Description
A 28-year-old man with history of hypertension sustained trauma in 2017, with closed right proximal tibial fracture. Internal fixation achieved consolidation, but was associated with varus malpositioning of the medial tibial plateau and iterative patellar luxation (figure 1A). The patient reported wound healing several weeks after surgery, and no postoperative infection was suspected. Tibial osteotomy with one-stage exchange of the fixation hardware and bone grafting was performed (figure 1B). There were no macroscopic intraoperative signs of infection. Several bone samples were sent to bacteriology and pathology. The five microbiology samples all revealed Cutibacterium acnes (eg, Propionibacterium acnes) in culture at day 14. Histology revealed plasma cell infiltration, without polymorphonuclear cells (PMNs) (figure 1C,D); histological sections of the synovial sample showed a vascular-exudative inflammatory reaction with vascular dilation, oedema between the collagen fibres and significant, predominantly perivascular, plasma cell infiltration, with more than five plasma cells per field at high magnification (400×) (figure 1D).
Figure 1.
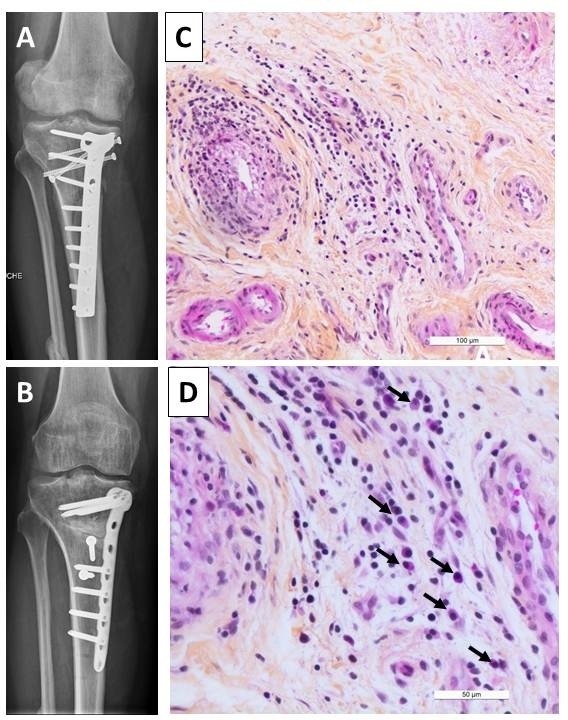
(A) X-ray showing osteosynthesis with consolidation, but with varus malpositioning of the medial tibial plateau; (B) X-ray showing the new internal fixation with bone grafting, with consolidation; (C) vascular exudative inflammatory reaction; (D) plasma cell infiltration. Black arrows indicate plasma cells.
The patient received 3-month therapy with clindamycin (600 mg 4 times/day, totalling 2400 mg/day). During the 18-months’ follow-up, consolidation was obtained, with significant improvement in function.
Fracture-related infection (FRI) is a common bone and joint infection (BJI). Diagnosis of early FRI is usually easy if the patient presents with fistula, wound breakdown or purulent discharge. Late FRI can be suspected in patients without consolidation and/or with implant loosening. Intraoperative samples are crucial to categorise patients as infected, especially if there are no clinical signs of infection. Presence of the same microorganism in culture from at least three different specimens is a confirmatory criterion for FRI.1 In our patient, despite consolidation and absence of signs of infection, all intraoperative samples revealed C. acnes, a slow-growing low-virulence bacterium frequently involved in chronic BJI. Histology can help diagnose infection, and PMN infiltration is a classical criterion for prosthetic joint infection, osteomyelitis and FRI; it is defined as >5 neutrophils per high-power field in 5 high-power fields on histological analysis of periprosthetic tissue at 400× magnification.2 However, this criterion lacks sensitivity, especially in chronic infection.3 Plasma cells are mainly present in chronic inflammatory reactions, such as inflammatory rheumatism caused by autoimmune disease, and rheumatoid arthritis in particular. Here, the only cause of chronic inflammation was chronic BJI due to C. acnes. We hypothesised that the response of the human immune system to slow-growing bacteria such as C. acnes in the context of implant-associated BJI could be mediated by plasma cells, with or without presence of PMNs. Further investigations in a cohort of patients with implant-associated chronic BJI are required to determine whether plasma cell infiltration on histology contributes to diagnosis.
Learning points.
Cutibacterium acnes fracture-related infection (FRI) could be diagnosed in patients without clinical signs of infection and with bone consolidation.
Polymorphonuclear cell infiltration could not be detected on histological analysis in patients with C. acnes FRI.
Plasma cell infiltration could be detected in patients with C. acnes FRI and may be a potential marker of such infection.
Acknowledgments
Lyon Bone and Joint Infection Study Group: Coordinator: TF; Infectious Diseases Specialists—TF, Florent Valour, Thomas Perpoint, Patrick Miailhes, Florence Ader, Sandrine Roux, Agathe Becker, Claire Triffault-Fillit, Anne Conrad, Cécile Pouderoux, Marie-Elodie Langlois, Marielle Perry, Fatiha Daoud, Johanna Lippman, Evelyne Braun, Christian Chidiac; Surgeons—Sébastien Lustig, Elvire Servien, Cécile Batailler, Romain Gaillard, Stanislas Gunst, Julien Roger, Charles Fiquet, Michel Henri Fessy, Anthony Viste, Philippe Chaudier, Jean Luc Besse, Lucie Louboutin, Gaël Gaudin, Tanguy Ledru, Adrien Van Haecke, Quentin Ode, Marcelle Mercier, Florie Alech-Tournier, Sébastien Martres, Franck Trouillet, Cédric Barrey, Emmanuel Jouanneau, Timothée Jacquesson, Ali Mojallal,
Sophie Brosset, Fabien Boucher, Hristo Shipkov, Joseph Chateau, Philippe Céruse, Carine Fuchsmann, Arnaud Gleizal; Anesthesiologists—Frédéric Aubrun, Mikhail Dziadzko, Caroline Macabéo; Microbiologists—Frederic Laurent, Laetitia Beraut, Céline Dupieux, Camille Kolenda, Jérôme Josse, Claude-Alexandre Gustave; Imaging—Fabien Craighero, Loic Boussel, Jean-Baptiste Pialat; Nuclear Medicine—Isabelle Morelec, Marc Janier, Francesco Giammarile; PK/PD specialists—Michel Tod, Marie-Claude Gagnieu, Sylvain Goutelle; Clinical research assistant and database manager—Eugénie Mabrut.
Footnotes
Contributors: TF and CB participated to the patient care. TF and AT wrote the draft of the manuscript. AT, CB, MB and TF improved the final version of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Morgenstern M, Kühl R, Eckardt H, et al. . Diagnostic challenges and future perspectives in fracture-related infection. Injury 2018;49:S83–90. 10.1016/S0020-1383(18)30310-3 [DOI] [PubMed] [Google Scholar]
- 2. Parvizi J, Tan TL, Goswami K, et al. . The 2018 definition of periprosthetic hip and knee infection: an evidence-based and validated criteria. J Arthroplasty 2018;33:1309–14. 10.1016/j.arth.2018.02.078 [DOI] [PubMed] [Google Scholar]
- 3. Bori G, Soriano A, García S, et al. . Low sensitivity of histology to predict the presence of microorganisms in suspected aseptic loosening of a joint prosthesis. Mod Pathol 2006;19:874–7. 10.1038/modpathol.3800606 [DOI] [PubMed] [Google Scholar]


