Abstract
Our objective was to test the feasibility of, fidelity to, and initial impact of a brief, glaucoma-specific motivational interviewing (MI) training program for ophthalmic para-professionals. This prospective, mixed-methods study had two components, one for staff and one for patients. Staff fidelity to MI principles was graded though audio-recorded encounters after initial and final training sessions. After training, patients graded staff for adherence to autonomy supportive care. Semi-structured interviews with para-professionals elicited feedback about the training and about their ability to implement MI in clinic. The impact on patient satisfaction with staff communication, eye drop instillation self-efficacy, and overall health activation was assessed using a survey pre- and post-training. Para-professionals met two of three program goals for MI skills and improved in their overall scores for MI fidelity. Para-professionals noted lack of time in clinic as a significant barrier to implementing counseling. Patient satisfaction with staff communication increased after the training (p=0.04) among patients who rated their staff above the mean for providing autonomy supportive care. The intervention did not improve patients’ eye drop instillation self-efficacy or overall health activation. Training para-professional staff in brief, glaucoma-specific MI techniques is feasible and may improve patient satisfaction, though dedicated time in clinic is needed to implement MI counseling into glaucoma practice.
Keywords: Motivational interviewing training, glaucoma, satisfaction, feasibility, fidelity
Although medication reduces vision loss from glaucoma, (Garway-Heath et al., 2015) (Heijl et al., 2002), glaucoma remains the third leading cause of visual impairment in the United States (National Eye Institute, 2016). This is, in part, because at least one-half of glaucoma patients are essentially “untreated” as they do not adhere to their medications (Olthoff, Schouten, van de Borne, & Webers, 2005), (Reardon, Kotak, & Schwartz, 2011). Ineffective self-management behaviors and poor clinical outcomes disproportionately affect racial and ethnic minority populations and the elderly (Congdon et al., 2004),(Murakami et al., 2011). Adherence to glaucoma medications is rarely addressed during the clinical encounter (B. Sleath et al., 2014), (Sleath, Sayner, et al., 2015). Glaucoma education, counseling programs, and teaching eye drop instillation are not part of standard glaucoma care (Sleath, Blalock, et al., 2015; B. L. Sleath et al., 2014). A recent Cochrane Review of medication adherence interventions found that counseling using motivational interviewing was the most successful approach to increasing adherence across a wide range of chronic diseases (Nieuwlaat et al., 2014).
Qualitative research has identified ambivalence about the diagnosis and treatment in the face of this chronic asymptomatic disease to be a key barrier to medication adherence and effective self-management (Friedman 2008). Motivational interviewing (MI) has been used successfully to influence positive behavior change in other chronic asymptomatic diseases where ambivalence and poor motivation are common, such as in medication adherence to improve blood pressure control (Ogedegbe 2008). Eye drop instillation is a moderately difficult behavior, requiring grip strength, good vision and hand-eye coordination, all of which can be limited in an older population with eye disease. One-fifth of patients cannot correctly instill their eye drop medications, making good adherence impossible from the start (Stone, Robin, Novack, Covert, & Cagle, 2009). MI based approaches have been shown to improve moderately difficult health behaviors, such as eye drop instillation. MI based approaches have also been shown to improve behaviors with a high level of psychological resistance, such as taking chronic daily medications for asymptomatic conditions (Resnicow 2017).
MI engages patients by strengthening a person’s own motivation and commitment to change a health behavior (W. R. Miller & Rollnick, 2012). There are five core skills to MI: asking open-ended questions, affirming, reflecting, summarizing, and obtaining permission to provide information and advice (W. R. Miller, Rollnick, S., 2012). These skills help elicit ‘change talk’, through which counselors help patients talk themselves into change. A key component that underlies the spirit of MI is expressing empathy, which promotes rapport between the counselor and the participant.
A meta-analysis of 48 MI interventions determined that MI had a 55% increased odds of improved self-management behavior over standard health professional advice (Lundahl et al., 2013). This meta-analysis found that MI was more often successful when delivered by a mental health professional rather than a physician, dietician or nurse. A number of successful interventions conducted after this meta-analysis have focused on training health professionals – pharmacists (Caponnetto 2017), physicians (Dempsey 2018), nurses (Salimzadeh 2018), and physicians and office staff (Pollack 2016) - in conducting MI sessions outside of a standard clinic visit. Yet, no studies to date have evaluated training only para-professional staff in MI approaches for use during their usual work flow in real-life clinical settings. Therefore, the purpose of the current study was to test the feasibility, fidelity to, and initial impact of a glaucoma-specific brief motivational interviewing training program where para-professional staff learned to counsel patients about medication adherence and teach eye drop instillation during their regular clinic visit. We assessed the training’s impact on patient satisfaction with provider communication, eye drop instillation self-efficacy and overall health activation.
Methods
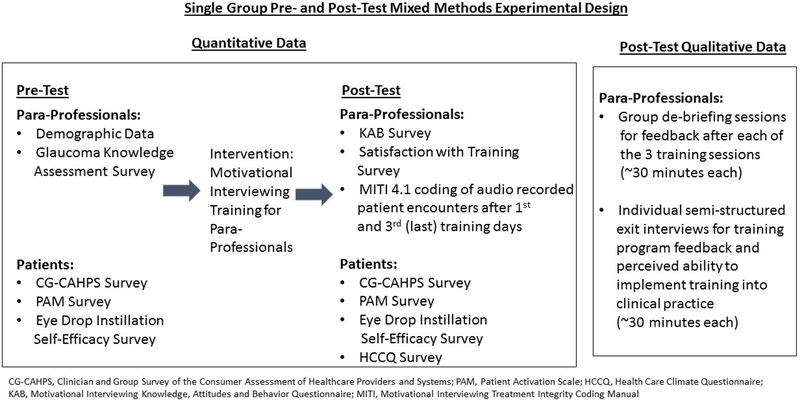
This was a prospective, mixed-methods observational study using a pre-post intervention design consisting of two components: one centered on the para-professional staff members undergoing the MI training and the second focused on the experiences of glaucoma patients who interacted with the trained staff (Figure 1). The program taught 8 glaucoma para-professional staff members the skills to teach eye drop instillation and to facilitate a brief MI-based conversation with patients about medication adherence. We assessed the program’s feasibility and acceptability, and the fidelity of the para-professional staff to the new MI skill. We evaluated the impact of the training on the primary outcome of patients’ satisfaction with provider communication. We also explored changes in eye drop instillation self-efficacy and overall health activation of patients who received counseling from the trained staff, both of which are key mediators of improved adherence and outcomes. IRB approval was obtained from the University of Michigan for this research.
Figure 1.
Flow diagram depicting mixed methods experimental design testing the feasibility and initial impact of a glaucoma-specific brief motivational interviewing training program for para-professional staff
Glaucoma-Specific Brief MI Training Program Development
The brief, glaucoma-specific MI training program was developed by two behavioral psychologists (KR, PK) and a psychotherapist (CM) trained through the Motivational Interviewing Network of Trainers (MINT). The program included 3 training sessions covering 16 hours of didactic group training and 2 hours of individualized coaching administered over 3 days, each within a month of the last. The first training session (8 hours) taught reflective listening, asking open-ended questions, using affirmations, using elicit-provide-elicit to teach eye drop instillation, and summarizing (W. R. Miller, Rollnick, S., 2012). Using elicit-provide-elicit includes assessing the patients’ knowledge prior to giving information, asking permission to give new information, and then following up by eliciting patients’ response to the new information to evaluate their understanding. The second training session (4 hours) taught how to problem-solve issues that arose in patient encounters and making complex reflections. A reflection is a statement that paraphrases what the patient said to demonstrate active listening; a complex reflection is a statement that paraphrases and adds significant meaning. The third training session (4 hours) taught how to identify and promote change talk and develop an action plan to improve medication adherence. A video collection of glaucoma patients explaining their reasons for discontinuing their glaucoma medications was used for role playing. Each training session included both didactic presentations and role-playing.
Quantitative Assessment of Para-Professional Staff’s Fidelity to the Training
Before training, participating staff’s glaucoma knowledge, age, ophthalmology work experience, and education were recorded. After each training session, participating staff audio recorded 1–2 patient encounters which were independently coded by two MINT trainers to assess fidelity to MI counseling using the Motivational Interviewing Treatment Integrity Coding Manual 4.2.1 (MITI) (Moyers, 2014), and to assess whether staff were meeting the program goals. The MITI uses both global assessment across 4 domains (cultivating behavior change talk, softening sustain talk, partnership, empathy) as well as behavior counts to assess fidelity to MI counseling. The global relational score is calculated as the score for partnership plus empathy divided by two. (Moyers 2014) Staff audio-recorded 1–2 patient encounters after each training session as this was what was clinically feasible. Due to short (<10 minute) staff-patient encounters, we focused on the relational global measures (partnership and empathy) and behavior counts (percent complex reflections and reflection to question ratio) (Table 1). There were three main program goals to assess if MI could enhance patient-provider interaction while teaching better eye drop instillation. The goals of training were for staff to: 1) use at least one reflective listening statement, 2) use elicit-provide-elicit to give advice, and 3) use at least a 1:1 ratio of open-ended to closed-ended questions. Two encounters were graded after the last training session, one where staff practiced with each other and one where they used their skills in a clinical encounter. Each of the two MINT trainers graded all of the staff members at each training time point. Previous studies have demonstrated that peer coaches (Goldman 2015) and community health workers (Dewing 2014) do not all attain MI proficiency after brief training. Therefore, we set separate training goals outside of attaining full MI proficiency because we hypothesized that the non-mental health care provider staff in this study who underwent a brief training may not be able to attain counseling proficiency on a rubric used to assess mental health care professionals. Based on prior studies of key features contributing to MI effectiveness (do Valle Nascimento 2017), we ascertained that using open-ended questions and making reflections were the key skills that were important for practitioners to master. We thus focused on those skills for our evaluation of training success and fidelity.
Table 1.
Definitions and Proficiency Thresholds for MITI 4.1 (18) Scores Utilized
| Summary Score | Definition | Fair Proficiency | Proficient |
|---|---|---|---|
| Relational Component | How well the counselor demonstrates 1) Partnership in which they do not assume the role of the expert but rather encourage power sharing in the interaction so that the patient’s contributions influence the course of the discussion and 2) Empathy in which the counselor demonstrates a deep understanding of the patient’s perspective and situation. | 4/5 on a Likert scale | 5/5 on a Likert scale |
| Percent Complex Reflections | While simple reflections convey an understanding of what the patient says, complex reflections add meaning to what the patient has said. | 40% | 50% |
| Reflection: Question | Number of all reflective statements compared to number of total questions asked. | 1:1 | 2:1 |
After training, staff completed a survey using two validated instruments, one to assess satisfaction with training (Goldman 2015), and their knowledge of, attitudes toward, behavior surrounding, and value attributed to MI (Knowledge, Attitudes and Behavior(KAB) Scale) (Cook et al., 2017). Satisfaction with training was assessed from agreement with 13 statements, each scored on a 5-point Likert scale (Goldman 2015). A mean of the 13 responses was calculated with higher scores indicating increased satisfaction. KAB subscale scores were calculated as the mean of included items, each scored on a 5-point scale, with higher scores indicating better outcomes (Cook 2017).
Descriptive statistics were used to summarize staff characteristics. MITI scores and program goal attainment were summarized after the first and last training sessions and change was evaluated with mixed linear regression models. Differences in grading between coders were investigated with a fixed coder effect and retained in models if significant. These models accounted for the correlation between coder scores of the same staff member with an unstructured correlation structure.
Qualitative Assessment of Training by Para-Professional Staff to Refine the Program
After each training session, a 30-minute feedback session was conducted with two of the authors (CM, PANC). After all training, staff completed a 30-minute, semi-structured interview (with PANC) to provide feedback about the entire program and their ability to implement what they had learned into clinical practice (Appendices A & B). Interviews were audio recorded and transcribed verbatim. The authors (PANC, OK) used grounded theory to analyze the interviews (Creswell, 2016). The researchers wrote memos to identify themes in transcripts and worked together to form a code-book for all agreed upon codes. They independently analyzed the transcripts using these codes. Discrepancies were evaluated and discussed until consensus was met. If consensus was not reached, a third researcher (CM) adjudicated. Interview transcripts were re-evaluated for themes based on patient assessment of staff adherence to MI. A joint display combined the qualitative and quantitative data.
Quantitative Assessment of Patient Outcomes
One month before staff underwent MI training, a convenience sample of patients ≥18 years of age attending the glaucoma clinic in a large Midwestern academic medical center (University of Michigan, Ann Arbor, MI) and taking ≥1 glaucoma medication were asked to complete a survey about satisfaction with staff communication, health activation, and eye drop instillation self-efficacy. Those who agreed to participate completed informed consent and the 23-item survey. Patients were excluded if they did not speak English or had cognitive impairment. During their next scheduled glaucoma visit, 5–13 months after completion of the initial survey and after staff completed MI training, participants repeated the survey and answered 15 additional questions assessing staff’s ability to provide autonomy supportive care.
The patient survey included scales from 4 validated instruments. The four question provider communication sub-scale from the Clinician and Group Survey of the Consumer Assessment of Healthcare Providers and Systems (CG-CAHPS) (Department of Health and Human Services, 2015) assessed satisfaction with provider communication with higher scores indicating better provider communication (scale 1–3); the mean was designated as the scale score. The Patient Activation Measure (PAM) (Skolasky et al., 2011), was used to assess whether patients have the knowledge, skills, and confidence to manage their health and health care. The PAM score ranges from 1–100 with higher score indicating better patient activation (Hibbard 2003; Hibbard 2004). The Eye Drop Instillation Self-efficacy Scale (EDISE) (Sleath et al., 2012) includes 6 questions assessing a patient’s confidence with administering their glaucoma medication. Question responses were recorded on 3-point scale with higher scores indicating increased confidence; the mean was designated as the scale score. Lastly, patients rated staff communication after the training with the Health Care Climate Questionnaire (HCCQ) (Williams & Deci, 2001). The HCCQ measures ability to provide autonomy supportive care consistent with an MI counseling style and includes 15 questions about whether patients felt staff listened well, demonstrated empathy, and asked permission to give advice (Williams & Deci, 2001). Responses to each question are graded on a 7-point Likert scale and an overall score is calculated from the mean of all questions. Patients did not assess staff HCCQ scores before the training as they were not assigned the same staff member both before and after the training.
Descriptive statistics were used to summarize patient characteristics. Patients who completed the study were compared to participants who dropped out with two-sample t-, Wilcoxon, Chi-square, and Fisher’s exact tests. Survey scores were summarized with means and standard deviations (SD) at both pre- and post-MI counseling visits and compared for differences with paired t-tests. In the subset of patients who rated their providers as above the mean for adherence to MI principles (HCCQ score), pre- and post-MI survey scores were compared with paired t-tests. SAS version 9.4 was used for all statistical analyses (SAS Institute, Cary, NC).
Results
Quantitative Para-Professional Staff Outcomes
Four glaucoma technicians, two comprehensive ophthalmology technicians, and two medical assistants participated in the brief-MI training program. Seven staff completed the entire program (88%) and all staff completed the staff surveys and interviews. Staff were on average 32.0 years old (SD=4.6), 88% female (n=7), and had been working in ophthalmology for a mean of 6.1 years (SD=5.5). Most had at least some college education (n=7) and 3 had completed an undergraduate degree. Glaucoma knowledge test scores showed an average of 96% of items answered correctly (range 86%−100%). Recorded patient encounters were on average 6.4 ± 5.1 minutes, and the median encounter length was 4.9 minutes.
After completion of training, all staff met two goals of the program: using at least one reflection (mean=4, range=1–8 in the practice session) and using at least a 1:1 ratio of closed-ended to open-ended questions (range from 1:1 to 1:4). For the third goal, using elicit-provide elicit, staff used this during 12.5% of initial encounters and 42% of their final encounters.
Staff showed significant improvement in their MI global relational scores, comprised of the partnership and empathy scores, between the first and last training sessions (Table 2). Partnership and empathy scores showed average improvement of 1.0 and 1.4 points for the practice sessions (p=0.007 and p=0.01, respectively), and average improvement of 0.3 and 1.0 points for the clinic patient encounter sessions (p=0.3 and p=0.0002, respectively). Staff had average scores of 3.3 and 2.8 for MITI relational scores during their practice sessions and clinical patient encounter session, respectively, where 4/5 indicates proficiency. These scores showed significant improvement from the first training session scores (p=0.01 and p=0.004, respectively). Staff had a reflection to question ratio of about 1:3 where a 1:1 reflection to question ratio is required for MI proficiency. Staff made 39% of their reflections complex during the practice session and did not use any complex reflections during their clinical encounters (Table 2). Therefore, none of the staff met full MI proficiency criteria after completing the training program. No coder differences were found for any of the MITI scale outcomes.
Table 2.
Comparison of motivational interviewing treatment integrity (MITI) scores after first and third (final) training sessions, during the practice session and during the clinical patient encounter
| MITI Scale | Post Training #1 (n=14*) | Post Training #3 (n=14*) | Change (n=14*) | P-value** | Post Training #3 (n=12*) | Change (n=12*) | P-value** |
|---|---|---|---|---|---|---|---|
| Partnership | |||||||
| Mean (SD) | 1.9 (0.7) | 2.9 (0.5) | 1.0 (0.8) | 0.01 | 2.3 (0.9) | 0.3 (1.2) | 0.3 |
| Min, Max | 1.0, 3.0 | 2.0, 4.0 | 0.0, 2.0 | 1.0, 4.0 | −1.0, 2.0 | ||
| Empathy | |||||||
| Mean (SD) | 2.2 (1.1) | 3.6 (0.5) | 1.4 (1.2) | 0.01 | 3.2 (0.8) | 1.0 (1.4) | 0.0002 |
| Min, Max | 1.0, 4.0 | 3.0, 4.0 | 0.0, 3.0 | 1.0, 4.0 | −1.0, 3.0 | ||
| Relational*** | |||||||
| Mean (SD) | 2.1 (0.8) | 3.3 (0.4) | 1.2 (0.9) | 0.01 | 2.8 (0.8) | 0.6 (1.2) | 0.004 |
| Min, Max | 1.0, 3.5 | 2.5, 3.5 | 0.0, 2.5 | 1.0, 4.0 | −1.0, 2.5 | ||
| # Simple Reflections | |||||||
| Mean (SD) | 2.4 (2.4) | 2.3 (1.0) | −0.1 (3.1) | 0.9 | 1.8 (1.8) | −0.3 (2.5) | 0.7 |
| Min, Max | 0.0, 7.0 | 1.0, 4.0 | −6.0, 4.0 | 0.0, 5.0 | −7.0, 3.5 | ||
| # Complex Reflection | |||||||
| Mean (SD) | 0.9 (0.9) | 1.8 (1.1) | 0.9 (1.2) | 0.07 | 0.1 (0.4) | −0.7 (1.2) | 0.2 |
| Min, Max | 0.0, 3.0 | 0.0, 4.0 | −1.0, 2.0 | 0.0, 1.5 | −3.0, 1.5 | ||
| % Complex Reflections | |||||||
| Mean (SD) | 30% (36%) | 39% (19%) | 11% (40%) | 0.4 | 1% (3%) | −39% (44%) | 0.1 |
| Min, Max | 0%, 100% | 0%, 67% | −50%, 54% | 0%, 9% | −100%, 9% | ||
| # Reflections | |||||||
| Mean (SD) | 3.3 (2.6) | 4.1 (1.9) | 0.8 (3.8) | 0.4 | 1.9 (1.9) | −1.0 (2.5) | 0.7 |
| Min, Max | 0.0, 8.0 | 1.0, 8.0 | −6.0, 6.0 | 0.0, 5.0 | −8.0, 1.5 | ||
| # Questions | |||||||
| Mean (SD) | 14.6 (6.6) | 7.6 (3.2) | −7.0 (8.6) | 0.07 | 14.5 (9.0) | 0.0 (5.1) | 0.8 |
| Min, Max | 5.0, 28.0 | 3.0, 13.0 | 23.0, 6.0 | 3.0, 26.0 | −7.0, 12.0 | ||
| % Reflections | |||||||
| Mean (SD) | 16% (12%) | 37% (18%) | 20% (27%) | 0.1 | 9% (10%) | −5% (12%) | 0.4 |
| Min, Max | 0%, 40% | 8%, 63% | −19%, 63% | 0%, 27% | −40%, 5% |
n=14 (practice session from 7 technicians were graded twice, once by each of 2 coders), n=12 (clinical patient encounters from 6 technicians were graded twice, once by each of 2 coders);
p-value from a mixed linear regression model testing for a significant change in grading measurement between post training session #1 and post training sessions #3. No significant effects of coder were found;
MITI relational is a mean of MITI partnership and empathy items;
SD=standard deviation; Min=minimum; Max=maximum
Staff reported a mean satisfaction with training score of 4.2 out of 5.0 (SD=0.3). On average, staff rated their knowledge of MI after training at 3.8 (SD=0.6) and the value of MI in their practice at 4.8 (SD=0.4) on a 5-point Likert scale. They rated their attitude towards helping people find their own reasons for change instead of giving unsolicited advice at 3.5 (SD=0.7). The lowest score staff gave in their self-assessment was regarding their ability to implement MI in their clinical encounters (mean=3.2, SD=0.8, 5-point Likert scale).
Qualitative Para-Professional Staff Outcomes
In exit interviews, all staff said MI training was valuable, improved their communication with patients, and increased job satisfaction. One staff member said “I feel a lot more confident talking with patients. I just felt more confident overall about my ability to help the patient.” Another participant said “I think that by taking this class all of us are probably better at talking to the patients about finding things out, about helping seeing barriers and seeing potential reasons why they might not be taking them, because it’s always just ‘They don’t want to or they are forgetting,’ but I think there is a lot more than that. I think it gives us the weapons to break down the barriers they have about why they might not be taking the drops.” Several participants stated that they wished MI had been part of their initial training as a technician, “I feel like we should have learned [MI] when we were [in the] …ophthalmic technician [training] program.” Technicians who were rated above average on autonomy supportiveness by the patients they counseled more frequently made statements that were consistent with MI spirit and technique (Joint Display Table 3).
Table 3.
Joint Display: Themes from Staff Rated Above and Below the Mean for Autonomy Supportiveness (measured by HCCQ)
| Below Mean HCCQ Score (Theme, Illustrative quote) |
Above Mean HCCQ Score (Theme, Illustrative quote) |
|
|---|---|---|
| Demonstrating MI Spirit | Classified patients as “difficult,” demonstrating that they were wrestling with patients over behavior change instead of rolling with resistance: “A lot of times, it’s hard to get information on a patient” though other times “that other [patient] was easy” |
Worked to make all patients feel comfortable and acknowledged the importance of rapport: “patients are getting a lot out of the way that we’re talking to them and making them feel comfortable” and “if the patient does not feel comfortable with you, they are not going to take what you say seriously” |
| Demonstrating MI Techniques | Asking more closed-ended questions: “‘Do you every have trouble with aim?’ I actually asked that directly” |
Using affirmations: “you might not be getting them in seven days but you have got them in six days and that’s awesome…” |
Staff valued doing the MI training in-person and with the one-on-one coaching sessions. One person commented that “you can read about [MI] all you want, but then it’s like reading how to work on a slit lamp.” Participants also found the individualized coaching sessions valuable. One participants said “it was good to… talk one on one and get a little bit more in depth of what we’re doing wrong or doing right… maybe you’re a little more afraid to ask in front of a big group.”
Trained staff identified a number of barriers to implementing MI brief counseling in clinic. All eight participants cited lack of time. One person said: “[Time is] a barrier from really being able to …dig a little deeper and say ‘what if any problems are you having with instilling your drops?’” Another participant suggested that “… if we had an appointment time where it was just set out for that [education and counseling] for patients who are struggling, I think it would be awesome.” Other barriers staff identified were the perception that patients’ educational needs exceeded the scope of paraprofessionals practice (8/8 participants), and the need for physician-approved, standardized educational content (6/8 participants). Staff also said that poor communication between the para-professional staff and physicians (5/8 participants) made it difficult for staff to feel empowered to take a role in educating patients. One participant commented that “some physicians are hesitant towards us being able to educate patients… I don’t know if it’s mis-information they think that we’re supplying.” Another participant noted that “if they [the physicians] understood more about the… information … we’re trying to present to patients, I think they would be more on board.” If staff were presenting standardized content that physicians approved, staff felt that physicians would be more amenable to an expanded patient education role for technicians.
Initial Impact of Intervention on Quantitative Patient Outcomes
A total of 102 glaucoma patients were recruited for the study and 79% (n=81) completed both the baseline and follow-up surveys and were seen by one of the staff who completed the MI training program. Patients were on average 70.6 years old (SD=13.0), 51% female, 83% Caucasian and 66% had a diagnosis of severe stage glaucoma. Better eye presenting visual acuity was on average 0.11±0.24 LogMar (20/25 Snellen equivalent, range −0.12 to 1.60). Patients who completed the study were similar to those who dropped out, except that participants who dropped-out were more likely to be new visit patients (p=0.005). In the subgroup of patients who rated their paraprofessional staff above the mean for autonomy supportive communication (n=39), there was significantly higher satisfaction with technician communication after the training (pre-training mean=2.8, SD=0.4; post-training mean=3.0, SD=0.1, p=0.04). Among the entire sample, participants did not show significant improvement in satisfaction with staff communication (CG-CAHPS baseline score 2.7±0.3 to 2.7±0.3 post-training, p=0.5), health activation (PAM baseline score 66.9±14.1 to 66.5±14.0 post-training, p=0.7), or eye drop instillation self-efficacy (EDISE baseline score 2.9±0.3 to 2.9±0.2 post-training) after interacting with staff who went through MI training (Table 4).
Table 4.
Descriptive statistics on patient outcomes, pre- and post-intervention
| Pre-MI Intervention | Post-MI Intervention | Change | ||||||
|---|---|---|---|---|---|---|---|---|
| Score | N | Mean (SD) | Min, Max | Mean (SD) | Min, Max | Mean (SD) | Min, Max | P-value* |
| Full Patient Sample (n=81) | ||||||||
| CG-CAHPS score | 78 | 2.9 (0.3) | 1.3, 3.0 | 2.9 (0.2) | 1.8, 3.0 | 0.07 (0.35) | −0.50, 1.75 | 0.08 |
| PAM 10 Score | 79 | 66.9 (14.1) | 40.9, 100.0 | 66.5 (14.0) | 42.9, 100.0 | −0.46 (11.6) | −37.4, 34.1 | 0.7 |
| EDISE score | 81 | 2.7 (0.3) | 2.0, 3.0 | 2.7 (0.3) | 2.0, 3.0 | 0.02 (0.30) | 1.0, 0.8 | 0.5 |
| Patients who rated their para-profession above average for autonomy support (n=39) | ||||||||
| CG-CAHPS score | 39 | 2.8 (0.4) | 1.3, 3.0 | 3.0 (0.1) | 2.5, 3.0 | 0.13 (0.39) | −0.5, 1.75 | 0.04 |
| PAM 10 Score | 38 | 67.0 (14.4) | 40.9, 100.0 | 66.0 (12.8) | 42.9, 100.0 | −0.92 (10.4) | −27.7, 19.5 | 0.6 |
| EDISE score | 39 | 2.7 (0.3) | 2.0, 3.0 | 2.7 (0.3) | 2.0, 3.0 | 0.02 (0.29) | −1.0, 0.5 | 0.7 |
MI, Motivational Interviewing; SD, Standard Deviation; Min, Minimum; Max, Maximum; CG-CAHPS, Clinician and Group Survey of the Consumer Assessment of Healthcare Providers and Systems; PAM, Patient Activation Measure; EDISE, Eye Drop Installation Self-Efficacy
Discussion
This is the first study to assess feasibility and acceptability of providing training to all para-professional ophthalmology staff in a clinic in brief, glaucoma-specific, MI-based counseling and examine the initial impact on patient outcomes. The most notable finding from this work was that participants who rated the counseling they received from the trained technicians as above the mean on the validated scale for autonomy supportive communication had significantly higher satisfaction with their communication than those whose technicians scored lower on autonomy supportive communication (p=0.04). Our study reinforces other studies’ findings of the importance of autonomy supportive communication for improving patient outcomes (Leahey TM 2013; Palacio et al 2016; Ostlund et al 2016). A recent meta-analysis (Palacio et al., 2016) of studies investigating the impact of MI on medication adherence found that MI counselors who underwent a fidelity assessment of their MI skills had a significant impact on improving medication adherence compared to those without an assessment. These findings reinforce the value of counseling that has high fidelity to MI principles, underscoring the importance of providing continued booster training and assessing fidelity of paraprofessionals undergoing MI training. In addition, only retaining those able to achieve an adequate level of autonomy supportive communication to serve as counselors should be considered.
After training, all seven staff met the first two program goals of using at least one reflective listening statement and using ≥1:1 ratio of open-ended to closed-ended questions. Staff significantly improved in their MI spirit scores of partnership and empathy, the third program goal, over the course of the training. Staff showed more improvement in a simulated context when practicing their new skills with peers than in actual practice during their clinical encounters. This demonstrates that mastering MI counseling skills takes perseverance and practice. Staff rated their knowledge of MI and their attitude toward using MI highly after the training. They rated their MI knowledge similar to 45 ophthalmic technicians from a recent, large-scale training project at the University of Colorado where staff underwent 8 hours of training (Paul Cook, unpublished data) (mean ± SD of 3.8±0.6 vs. 3.9±0.5, respectively). Though they gave themselves a high self-rating for MI knowledge, it was still difficult for all of the staff to implement their knowledge into practice and they did not meet full criteria for MI competency. This finding underscores the importance of choosing only staff who demonstrate the ability to use their MI counseling skills in practice to be the ones who provide patient counseling. Additionally, those staff need on-going supervision, assessment of fidelity, and support to maintain their skills.
We examined changes in skills and attitudes important for patients’ glaucoma self-management; at baseline most patients in the sample already scored well on these measures. Overall, patients had good eye drop instillation self-efficacy. The mean score of 2.7 (SD=0.3) both before and after the intervention was high compared to other studies (Sleath et al., 2010). Patients in our study also had good health activation. Average PAM scores before (66.9±14.1) and after (66.5±14.0) training showed Level 3 activation (Skolasky et al., 2011). This places the average patient in our sample as beginning to take an active role in their healthcare. MI counseling is more helpful for patients who have low self-efficacy or low health activation. Satisfaction with staff communication was also high before the intervention, so it was notable that there was significant improvement after the intervention among patients who scored staff above average on autonomy-supportive communication (pre mean=2.8, post mean=3.0). Similarly, in a recent study, Cook and colleagues found that among patients with reasonable medication adherence at baseline, MI based counseling delivered by ophthalmic technicians outside the clinic visit did not improve medication adherence more than using phone call reminders (Cook 2018). In future MI counseling interventions with glaucoma patients, it will be essential to recruit patients with low activation, low eye drop instillation self-efficacy, or poor glaucoma medication adherence in order to assess the effectiveness of interventions among patients with higher need.
In this study, we evaluated the impact of integrating MI techniques into a standard clinical encounter of no longer than ten minutes. Even though the intervention was brief, one of the most commonly reported barriers to implementing MI from our staff was a lack of time. Staff suggested that if patients with low medication adherence or difficulties with eye drop administration could be identified, it would be helpful to schedule a separate appointment dedicated to education and counseling. Under these conditions, they felt it would be more feasible to deliver counseling and education using the MI skills they had learned. In order to effect behavior change, longer time periods will need to be dedicated to counseling in clinic; a systematic review of studies investigating the impact of MI on heath behavior change found that the average time patients received MI counseling for successful interventions was 106 minutes (Lundahl et al., 2013).
Another important implication of our findings is that expanding the role of all ophthalmic para-professional staff to deliver high quality MI counseling may not be realistic. In an MI-based sexual risk reduction intervention in South Africa, investigators found that all lay health care workers were not delivering MI consistent counseling after an initial 35-hour training, but the majority improved greatly in their adherence to MI principles after 18 hours of refresher training and continued supervision (Dewing et al., 2014). Our training session included on-going supervision during the study period, but would need to include continued booster training sessions to maintain high fidelity to MI principles. Identifying which staff excel at MI and focusing on their professional development as counselors could be another strategy to improve outcomes.
Our findings also suggest the potential value of using technology to expand the amount of support para-professional staff are able to provide patients. eHealth tools have been utilized by staff to give patients personalized yet standardized information. In one eHealth intervention, lay healthcare workers used an interactive tablet-based program to provide individualized diabetes information to low-income Latino and African American adults with diabetes. Those who received this personalized intervention reported significantly less diabetes-related distress and greater improvement in satisfaction with medication information than those who received standard, non-personalized diabetes education (Heisler et al., 2014). Our staff noted they would feel more empowered to counsel and educate patients if they had a tool that offered educational content approved by their physicians. We have developed a tool to allow para-professional staff to deliver glaucoma counseling and education personalized to each patient’s diagnosis, treatments, test results, barriers to optimal medication adherence, and personal values (Killeen et al., 2016). This eHealth tool also provides prompts to help guide para-professional staff through an MI based conversation, potentially decreasing the MI skill level needed to effectively guide behavior change among glaucoma patients.
There were a number of limitations to our study. First, the principal investigator, a glaucoma specialist who practices in the clinic where the majority of particpating staff work, was present for the de-briefing sessions after training and conducted the exit interviews. This may have limited negative feedback, though staff did offer much constructive criticism. Second, our convenience sample of patients does not represent the target population of patients with low health activation, self-efficacy or low medication adherence ideal for MI intervention, as the focus of this study was on the feasibliilty and acceptability of the program for staff. Future research should target higher risk populations. Due to the small sample size of staff, inter-grader agreement for MITI scoring was not reported. However, we tested for differences in coder grading of program staff in our mixed linear regression models and found no significant differences between coders. Additionally, staff clinical encounters were short (<10 minutes), making it difficult to fully grade the encounters according to all MITI 4.1 criteria (Moyers, 2014). Future implementation efforts need to identify ways to deliver longer, behavior change oriented counseling sessions at convenient times for patients.
In conclusion, we found that while it is feasible and acceptable to train glaucoma para-professional staff in brief, glaucoma-specific MI techniques, a number of features of such a program need to be improved. First, staff will need more time during the clinical encounter to implement MI skills to allow them to practice behavior-change oriented counseling. The program will need to include both an initial MI training session as well as booster sessions and supervision to maintain skills and assure adherence to MI technique. Supervision by trained counselors with validated MI grading tools is necessary to provide staff with continued feedback on their audio-recorded patient encounters.
Once we have a standardized training and certification program for glaucoma counseling for our para-professional staff, as a glaucoma community, we can work with the Centers for Medicare and Medicaid Services to develop reimbursement paradigms for glaucoma counseling (Federal Register, 2000). This would enable the ophthalmic community to provide self-management support for people with glaucoma similar to what is already standard of care for people with diabetes.
Acknowledgments
This research was supported in part by, the Blue Cross Blue Shield Foundation of Michigan, the American Glaucoma Society Young Clinician Scientist Award, Research to Prevent Blindness Career Development Award, the David L. Epstein, MD Chandler Grant Society Clinician-Scientist Award, and the National Eye Institute 1K23EY025320.
Appendix A.
Motivational Interviewing Training Didactic Session De-Briefing Guide
Training Goals
What are some things you will take away from today’s training?
What, if anything, do you feel you need more training or practice on?
Which if any of the skills learned during today’s training do you think will be easy to implement in your day to day clinical work?
Which if any of the skills learned today do you think will be challenging to implement in your day to day clinical work?
Presentation Feedback
- We are developing this training program, what if anything could have been presented better or differently?
- How if at all could the order in which the skills were presented be improved?
Do you feel like it would have been helpful to have had materials to read prior to the training? And if so on what topics?
In what ways if at all were the role play activities helpful or not helpful?
Perception of Clinical Impact of Training
What if anything changed following today’s training in how you will teach eye drop instillation?
- How do you think learning these new communication techniques might impact the way you talk with your patients?
- How do you think patients might feel walking away from your interaction?
Appendix B.
Exit Interview Semi-Structured Interview Guide
Training Organization
- How, if at all, could the timing of the trainings have been improved?
- In terms of time in between the three trainings (shorter, longer, same)?
- Length of the trainings (full day plus 2 ½ day’s)?
What was your experience of the order of the material presented?
Do you feel like it would have been helpful to have had materials to read prior to the training? And if so on what topics?
Presenter
- What was your experience of how the information was presented?
- Was the content presented in a practical way?
- Did the material feel organized in a way that helped you learn?
- How or how not?
- Did the content feel appropriate to your skill level?
- How was the balance between instruction and practice?
How would you describe the presenter’s knowledge of the subjects presented?
How was the engagement of the presenter with you as participants?
Perception of Clinical Impact of Training
How do you think learning these new communication techniques might impact the way you talk/engage with your patients?
- What do you see as barriers to using these techniques in clinic?
- Is the clinical environment supportive to using these skills?
- Facilitate use of these skills? Or does something need to change in the environments (space, time, other tech/MD perspective on education)?
References
- Agency for Healthcare Research and Quality. (2015, June 23). CAHPS Clinician & Group Survey. Retrieved from https://cahps.ahrq.gov/surveys-guidance/cg/instructions/index.html.
- Caponnetto P, Dipiazza J, Aiello MR & Polosa R (2017). Training pharmacists in the stage-of-change model of smoking cessation and motivational interviewing: A randomized controlled trial. Health Psychology Open, 4, 2055102917736429. doi: 10.1177/2055102917736429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Congdon N, O’Colmain B, Klaver CC, Klein R, Munoz B, Friedman DS, Kempen J, …Eye Diseases Prevelance Research Group. (2004). Causes and prevalence of visual impairment among adults in the United States. Archives of Ophthalmolgy, 122, 477–485. doi: 10.1001/archopht.122.4.477 [DOI] [PubMed] [Google Scholar]
- Cook PF, Manzouri S, Aagaard L, O’Connell L, Corwin M & Gance-Cleveland B (2016). Results from 10 years of interprofessional training on motivational interviewing. Evaluation & the Health Profession, 40, 159–179. doi: 10.1177/0163278716656229 [DOI] [PubMed] [Google Scholar]
- Cook PF, Schmiege SJ, Mansberger SL, Sheppler C, Kammer J, Fitzgerald T & Kahook MY (2017). Motivational interviewing or reminders for glaucoma medication adherence: Results of a multi-site randomised controlled trial. Psychology & Health, 32, 145–165. doi: 10.1080/08870446.2016.1244537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell J (2016). Thirty essential skills for the qualitative researcher. Thousand Oaks, CA: SAGE Publishers. [Google Scholar]
- Dempsey AF, Pyrzanowski J, Lockhart S, Barnard J, Campagna EJ, Garrett K,… O’Leary ST (2018). Effect of a health care professional communication training intervention on adolescent human papillomavirus vaccination: A cluster randomized clinical trial. JAMA Pediatrics, 172, e180016. doi: 10.1001/jamapediatrics.2018.0016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewing S, Matthews C, Colete A, Schaay N, Simbayi L & Louw J (2014). Lay counselors’ ability to deliver counseling for behavior change. Journal of Consulting and Clinical Psychology, 82, 19–29. doi: 10.1037/a0034659 [DOI] [PubMed] [Google Scholar]
- do Valle Nascimento TM, Resnicow K, Nery M, Brentani A, Kaselitz E, Agrawal P,… Heisler M (2017). A pilot study of a community health agent-led type 2 diabetes self-management program using motivational interviewing-based approaches in a public primary care center in Sao Paulo, Brazil. BMC Health Services Research, 17, 32. doi: 10.1186/s12913-016-1968-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman DS, Hahn SR, Gelb L, Tan J, Shah SN, Kim EE, …Quigley HA (2008). Doctor-patient communication, health-related beliefs, and adherence in glaucoma results from the Glaucoma Adherence and Persistency Study. Ophthalmology, 115, 1320–1327, e1321–1323. doi: 10.1016/j.ophtha.2007.11.023 [DOI] [PubMed] [Google Scholar]
- Garway-Heath DF, Crabb DP, Bunce C, Lascaratos G, Amalfitano F, Anand N,…Zeyen TG (2015). Latanoprost for open-angle glaucoma (UKGTS): a randomised, multicentre, placebo-controlled trial. Lancet, 385, 1295–1304. doi: 10.1016/S0140-6736(14)62111-5 [DOI] [PubMed] [Google Scholar]
- Goldman ML, Ghorob A, Hessler D, Yamamoto R, Throm DH & Bodenheimer T (2015). Are low-income peer health coaches able to master and utilize evidence-based health coaching? Annals of Family Medicine, 13, S36–41. doi: 10.1370/afm.1756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M & Early Manifest Glaucoma Trial Group. (2002). Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Archives of Ophthalmology, 120, 1268–1279. [DOI] [PubMed] [Google Scholar]
- Heisler M, Choi H, Palmisano G, Mase R, Richardson C, Fagerlin A,…An LC (2014). Comparison of community health worker-led diabetes medication decision-making support for low-income Latino and African American adults with diabetes using e-health tools versus print materials: a randomized, controlled trial. Annals of Internal Medicine, 161, S13–22. doi: 10.7326/M13-3012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killeen OJ, Mackenzie C, Heisler M, Resnicow K, Lee PP & Newman-Casey PA (2016). User-centered design of the eyeGuide: A tailored glaucoma behavior change program. Journal of Glaucoma, 25, 815–821. doi: 10.1097/IJG.0000000000000431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leahey TM & Wing RR (2013). A randomized controlled pilot study testing three types of health coaches for obesity treatment: Professional, peer, and mentor. Obesity (Silver Spring), 21, 928–934. doi: 10.1002/oby.20271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundahl B, Moleni T, Burke BL, Butters R, Tollefson D, Butler C & Rollnick S (2013). Motivational interviewing in medical care settings: a systematic review and meta-analysis of randomized controlled trials. Patient Education And Counseling, 93, 157–168. doi: 10.1016/j.pec.2013.07.012 [DOI] [PubMed] [Google Scholar]
- Medicare Program; Expanded Coverage for Outpatient Diabetes Self-Management Training and Diabetes Outcome Measurements, 65 Fed. Reg. 83,129 (proposed Dec. 29, 2000) (to be codified at 42 C.F.R. pts. 410, 414, 424, 480, 498). [PubMed]
- Miller WR & Rollnick S (2012). Meeting in the middle: motivational interviewing and self-determination theory. International Journal of Behavioral Nutirtion and Physical Activity Act, 9, 25. doi: 10.1186/1479-5868-9-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Rollnick S (2012). Motivational interviewing: helping people change 3rd ed.). New York, NY: The Guilford Press. [Google Scholar]
- Moyers TB, Manuel JK, & Ernst D (2014). Motivational interviewing treatment integrity coding manual 4.1. Retrieved from https://casaa.unm.edu/download/miti4_1.pdf [DOI] [PMC free article] [PubMed]
- Murakami Y, Lee BW, Duncan M,Kao A, Huang JY, Singh K & Lin SC (2011). Racial and ethnic disparities in adherence to glaucoma follow-up visits in a county hospital population. Archives of Ophthalmology, 129, 872–878. doi: 10.1001/archophthalmol.2011.163 [DOI] [PubMed] [Google Scholar]
- National Eye Institute. (2016, April). Prevalence of adult vision impairment and age-related eye diseases in America. Retrieved from: https://nei.nih.gov/eyedata/adultvision_usa.
- Nieuwlaat R, Wilczynski N, Navarro T, Hobson N, Jeffery R, Keepanasseril A, …Haynes RB (2014). Interventions for enhancing medication adherence. Cochrane Database Of Systematic Reviews, 11, CD000011. doi: 10.1002/14651858.CD000011.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogedegbe G, Chaplin W, Schoenthaler A, Statman D, Berger D, Richardson T,… Allergrante JP (2008). A practice-based trial of motivational interviewing and adherence in hypertensive African Americans. American Journal of Hypertension, 21, 1137–1143. doi: 10.1038/ajh.2008.240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olthoff CM, Schouten JS, Van de Borne BW & Webers CA (2005). Noncompliance with ocular hypotensive treatment in patients with glaucoma or ocular hypertension an evidence-based review. Ophthalmology, 112, 953–961. doi: 10.1016/j.ophtha.2004.12.035 [DOI] [PubMed] [Google Scholar]
- Ostlund AS, Wadensten B, Haggstrom E, Lindqvist H & Kristofferzon ML (2016). Primary care nurses’ communication and its influence on patient talk during motivational interviewing. Journal of Advanced Nursing, 72, 2844–2856. doi: 10.1111/jan.13052 [DOI] [PubMed] [Google Scholar]
- Palacio A, Garay D, Langer B, Taylor J, Wood BA & Tamariz L (2016). Motivational interviewing improves medication adherence: A systematic review and meta-analysis. Journal of General Internal Medicine, 31, 929–940. doi: 10.1007/s11606-016-3685-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reardon G, Kotak S & Schwartz GF (2011). Objective assessment of compliance and persistence among patients treated for glaucoma and ocular hypertension: A systematic review. Patient Preference and Adherence, 5, 441–463. doi: 10.2147/PPA.S23780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnicow K, Teixeira PJ & Williams GC (2017). Efficient allocation of public health and behavior change resources: The “Difficulty by Motivation” matrix. American Journal of Public Health, 107, 55–57. doi: 10.2105/AJPH.2016.303526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salimzadeh H, Khabiri R, Khazaee-Pool M, Salimzadeh S, Delavari A (2018) Motivational interviewing and screening colonoscopy in high-risk individuals. A randomized controlled trial. Patient Education and Counseling, 101, 1082–1087. doi: 10.1016/j.pec.2018.01.015 [DOI] [PubMed] [Google Scholar]
- Skolasky RL, Green AF, Scharfstein D, Boult C, Reider L & Wegener ST (2011). Psychometric properties of the patient activation measure among multimorbid older adults. Health Services Research, 46, 457–478. doi: 10.1111/j.1475-6773.2010.01210.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sleath B, Blalock SJ, Carpenter DM, Muir KW, Sayner R, Lawrence S,… Robin AL (2014). Provider education about glaucoma and glaucoma medications during videotaped medical visits. Journal of Ophthalmolgy, 2014, 238939. doi: 10.1155/2014/238939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sleath B, Blalock SJ, Carpenter DM, Sayner R, Muir KW, Slota C, … Robin AL (2015). Ophthalmologist-patient communication, self-efficacy, and glaucoma medication adherence. Ophthalmology, 122, 748–754. doi: 10.1016/j.ophtha.2014.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sleath B, Blalock SJ, Robin A, Hartnett ME, Covert D, Devellis B & Giangiacomo A (2010). Development of an instrument to measure glaucoma medication self-efficacy and outcome expectations. Eye (London), 24, 624–631. doi: 10.1038/eye.2009.174 [DOI] [PubMed] [Google Scholar]
- Sleath B, Blalock SJ, Stone JL, Skinner AC, Covert D, Muir K & Robin AL (2012). Validation of a short version of the glaucoma medication self-efficacy questionnaire. British Journal of Ophthalmol, 96, 258–262. doi: 10.1136/bjo.2010.199851 [DOI] [PubMed] [Google Scholar]
- Sleath B, Sayner R, Blalock SJ, Carpenter DM, Muir KW, Hartnett ME,… Robin AL (2015). Patient question-asking about glaucoma and glaucoma medications during videotaped medical visits. Health Communication, 30, 660–668. doi: 10.1080/10410236.2014.888387 [DOI] [PubMed] [Google Scholar]
- Sleath BL, Blalcok SJ, Muir KW, Carpenter DM, Lawrence SD, Giangiacomo AL,… Robin AL (2014). Determinants of self-reported barriers to glaucoma medicine administration and adherence: A multisite study. Annuals of Pharmacotherapy, 48, 856–862. doi: 10.1177/1060028014529413 [DOI] [PubMed] [Google Scholar]
- Stone JL, Robin AL, Novack GD, Covert DW & Cagle GD (2009). An objective evaluation of eyedrop instillation in patients with glaucoma. Archives of Ophthalmolgy, 127, 732–736. doi: 10.1001/archophthalmol.2009.96. [DOI] [PubMed] [Google Scholar]
- Williams GC & Deci EL (2001). Activating patients for smoking cessation through physician autonomy support. Medical Care, 39, 813–823. [DOI] [PubMed] [Google Scholar]