Abstract
A young man endures many years with classic symptoms of Addison’s disease due to difficulties in distinguishing this rare condition, whose features are non-specific and insidious in nature. With all facts on hand, the patient’s notable history of psychiatric disorders, namely depression, anxiety and social isolation, as well as signs of extreme fatigue and syncope may well have been caused by a gradual onset of primary adrenal insufficiency. Long delays in diagnosis are not uncommon, as in this case where the actual condition was identified just in time when the patient presented with a life-threatening cardiovascular collapse.
Keywords: adrenal disorders, adult intensive care
Background
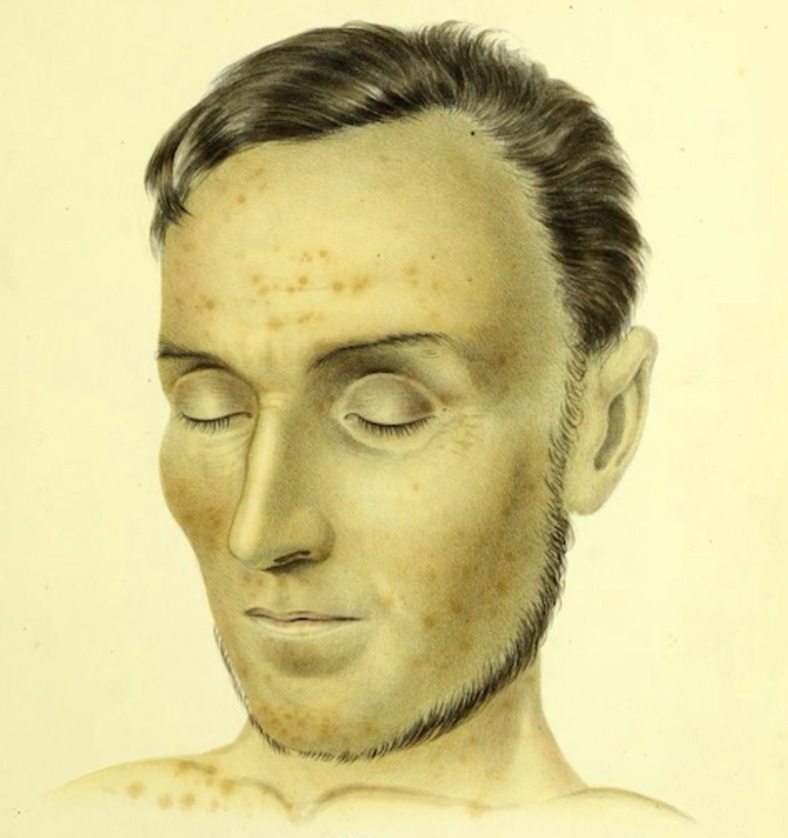
Adrenal insufficiency and its deceiving appearance were originally described by Addison.1 Addison’s compelling characterisation still persists; the discolouration of the skin, faintness, loss of appetite and extreme debility that the ‘body wastes’ and that ‘the patient at length gradually sinks and expires’ (figure 1).1 Nevertheless, over one and a half century later, we still struggle to recognise the clinical presentation and still fear the potentially fatal nature.
Figure 1.
A 58-year-old man with suspected adrenal disease, suffering from loss of appetite and great debility.1
Case presentation
A 33-year-old young man alerts an ambulance because of weakness of such a severe degree that intake of food and medications has been insufficient for some time. Postural dizziness and fatigue have bound him to the sofa, and he has slowly been deteriorating as features of social isolation, lack of concern and extreme exhaustion have become more and more prevailing.
Medical history of interest: In his adolescence, the patient underwent treatment with isotretinoin because of severe acne. The patient was diagnosed with hypothyroidism approximately 10 years ago, and at least initially complied with levothyroxine therapy. Thereafter, a concerned general practitioner referred the patient to an endocrinologist for assessment of long-standing and disabling problems with excessive sweating, accompanied by a tendency towards social isolation. Already then, the patient met criteria for moderate depression, which had not been helped by psychologist contact. During assessment by the endocrinologist, problems with upset stomach and general arthralgia were noted and it was even then morning serum cortisol was measured for the first time, resulting in a normal value of 680 nmol/L. A repeated measurement 2 years later (now year 2013) showed a lower, yet still ‘normal’ (ie, within reference range), value of 360 nmol/L. Interestingly, the patient has also been admitted to the cardiology ward because of sinus tachycardia (120 beats/min at rest and 190 beats/min during a stroll in the corridor) as well as repeated syncope, tests then suggestive of orthostatic hypotension. Additional medical history involves a vast spectrum of psychiatric disorders such as hypersomnia, depression, anxiety and social phobia along with personality traits of obsessive, compulsive and perfectionist manner. He has earlier been treated with a cocktail of psychiatric medications with little or no effect.
Family history: Mother with pernicious anaemia and hypothyroidism. Maternal grandfather with schizophrenia, who committed suicide at 37 years of age.
Shortly after the ambulance personnel’s arrival the patient becomes unconscious. The pulse in the carotid artery can be palpated but the blood pressure is immeasurable despite repeated attempts. Intraosseous access is established and Ringer‘s acetate infused. ECG shows a sinus tachycardia of 115 beats/minute, without any major pathological signs, and is even assessed by a distant cardiologist. Once in the emergency department a blood pressure of 59/18 mm Hg is found. The body temperature and plasma glucose level are normal. He receives recurrent doses of diluted norepinephrine and epinephrine, is still unconscious and therefore intubated without complications. Laboratory results reveal severe hyponatraemia (S-Na 108 mmol/L) and hyperkalaemia (S–K 5.9 mmol/L), which in combination with cardiovascular shock raises the suspicion of adrenal crisis.
Investigations, differential diagnosis and treatments
The patient receives a large dose of hydrocortisone without delay, together with several litres of intravenous crystalloids and broad-spectrum antibiotics in case infection is a precipitating factor. The patient then undergoes a head and chest CT without any significant findings (eg, pulmonary embolism) and is thereafter admitted to the intensive care unit. The major cardiovascular collapse is handled with a norepinephrine infusion, which reaches a maximum of 1.06 µg/kg/min, as well as full dose milrinone, in addition to the already mentioned fluid resuscitation. The hyponatraemia is corrected cautiously. On closer examination, it is evident that the patient exhibits classic hyperpigmentation on typical locations such as the vermilion border of the lips, the palmar creases, the knuckles and paraumbilically. Even a sacral pressure ulcer is noted. Levothyroxine is administered because of supposed concomitant hypothyroidism with overlapping symptoms, as the anamnesis suggested noncompliance. The picture may also be blurred by the patient’s malnourished state, reflected by low serum albumin and elevated prothrombin time (the latter possibly suggestive of vitamin K deficiency). Anorexia nervosa is also discussed from a differential diagnostic point of view.
Short after admission an echocardiography is performed signalling heart failure with an ejection fraction of approximately 15%–25%, the picture resembling takotsubo, that is, stress, cardiomyopathy (video 1). N-terminal pro-B-type natriuretic peptide (NT-pro-BNP) reaches a maximum value of over 35 000 ng/L. Haemodynamic compromise consequently leads to transient ischaemic hepatitis (aspartate aminotransferase (ASAT) 190 µkat/L, alanine aminotransferase (ALAT) 60 µkat/L, bilirubin 54 µmol/L, prothrombin time/international normalized ratio (PT/INR) 2.5), which is treated with acetylcysteine infusion, in addition to the already recognised prerenal failure. From day 4, there are clinical signs of successive cardiovascular improvement, which is confirmed by repeated ultrasound screenings and approximately 3 weeks following the adrenal crisis the cardiac function is found to be fully recovered. The patient regains consciousness, is successfully extubated on day 6 and eventually discharged from the intensive care unit on day 8.
Video 1.
Endocrinologists are repeatedly consulted and as the initial tests are inconclusive of adrenal insufficiency and the primary response to high-dose hydrocortisone scarce the diagnosis halters for a while. After re-examination of morning values of serum cortisol (80 nmol/L) and plasma adrenocorticotropic hormone (ACTH) (194 pmol/L, ie, over 10 times the upper limit of reference range), the diagnosis primary adrenal insufficiency is confirmed. From now on, the patient receives continuous treatment with hydrocortisone and even mineralocorticoid. Subsequent measurement of autoantibodies 21-hydroxylase (5.6 kE/L, reference <0.4) distinguishes the cause as autoimmune adrenalitis. Other rarer causes of primary adrenal insufficiency, such as infiltrative diseases, adrenoleukodystrophy, haemochromatosis and malignancy, are ruled out. Screening for celiac disease proves negative. An abdominal CT is normal.
The patient is for some inexplicable reason mute with psychomotor immobility, whereby MRI is performed to exclude central pontine myelinolysis and anoxic brain injury. Additionally, limbic encephalitis is ruled out by electroencephalography (EEG) and lumbar puncture. The state is interpreted as catatonia and several electroconvulsive therapy (ECT) sessions follow.
The succeeding recovery is truly astonishing; the patient reacquires insightfulness, becomes deeply concerned about his dishevelled appearance and even reconnects with his mother after many years of silence.
Outcome and follow-up
Thanks to the essential supplementation of hydrocortisone, along with fludrocortisone, and an acute series of ECT, this young man is revitalised and can be discharged after 5 weeks of in-hospital care. At the time of this article’s submission, approximately 11 months after the adrenal crisis, the patient is living a relatively independent life, by himself in an apartment, no longer needing home care service. The patient shows initiative, wanting to return to work after 3 years of unemployment and has now regular contact with his family. He is aware of his chronic disease that requires lifelong medication and attentiveness. Since the initiation of hydrocortisone therapy, the patient’s psychiatric state has improved considerably, and he only required mirtazapine for sleep stabilisation temporarily. The patient has no longer follow-ups via the psychiatric clinic, where they are amazed by the dramatic improvement.
Discussion
This case report highlights many important aspects of adrenal insufficiency and crisis. Above all, it illustrates the difficulty to recognise the non-specific insidious symptoms that often develop during several years and the resultant suffering the patient experiences as the diagnosis is delayed. Given the medical history, symptoms and signs may have been present for as many as 10 years; the postural hypotension, syncope, arthralgia, diarrhoea, fatigue and all the psychiatric disorders that notably did not improve by medication, were probably caused by primary adrenal insufficiency all along. The diagnosis adrenal insufficiency is extremely challenging in early stages and can even delude endocrinologists. Morning values of S-cortisol were measured both 6 and 8 years prior to the adrenal crisis, but unfortunately without concomitant assessment of ACTH—supposedly because the cortisol values were mere screening samples and the degree of suspicion was unfortunately low at the time. Since these values were within a possible normal range, it may have led to insufficient consideration and careless, incorrect, discarding of the diagnosis adrenal insufficiency. This shows that interpretation of S-cortisol is difficult and that adrenal insufficiency should not be ruled out with random values.2 Only higher values within the normal range generally exclude primary adrenal insufficiency (>550 nmol/L),3 and besides repeated evaluations one should simultaneously measure ACTH, where a morning value of double the reference range’s upper limit suggests adrenal insufficiency and thereto determines the cause as primary. Unless these results are unambiguous, it is recommended to confirm the diagnosis with the gold standard ACTH stimulation test.4 Current clinical guidelines propose that patients diagnosed with primary adrenal insufficiency should be evaluated for mineralocorticoid deficiency. However, in cases with an autoimmune origin the zona glomerulosa is often affected first, with consequential increases in plasma renin activity and normal to low serum aldosterone levels then being the earliest signs of the disease. We, therefore, contemplate whether it may be advantageous to assess a possible mineralocorticoid deficiency already in initial stages of suspected primary adrenal insufficiency to earlier approach—but note, not exclude—the diagnosis. Certainly, our patient had long-standing signs and symptoms of mineralocorticoid deficiency presenting as electrolyte disturbances, although initially subtle, as well as postural hypotension related to volume depletion. Either way it is unequivocal that we must above all raise our vigilance, more generously suspect adrenal insufficiency and allow our clinical judgement to guide us to more meticulous evaluation of possible cases.3
Besides its perplexing presentation and subtle onset, primary adrenal insufficiency is also rare why it is not uncommon that the diagnosis is delayed or missed. In fact, approximately 50% of all cases are first recognised when the patient eventually presents with a life-threatening adrenal crisis. It is, therefore, important to suspect adrenal crisis in all acutely ill patients with cardiovascular collapse. The therapeutic threshold should be low and parenteral administration of 100 mg hydrocortisone should not be delayed awaiting diagnostic measures.5 Further treatment with an additional 200 mg hydrocortisone distributed over the coming 24 hours, along with fluid replacement and careful electrolyte correction follows. Although recovery usually is quick and miraculous, improvement can sometimes withstand nearly a week, especially in cases where chronic adrenal insufficiency has gone undetected for a longer period of time and finally presents with an affected level of consciousness.6 Regarding our patient, both the medical history and the lower, yet significant, titres of 21-hydroxylase autoantibodies supports that the disease has existed, but failed to be diagnosed, for a longer period of time.7 In this specific case, the recovery was extraordinarily slow and even developed into catatonia, which is appreciated to be a result of the patient’s extremely serious medical state rather than an expression of a primary psychiatric disease.8 Even though the patient has a positive family history of psychiatric disorders, the fact that the patient’s earlier psychiatric symptoms never responded to psychiatric medications but splendidly subsided with hydrocortisone treatment makes it reasonable to believe that the psychiatric disorders were misinterpretations of adrenal insufficiency all along. The fact that the patient was under severe physical stress may also be depicted by the presence of takotsubo syndrome, and the association between adrenal insufficiency and reversible myocardial systolic dysfunction has been reported in several other cases, for instance by Ukita et al and Elikowski et al.9 10 Moreover, it is interesting that the vital steroid treatment of adrenal crisis may in fact worsen cardiac function as the myocardium then becomes even more sensitive, than the cortisone-deprived myocardium itself, to catecholamine-induced cardiomyopathy.11
Furthermore, this case report also denotes the intricate association between thyroid disease and adrenal insufficiency. On the one hand, in the presence of another autoimmune disease, for example, hypothyroidism, there is an increased risk of adrenalitis and the diagnostic boundary for primary adrenal insufficiency should be lowered.12 On the other hand, an elevated thyroid-stimulating hormone (TSH) may be a mere feature of adrenal insufficiency, predating many other signs or symptoms.13 Note that in these cases treatment with levothyroxine may actually precipitate an adrenal crisis. Regarding our patient, he was diagnosed with hypothyroidism a decade ago, based on a slight increase in TSH (5.6 mlU/L), while T4 and antithyroid peroxidase antibodies were normal. As the patient was critically ill suffering from adrenal crisis, thyroidal laboratory results unsurprisingly indicated low T3 syndrome and are thus insignificant. Time will tell whether the patient actually suffers from hypothyroidism in addition to Addison’s disease, or if levothyroxine therapy, which already has been halved, can be ceased completely as thyroid hormone status may normalise by hydrocortisone treatment.
This is only one of many cases that depicts the diagnostic struggle of Addison’s disease. It is frequently mistaken for psychiatric disorders, such as depression, apathy, anxiety or even psychosis, and already in the originally described cases by Addison it is obvious that these traits often precede other symptoms.1 14 Another case, strikingly similar to our own, describes a young man lacking concern for his deteriorating health, who was appreciated to suffer from both obsessional traits and depression; later a mistaken diagnosis of anorexia nervosa was made before primary adrenal insufficiency was confirmed.15 Other cases presenting as anorexia nervosa can be found in the literature, which is not surprising given that vomiting along with weight loss are common manifestations of adrenal insufficiency.16 Even then, as always, the cardinal sign of extreme fatigue prevails and the importance of suspecting and not so readily dismissing this rare diagnosis cannot be stressed enough, before the symptoms of debility and lack of concern for their own physical state make the affected ‘sink and expire’ and eventually encounter a life-threatening adrenal crisis at a much too young age.
Patient’s perspective.
‘As I reminisce about the past, the most striking features were exhaustion and fatigue, which demanded an extraordinary amount of sleep. The faintness and dizziness disabled me, and I was eventually affected by amnesia for a longer period, from approximately 2 months before the adrenal crisis until after the third ECT session. All the earlier unspecific signs, especially the psychiatric symptoms that were so difficult to treat, made me feel like a hopeless case—but now with the correct diagnosis and treatment, I have hope for the future.’
Learning points.
All acutely ill patients who present with possible signs of adrenal crisis, such as cardiovascular collapse, should immediately be treated with 100 mg hydrocortisone intravenously. The therapeutic threshold for administering the life-saving drug should be low and not delayed by diagnostic measures.17
Suspect chronic adrenal insufficiency in patients with gradual onset of non-specific symptoms such as fatigue, postural dizziness, weight loss, gastrointestinal manifestations or psychiatric disorders. The condition should not be ruled out by a single cortisol measurement, instead our clinical judgement should guide us to more dedicatedly reevaluate suspected cases.
An elevated TSH may be a feature of Addison’s disease, and note that thyroxine therapy can precipitate an adrenal crisis in these individuals.18
Footnotes
Contributors: PJ and LB have treated the patient and planned for the case report. The manuscript was primarily written by PJ and revised by LB.
Funding: This study was funded by The Swedish state under the agreement between the Swedish government and the county councils, the ALF agreement grand number(ALFGBG-772521); The Healthcare Board, Region Västra Götaland grand number (VGFOUREG-833561).
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Addison T. On the constitutional and local effects of disease of the suprarenal capsules. D. Highley, London, 1855. Available: https://archive.org/details/b21298786/page/n5
- 2. Elsevier Point of Care Primary adrenal insufficiency, clinical overview. Available: https://www.clinicalkey.com/#!/content/67-s2.0-74c5f862-11e4-4bfd-abe8-8409af9fe071 [Accessed 8 May 2019].
- 3. Charmandari E, Nicolaides NC, Chrousos GP. Adrenal insufficiency. The Lancet 2014;383:2152–67. 10.1016/S0140-6736(13)61684-0 [DOI] [PubMed] [Google Scholar]
- 4. Bornstein SR, Allolio B, Arlt W, et al. . Diagnosis and treatment of primary adrenal insufficiency: an endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2016;101:364–89. 10.1210/jc.2015-1710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Amrein K, Martucci G, Hahner S. Understanding adrenal crisis. Intensive Care Med 2018;44:652–5. 10.1007/s00134-017-4954-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Allolio B. Extensive expertise in endocrinology: adrenal crisis. Eur J Endocrinol 2015;172:R115–24. 10.1530/EJE-14-0824 [DOI] [PubMed] [Google Scholar]
- 7. Degros V, Pons L, Ghulam A, et al. . [21-hydroxylase autoantibodies as a marker of adrenal involvement in patients with autoimmune endocrinopathies]. Ann Biol Clin 1999;57:705–9. [PubMed] [Google Scholar]
- 8. Daniels J. Catatonia: clinical aspects and neurobiological correlates. J Neuropsychiatry Clin Neurosci 2009;21:371–80. 10.1176/jnp.2009.21.4.371 [DOI] [PubMed] [Google Scholar]
- 9. Ukita C, Miyazaki H, Toyoda N, et al. . Takotsubo cardiomyopathy during acute adrenal crisis due to isolated adrenocorticotropin deficiency. Intern Med 2009;48:347–52. 10.2169/internalmedicine.48.1662 [DOI] [PubMed] [Google Scholar]
- 10. Elikowski W, Małek-Elikowska M, Greberska W, et al. . Takotsubo syndrome in a patient with adrenal insufficiency, severe hyponatremia and coexistent coronary artery disease. Pol Merkur Lekarski 2019;46:182–6. [PubMed] [Google Scholar]
- 11. Gupta S, Goyal P, Idrees S, et al. . Association of endocrine conditions with takotsubo cardiomyopathy: a comprehensive review. J Am Heart Assoc 2018;7:e009003 10.1161/JAHA.118.009003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Barthel A, Benker G, Berens K, et al. . An update on Addison's disease. Exp Clin Endocrinol Diabetes 2019;127:165–75. 10.1055/a-0804-2715 [DOI] [PubMed] [Google Scholar]
- 13. Saevik Å B, Åkerman A-K, Grønning K, et al. . Clues for early detection of autoimmune Addison's disease - myths and realities. J Intern Med 2018;283:190–9. 10.1111/joim.12699 [DOI] [PubMed] [Google Scholar]
- 14. Nieman LK. Clinical manifestations of adrenal insufficiency in adults. UpToDate. topic 159, version 13.0. Available: https://www.uptodate.com/contents/clinical-manifestations-of-adrenal-insufficiency-in-adults?search=Clinical%20manifestations%20of%20adrenal%20insufficiency%20in%20adults.&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1 [Accessed 23 Apr 2019].
- 15. Tobin MV, Morris AI. Addison's disease presenting as anorexia nervosa in a young man. Postgrad Med J 1988;64:953–5. 10.1136/pgmj.64.758.953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nicholls K, Boggis N, Pandya N. Anorexia nervosa: a mistaken diagnosis. BMJ Case Rep 2016;2016:bcr2015214058 10.1136/bcr-2015-214058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Arlt W, Society for Endocrinology Clinical Committee . Society for endocrinology endocrine emergency guidance: emergency management of acute adrenal insufficiency (adrenal crisis) in adult patients. Endocr Connect 2016;5:G1–3. 10.1530/EC-16-0054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shaikh MG, Lewis P, Kirk JMW. Thyroxine unmasks Addison's disease. Acta Paediatr 2004;93:1663–5. 10.1111/j.1651-2227.2004.tb00860.x [DOI] [PubMed] [Google Scholar]