Description
A 66-year-old man presented with abdominal pain, testicular swelling and weight loss. He was initially investigated with a CT of his chest, abdomen and pelvis and a testicular ultrasound. The CT revealed a mediastinal mass, a solitary pulmonary nodule and an exophytic mass arising from the gastric fundus (figure 1A–E). The mediastinal mass was slightly heterogeneous, invading the superior vena cava (SVC) and right atrium (figure 1A–C). The gastric mass showed heterogeneous enhancement with gastric wall thickening and luminal narrowing (figure 1D). Ultrasound imaging of the testis demonstrated a well-defined heterogeneous, hyporeflective lesion with peripheral vascularity (figure 2A,B). Further evaluation with 18F-FDG PET/CT showed mild to moderate FDG uptake in the thoracic and gastric lesions (figure 2C and D). MRI confirmed the invasion of the right atrium and SVC (figure 2E).
Figure 1.
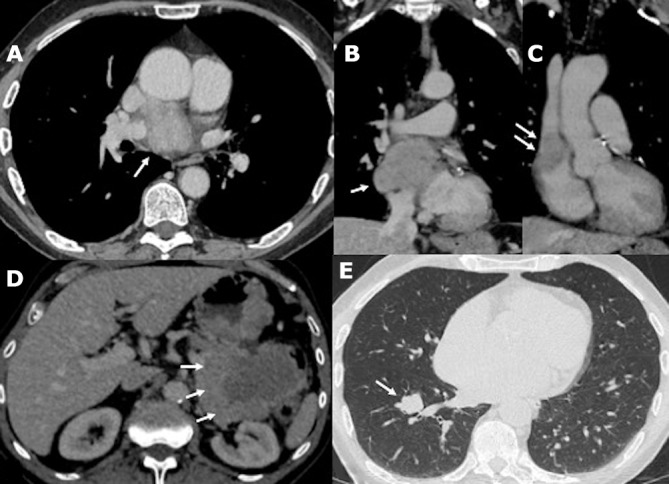
(A–C) Contrast-enhanced CT images with axial and coronal reconstructions show a slightly heterogeneous mediastinal mass with right atrial and superior vena cava invasion (arrows). (D) Axial contrast-enhanced CT image shows a heterogeneous enhancing gastric mass with exophytic and intraluminal components (arrows). (E) Axial CT image shows a single lung nodule is demonstrated within the right lower lobe (arrow).
Figure 2.
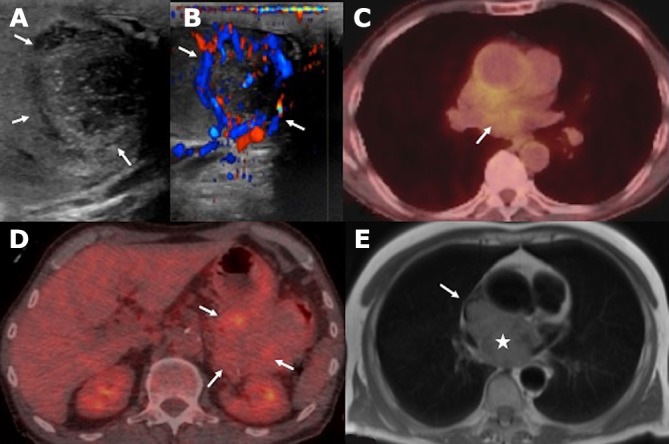
(A, B) Testicular ultrasound with B-mode and colour Doppler shows a heterogeneous, hyporeflective lesion with peripheral vascularity (arrows). (C, D) PET/CT images show moderate FDG uptake of the mediastinal mass and mild metabolic activity of the gastric mass (arrows). (E) Axial post-gadolinium T1 MR imaging of the thorax confirms the aggressive features of the mediastinal mass with right atrial (asterisk) and superior vena cava invasion (arrow).
A diagnosis of extramedullary plasmacytoma was established following gastroscopy and gastric biopsy. Bone marrow aspirate and trephine revealed no myeloma infiltration but biochemically he had oligosecretory disease with an IgG Kappa paraprotein of 8 g/L at presentation. Histology following orchiectomy confirmed plasmacytoma. The patient was treated with standard first-line treatment for myeloma (bortezomib, thalidomide and dexamethasone), but despite showing an initial partial response to treatment, his disease subsequently progressed and treatment was therefore escalated to dexamethasone, thalidomide, cisplatin, doxorubicin, cyclophosphamide and etoposide with near complete response.
Plasma cell dyscrasias can present with soft-tissue lesions in the context of multiple myeloma; the lesions either originate from bone or occur secondary to haematogenous spread, in which case they are called extramedullary plasmacytomas (EMPs). Solitary plasmacytomas present as single soft-tissue masses without systemic involvement, either originating from bone (solitary osseous plasmacytoma) or soft tissues, when they are termed solitary extramedullary plasmacytoma (SEP).1–3 SEP is rare, accounting for 3% of all plasma cell neoplasms.4 Differentiation between EMP and SEP is clinically important from a prognostication point of view, as survival outcomes are worse in EMP.5 Accurate diagnosis is also important in terms of initiating treatment, as SEP is potentially curative with localised radiotherapy.6 However, there remains no clear consensus regarding treatment for multifocal SEPs, and in practice as described in this case, these are often treated as myeloma.
SEP can occur anywhere in the body, with head and neck being the the most common site of disease. Involvement of the mediastinum, retroperitoneum or gastrointestinal tract is rare.7 In fact, multifocal disease with simultaneous involvement of multiple sites, as in our case, is rarely reported.2 8 There is limited literature on the cross-sectional imaging appearances of SEP, with conflicting reports on the pattern of contrast enhancement and invasion into the adjacent vasculature. Yoon et al described two cases of gastric SEP that demonstrated gastric wall thickening and poor enhancement.9 In contrast to this, Zhao et al described a well-circumscribed extraluminal gastric mass showing homogeneous contrast enhancement.10 There are only a handful of reports on intrathoracic SEPs. Sato et al reported a well-defined homogeneous mediastinal lesion without vascular invasion.4 On the other hand, Zhang et al described a mediastinal SEP that occluded the right pulmonary artery and invaded the SVC.11 Testicular SEP can have variable appearances on ultrasound, but as in our case, the most widely described sonographic appearance is that of a hyporeflective, heterogeneous mass with increased vascularity.12 13 However, there are cases of diffusely enlarge, heterogeneous testicles without a focal lesion.14 15 Similar to our case, the majority of the described pulmonary SEPs present as a solitary nodule or mass; however, reticulonodular opacities have also been described.16 17
The described heterogeneity on imaging can be diagnostically challenging, resulting in a broad differential diagnosis including lymphoma and metastases.18
Learning points.
Extramedullary plasmacytomas can present anywhere in the body. The differential diagnosis includes lymphoma and metastases. A background of multiple myeloma can narrow the differential diagnosis.
The imaging features tend to be that of infiltrative soft-tissue masses with varying degree of vascularity and invasion into the neighbouring structures.
Solitary extramedullary plasmacytoma (SEP) is a very rare plasma cell dyscrasia with a better prognosis than multiple myeloma. Radiological suspicion of the features of SEP in the absence of multiple myeloma is important leading to early diagnosis and prompt treatment.
Footnotes
Contributors: Identified the case: HR, KS. Conception and design: KS. Literature search: JG. Drafting the manuscript: JG, CA. Revising the manuscript critically for important intellectual content: HR, KS, CA, JG. Final approval of the version to be published: HR, KS, CA, JG.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Touzeau C, Moreau P. How I treat extramedullary myeloma. Blood 2016;127:971–6. 10.1182/blood-2015-07-635383 [DOI] [PubMed] [Google Scholar]
- 2. Naymagon L, Abdul-Hay M. Primary extramedullary plasmacytoma with diffuse lymph node involvement: a case report and review of the literature. J Med Case Rep 2019;13 10.1186/s13256-019-2087-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bladé J, Fernández de Larrea C, Rosiñol L, et al. Soft-tissue plasmacytomas in multiple myeloma: incidence, mechanisms of extramedullary spread, and treatment approach. JCO 2011;29:3805–12. 10.1200/JCO.2011.34.9290 [DOI] [PubMed] [Google Scholar]
- 4. Sato K, Fumimoto S, Fukada T, et al. Extramedullary plasmacytoma arising from the anterior mediastinum. Ann Thorac Surg 2017;103:e393–5. 10.1016/j.athoracsur.2016.10.064 [DOI] [PubMed] [Google Scholar]
- 5. Sevcikova S, Minarik J, Stork M, et al. Extramedullary disease in multiple myeloma—controversies and future directions. Blood Rev 2019;36:32–9. 10.1016/j.blre.2019.04.002 [DOI] [PubMed] [Google Scholar]
- 6. Pan-London Haemato-Oncology clinical guidelines; plasma cell disorders, 2018. Available: https://www.kingshealthpartners.org/institutes/haematology/pan-london-blood-cancer-guidelines [Accessed 24 Oct 2019].
- 7. Daghighi MH, Poureisa M, Shimia M, et al. Extramedullary plasmacytoma presenting as a solitary mass in the intracranial posterior fossa. Iran J Radiol 2012;9:223–6. 10.5812/iranjradiol.8759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ooi GC, Chim JC-S, Au W-Y, et al. Radiologic manifestations of primary solitary extramedullary and multiple solitary plasmacytomas. AJR Am J Roentgenol 2006;186:821–7. 10.2214/AJR.04.1787 [DOI] [PubMed] [Google Scholar]
- 9. Yoon SE, Ha HK, Lee YS, et al. Upper gastrointestinal series and CT findings of primary gastric plasmacytoma: report of two cases. AJR Am J Roentgenol 1999;173:1266–8. 10.2214/ajr.173.5.10541102 [DOI] [PubMed] [Google Scholar]
- 10. Zhao Z-H, et al. Imaging findings of primary gastric plasmacytoma: a case report. WJG 2014;20 10.3748/wjg.v20.i29.10202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zhang H, Miao Q, Liu J, et al. Complete resection of a mediastinal solitary extramedullary plasmacytoma and reconstruction of right pulmonary artery and superior vena cava. Ann Thorac Surg 2011;92:2244–6. 10.1016/j.athoracsur.2011.05.047 [DOI] [PubMed] [Google Scholar]
- 12. Bude RO. Testicular plasmacytoma: appearance on gray-scale and power Doppler sonography. J Clin Ultrasound 1999;27:345–6. [DOI] [PubMed] [Google Scholar]
- 13. Croft GV, Albertyn LE. Sonographic appearance of plasmacytoma of the testis. Australas Radiol 1992;36:265–7. 10.1111/j.1440-1673.1992.tb03167.x [DOI] [PubMed] [Google Scholar]
- 14. Bortolotto C, Ori-Belometti G, Rodolico G, et al. Plasmacytoma of the testis in a patient with previous multiple myeloma: sonographic appearance. J Ultrasound 2016;19:153–5. 10.1007/s40477-016-0196-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lue K, Emtage JB, Pariñas MA, et al. An extramedullary plasmacytoma located in the testicle: a case report and review of the literature. Can Urol Assoc J 2015;9:240–2. 10.5489/cuaj.2531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kim S-H, Kim TH, Sohn JW, et al. Primary pulmonary plasmacytoma presenting as multiple lung nodules. Korean J Intern Med 2012;27:111–3. 10.3904/kjim.2012.27.1.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lazarevic V, Cemerikic-Martinovic V, Suvajdzic N, et al. Diffuse primary plasmacytoma of the lung. Haematologia 2001;31:161–5. 10.1163/15685590152492972 [DOI] [PubMed] [Google Scholar]
- 18. Hall MN, Jagannathan JP, Ramaiya NH, et al. Imaging of extraosseous myeloma: CT, PET/CT, and MRI features. AJR Am J Roentgenol 2010;195:1057–65. 10.2214/AJR.10.4384 [DOI] [PubMed] [Google Scholar]


