Abstract
Classic Kaposi’s sarcoma (CKS) is an angioproliferative cutaneous neoplasm which currently lacks a well-defined treatment regimen. Because the disease is often localized, topical therapies offer therapeutic potential without the morbidity of systemic or surgical treatment. Timolol, a topical β-adrenergic receptor antagonist, has shown promise in the treatment of CKS in individual cases. Here we report a patient with classic Kaposi’s sarcoma who failed treatment with 0.5% topical timolol three times daily for 12 weeks. Topical timolol use has been previously reported in eight patients with CKS who all responded to treatment with no adverse effects. Our divergent experience from the literature implies that while topical timolol may be an effective and safe treatment alternative to traditional therapies for patients with CKS, further prospective studies are needed.
Keywords: kaposi's sarcoma, topical, timolol, classic kaposi sarcoma, case report
Introduction
Kaposi’s sarcoma (KS) is an angioproliferative neoplasm of endothelial origin associated with human herpesvirus 8 (HHV-8) and human immunodeficiency virus (HIV) infection. Classic Kaposi’s sarcoma (CKS), one of four subtypes of KS, is characterized by dark-colored cutaneous lesions most frequently occurring on the distal extremities of the lower legs and feet in middle-aged to elderly males. Lesions develop slowly, and although CKS is rarely responsible for death, complications such as pain, ulceration, lymphedema, and bleeding are common [1]. Traditional management of CKS is usually individualized and targeted towards alleviating lymphedema, decreasing the size of lesions, and delaying or preventing disease progression with surgery, radiation, and/or chemotherapy. These treatments may cause significant adverse effects [2]. Localized topical therapies have unique potential for CKS, as the disease rarely involves lymph nodes, mucous membranes, or visceral organs [3]. Topical treatments for CKS could avoid subjecting patients to the cost of surgery or adverse effects of systemic chemotherapy or radiotherapy.
Timolol, a nonselective β-adrenergic receptor antagonist, is of particular interest in treating CKS due to its effectiveness in the treatment of infantile hemangiomas [4]. However, the use of timolol in CKS treatment has not been validated. Here we report failure of topical timolol in CKS. We also summarize and elucidate the current literature reporting the use of topical timolol in the treatment of CKS.
Case presentation
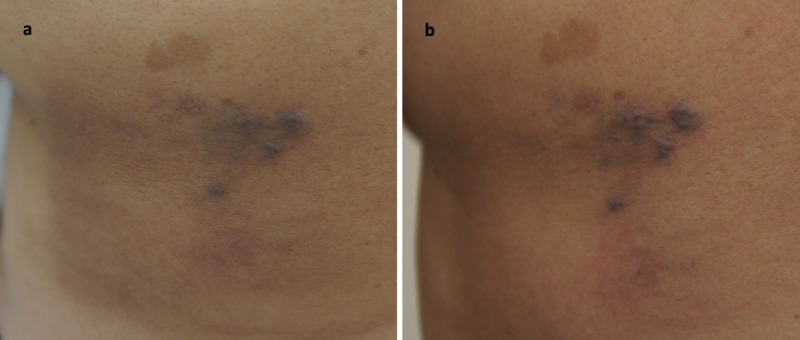
A 55-year-old woman with a history of hypertension and colonic adenoma presented with a cluster of 6-10 moderately well-demarcated, dark purple papules and plaques ranging in size from 5 mm to 20 mm in the left mid-back region (Figure 1a). Histology revealed proliferation of spindle-like endothelial cells with slit-like vascular spaces and extravasation of red blood cells, consistent with CKS. Lesions were positive for HHV-8 following immunohistochemical staining, confirming diagnosis. The patient was HIV negative and was not taking any immunosuppressive drugs. With the diagnosis of CKS, the patient first received radiation therapy but without change in size or appearance of the lesions. She was then prescribed treatment with timolol ophthalmic gel-forming solution 0.5% twice per day, but she reported application of the solution to lesions three times per day. After 12 weeks of timolol application, although no adverse effects from treatment occurred, there was no improvement in size or appearance of the lesions (Figure 1b). Timolol treatment was stopped at this point, and the patient was started on local interferon alpha injections twice weekly.
Figure 1. Classic Kaposi’s sarcoma, affecting the middle region of left mid-back.
(a) Idiopathic, asymptomatic, well-delineated lesions. (b) No significant improvement at 12 weeks with 0.5% topical timolol solution applied three times per day.
Discussion
To date, there have been eight cases published reporting the use of topical timolol to treat CKS (Table 1) [5-8]. Notably, the median age of reported cases was 74.5 years with a majority (75%) being male, consistent with the known demographics of CKS. Most patients (75%) presented with papules or plaques, although presentations also included discolored macules or bleeding nodules. All patients were HIV-negative and received topical timolol twice per day, with strengths varying between 0.1% and 0.5%. One patient was also receiving bisoprolol, an oral β-adrenergic receptor antagonist, to manage hypertension during timolol treatment; other medications of the remaining patients were not reported. All patients reported in the literature responded to treatment, with lesions rapidly remitting in 37.5% of cases following timolol treatment. Of the patients that experienced complete resolution, disease recurrence monitoring was not reported for three patients, but no others experienced recurrence at a mean follow-up of 12.3 months. Importantly, there were no adverse effects experienced from timolol treatment, with all but one case reporting data on adverse effects.
Table 1. Summary of case reports of CKS treated with topical timolol.
CKS: Classic Kaposi’s sarcoma
| Source | Sex, age | Location of disease | Clinical presentation | Timolol strength | Treatment duration | Treatment response | Follow-up, mo. |
| Gupta et al. (this report) | F, 55 | Left mid-back | Purple papules | 0.5% | 12 weeks | No response | N/A |
| Abdelmaksoud et al., 2017 [5] | M, 52 | Left leg | Plaque | 0.1% | 5 weeks | Complete resolution | 10 |
| Abdelmaksoud et al., 2017 [5] | F, 70 | Left foot | Plaque & nodule | 0.1% | 5 weeks | Complete resolution | 9 |
| Abdelmaksoud et al., 2017 [5] | M, 65 | Right leg | Plaque | 0.1% | 4 weeks | Complete resolution | 6 |
| Sainz-Gaspar et al., 2017 [6] | M, 71 | Glans penis | Red-purple macules & papules | 0.5% | 24 weeks | Complete resolution | 10 |
| Alcántara-Reifs et al., 2016 [7] | M, 89 | Medial toes bilaterally | Purple macules & nodules | 0.5% | 12 weeks | Complete resolution | 5 |
| Alcántara-Reifs et al., 2016 [7] | M, 83 | Medial right ring finger | Bleeding, red nodule | 0.5% | 18 weeks | Resolution to residual macular appearance | 4 |
| Meseguer-Yebra et al., 2015 [8] | M, 78 | Right foot | Erosive papule | 0.5% | 12 weeks | Complete resolution | 22 |
| Meseguer-Yebra et al., 2015 [8] | F, 94 | Right leg | Papule | 0.5% | 12 weeks | Resolution to residual macular appearance | 20 |
Our patient had a divergent outcome compared to previously reported cases of topical timolol for CKS, with the treatment failing to produce an effect after failed radiation therapy. This is in contrast to all other cases published in the literature, in which each patient achieved either partial or complete disease resolution. This may highlight the positive bias surrounding timolol treatment, as there may have been additional negative or equivocal results related to timolol use that were not published. While topical timolol may be an effective therapy for patients with CKS, it is important to consider this bias and plan for other treatment options if timolol treatment is attempted and fails.
Topical timolol has largely been shown to be effective in the treatment of infantile hemangiomas with a 96% response rate [4, 9]; in addition, evidence is emerging for its use in other conditions including pyogenic granulomas, recalcitrant wounds, chronic ulcers, and port-wine stains [10]. The mechanism of action of timolol is unclear but previous studies have shown that KS lesions are dependent on β-adrenergic signaling for the reactivation of HHV-8, resulting in proliferation of KS [11]. This finding supports a potential explanation for the reported effectiveness of timolol for CKS lesions on a molecular level.
Experience with timolol in other types of KS, including HIV-associated, endemic, and iatrogenic KS (usually resulting from immunosuppressive therapy), is limited. One case of timolol use in HIV-associated KS has been reported, where the use of 0.1% topical timolol twice daily led to remission at six weeks of treatment and no sign of recurrence at four-month follow-up [5]. Use of 0.5% topical timolol solution three times per day in iatrogenic KS following radiation therapy also improved ulceration and lymphadenopathy after 17 weeks in another case [12]. Neither of these cases reported adverse effects from treatment. While current evidence remains limited, these cases suggest that timolol may have potential to treat other forms of KS.
Timolol is one of a number of topical treatments emerging in CKS. Previous case reports have described clinical responses to 5% imiquimod [13], 0.5% rapamycin [14], and 0.1% alitretinoin [15]. However, with the exception of imiquimod, these have been reported as single case reports, with variable response [16].
Conclusions
All cases in the current literature reporting the use of topical timolol treatment in CKS have demonstrated clinical response with no recurrence at follow-up for those that achieved complete resolution. However, this case report demonstrates that the treatment may not be effective in all patients. Together, this suggests that the use of topical timolol may be a safe and effective treatment option for individuals with localized CKS, but further controlled trials are warranted.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
References
- 1.Kaposi's sarcoma: etiology and pathogenesis, inducing factors, causal associations, and treatments: facts and controversies. Ruocco E, Ruocco V, Tornesello ML, Gambardella A, Wolf R, Buonaguro FM. Clin Dermatol. 2013;31:413–422. doi: 10.1016/j.clindermatol.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Treatments for classic Kaposi sarcoma: a systematic review of the literature. Regnier-Rosencher E, Guillot B, Dupin N. J Am Acad Dermatol. 2013;68:313–331. doi: 10.1016/j.jaad.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 3.Kaposi sarcoma in unusual locations. Pantanowitz L, Dezube BJ. BMC Cancer. 2008;8:190. doi: 10.1186/1471-2407-8-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Topical timolol: a safer alternative for complicated and un-complicated infantile hemangiomas. Ambika H, Sujatha C, Kumar YH. Indian J Dermatol. 2013;58:330. doi: 10.4103/0019-5154.113997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Classic and HIV-related Kaposi sarcoma treated with 0.1% topical timolol gel. Abdelmaksoud A, Filoni A, Giudice G, Vestita M. J Am Acad Dermatol. 2017;76:153–155. doi: 10.1016/j.jaad.2016.08.041. [DOI] [PubMed] [Google Scholar]
- 6.Topical timolol for treatment of penile Kaposi sarcoma in HIV-negative patient. Sainz-Gaspar L, Suarez-Penaranda JM, Pousa-Martinez M, Vazquez-Veiga H, Fernandez-Redondo V. Dermatol Ther. 2017;30:0. doi: 10.1111/dth.12519. [DOI] [PubMed] [Google Scholar]
- 7.Classic Kaposi's sarcoma treated with topical 0.5% timolol gel. Alcantara-Reifs CM, Salido-Vallejo R, Garnacho-Saucedo GM, Velez Garcia-Nieto A. Dermatol Ther. 2016;29:309–311. doi: 10.1111/dth.12381. [DOI] [PubMed] [Google Scholar]
- 8.Successful treatment of classic Kaposi sarcoma with topical timolol: report of two cases. Meseguer-Yebra C, Cardenoso-Alvarez ME, Bordel-Gomez MT, Fraile-Alonso MC, Perez-Losada ME, Sanchez-Estella J. Br J Dermatol. 2015;173:860–862. doi: 10.1111/bjd.13746. [DOI] [PubMed] [Google Scholar]
- 9.Topical timolol vs. oral propranolol for the treatment of superficial infantile hemangiomas. Wu HW, Wang X, Zhang L, Zheng JW, Liu C, Wang YA. Front Oncol. 2018;8:605. doi: 10.3389/fonc.2018.00605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Topical timolol: an effective treatment option for agminated pyogenic granuloma. McGinness A, Gillam A, Yeh I, Mathes EF. Pediatr Dermatol. 2018;35:300–303. doi: 10.1111/pde.13575. [DOI] [PubMed] [Google Scholar]
- 11.Beta-adrenoreceptors reactivate Kaposi's sarcoma-associated herpesvirus lytic replication via PKA-dependent control of viral RTA. Chang M, Brown HJ, Collado-Hidalgo A, et al. J Virol. 2005;79:13538–13547. doi: 10.1128/JVI.79.21.13538-13547.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Treatment of cutaneous iatrogenic Kaposi sarcoma with topical timolol. Chap S, Vu M, Robinson AJ, Braue A, Varigos GA, Scardamaglia L. Australas J Dermatol. 2017;58:242–243. doi: 10.1111/ajd.12650. [DOI] [PubMed] [Google Scholar]
- 13.Kaposi's sarcoma responding to topical imiquimod 5% cream: a case report. Benomar S, Boutayeb S, Benzekri L, Errihani H, Hassam B. Cases J. 2009;2:7092. doi: 10.4076/1757-1626-2-7092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Classic Kaposi's sarcoma treated with topical rapamycin. Diaz-Ley B, Grillo E, Rios-Buceta L, Paoli J, Moreno C, Vano-Galvan S, Jaen-Olasolo P. Dermatol Ther. 2015;28:40–43. doi: 10.1111/dth.12182. [DOI] [PubMed] [Google Scholar]
- 15.Topical 0.1% alitretinoin gel for classic Kaposi sarcoma. Morganroth GS. Arch Dermatol. 2002;138:542–543. doi: 10.1001/archderm.138.4.542. [DOI] [PubMed] [Google Scholar]
- 16.Failure of topical 0.1% alitretinoin gel for classic Kaposi sarcoma: first European experience. Rongioletti F, Zaccaria E, Viglizzo G. Br J Dermatol. 2006;155:856–857. doi: 10.1111/j.1365-2133.2006.07392.x. [DOI] [PubMed] [Google Scholar]