Abstract
Objective:
To describe trends in prevalent and incident stimulant prescribing between 2008 and 2017 in California.
Method:
Statewide trends were estimated by age and sex category for prevalent (any) and incident (no prescriptions in the preceding two years) stimulant prescribing while adjusting for area-level covariates.
Results:
Prevalent prescribing rates increased by 126%, while incident prescribing increased 23%. Patients aged 25 to 44 years experienced over 200% increases in prevalent prescribing and 34% to 55% increases in incident prescribing. Among patients older than 25, women had consistently higher prescribing rates than men. ZIP code tabulation areas with the largest minority populations had the lowest baseline prescribing rates but experienced the greatest annual prescription rate increases.
Conclusion:
Adult stimulant prescribing increased substantially for early working aged adults. Prescription rates were greater for women than men.
Introduction
Prescription stimulants are the most common treatment for adult attention deficit hyperactivity disorder (ADHD), which typically manifests in childhood and persists through adulthood. Untreated ADHD is linked to significant problems in academic, social, and family settings (National Institute of Mental Health, 2016), and is among the most common of all adult mental disorders. A 2006 national survey reported an adult ADHD prevalence of 4.4% (Kessler et al., 2006), and analysis of healthcare utilization data indicates steady increases in prevalence from 1999–2010 (Oehrlein, Burcu, Safer, & Zito, 2016). Changes to the diagnostic criteria for ADHD in the DSM-5 also contributed to an increase in ADHD diagnoses among young adults (Matte et al., 2015).
Prescription stimulants are the mainstay of treatment for ADHD. Most stimulants prescribed to adults are for ADHD, though they are also prescribed for obesity, narcolepsy, depression, and cognitive impairment (Olfson, Blanco, Wang, & Greenhill, 2013; Safer, 2016). Analysis of the 2006–2009 National Ambulatory Medical Care Survey revealed that 67% of all office-based visits that included a stimulant prescription were associated with an ADHD diagnosis (Olfson et al., 2013). Thus, increases in ADHD prevalence have been accompanied by increased stimulant prescribing, from a reported 10 million prescriptions in 1993 to 58 million in 2014 (Safer, 2016). Two recent longitudinal studies show increases in stimulant prescribing but were limited to analysis of drug weights (Piper et al., 2018) and claims from a single commercial insurer (Burcu, Zito, Metcalfe, Underwood, & Safer, 2016). No prior studies have examined trends in first-time stimulant prescriptions.
In this study, we used data from California’s prescription drug monitoring program to identify annual age- and sex-specific trends in prevalent and incident stimulant prescribing to adults, adjusting for key demographic factors at the ZIP code tabulation area (ZCTA) level. Secondary analysis utilized these models to further examine prescribing rates and longitudinal trends by the aforementioned ZCTA-level demographics, specifically racial composition (Friedman et al., 2019; Kessler et al., 2005; Oehrlein et al., 2016), socioeconomic status (SES) (Friedman et al., 2019), and rurality (McDonald & Jalbert, 2013). In addition to helping understand trends in ADHD diagnoses, improved characterization of increased stimulant prescribing is important due to stimulants’ serious adverse effects; for example, stimulant-related myocardial infarction and cardiomyopathy appear to be increasing among adults (Lakhan & Kirchgessner, 2012). Finally, prescribing trends have implications for stimulant-related misuse, abuse and overdose. Adult emergency department visits associated with prescription stimulant misuse increased by 156% between 2006 and 2011 (Chen et al., 2016), while overdose deaths involving psychostimulants increased 33.3% from 2015 to 2016 (Seth, Scholl, Rudd, & Bacon, 2018), with increases observed across all sex-specific age (Seth et al., 2018) and racial groups (Shiels, Freedman, Thomas, & Berrington de Gonzalez, 2018). The predominant source of prescription stimulant misuse is diversion of legally prescribed medications to friends and family (Cassidy et al., 2015), so identifying populations with the greatest increases in stimulant prescribing can help to identify populations that are high-priority targets for efforts to prevent, diagnose and treat stimulant use disorders and to prevent stimulant-related overdose.
Methods
Prescription Data
Data on prescribed stimulants and patient information were obtained through California’s prescription drug monitoring program, the Controlled Substance, Utilization, Review and Evaluation System (CURES). CURES includes all outpatient Schedule II through IV controlled substance prescriptions dispensed in the state. We identified prescription stimulants by cross-referencing national drug codes in CURES against widely available prescription drug compendia. All ambiguous cases were manually reviewed and classified by a clinical pharmacist with expertise in controlled substances (see Supplementary Table 1 for the list of National Drug Codes utilized for this analysis). Prescription stimulant records between the years 2008 and 2017, for patients aged 15 years or older, were utilized for this analysis. Patient information includes patient age, sex, and ZIP code. Patient ZIP codes were converted to ZCTAs using a U.S. Census relationship file (United States Census Bureau, 2014). Prescription data contained a unique encrypted patient ID, which allowed us to link prescriptions to individual patients over time.
Population and Demographic Data
Statewide population estimates by sex and age were taken from the U.S. Census Bureau’s Population Estimates program (United States Census Bureau Population Estimates Program, 2018). ZCTA population estimates by sex and age were obtained from 5-year American Community Survey (ACS) data (United States Census Bureau, 2018). These data were used as point estimates for the mid-year of each ACS 5-year period (e.g., 2012 as the mid-year from the 2010–2014 ACS dataset). A best-fit line, using an ordinary least squares approach, was constructed between these estimates, and the resulting parameters used to extrapolate the population totals for the remaining non-midpoint years (2008, 2016, and 2017). Annual ZCTA estimates for each age group, by sex, were then multiplied by the ratio of the statewide population estimate, from the U.S. Census Bureau’s Population Estimates program, to the sum of all California ZCTA estimates, as derived from ACS data, for the given year.
Demographics at the ZCTA level included measures of SES, race, and rurality. SES and racial demographics from the 2013–2017 ACS were used for analyses. An index based on the Yost criteria was constructed using principle component analysis of rank-transformed data to estimate SES (Yost, Perkins, Cohen, Morris, & Wright, 2001). The following variables were used to construct the index: median household income, proportion of residents unemployed, proportion of households below 150% of the poverty threshold, and proportion of residents employed in one of the following industries: service, natural resource, construction, maintenance, production, transportation, or material moving. Median rent and household value were excluded due to large amounts of missing data. Racial composition was measured by calculating the proportion of white residents for each ZCTA. Both SES and proportion-white were categorized into quintiles. ZCTA rural status was determined from the 2010 Rural Urban Commuting Area Codes (United States Department of Agriculture, 2016). Codes were condensed into a binary “metropolitan” and “non-metropolitan” classification for each ZCTA.
Statistical Analysis
We first examined unadjusted statewide longitudinal prevalent and incident prescribing rates by age group (15–24, 25–34, 35–44, 45–54, 55–64, ≥65) and sex. We defined incident prescriptions as prescriptions to patients with no other stimulant prescriptions in the preceding two years (730 days). Multivariable analysis utilized Poisson regression models with robust standard errors to determine age and sex-specific longitudinal trends, while adjusting for covariates at the ZCTA level. Separate models for prevalent prescriptions, from 2008 to 2017, and incident prescriptions, from 2010 to 2017, were constructed. Counts were offset by log-transformed ZCTA population totals to allow for estimation of rate ratios (RR) and 95% confidence intervals (95% CI). Models utilized generalized estimated equations to account for within-ZCTA repeated measures. Interaction terms between age, year, and sex were included in the model to estimate the effect of year on prescription rates across sex and age categories. Adjusted multivariable models were further utilized to examine stimulant prescribing rates and longitudinal trends by ZCTA-level demographics, such as racial composition, SES, and rurality. Analysis was conducted in SAS version 9.4 (SAS Institute, Cary NC); PROC GENMOD was used to perform the adjusted analyses. This study was approved by the University of California Davis Institutional Review Board and the California Committee for the Protection of Human Subjects.
Results
Analysis of 26,394,510 stimulants prescribed to 2,629,033 patients in California, of whom 60.0% were female, with an overall mean (SD) age of 38.8 (16.0) years, revealed increases in both prevalent and incident prescribing rates over time. Between 2008 and 2017, prevalent stimulant prescribing increased by 125.9% (52.5 to 118.6 per thousand) and the proportion of the state population prescribed any stimulants increased from 1.36% to 2.41% (Supplementary Table 2). Incident prescribing increased by 22.8% (7.9 to 9.7 per thousand) between 2010 and 2017.
Prescription rates increased from 2008 to 2017 for all age and sex categories, with the greatest increase among patients between 25 and 44 years of age (Figure 1). Among patients 25 to 34 years old, prescriptions increased 267.5% (32.5 to 119.2 per thousand) for males and 220.0% (62.4 to 199.7 per thousand) for females. Among patients 35 to 44 years old, prescriptions increased 203.8% (32.6 to 99.1 per thousand) for males and 211.7% (68.2 to 212.5 per thousand) for females.
Figure 1:
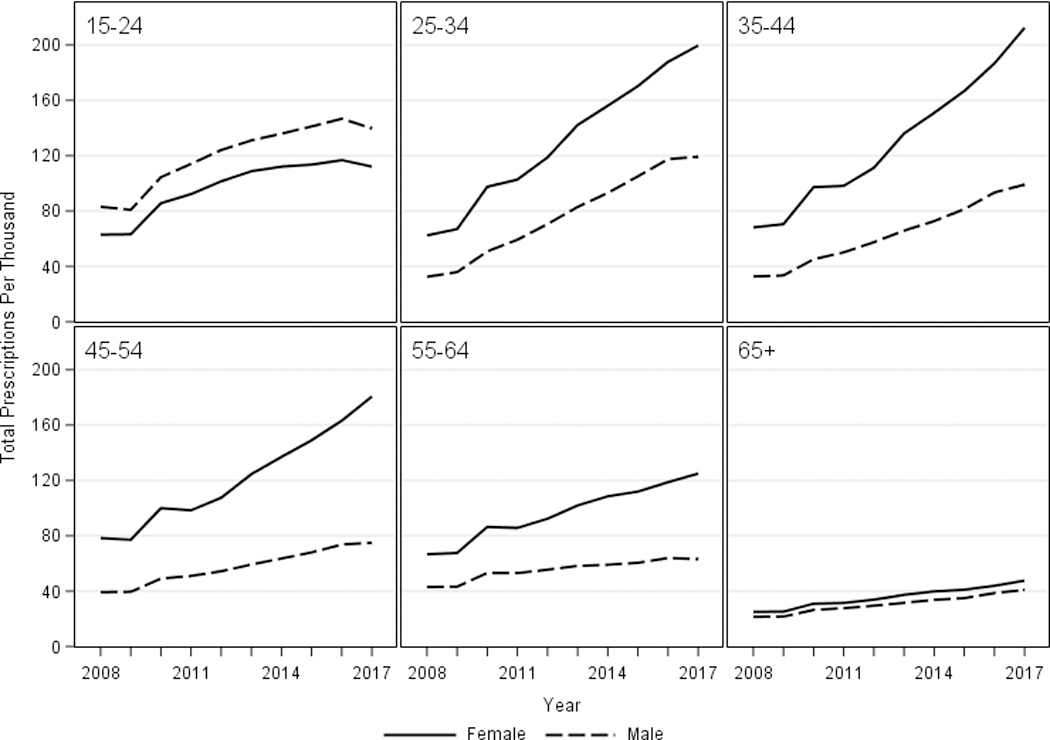
Unadjusted prevalent stimulant prescribing rates, per 1,000 California residents, between 2008 and 2017 by age group and sex
Prescription data are from the Controlled Substance, Utilization, Review and Evaluation System, California’s prescription drug monitoring program. Statewide population totals are from the United States Census Bureau’s Population Estimates program.
Increases in incident stimulant prescribing were mostly limited to 25 to 44 year-old male patients and 25 to 54 year-old female patients (Figure 2). Baseline incident prescribing rates for males were highest for those aged 15 to 24 years, but increased only 4.7% between 2010 and 2017 (from 11.2 to 11.7 per thousand). Meanwhile, the greatest increases for male incident prescribing occurred in the 25 to 34 and 35 to 44 age groups at 55.3% (5.9 to 9.2 per thousand) and 45.5% (4.6 to 6.7 per thousand), respectively. Female patients aged 35 to 44 years had the highest incident prescribing rates in both 2010 (12.8 per thousand) and 2017 (19.1 per thousand). They also experienced the greatest increase in incident prescribing among all female age groups (49.5%); notable increases in incident prescribing also occurred for female patients aged 25 to 34 (34.2%: 14.8 to 19.9 per thousand) and 45 to 54 years (43.0%: 10.3 to 14.7 per thousand).
Figure 2:
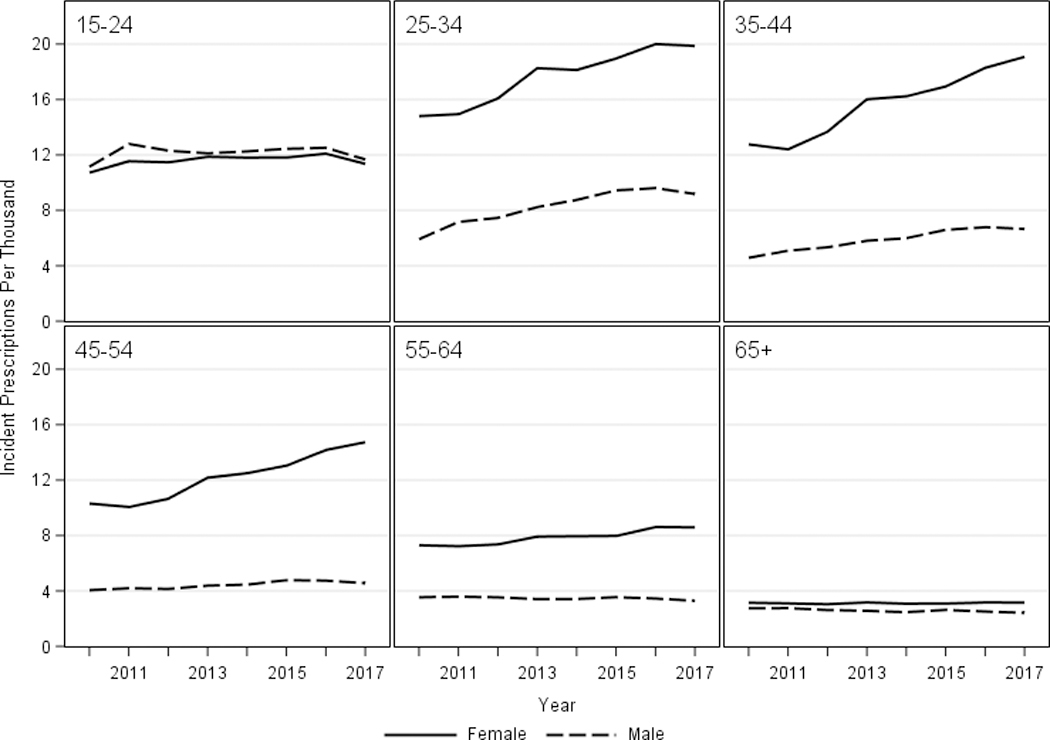
Unadjusted incident stimulant prescribing rates, per 1,000 California residents, between 2010 and 2017 by age group and sex
Incident prescriptions are defined as prescriptions to patients with no other stimulant prescriptions in the preceding two years (730 days). Prescription data are from the Controlled Substance, Utilization, Review and Evaluation System, California’s prescription drug monitoring program. Statewide population totals are from the United States Census Bureau’s Population Estimates program.
Results for prevalent prescribing were similar after adjusting for ZCTA-level demographics. Adjusted overall prescribing still increased for every age and sex category, with the highest rates of increase for males and females aged 25 to 44 (Table 1). Prescribing rates increased an average of 15.1% per year (95% CI = [14.7, 15.5]) for males aged 25 to 34, 13.5% per year (95% CI = [13.2, 13.9]) for males aged 35 to 44 years, 13.2% per year (95% CI = [12.7, 13.7]) for women aged 25 to 34, and 13.7% per year (95% CI = [13.1, 14.3]) for women aged 35–44.
Table 1.
Adjusteda analyses for the effect of year for age- and sex-specific patient categories on prevalent stimulant prescription rates – California, 2008 to 2017
| Patient Age |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 15–24 |
25–34 |
35–44 |
45–54 |
55–64 |
≥ 65 |
|||||||
| Year | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI |
| Males | ||||||||||||
| 2008 | Ref | Ref | Ref | Ref | Ref | Ref | ||||||
| 2009 | 0.97 | [0.96, 0.99] | 1.11 | [1.08, 1.13] | 1.03** | [1.01, 1.05] | 1.01† | [0.99, 1.02] | 1.01† | [0.99, 1.03] | 1.01† | [0.98, 1.03] |
| 2010 | 1.26 | [1.24, 1.28] | 1.57 | [1.53, 1.60] | 1.39 | [1.36, 1.42] | 1.26 | [1.23, 1.28] | 1.25 | [1.22, 1.28] | 1.23 | [1.19, 1.26] |
| 2011 | 1.38 | [1.35, 1.40] | 1.82 | [1.78, 1.86] | 1.54 | [1.51, 1.58] | 1.31 | [1.28, 1.34] | 1.25 | [1.22, 1.28] | 1.29 | [1.25, 1.33] |
| 2012 | 1.49 | [1.47, 1.52] | 2.17 | [2.11, 2.22] | 1.77 | [1.73, 1.82] | 1.41 | [1.37, 1.44] | 1.32 | [1.28, 1.35] | 1.36 | [1.32, 1.41] |
| 2013 | 1.58 | [1.54, 1.61] | 2.55 | [2.48, 2.62] | 2.03 | [1.98, 2.09] | 1.54 | [1.50, 1.57] | 1.39 | [1.35, 1.43] | 1.46 | [1.41, 1.51] |
| 2014 | 1.63 | [1.60, 1.67] | 2.86 | [2.78, 2.94] | 2.25 | [2.19, 2.31] | 1.65 | [1.60, 1.69] | 1.41 | [1.37, 1.45] | 1.56 | [1.50, 1.61] |
| 2015 | 1.70 | [1.66, 1.74] | 3.23 | [3.14, 3.33] | 2.51 | [2.44, 2.58] | 1.77 | [1.72, 1.81] | 1.45 | [1.41, 1.50] | 1.61 | [1.56, 1.67] |
| 2016 | 1.76 | [1.72, 1.81] | 3.61 | [3.50, 3.72] | 2.89 | [2.81, 2.97] | 1.92 | [1.87, 1.97] | 1.54 | [1.50, 1.59] | 1.77 | [1.71, 1.84] |
| 2017 | 1.68 | [1.63, 1.73] | 3.66 | [3.54, 3.79] | 3.07 | [2.98, 3.16] | 1.96 | [1.91, 2.02] | 1.53 | [1.48, 1.58] | 1.87 | [1.81, 1.94] |
| RRCb | 1.064 | [1.060, 1.067] | 1.151 | [1.147, 1.155] | 1.135 | [1.132, 1.139] | 1.081 | [1.077, 1.084] | 1.047 | [1.044, 1.051] | 1.071 | [1.067, 1.076] |
| Females | ||||||||||||
| 2008 | Ref | Ref | Ref | Ref | Ref | Ref | ||||||
| 2009 | 1.00† | [0.99, 1.02] | 1.07 | [1.06, 1.09] | 1.03 | [1.02, 1.05] | 0.99* | [0.97, 1.00] | 1.02** | [1.01, 1.04] | 1.01† | [0.98, 1.03] |
| 2010 | 1.36 | [1.34, 1.39] | 1.56 | [1.53, 1.60] | 1.43 | [1.40, 1.46] | 1.28 | [1.26, 1.30] | 1.31 | [1.28, 1.33] | 1.24 | [1.20, 1.27] |
| 2011 | 1.47 | [1.44, 1.50] | 1.64 | [1.61, 1.68] | 1.45 | [1.42, 1.48] | 1.27 | [1.24, 1.29] | 1.30 | [1.28, 1.33] | 1.25 | [1.22, 1.29] |
| 2012 | 1.61 | [1.58, 1.65] | 1.90 | [1.86, 1.95] | 1.65 | [1.61, 1.68] | 1.39 | [1.36, 1.41] | 1.41 | [1.38, 1.44] | 1.35 | [1.31, 1.39] |
| 2013 | 1.73 | [1.69, 1.77] | 2.28 | [2.22, 2.34] | 2.02 | [1.96, 2.07] | 1.61 | [1.57, 1.64] | 1.57 | [1.53, 1.60] | 1.48 | [1.43, 1.52] |
| 2014 | 1.78 | [1.73, 1.83] | 2.50 | [2.43, 2.57] | 2.24 | [2.17, 2.31] | 1.77 | [1.72, 1.82] | 1.67 | [1.63, 1.71] | 1.58 | [1.53, 1.63] |
| 2015 | 1.80 | [1.75, 1.85] | 2.72 | [2.64, 2.81] | 2.48 | [2.40, 2.56] | 1.93 | [1.88, 1.98] | 1.73 | [1.68, 1.77] | 1.63 | [1.58, 1.68] |
| 2016 | 1.85 | [1.80, 1.91] | 3.00 | [2.90, 3.11] | 2.78 | [2.68, 2.88] | 2.12 | [2.05, 2.19] | 1.84 | [1.79, 1.89] | 1.74 | [1.68, 1.79] |
| 2017 | 1.78 | [1.72, 1.84] | 3.19 | [3.07, 3.31] | 3.17 | [3.04, 3.31] | 2.35 | [2.26, 2.44] | 1.94 | [1.88, 2.00] | 1.88 | [1.82, 1.94] |
| RRCb | 1.067 | [1.063, 1.070] | 1.132 | [1.127, 1.137] | 1.137 | [1.131, 1.143] | 1.103 | [1.099, 1.108] | 1.074 | [1.070, 1.078] | 1.072 | [1.068, 1.076] |
Note. RR = rate ratio; CI = confidence interval; Ref = referent group; RRC, rate ratio change
p < 0.001 unless otherwise indicated,
p > 0.05.
0.01 < p < 0.05.
0.001 < p < 0.01.
Poisson models utilizing general estimating equations; covariates included ZCTA-level socioeconomic status quintile and proportion of white residents (both derived from the 2013–2017 American Community Survey), and rurality (metropolitan versus non-metropolitan) derived from the 2010 Rural-Urban Commuting Area codes.
Annual prescribing rate change, adjusted for aforementioned covariates and expressed as rate ratios, from 2008 to 2017 across all ZCTAs in the named category.
Similar to unadjusted results, adjusted analysis of incident prescription rates revealed substantial growth in males aged 25 to 44 years and females aged 25–54 (Table 2). Male incident prescribing increased annually by 6.1% (95% CI = [5.7, 6.5]), 5.7% (95% CI = [5.3, 6.1]), 2.5% (95% CI = [2.1, 2.9]) for patients aged 25 to 34, 35 to 44, and 45 to 54 years, respectively. Females experienced annual increases of 4.7% (95% CI = [4.1, 5.3]), 6.6% (95% CI = [6.0, 7.3]), 6.1% (95% CI = [5.6, 6.6]) for the 25 to 34, 35 to 44, and 45 to 54 age groups, respectively.
Table 2:
Adjusteda analyses for the effect of year for age- and sex-specific patient categories on incidentb stimulant prescription rates – California, 2010 to 2017
| Patient Age |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 15–24 |
25–34 |
35–44 |
45–54 |
55–64 |
≥ 65 |
|||||||
| Year | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI |
| Males | ||||||||||||
| 2010 | Ref | Ref | Ref | Ref | Ref | Ref | ||||||
| 2011 | 1.15 | [1.12, 1.18] | 1.20 | [1.17, 1.24] | 1.12 | [1.08, 1.15] | 1.03* | [1.00, 1.07] | 1.02† | [0.98, 1.06] | 1.01† | [0.97, 1.05] |
| 2012 | 1.10 | [1.08, 1.13] | 1.25 | [1.22, 1.28] | 1.17 | [1.14, 1.20] | 1.03* | [1.00, 1.06] | 1.00† | [0.97, 1.04] | 0.96* | [0.92, 0.99] |
| 2013 | 1.09 | [1.06, 1.11] | 1.38 | [1.35, 1.41] | 1.27 | [1.24, 1.31] | 1.09 | [1.06, 1.12] | 0.97† | [0.94, 1.00] | 0.92 | [0.88, 0.96] |
| 2014 | 1.10 | [1.07, 1.12] | 1.47 | [1.43, 1.50] | 1.31 | [1.28, 1.35] | 1.10 | [1.07, 1.14] | 0.98† | [0.95, 1.02] | 0.89 | [0.85, 0.92] |
| 2015 | 1.11 | [1.09, 1.14] | 1.58 | [1.54, 1.62] | 1.44 | [1.40, 1.48] | 1.19 | [1.15, 1.22] | 1.02† | [0.98, 1.05] | 0.94** | [0.90, 0.98] |
| 2016 | 1.12 | [1.09, 1.15] | 1.61 | [1.56, 1.65] | 1.49 | [1.44, 1.53] | 1.18 | [1.15, 1.22] | 0.99† | [0.96, 1.02] | 0.90 | [0.86, 0.94] |
| 2017 | 1.05** | [1.02, 1.07] | 1.54 | [1.49, 1.58] | 1.46 | [1.42, 1.50] | 1.14 | [1.11, 1.18] | 0.95** | [0.91, 0.98] | 0.87 | [0.84, 0.91] |
| RRCc | 1.002† | [0.999, 1.006] | 1.061 | [1.057, 1.065] | 1.057 | [1.053, 1.061] | 1.025 | [1.021, 1.029] | 0.995* | [0.991, 0.999] | 0.981 | [0.976, 0.986] |
| Females | ||||||||||||
| 2010 | Ref | Ref | Ref | Ref | Ref | Ref | ||||||
| 2011 | 1.08 | [1.05, 1.10] | 1.01† | [0.98, 1.03] | 0.97* | [0.95, 1.00] | 0.98† | [0.96, 1.00] | 0.99† | [0.96, 1.02] | 0.99† | [0.95, 1.02] |
| 2012 | 1.07 | [1.05, 1.09] | 1.09 | [1.06, 1.11] | 1.07 | [1.05, 1.10] | 1.04** | [1.02, 1.06] | 1.01† | [0.99, 1.04] | 0.96* | [0.92, 0.99] |
| 2013 | 1.11 | [1.08, 1.14] | 1.23 | [1.20, 1.27] | 1.26 | [1.22, 1.30] | 1.19 | [1.16, 1.22] | 1.09 | [1.06, 1.12] | 1.00† |
[0.97, 1.04] |
| 2014 | 1.10 | [1.07, 1.13] | 1.22 | [1.19, 1.26] | 1.28 | [1.24, 1.32] | 1.22 | [1.19, 1.25] | 1.10 | [1.07, 1.13] | 0.97† | [0.94, 1.00] |
| 2015 | 1.10 | [1.07, 1.14] | 1.28 | [1.23, 1.32] | 1.33 | [1.29, 1.38] | 1.27 | [1.24, 1.31] | 1.10 | [1.07, 1.13] | 0.97† | [0.94, 1.01] |
| 2016 | 1.13 | [1.09, 1.16] | 1.35 | [1.30, 1.40] | 1.44 | [1.39, 1.50] | 1.39 | [1.34, 1.44] | 1.20 | [1.16, 1.23] | 0.99† | [0.95, 1.02] |
| 2017 | 1.06** | [1.02, 1.10] | 1.34 | [1.28, 1.40] | 1.51 | [1.44, 1.57] | 1.45 | [1.39, 1.50] | 1.19 | [1.16, 1.23] | 0.99† | [0.95, 1.02] |
| RRCc | 1.008** | [1.004, 1.013] | 1.047 | [1.041, 1.053] | 1.066 | [1.060, 1.073] | 1.061 | [1.056, 1.066] | 1.029 | [1.025, 1.034] | 0.999† | [0.995, 1.004] |
Note. RR = rate ratio; CI = confidence interval; Ref = referent group; RRC, rate ratio change
p < 0.001 unless otherwise indicated,
p > 0.05.
0.01 < p < 0.05.
0.001 < p < 0.01.
Poisson models utilizing general estimating equations; covariates included ZCTA-level socioeconomic status quintile and proportion of white residents (both derived from the 2013–2017 American Community Survey), and rurality (metropolitan versus non-metropolitan) derived from the 2010 Rural-Urban Commuting Area codes.
No stimulant prescriptions in the preceding two years (730 days).
Annual prescribing rate change, adjusted for aforementioned covariates and expressed as rate ratios, from 2010 to 2017 across all ZCTAs in the named category.
Associations between ZCTA-level racial, SES, and rural characteristics and stimulant prescribing are presented in Table 3. Prescription rates in non-metropolitan ZCTAs were lower than those in metropolitan ZCTAs (RR = 0.81, 95% CI = [0.74, 0.88]). Higher SES and higher proportion-white populations were both associated with greater rates of stimulant prescribing. The quintile with the highest SES had prescribing rates 1.79 (95% CI = [1.64, 1.95]) times the rates of the lowest SES quintile. The effect of race on prescribing rates was even more pronounced. Prescriptions for patients living in ZCTAs with the highest proportion-white population were 3.86 (95% CI = [3.38, 4.42]) times as high as rates for patients living in ZCTAs with the lowest proportion-white. Longitudinal trends showed greater increases in areas with smaller prescribing rates. Adjusted annual rate increases in stimulant prescribing were greatest in the lowest proportion-white areas (RR = 1.095, 95% CI = [1.087, 1.104]) and least in the highest (RR = 1.046, 95% CI = [1.040, 1.053]); while also greater in non-metropolitan areas (RR = 1.068, 95% CI = [1.064, 1.072]) relative to metropolitan areas (RR = 1.030, 95% CI = [1.022, 1.038]). Unlike racial and rural covariates, rates increased similarly across all SES categories.
Table 3:
Analysesa of ZIP code tabulation area (ZCTA) level effects on prevalent and incident stimulant prescribing rates in California
| Variable | All Prescriptions |
Incidentb Prescriptions |
||||||
|---|---|---|---|---|---|---|---|---|
| RR | 95% CI | RRCc | 95% CI | RR | 95% CI | RRCc | 95% CI | |
| Rural Classificationd | ||||||||
| Metropolitan | Ref | 1.030 | [1.022, 1.038] | Ref | 0.968 | [0.958, 0.979] | ||
| Non-Metropolitan | 0.81 | [0.74, 0.88] | 1.068 | [1.064, 1.072] | 0.88** | [0.79, 0.97] | 1.011 | [1.006, 1.015] |
| SESe | ||||||||
| Very Low | Ref | 1.068 | [1.058, 1.079] | Ref | 1.018* | [1.004, 1.032] | ||
| Low | 1.14 | [1.06, 1.23] | 1.069 | [1.059, 1.078] | 1.02† | [0.94, 1.10] | 1.017 | [1.007, 1.027] |
| Medium | 1.22 | [1.12, 1.32] | 1.071 | [1.064, 1.079] | 1.02† | [0.94, 1.11] | 1.013** | [1.005, 1.022] |
| High | 1.39 | [1.28, 1.51] | 1.068 | [1.063, 1.074] | 1.08† | [0.99, 1.17] | 1.004† | [0.998, 1.011] |
| Very High | 1.79 | [1.64, 1.95] | 1.060 | [1.055, 1.065] | 1.20 | [1.10, 1.31] | 0.994* | [0.989, 0.999] |
| Proportion Whitee | ||||||||
| < 23.2% | Ref | 1.095 | [1.087, 1.104] | Ref | 1.042 | [1.033, 1.051] | ||
| 23.2% – 45.3% | 1.73 | [1.62, 1.85] | 1.067 | [1.061, 1.073] | 1.56 | [1.46, 1.67] | 1.008* | [1.000, 1.016] |
| 45.4% – 64.3% | 2.39 | [2.22, 2.56] | 1.062 | [1.057, 1.068] | 1.94 | [1.81, 2.08] | 1.001† | [0.995, 1.007] |
| 64.4% – 80.0% | 3.11 | [2.87, 3.37] | 1.055 | [1.050, 1.060] | 2.41 | [2.23, 2.61] | 0.987 | [0.982, 0.992] |
| > 80.0% | 3.86 | [3.38, 4.42] | 1.046 | [1.040, 1.053] | 2.81 | [2.45, 3.22] | 0.979 | [0.972, 0.986] |
Note. RR = rate ratio; CI = confidence interval; Ref = referent group; RRC = rate ratio change; SES = socioeconomic status
p < 0.001 unless otherwise indicated,
p > 0.05.
0.01 < p < 0.05.
0.001 < p < 0.01.
Poisson models utilizing general estimating equations; covariates included patient age, gender, year of data, and the three-way interaction of year, gender, and age.
No stimulant prescriptions in the preceding two years (730 days).
Annual prescribing rate change, adjusted for aforementioned covariates and expressed as rate ratios, from 2008 to 2017 (all prescriptions) or from 2010 to 2017 (incident prescriptions) across all ZCTAs in the named category.
Derived from 2010 Rural-Urban Commuting Area Codes.
Derived from 2013–2017 American Community Survey
Incident prescribing rates were positively associated with both higher SES and higher proportion-white ZCTAs. The effect of SES was significant only for the highest level ZCTAs, which had incident prescribing rates 1.20 (95% CI = [1.10, 1.31]) times those ZCTAs in the lowest SES quintile. ZCTAs with the highest proportion-white had rates 2.81 (95% CI = [2.45, 3.22]) times those ZCTAs with the lowest proportion-white.
Adjusted longitudinal trends, between 2010 and 2017, were comparable to those observed for prevalent prescriptions. ZCTAs with lower proportion-white had the greatest annual increases in incident prescribing (RR = 1.042, 95% CI = [1.033, 1.051]) with consistent and minimal changes across SES groups. Incident prescribing grew (RR = 1.011 per year, 95% CI = [1.006, 1.015]) and decreased (RR = 0.968 per year, 95% CI = [0.958, 0.979]) slightly in non-metropolitan and metropolitan areas, respectively.
Discussion
Analyses of a decade’s worth of population-based prescribing data, from a large, populous, and diverse state, found that stimulant prescribing more than doubled overall and increased for adults in all age groups. Patients aged 25 to 44 years disproportionately contributed to this increase, as prescribing rates in this age group more than tripled between 2008 and 2017. Prescribing rates were considerably higher for women than for men; however, rates of increase were generally similar for men and women. In 2008, males aged 15 to 24 had the highest prescribing rate, but by 2017, prescribing was highest among female patients aged 35 to 44.
Our analysis also revealed a 22.8% increase in first-time stimulant patients during the study period. Again, the greatest increases were among patients between 25 and 44 years of age, and ranged from 34% to 55%. From 2010 through 2017, incident prescribing rates were highest for female patients 25 to 34 years of age. To our knowledge, this is the first study to examine first-time stimulant patients and to report longitudinal trends in incident stimulant use.
The substantial increases in stimulant use among young to middle-aged adults documented in this study are likely due in large part to increases in the diagnosis and treatment of adult ADHD, which has been historically undertreated, despite evidence that the majority of children with ADHD report symptoms persisting into adulthood (Bernardi et al., 2012; Biederman, Petty, Evans, Small, & Faraone, 2010; Kessler et al., 2005). Some increases in prescribing rates may reflect the expanded use of stimulants for other conditions beyond the treatment of ADHD; a 2016 review reported a growth in stimulant treatment absent an ADHD diagnosis among non-psychiatrist physicians (Safer, 2016).
Despite increases in prescribing, the proportion of adults receiving prescription stimulants remains considerably lower than the estimated national prevalence of adult ADHD. A study of 18 to 44 year olds found an estimated national prevalence of 4.4% (Kessler et al., 2006). Our results show that in 2017, the proportion of Californians, aged 15 to 44 years old, prescribed stimulants (3.04%) was 31% lower than this estimate. This discrepancy appears solely due to male stimulant prescribing. Men (2.35%) were prescribed stimulants at less than half the reported prevalence of males diagnosed with ADHD nationwide (5.4%); while women were prescribed at a proportion (3.77%) greater than the reported national prevalence (3.2%). These differences may indicate an underutilization of stimulant pharmacotherapy to treat adult male ADHD in California.
Both prevalent and incident prescription rates were consistently higher for women than men for ages 25 and older. These differences likely reflect women, who were untreated as children, self-referring for treatment later as adults. Boys with ADHD tend to exhibit greater levels of disruptive externalizing behavior than girls with ADHD, leading to under-diagnosis and treatment of ADHD for girls relative to boys (Williamson & Johnston, 2015). Some mothers may seek treatment for themselves when they recognize they have symptoms of inattention similar to those diagnosed in their children. Additionally, women, who were undiagnosed through childhood, may experience greater difficulty managing symptoms of ADHD in their adult lives and seek treatment (Castle, Aubert, Verbrugge, Khalid, & Epstein, 2007). Though ADHD remains the primary reason for the prescription of stimulants, differences may also be partially explained by increases in prescribing absent an ADHD diagnosis (Olfson et al., 2013). Women may be more likely to receive stimulant therapy for non-ADHD diagnoses; particularly for the treatment of obesity (Ganguly et al., 2018). These findings are consistent with previous studies of adult stimulant prescribing (Burcu et al., 2016; Oehrlein et al., 2016; Olfson et al., 2013); however, our study is the first to examine these trends in a population-based data set that is not restricted by health system or payer type.
Rates of stimulant prescribing were higher in metropolitan areas and in areas with more white residents and higher overall SES. These area-level effects were most pronounced for race; ZCTAs with the greatest concentration of white residents had nearly four times the prescribing rates of ZCTAs with the smallest white populations. This result is consistent with prior studies showing substantially higher prescribing rates among whites relative to minority patients (Friedman et al., 2019; Kessler et al., 2006; Oehrlein et al., 2016), and likely reflects racial disparities in treatment and diagnosis of ADHD between these groups (Coker et al., 2016). The finding that prescribing is associated with population density is also consistent with the sparse body of literature on population-based stimulant prescribing trends (McDonald & Jalbert, 2013).
To our knowledge, this is the first study to track area-level trends of stimulant prescribing by SES, racial, and rural characteristics. We found that ZCTAs with lower proportion-white populations had greater growth in prescribing despite having lower baseline prescribing rates. Similarly, non-metropolitan ZCTAs had greater increases in prescribing than metropolitan ones despite having lower baseline rates of prevalent and incident prescribing. Trends in prescribing were fairly consistent across all levels of SES. These findings seem to indicate that racial and geographic disparities in stimulant prescribing may be decreasing over time, however additional research is needed to further characterize differences in stimulant prescribing by socioeconomic, racial, and urban-rural characteristics.
This study has limitations. Data are from one state only with a relatively low rate of ADHD diagnoses (Visser, 2005) and stimulant prescribing (Paulozzi, Strickler, Kreiner, & Koris, 2015; Piper et al., 2018) limiting the generalizability of our findings to other states. However, prescribing trends in California are likely similar to trends for adults in some other states; the Centers for Disease Control and Prevention have shown that ADHD diagnosis and stimulant prescribing trends for children in California do mirror national trends (Centers for Disease Control, 2019). Prescription drug monitoring programs record prescriptions filled by pharmacies, including prescriptions that are filled but not picked up by patients. These data do not capture stimulant consumption and provide no direct information on medication misuse or diversion. Prescription records also contain no information on diagnosis; however, the majority of stimulants are prescribed for ADHD (Olfson et al., 2013). Finally, results regarding demographics were made at the ZCTA level and therefore should not be interpreted as evidence of associations at the patient level.
This study analyzed a large database of controlled substance prescriptions in California to estimate trends in stimulant prescribing among adults. The dramatic increases in stimulant prescribing among 25–44 year olds during the past decade mirrors documented increases in ADHD diagnosis during that period (Oehrlein et al., 2016); however, the gap between male stimulant prescribing and national prevalence estimates of ADHD may indicate underprescribing and warrants further examination. This growth in prescribing is concerning in light of recent increases in stimulant misuse and stimulant-related overdose rates (Seth et al., 2018), particularly among early working age adults (25–44) who have a high rate of substance use disorder (Vasilenko, Evans-Polce, & Lanza, 2017). Diversion of legitimately prescribed stimulants is the most common source of misused stimulants (Cassidy et al., 2015), therefore improved strategies for identifying prescription stimulant misuse among early working age adults is a particularly important avenue for further study. Finally, the strong association between prescribing rates and proportion white ZCTA are concerning and further research is needed to identify the extent to which these area-level associations reflect under-diagnosis of ADHD among minority patients (versus overprescribing for white patients) in order to identify strategies for reducing racial/ethnic disparities in this area.
Supplementary Material
Acknowledgments
The authors would like to acknowledge Eryn Murphy for her contributions to this study.
This work was supported by the National Institute on Drug Abuse (R01DA044282). Dr. Henry is supported by National Institute on Drug Abuse Career Development Award K23DA043052.
Footnotes
The authors have no conflicts of interest to disclose.
References
- Bernardi S, Faraone SV, Cortese S, Kerridge BT, Pallanti S, Wang S,& Blanco C. (2012). The lifetime impact of attention deficit hyperactivity disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Psychol Med, 42(4), 875–887. doi: 10.1017/S003329171100153X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman J, Petty CR, Evans M, Small J,& Faraone SV (2010). How persistent is ADHD? A controlled 10-year follow-up study of boys with ADHD. Psychiatry Res, 177(3), 299–304. doi: 10.1016/j.psychres.2009.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burcu M, Zito JM, Metcalfe L, Underwood H,& Safer DJ (2016). Trends in Stimulant Medication Use in Commercially Insured Youths and Adults, 2010–2014. JAMA Psychiatry, 73(9), 992–993. doi: 10.1001/jamapsychiatry.2016.1182 [DOI] [PubMed] [Google Scholar]
- Cassidy TA, Varughese S, Russo L, Budman SH, Eaton TA, & Butler SF (2015). Nonmedical Use and Diversion of ADHD Stimulants Among U.S. Adults Ages 18–49: A National Internet Survey. J Atten Disord, 19(7), 630–640. doi: 10.1177/1087054712468486 [DOI] [PubMed] [Google Scholar]
- Castle L, Aubert RE, Verbrugge RR, Khalid M,& Epstein RS (2007). Trends in medication treatment for ADHD. J Atten Disord, 10(4), 335–342. doi: 10.1177/1087054707299597 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control. (2019). Parent-Reported Diagnosis of ADHD by a Health Care Provider and Medication Treatment Among Children 4–17 Years: National Survey of Children’s Health – 2003 to 2011 – Data Profiles by State. Retrieved from https://www.cdc.gov/ncbddd/adhd/stateprofiles/index.html
- Chen LY, Crum RM, Strain EC, Alexander GC, Kaufmann C,& Mojtabai R. (2016). Prescriptions, nonmedical use, and emergency department visits involving prescription stimulants. J Clin Psychiatry, 77(3), e297–304. doi: 10.4088/JCP.14m09291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coker TR, Elliott MN, Toomey SL, Schwebel DC, Cuccaro P, Tortolero Emery S,. . . Schuster MA (2016). Racial and Ethnic Disparities in ADHD Diagnosis and Treatment. Pediatrics, 138(3). doi: 10.1542/peds.2016-0407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman J, Kim D, Schneberk T, Bourgois P, Shin M, Celious A,& Schriger DL (2019). Assessment of Racial/Ethnic and Income Disparities in the Prescription of Opioids and Other Controlled Medications in California. JAMA Intern Med. doi: 10.1001/jamainternmed.2018.6721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganguly R, Tian Y, Kong SX, Hersloev M, Hobbs T, Smolarz BG, . . . Weng W. (2018). Persistence of newer anti-obesity medications in a real-world setting. Diabetes Res Clin Pract, 143, 348–356. doi: 10.1016/j.diabres.2018.07.017 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O,. . . Zaslavsky AM (2006). The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry, 163(4), 716–723. doi: 10.1176/ajp.2006.163.4.716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Adler LA, Barkley R, Biederman J, Conners CK, Faraone SV, . . . Zaslavsky AM (2005). Patterns and predictors of attention-deficit/hyperactivity disorder persistence into adulthood: results from the national comorbidity survey replication. Biol Psychiatry, 57(11), 1442–1451. doi: 10.1016/j.biopsych.2005.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakhan SE, & Kirchgessner A. (2012). Prescription stimulants in individuals with and without attention deficit hyperactivity disorder: misuse, cognitive impact, and adverse effects. Brain Behav, 2(5), 661–677. doi: 10.1002/brb3.78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matte B, Anselmi L, Salum GA, Kieling C, Goncalves H, Menezes A,. . . Rohde LA (2015). ADHD in DSM-5: a field trial in a large, representative sample of 18- to 19-year-old adults. Psychol Med, 45(2), 361–373. doi: 10.1017/S0033291714001470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald DC, & Jalbert SK (2013). Geographic variation and disparity in stimulant treatment of adults and children in the United States in 2008. Psychiatr Serv, 64(11), 1079–1086. doi: 10.1176/appi.ps.004442012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Mental Health. (2016). Could I Have Attention-Deficit/Hyperactivity Disorder (ADHD)? Retrieved from https://www.nimh.nih.gov/health/publications/could-i-have-adhd/index.shtml#pub2
- Oehrlein EM, Burcu M, Safer DJ, & Zito JM (2016). National Trends in ADHD Diagnosis and Treatment: Comparison of Youth and Adult Office-Based Visits. Psychiatr Serv, 67(9), 964–969. doi: 10.1176/appi.ps.201500269 [DOI] [PubMed] [Google Scholar]
- Olfson M, Blanco C, Wang S,& Greenhill LL (2013). Trends in office-based treatment of adults with stimulants in the United States. J Clin Psychiatry, 74(1), 43–50. doi: 10.4088/JCP.12m07975 [DOI] [PubMed] [Google Scholar]
- Paulozzi LJ, Strickler GK, Kreiner PW, & Koris CM (2015). Controlled Substance Prescribing Patterns--Prescription Behavior Surveillance System, Eight States, 2013. MMWR Surveill Summ, 64(9), 1–14. doi: 10.15585/mmwr.ss6409a1 [DOI] [PubMed] [Google Scholar]
- Piper BJ, Ogden CL, Simoyan OM, Chung DY, Caggiano JF, Nichols SD, & McCall KL (2018). Trends in use of prescription stimulants in the United States and Territories, 2006 to 2016. PLOS ONE, 13(11), e0206100. doi: 10.1371/journal.pone.0206100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safer DJ (2016). Recent Trends in Stimulant Usage. J Atten Disord, 20(6), 471–477. doi: 10.1177/1087054715605915 [DOI] [PubMed] [Google Scholar]
- Seth P, Scholl L, Rudd RA, & Bacon S. (2018). Overdose Deaths Involving Opioids, Cocaine, and Psychostimulants - United States, 2015–2016. MMWR Morb Mortal Wkly Rep, 67(12), 349–358. doi: 10.15585/mmwr.mm6712a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiels MS, Freedman ND, Thomas D,& Berrington de Gonzalez A. (2018). Trends in U.S. Drug Overdose Deaths in Non-Hispanic Black, Hispanic, and Non-Hispanic White Persons, 2000–2015. Ann Intern Med, 168(6), 453–455. doi: 10.7326/M17-1812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau. (2014). Overview of the 2010 ZIP Code Tabulation Area (ZCTA) Relationship Files. Retrieved from https://www.census.gov/geo/maps-data/data/zcta_rel_overview.html
- United States Census Bureau. (2018). American Community Survey (ACS). Retrieved from https://www.census.gov/programs-surveys/acs
- United States Census Bureau Population Estimates Program. (2018). Population and Housing Unit Estimates. Retrieved from https://www.census.gov/programs-surveys/popest.html
- United States Department of Agriculture. (2016). 2010 Rural-Urban Commuting Area (RUCA) Codes. Retrieved from https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/documentation/
- Vasilenko SA, Evans-Polce RJ, & Lanza ST (2017). Age trends in rates of substance use disorders across ages 18–90: Differences by gender and race/ethnicity. Drug and Alcohol Dependence, 180, 260–264. doi: 10.1016/j.drugalcdep.2017.08.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser SN, Lesesne CA,. (2005). Mental health in the United States. Prevalence of diagnosis and medication treatment for attention-deficit/hyperactivity disorder--United States, 2003. MMWR Morb Mortal Wkly Rep, 54(34), 842–847. [PubMed] [Google Scholar]
- Williamson D,& Johnston C. (2015). Gender differences in adults with attention-deficit/hyperactivity disorder: A narrative review. Clin Psychol Rev, 40, 15–27. doi: 10.1016/j.cpr.2015.05.005 [DOI] [PubMed] [Google Scholar]
- Yost K, Perkins C, Cohen R, Morris C,& Wright W. (2001). Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control, 12(8), 703–711. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


