Abstract
A 39-year-old Caucasian man presented with headaches and retro-orbital pain but normal vision. Bilateral optic nerve swelling was found on funduscopy though optic nerve function and computed perimetry were normal and there was no relative afferent pupillary defect. CT venogram and MRI were unremarkable. Cerebrospinal fluid (CSF) opening pressure was normal on lumbar puncture and Treponema pallidum antibodies and T. pallidum particle agglutination test were positive on CSF analysis. He tested negative for HIV. Symptoms rapidly resolved with 2 weeks of intravenous benzylpenicillin. At 1 month follow-up, the right optic nerve swelling had reduced while the left optic nerve swelling had increased; his vision remained unaffected and he was symptom free and continued to have no objective evidence of optic nerve dysfunction.
Keywords: syphilis, visual pathway
Background
Syphilis is a sexually transmitted bacterial infection caused by the spirochete Treponema pallidum. The WHO estimated 18 million prevalent cases worldwide in individuals aged 15–49 in 2012 and 5.6 million new cases that year.1 The number of identified cases of syphilis has risen in the past two decades with a current median case rate of 17.7 cases per 100 000 men and 17.2 cases per 100 000 women.2 Approximately 58% of new diagnoses of primary and secondary syphilis in 2017 occurred in men who have sex with men.3 It has been estimated that an HIV coinfection occurs in 45% of this population, compared with 9% of cases in men who have sex with women and 4.5% of women.3
Syphilis is unique among sexually transmitted infections in that it can affect any part of the eye at any stage of the disease, including the cornea, the anterior and posterior uvea, the retina and its vasculature and the optic nerve.4 We describe a rare case of bilateral syphilitic optic perineuritis in an HIV-negative patient with no visual symptoms and no demonstrable optic nerve dysfunction.
Case presentation
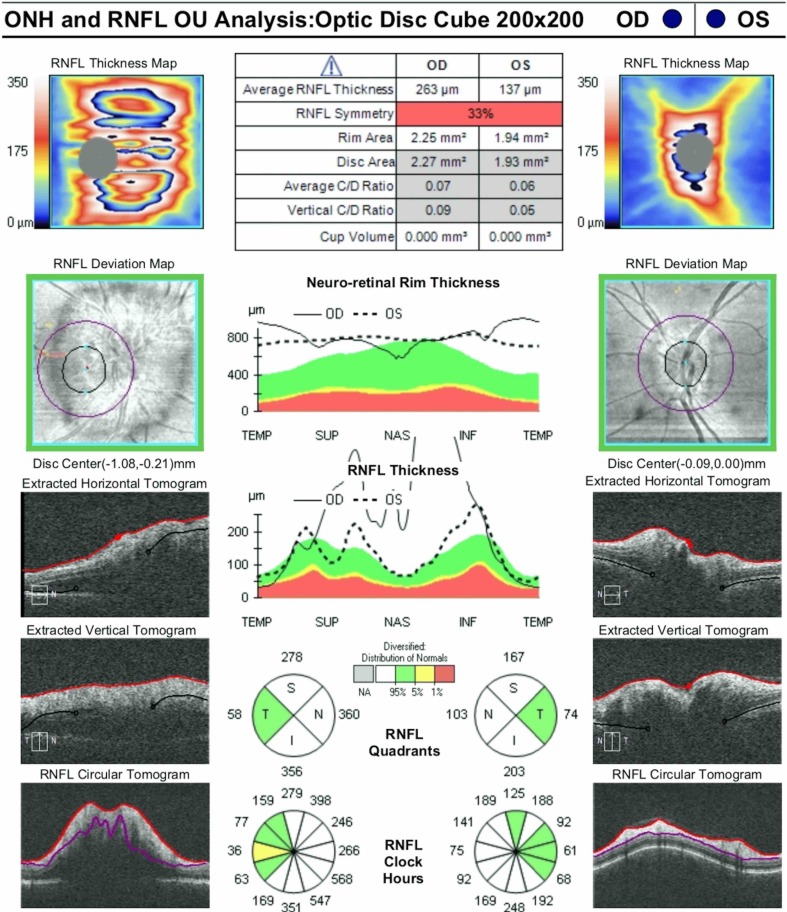
A 39-year-old Caucasian man presented to an eye emergency department following 3 weeks of intermittent headaches occurring on both temples and retro-orbital pain (right worse than left) that worsened with eye movement. He denied any changes to his vision. He was emmetropic and had no prior ocular history. He took desvenlafaxine for major depressive disorder and Truvada for HIV pre-exposure prophylaxis. He was in a same-sex open relationship and engaged in casual unprotected sexual encounters with several male partners. Screening for sexually transmitted infections within the past 6 months was negative. He denied intravenous drug use. On examination, his uncorrected visual acuity was 6/6 right eye and 6/6 left eye. Intraocular pressure was 11 mm Hg right eye and 14 mm Hg left eye. Pupillary constriction to light and accommodation was brisk in each eye, and there was no relative afferent pupillary defect in either eye. There was no subjective brightness desaturation, and colour vision on Ishihara plate testing was normal in both eyes. Anterior segment examination was normal, with no conjunctival injection, keratic precipitates, anterior chamber cells or vitreous cells. Dilated funduscopy revealed bilateral swollen optic nerves (worse in the right eye) with blurred disc margins (figures 1 and 2). The remainder of the retinal examination was normal, with no retinitis or vasculitis. Average retinal nerve fibre layer (RNFL) thickness on optical coherence tomography (OCT) was 263 µm right eye and 137 µm left eye (figure 3). Visual fields on 24–2 Humphrey computed perimetry were full in each eye, with no central scotoma or enlarged blind spot. Peripheral neurological examination and systemic physical examination was unremarkable.
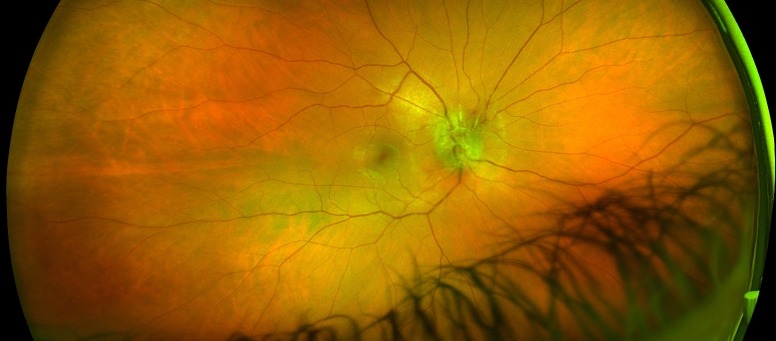
Figure 1.
Colour fundus photograph of the right eye at presentation, demonstrating optic nerve head swelling and blurred margins.
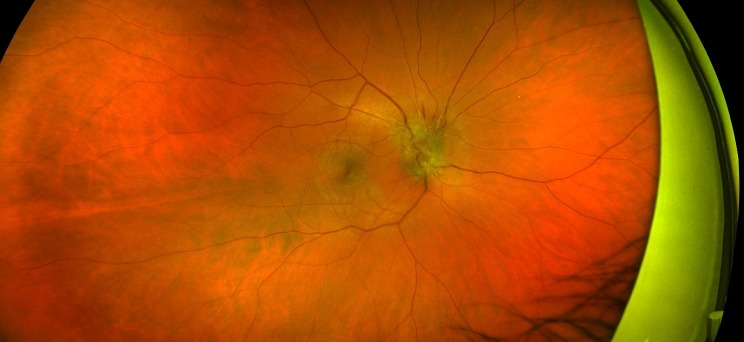
Figure 2.
Colour fundus photograph of the left eye at presentation, demonstrating mild optic nerve head swelling and blurred nasal margins.
Figure 3.
Optical coherence tomography of the retinal nerve fibre layers of both optic nerves at presentation. OD, oculus dexter; ONH, optic nerve head; OS, oculus sinister; OU, oculus uterque; RNFL, retinal nerve fibre layer; INF, inferior; NAS, nasal; SUP, superior; TEMP, temporal.
Investigations
CT venogram did not demonstrate dural venous sinus thrombosis, mass lesion or radiological features of raised intracranial pressure. MRI imaging of the brain and spinal cord was unremarkable, and there was no gadolinium enhancement. Erythrocyte sedimentation rate was 16 mm/hour, and C-reactive protein was 7 mg/L. White cell count was within normal limits at 7.50×109/L. HIV antigen/antibody test was negative. Serum T. pallidum antibodies were detected, rapid plasma reagin (RPR) was reactive (titre 1:128), and T. pallidum particle agglutination (TPPA) screen was reactive (titre >1:320). A lumbar puncture was performed with an opening pressure of 17 cmH2O. Cerebrospinal fluid (CSF) protein was 0.50 g/L, and glucose was 3.8 mmol/L. CSF T. pallidum antibodies were detected, and TPPA screen was reactive (titre 1:80). CSF PCR for Epstein-Barr virus, cytomegalovirus, herpes simplex virus 1 and 2, enterovirus, adenovirus and cryptococcus were not detected.
Differential diagnosis
Syphilitic optic neuritis is distinct from syphilitic optic perineuritis in that the former will feature gadolinium enhancement of the optic nerve on MRI imaging.5 Typical optic neuritis and other causes of atypical optic neuritis beyond syphilis must be considered in cases of painful optic nerve swelling (particularly if unilateral) as optic neuritis presents with similar symptoms. MRI with gadolinium is an important investigation in optic neuritis as enhancement of the optic nerve on MRI would occur in typical optic neuritis.6 Other causes of atypical optic neuritis (such as sarcoidosis, HIV, Bartonella, neuromyelitis optica (NMO) and systemic lupus erythematosus) are excluded through history and relevant investigations (eg, serum ACE, HIV serology, Bartonella serology, anti-NMO antibodies and antinuclear antibodies).7–9
Treatment
Following the diagnosis of neurosyphilis, the patient was treated with intravenous benzylpenicillin 1.8 g 4 hourly for a total of 14 days.
Outcome and follow-up
At completion of treatment, the patient noted cessation of his headaches, and retro-orbital pain and his vision remained unaffected. After 1 month, his right optic nerve swelling had improved on funduscopy (figure 4), and the average RNFL thickness had reduced to 238 µm. His left optic nerve appeared slightly more swollen (figure 5), and RNFL thickness had increased to 201 µm. However, he remained asymptomatic, and uncorrected visual acuity was stable at 6/6 in each eye. His syphilis serology at 1 month remained unchanged despite treatment, with T. pallidum antibodies detected, reactive RPR (titre 1:128) and reactive TPPA (titre >1:320). He continued to have no evidence of optic nerve dysfunction with no relative afferent pupillary defect, normal colour vision and no visual field defects on computed perimetry.
Figure 4.
Colour fundus photograph of the right eye at 1 month follow-up, demonstrating mild improvement in optic nerve head swelling. A superior peripapillary splinter haemorrhage has developed.
Figure 5.
Colour fundus photograph of the left eye at 1 month follow-up, demonstrating mild increase in optic nerve head swelling at the nasal margin.
Discussion
Incidence of syphilis is increasing in spite of availability of effective diagnosis and treatment.10 The overall increase in syphilis incidence has naturally led to an increased prevalence of ocular syphilitic involvement.11 Ocular involvement is reported to occur in less than 1% to 10% of all cases of syphilis,12–15 with the optic nerve involved in approximately 20% of cases of ocular syphilis.11 Syphilis was responsible for 2.27% of cases of optic neuritis in one study involving 132 patients.16 It is important to exclude syphilis as a differential diagnosis of optic nerve swelling as treatment with corticosteroids for presumed inflammatory causes (such as typical optic neuritis or sarcoidosis) may worsen cases of neurosyphilis.17 The patient in this case did not present with any features of optic nerve dysfunction in either eye, and he was visually asymptomatic at presentation during the treatment course and even during follow-up when his left optic nerve swelling had worsened on funduscopy and OCT. To the author’s knowledge, bilateral syphilitic optic neuropathy in an HIV-negative patient has only been reported twice in the literature,18 19 and only one of those cases was visually asymptomatic.19 No reported cases have featured lack of demonstrable optic nerve dysfunction on examination.
Due to the frequency of eye involvement and optic nerve involvement in syphilis, health practitioners should have a low threshold to refer patients to an ophthalmologist for a comprehensive dilated examination with any eye symptoms reported by affected patients. Syphilis must be considered as a differential diagnosis in all cases of optic nerve swelling,20 especially as early treatment with penicillin remains effective with high cure rates.4 21 However, poor visual outcome in spite of prompt treatment has been reported.22
Learning points.
Syphilis must be excluded in all cases of unilateral or bilateral optic nerve swelling, regardless of symptoms, HIV status, gender and sexual orientation.
Treatment of optic neuritis with parenteral corticosteroids should be deferred until syphilis has been excluded.
Treatment with intravenous penicillin for 2 weeks remains an effective mainstay of treatment with usually excellent outcomes.
Health practitioners should have a low threshold to refer patients to an ophthalmologist following a diagnosis of syphilis.
Patients diagnosed with syphilis in a non-sexual health or genitourinary medicine setting should be referred to a specialist sexual health service for a full sexual health screen for all other sexually transmitted infections. Advice regarding prevention (eg, barrier protection and pre-exposure prophylaxis) and contact tracing should be provided.
Footnotes
Contributors: JY is the sole author and contributor to this work.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Newman L, Rowley J, Vander Hoorn S, et al. Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and global reporting. PLoS One 2015;10:e0143304 10.1371/journal.pone.0143304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization Report on globally sexually transmitted infection surveillance, 2015. Available: http://apps.who.int/iris/bitstream/handle/10665/249553/9789241565301-eng.pdf;jsessionid=25DA348EE7CDFC387C271F7767AFD756?sequence=1a [Accessed on May 16, 2018].
- 3. United States Centers for Disease Control and Prevention Sexually transmitted disease surveillance, 2017. Available: https://www.cdc.gov/std/stats17/tables/27.htm [Accessed on February 15, 2019].
- 4. Kiss S, Damico FM, Young LH. Ocular manifestations and treatment of syphilis. Semin Ophthalmol 2005;20:161–7. 10.1080/08820530500232092 [DOI] [PubMed] [Google Scholar]
- 5. Wals KT, Ansari H, Kiss S, et al. Simultaneous occurrence of neuroretinitis and optic perineuritis in a single eye. J Neuroophthalmol 2003;23:24–7. 10.1097/00041327-200303000-00006 [DOI] [PubMed] [Google Scholar]
- 6. Purvin V, Kawasaki A, Jacobson DM. Optic perineuritis: clinical and radiographic features. Arch Ophthalmol 2001;119:1299–306. 10.1001/archopht.119.9.1299 [DOI] [PubMed] [Google Scholar]
- 7. Jenkins TM, Toosy AT. Optic neuritis: the eye as a window to the brain. Curr Opin Neurol 2017;30:61–6. 10.1097/WCO.0000000000000414 [DOI] [PubMed] [Google Scholar]
- 8. Voss E, Raab P, Trebst C, et al. Clinical approach to optic neuritis: pitfalls, red flags and differential diagnosis. Ther Adv Neurol Disord 2011;4:123–34. 10.1177/1756285611398702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Warren FA. Atypical optic neuritis. J Neuroophthalmol 2014;34:e12–13. 10.1097/WNO.0000000000000180 [DOI] [PubMed] [Google Scholar]
- 10. Patton ME, Su JR, Nelson R, et al. Primary and secondary syphilis--United States, 2005-2013. MMWR Morb Mortal Wkly Rep 2014;63:402–6. [PMC free article] [PubMed] [Google Scholar]
- 11. Tucker JD, Li JZ, Robbins GK, et al. Ocular syphilis among HIV-infected patients: a systematic analysis of the literature. Sex Transm Infect 2011;87:4–8. 10.1136/sti.2010.043042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Apinyawasisuk S, Poonyathalang A, Preechawat P, et al. Syphilitic optic neuropathy: re-emerging cases over a 2-year period. Neuroophthalmology 2016;40:69–73. 10.3109/01658107.2015.1134586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Oliver SE, Aubin M, Atwell L, et al. Ocular syphilis - eight jurisdictions, United States, 2014-2015. MMWR Morb Mortal Wkly Rep 2016;65:1185–8. 10.15585/mmwr.mm6543a2 [DOI] [PubMed] [Google Scholar]
- 14. Tamesis RR, Foster CS. Ocular syphilis. Ophthalmology 1990;97:1281–7. 10.1016/S0161-6420(90)32419-3 [DOI] [PubMed] [Google Scholar]
- 15. Chao JR, Khurana RN, Fawzi AA, et al. Syphilis: reemergence of an old adversary. Ophthalmology 2006;113:2074–9. 10.1016/j.ophtha.2006.05.048 [DOI] [PubMed] [Google Scholar]
- 16. Qiu H, Wei S. Clinical analysis of the etiology of optic neuritis in patients at different ages in China. Eye Sci 2012;27:98–101. 10.3969/j.issn.1000-4432.2012.02.010 [DOI] [PubMed] [Google Scholar]
- 17. Rescigno RJ, Glatman M, Patel SN. A complicated case of sarcoidosis. Neurosyphilis. JAMA Ophthalmol 2014;132:649–50. 10.1001/jamaophthalmol.2014.179 [DOI] [PubMed] [Google Scholar]
- 18. Nolan NS, Gibbons LE, Hepburn MA, et al. Optic neuritis caused by the re-emerging great masquerader. BMJ Case Rep 2018;11:e225635 10.1136/bcr-2018-225635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Parker SE, Pula JH. Neurosyphilis presenting as asymptomatic optic perineuritis. Case Rep Ophthalmol Med 2012;2012:621872 10.1155/2012/621872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Klein A, Fischer N, Goldstein M, et al. The great imitator on the rise: ocular and optic nerve manifestations in patients with newly diagnosed syphilis. Acta Ophthalmol 2019;97:e641–7. 10.1111/aos.13963 [DOI] [PubMed] [Google Scholar]
- 21. Workowski KA, Bolan GA, Centers for Disease Control and Prevention . Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 2015;64:1–137. [PMC free article] [PubMed] [Google Scholar]
- 22. Kowalski T, Fuzzard D, Williams I, et al. Bilateral syphilitic optic neuropathy with secondary autoimmune optic neuropathy and poor visual outcome. Case Rep Ophthalmol 2019;10:81–8. 10.1159/000496142 [DOI] [PMC free article] [PubMed] [Google Scholar]