Introduction
Defining clinical margins of lentigo maligna (LM), lentigo maligna melanoma (LMM), and acral melanoma can be challenging when planning surgical excision. This is mainly due to the presence of pathology in normal-looking or lightly pigmented surrounding skin, which can result in incomplete excisions. The Wood lamp has many useful applications in dermatology practice, including skin infections (erythrasma, tinea capitis), pigmentary changes (vitiligo, melasma), and porphyria. However, publications addressing its use in dermatology surgery are scarce. We present a case series of 5 patients who presented to our clinic with suspicious pigmented lesions.
Case Presentation
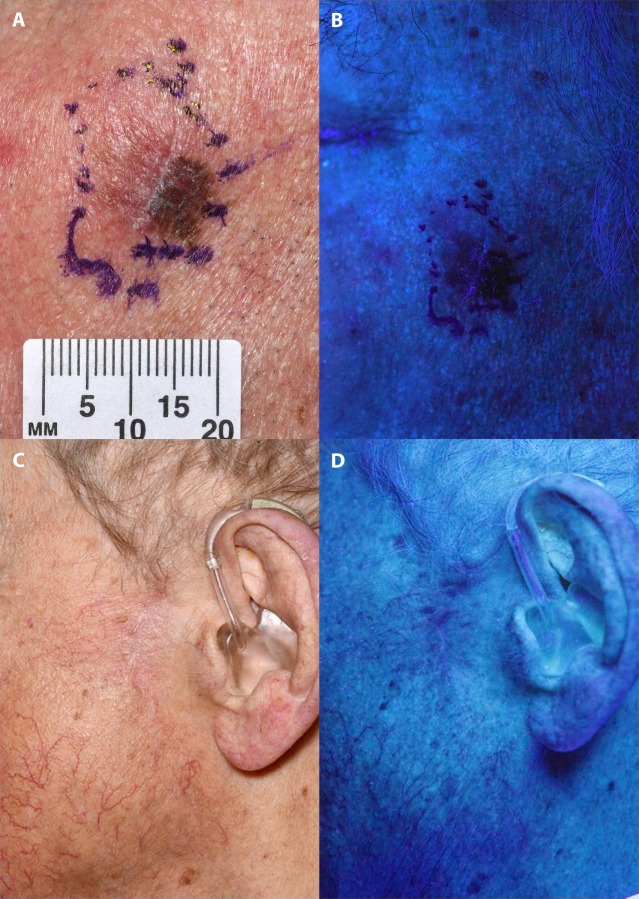
In our cohort of 5 patients (3 male, 2 female) the mean age was 77 years old (range 67–86). The lesions were on the face (n = 3), scalp (n = 1), and toe (n = 1). Nikon D33S camera (Nikon, Tokyo, Japan) was used for clinical photography and Heine Delta 20T dermatoscope (Heine Optotechnik, Herrsching, Germany) was used for dermoscopic images. All patients were examined under Wood lamp (365 nm) in a dark, windowless room. Digital photographs were captured and saved in the patients’ e-records to be reviewed before surgery. As seen in Figure 1, A and B, Wood light examination demonstrated hyperchromatic areas extending beyond the clinically/dermoscopic discernible pigmentation. These findings guided the surgeon to determine the surgical margins (0.5 cm) using Wood light. Complete excision demonstrated by histological clearance was achieved in all 5 cases, confirmed by parallel sections of the margins. One patient who had LMM with Breslow 0.3 mm required further wide local excision. Two of the 5 patients were examined under Wood lamp following previous incomplete excisions (with 0.5 cm margin) where no baseline Wood lamp examination was undertaken. The site and extent of residual LM were clearly visible under Wood lamp (Figure 1, C and D), facilitating complete clearance in the re-excision.
Figure 1.
(A,B) A lentiginous melanoma on the left cheek. Wood light illuminates the area lacking pigment anteriorly and superiorly. (C,D) Wood lamp examination of a scar following incomplete excision of a lentigo maligna shows the residual lentigo maligna at the upper edge of the scar.
Conclusions
The presence of melanin can be difficult to observe by the naked eye because of melanin’s tendency to absorb radiation spanning the electromagnetic spectrum (350–1,200 mm), especially in the shorter wavelength [1]. Wood light unique photo-interaction with melanin makes it ideal to assess the extent of pigmented lesions where areas of increased concentrations of epidermal melanin will appear darker by contrast to the normal skin. Therefore, the value of Wood light in defining surgical margins is limited in patients with photo-damaged skin and concurrent solar lentigines. In this report we have shown that Wood light is very helpful in determining margins of lentiginous melanomas before surgical excision. Walsh et al [2] also demonstrated that 11.7% of patients with melanoma in situ (n = 60) had Wood light enhancement beyond the visible margins of biopsy and the use of Wood lamp increased the average wound size in patients. A comparative study is warranted to examine surgical clearance between excisions based on Wood lamp illumination vs clinical and dermoscopic examination alone. No long-term follow-up was needed for our cohort of patients following confirmed complete excisions. However, this should be considered in future research with a larger sample size to investigate recurrence rates.
Advances in technology will continue to modify the way we monitor and manage pigmented skin lesions. For example, in-vivo confocal microscopy has already proven beneficial in assessing surgical and medical approaches in the treatment of LM [3,4]. However, it is important not to forget the utility of simple yet helpful instruments such as Wood light, which is widely available in our dermatology departments.
Footnotes
Funding: None.
Competing interests: The authors have no conflicts of interest to disclose.
Authorship: All authors have contributed significantly to this publication.
References
- 1.Paraskevas LR, Halpern AC. Utility of the Wood’s light: five cases from a pigmented lesion clinic. Br J Dermatol. 2005;152(5):1039–1044. doi: 10.1111/j.1365-2133.2005.06346.x. [DOI] [PubMed] [Google Scholar]
- 2.Walsh SB, Varma R, Raimer D, et al. Utility of Wood’s light in margin determination of melanoma in situ after excisional biopsy. Dermatol Surg. 2015;41(5):572–578. doi: 10.1097/DSS.0000000000000345. [DOI] [PubMed] [Google Scholar]
- 3.Couty E, Tognetti L, Labeille B, et al. In vivo reflectance confocal microscopy combined with the “spaghetti technique” for the identification of surgical margins of lentigo maligna: experience in 70 patients. J Eur Acad Dermatol Venereol. 2018;32(9):e366–e368. doi: 10.1111/jdv.14947. [DOI] [PubMed] [Google Scholar]
- 4.Champin J, Parrot JL, Cinotti E, et al. In vivo reflectance confocal microscopy to optimize the spaghetti technique for defining surgical margins of lentigo maligna. Dermatol Surg. 2014;40(3):247–256. doi: 10.1111/dsu.12432. [DOI] [PubMed] [Google Scholar]