Abstract
OBJECTIVES
Since its introduction in 2002, the staging system for congenital cholesteatoma, as defined by Potsic, has been used widely owing to its simplicity and predictability. The aim of the present study was to analyze the clinical characteristics and surgical treatment outcomes of congenital cholesteatoma and to correlate them with postoperative recurrence.
MATERIALS and METHODS
A retrospective chart review was performed for 38 patients who were diagnosed with congenital cholesteatoma and who underwent surgical resection between August 2007 and November 2014 at the Department of Otorhinolaryngology of our hospital.
RESULTS
The mean age of the patients was 7.9±8.2 years, and the number of males and females was 20 and 18, respectively. The mean follow-up period was 30±26 months. Of the 38 patients, 9 (24%) had residual or recurrent cholesteatoma during follow-up examination after primary surgery. The results showed that the size (≥4 mm) of the lesion was significantly correlated with residual or recurrent disease (p=0.026). The disease extent (single vs. multiple quadrant involvement), type (closed vs. open type), and stage; applied surgical method (with mastoidectomy vs. without mastoidectomy); and preoperative hearing level (normal vs. abnormal) were not significantly correlated with residual or recurrent disease.
CONCLUSION
The disease extent, type, and stage; applied surgical methods; and preoperative hearing level were not significantly correlated with residual or recurrent disease. The size (≥4 mm) of congenital cholesteatoma was significantly correlated with residual or recurrent disease.
Keywords: Congenital cholesteatoma, stage, size, treatment
INTRODUCTION
The diagnostic criteria for congenital cholesteatoma include the presence of a pearly white mass medial to an intact tympanic membrane, with normal pars tensa and pars flaccida, and no history of otorrhea, tympanic membrane perforation, or previous otologic procedure [1].
The staging system for congenital cholesteatoma was defined by Potsic et al. [2] as follows: stage I, single quadrant: no ossicular involvement or mastoid extension; stage II, multiple quadrants: no ossicular involvement or mastoid extension; stage III, ossicular involvement: with erosion of ossicles, requiring surgical removal for the eradication of disease, without mastoid extension; and stage IV, with mastoid extension (regardless of other findings). Since its introduction in 2002, this staging system has been used widely owing to its simplicity and predictability [3–6].
Several studies have identified factors affecting the recurrence of congenital cholesteatoma; it has been demonstrated that the recurrence rate is associated with the initial stage of disease and the involvement of ossicles, among other factors [3, 7–9]. In contrast, there is relatively less information in the literature regarding the size of congenital cholesteatoma.
The aim of the present study was to analyze the clinical characteristics and surgical treatment outcome of congenital cholesteatoma and to correlate them with postoperative recurrence, with a review of the relevant literature.
MATERIALS AND METHODS
A retrospective chart review was performed for 38 patients who were diagnosed with congenital cholesteatoma and who underwent surgical resection between August 2007 and November 2014 at the Department of Otorhinolaryngology of our hospital.
The present study was approved by the appropriate institutional review board of our hospital (2017AS0020).
In the present study, data of 38 patients who underwent surgical removal of congenital cholesteatoma, which was diagnosed in accordance with the widely used criteria described by Potsic et al. [6], were analyzed.
The medical records of the patients, including data regarding demographic characteristics, brief history, otological examination findings, preoperative radiological findings on temporal bone computed tomography (TBCT), preoperative hearing test results, and type of surgery, as well as follow-up records, including information on postoperative hearing test results and whether staged or second operation was performed, were reviewed retrospectively.
The location, size, type, and stage of congenital cholesteatoma were used to investigate the clinical characteristics of congenital cholesteatoma. Preoperative size of the lesion was measured on preoperative TBCT of the patients, and postoperative size was measured as the major axis of the specimen of congenital cholesteatoma acquired during surgery.
Furthermore, postoperative recurrence rate was assessed according to the above findings and the type of surgery performed.
Statistical Analysis
Fisher’s exact test was used to confirm the statistically significant association between various factors. Statistical analysis was performed using SPSS version 20.0 statistical software (SPSS Inc., Chicago, IL, USA). A p value ≤0.05 was considered to be statistically significant.
RESULTS
A total of 38 patients who underwent surgical removal of congenital cholesteatoma between August 2007 and November 2014 were enrolled in the study.
The mean age of the patients was 7.9±8.2 years, and the male-to-female ratio was 20:18. The average follow-up duration after primary surgery was 30±26 (3–88) months. The average cholesteatoma size on preoperative TBCT was 4.1±2.2 mm, and the average size intraoperatively was recorded as 4.6±4.3 mm. There was no significant difference between the size of the cholesteatoma estimated by TBCT and that measured during surgery.
The number of patients with single quadrant involvement was 27 (71%), and the number of patients with multiple quadrant involvement was 11 (29%).
The distribution of patients according to the stage of congenital cholesteatoma was as follows: 16 patients had stage I cholesteatoma, 4 patients had stage II cholesteatoma, 11 patients had stage III cholesteatoma, and seven patients had stage IV cholesteatoma. The most frequently involved single quadrant was the anterior superior quadrant. The rate of residual or recurrent disease according to stage was as follows: 1 out of 16 patients at stage I (6%), 2 out of 4 patients at stage II (50%), 4 out of 11 patients at stage III (36%), and 2 out of 7 patients at stage IV (29%). Detailed data for each stage are given in Table 1.
Table 1.
Characteristics of congenital cholesteatoma according to stage
| Stage | No. of patients | Mean age (year) | Location | Type | Residual or recurrent |
|---|---|---|---|---|---|
| I | 16 | 3.7±2.9 | ASQ 11, PSQ 4, AIQ 1 | Closed 15, open 1 | 1 (6%) |
| II | 4 | 6.8±4.3 | ASQ+AIQ 2, PSQ+PIQ 1, AIQ+PIQ 1 | Closed 2, open 2 | 2 (50%) |
| III | 11 | 9.6±6.5 | ASQ 1, PSQ 6, PIQ 1, PSQ+PIQ 1, PSQ+AIQ+PIQ 1, all 1 | Closed 2, open 9 | 4 (36%) |
| IV | 7 | 11.6±5.8 | ASQ 1, PSQ 1, PIQ 1, PSQ+PIQ 1, ASQ+PSQ+PIQ 1, all 2 | Open 7 | 2 (29%) |
The average age and the ratio of open-type cholesteatoma are positively correlated with the stage.
ASQ: anterior superior quadrant; PSQ: posterior superior quadrant; AIQ: anterior inferior quadrant; PIQ: posterior inferior quadrant
Clinical stage tends to be higher in older patients, and the proportion of open-type cholesteatoma was increased in higher stages. The rate of residual or recurrent disease was significantly higher in higher stages than in stage I. The mean follow-up periods were 13 months in stage 1 patients and 54 months in stage 4 patients. The higher was the stage, the longer was the follow-up period.
The mean threshold of air conduction in the preoperative hearing test was as follows: 8.0±6.2 dB at stage I, 33.5±14.5 dB at stage II, 34.8±8.9 dB at stage III, and 60.3±12.4 dB at stage IV (Table 2). Worse thresholds were recorded in cases with higher stages.
Table 2.
ABR threshold and results of PTA according to the stage of congenital cholesteatoma
| Stage | ABR threshold | PTA |
|---|---|---|
| I | 21.0±1.6 dB | BC: 2.8±0.5 dB, AC: 8.0±6.2 dB |
| II | 30.0 dB | BC: 2.0±0.7 dB, AC: 33.5±14.5 dB |
| III | 30.0 dB | BC: 5.5±3.8 dB, AC: 34.8±8.9 dB |
| IV | N/A | BC: 22.4±12.1 dB, AC: 60.3±12.4 dB |
ABR: auditory brainstem response; PTA: pure tone audiometry; N/A: not available; BC: bone conduction; AC: air conduction
ABR data were not available for stage 4 patients.
Of the 38 patients, 28 (74%) underwent removal of cholesteatoma without mastoidectomy, and 10 (25%) underwent mastoidectomy with removal of cholesteatoma (Table 3).
Table 3.
Surgical techniques used for congenital cholesteatoma removal according to stage
| Stage | Cholesteatoma removal | Cholesteatoma removal+tympanoplasty (ossiculoplasty) | Cholesteatoma removal+mastoidectomy | Mastoidectomy+tympanoplasty (ossiculoplasty) |
|---|---|---|---|---|
| I | 11 | 4 | 1 | 0 |
| II | 2 | 2 | 0 | 0 |
| III | 2 | 7 | 0 | 2 |
| IV | 0 | 0 | 0 | 7 |
Nine (24%) patients had residual or recurrent cholesteatoma during follow-up examination after primary surgery. A higher recurrence rate was observed in patients with multiple quadrant involvement (46%, n=5/11) than in those with single quadrant involvement (15%, n=4/27), but there was no statistical correlation between the two groups (p=0.088) (Figure 1a).
Figure 1. a, b.
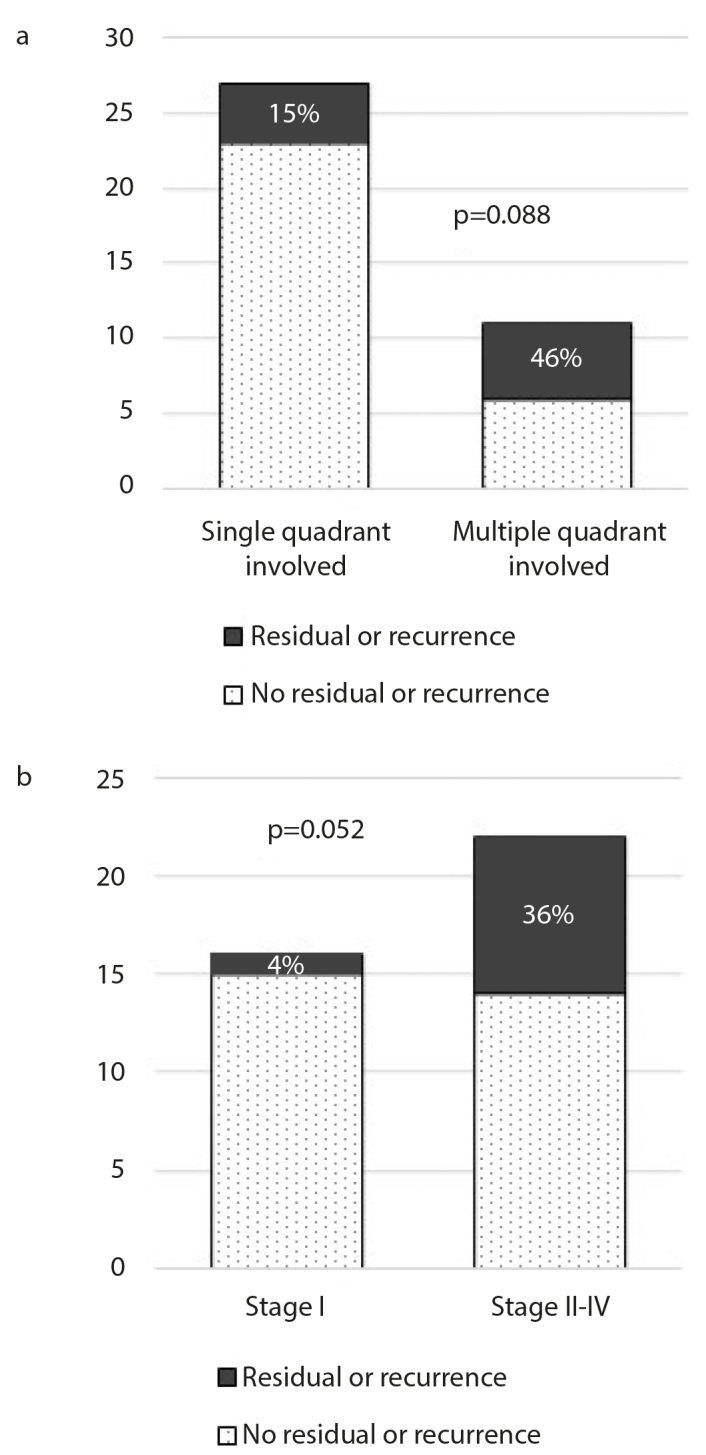
The recurrence rate of congenital cholesteatoma according to the number of involved quadrants (a) and stage (b).
A higher recurrence rate was observed in patients with stage I cholesteatoma (36%, n=8/22) than in those with higher stage cholesteatoma (4%, n=1/16), but there was no statistical correlation between the two groups (p=0.052) (Figure 1b).
A size ≥4 mm (38%, n=8/21) was more significantly associated with residual or recurrent disease than a size <4 mm (6%, n=1/17) (p=0.026) (Figure 2a). The size of the cholesteatoma was measured on preoperative TBCT.
Figure 2. a, b.
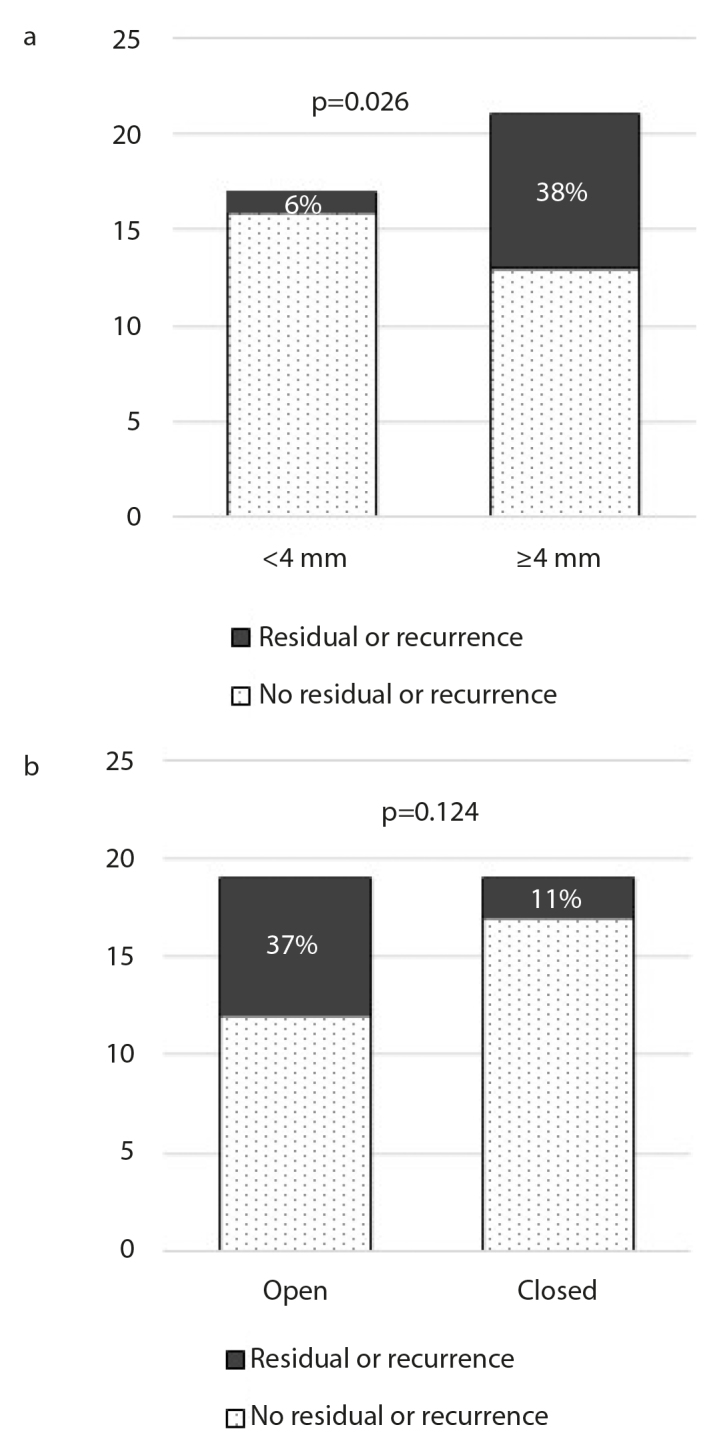
The recurrence rate of congenital cholesteatoma according to size (a) and type (b). The size of the cholesteatoma was measured on preoperative temporal bone computed tomography.
A higher recurrence rate was observed in patients with open-type cholesteatoma (37%, n=7/19) than in those with closed-type cholesteatoma (11%, n=2/19), but there was no statistical correlation between the two groups (p=0.124) (Figure 2b).
In the present study, the type of surgical technique was not significantly correlated with recurrence rate (cholesteatoma removal without mastoidectomy (21%, n=6/28) vs. mastoidectomy (30%, n=3/10)) (p=0.673) (Figure 3a).
Figure 3. a, b.
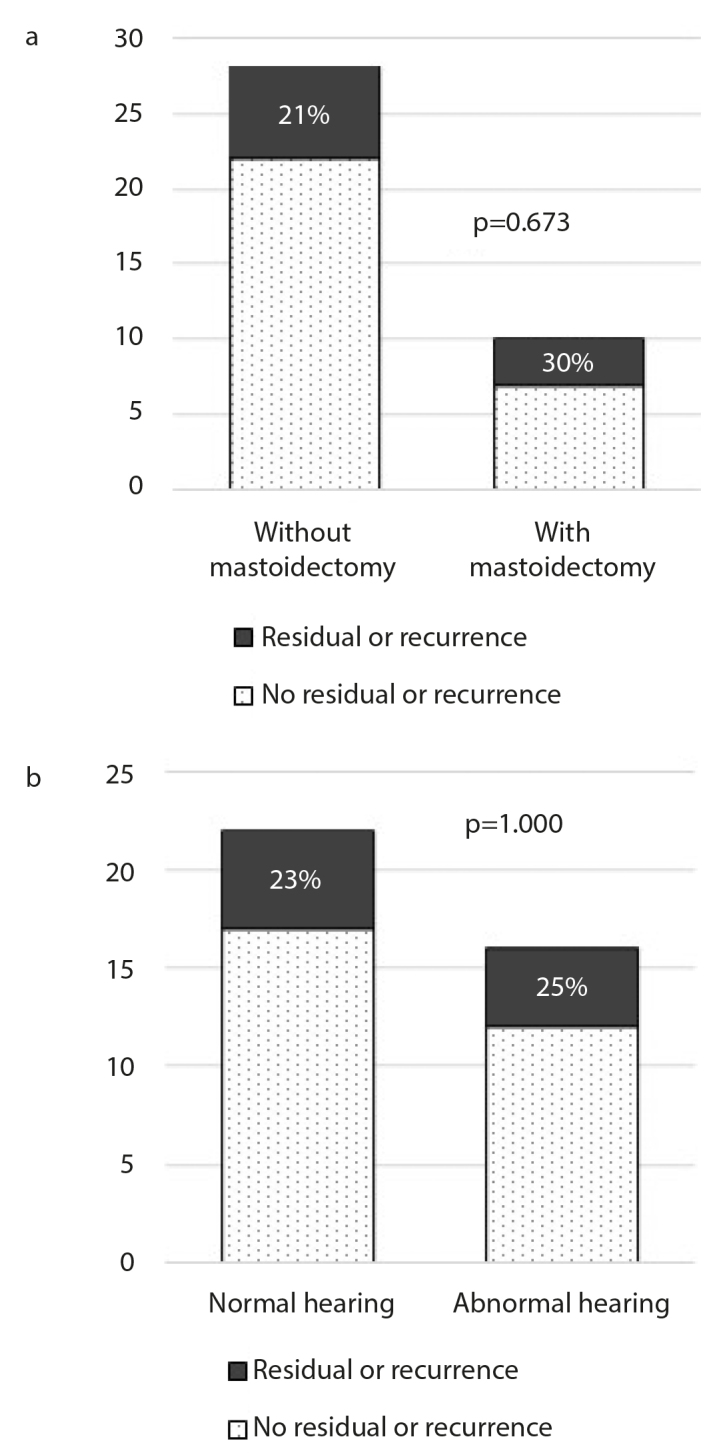
The recurrence rate of congenital cholesteatoma according to the applied surgical technique (a) and preoperative hearing level (b).
There was no statistical difference in the rate of residual or recurrent disease between the group with normal preoperative hearing (23%, n=5/22) and the group with abnormal hearing (25%, n=4/16) (p=1.00) (Figure 3b).
DISCUSSION
In the present study, the recurrence rate was 24%, which was not significantly different from that reported in previous studies [3, 4, 10–13]. The rate of occurrence of the open-type cholesteatoma tended to be increased in higher stages, and although not statistically significant, the recurrence rate in higher stages tended to be higher, which is in agreement with the findings of existing researches.
The recurrence rate was significantly higher when the size of the cholesteatoma was >4 mm. As the size of the cholesteatoma is not included in the staging system as devised by Potsic, and few studies have been conducted on the relationship between the recurrence rate and the size of the cholesteatoma, there might be scope for improvement of the staging system, and results from a study with a sample size larger than ours may be useful in this regard. Since the results of the size analysis of congenital cholesteatoma had not been studied earlier, in the current study, the recurrence rate was analyzed according to size, and it was significantly higher for lesions ≥4 mm.
Although not statistically significant, the recurrence rate was higher in open-type cholesteatoma (37%, n=7/19) than in closed-type cholesteatoma; this result supports the suggestion by McGil et al. [14] that a second-look operation should be performed in cases with open-type cholesteatoma and the suggestion by Kim et al. [8] that the recurrence rate is higher in cases with open-type cholesteatoma [15].
In the present study, the surgical technique used was categorized according to whether mastoidectomy was performed or if only congenital cholesteatoma removal was performed, but there was no significant difference in the recurrence rate between patients who underwent these two procedures; this finding is in agreement with the results reported by Kim et al. [8].
There was no statistically significant difference in the rates of residual or recurrent disease between the group with normal preoperative hearing and the group with abnormal hearing. Considering that the hearing threshold becomes worse when the stage is higher, it is an unexpected result, and this may be because at higher stages, the disease recurred at similar rates in the group with normal hearing, as well as the group with abnormal hearing.
Since its introduction in 2002, the staging system for congenital cholesteatoma as described by Potsic et al. has been used widely owing to its simplicity and predictability. Several follow-up studies have shown a correlation between the stage of congenital cholesteatoma and the rate of residual or recurrent disease [3, 4]. Our goal was to identify additional factors that are significantly associated with the occurrence of residual disease and to contribute to the improvement of the staging system for congenital cholesteatoma.
With regard to the studies on the identification of factors affecting the recurrence rate of congenital cholesteatoma, Lazard et al. [7] reported that there is a tendency for more frequent recurrence in cases undergoing atticotomy and cases with stapes destruction. Further, Kim et al. [8] contended that a second-look operation should be performed in cases with open-type cholesteatoma, advanced-stage cholesteatoma, or supra-structure erosion. Stapleton et al. [3] revealed that the recurrence rate is affected by the extent of the initial disease, degree of ossicular erosion, and need for ossicular removal. Additionally, Yoo et al. [9] suggested that longer duration of symptoms, poor mastoid pneumatization, older age, and advanced cholesteatoma also affect the recurrence of congenital cholesteatoma.
In the present study, only size was found to be a statistically significant factor associated with the recurrence of congenital cholesteatoma. The tendency of other factors evaluated was similar to that noted in previous studies, but none of those factors showed statistical significance. Currently, Potsic’s staging system does not include size, and including the measurement of the size on preoperative TBCT in the existing staging system may help to predict the recurrence rate more easily.
CONCLUSION
The size (≥4 mm) of congenital cholesteatoma was significantly correlated with residual or recurrent disease. The disease extent, type, and stage; applied surgical methods; and preoperative hearing level were not significantly correlated with residual or recurrent disease.
Footnotes
This study was presented at the 21st Combined Congress of Otorhinolaryngology-Head and Neck Surgery, October 23, 2015, Gunsan City, Republic of Korea.
Ethics Committee Approval: Ethics committee approval was received for this study from Korea University Ansan Hospital (2017AS0020).
Informed Consent: Informed consent is not necessary due to the retrospective nature of this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - J.C.; Design - I.S.S., W.G.H., M.H.Y., J.C.; Supervision - Y.C.R., J.C.; Resources - I.S.S., W.G.H., K.J.N.; Materials - I.S.S., W.G.H., K.J.N.; Data Collection and/or Processing - I.S.S., W.G.H.; Analysis and/or Interpretation - I.S.S., W.G.H., K.H.L., K.J.N., J.C.; Literature Search - I.S.S., Y.C.R.; Writing the Manuscript - I.S.S., W.G.H.; Critical Review - I.S.S., J.C.
Conflict of Interest: The authors declare that they have no conflict of interest.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Levenson MJ, Michaels L, Parisier SC. Congenital cholesteatomas of the middle ear in children: origin and management. Otolaryngol Clin North Am. 1989;22:941–54. [PubMed] [Google Scholar]
- 2.Potsic WP, Samadi DS, Marsh RR, Wetmore RF. A staging system for congenital cholesteatoma. Arch Otolaryngol Head Neck Surg. 2002;128:1009–12. doi: 10.1001/archotol.128.9.1009. [DOI] [PubMed] [Google Scholar]
- 3.Stapleton AL, Egloff AM, Yellon RF. Congenital cholesteatoma: predictors for residual disease and hearing outcomes. Arch Otolaryngol Head Neck Surg. 2012;138:280–5. doi: 10.1001/archoto.2011.1422. [DOI] [PubMed] [Google Scholar]
- 4.Yamatodani T, Mizuta K, Hosokawa K, Takizawa Y, Sugiyama K, Nakanishi H, et al. Congenital middle ear cholesteatoma: experience from 26 surgical cases. Ann Otol Rhinol Laryngol. 2013;122:316–21. doi: 10.1177/000348941312200505. [DOI] [PubMed] [Google Scholar]
- 5.Takagi T, Gyo K, Hakuba N, Hyodo J, Hato N. Clinical features, presenting symptoms, and surgical results of congenital cholesteatoma based on Potsic’s staging system. Acta Otolaryngol. 2014;134:462–7. doi: 10.3109/00016489.2013.875218. [DOI] [PubMed] [Google Scholar]
- 6.Potsic WP, Korman SB, Samadi DS, Wetmore RF. Congenital cholesteatoma: 20 years’ experience at The Children’s Hospital of Philadelphia. Otolaryngol Head Neck Surg. 2002;126:409–14. doi: 10.1067/mhn.2002.123446. [DOI] [PubMed] [Google Scholar]
- 7.Lazard DS, Roger G, Denoyelle F, Chauvin P, Garabédian EN. Congenital cholesteatoma: risk factors for residual disease and retraction pockets--a report on 117 cases. Laryngoscope. 2007;117:634–7. doi: 10.1097/mlg.0b013e318030ac8c. [DOI] [PubMed] [Google Scholar]
- 8.Kim DK, Kim HM, Suh MW, Lee JH, Oh SH, Kim CS, et al. Analysis of Risk Factors for the Occurrence of Residual Cholesteatoma after Congenital Cholesteatoma Surgery. Korean J Otolaryngol-Head Neck Surg. 2008;51:120–4. doi: 10.1016/j.otohns.2008.04.028. [DOI] [Google Scholar]
- 9.Yoo SW, Kwon SY, Kim HJ. Risk Factors of Post-Operative Recidivism in Congenital Cholesteatoma of the Middle Ear. Korean J Otolaryngol-Head Neck Surg. 2014;57:664–70. doi: 10.3342/kjorl-hns.2014.57.10.664. [DOI] [Google Scholar]
- 10.Friedberg J. Congenital cholesteatoma. Laryngoscope. 1994;104:1–24. doi: 10.1288/00005537-199403001-00001. [DOI] [PubMed] [Google Scholar]
- 11.Levenson MJ, Parisier SC, Chute P, Wenig S, Juarbe C. A review of twenty congenital cholesteatomas of the middle ear in children. Otolaryngol Head Neck Surg. 1986;94:560–7. doi: 10.1177/019459988609400605. [DOI] [PubMed] [Google Scholar]
- 12.Kojima H, Tanaka Y, Shiwa M, Sakurai Y, Moriyama H. Congenital cholesteatoma clinical features and surgical results. Am J Otolaryngol. 2006;27:299–305. doi: 10.1016/j.amjoto.2005.11.016. [DOI] [PubMed] [Google Scholar]
- 13.Lee SH, Jang JH, Lee D, Lee HR, Lee KY. Surgical outcomes of early congenital cholesteatoma: minimally invasive transcanal approach. Laryngoscope. 2014;124:755–9. doi: 10.1002/lary.24313. [DOI] [PubMed] [Google Scholar]
- 14.Bacciu A, Di Lella F, Pasanisi E, Gambardella I, Saccardi MS, Bacciu S, et al. Open vs closed type congenital cholesteatoma of the middle ear: two distinct entities or two aspects of the same phenomenon? Int J Pediatr Otorhinolaryngol. 2014;78:2205–9. doi: 10.1016/j.ijporl.2014.10.014. [DOI] [PubMed] [Google Scholar]
- 15.McGil TJ, Merchant S, Healy GB, Friedman EM. Congenital cholesteatoma of the middle ear in children: a clinical and histopathological report. Laryngoscope. 1991;101:606–13. doi: 10.1288/00005537-199106000-00006. [DOI] [PubMed] [Google Scholar]


