Abstract
OBJECTIVES
This study aimed to evaluate the efficacy of the repositioning maneuver on quality of life in elderly patients with dizziness and/or vertigo.
MATERIALS and METHODS
This controlled, prospective randomized clinical trial was conducted in elderly patients aged 65 years and above with a positive history of benign paroxysmal positional vertigo (BPPV), presence of vertigo, and no observable nystagmus during the Dix-Hallpike test, so-called Subjective BPPV (S-BPPV). Individuals were evaluated by visual analog scale (VAS) and dizziness handicap inventory (DHI). Groups were defined as treatment (treated with Epley maneuver bilaterally) or no treatment control (no treatment modality or canalith repositioning maneuver). Ten days after the first assessment, all patients were reassessed using VAS and DHI.
RESULTS
A total of 50 patients were randomized into two groups: 25 to the treatment group, and 25 to the control group. No significant differences were observed for baseline VAS and total DHI scores between the groups (p=0.636, p=0.846, respectively). On the other hand, after the reassessment, VAS and total DHI scores were both significantly reduced in the treatment group (p<0.001, p<0.001, respectively), but no reduction in either score was found in the control group (p=0.216, p=0.731, respectively).
CONCLUSION
This study showed that elderly patients with S-BPPV benefit from the Epley maneuver, in particular global and disease-specific quality of life.
Keywords: Benign paroxysmal positional vertigo, quality of life, epley maneuver, dizziness handicap inventory, visual analog scale, elderly
INTRODUCTION
Dizziness, vertigo, and imbalance are medical conditions that elderly people frequently complain of [1]. These conditions give rise to immobility and limitations in daily activities for them [1, 2]. In addition, especially in this population, dizziness is an important risk factor for morbidity related to falls and serious injuries [2]. A peripheral vestibular disorder or a central neurological problem may cause dizziness, but peripheral causes are more common with age [3]. The incidence of dizziness increases with age, and its prevalence varies from 36% to 45% in the elderly population [4, 5]. One of the most common medical conditions that cause peripheral dizziness in elderly patients (42%) is benign paroxysmal positional vertigo (BPPV) [6].
BPPV is diagnosed by the characteristic anamnesis and nystagmus using provocation tests [7]. In some cases, even though patients reporting dizziness have a characteristic history of BPPV, nystagmus may not be observed during the Dix-Hallpike maneuver. In these cases, repetition of the Dix-Hallpike maneuver at different times and use of the supine roll maneuver have been recommended to evaluate horizontal canal BPPV (h-BPPV) [7]. If there is an absence of nystagmus and presence of vertigo during the provocative maneuver with a positive history for BPPV, this phenomenon is called “subjective BPPV” (S-BPPV) [8]. Patients with S-BPPV constitute 12%–48% of the total number of BPPV cases [9, 10]. The Epley maneuver is recommended for the treatment of both of S-BPPV and objective posterior canal BPPV (p-BPPV) [8, 11].
This prospective randomized study aimed to evaluate the efficacy of the Epley maneuver on the quality of life in elderly patients with a positive history of BPPV but without any observable nystagmus during the Dix-Hallpike test.
MATERIALS AND METHODS
This clinical trial enrolled elderly patients aged 65 years and above with dizziness or vertigo and with diagnosed anamnesis [(i) rotatory dizziness or vertigo triggered by head position, (ii) occurs with short latency and with duration of vertigo less than a minute, (iii) no relationship between cochlear symptoms and dizziness or vertigo, (iv) no additional neurologic symptoms or central nervous system disorder]. The presence of vertigo and absence of detectable nystagmus during the Dix-Hallpike maneuver indicated S-BPPV. All patients underwent the bilateral supine roll test to exclude h-BPPV as recommended in guidelines for BPPV [7].
The following patients were excluded from the study: patients with cochlear symptoms related to vertigo or dizziness, with a history of previously diagnosed BPPV or other peripheral vestibular disorders, positive supine roll test, more vertiginous symptoms during the supine roll test other than the Dix-Hallpike test, taking any anti-vertiginous drugs, patients with abnormal findings of the ear such as infection, tympanic membrane perforation, cholesteatoma, or tumor, vertebrobasilar insufficiency, central nervous system diseases, abnormal intracranial findings fromof magnetic resonance imaging (MRI), limited cervical and head movements, cervical neurological symptoms, uncontrolled systemic diseases, or patients who were unable to communicate, for example, understanding and responding to verbal commands. This study was conducted as a single-center, prospective, randomized, and controlled trial. The local ethics committee approved this study (No. 20.478.486). This study was performed according to the principles of the Declaration of Helsinki. Informed written consent was obtained from the subjects.
Elderly patients with the abovementioned symptoms for study inclusion underwent a complete otorhinolaryngological examination by an otorhinolaryngologist and neurological examination by a neurologist. All patients underwent MRI to exclude central nervous disorders. In the study, all maneuvers were performed by the same physician. If there was no observable nystagmus during the Dix-Hallpike maneuver and supine roll test performed bilaterally with Frenzel glasses, the patients were randomized into two groups: the treatment group (the Epley maneuver was performed bilaterally), and the no treatment control group (the Epley maneuver or other canalith repositioning maneuvers were not performed). We did not identify any affected side, and repositioning maneuvers were applied on both sides in the treatment group. All patients were evaluated by visual analog scale (VAS) and dizziness handicap inventory (DHI) on day 1 before the physical examination and again 10 days after the first visit. Global quality of life of patients assessed by VAS ranged from 0 (best) to 10 (worst) [12]. The Turkish version of the DHI used in the study had been adapted and validated previously [13]. The DHI is a widely used validated scale to assess the extent of disability of patients with vertigo. It consists of 25 questions and 3 subscales that evaluate physical (DHI-P, 7 items), emotional (DHI-E, 9 items), and functional (DHI-F 9 items) outcomes of patients. The total score of the DHI can vary between 0 (no disability) and 100 (severe disability) [14].
Statistical Analysis
The data were analyzed and processed using a statistical software (SPSS for Mac v.20.0; SPSS Inc., Chicago, IL, USA). We determined that at least 22 patients in each group should be enrolled to achieve a power of 85%, allowing for a type I error of 0.05 and effect size of 0.95. Allowing for %10 loss to follow-up, 25 patients per group were needed. Quantitative variables were summarized as mean±SD. The chi-square test was used to compare categorical variables. The Mann-Whitney U-test and Wilcoxon test were used with the level of significance set at p<0.05.
RESULTS
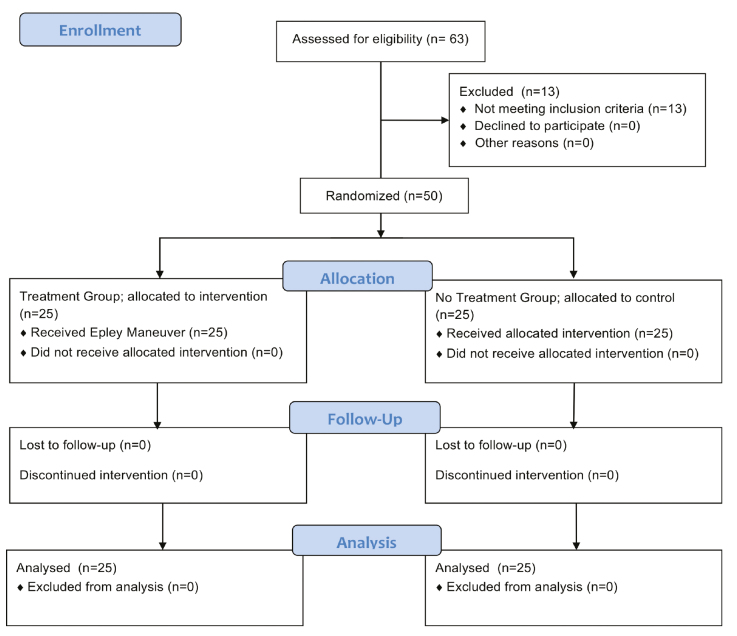
A total of 63 patients were assessed for inclusion in the study, and 13 patients were excluded as they did not meet the inclusion criteria. Fifty individuals with dizziness and vertigo complaints were enrolled in the study and randomized into 25 treatment group subjects and 25 control group subjects. Figure 1 shows a “Consolidated Standards of Reporting Trials” (CONSORT) flow chart for the study. The mean ages of patients in the treatment group and control group were 70.2±5.15 and 71.8±6.09 years, respectively (Table 1). The patients in both groups were similar in terms of age and sex (p=0.344, p=0.544, respectively). Table 1 includes all characteristics of the treatment and control groups including VAS and DHI scores.
Figure 1.
Flow chart for this study.
Table 1.
Demographics of treatment and control groups with dizziness or vertigo
| Treatment group | Control group | p | |||
|---|---|---|---|---|---|
| Sex, n (F/M) | 25 (16/9) | 25 (18/7) | 0.544 | ||
| Age, mean±SD, years | 70.2±5.15 | 71.8±6.09 | 0.344 | ||
| VAS score, mean±SD | 7.5±1.92 | 7.8±1.69 | 0.636 | ||
| DHI score, mean±SD | Total | 51±25.79 | 50.5±25.03 | 0.846 | |
| Subscale | Physical score | 17±8.53 | 17.8±8.22 | 0.784 | |
| Emotional score | 13.8±8.82 | 12.4±10.03 | 0.546 | ||
| Functional score | 20.2±11.11 | 20.6±9.57 | 0.922 | ||
DHI: Dizziness Handicap Inventory; VAS: Visual Analog Scale.
VAS and total DHI scores at the start of the study were not statistically significantly different between the treatment group and control group (p=0.636, p=0.846; respectively, Table 1). Table 2 shows that the VAS, total, and subscale DHI scores (DHI-P, DHI-E, and DHI-F) statistically significantly improved after the Epley maneuver (VAS1stVisit=7.5±1.92, VAS2ndVisit=6.3±2.11, p<0.001; Total-DHI1stVisit=51±25.79, Total-DHI2ndVisit=40.6±23.21, p<0.001; DHI-P1stVisit=17±8.53, DHI-P2ndVisit=13.8±7.68, p=0.001; DHI-E1stVisit=13.8±8.82, DHI-E2ndVisit=11±8.21, p=0.003; DHI-F1stVisit=20.2±11.11, DHI-F2ndVisit=16±9.63, p=0.001). On the other hand, in the control group, no significant difference was observed between VAS, total, and subscale DHI scores for the first and second visits (VAS1stVisit=7.8±1.69, VAS2ndVisit=7.5±1.53, p=0.216; Total-DHI1stVisit=50.5±25.03, Total-DHI2ndVisit=48.5±21.29, p=0.731; DHI-P1stVisit=17.8±8.22, DHI-P2ndVisit=16.5±7.62, p=0.169; DHI-E1stVisit=12.4±10.03, DHI-E2ndVisit=13±8.66, p=0.311; DHI-F1stVisit=20.6±9.57, DHI-F2ndVisit=19.4±8.48, p=0.292). In addition, significant improvements were observed in VAS and total DHI scores in patients who underwent the Epley maneuver compared to those in the control group as shown in Table 3 (p=0.024, p=0.003, respectively).
Table 2.
VAS and DHI scores at the time of the first and second assessments in the treatment and control groups
| Treatment group | Control group | |||||||
|---|---|---|---|---|---|---|---|---|
| First assessment | Second assessment | p | First assessment | Second assessment | p | |||
| VAS score, mean±SD | 7.5±1.92 | 6.3±2.11 | <0.001 | 7.8±1.69 | 7.5±1.53 | 0.216 | ||
| DHI score, mean±SD | Total | 51±25.79 | 40.6±23.21 | <0.001 | 50.5±25.03 | 48.5±21.29 | 0.731 | |
| Subscale | Physical | 17±8.53 | 13.8±7.68 | 0.001 | 17.8±8.22 | 16.5±7.62 | 0.169 | |
| Emotional | 13.8±8.82 | 11±8.21 | 0.003 | 12.4±10.03 | 13±8.66 | 0.311 | ||
| Functional | 20.2±11.11 | 16±9.63 | 0.001 | 20.6±9.57 | 19.4±8.48 | 0.292 | ||
DHI: Dizziness Handicap Inventory; VAS: Visual Analog Scale.
Table 3.
Comparison of improvement in VAS and DHI scores between treatment and control groups
| Treatment group | Control group | p | |||
|---|---|---|---|---|---|
| Improvement in VAS score, mean±SD | 1.2±1.3 | 0.3±1.21 | 0.024 | ||
| Improvement in DHI score, mean±SD | Total DHI score | 10.8±11.5 | 2±10 | 0.003 | |
| Subscale | Physical score | 3.5±3.84 | 1.4±4.31 | 0.025 | |
| Emotional score | 3.2±4.12 | −0.72±2.64 | <0.001 | ||
| Functional score | 4.6±4.92 | 1.28±5.22 | 0.013 | ||
DHI: Dizziness Handicap Inventory; VAS: Visual Analog Scale.
DISCUSSION
Dizziness and/or vertigo induce falls in elderly adults. Fracture or severe head injury is observed in 10%–15% of falls and is responsible for more than 90% of hip fractures [15, 16]. BPPV is the underlying cause for more than one-third of elderly patients who visit neuro-otology clinics with dizziness/vertigo [6]. Nystagmus might not be observed during the Dix-Hallpike test in some patients with a positive BPPV history.
Perhaps the most important of the possible results of these observations is that the positive predictive value of the Dix-Hallpike test is over 80%, while the negative predictive value is about 50% [17]. It has been shown in the literature that characteristics of otoconia such as smaller size and smaller amounts affect latent period, severity, duration, and presence of nystagmus [18, 19]. In addition, separated otoconia particles create more severe nystagmus than clumped particles [20]. Osteoporotic changes closely related to BPPV might alter the properties of otoconia and lead to changes in the nature of the nystagmus expected to be observed in elderly patients with BPPV [21]. As a result of the abovementioned changes, adequate and strong signals might be generated for vertiginous symptoms, and at the same time, absence of signals at a sufficiently strong level for stimulation of the vestibulo-ocular pathway might also occur in these cases and with no observable nystagmus [22].
The treatment of BPPV can be divided into canalith repositioning maneuvers and vestibular rehabilitation [7]. In p-BPPV, the recommended treatment modality is the Epley maneuver, according to the guidelines for BPPV [7]; and it has been found to be more effective than vestibular rehabilitation indicated as a second option [23]. In geriatric patients with p-BPPV, additional vestibular rehabilitation along with the Epley maneuver did not have any effect on BPPV recurrence compared to using only the Epley maneuver [24]. In addition, the Epley maneuver had positive effects on the quality of life in elderly patients with p-BPPV. Total DHI, subscale DHI, and VAS scores were significantly ameliorated seven days after the Epley maneuver in elderly patients with p-BPPV; however, those patients also received anti-vertiginous medications during the assessment [25]. In elderly patients with p-BPPV evaluated 30 days after the Epley maneuver using a 36-item Short Form Health Survey and a short form of the DHI (S-DHI, a screening version of the DHI), total scores of the S-DHI were significantly reduced [26]. In that study, role physical, body pain, vitality, social functioning, and mental health scores were significantly decreased, but no difference was observed in scores of physical functioning, general health, and role emotional [26]. Van der Zaag-Loonen et al. [27] stated that there was no difference in baseline DHI scores in elderly patients with p-BPPV vs patients with S-BPPV. DHI scores of p-BBPV decreased after the Epley maneuver; however, no data on the outcomes of S-BPPV patients were shared in that study. In this study, global quality of life in elderly patients with S-BPPV was assessed by VAS, and its score was significantly ameliorated in the treatment group; on the other hand, no score changes were observed in the no treatment control group.
As mentioned above, the Epley maneuver had positive effects on quality of life in elderly patients with p-BPPV. On the other hand, our literature survey showed that there has been no study that evaluated the efficacy of the Epley maneuver on quality of life in only elderly patients with S-BPPV. However, in a study in which patients with S-BPPV were evaluated in all age groups, the Epley maneuver significantly reduced the DHI scores, and the maneuver showed similar improvements in patients with either p-BPPV or S-BPPV; however, in that study, individuals did not undergo the supine roll test, and S-BPPV was diagnosed with latent onset of vertigo [28]. Other canalith repositioning maneuvers were also shown to be effective in treating vertiginous symptoms in patients with S-BPPV; however, both of these studies focused on posterior canal diseases and were evaluated with only the Dix-Hallpike test [22, 29]. Furthermore, canalith repositioning procedures had similar therapeutic effects in patients with S-BPPV and BPPV of all ages who underwent the Dix-Hallpike and supine roll tests; however, nystagmus was evaluated by naked-eye assessment in that study [30]. Weider et al. [10] showed that the one-year cure rate was 56% in patients with S-BPPV who underwent canalith repositioning maneuvers; and the possible cause of that lower rate (compared to the cure rate of the Epley maneuver in patients with BPPV) might be vestibular atelectasis or another disease.
In this study, similar to the abovementioned results, the Epley maneuver ameliorated the patients’ global and disease-specific quality of life, and total and subscale DHI scores were significantly decreased in the short term in elderly patients with S-BPPV. In our study, nystagmus was assessed by Frenzel lenses, which is a more sensitive method than naked-eye examination. Canalith repositioning maneuvers such as the Epley or Semont maneuvers were also recommended in the treatment of S-BPPV [8]. In particular, if BPPV is considered to be present in elderly patients with a positive history of BPPV but not nystagmus, canalith repositioning maneuvers should be immediately performed to prevent morbidity because, in untreated BPPV cases, spontaneous resolution might start within one month [23, 31].
CONCLUSION
To the best of our knowledge, this is the first study in which the efficacy of the Epley maneuver on quality of life in elderly patients with S-BPPV has been analyzed. It showed that the Epley maneuver had positive effects on quality of life in elderly patients with a positive history of BPPV and no observable nystagmus during the Dix-Hallpike and supine roll tests. In addition, this study suggested that this treatment modality could not only improve the quality of life in elderly patients but also prevent BPPV-related morbidities.
Footnotes
Ethics Committee Approval: Ethics Committee Approval was received for this study from the Ethics Committee of Manisa Celal Bayar University (26.07.2017-20.478.486).
Informed Consent: Written informed consent was obtained from the patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – U.U., D.U., G.A., O.Ç.; Design - U.U., D.U., G.A., O.Ç.; Supervision - G.A., O.Ç; Resource - U.U., D.U.; Materials - U.U., D.U.;Data Collection and/or Processing - U.U., D.U.,Analysis and/or Interpretation - U.U. Literature Search - U.U., D.U.; Writing - U.U., D.U., G.A., O.Ç.; Critical Reviews - G.A., O.Ç.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Aggarwal NT, Bennett DA, Bienias JL, Mendes de Leon CF, Morris MC, Evans DA. The prevalence of dizziness and its association with functional disability in a biracial community population. J Gerontol A Biol Sci Med Sci. 2000;55:M288–92. doi: 10.1093/gerona/55.5.M288. [DOI] [PubMed] [Google Scholar]
- 2.Mueller M, Strobl R, Jahn K, Linkohr B, Peters A, Grill E. Burden of disability attributable to vertigo and dizziness in the aged: results from the KORA-Age study. Eur J Public Health. 2014;24:802–7. doi: 10.1093/eurpub/ckt171. [DOI] [PubMed] [Google Scholar]
- 3.Muelleman T, Shew M, Subbarayan R, Shum A, Sykes K, Staecker H, et al. Epidemiology of Dizzy Patient Population in a Neurotology Clinic and Predictors of Peripheral Etiology. Otol Neurotol. 2017;38:870–5. doi: 10.1097/MAO.0000000000001429. [DOI] [PubMed] [Google Scholar]
- 4.Gopinath B, McMahon CM, Rochtchina E, Mitchell P. Dizziness and vertigo in an older population: the Blue Mountains prospective cross-sectional study. Clin Otolaryngol. 2009;34:552–6. doi: 10.1111/j.1749-4486.2009.02025.x. [DOI] [PubMed] [Google Scholar]
- 5.de Moraes SA, Soares WJ, Rodrigues RA, Fett WC, Ferriolli E, Perracini MR. Dizziness in community-dwelling older adults: a population-based study. Braz J Otorhinolaryngol. 2011;77:691–9. doi: 10.1590/S1808-86942011000600003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uneri A, Polat S. Vertigo, dizziness and imbalance in the elderly. J Laryngol Otol. 2008;122:466–9. doi: 10.1017/S0022215107000424. [DOI] [PubMed] [Google Scholar]
- 7.Bhattacharyya N, Gubbels SP, Schwartz SR, Edlow JA, El-Kashlan H, Fife T, et al. Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo (Update) Otolaryngol Head Neck Surg. 2017;156(Suppl 3):S1–S47. doi: 10.1177/0194599816689667. [DOI] [PubMed] [Google Scholar]
- 8.Jung JY, Kim SH. Comparison between objective and subjective benign paroxysmal positional vertigo: clinical features and outcomes. Acta Otolaryngol. 2016;136:1267–72. doi: 10.1080/00016489.2016.1203990. [DOI] [PubMed] [Google Scholar]
- 9.Norre ME. Reliability of examination data in the diagnosis of benign paroxysmal positional vertigo. Am J Otol. 1995;16:806–10. [PubMed] [Google Scholar]
- 10.Weider DJ, Ryder CJ, Stram JR. Benign paroxysmal positional vertigo: analysis of 44 cases treated by the canalith repositioning procedure of Epley. Am J Otol. 1994;15:321–6. [PubMed] [Google Scholar]
- 11.Abdelghaffar H. Effect of Canalith Repositioning Procedures (CRP) in Management of Subjective Benign Paroxysmal Positional Vertigo. J Int Adv Otol. 2010:34–8. [Google Scholar]
- 12.de Boer AG, van Lanschot JJ, Stalmeier PF, van Sandick JW, Hulscher JB, de Haes JC, et al. Is a single-item visual analogue scale as valid, reliable and responsive as multi-item scales in measuring quality of life? Qual Life Res. 2004;13:311–20. doi: 10.1023/B:QURE.0000018499.64574.1f. [DOI] [PubMed] [Google Scholar]
- 13.Canbal M, Cebeci S, Çamur Duyan G, Kurtaran H, Arslan I. A Study of Reliability and Validity for the Turkish Version of Dizziness Handicap Inventory. Turkish Journal of Family Medicine and Primary Care. 2016;10:19–24. doi: 10.5455/tjfmpc.198514. [DOI] [Google Scholar]
- 14.Jacobson GP, Newman CW. The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg. 1990;116:424–7. doi: 10.1001/archotol.1990.01870040046011. [DOI] [PubMed] [Google Scholar]
- 15.Zaag-Loonen HV, Bruintjes T, Leeuwen RV. Probable Benign Paroxysmal Positional Vertigo Converts into Definite BPPV in One in Six Patients. J Int Adv Otol. 2018;14:456–8. doi: 10.5152/iao.2018.4862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ishiyama G. Imbalance and vertigo: the aging human vestibular periphery. Semin Neurol. 2009;29:491–9. doi: 10.1055/s-0029-1241039. [DOI] [PubMed] [Google Scholar]
- 17.Hanley K, TOD Symptoms of vertigo in general practice: a prospective study of diagnosis. Br J Gen Pract. 2002;52:809–12. [PMC free article] [PubMed] [Google Scholar]
- 18.Squires TM, Weidman MS, Hain TC, Stone HA. A mathematical model for top-shelf vertigo: the role of sedimenting otoconia in BPPV. J Biomech. 2004;37:1137–46. doi: 10.1016/j.jbiomech.2003.12.014. [DOI] [PubMed] [Google Scholar]
- 19.Rajguru SM, Rabbitt RD. Afferent responses during experimentally induced semicircular canalithiasis. J Neurophysiol. 2007;97:2355–63. doi: 10.1152/jn.01152.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hain TC, Squires TM, Stone HA. Clinical implications of a mathematical model of benign paroxysmal positional vertigo. Ann N Y Acad Sci. 2005;1039:384–94. doi: 10.1196/annals.1325.036. [DOI] [PubMed] [Google Scholar]
- 21.Kim SY, Han SH, Kim YH, Park MH. Clinical features of recurrence and osteoporotic changes in benign paroxysmal positional vertigo. Auris Nasus Larynx. 2017;44:156–61. doi: 10.1016/j.anl.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 22.Haynes DS, Resser JR, Labadie RF, Girasole CR, Kovach BT, Scheker LE, et al. Treatment of benign positional vertigo using the semont maneuver: efficacy in patients presenting without nystagmus. Laryngoscope. 2002;112:796–801. doi: 10.1097/00005537-200205000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Wegner I, Niesten ME, van Werkhoven CH, Grolman W. Rapid Systematic Review of the Epley Maneuver versus Vestibular Rehabilitation for Benign Paroxysmal Positional Vertigo. Otolaryngol Head Neck Surg. 2014;151:201–7. doi: 10.1177/0194599814534940. [DOI] [PubMed] [Google Scholar]
- 24.Ribeiro KM, Ferreira LM, Freitas RV, Silva CN, Deshpande N, Guerra RO. “Positive to Negative” Dix-Hallpike test and Benign Paroxysmal Positional Vertigo recurrence in elderly undergoing Canalith Repositioning Maneuver and Vestibular Rehabilitation. Int Arch Otorhinolaryngol. 2016;20:344–52. doi: 10.1055/s-0036-1572528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Silva CN, Ribeiro KM, Freitas RV, Ferreira LM, Guerra RO. Vertiginous Symptoms and Objective Measures of Postural Balance in Elderly People with Benign Paroxysmal Positional Vertigo Submitted to the Epley Maneuver. Int Arch Otorhinolaryngol. 2016;20:61–8. doi: 10.1055/s-0035-1565915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gamiz MJ, Lopez-Escamez JA. Health-related quality of life in patients over sixty years old with benign paroxysmal positional vertigo. Gerontology. 2004;50:82–6. doi: 10.1159/000075558. [DOI] [PubMed] [Google Scholar]
- 27.van der Zaag-Loonen HJ, van Leeuwen RB, Bruintjes TD, van Munster BC. Prevalence of unrecognized benign paroxysmal positional vertigo in older patients. Eur Arch Otorhinolaryngol. 2015;272:1521–4. doi: 10.1007/s00405-014-3409-4. [DOI] [PubMed] [Google Scholar]
- 28.Huebner AC, Lytle SR, Doettl SM, Plyler PN, Thelin JT. Treatment of objective and subjective benign paroxysmal positional vertigo. J Am Acad Audiol. 2013;24:600–6. doi: 10.3766/jaaa.24.7.8. [DOI] [PubMed] [Google Scholar]
- 29.Tirelli G, D’Orlando E, Giacomarra V, Russolo M. Benign positional vertigo without detectable nystagmus. Laryngoscope. 2001;111:1053–6. doi: 10.1097/00005537-200106000-00022. [DOI] [PubMed] [Google Scholar]
- 30.Balatsouras DG, Korres SG. Subjective benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2012;146:98–103. doi: 10.1177/0194599811425158. [DOI] [PubMed] [Google Scholar]
- 31.von Brevern M, Seelig T, Radtke A, Tiel-Wilck K, Neuhauser H, Lempert T. Short-term efficacy of Epley’s manoeuvre: a double-blind randomised trial. J Neurol Neurosurg Psychiatry. 2006;77:980–2. doi: 10.1136/jnnp.2005.085894. [DOI] [PMC free article] [PubMed] [Google Scholar]