, Samani NJ, Webster J, Zeggini E, Beckmann JS, Bergmann S, Lim N, Song K, Vollenweider P, Waeber G, Waterworth DM, Yuan X, Groop L, Orho-Melander M, Allione A, Di Gregorio A, Guarrera S, Panico S, Ricceri F, Romanazzi V, Sacerdote C, Vineis P, Barroso I, Sandhu MS, Luben RN, Crawford GJ, Jousilahti P, Perola M, Boehnke M, Bonnycastle LL, Collins FS, Jackson AU, Mohlke KL, Stringham HM, Valle TT, Willer CJ, Bergman RN, Morken MA, Döring A, Gieger C, Illig T, Meitinger T, Org E, Pfeufer A, Wichmann HE, Kathiresan S, Marrugat J, O’Donnell CJ, Schwartz SM, Siscovick DS, Subirana I, Freimer NB, Hartikainen AL, McCarthy MI, O’Reilly PF, Peltonen L, Pouta A, de Jong PE, Snieder H, van Gilst WH, Clarke R, Goel A, Hamsten A, Peden JF, Seedorf U, Syvänen AC, Tognoni G, Lakatta EG, Sanna S, Scheet P, Schlessinger D, Scuteri A, Dörr M, Ernst F, Felix SB, Homuth G, Lorbeer R, Reffelmann T, Rettig R, Völker U, Galan P, Gut IG, Hercberg S, Lathrop GM, Zelenika D, Deloukas P, Soranzo N, Williams FM, Zhai G, Salomaa V, Laakso M, Elosua R, Forouhi NG, Völzke H, Uiterwaal CS, van der Schouw YT, Numans ME, Matullo G, Navis G, Berglund G, Bingham SA, Kooner JS, Connell JM, Bandinelli S, Ferrucci L, Watkins H, Spector TD, Tuomilehto J, Altshuler D, Strachan DP, Laan M, Meneton P, Wareham NJ, Uda M, Jarvelin MR, Mooser V, Melander O, Loos RJ, Elliott P, Abecasis GR, Caulfield M, Munroe PB; Wellcome Trust Case Control Consortium. Genome-wide association study identifies eight loci associated with blood pressure. Nat Genet. 2009;41(6):666–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Levy D, Ehret GB, Rice K, Verwoert GC, Launer LJ, Dehghan A, Glazer NL, Morrison AC, Johnson AD, Aspelund T, Aulchenko Y, Lumley T, Köttgen A, Vasan RS, Rivadeneira F, Eiriksdottir G, Guo X, Arking DE, Mitchell GF, Mattace-Raso FU, Smith AV, Taylor K, Scharpf RB, Hwang SJ, Sijbrands EJ, Bis J, Harris TB, Ganesh SK, O’Donnell CJ, Hofman A, Rotter JI, Coresh J, Benjamin EJ, Uitterlinden AG, Heiss G, Fox CS, Witteman JC, Boerwinkle E, Wang TJ, Gudnason V, Larson MG, Chakravarti A, Psaty BM, van Duijn CM. Genome-wide association study of blood pressure and hypertension. Nat Genet. 2009;41(6):677–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Tabara Y, Kohara K, Kita Y, Hirawa N, Katsuya T, Ohkubo T, Hiura Y, Tajima A, Morisaki T, Miyata T, Nakayama T, Takashima N, Nakura J, Kawamoto R, Takahashi N, Hata A, Soma M, Imai Y, Kokubo Y, Okamura T, Tomoike H, Iwai N, Ogihara T, Inoue I, Tokunaga K, Johnson T, Caulfield M, Munroe P, Umemura S, Ueshima H, Miki T; Global Blood Pressure Genetics Consortium. Common variants in the ATP2B1 gene are associated with susceptibility to hypertension: the Japanese Millennium Genome Project. Hypertension. 2010;56(5):973–980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Liu C, Li H, Qi Q, Lu L, Gan W, Loos RJ, Lin X. Common variants in or near FGF5, CYP17A1 and MTHFR genes are associated with blood pressure and hypertension in Chinese Hans. J Hypertens. 2011;29(1):70–75. [DOI] [PubMed] [Google Scholar]
- 172. Li X, Ling Y, Lu D, Lu Z, Liu Y, Chen H, Gao X. Common polymorphism rs11191548 near the CYP17A1 gene is associated with hypertension and systolic blood pressure in the Han Chinese population. Am J Hypertens. 2013;26(4):465–472. [DOI] [PubMed] [Google Scholar]
- 173. Lin Y, Lai X, Chen B, Xu Y, Huang B, Chen Z, Zhu S, Yao J, Jiang Q, Huang H, Wen J, Chen G. Genetic variations in CYP17A1, CACNB2 and PLEKHA7 are associated with blood pressure and/or hypertension in She ethnic minority of China. Atherosclerosis. 2011;219(2):709–714. [DOI] [PubMed] [Google Scholar]
- 174. Xi B, Shen Y, Zhao X, Chandak GR, Cheng H, Hou D, Li Y, Ott J, Zhang Y, Wang X, Mi J. Association of common variants in/near six genes (ATP2B1, CSK, MTHFR, CYP17A1, STK39 and FGF5) with blood pressure/hypertension risk in Chinese children. J Hum Hypertens. 2014;28(1):32–36. [DOI] [PubMed] [Google Scholar]
- 175. Yanagisawa M, Kurihara H, Kimura S, Tomobe Y, Kobayashi M, Mitsui Y, Yazaki Y, Goto K, Masaki T. A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature. 1988;332(6163):411–415. [DOI] [PubMed] [Google Scholar]
- 176. Rossi GP, Sacchetto A, Cesari M, Pessina AC. Interactions between endothelin-1 and the renin–angiotensin–aldosterone system. Cardiovasc Res. 1999;43(2):300–307. [DOI] [PubMed] [Google Scholar]
- 177. Greenberg BH. Endothelin and endothelin receptor antagonists in heart failure. Congest Heart Fail. 2002;8(5):257–261. [DOI] [PubMed] [Google Scholar]
- 178. Asai T, Ohkubo T, Katsuya T, Higaki J, Fu Y, Fukuda M, Hozawa A, Matsubara M, Kitaoka H, Tsuji I, Araki T, Satoh H, Hisamichi S, Imai Y, Ogihara T. Endothelin-1 gene variant associates with blood pressure in obese Japanese subjects: the Ohasama Study. Hypertension. 2001;38(6):1321–1324. [DOI] [PubMed] [Google Scholar]
- 179. Letizia C, Cerci S, De Toma G, D’Ambrosio C, De Ciocchis A, Coassin S, Scavo D. High plasma endothelin-1 levels in hypertensive patients with low-renin essential hypertension. J Hum Hypertens. 1997;11(7):447–451. [DOI] [PubMed] [Google Scholar]
- 180. Tan JW, Gupta T, Manosroi W, Yao TM, Hopkins PN, Williams JS, Adler GK, Romero JR, Williams GH. Dysregulated aldosterone secretion in persons of African descent with endothelin-1 gene variants. JCI Insight. 2017;2(23):95992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Panoulas VF, Douglas KM, Smith JP, Taffé P, Stavropoulos-Kalinoglou A, Toms TE, Elisaf MS, Nightingale P, Kitas GD. Polymorphisms of the endothelin-1 gene associate with hypertension in patients with rheumatoid arthritis. Endothelium. 2008;15(4):203–212. [DOI] [PubMed] [Google Scholar]
- 182. Tiret L, Poirier O, Hallet V, McDonagh TA, Morrison C, McMurray JJ, Dargie HJ, Arveiler D, Ruidavets JB, Luc G, Evans A, Cambien F. The Lys198Asn polymorphism in the endothelin-1 gene is associated with blood pressure in overweight people. Hypertension. 1999;33(5):1169–1174. [DOI] [PubMed] [Google Scholar]
- 183. Aggarwal PK, Jain V, Srinivasan R, Jha V. Maternal EDN1 G5665T polymorphism influences circulating endothelin-1 levels and plays a role in determination of preeclampsia phenotype. J Hypertens. 2009;27(10):2044–2050. [DOI] [PubMed] [Google Scholar]
- 184. Fang Z, Li M, Ma Z, Tu G. Association of endothelin-1 gene polymorphisms with essential hypertension in a Chinese population. Genet Mol Res. 2017;16(3). [DOI] [PubMed] [Google Scholar]
- 185. Ahmed M, Rghigh A. Polymorphism in endothelin-1 gene: an overview. Curr Clin Pharmacol. 2016;11(3):191–210. [DOI] [PubMed] [Google Scholar]
- 186. Banno M, Hanada H, Kamide K, Kokubo Y, Kada A, Yang J, Tanaka C, Takiuchi S, Horio T, Matayoshi T, Yasuda H, Nagura J, Tomoike H, Kawano Y, Miyata T. Association of genetic polymorphisms of endothelin-converting enzyme-1 gene with hypertension in a Japanese population and rare missense mutation in preproendothelin-1 in Japanese hypertensives. Hypertens Res. 2007;30(6):513–520. [DOI] [PubMed] [Google Scholar]
- 187. Ikeda T, Ohta H, Okada M, Kawai N, Nakao R, Siegl PK, Kobayashi T, Maeda S, Miyauchi T, Nishikibe M. Pathophysiological roles of endothelin-1 in Dahl salt-sensitive hypertension. Hypertension. 1999;34(3):514–519. [DOI] [PubMed] [Google Scholar]
- 188. Rothermund L, Luckert S, Kossmehl P, Paul M, Kreutz R. Renal endothelin ETA/ETB receptor imbalance differentiates salt-sensitive from salt-resistant spontaneous hypertension. Hypertension. 2001;37(2):275–280. [DOI] [PubMed] [Google Scholar]
- 189. Kisanuki YY, Emoto N, Ohuchi T, Widyantoro B, Yagi K, Nakayama K, Kedzierski RM, Hammer RE, Yanagisawa H, Williams SC, Richardson JA, Suzuki T, Yanagisawa M. Low blood pressure in endothelial cell–specific endothelin 1 knockout mice. Hypertension. 2010;56(1):121–128. [DOI] [PubMed] [Google Scholar]
- 190. Imamov O, Shim GJ, Warner M, Gustafsson JA. Estrogen receptor β in health and disease. Biol Reprod. 2005;73(5):866–871. [DOI] [PubMed] [Google Scholar]
- 191. Cooke PS, Nanjappa MK, Ko C, Prins GS, Hess RA. Estrogens in male physiology. Physiol Rev. 2017;97(3):995–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192. Peter I, Shearman AM, Zucker DR, Schmid CH, Demissie S, Cupples LA, Larson MG, Vasan RS, D’Agostino RB, Karas RH, Mendelsohn ME, Housman DE, Levy D. Variation in estrogen-related genes and cross-sectional and longitudinal blood pressure in the Framingham Heart Study. J Hypertens. 2005;23(12):2193–2200. [DOI] [PubMed] [Google Scholar]
- 193. Chen C, Li Y, Chen F, Pan H, Shen H, Sun Z, Wu Y, Zhou J, Ba L, Zhao J. Estrogen receptor beta genetic variants and combined oral contraceptive use as relates to the risk of hypertension in Chinese women. Arch Med Res. 2010;41(8):599–605. [DOI] [PubMed] [Google Scholar]
- 194. Manosroi W, Tan JW, Rariy CM, Sun B, Goodarzi MO, Saxena AR, Williams JS, Pojoga LH, Lasky-Su J, Cui J, Guo X, Taylor KD, Chen YI, Xiang AH, Hsueh WA, Raffel LJ, Buchanan TA, Rotter JI, Williams GH, Seely EW. The association of estrogen receptor-β gene variation with salt-sensitive blood pressure. J Clin Endocrinol Metab. 2017;102(11):4124–4135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195. Iwai N, Tago N, Yasui N, Kokubo Y, Inamoto N, Tomoike H, Shioji K. Genetic analysis of 22 candidate genes for hypertension in the Japanese population. J Hypertens. 2004;22(6):1119–1126. [DOI] [PubMed] [Google Scholar]
- 196. Zhu Y, Bian Z, Lu P, Karas RH, Bao L, Cox D, Hodgin J, Shaul PW, Thoren P, Smithies O, Gustafsson JA, Mendelsohn ME. Abnormal vascular function and hypertension in mice deficient in estrogen receptorβ. Science. 2002;295(5554):505–508. [DOI] [PubMed] [Google Scholar]
- 197. Arias-Loza PA, Hu K, Dienesch C, Mehlich AM, König S, Jazbutyte V, Neyses L, Hegele-Hartung C, Heinrich Fritzemeier K, Pelzer T. Both estrogen receptor subtypes, α and β, attenuate cardiovascular remodeling in aldosterone salt-treated rats. Hypertension. 2007;50(2):432–438. [DOI] [PubMed] [Google Scholar]
- 198. Shi Y, Lan F, Matson C, Mulligan P, Whetstine JR, Cole PA, Casero RA, Shi Y. Histone demethylation mediated by the nuclear amine oxidase homolog LSD1. Cell. 2004;119(7):941–953. [DOI] [PubMed] [Google Scholar]
- 199. Lan F, Nottke AC, Shi Y. Mechanisms involved in the regulation of histone lysine demethylases. Curr Opin Cell Biol. 2008;20(3):316–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Williams JS, Chamarthi B, Goodarzi MO, Pojoga LH, Sun B, Garza AE, Raby BA, Adler GK, Hopkins PN, Brown NJ, Jeunemaitre X, Ferri C, Fang R, Leonor T, Cui J, Guo X, Taylor KD, Ida Chen YD, Xiang A, Raffel LJ, Buchanan TA, Rotter JI, Williams GH, Shi Y. Lysine-specific demethylase 1: an epigenetic regulator of salt-sensitive hypertension. Am J Hypertens. 2012;25(7):812–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201. Krug AW, Tille E, Sun B, Pojoga L, Williams J, Chamarthi B, Lichtman AH, Hopkins PN, Adler GK, Williams GH. Lysine-specific demethylase-1 modifies the age effect on blood pressure sensitivity to dietary salt intake. Age (Dordr). 2013;35(5):1809–1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Pojoga LH, Williams JS, Yao TM, Kumar A, Raffetto JD, do Nascimento GR, Reslan OM, Adler GK, Williams GH, Shi Y, Khalil RA. Histone demethylase LSD1 deficiency during high-salt diet is associated with enhanced vascular contraction, altered NO-cGMP relaxation pathway, and hypertension. Am J Physiol Heart Circ Physiol. 2011;301(5):H1862–H1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Chen SY, Bhargava A, Mastroberardino L, Meijer OC, Wang J, Buse P, Firestone GL, Verrey F, Pearce D. Epithelial sodium channel regulated by aldosterone-induced protein sgk. Proc Natl Acad Sci USA. 1999;96(5):2514–2519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Lang F, Böhmer C, Palmada M, Seebohm G, Strutz-Seebohm N, Vallon V. (Patho)physiological significance of the serum- and glucocorticoid-inducible kinase isoforms. Physiol Rev. 2006;86(4):1151–1178. [DOI] [PubMed] [Google Scholar]
- 205. Lou Y, Zhang F, Luo Y, Wang L, Huang S, Jin F. Serum and glucocorticoid regulated kinase 1 in sodium homeostasis. Int J Mol Sci. 2016;17(8):E1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Rao AD, Sun B, Saxena A, Hopkins PN, Jeunemaitre X, Brown NJ, Adler GK, Williams JS. Polymorphisms in the serum- and glucocorticoid-inducible kinase 1 gene are associated with blood pressure and renin response to dietary salt intake. J Hum Hypertens. 2013;27(3):176–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Zhang D, Gu D, He J, Hixson JE, Rao DC, Li C, He H, Chen J, Huang J, Chen J, Rice TK, Chen S, Kelly TN. Associations of the serum/glucocorticoid regulated kinase genes with BP changes and hypertension incidence: the Gensalt Study. Am J Hypertens. 2017;30(1):95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208. Chu C, Wang Y, Wang M, Mu JJ, Liu FQ, Wang L, Ren KY, Wang D, Yuan ZY. Common variants in serum/glucocorticoid regulated kinase 1 (SGK1) and blood pressure responses to dietary sodium or potassium interventions: a family-based association study. Kidney Blood Press Res. 2015;40(4):424–434. [DOI] [PubMed] [Google Scholar]
- 209. Wulff P, Vallon V, Huang DY, Völkl H, Yu F, Richter K, Jansen M, Schlünz M, Klingel K, Loffing J, Kauselmann G, Bösl MR, Lang F, Kuhl D. Impaired renal Na+ retention in the sgk1-knockout mouse. J Clin Invest. 2002;110(9):1263–1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210. De Mello WC. Local renin angiotensin aldosterone systems and cardiovascular diseases. Med Clin North Am. 2017;101(1):117–127. [DOI] [PubMed] [Google Scholar]
- 211. Song GG, Bae SC, Kim JH, Lee YH. The angiotensin-converting enzyme insertion/deletion polymorphism and susceptibility to rheumatoid arthritis, vitiligo and psoriasis: a meta-analysis. J Renin Angiotensin Aldosterone Syst. 2015;16(1):195–202. [DOI] [PubMed] [Google Scholar]
- 212. Hollenberg NK, Williams GH. The renal response to converting enzyme inhibition and the treatment of sodium-sensitive hypertension. Clin Exp Hypertens A. 1987;9(2–3):531–541. [DOI] [PubMed] [Google Scholar]
- 213. Bavishi C, Bangalore S, Messerli FH. Renin angiotensin aldosterone system inhibitors in hypertension: is there evidence for benefit independent of blood pressure reduction? Prog Cardiovasc Dis. 2016;59(3):253–261. [DOI] [PubMed] [Google Scholar]
- 214. Wong PY, Talamo RC, Williams GH, Colman RW. Response of the kallikrein-kinin and renin-angiotensin systems to saline infusion and upright posture. J Clin Invest. 1975;55(4):691–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215. Zhang L, Miyaki K, Araki J, Song Y, Kimura T, Omae K,Muramatsu M. Interaction of angiotensin I-converting enzyme insertion-deletion polymorphism and daily salt intake influences hypertension in Japanese men. Hypertens Res. 2006;29(10):751–758. [DOI] [PubMed] [Google Scholar]
- 216. Das M, Pal S, Ghosh A. Angiotensin converting enzyme gene polymorphism (insertion/deletion) and hypertension in adult Asian Indians: a population-based study from Calcutta, India. Hum Biol. 2008;80(3):303–312. [DOI] [PubMed] [Google Scholar]
- 217. Caprioli J, Mele C, Mossali C, Gallizioli L, Giacchetti G, Noris M, Remuzzi G, Benigni A. Polymorphisms of EDNRB, ATG, and ACE genes in salt-sensitive hypertension. Can J Physiol Pharmacol. 2008;86(8):505–510. [DOI] [PubMed] [Google Scholar]
- 218. Ramachandran V, Ismail P, Stanslas J, Shamsudin N, Moin S, Mohd Jas R. Association of insertion/deletion polymorphism of angiotensin-converting enzyme gene with essential hypertension and type 2 diabetes mellitus in Malaysian subjects. J Renin Angiotensin Aldosterone Syst. 2008;9(4):208–214. [DOI] [PubMed] [Google Scholar]
- 219. Mandò C, Antonazzo P, Tabano S, Zanutto S, Pileri P, Somigliana E, Colleoni F, Martinelli A, Zolin A, Benedetto C, Marozio L, Neri I, Facchinetti F, Miozzo M, Cetin I. Angiotensin-converting enzyme and adducin-1 polymorphisms in women with preeclampsia and gestational hypertension. Reprod Sci. 2009;16(9):819–826. [DOI] [PubMed] [Google Scholar]
- 220. Miao HW, Gong H. Correlation of ACE gene deletion/insertion polymorphism and risk of pregnancy-induced hypertension: a meta-analysis based on 10,236 subjects. J Renin Angiotensin Aldosterone Syst. 2015;16(4):982–994. [DOI] [PubMed] [Google Scholar]
- 221. He J, Bian Y, Gao F, Li M, Qiu L, Wu W, Zhou H, Liu G, Xiao C. RNA interference targeting the ACE gene reduced blood pressure and improved myocardial remodelling in SHRs. Clin Sci (Lond). 2009;116(3):249–255. [DOI] [PubMed] [Google Scholar]
- 222. Heidari F, Vasudevan R, Mohd Ali SZ, Ismail P, Etemad A, Pishva SR, Othman F, Abu Bakar S. Association of insertion/deletion polymorphism of angiotensin-converting enzyme gene among Malay male hypertensive subjects in response to ACE inhibitors. J Renin Angiotensin Aldosterone Syst. 2015;16(4):872–879. [DOI] [PubMed] [Google Scholar]
- 223. Katori M, Majima M. Pivotal role of renal kallikrein-kinin system in the development of hypertension and approaches to new drugs based on this relationship. Jpn J Pharmacol. 1996;70(2):95–128. [DOI] [PubMed] [Google Scholar]
- 224. Braun A, Maier E, Kammerer S, Müller B, Roscher AA. A novel sequence polymorphism in the promoter region of the human B2-bradykinin receptor gene. Hum Genet. 1996;97(5):688–689. [DOI] [PubMed] [Google Scholar]
- 225. Gu D, Zhao Q, Kelly TN, Hixson JE, Rao DC, Cao J, Chen J, Li J, Chen J, Ji X, Hu D, Wang X, Liu DP, He J. The role of the kallikrein-kinin system genes in the salt sensitivity of blood pressure: the GenSalt Study. Am J Epidemiol. 2012;176(Suppl 7):S72–S80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226. Gainer JV, Brown NJ, Bachvarova M, Bastien L, Maltais I, Marceau F, Bachvarov DR. Altered frequency of a promoter polymorphism of the kinin B2 receptor gene in hypertensive African-Americans. Am J Hypertens. 2000;13(12):1268–1273. [DOI] [PubMed] [Google Scholar]
- 227. Bhupatiraju C, Patkar S, Pandharpurkar D, Joshi S, Tirunilai P. Association and interaction of −58C>T and ±9 bp polymorphisms of BDKRB2 gene causing susceptibility to essential hypertension. Clin Exp Hypertens. 2012;34(3):230–235. [DOI] [PubMed] [Google Scholar]
- 228. Fu Y, Katsuya T, Matsuo A, Yamamoto K, Akasaka H, Takami Y, Iwashima Y, Sugimoto K, Ishikawa K, Ohishi M, Rakugi H, Ogihara T. Relationship of bradykinin B2 receptor gene polymorphism with essential hypertension and left ventricular hypertrophy. Hypertens Res. 2004;27(12):933–938. [DOI] [PubMed] [Google Scholar]
- 229. Kopkan L, Husková Z, Jíchová Š, Červenková L, Červenka L, Saifudeen Z, El-Dahr SS. Conditional knockout of collecting duct bradykinin B2 receptors exacerbates angiotensin II-induced hypertension during high salt intake. Clin Exp Hypertens. 2016;38(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230. Virkki LV, Wilson DA, Vaughan-Jones RD, Boron WF. Functional characterization of human NBC4 as an electrogenic Na+-HCO3− cotransporter (NBCe2). Am J Physiol Cell Physiol. 2002;282(6):C1278–C1289. [DOI] [PubMed] [Google Scholar]
- 231. Sassani P, Pushkin A, Gross E, Gomer A, Abuladze N, Dukkipati R, Carpenito G, Kurtz I. Functional characterization of NBC4: a new electrogenic sodium-bicarbonate cotransporter. Am J Physiol Cell Physiol. 2002;282(2):C408–C416. [DOI] [PubMed] [Google Scholar]
- 232. Gildea JJ, Xu P, Kemp BA, Carlson JM, Tran HT, Bigler Wang D, Langouët-Astrié CJ, McGrath HE, Carey RM, Jose PA, Felder RA. Sodium bicarbonate cotransporter NBCe2 gene variants increase sodium and bicarbonate transport in human renal proximal tubule cells. PLoS One. 2018;13(4):e0189464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233. Carey RM, Schoeffel CD, Gildea JJ, Jones JE, McGrath HE, Gordon LN, Park MJ, Sobota RS, Underwood PC, Williams J, Sun B, Raby B, Lasky-Su J, Hopkins PN, Adler GK, Williams SM, Jose PA, Felder RA. Salt sensitivity of blood pressure is associated with polymorphisms in the sodium-bicarbonate cotransporter. Hypertension. 2012;60(5):1359–1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234. Barkley RA, Chakravarti A, Cooper RS, Ellison RC, Hunt SC, Province MA, Turner ST, Weder AB, Boerwinkle E; Family Blood Pressure Program. Positional identification of hypertension susceptibility genes on chromosome 2. Hypertension. 2004;43(2):477–482. [DOI] [PubMed] [Google Scholar]
- 235. Wen D, Yuan Y, Warner PC, Wang B, Cornelius RJ, Wang-France J, Li H, Boettger T, Sansom SC. Increased epithelial sodium channel activity contributes to hypertension caused by Na+-HCO3− cotransporter electrogenic 2 deficiency. Hypertension. 2015;66(1):68–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236. Hirawa N, Fujiwara A, Umemura S. ATP2B1 and blood pressure: from associations to pathophysiology. Curr Opin Nephrol Hypertens. 2013;22(2):177–184. [DOI] [PubMed] [Google Scholar]
- 237. Lee S, Kim SH, Shin C. Interaction according to urinary sodium excretion level on the association between ATP2B1 rs17249754 and incident hypertension: the Korean genome epidemiology study. Clin Exp Hypertens. 2016;38(4):352–358. [DOI] [PubMed] [Google Scholar]
- 238. Xu J, Qian HX, Hu SP, Liu LY, Zhou M, Feng M, Su J, Ji LD. Gender-specific association of ATP2B1 variants with susceptibility to essential hypertension in the Han Chinese population. BioMed Res Int. 2016;2016:1910565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239. Wang Y, Zhang Y, Li Y, Zhou X, Wang X, Gao P, Jin L, Zhang X, Zhu D. Common variants in the ATP2B1 gene are associated with hypertension and arterial stiffness in Chinese population. Mol Biol Rep. 2013;40(2):1867–1873. [DOI] [PubMed] [Google Scholar]
- 240. Shin YB, Lim JE, Ji SM, Lee HJ, Park SY, Hong KW, Lim M, McCarthy MI, Lee YH, Oh B. Silencing of Atp2b1 increases blood pressure through vasoconstriction. J Hypertens. 2013;31(8):1575–1583. [DOI] [PubMed] [Google Scholar]
- 241. Fujiwara A, Hirawa N, Fujita M, Kobayashi Y, Okuyama Y, Yatsu K, Katsumata M, Yamamoto Y, Ichihara N, Saka S, Toya Y, Yasuda G, Goshima Y, Tabara Y, Miki T, Ueshima H, Ishikawa Y, Umemura S. Impaired nitric oxide production and increased blood pressure in systemic heterozygous ATP2B1 null mice. J Hypertens. 2014;32(7):1415–1423. [DOI] [PubMed] [Google Scholar]
- 242. Kobayashi Y, Hirawa N, Tabara Y, Muraoka H, Fujita M, Miyazaki N, Fujiwara A, Ichikawa Y, Yamamoto Y, Ichihara N, Saka S, Wakui H, Yoshida S, Yatsu K, Toya Y, Yasuda G, Kohara K, Kita Y, Takei K, Goshima Y, Ishikawa Y, Ueshima H, Miki T, Umemura S. Mice lacking hypertension candidate gene ATP2B1 in vascular smooth muscle cells show significant blood pressure elevation. Hypertension. 2012;59(4):854–860. [DOI] [PubMed] [Google Scholar]
- 243. Wang Y, O’Connell JR, McArdle PF, Wade JB, Dorff SE, Shah SJ, Shi X, Pan L, Rampersaud E, Shen H, Kim JD, Subramanya AR, Steinle NI, Parsa A, Ober CC, Welling PA, Chakravarti A, Weder AB, Cooper RS, Mitchell BD, Shuldiner AR, Chang YP. Whole-genome association study identifies STK39 as a hypertension susceptibility gene. Proc Natl Acad Sci USA. 2009;106(1):226–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244. Delpire E, Gagnon KB. SPAK and OSR1: STE20 kinases involved in the regulation of ion homoeostasis and volume control in mammalian cells. Biochem J. 2008;409(2):321–331. [DOI] [PubMed] [Google Scholar]
- 245. Moriguchi T, Urushiyama S, Hisamoto N, Iemura S, Uchida S, Natsume T, Matsumoto K, Shibuya H. WNK1 regulates phosphorylation of cation-chloride-coupled cotransporters via the STE20-related kinases, SPAK and OSR1. J Biol Chem. 2005;280(52):42685–42693. [DOI] [PubMed] [Google Scholar]
- 246. Rhee MY, Yang SJ, Oh SW, Park Y, Kim CI, Park HK, Park Cy. Novel genetic variations associated with salt sensitivity in the Korean population. Hypertens Res. 2011;34(5):606–611. [DOI] [PubMed] [Google Scholar]
- 247. Persu A, Evenepoel L, Jin Y, Mendola A, Ngueta G, Yang WY, Gruson D, Horman S, Staessen JA, Vikkula M; BELHYPGEN Consortium. STK39 and WNK1 are potential hypertension susceptibility genes in the BELHYPGEN Cohort. Medicine (Baltimore). 2016;95(15):e2968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248. Zhao H, Qi Y, Wang Y, Wang Y, Lu C, Xiao Y, Wang B, Niu W. Interactive contribution of serine/threonine kinase 39 gene multiple polymorphisms to hypertension among northeastern Han Chinese. Sci Rep. 2014;4(1):5116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249. Umedani LV, Chaudhry B, Mehraj V, Ishaq M. Serene threonine kinase 39 gene single nucleotide A-G polymorphism rs35929607 is weakly associated with essential hypertension in population of Tharparkar, Pakistan. J Pak Med Assoc. 2013;63(2):199–205. [PubMed] [Google Scholar]
- 250. Fava C, Danese E, Montagnana M, Sjögren M, Almgren P, Engström G, Nilsson P, Hedblad B, Guidi GC, Minuz P, Melander O. Serine/threonine kinase 39 is a candidate gene for primary hypertension especially in women: results from two cohort studies in Swedes. J Hypertens. 2011;29(3):484–491. [DOI] [PubMed] [Google Scholar]
- 251. Shin DJ, Lee SH, Park S, Jang Y. Association between serine/threonine kinase 39 gene polymorphism, hypertension, and other cardiovascular risk factors in Koreans. Korean Circ J. 2013;43(1):13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252. Xu J, Ji LD, Zhang LN, Dong CZ, Fei LJ, Hua S, Tsai JY, Zhang YP. Lack of association between STK39 and hypertension in the Chinese population. J Hum Hypertens. 2013;27(5):294–297. [DOI] [PubMed] [Google Scholar]
- 253. Duarte JD, Lobmeyer MT, Wang Z, Chapman AB, Gums JG, Langaee TY, Boerwinkle E, Turner ST, Johnson JA. Lack of association between polymorphisms in STK39, a putative thiazide response gene, and blood pressure response to hydrochlorothiazide. Pharmacogenet Genomics. 2010;20(8):516–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254. Donner KM, Hiltunen TP, Hannila-Handelberg T, Suonsyrjä T, Kontula K. STK39 variation predicts the ambulatory blood pressure response to losartan in hypertensive men. Hypertens Res. 2012;35(1):107–114. [DOI] [PubMed] [Google Scholar]
- 255. Xu BE, Lee BH, Min X, Lenertz L, Heise CJ, Stippec S, Goldsmith EJ, Cobb MH. WNK1: analysis of protein kinase structure, downstream targets, and potential roles in hypertension. Cell Res. 2005;15(1):6–10. [DOI] [PubMed] [Google Scholar]
- 256. Wilson FH, Disse-Nicodème S, Choate KA, Ishikawa K, Nelson-Williams C, Desitter I, Gunel M, Milford DV, Lipkin GW, Achard JM, Feely MP, Dussol B, Berland Y, Unwin RJ, Mayan H, Simon DB, Farfel Z, Jeunemaitre X, Lifton RP. Human hypertension caused by mutations in WNK kinases. Science. 2001;293(5532):1107–1112. [DOI] [PubMed] [Google Scholar]
- 257. Frey MK, Dao F, Olvera N, Konner JA, Dickler MN, Levine DA. Genetic predisposition to bevacizumab-induced hypertension. Gynecol Oncol. 2017;147(3):621–625. [DOI] [PubMed] [Google Scholar]
- 258. Liu F, Lian Q, Ren J, Ren K, Wang Y, Wang D, Chu C, Wang L, Guo T, Liu E, Mu J, Yuan Z. Lack of family-based association between common variations in WNK1 and blood pressure level. Med Sci Monit. 2014;20:1958–1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259. Zambrowicz BP, Abuin A, Ramirez-Solis R, Richter LJ, Piggott J, BeltrandelRio H, Buxton EC, Edwards J, Finch RA, Friddle CJ, Gupta A, Hansen G, Hu Y, Huang W, Jaing C, Key BW Jr, Kipp P, Kohlhauff B, Ma ZQ, Markesich D, Payne R, Potter DG, Qian N, Shaw J, Schrick J, Shi ZZ, Sparks MJ, Van Sligtenhorst I, Vogel P, Walke W, Xu N, Zhu Q, Person C, Sands AT. Wnk1 kinase deficiency lowers blood pressure in mice: a gene-trap screen to identify potential targets for therapeutic intervention. Proc Natl Acad Sci USA. 2003;100(24):14109–14114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260. Turner ST, Schwartz GL, Chapman AB, Boerwinkle E. WNK1 kinase polymorphism and blood pressure response to a thiazide diuretic. Hypertension. 2005;46(4):758–765. [DOI] [PubMed] [Google Scholar]
- 261. Catt KJ, Mendelsohn FA, Millan MA, Aguilera G. The role of angiotensin II receptors in vascular regulation. J Cardiovasc Pharmacol. 1984;6(Suppl 4):S575–S586. [DOI] [PubMed] [Google Scholar]
- 262. Higuchi S, Ohtsu H, Suzuki H, Shirai H, Frank GD, Eguchi S. Angiotensin II signal transduction through the AT1 receptor: novel insights into mechanisms and pathophysiology. Clin Sci (Lond). 2007;112(8):417–428. [DOI] [PubMed] [Google Scholar]
- 263. Henderson SO, Haiman CA, Mack W. Multiple polymorphisms in the renin- angiotensin-aldosterone system (ACE, CYP11B2, AGTR1) and their contribution to hypertension in African Americans and Latinos in the multiethnic cohort. Am J Med Sci. 2004;328(5):266–273. [DOI] [PubMed] [Google Scholar]
- 264. Chandra S, Narang R, Sreenivas V, Bhatia J, Saluja D, Srivastava K. Association of angiotensin II type 1 receptor (A1166C) gene polymorphism and its increased expression in essential hypertension: a case-control study. PLoS One. 2014;9(7):e101502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265. Jinmin L, Jianmin L, Shuqin Z, Xueqiu L, Shuyi T. The polymorphism of angiotensin-receptor gene A1166C in familial hypertension and its distribution in the Han Yellow race of China. Saudi Med J. 2013;34(10):1007–1012. [PubMed] [Google Scholar]
- 266. Shahin DS, Irshaid YM, Saleh AA. The A1166C polymorphism of the AT1R gene is associated with an early onset of hypertension and high waist circumference in Jordanian males attending the Jordan University Hospital. Clin Exp Hypertens. 2014;36(5):333–339. [DOI] [PubMed] [Google Scholar]
- 267. Kooffreh ME, Anumudu CI, Duke R, Okpako EC, Kumar PL. Angiotensin II type 1 receptor A1166C gene polymorphism and essential hypertension in Calabar and Uyo cities, Nigeria. Indian J Hum Genet. 2013;19(2):213–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268. Jain S, Prater A, Pandey V, Rana A, Puri N, Kumar A. A haplotype of angiotensin receptor type 1 associated with human hypertension increases blood pressure in transgenic mice. J Biol Chem. 2013;288(52):37048–37056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269. Gong HT, Ma XL, Chen BX, Xu XY, Li Q, Guo CX, Du FH. Polymorphisms of the angiotensin II type 1 receptor gene affect antihypertensive response to angiotensin receptor blockers in hypertensive Chinese. Genet Mol Res. 2013;12(2):2068–2075. [DOI] [PubMed] [Google Scholar]
- 270. Kurland L, Hallberg P, Melhus H, Liljedahl U, Hashemi N, Syvänen AC, Lind L, Kahan T. The relationship between the plasma concentration of irbesartan and the antihypertensive response is disclosed by an angiotensin II type 1 receptor polymorphism: results from the Swedish Irbesartan Left Ventricular Hypertrophy Investigation vs. Atenolol (SILVHIA) Trial. Am J Hypertens. 2008;21(7):836–839. [DOI] [PubMed] [Google Scholar]
- 271. Zhan X, Bates B, Hu XG, Goldfarb M. The human FGF-5 oncogene encodes a novel protein related to fibroblast growth factors. Mol Cell Biol. 1988;8(8):3487–3495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272. Hanaka H, Hamada T, Ito M, Nakashima H, Tomita K, Seki S, Kobayashi Y, Imaki J. Fibroblast growth factor-5 participates in the progression of hepatic fibrosis. Exp Anim. 2014;63(1):85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273. Takeuchi F, Isono M, Katsuya T, Yamamoto K, Yokota M, Sugiyama T, Nabika T, Fujioka A, Ohnaka K, Asano H, Yamori Y, Yamaguchi S, Kobayashi S, Takayanagi R, Ogihara T, Kato N. Blood pressure and hypertension are associated with 7 loci in the Japanese population. Circulation. 2010;121(21):2302–2309. [DOI] [PubMed] [Google Scholar]
- 274. Niu W, Zhang Y, Ji K, Gu M, Gao P, Zhu D. Confirmation of top polymorphisms in hypertension genome wide association study among Han Chinese. Clin Chim Acta. 2010;411(19–20):1491–1495. [DOI] [PubMed] [Google Scholar]
- 275. Li J, Shi J, Huang W, Sun J, Wu Y, Duan Q, Luo J, Lange LA, Gordon-Larsen P, Zheng SL, Yuan W, Wang Y, Popkin BM, Mo Z, Xu J, Du S, Mohlke KL, Lange EM. Variant mear FGF5 has stronger effects on blood pressure in chinese with a higher body mass index. Am J Hypertens. 2015;28(8):1031–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276. Xi B, Shen Y, Reilly KH, Wang X, Mi J. Recapitulation of four hypertension susceptibility genes (CSK, CYP17A1, MTHFR, and FGF5) in East Asians. Metabolism. 2013;62(2):196–203. [DOI] [PubMed] [Google Scholar]
- 277. Oldham WM, Hamm HE. Heterotrimeric G protein activation by G-protein-coupled receptors. Nat Rev Mol Cell Biol. 2008;9(1):60–71. [DOI] [PubMed] [Google Scholar]
- 278. Tesmer JJ. The quest to understand heterotrimeric G protein signaling. Nat Struct Mol Biol. 2010;17(6):650–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279. El Din Hemimi NS, Mansour AA, Abdelsalam MM. Prediction of the risk for essential hypertension among carriers of C825T genetic polymorphism of G protein β3 (GNB3) gene. Biomark Insights. 2016;11:69–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280. Nejatizadeh A, Kumar R, Stobdan T, Pasha MQ. Association of GNB3 C825T polymorphism with plasma electrolyte balance and susceptibility to hypertension. Genet Mol Biol. 2011;34(4):553–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281. Kumar R, Kohli S, Alam P, Barkotoky R, Gupta M, Tyagi S, Jain SK, Pasha MA. Interactions between the FTO and GNB3 genes contribute to varied clinical phenotypes in hypertension. PLoS One. 2013;8(5):e63934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282. Kabadou IA, Soualmia H, Jemaa R, Feki M, Kallel A, Souheil O, Taieb SH, Sanhaji H, Kaabachi N. G protein β3 subunit gene C825T and angiotensin converting enzyme gene insertion/deletion polymorphisms in hypertensive Tunisian population. Clin Lab. 2013;59(1–2):85–92. [DOI] [PubMed] [Google Scholar]
- 283. Li M, Zhang B, Li C, Liu JL, Wang LJ, Liu Y, Wang ZG, Wen SJ. G-protein beta 3 subunit polymorphisms and essential hypertension: a case-control association study in northern Han Chinese. J Geriatr Cardiol. 2015;12(2):127–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284. Matayoshi T, Kamide K, Takiuchi S, Yoshii M, Miwa Y, Takami Y, Tanaka C, Banno M, Horio T, Nakamura S, Nakahama H, Yoshihara F, Inenaga T, Miyata T, Kawano Y. The thiazide-sensitive Na+-Cl− cotransporter gene, C1784T, and adrenergic receptor-β3 gene, T727C, may be gene polymorphisms susceptible to the antihypertensive effect of thiazide diuretics. Hypertens Res. 2004;27(11):821–833. [DOI] [PubMed] [Google Scholar]
- 285. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SCJ, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269–1324. [DOI] [PubMed] [Google Scholar]
- 286. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JLJ Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. [DOI] [PubMed] [Google Scholar]