Abstract
Context
Weight loss is strongly recommended for overweight and obese adults with type 2 diabetes. Unintentional weight loss is associated with increased risk of all-cause mortality, but few studies have examined its association with cardiovascular outcomes in patients with diabetes.
Objective
To evaluate 2-year weight change and subsequent risk of cardiovascular events and mortality in established type 2 diabetes.
Design and Setting
The Action in Diabetes and Vascular Disease: Preterax and Diamicron-MR Controlled Evaluation was an international, multisite 2×2 factorial trial of intensive glucose control and blood pressure control. We examined 5 categories of 2-year weight change: >10% loss, 4% to 10% loss, stable (±<4%), 4% to 10% gain, and >10% gain. We used Cox regression with follow-up time starting at 2 years, adjusting for intervention arm, demographics, cardiovascular risk factors, and diabetes medication use from the 2-year visit.
Results
Among 10 081 participants with valid weight measurements, average age was 66 years. By the 2-year examination, 4.3% had >10% weight loss, 18.4% had 4% to 10% weight loss, and 5.3% had >10% weight gain. Over the following 3 years of the trial, >10% weight loss was strongly associated with major macrovascular events (hazard ratio [HR], 1.75; 95% confidence interval [CI], 1.26-2.44), cardiovascular mortality (HR, 2.76; 95% CI, 1.87-4.09), all-cause mortality (HR, 2.79; 95% CI, 2.10-3.71), but not major microvascular events (HR, 0.91; 95% CI, 0.61-1.36), compared with stable weight. There was no evidence of effect modification by baseline body mass index, age, or type of diabetes medication.
Conclusions
In the absence of substantial lifestyle changes, weight loss may be a warning sign of poor health meriting further workup in patients with type 2 diabetes.
Type 2 diabetes is characterized by metabolic dysregulation primarily due to excess adiposity, resulting in an increased risk of cardiovascular disease (1, 2). Intentional weight loss of >5% is strongly recommended for overweight or obese patients with type 2 diabetes (grade A evidence by the American Diabetes Association) (3). Numerous studies have shown that intentional weight loss reduces blood pressure and improves lipids and glycemic control in diabetes (4–6). The largest trial of intentional weight loss in diabetes, Look AHEAD, achieved a mean weight loss of 6% in the intervention arm over 4 years (4). It did not, however, find a reduction in cardiovascular events, likely because of the substantially lower than expected cardiovascular disease event rate and the uptake of statins and other pharmacological treatments for cardiovascular risk factors, particularly in the control arm (7). A post hoc analysis of Look AHEAD found that participants with >10% weight loss at 1 year had a significantly lower cardiovascular event rate, supporting the original hypothesis that intentional weight loss improves cardiovascular health (8). However, only 36% of intervention arm participants achieved >10% weight loss at 1 year. Other studies have also seen considerable challenges in long-term intentional weight loss, even among highly motivated and supported clinical trial participants (9). A recent observational study among participants with screen-detected diabetes demonstrated that >5% weight loss in the year following diabetes diagnosis was associated with reduced cardiovascular events after 10 years, suggesting that weight loss may be most beneficial early in the diabetes disease course (10). Thus, large and sustained intentional weight loss likely improves cardiovascular health in diabetes but is uncommon.
In contrast, unintentional weight loss is generally indicative of deteriorating health and is associated with all-cause and cardiovascular mortality (11–14). Unintentional weight loss of >10 pounds is considered a marker of loss of physiologic reserve (15) and is more likely than intentional weight loss to include loss of fat-free mass, including bone and muscle (16). It is unclear how unintentional weight loss affects risk of nonfatal cardiovascular events in the setting of diabetes.
Given the strong recommendation for weight loss in diabetes, yet the substantial difficulty in achieving sustained, clinically significant intentional weight loss, it is important to consider the consequences of unintentional weight loss. Unintentional weight loss is a substantial concern among older adults but can also affect younger individuals, particularly those with comorbid conditions (17–19). It is possible that large weight loss may affect younger adults with diabetes differently than older adults. Additionally, individuals who are not overweight or obese may have more negative consequences of weight loss compared with overweight or obese. Further, because many diabetes medications influence weight (20), weight changes resulting from these medications may be less detrimental. The objectives of this study were (1) to determine whether weight change over 2 years was associated with subsequent cardiovascular outcomes and death in adults with diabetes and (2) to examine whether this association was modified by baseline body mass index (BMI), age, or type of glucose-lowering medications.
Methods
Study population
The Action in Diabetes and Vascular Disease: Preterax and Diamicron-MR Controlled Evaluation (ADVANCE) trial had a 2×2 factorial design (21). One arm tested the effects of intensive glucose lowering (target hemoglobin A1c [HbA1c] of <6.5% with use of gliclazide modified release, plus other drugs as required) versus standard glucose control targeting HbA1c according to local guidelines. A second arm tested the effects of blood pressure-lowering using a combination pill of perindopril (4 mg) and indapamide (1.25 mg) compared with placebo. From 2001 to 2003, the trial enrolled 11 140 participants with type 2 diabetes ≥55 years of age, at high risk of cardiovascular disease, and without long-term insulin use in 20 countries (21). The blood pressure intervention ended in June 2007 (median follow-up, 4.4 years) and the intensive glucose-lowering intervention ended in January 2008 (median follow-up, 5.0 years). The trial showed beneficial effects of both intensive glucose-lowering and blood pressure-lowering on the primary endpoint of combined microvascular and macrovascular events (22, 23). Two years after the trial close-out, all study sites were invited to participate in ADVANCE-ON, a 5-year observational follow-up of trial participants. Of the original 215 study sites, 172 (80%) agreed to participate, and 10 082 participants were enrolled in ADVANCE-ON beginning in January 2010 (24). Closeout visits for ADVANCE-ON were conducted in 2013 and 2014. All participants gave written informed consent.
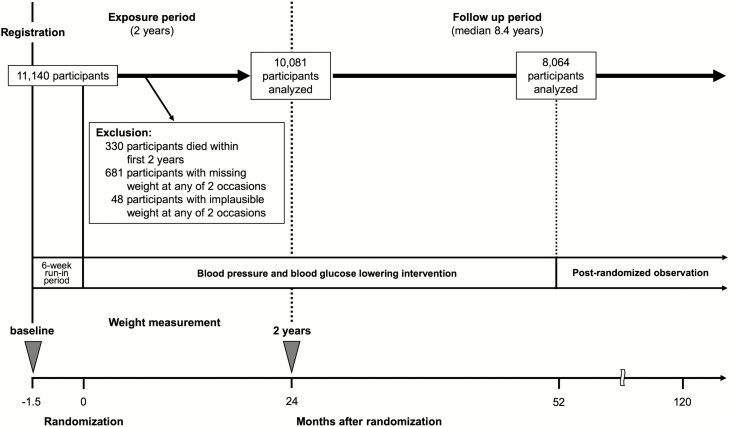
Of 11 140 ADVANCE participants, we excluded those who died before their year 2 study visit (n = 330) or who were missing weight either at baseline (n = 4) or 2 years (n = 677) (Fig. 1). We also excluded participants with implausible weights at either baseline or year 2 based on large (>25% or >20 kg) change that was inconsistent with measurements at subsequent clinic visits (n = 48). Our study population thus included 10 081 participants with validated measurements of weight at baseline and at 2 years in ADVANCE. Our analyses using the extended follow-up time from ADVANCE-ON included 8064 participants.
Figure 1.
Study design and identification of the analytic cohort.
Participants were excluded from the analysis of major macrovascular events if they had a major macrovascular event before 2 years (n = 249). Participants were excluded from the analysis of microvascular events if they had a microvascular event before 2 years (n = 377).
Weight change
During the ADVANCE trial, weight was measured biannually. We calculated percentage weight change at 2 years by subtracting the baseline weight from the 2-year weight and dividing by the baseline weight. We chose 2 years after baseline because it represented a long-term change in weight, whereas a 1-year change may have represented short-term fluctuations that were not sustained. We categorized weight change at 2 years into 5 groups: >10% weight loss, 4% to 10% weight loss, ±<4% (stable), 4% to 10% weight gain, and >10% weight gain. These cutpoints were motivated by the literature on unintentional weight loss: 1 study showed that 4% was an optimal threshold for defining clinically important unintentional weight loss (18), whereas 10% weight loss is indicative of catabolism and significant loss of muscle mass (25).
In the context of ADVANCE, participants who were randomized to the intensive glucose-lowering arm were more likely to have received diabetes medications known to increase weight, including sulfonylureas, insulin, and thiazolidinediones (TZDs) (23). To account for weight change related to diabetes medication use, we adjusted for medication use at year 2 in our primary analysis. We also conducted sensitivity analyses stratified by medication use after excluding TZDs, given the controversy surrounding TZDs during this time (26).
Outcomes
The primary endpoint in ADVANCE was a composite of major macrovascular and microvascular events (23). Major macrovascular events included death from cardiovascular causes, nonfatal myocardial infarction, and nonfatal stroke. Major microvascular events were new or worsening nephropathy (development of albumin-to-creatinine ratio >300 mg/g or doubling of serum creatinine to >2.25 mg/dL), the need for renal replacement therapy, or retinopathy (proliferative retinopathy, macular edema, blindness, or retinal photocoagulation therapy). Cardiovascular death and all-cause death were also recorded. We examined these 4 endpoints (major macrovascular events, major microvascular events, cardiovascular death, and all-cause death) in ADVANCE. Because major microvascular events were not able to be assessed in ADVANCE-ON (24), we examined major macrovascular events, cardiovascular death, and all-cause death in combined data from ADVANCE and ADVANCE-ON.
Statistical analysis
We examined baseline characteristics of ADVANCE participants by category of 2-year weight change. To examine the association of weight change categories with each endpoint, we used Cox proportional hazards regression. For major macrovascular and major microvascular events, we excluded individuals with that endpoint before the 2-year visit and began follow-up time at the 2-year visit. To control for potential confounding, we adjusted for age, sex, country grouping (Asia/Eastern Europe/established market economies), baseline HbA1c, baseline systolic blood pressure, history of macrovascular disease at baseline, history of microvascular disease at baseline, randomized glucose treatment assignment, randomized blood pressure treatment assignment, baseline smoking status (current/former/never), baseline statin use, and diabetes medication use (metformin/TZDs/sulfonylureas/insulin) at year 2. We also examined whether further adjustment for baseline waist-to-height ratio, a better predictor of cardiovascular disease than BMI (27, 28), attenuated the results. The proportional hazards assumption was checked using visual examination of the log negative log survival plots.
To determine if the type of glucose-lowering treatment might alter the association between weight change and cardiovascular outcomes, we first excluded the small number of people who took TZDs. We then tested for interaction of weight change categories with metformin using likelihood ratio tests. We hypothesized that given metformin’s known propensity to cause weight loss (20), weight loss with metformin may have neutral or protective effects on macrovascular events and mortality. We additionally conducted sensitivity analyses to determine if the association between weight change and cardiovascular and mortality outcomes varied by baseline BMI (<25 vs. ≥25) or age (<65 vs. ≥65), using likelihood ratio tests. Finally, we tested for potential interaction by blood pressure treatment as well as by diuretic use because diuretics are known to cause weight loss resulting from fluid loss (29).
Finally, because weight loss benefit for cardiovascular disease is primarily through improvements to cardiovascular risk factors, we examined unadjusted means and standard deviations of 2-year levels and 2-year change in HbA1c, systolic and diastolic blood pressure, total cholesterol, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, and triglycerides. We used a linear test for trend to determine whether changes in weight were linearly associated with changes in cardiovascular risk factors.
Results
At 2 years, of the 10 081 participants, the majority were weight stable (5713, 56.7%), whereas 432 (4.3%) had weight loss >10%, 1854 (18.4%) had weight loss of 4% to 10%, 1548 (15.4%) had weight gain of 4% to 10%, and 534 (5.3%) had weight gain >10%. Individuals with large weight loss were more likely to be older, female, randomized to perindopril/indapamide, have a larger BMI at baseline, have lower HbA1c, and longer diabetes duration (Table 1). Individuals with large weight loss were also more likely to have a history of macrovascular disease and were less likely to be on insulin.
Table 1.
Baselinea Characteristics of Participants by 2-Y Weight Change Categories
| >10% Weight Loss n = 432 (4.3%) | 4–10% Weight Loss n = 1854 (18.4%) | Stable (±<4%) n = 5713 (56.7%) | 4–10% Weight Gain n = 1548 (15.4%) | >10% Weight Gain n = 534 (5.3%) | |
|---|---|---|---|---|---|
| Age, y | 66.4 (6.8) | 66.1 (6.3) | 65.5 (6.3) | 65.4 (6.2) | 64.8 (6.2) |
| Female, % | 52.1 | 44.2 | 40.1 | 42.7 | 49.1 |
| Intensive glycemic control arm, % | 50.2 | 47.4 | 48.7 | 57.8 | 57.9 |
| Perindopril/indapamide arm, % | 56.2 | 56.4 | 49.1 | 45.4 | 48.7 |
| Region, % | |||||
| Established market economiesb | 39.8 | 41.9 | 42.7 | 46.8 | 39.1 |
| Eastern Europeb | 17.1 | 17.1 | 19.1 | 20.9 | 19.1 |
| Asiab | 43.1 | 41.0 | 38.2 | 32.4 | 41.8 |
| BMI, kg/m2 | 29.6 (6.1) | 28.9 (5.1) | 28.2 (4.9) | 28.1 (5.4) | 26.7 (5.2) |
| Waist-to-height ratio | 0.61 (0.09) | 0.60 (0.07) | 0.59 (0.07) | 0.59 (0.08) | 0.58 (0.08) |
| HbA1c, % | 7.3 (1.4) | 7.4 (1.4) | 7.5 (1.5) | 7.6 (1.8) | 7.9 (1.9) |
| Systolic blood pressure | 146 (22) | 145 (22) | 145 (21) | 144 (22) | 144 (22) |
| Diastolic blood pressure | 80 (11) | 81 (11) | 81 (11) | 80 (11) | 81 (11) |
| Total cholesterol | 203 (46) | 202 (46) | 201 (47) | 200 (46) | 202 (47) |
| HDL cholesterol | 48 (14) | 49 (14) | 48 (13) | 49 (14) | 50 (15) |
| Triglycerides | 171 (105) | 174 (112) | 174 (113) | 175 (123) | 170 (110) |
| Diabetes duration, y | 7.3 (5.8) | 7.9 (6.4) | 7.9 (6.3) | 7.7 (6.3) | 8.4 (6.9) |
| History of macrovascular disease, % | 34.0 | 34.1 | 31.1 | 32.0 | 31.6 |
| History of microvascular disease, % | 13.7 | 8.3 | 9.5 | 10.9 | 13.9 |
| Smoking, % | |||||
| Current smoker | 15.5 | 13.4 | 13.6 | 13.9 | 15.0 |
| Former smoker | 25.0 | 27.8 | 28.0 | 28.7 | 23.2 |
| Medication use at year 2, % | |||||
| Sulfonylurea | 44.7 | 45.3 | 46.5 | 53.6 | 54.3 |
| Metformin | 69.2 | 72.8 | 67.5 | 62.9 | 61.2 |
| Insulin | 11.1 | 11.2 | 16.3 | 26.9 | 37.5 |
| Thiazolidinediones | 3.2 | 5.0 | 8.5 | 14.5 | 15.7 |
Data are mean (standard deviation) unless noted as %.
Abbreviations: BMI, body mass index; HDL, high-density lipoprotein.
aBaseline is the time of randomization for all variables except medication use from year 2.
bEstablished market economies: Australia, New Zealand, Canada, Ireland, United Kingdom, France, Italy, Germany, the Netherlands. Eastern Europe: Czech Republic, Estonia, Hungary, Lithuania, Poland, Russia, Slovakia. Asia: China, India, Malaysia, Philippines.
Median follow-up time after the year 2 visit for major macrovascular events was 3.0 years during ADVANCE and 8.4 years for ADVANCE-ON; 591 had a major macrovascular outcome during ADVANCE and an additional 978 had this outcome during ADVANCE-ON. For major microvascular events, the median follow-up time after the year 2 visit was 3.0 years and 706 had the endpoint during ADVANCE. For cardiovascular death, median follow-up time was 3.0 years with 290 events during ADVANCE and 8.6 years, with 121 additional events during ADVANCE-ON. For all-cause death, median follow-up time was 3.0 years, with 600 events during ADVANCE and 8.6 years with 529 additional events during ADVANCE-ON.
After adjustment, large weight loss was strongly associated with the major macrovascular events (hazard ratio [HR], 1.75, 95% confidence interval [95% CI], 1.26-2.44) during ADVANCE (Table 2). Large weight loss was associated with more than 2.5 times greater risk of cardiovascular mortality (HR, 2.76; 95% CI, 1.87-4.09) and all-cause mortality (HR, 2.79; 95% CI, 2.10-3.71). Moderate (4%-10%) weight loss was also associated with increased risk of all-cause mortality (HR, 1.43; 95% CI, 1.16-1.76) and was not associated with the other endpoints. Large weight gain (>10%) was marginally associated with major macrovascular events (HR, 1.40; 95% CI, 1.00-1.95). For all endpoints, adjusting for cardiovascular risk factors after adjusting for demographics only minimally attenuated the results. Additional adjustment for baseline waist-to-height ratio did not change the results (data not shown).
Table 2.
HRs (95% CIs) of Major Clinical Endpoints According to Categories of 2-Year Weight Change, ADVANCE Trial Participants, n = 10 081
| >10% Weight Loss n = 432 (4.3%) | 4–10% Weight Loss n = 1854 (18.4%) | Stable (±<4%) n = 5713 (56.7%) | 4–10% Weight Gain n = 1548 (15.4%) | >10% Weight Gain n = 534 (5.3%) | |
|---|---|---|---|---|---|
| Major macrovascular events | |||||
| Cases/no.a | 40/412 | 112/1798 | 323/5587 | 76/1515 | 40/520 |
| Crude incidence rate (95% CI), per 100 PY | 9.7 (7.0, 13.0) | 6.2 (5.2, 7.4) | 5.8 (5.2, 6.4) | 5.0 (4.0, 6.2) | 7.7 (5.6, 10.3) |
| Model 1b, HR (95% CI) | 1.81 (1.30-2.51) | 1.09 (0.88-1.35) | 1 [ref] | 0.89 (0.69-1.14) | 1.50 (1.08-2.09) |
| Model 2b, HR (95% CI) | 1.75 (1.26-2.44) | 1.08 (0.87-1.34) | 1 [ref] | 0.84 (0.66-1.09) | 1.40 (1.00-1.95) |
| Microvascular events | |||||
| Cases/no.a | 26/415 | 119/1797 | 397/5522 | 111/1468 | 53/502 |
| Crude incidence rate (95% CI), per 100 PY | 6.3 (4.1-9.0) | 6.6 (5.5-7.9) | 7.2 (6.5-7.9) | 7.6 (6.3-9.0) | 10.6 (8.0-13.6) |
| Model 1b, HR (95% CI) | 0.88 (0.59-1.31) | 0.91 (0.74-1.12) | 1 [ref] | 1.09 (0.88-1.35) | 1.50 (1.13-2.00) |
| Model 2b, HR (95% CI) | 0.91 (0.61-1.36) | 0.96 (0.78-1.19) | 1 [ref] | 0.98 (0.79-1.21) | 1.22 (0.91-1.64) |
| Cardiovascular mortality | |||||
| Cases/no.a | 31/432 | 53/1854 | 156/5713 | 38/1548 | 12/534 |
| Crude incidence rate (95% CI), per 100 PY | 7.2 (4.9-10.0) | 2.9 (2.1-3.7) | 2.7 (2.3-3.2) | 2.5 (1.7-3.4) | 2.2 (1.2-3.9) |
| Model 1b, HR (95% CI) | 2.82 (1.91-4.15) | 1.06 (0.77-1.45) | 1 [ref] | 0.93 (0.65-1.32) | 0.96 (0.53-1.72) |
| Model 2b, HR (95% CI) | 2.76 (1.87-4.09) | 1.06 (0.77-1.46) | 1 [ref] | 0.85 (0.59-1.21) | 0.83 (0.46-1.50) |
| All-cause mortality | |||||
| Cases/no.a | 58/432 | 133/1854 | 293/5713 | 81/1548 | 35/534 |
| Crude incidence rate (95% CI), per 100 PY | 13.4 (10.4-17.0) | 7.2 (6.0-8.4) | 5.1 (4.6-5.7) | 5.2 (4.2-6.5) | 6.6 (4.6-9.0) |
| Model 1b, HR (95% CI) | 2.79 (2.10-3.70) | 1.40 (1.14-1.72) | 1 [ref] | 1.05 (0.82-1.35) | 1.48 (1.04-2.10) |
| Model 2b, HR (95% CI) | 2.79 (2.10-3.71) | 1.43 (1.16-1.76) | 1 [ref] | 0.98 (0.76-1.25) | 1.33 (0.93-1.89) |
Abbreviations: CI, confidence interval; HR, hazard ratio. PY, person-years.
aParticipants were censored from a given analysis if they had the event before the weight measurement at year 2.
bModel 1: age, sex, region. Model 2: age, sex, region, baseline hemoglobin A1c, baseline systolic blood pressure, history of macrovascular disease at baseline, history of microvascular disease at baseline, glucose treatment assignment, blood pressure treatment assignment, baseline smoking status (current/former/never), baseline statin use, and diabetes medication (metformin/thiazolidinediones/sulfonylureas/insulin) use at year 2.
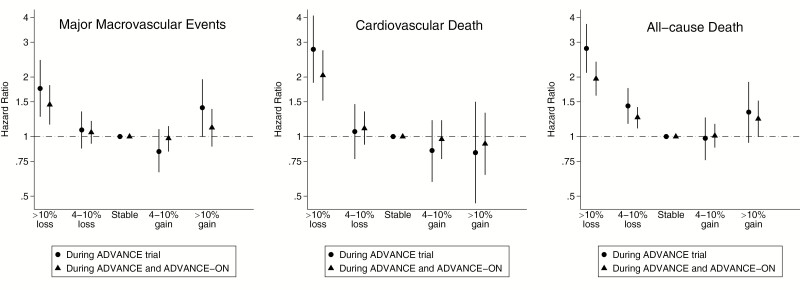
The results for ADVANCE and overall, including ADVANCE-ON, were similar for major macrovascular events, cardiovascular death, and all-cause death (Fig. 2). For major macrovascular events, both large weight gain and large weight loss appeared more harmful in the short-term rather than the long-term follow-up. For both cardiovascular death and all-cause death, the association of large weight loss was stronger in ADVANCE than after the additional follow-up in ADVANCE-ON.
Figure 2.
Adjusted* hazard ratios and 95% confidence intervals of major macrovascular events, cardiovascular death, and all-cause death according to categories of 2-year weight change, ADVANCE and ADVANCE-ON, n = 10 081.
*Adjusted for age, sex, region, baseline hemoglobin A1c, baseline systolic blood pressure, history of macrovascular disease at baseline, history of microvascular disease at baseline, glucose treatment assignment, blood pressure treatment assignment, baseline smoking status (current/former/never), baseline statin use, and diabetes medication (metformin/thiazolidinediones/sulfonylureas/insulin) use at year 2.
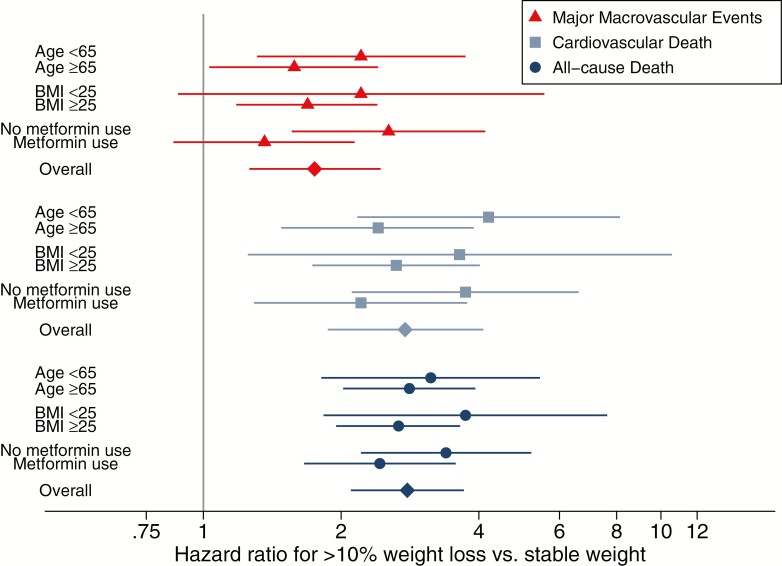
We found no significant effect modifications of the associations between >10% weight loss, compared with stable weight, and cardiovascular events, cardiovascular death, or death by baseline age BMI or metformin use at year 2 (Fig. 3). Metformin users with >10% weight loss appeared to not have increased risk of cardiovascular events, but the overall interaction between weight change category and metformin use was not statistically significant (P for interaction = 0.15). We also did not see any effect modification by blood pressure arm or diuretic use (data not shown).
Figure 3.
Hazard ratios (95% confidence intervals) for major macrovascular events and cardiovascular and all-cause death for >10% weight loss over 2 years (vs. stable weight), by age, BMI, and metformin use.
All P for interaction with weight change categories >0.05. Models adjusted for age, sex, region, baseline hemoglobin A1c, baseline systolic blood pressure, history of macrovascular disease at baseline, history of microvascular disease at baseline, glucose treatment assignment, blood pressure treatment assignment, baseline smoking status (current/former/never), baseline statin use, and diabetes medication (metformin/thiazolidinediones/sulfonylureas/insulin) use at year 2 (unless variable was being tested for interaction). Models evaluating interaction by metformin use excluded individuals using thiazolidinediones at year 2. BMI, body mass index.
Lee et al. The Risks of Cardiovascular Disease and Mortality Following Weight Change in Adults with Diabetes: Results from ADVANCE.
The associations of 2-year weight change with year 2 levels and 2-year change in cardiovascular risk factors were mixed (Table 3). For HbA1c, as with baseline levels, year 2 levels were different across weight change categories, but the 2-year changes did not differ by weight change categories in either the intensive or standard glucose treatment arms. For all other cardiovascular disease risk factors, weight change was significantly associated with both year 2 levels and 2-year changes (except for year 2 levels of low-density lipoprotein cholesterol), with improvement in cardiovascular risk factors among those who lost weight and mixed results among those who gained the most weight.
Table 3.
Unadjusted Means (SD) of Blood Pressure, HbA1c, and Lipids by Intervention Arms and Weight Change At 2 Years
| >10% Weight Loss | 4–10% Weight Loss | Stable (±<4%) | 4–10% Weight Gain | >10% Weight Gain | P for Trend | |
|---|---|---|---|---|---|---|
| Intensive HbA1c arm, n (%) | 217 (4.3%) | 878 (17.3%) | 2782 (54.8%) | 894 (17.6%) | 309 (6.1%) | |
| HbA1c y 2 | 6.4 (0.9) | 6.6 (1.0) | 6.7 (1.0) | 6.8 (1.0) | 6.8 (0.9) | <0.001 |
| HbA1c change (baseline to y 2) | –0.9 (1.5) | –0.8 (1.4) | –0.7 (1.4) | –0.7 (1.6) | –1.1 (1.8) | 0.79 |
| Standard HbA1c arm, n (%) | 215 (4.3%) | 976 (19.5%) | 2931 (58.6%) | 654 (13.1%) | 225 (4.5%) | |
| HbA1c y 2 | 6.8 (1.4) | 7.2 (1.4) | 7.3 (1.3) | 7.5 (1.5) | 7.4 (1.3) | <0.001 |
| HbA1c change (baseline to y 2) | –0.4 (1.4) | –0.3 (1.3) | –0.1 (1.4) | –0.1 (1.7) | –0.4 (1.8) | 0.09 |
| Intervention BP arm, n (%) | 243 (4.8%) | 1045 (20.7%) | 2803 (55.5%) | 703 (13.9%) | 260 (5.1%) | |
| SBP y 2 | 131.1 (18.3) | 132.2 (18.3) | 135.5 (18.2) | 136.9 (18.7) | 137.0 (17.3) | <0.001 |
| SBP change (baseline to y 2) | –6.8 (20.5) | –4.1 (19.2) | –2.1 (18.0) | –0.6 (19.9) | 1.3 (20.5) | <0.001 |
| DBP y 2 | 73.1 (10.3) | 73.9 (9.7) | 76.1 (9.9) | 75.9 (9.9) | 75.9 (10.1) | <0.001 |
| DBP change (baseline to y 2) | –4.7 (11.5) | –3.2 (10.1) | –1.9 (9.9) | –1.8 (10.6) | –1.1 (10.6) | <0.001 |
| Placebo BP arm, n (%) | 189 (3.8%) | 809 (16.1%) | 2910 (57.9%) | 845 (16.8%) | 274 (5.5%) | |
| SBP y 2 | 135.1 (18.9) | 138.7 (18.6) | 141.0 (18.3) | 141.7 (18.5) | 143.1 (19.9) | <0.001 |
| SBP change (baseline to y 2) | –2.8 (21.0) | 1.2 (19.7) | 4.2 (19.2) | 4.7 (20.2) | 5.9 (21.4) | <0.001 |
| DBP y 2 | 74.6 (10.6) | 75.9 (10.3) | 78.2 (9.7) | 78.5 (9.6) | 79.2 (10.0) | <0.001 |
| DBP change (baseline to y 2) | –2.4 (10.1) | –1.3 (10.4) | 0.6 (10.2) | 0.7 (10.4) | 1.3 (10.7) | <0.001 |
| All participants, n (%) | 432 (4.3%) | 1854 (18.4%) | 5713 (56.7%) | 1548 (15.4%) | 534 (5.3%) | |
| Total cholesterol y 2 | 188.7 (42.5) | 187.3 (44.6) | 185.4 (41.8) | 188.3 (42.6) | 189.5 (43.2) | 0.04 |
| Total cholesterol change (baseline to y 2) | –12.2 (42.2) | –15.1 (40.1) | –16.5 (39.3) | –12.0 (41.5) | –12.3 (43.3) | 0.004 |
| HDL y 2 | 49.0 (13.5) | 50.2 (14.5) | 50.0 (15.1) | 47.8 (13.6) | 48.6 (13.9) | <0.001 |
| HDL change (baseline to y 2) | 0.6 (12.0) | 2.1 (13.0) | 1.2 (13.4) | –0.7 (12.0) | –1.1 (11.9) | <0.001 |
| LDL y 2 | 109.9 (36.3) | 109.5 (38.9) | 108.2 (36.8) | 108.7 (35.6) | 112.2 (38.4) | 0.20 |
| LDL change (baseline to y 2) | –10.1 (37.6) | –15.0 (41.6) | –12.7 (36.4) | –10.3 (36.8) | –7.4 (40.2) | <0.001 |
| Triglycerides y 2 | 165.4 (105.6) | 146.2 (95.9) | 153.5 (89.8) | 174.5 (116.0) | 166.5 (96.5) | <0.001 |
| Triglycerides change (baseline to y 2) | –9.2 (98.7) | –24.1 (112.2) | –20.3 (106.1) | –0.0 (118.0) | –4.3 (94.5) | <0.001 |
Abbreviations: BP, blood pressure; DBP, diastolic blood pressure; HbA1c, hemoglobin A1c; LDL, low-density lipoprotein; SBP, systolic blood pressure; SD, standard deviation; y, year.
Discussion
This large prospective study of adults with type 2 diabetes participating in ADVANCE found that >10% weight loss was associated with >2 times higher risk of cardiovascular and all-cause mortality and was associated with 75% greater risk of major macrovascular events, compared with adults with stable weight. These associations were not significantly modified by metformin use, age, or baseline BMI. The increased risk of cardiovascular events and death in those with >10% weight loss occurred despite improvements in cardiovascular risk factors. Because cardiovascular risk factors improved more in those with 4% to 10% weight loss compared with >10% weight loss, it is possible that a fraction of individuals from the >10% loss group had worsening cardiovascular risk factors and were at a higher risk of cardiovascular events and mortality. Our study suggests that >10% weight loss can be a marker of increased cardiovascular risk and mortality.
To our knowledge, this is the first study to demonstrate that substantial weight loss in diabetes may be associated with increased risk of cardiovascular events. Previous studies in the general population found mixed results for weight loss and mortality, but the consensus is that unintentional weight loss is strongly tied to increased mortality (30). These studies also indicated that there is heterogeneity in the effect of weight loss by intentionality (11–14, 31–33). In a study of middle-aged men, unintentional weight loss was associated with 15% increased risk of mortality in individuals with existing health conditions but not in individuals without existing health conditions (12), whereas intentional weight loss in both groups had no association with death. In an analysis of women from the same cohort, there was no association between unintentional weight loss and risk of mortality, regardless of existing health conditions, whereas intentional weight loss among those with existing health conditions was protective (31). A study of older British men found that unintentional weight loss was associated with a 71% increased risk of mortality, compared with those with stable weight, and that the association of intentional weight loss with mortality differed by whether the weight loss was due to personal choice or to doctors’ advice (13). Overall, these studies showed relatively less risk with unintentional weight loss compared with our finding of 179% greater mortality risk with >10% weight loss. This could be due to other studies’ reliance on self-reported weight and inclusion of all amounts of weight loss compared with our high threshold of >10% weight loss. Additionally, some but not all studies found older adults had worse outcomes following weight loss (11, 13), whereas our study found no difference in associations by age. We found that substantial weight loss in adults aged 55 to 65 with diabetes was similarly indicative of poor prognosis as compared with older adults in our study population.
We also found increased risk of cardiovascular events and mortality following >10% weight loss despite a decrease in cardiovascular risk factors by year 2. Although this may seem counterintuitive, it is consistent with other literature showing that the association of cardiovascular risk factors with cardiovascular events and mortality becomes weaker and sometimes inverse with increasing age (34–36) and frailty (37, 38). Thus, as overall health declines, cardiovascular risk factors become less indicative of future risk.
The extremes of weight change tended to be more strongly associated with outcomes in the shorter term follow-up of ADVANCE compared with the longer term follow-up of ADVANCE-ON. This could be due to subsequently changing weight that reduced the long-term effects, or, for large weight loss, the cardiometabolic benefits of weight loss may act over a longer time frame.
Patterns of intentional weight loss vary substantially, but during intensive weight loss attempts, weight often initially sharply declines during the first few months and then is slowly regained over the subsequent months to years (39). Although clinical trials aim for sustained weight loss of 7% (7, 40, 41), in real-world settings, intentional weight loss attempts average between 3% and 5% during the first 3 months to 1 year (42, 43). However, the magnitude of unintentional weight loss may be similar to intentional weight loss, with several studies showing self-reported unintentional weight loss around 4% to 5% (13, 18). Medicare-certified nursing homes are required to report on individuals losing >5% weight in 30 days or >10% in 180 days because these rapid losses may indicate failing health. In our study, we defined the highest category of weight loss to be >10% over 2 years, a high threshold that likely captures mostly individuals with unintentional weight loss and a small fraction of individuals with intentional weight loss. Providers should be aware of the difficulties of achieving sustained intentional weight loss. Even among middle-aged patients with diabetes, modest or large weight loss in the absence of dietary and exercise modifications is potentially a cause for concern.
Other studies have noted that frequent weight changes, or weight cycling, may independently contribute to increased morbidity and mortality (44, 45). In a sensitivity analysis, we controlled for weight cycling (defined as >5-kg gain and loss within the first 2 years) and our results did not change (data not shown), indicating that weight cycling does not explain the association between large weight loss and cardiovascular disease and mortality.
Unintentional weight loss may be due to a variety of causes. Although unintentional weight loss is often thought to be due to undiagnosed illness, such as cancer, many cases of unintentional weight loss are idiopathic even after clinical investigation (25, 46). Among older adults, unintentional weight loss may be related to diminished appetite due to decreased physical activity, difficulty with dentition, drug interactions, depression, dementia, or loss in taste and/or smell (25). It is important to identify the causes so the appropriate corrective actions can be taken, such as fitting dentures for people with poor dentition, changing medications or their timing to reduce influence on appetite, and increasing caloric intake through adding preferred foods or increasing the size of the favorite meal of the day (25).
Unintentional weight loss likely represents a loss of physical reserve and activation of catabolic pathways with wide-ranging harms. The physiology of unintentional weight loss has primarily been studied in cachexia, in which increases in catabolic cytokines contribute to myocyte apoptosis and inflammation (47). Large weight loss with nutritional deficiencies could also lead to electrolyte imbalances, causing cardiac arrhythmias.
There are several limitations to our study. First, we were not able to determine whether weight change was intentional or unintentional. The observed detrimental effects of weight loss on mortality are more consistent with unintentional weight loss, but there was likely a mix of intentional and unintentional weight loss. Second, this trial may miss some of the potential metabolic benefits of weight loss because of the interventions for blood pressure and HbA1c. We observed that, although participants’ 2-year weight change was not correlated with 2-year HbA1c change, other cardiovascular risk factors did improve with weight loss, suggesting that the cardiometabolic benefits of weight loss were realized except for HbA1c. Third, we were underpowered to look at interactions, and thus results by medication use should be interpreted appropriately. Fourth, we did not have information available on diet, which likely influences both weight and cardiovascular disease (48, 49). Finally, we were not able to evaluate the long-term association of weight change with microvascular events because of the change in endpoint definition for ADVANCE-ON.
Our study also has several important strengths. ADVANCE was a large trial with ethnically diverse participants and adjudicated endpoints. Second, weight was measured, rather than self-reported, increasing the validity of our primary exposure of interest, weight change. Third, because medications were closely monitored, we were able to determine if glucose-lowering medication use altered the association of weight change with outcomes.
In conclusion, our study demonstrated a detrimental association of weight loss on cardiovascular outcomes and mortality in adults with type 2 diabetes. Because many causes of unintentional weight loss can be mitigated (25, 46), timely assessment is critical. Unless patients specifically report lifestyle changes to lose weight, even modest weight loss may be a marker of declining health for which further clinical investigation is merited.
Acknowledgments
The authors thank ADVANCE staff and participants for their valuable contributions.
Financial Support: This research was supported in part by National Institutes of Health (NIH)/National Institute of Diabetes and Digestive and Kidney (NIDDK) grant R01DK108784 (E.S.). A.K.L. and B.W. were supported by NIH/National Heart, Lung, and Blood Institute grant T32HL007024. E.S. was also supported by NIH/NIDDK grant K24DK106414. J.C. and M.W. were supported by the National Health and Medical Council of Australia. The ADVANCE Trial was supported by grants from Servier (the major financial sponsor) and the National Health and Medical Research Council of Australia (211086 and 358395). Servier manufactures gliclazide (modified release) and the fixed combination of perindopril and indapamide. ADVANCE-ON was supported by the National Health and Medical Research Council of Australia (1006367, 358395, and 571281), a joint grant from Diabetes UK and the British Heart Foundation (28562), and an unrestricted educational grant from Servier International. The authors of this manuscript had control in the development of the statistical analysis plan and data analysis and the funder had no role in the decision to submit this manuscript for publication.
Author Contributions: A.K.L. conceived and designed the study, conducted statistical analyses, and wrote the manuscript. M.W. provided guidance for the statistical analysis and made critical revisions to the manuscript for important intellectual content. D.W. also conducted statistical analyses and made critical revisions to the manuscript for important intellectual content. E.S. helped to conceive and design the study, provided guidance for the statistical analysis, and made critical revisions to the manuscript for important intellectual content. All other authors made critical revisions to the manuscript for important intellectual content. E.S. is the guarantor of this work and had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Glossary
Abbreviations
- BMI
body mass index
- 95% CI
95% confidence interval
- HbA1c
hemoglobin A1c
- HR
hazard ratio
- TZD
thiazolidinedione
Additional Information
Prior Presentation: Parts of this study were presented in abstract form at the American Diabetes Association Scientific Sessions, San Diego, CA, 9-13 June 2017.
Data Availability: The datasets generated during and/or analyzed during the current study are not publicly available but may be available from the corresponding author on reasonable request.
Disclosure Summary: The authors have nothing to disclose.
References
- 1. Fox CS, Golden SH, Anderson C, et al.; American Heart Association Diabetes Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Clinical Cardiology, Council on Cardiovascular and Stroke Nursing, Council on Cardiovascular Surgery and Anesthesia, Council on Quality of Care and Outcomes Research; American Diabetes Association . Update on prevention of cardiovascular disease in adults with type 2 diabetes mellitus in light of recent evidence: a scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care. 2015;38(9):1777–1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Halter JB, Musi N, McFarland Horne F, et al. Diabetes and cardiovascular disease in older adults: current status and future directions. Diabetes. 2014;63(8):2578–2589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. American Diabetes Association. Standards of medical care in diabetes-- 2019. Diabetes Care. 2019;42(Suppl 1):S81–S89. [DOI] [PubMed] [Google Scholar]
- 4. Wing RR, Lang W, Wadden TA, et al.; Look AHEAD Research Group . Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34(7):1481–1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Franz MJ, Boucher JL, Rutten-Ramos S, VanWormer JJ. Lifestyle weight-loss intervention outcomes in overweight and obese adults with type 2 diabetes: a systematic review and meta-analysis of randomized clinical trials. J Acad Nutr Diet. 2015;115(9):1447–1463. [DOI] [PubMed] [Google Scholar]
- 6. Wing RR, The Look AHEAD Research Group . Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus. Arch Intern Med. 2010;170(17):1566–1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. The Look AHEAD Research Group. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med. 2013;155–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. The Look AHEAD Research Group. Association of the magnitude of weight loss and changes in physical fitness with long-term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: a post-hoc analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol. 2016;4(11):913–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dombrowski SU, Avenell A, Sniehott FF. Behavioural interventions for obese adults with additional risk factors for morbidity: systematic review of effects on behaviour, weight and disease risk factors. Obes Facts. 2010;3(6):377–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Strelitz J, Ahern AL, Long GH, Moderate weight change following diabetes diagnosis and 10 year incidence of cardiovascular disease and mortality. Diabetologia. 2019;62(8):1391–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wedick NM, Barrett-Connor E, Knoke JD, Wingard DL. The relationship between weight loss and all-cause mortality in older men and women with and without diabetes mellitus: the Rancho Bernardo study. J Am Geriatr Soc. 2002;50(11):1810–1815. [DOI] [PubMed] [Google Scholar]
- 12. Williamson DF, Pamuk E, Thun M, Flanders D, Byers T, Heath C. Prospective study of intentional weight loss and mortality in overweight white men aged 40-64 years. Am J Epidemiol. 1999;149(6):491–503. [DOI] [PubMed] [Google Scholar]
- 13. Wannamethee SG, Shaper AG, Lennon L. Reasons for intentional weight loss, unintentional weight loss, and mortality in older men. Arch Intern Med. 2005;165(9):1035–1040. [DOI] [PubMed] [Google Scholar]
- 14. Chen Y, Yang X, Wang J, Li Y, Ying D, Yuan H. Weight loss increases all-cause mortality in overweight or obese patients with diabetes: a meta-analysis. Medicine (Baltimore). 2018;97(35):e12075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fried LP, Tangen CM, Walston J, et al. Cardiovascular Health Study Collaborative Research Group . Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M156. [DOI] [PubMed] [Google Scholar]
- 16. Ensrud KE, Ewing SK, Stone KL, Cauley JA, Bowman PJ, Cummings SR; Study of Osteoporotic Fractures Research Group . Intentional and unintentional weight loss increase bone loss and hip fracture risk in older women. J Am Geriatr Soc. 2003;51(12):1740–1747. [DOI] [PubMed] [Google Scholar]
- 17. Rabinovitz M, Pitlik SD, Leifer M, Garty M, Rosenfeld JB. Unintentional weight loss. A retrospective analysis of 154 cases. Arch Intern Med. 1986;146(1):186–187. [DOI] [PubMed] [Google Scholar]
- 18. Wallace JI, Schwartz RS, LaCroix AZ, Uhlmann RF, Pearlman RA. Involuntary weight loss in older outpatients: incidence and clinical significance. J Am Geriatr Soc. 1995;43(4):329–337. [DOI] [PubMed] [Google Scholar]
- 19. Thompson MP, Morris LK. Unexplained weight loss in the ambulatory elderly. J Am Geriatr Soc. 1991;39(5):497–500. [DOI] [PubMed] [Google Scholar]
- 20. Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38(1):140–149. [DOI] [PubMed] [Google Scholar]
- 21. ADVANCE Management Committee. Study rationale and design of the ADVANCE study: a randomised trial of blood pressure lowering and intensive glucose control in high-risk individuals with type 2 diabetes mellitus. Action in diabetes and vascular disease: preterax and diamicron modified-R. Diabetologia. 2001;44:1118–1120. [DOI] [PubMed] [Google Scholar]
- 22. ADVANCE Collaborative Group. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet. 2007;370:829–840. [DOI] [PubMed] [Google Scholar]
- 23. ADVANCE Collaborative Group. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358(24):2560–2572. [DOI] [PubMed] [Google Scholar]
- 24. Zoungas S, Chalmers J, Neal B, et al.; ADVANCE-ON Collaborative Group . Follow-up of blood-pressure lowering and glucose control in type 2 diabetes. N Engl J Med. 2014;371(15):1392–1406. [DOI] [PubMed] [Google Scholar]
- 25. Bouras EP, Lange SM, Scolapio JS. Rational approach to patients with unintentional weight loss. Mayo Clin Proc. 2001;76(9):923–929. [DOI] [PubMed] [Google Scholar]
- 26. Tanne JH. FDA places “black box” warning on antidiabetes drugs. Bmj. 2007;334(7606):1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rådholm K, Chalmers J, Ohkuma T, et al. Use of the waist-to-height ratio to predict cardiovascular risk in patients with diabetes: results from the ADVANCE-ON study. Diabetes Obes Metab. 2018;20(8):1903–1910. [DOI] [PubMed] [Google Scholar]
- 28. Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012;13(3):275–286. [DOI] [PubMed] [Google Scholar]
- 29. Freis ED, Reda DJ, Materson BJ. Volume (weight) loss and blood pressure response following thiazide diuretics. Hypertension. 1988;12(3):244–250. [DOI] [PubMed] [Google Scholar]
- 30. Harrington M, Gibson S, Cottrell RC. A review and meta-analysis of the effect of weight loss on all-cause mortality risk. Nutr Res Rev. 2009;22(1):93–108. [DOI] [PubMed] [Google Scholar]
- 31. Williamson DF, Pamuk E, Thun M, Flanders D, Byers T, Heath C. Prospective study of intentional weight loss and mortality in never-smoking overweight US white women aged 40-64 years. Am J Epidemiol. 1995;141(12):1128–1141. [DOI] [PubMed] [Google Scholar]
- 32. Williamson DF, Thompson TJ, Thun M, Flanders D, Pamuk E, Byers T. Intentional weight loss and mortality among overweight individuals with diabetes. Diabetes Care. 2000;23(10):1499–1504. [DOI] [PubMed] [Google Scholar]
- 33. Wannamethee SG, Shaper AG, Walker M. Weight change, weight fluctuation, and mortality. Arch Intern Med. 2002;162(22):2575–2580. [DOI] [PubMed] [Google Scholar]
- 34. Weverling-Rijnsburger AW, Blauw GJ, Lagaay AM, Knook DL, Meinders AE, Westendorp RG. Total cholesterol and risk of mortality in the oldest old. Lancet. 1997;350(9085):1119–1123. [DOI] [PubMed] [Google Scholar]
- 35. Fried LP, Kronmal RA, Newman AB, et al. Risk factors for 5-year mortality in older adults: the Cardiovascular Health Study. JAMA. 1998;279(8):585–592. [DOI] [PubMed] [Google Scholar]
- 36. Satish S, Freeman DH Jr, Ray L, Goodwin JS. The relationship between blood pressure and mortality in the oldest old. J Am Geriatr Soc. 2001;49(4):367–374. [DOI] [PubMed] [Google Scholar]
- 37. Odden MC, Peralta CA, Haan MN, Covinsky KE. Rethinking the association of high blood pressure with mortality in elderly adults: the impact of frailty. Arch Intern Med. 2012;172(15):1162–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ravindrarajah R, Hazra NC, Hamada S, et al. Systolic blood pressure trajectory, frailty, and all-cause mortality >80 years of age: cohort study using electronic health records. Circulation. 2017;135(24):2357–2368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dombrowski SU, Knittle K, Avenell A, Araújo-Soares V, Sniehotta FF. Long term maintenance of weight loss with non-surgical interventions in obese adults: systematic review and meta-analyses of randomised controlled trials. BMJ. 2014;348:g2646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. The Look AHEAD Research Group. Look AHEAD (Action for Health in Diabetes): design and methods for a clinical trial of weight loss for the prevention of cardiovascular disease in type 2 diabetes. Control Clin Trials. 2003;24(5):610–628. [DOI] [PubMed] [Google Scholar]
- 41. Knowler WC, Barrett-Connor E, Fowler SE, et al.; Diabetes Prevention Program Research Group . Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ali MK, Echouffo-Tcheugui J, Williamson DF. How effective were lifestyle interventions in real-world settings that were modeled on the diabetes prevention program? Health Aff (Millwood). 2012;31(1):67–75. [DOI] [PubMed] [Google Scholar]
- 43. Gudzune KA, Doshi RS, Mehta AK, et al. Efficacy of commercial weight-loss programs: an updated systematic review. Ann Intern Med. 2015;162(7):501–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mehta T, Smith DL Jr, Muhammad J, Casazza K. Impact of weight cycling on risk of morbidity and mortality. Obes Rev. 2014;15(11):870–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bangalore S, Fayyad R, Laskey R, DeMicco DA, Messerli FH, Waters DD. Body-weight fluctuations and outcomes in coronary disease. N Engl J Med. 2017;376(14):1332–1340. [DOI] [PubMed] [Google Scholar]
- 46. Marton KI, Sox HC Jr, Krupp JR. Involuntary weight loss: diagnostic and prognostic significance. Ann Intern Med. 1981;95(5):568–574. [DOI] [PubMed] [Google Scholar]
- 47. Argilés JM, Busquets S, Stemmler B, López-Soriano FJ. Cachexia and sarcopenia: mechanisms and potential targets for intervention. Curr Opin Pharmacol. 2015;22:100–106. [DOI] [PubMed] [Google Scholar]
- 48. Mazidi M, Katsiki N, Mikhailidis DP, Sattar N, Banach M. Lower carbohydrate diets and all-cause and cause-specific mortality: a population-based cohort study and pooling of prospective studies. Eur Heart J. 2019;1–10. [DOI] [PubMed] [Google Scholar]
- 49. Tobias DK, Chen M, Manson JE, Ludwig DS, Willett W, Hu FB. Effect of low-fat diet interventions versus other diet interventions on long-term weight change in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2015;3(12):968–979. [DOI] [PMC free article] [PubMed] [Google Scholar]