Abstract
Malrotation is part of a spectrum of small and large bowel positional and fixational abnormalities caused by the failure of the fetal intestine to complete a 270-degree rotation around the superior mesenteric artery axis. Rarely, it presents in the adult as a cause of acute small bowel obstruction. Chronic symptoms of malrotation in adults are subtle, and include intermittent abdominal pain, nausea and vomiting. We present two cases of malrotation in octogenarian men presenting acutely with small bowel obstruction. Both patients were treated with emergency surgery. In one case the chronic symptoms resolved postoperatively. Malrotation and midgut volvulus should be considered as a rare differential diagnosis for small bowel obstruction in adults. Suspicions should be increased when there is a history of recurrent presentations with similar symptoms.
Keywords: Intestinal malrotation, Case reports, Adult, Midgut, Volvulus
Background
Malrotation describes the complete or partial failure of the fetal intestine to rotate 270-degrees anticlockwise around the superior mesenteric artery axis.1 Incidence is approximately 0.2% of live births worldwide.2 Failure of rotation results in a spectrum of positional and fixational abnormalities of the small and large intestines.
Malrotation presents within the first week of life in 40%, and within the first year in 75–85%. The remaining patients are typically diagnosed in childhood, but rarely present in adulthood.1 We present two unusual cases of adult midgut malrotation in patients aged over 80 years of age with small bowel obstruction.
Case history
Case one
An 80-year-old man presented with a four-day history of nausea and vomiting and a five-day history of constipation. He denied abdominal pain. The vomiting was of small volume and occurred 10–15 times a day. He had previously presented on multiple occasions with episodes of vomiting, mild abdominal pain and abdominal distention. Small bowel obstruction had been diagnosed and treated conservatively.
Routine bloods showed a raised white cell count and C-reactive protein, hypokalaemia, hyponatraemia and an acute kidney injury. An erect plain film chest x-ray showed no free intraperitoneal air. A diagnosis of small bowel obstruction was made and he was initially treated conservatively with nasogastric tube insertion and intravenous fluids.
Computed tomography (CT) with intravenous contrast showed dilatation of the distal oesophagus, stomach and duodenum, and a cutoff point at the third/fourth part of the duodenum with a twist in the small bowel mesentery (Fig 1A). The terminal ileum and caecum were located in the left upper quadrant (Fig 1B). An oesophagogastroduodenoscopy was attempted, but the scope was unable to pass the point of obstruction at D3.
Figure 1.
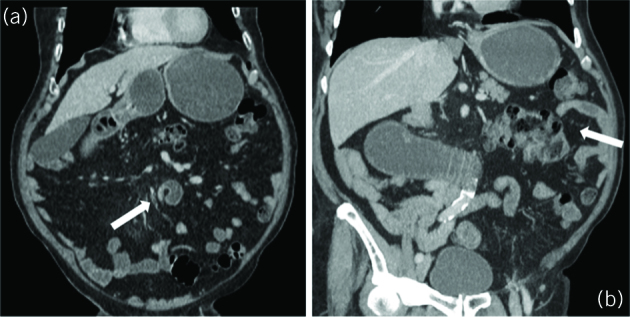
Computed tomography of the abdomen and pelvis with intravenous contrast; coronal view. (A) A smooth narrowing and ‘beaking’ of the distal duodenum is seen at D3/D4 (arrow) with no obvious mass. There is dilation of the stomach. (B) There is distention of the stomach and visualised section of the duodenum. The small bowel loops are predominantly on the right, and the caecum and ileocaecal valve (arrow) is located in the left upper quadrant.
The patient then underwent a laparotomy on admission day nine, with adhesiolysis, detorsion of the mesentery and gastrojejunostomy to bypass the obstruction. CT with oral and intravenous contrast at seven days post-surgery showed patency of the anastomosis. The superior mesenteric vein was also seen to the left of the superior mesenteric artery. The postoperative period was unremarkable and the patient was discharged 16 days after the procedure. On the day of discharge the patient was readmitted due to wound dehiscence. This was repaired with antibiotic cover. There were no further issues and the patient was well at one month follow-up.
Case two
An 83-year-old man presented with nausea and vomiting, predominantly after meals. The vomiting was of small volume and had been continuing for one week. The patient had no abdominal pain on admission and reported no longstanding abdominal pain or other pertinent symptoms.
Bloods tests on admission showed hyponatraemia, a raised white cell count, and a mildly raised C-reactive protein and amylase. Abdominal and chest x-rays were unremarkable. Non-contrast CT showed a distended and fluid filled stomach and duodenum, with a transition point at the junction of the third and fourth part of the duodenum (Fig 2A). The superior mesenteric vein was to the right of the artery, and the caecum was located in the left upper quadrant (Fig 2B). The whirlpool sign was also noted anterior to the dilated duodenum (Fig 2C). A diagnosis of malrotation was made.
Figure 2.
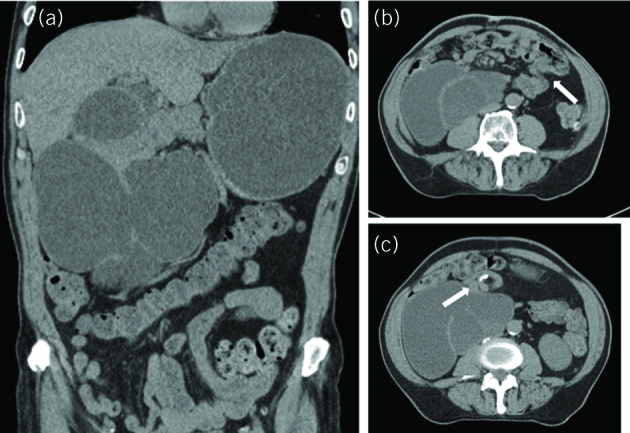
Non-contrast computed tomography of the abdomen and pelvis; coronal and axial views. (A) There is distention of the stomach and duodenum. The duodenum is located predominantly on the right. (B) The ileocaecal valve (arrow) is shown in the left upper quadrant. (C) Whirlpool sign (arrow) anterior to the dilated duodenum.
The patient also underwent an emergency laparotomy on the fourth day of admission, with adhesiolysis, detorsion of the malrotated bowel and gastrojejunostomy. Postoperatively, the patient had a central venous line inserted for parenteral nutrition and was admitted to the intensive care unit. The patient also had a prolonged ileus postoperatively, treated with metoclopramide, domperidone and erythromycin.
The central line subsequently became infected, with blood cultures positive for Klebsiella pneumoniae, which was successfully treated with antibiotics. The patient was stepped down from intensive care and started on nasojejunal feeding until he was able to tolerate oral intake. He was discharged 27 days after the procedure. He was reviewed as an outpatient two weeks later and reported improvement of symptoms, with improved food tolerance and no postprandial vomiting.
Discussion
Malrotation is rarely diagnosed beyond infancy, with 75–85% presenting within the first year of life.1 Typically, intestinal torsion due to malrotation presents with sudden abdominal pain, nausea, vomiting and obstipation. Chronic symptoms include intermittent abdominal pain, nausea and vomiting, diarrhoea or constipation, food intolerance and bloating.3
The most accurate diagnostic imaging modality is oral and intravenous contrast-enhanced CT. Ultrasound is a less useful modality for assessing malrotation in an adult, although Doppler ultrasound can be used to evaluate the anatomy of the superior mesenteric artery.3 The classical diagnostic finding on imaging is the ‘whirlpool’ sign, where there is clockwise twisting of the midgut mesentery. This may be accompanied by reversal of the superior mesenteric artery and vein. Other imaging findings include the abnormal positioning of the duodenojejunal junction to the right of the vertebral column, large bowel located on the left and abnormal placement of the ileocaecal valve.
Although cases of symptomatic midgut volvulus have been reported to have resolved without surgical management,4 the standard treatment of both paediatric and adult malrotation is Ladd’s procedure. This consists of detorsion of the midgut volvulus, division of Ladd’s bands, fixation of the small and large bowel to the correct positions in the abdomen and appendicectomy. Ladd’s operation can be performed laparoscopically with similar outcomes to open.5 However, in patients with intestinal ischaemia, urgent laparotomy with bowel resection must be considered.
Conclusion
Malrotation in adult patients is a rare cause of acute abdominal pain. It should be considered as a differential in older patients presenting with small bowel obstruction, especially when there is a background of chronic abdominal pain, nausea and vomiting. Surgical management should be prompt to prevent serious morbidity and potential mortality.
References
- 1.McVay M, Kokoska ER, Jackson RJ, Smith SD. The changing spectrum of intestinal malrotation: diagnosis and management. Am J Surg 2007; : 712–719. [DOI] [PubMed] [Google Scholar]
- 2.Dietz DW, Walsh RM, Grundfest-Broniatowski S et al. Intestinal malrotation: a rare but important cause of bowel obstruction in adults. Dis Colon Rectum 2002; : 1,381–1,386. [DOI] [PubMed] [Google Scholar]
- 3.Matzke GM, Dozois EJ, Larson DW, Moir CR. Surgical management of intestinal malrotation in adults: comparative results for open and laparoscopic Ladd procedures. Surg Endosc 2005; : 1,416–1,419. [DOI] [PubMed] [Google Scholar]
- 4.Deniffel D, Goerke SM, Rummeny EJ, Laubenberger J. Novel variant of reversed midgut rotation; retro-arterial proximal jejunum and transverse colon: a case report and review of the literature. J Med Case Rep 2018; : 261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seymour NE, Andersen DK. Laparoscopic treatment of intestinal malrotation in adults. J Soc Laparoendosc Surg 2005; : 298–301. [PMC free article] [PubMed] [Google Scholar]


