Abstract
Background:
Florida became the first state in the U.S. South to legalize the use of medical marijuana to treat a variety of health conditions including chronic pain, epilepsy, and spasticity symptoms from multiple sclerosis. While there are over 200,000 medical marijuana patients in Florida, there remain financial, psychological, and insurance coverage barriers which reduce access for many patients.
Purpose:
This scoping review, with a focus on state health policy, first describes some clinical studies examining the therapeutic benefits of medical marijuana. Next, there is a discussion of the Florida regulatory environment and major legislation. Also, the review describes how the current Florida policy landscape presents challenges for physicians and patients.
Methods:
A scoping review of the literature was conducted in PubMed and Google Scholar using the search terms, “medical marijuana” and “medical cannabis” to identify research articles, newspaper reports, and government documents. The purpose of the review was to identify research investigating the therapeutic efficacy of medical marijuana and state policies affecting physician practice.
Results:
The review concluded there was general scientific consensus of therapeutic benefits for patients, especially for chronic pain, from the use of medical marijuana. The review also identified several barriers for physicians and patients around cost, stigma, and lack of insurance coverage which constrains use and access.
Discussion:
The review discusses several directions for future medical marijuana policy and research with the aim to improve therapeutic benefits for Florida patients.
Background
Marijuana, the dried leaves and flowers of the herbal plant Cannabis sativa, is the most commonly used illicit drug in the United States.1 Since 1970, marijuana has been classified as a Schedule I substance under the Controlled Substances Act and applied by the U.S. Drug Enforcement Agency (DEA). This class of drugs, substances, and chemicals are defined as those with no “currently accepted medical use and high potential for abuse.”2 However despite the federal ban, there are 33 legal medical marijuana states dating back to 1996, and 10 legal recreational marijuana states dating back to 2012.3 Florida became the first state in the U.S. South to allow residents to use medical marijuana following the passage of Ballot Amendment 2 in 2016.4 Medical marijuana, for the purposes of this review, refers to botanical cannabis, rather than to any marijuana-derived pharmaceutical product.
Despite the classification of marijuana as an illegal substance under federal law, a growing body of research has suggested marijuana has therapeutic benefits for a variety of health conditions. Clinical studies suggest medical marijuana may reduce neuropathic pain, nausea and vomiting due to chemotherapy, spasticity from multiple sclerosis (MS), intraocular pressure, and increase appetite.5,6 Because of the Schedule 1 classification, scientific studies of marijuana have been extremely limited in the U.S., yet researchers in Canada and Europe have conducted clinical trials of cannabis-derived drugs such as Sativex®, which addresses neuropathic pain in MS patients.7,8 Sativex® contains a 1:1 ratio of Delta-9-tetrahydrocannibinol (THC) to cannabidiol (CBD), which reduces some of the potential negative side effects of higher THC levels.9 To date however, the Food and Drug Administration (FDA) has only approved the use of marijuana for two rare and severe forms of epilepsy, which also places limits on the ability to cover the drug under health insurance plans.10 The FDA has approved one cannabis-derived and three cannabis-related pharmaceutical drug products.11 One of these products is Epidiolex® (derived from CBD), an oral solution for the treatment of seizures associated with severe forms of epilepsy. Another drug product is Cesamet® with the active ingredient nabilone, a synthetic analogue of THC, to treat nausea and vomiting associated with cancer chemotherapy. Marinol® and Syndros® are also FDA-approved and contain the active ingredient dronabinol, another synthetic form of THC, which is an antiemetic used to increase appetite in patients with the human immunodeficiency virus and to help patients experiencing wasting from cancer chemotherapy.
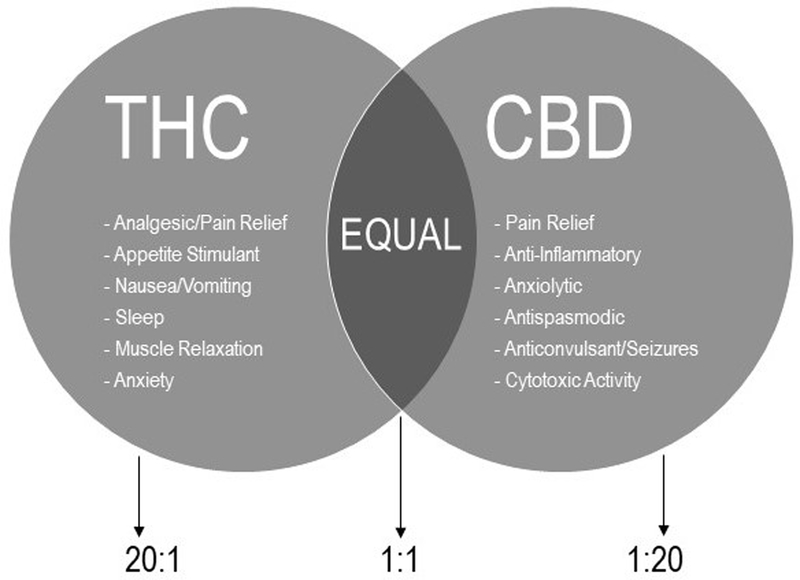
Marijuana contains over 100 different chemicals which are classified as cannabinoids, chemicals which can be used for medicinal purposes when using the whole unprocessed marijuana plant or its essential extracts.12 The two most well-known chemicals of this class are THC and CBD. THC content in recreational marijuana in the U.S. nearly doubled between 1997 and 2006, from 4.5% to 8.5%, which is notable because 1) higher THC levels are more likely to produce adverse psychological effects in naïve users, and 2) past recreational users who transition to medical users may be accustomed to higher THC levels.13 Depending on the strain, a higher percentage of CBD attenuates the risk of using high THC marijuana.14 Despite what is known about THC:CBD ratio combinations and their differential effects, medical marijuana laws do not provide guidance on THC levels for medical-grade marijuana.15 Figure 1 below illustrates how a drug company or medical marijuana treatment center (MMTC) might explain how the chemicals provide therapeutic benefits to patients. By modifying these ratios, individualized treatment might be offered to patients with a variety of mixture types available.
Figure 1.
Example of educational graphic to explain the therapeutic benefits of THC and CBD16
Because of the trend of legalizing the use of medical marijuana in more than half of all states, some medical organizations support reclassification of marijuana at the federal level as a Schedule II controlled substance.7 Furthermore, the medical marijuana treatment industry, pharmaceutical companies, and academia are invested in continuing the study of medical marijuana, as any other medical therapy has been studied, which would result in the drug being removed from the Schedule 1 category if the drug demonstrated effectiveness for certain medical conditions in placebo-controlled trials. However, most research has been limited to retrospective cohort studies, case studies, or observational studies creating a conundrum for developing an evidence base.14 Conducting more clinical studies would help inform physicians on proper dosing of cannabis-based medicines, yet the ability to conduct these studies is hampered by current legal and policy barriers, leading to a Catch-22. More research is needed to measure the therapeutic benefits for patients how cannabinoids affect human health.
This review begins with describing clinical studies on the therapeutic benefits of medical marijuana. This is followed by a discussion of the Florida regulatory environment and existing legislation which govern physician practice. The review also discusses barriers to patient access and health disparities. Marijuana, like any other drug therapy, involves both risks and benefits. There are potential harms related to chronic marijuana use such as the increased risk of motor vehicle crashes, worsening of schizophrenia or other related mental disorders in some individuals, and increased severity of respiratory symptoms, among other risks.17 It is with these caveats that this review proceeds to review the literature regarding the therapeutic benefits of medical marijuana and the current policy landscape in Florida.
Methods
A scoping review of the literature was conducted in PubMed and Google Scholar using the search terms, “medical marijuana” and “medical cannabis” to identify research articles for this review.18 In addition, an internet search was conducted using the search terms, “Florida medical marijuana law” to identify articles in newspapers and law journals for further information about challenges related to the decriminalization of medical marijuana in the state. The results of the literature search were compiled into an Endnote database. The purpose of conducting the scoping review was to document recent evidence on the therapeutic benefits of medical marijuana and identify challenges for physicians and patients in the context of decriminalization in Florida.
Results
The results from the literature search were comprised of primarily peer-reviewed articles (83 articles). The peer-reviewed articles were published between 2005 and 2019, with the bulk of the articles published since 2014 (74 articles). The articles primarily reported original research, but the literature search also included 14 literature review articles. Other document sources included government websites, Florida newspaper articles, Florida Bar Journal articles, Florida statutes, and consensus study reports (15 documents). The Physician Certification Pattern Review Panel Annual Report provided detailed data on medical marijuana recommendation patterns in Florida and information on certifying conditions.19 However, the report does not contain summary demographic information on medical marijuana patients.
Use of Marijuana in Modern Medicine
There is a growing interest in the research and use of medical marijuana and marijuana-based pharmaceuticals for the treatment and management of a variety of conditions. After a thorough review of all medical marijuana clinical studies by the National Academy of Sciences, Engineering, and Medicine, the panel concluded there was conclusive evidence that cannabis-based medicines are effective for the treatment of chronic pain, chemotherapy-induced nausea and vomiting, and symptoms of spasticity symptoms in MS patients.17 In a study by Crowell20 the most common reasons for indicating the use of medical marijuana among a group of patients in New Jersey were intractable skeletal spasticity, chronic pain, MS, and inflammatory bowel disease. Medical marijuana is generally indicated to be beneficial for the treatment of several conditions such as chronic non-malignant pain, poor appetite, nausea, depression, anxiety, arthritis, bruxism, chemotherapy-induced nausea and vomiting, chronic fatigue, depression, diabetes symptoms, spasticity from MS, epileptic seizures, and intestinal disorders.21
While medical marijuana has many potential uses, the primary therapeutic use is to treat chronic pain in adults. Chronic non-cancer pain is the most commonly cited use of medical marijuana in the U.S., Canada, and the Netherlands.22 While there is the general public perception that marijuana may be used to treat pain, to date, few large randomized controlled trials have been conducted to test this assumption. A systematic review of 15 trials on the effect of medical marijuana on non-cancer pain reported significant improvements in patients with neuropathic pain, and moderate improvement in fibromyalgia and rheumatoid arthritis.23 Another systematic review of 24 randomized controlled trials provided some evidence for the effectiveness of medical marijuana in the treatment of chronic pain conditions such as arthritic pain, headache, neuropathic pain, and visceral pain, especially by inhalation.24 However, more research is needed to establish the efficacy of different formulations of medical marijuana for pain treatment.
Chronic pain is a persistent and widespread public health problem, and opioids are commonly prescribed to treat pain. An Institute of Medicine report listed several causes of chronic pain prevalence which included: 1) rising obesity; 2) increase in number of cancer survivors; 3) complications from surgical procedures; and 4) musculoskeletal disorders in older adults.25 Medical marijuana is considered a safer alternative than opioids for patients who may be at risk for addiction and overdose. One national study identified that in states with medical marijuana laws and prescription drug monitoring programs, opioid-related deaths substantially decreased.26 Another national study reported that in states with medical marijuana laws, the opioid overdose rate decreased over time, from 20% in the first year to 33% by the sixth year since enactment of the laws.27 Population-wide opioid overdose deaths have decreased in states that have not stringently regulated the operation of medical marijuana dispensaries and are permitted more latitude in dispensing practices.28–32 For many pain patients, medical marijuana may be a safer alternative than prescription opioids.
Methods of Consuming Medical Marijuana
There are different ways for patients to use medical marijuana effectively. Marijuana is primarily inhaled, but other modes of use include ingestion of food prepared with marijuana oils (i.e., edibles), and topical applications. In Florida, products available for purchase include vape pens, vaporizers, capsules, oral syringes, drops, oils, topical creams, and smokable marijuana.33 There is also distinction between low-THC cannabis, defined as products with less than 0.8% of THC and more than 10% of CBD, compared with medical marijuana, which encompasses all forms of the plant – including low-THC marijuana – dispensed by a MMTC to qualified patients.
Qualifying Conditions for Medical Marijuana in Florida
In July 2014, the Florida Legislature passed the Compassionate Medical Use Act. In January 2015 qualified physicians were permitted to issue patient orders for low-THC cannabis under limited conditions, and in August 2016 the first low-THC cannabis and medical marijuana were made available. In February 2017, Medical Marijuana Use Registry identification cards were issued to patients, and qualified physicians could issue these cards to patients. In March 2019, smokable marijuana became available for qualified patients, which was previously not permitted.34 Once a patient’s identification card application is approved, the patient can fill an order at one of the licensed MMTCs following the physician’s recommendation.
The following medical conditions qualify a patient to receive medical marijuana: cancer, epilepsy, glaucoma, HIV-positive status and AIDS, post-traumatic stress disorder (PTSD), amyotrophic lateral sclerosis (ALS), Crohn’s Disease, Parkinson’s Disease, MS, terminal conditions, and chronic non-malignant pain.19 As of February 15, 2019, 2,082 physicians had completed the required training course on medical marijuana, which needs to be renewed every two years.35 As of April 2019, there were 114 licensed MMTCs. In 2018 (January through September), 1,070 physicians issued 174,254 certifications to 136,274 patients for low-THC cannabis and medical marijuana.19
Medical marijuana is currently being used primarily for pain management both in Florida and nationwide. Out of all the certifications in Florida, the top five conditions included: chronic non-malignant pain (27.7%), qualifying medical conditions other than chronic non-malignant pain or terminal conditions (27.3%), PTSD (23.6%), cancer (9.8%), and epilepsy (2.5%). There have been some advances to understand dispensing practices based on nationwide patient registry information. Analysis of state registry data nationwide for medical marijuana use (1999–2017) reported that chronic pain was the most common condition indicated (62%), followed by spasticity from MS, chemotherapy-induced nausea and vomiting, PTSD, and cancer.3 To bolster the case for responsible recommendations, over 85% of qualifying conditions (chromic pain, chemotherapy-induced nausea and vomiting, and spasticity from MS) were identified by the 2017 National Academies report as conditions with either conclusive or substantial evidence of therapeutic effectiveness.17
Florida Policy for Physicians
The Florida Department of Health Office of Medical Marijuana Use maintains a list of physicians who are permitted to order low-THC cannabis, medical marijuana, and drug delivery devices. Under current law, physicians certified to work in Florida are protected against criminal penalties for recommending medical marijuana to patients with qualifying conditions within specified guidelines. According to the law, a physician is authorized to order medical marijuana to treat patients suffering from a qualifying condition if the physician holds an active, unrestricted license as a physician (f.s. 458) or osteopathic physician (f.s. 459) and has successfully completed training.34 Training includes a two-hour course, per qualifying condition, and passing of an exam issued by their respective certifying Boards (Florida Board of Osteopathic Medicine or Florida Board of Medicine) each year. The $250 course covers information on rules and regulations, allowable conditions and delivery mechanisms, legal restrictions, and decision making for physicians on patient eligibility.36
Certifying Boards maintain documentation on how many patients are certified, the type of delivery mechanism used by patients, and the quantity of medical marijuana recommended. For certifying patients, physicians may only issue a certification with an in-person patient visit, and certifications cannot be issued through a telemedicine consultation. Qualified physicians are only able to issue three 70-day supplies in each consultation. Physicians are required to maintain a treatment plan that includes the dosage, route of administration (oral, skin, etc.), planned duration, monitoring of symptoms or other indicators of toleration. A recommending physician who violates these guidelines commits a first-degree misdemeanor punishable by fines up to $1,000 (f.s. 775.083(1)(d)) or imprisonment not exceeding one year (f.s. 775.082(4)).34
Clinical Challenges
A commentary by a physician group on their clinical experience in certifying patients for medical marijuana illustrates the difficulties physicians may face to meet the needs of their patients.37 They conducted a chart review of 166 patients in their practice in Chicago, Illinois and identified five factors which especially posed challenges for their practice. These included the following:
Suboptimal knowledge of effectiveness, dosage, delivery mechanism, indications, and drug interactions;
No educational standards for dispensary and medical staff training;
Poor communication and coordination of patient care;
Challenges with supply of dosing options; and
Access barriers for those wanting medical marijuana treatment.
Areas for improvement were identified in the commentary. For example, in terms of dispensary staff, there was a shortage of pharmacists and other trained staff, so if more pharmacists were available, they would be able to help with issues regarding potential drug interactions and dosing. Another issue involves the number of medical marijuana choices available for dosing (e.g., edibles, patches, oils, creams, inhalation). This menu of options can create confusion for physicians and patients in terms of dosing formulas to best address patient’s symptoms while minimizing side effects. In the commentary, the authors recommended better data-driven guidelines on these issues and potential drug interactions with other medications (e.g., opioids, benzodiazepines, and antidepressants).37 There is also the important role for medical marijuana cultivators and dispensaries to only supply the most effective medical marijuana preparations to solve issues of quality control, supply and product demand.
Barriers for Access to Medical Marijuana
Because of the current regulatory environment, there are barriers to medical marijuana access for patients. These include patient hesitancy to discuss medical marijuana options with physicians as well as paperwork burden and regulatory hurdles to become a qualified physician in order to start issuing certifications.38 Studies have reported that medical marijuana use is more predominant among European Americans and less likely among Black, Latino, Asian and foreign-born individuals.6,39 There are various reasons for the discrepancies in access such as disposable income, stigma, and physician preferences.39,40 Patients might feel stigma in asking their personal physician to issue a certification for medical marijuana use, or their personal physician might not be certified to recommend medical marijuana.38 A review article focused on barriers to medical marijuana access reported that medical marijuana use is more common among individuals who are employed, earn high incomes, and have health insurance.39
In addition to costs such as co-payments for the doctor’s visit, there are fees associated with obtaining a medical marijuana card. In Arizona, there is a $150 initial and renewal registration fee for the state’s program.39 In Florida, there is no insurance coverage for medical marijuana, and private insurers cite reasons for non-coverage including lack of FDA approval and the federal classification of marijuana as a Schedule 1 drug. For Florida residents, patients first need a medical consultation which costs $250 or more to be certified as a medical marijuana patient; however, the medical consultation cost may vary.41 Next, there is an initial $75 application fee for the identification card, which is valid for one year. Costs for the product which is obtained at the dispensary vary depending on the medical marijuana delivery option. If the patient purchases their own vaporizer to use with pre-filled cartridges, the unit costs between $100-$300 and cartridges cost between $35 and $60 depending on the amount and type or strain. Patients must be recertified every seven months which incurs another physician visit. Therefore, total costs for the first year of use can easily exceed $600, which could be a burden for low-income patients.
Physicians certified to recommend medical marijuana can charge what they deem as reasonable for a consultation. Furthermore, the cost of medical marijuana can range from $50 to $150 for certain amounts at dispensaries. Currently, dispensaries in Florida are not equally distributed throughout the state, thus reducing access to some populations, especially in rural areas. This may exacerbate equitable access and contribute to missed economic activity for Florida. In addition to the direct economic benefits for Florida from increased tax revenues which are redistributed to healthcare, there are other benefits of medical marijuana. These include reducing arrests for marijuana possession, which disproportionately affect minority communities, and sanctioning the medical and compassionate use of medical marijuana.4
Discussion
This review summarized numerous recent clinical studies and concludes that there is evidence that medical marijuana provides therapeutic benefits to patients for a variety of health conditions, but particularly for chronic pain patients, cancer patients with chemotherapy-induced nausea and vomiting, and MS patients with spasticity symptoms. However, there is a need for more controlled studies, especially in the areas of cancer pain, intestinal disorders, and mental health. Since medical marijuana is being recommended for patients suffering from PTSD and generalized anxiety disorder, more research is needed to demonstrate improvement in mental health outcomes for these debilitating conditions. Since this is a scoping review, there was no attempt to assess the quality of the controlled studies identified and included, therefore there are limitations in terms of recommendations for policy or practice since the rigor of the clinical studies was not assessed.42
In terms of the Florida regulatory environment, some of the laws governing dispensaries and MMTCs are currently experiencing legal challenges, so there could be future changes in the number of MMTCs allowed to operate in Florida for example, which is currently capped. Increasing the number of dispensaries that could reach into rural areas of the state would increase access. In the current policy environment, challenges also remain in terms of physician education and reducing stigma among healthcare providers to become a certifying physician. From the physician perspective, there is stigma from becoming qualified to provide patients with medical marijuana certifications. Since prescribing medical marijuana is illegal under federal law, according to an investigative report, physicians fear they might be at risk of being blacklisted by hospital systems, nursing homes, or hospices, which rely on Medicaid and Medicare reimbursement funds; moreover, another issue which might contribute to stigma occurs when physicians with poor reputations are filling the void to work in MMTCs.43
In the research arena, challenges remain to provide the funding necessary to establish the research infrastructure at Florida’s public universities and research institutes given the existing federal policies and shifting priorities for state research dollars. Currently, there is limited research on medical marijuana being conducted in Florida. One recent study funded by the Florida legislature with glioma patients at Moffitt Cancer Center in Tampa, Florida reported that only a third of patients were using medical marijuana and received benefits from its use for symptoms including pain, nausea, poor appetite, and anxiety, but they had received the recommendation from friends or family rather than a medical provider.44 The study highlighted the need for more patient and physician communication on the potential benefits of medical marijuana for some cancer patients. Future research in medical marijuana will hopefully lead to improved therapeutic benefits for patients and greater understanding of the effects of cannabinoids on human health.
Conclusions
This scoping review has identified ongoing and past research efforts to demonstrate the therapeutic benefits of medical marijuana and points to some possible areas of investigation for health policy research. Because Florida law keeps medical marijuana in the health domain and the drug has not been decriminalized, regulatory activities remain in the Florida Department of Health instead of other agencies which regulate alcohol and tobacco, as was done in Colorado for example.45 One of the greatest challenges in Florida is the need for quality physician training and for more physicians to receive certification to improve physician/patient communication and patient education on this emerging therapy option. Moreover, there is an important role for public health in policy development around excise and sales taxes and collecting population-wide state data on marijuana use ahead of the possibility of expanded decriminalization policies.
Acknowledgments
Research reported in this publication was supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number U54 MD007582. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The research was also supported by the Florida A&M University Medical Marijuana Education and Research Initiative.
Footnotes
The authors have no financial disclosures and no conflicts of interest to report.
References
- 1.Goldenberg M, IsHak WW, Danovitch I. Quality of life and recreational cannabis use. Am J Addict. 2017;26(1):8–25. [DOI] [PubMed] [Google Scholar]
- 2.U.S. Drug Enforcement Administration. Drug Scheduling. https://www.dea.gov/drug-scheduling/ Accessed April 2, 2019.
- 3.Boehnke KF, Gangopadhyay S, Clauw DJ, Haffajee RL.. Qualifying conditions of medical cannabis license holders in the United States. Health Aff (Millwood). 2019;38(2):295–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diaby V, Sanogo V, Xiao H, Zhong X, Dykes J, Judson C. Economic impact of the passage of the medical marijuana law in the state of Florida. SSRN. 2018. doi: 10.2139/ssrn.3265254 [DOI] [Google Scholar]
- 5.Bowen LL, McRae-Clark AL. Therapeutic benefit of smoked cannabis in randomized placebo-controlled studies. Pharmacotherapy. 2018;38(1):80–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reinarman C, Nunberg H, Lanthier F, Heddleston T.. Who are medical marijuana patients? Population characteristics from nine California assessment clinics. J Psychoactive Drugs. 2011;43(2):128–135. [DOI] [PubMed] [Google Scholar]
- 7.Bostwick JM. Blurred boundaries: The therapeutics and politics of medical marijuana. Mayo Clin Proc. 2012;87(2):172–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perras C Sativex for the management of multiple sclerosis symptoms. Issues Emerg Health Technol. 2005(72):1–4. [PubMed] [Google Scholar]
- 9.Russo E, Guy GW. A tale of two cannabinoids: The therapeutic rationale for combining tetrahydrocannabinol and cannabidiol. Med Hypotheses. 2006;66(2):234–246. [DOI] [PubMed] [Google Scholar]
- 10.Wise J FDA approves its first cannabis based medicine. BMJ. 2018;361:k2827. [DOI] [PubMed] [Google Scholar]
- 11.U.S. Food and Drug Administration. FDA and Marijuana: Questions and Answers. https://www.fda.gov/newsevents/publichealthfocus/ucm421168.htm/ Accessed February 18, 2019.
- 12.National Institute on Drug Abuse. Marijuana as Medicine. https://www.drugabuse.gov/publications/drugfacts/marijuana-medicine#references Accessed February 16, 2019.
- 13.McLaren J, Swift W, Dillon P, Allsop S. Cannabis potency and contamination: A review of the literature. Addiction. 2008;103(7):1100–1109. [DOI] [PubMed] [Google Scholar]
- 14.Sachs J, McGlade E, Yurgelun-Todd D. Safety and toxicology of cannabinoids. Neurotherapeutics. 2015;12(4):735–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sevigny EL, Pacula RL, Heaton P. The effects of medical marijuana laws on potency. Int J Drug Policy. 2014;25(2):308–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reed T, Shuffett ML. Barriers to achieving optimal success with medical cannabis: Opportunities for quality improvement. J Altern Complement Med. 2019;25(1):121–122. [DOI] [PubMed] [Google Scholar]
- 17.National Academies of Sciences Engineering, and Medicine. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Washington, D.C.: The National Academies Press; 2017. [PubMed] [Google Scholar]
- 18.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Florida Board of Medicine and Florida Board of Osteopathic Medicine. Physician Certification Pattern Review Panel Annual Report. Florida Department of Health; https://flboardofmedicine.gov/forms/PCPRP-annual-report-2019.pdf Accessed March 20, 2019. [Google Scholar]
- 20.Crowell TL. Understanding patients’ process to use medical marijuana: A southern New Jersey community engagement project. J Patient Exp. 2016;3(3):81–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McClure EA, King JS, Wahle A, et al. Comparing adult cannabis treatment-seekers enrolled in a clinical trial with national samples of cannabis users in the United States. Drug Alcohol Depend. 2017;176:14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Campbell G, Hall WD, Peacock A, et al. Effect of cannabis use in people with chronic non-cancer pain prescribed opioids: Findings from a 4-year prospective cohort study. Lancet Public Health. 2018;3(7):e341–e350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lynch ME, Campbell F. Cannabinoids for treatment of chronic non-cancer pain: A systematic review of randomized trials. Br J Clin Pharmacol. 2011;72(5):735–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aviram J, Samuelly-Leichtag G. Efficacy of cannabis-based medicines for pain management: A systematic review and meta-analysis of randomized controlled trials. Pain Physician. 2017;20(6):E755–E796. [PubMed] [Google Scholar]
- 25.Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, D.C; 2011. [PubMed] [Google Scholar]
- 26.Phillips E, Gazmararian J. Implications of prescription drug monitoring and medical cannabis legislation on opioid overdose mortality. J Opioid Manag. 2017;13(4):229–239. [DOI] [PubMed] [Google Scholar]
- 27.Bachhuber MA, Saloner B, Cunningham CO, Barry CL. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999–2010. JAMA Intern Med. 2014;174(10):1668–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bradford AC, Bradford WD, Abraham A, Bagwell Adams G. Association between US State medical cannabis laws and opioid prescribing in the Medicare Part D population. JAMA Intern Med. 2018;178(5):667–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liang D, Bao Y, Wallace M, Grant I, Shi Y. Medical cannabis legalization and opioid prescriptions: Evidence on US Medicaid enrollees during 1993–2014. Addiction. 2018;113(11):2060–2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shi Y, Liang D, Bao Y, An R, Wallace MS, Grant I. Recreational marijuana legalization and prescription opioids received by Medicaid enrollees. Drug Alcohol Depend. 2019;194:13–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Powell D, Pacula RL, Jacobson M. Do medical marijuana laws reduce addictions and deaths related to pain killers? J Health Econ. 2018;58:29–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wen H, Hockenberry JM. Association of medical and adult-use marijuana laws with opioid prescribing for Medicaid enrollees. JAMA Intern Med. 2018;178(5):673–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pounds M Pot products: Do you know what South Florida’s medical marijuana dispensaries sell? https://www.sun-sentinel.com/business/fl-bz-south-florida-pot-products-20181012-story.html Accessed February 18, 2019.
- 34.Medical use of marijuana, 381.986 (2018). [Google Scholar]
- 35.Florida Department of Health. Office of Medical Marijuana Use. http://www.floridahealth.gov/programs-and-services/office-of-medical-marijuana-use/ Accessed February 16, 2019.
- 36.Florida Medical Association. Florida Physician Medical Marijuana Course 2018 thru 2020. https://flmedical.inreachce.com/Details/Information/eb4d259d-9d3d-4c4c-b798-cc5781454fe0 Accessed June 12, 2019.
- 37.Temple LM, Lampert SL, Ewigman B. Barriers to achieving optimal success with medical cannabis: opportunities for quality improvement. J Altern Complement Med. 2019;25(1):5–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Satterlund TD, Lee JP, Moore RS. Stigma among California’s medical marijuana patients. J Psychoactive Drugs. 2015;47(1):10–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Valencia CI, Asaolu IO, Ehiri JE, Rosales C. Structural barriers in access to medical marijuana in the USA-a systematic review protocol. Syst Rev. 2017;6(1):154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Richmond MK, Pampel FC, Rivera LS, Broderick KB, Reimann B, Fischer L. Frequency and risk of marijuana use among substance-using health care patients in Colorado with and without access to state legalized medical marijuana. J Psychoactive Drugs. 2015;47(1):1–9. [DOI] [PubMed] [Google Scholar]
- 41.Call J Medical marijuana insurance in Florida? Lawmakers, agriculture commissioner pushing for it. Tallahassee Democrat. April 18, 2019. [Google Scholar]
- 42.Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libraries J. 2009;26:91–108. [DOI] [PubMed] [Google Scholar]
- 43.Johnson C Florida’s medical marijuana program is attracting troubled doctors: ‘It’s like the Wild Wild West’. Tampa Bay Times. May 4, 2018. [Google Scholar]
- 44.Reblin M, Sahebjam S, Peeri NC, Martinez YC, Thompson Z, Egan KM. Medical cannabis use in glioma patients treated at a comprehensive cancer center in Florida. J Palliat Med. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ghosh T, Van Dyke M, Maffey A, Whitley E, Gillim-Ross L, Wolk L. The public health framework of legalized marijuana in Colorado. Am J Public Health. 2016;106(1):21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]