Abstract
Fragile X syndrome, the leading heritable form of intellectual disability, is caused by hypermethylation and transcriptional silencing of large (CGG) repeat expansions (> 200 repeats) in the 5′ untranslated region of the fragile X mental retardation 1 (FMR1) gene. As a consequence of FMR1 gene silencing, there is little or no production of FMR1 protein (FMRP), an important element in normal synaptic function. Although the absence of FMRP has long been known to be responsible for the cognitive impairment in fragile X syndrome, the relationship between FMRP level and cognitive ability (IQ) is only imprecisely understood. To address this issue, a high-throughput, fluorescence resonance energy transfer (FRET) assay has been used to quantify FMRP levels in dermal fibroblasts, and the relationship between FMRP and IQ measures was assessed by statistical analysis in a cohort of 184 individuals with CGG-repeat lengths spanning normal (< 45 CGGs) to full mutation (> 200 CGGs) repeat ranges in fibroblasts. The principal findings of the current study are twofold: i) For those with normal CGG repeats, IQ is no longer sensitive to further increases in FMRP above an FMRP threshold of ~70% of the mean FMRP level; below this threshold, IQ decreases steeply with further decreases in FMRP; and ii) For the current cohort, a mean IQ of 85 (lower bound for the normal IQ range) is attained for FMRP levels that are only ~35% of the mean FMRP level among normal CGG-repeat controls. The current results should help guide expectations for efforts to induce FMR1 gene activity and for the levels of cognitive function expected for a given range of FMRP levels.
Introduction
Fragile X syndrome (FXS) is the leading heritable form of intellectual disability and the leading monogenic form of autism spectrum disorder (ASD). In addition to cognitive impairment, individuals with FXS can manifest a broad range of behavioral and psychiatric symptoms (e.g., hyperactivity, impulsivity, aggression, and anxiety), poor language development, seizures, and characteristic physical features (see Reviews [1, 2–4]). In nearly every instance, FXS is caused by expansion of a 5′ noncoding trinucleotide (CGG) beyond ~200 repeats (full mutation; FM) in the fragile X mental retardation 1 (FMR1) gene. These large CGG-repeat expansions generally lead to hypermethylation of the promoter and CGG-repeat regions, with attendant transcriptional silencing and little or no expression of the FMR1 protein (FMRP) [5–8]. FMRP, through its capacity as an RNA binding protein [9–13], plays a critical role in neuronal function by regulating the translation, transport, and stabilization of a substantial number of mRNAs involved in the development and maintenance of synaptic connections [11, 14–22], and through its role in the homeostatic control of systemic metabolism [1, 23]. FMRP has also been shown to play a role in both the DNA damage response and the maintenance of genome stability [24, 25], and in the regulation of ion channel activity through its direct interactions with ion channel proteins [26–28]. Reduction or absence of FMRP, with resultant effects on brain morphology and function [29–31], is thought to be directly responsible for the cognitive and behavioral problems that are core features of the FXS phenotype [1].
For those whose FMR1 gene retains at least partial activity, the association between the severity of intellectual disability and the degree of FMRP deficit remains ill-defined. For example, ample evidence shows that FMRP levels are moderately diminished in both peripheral and CNS cells that harbor FMR1 alleles in the premutation range (55–200 CGG repeats), in part due to reduced efficiency of translation of the expanded-repeat FMR1 mRNA [32–34] and due to the increased likelihood that the larger premutation alleles may be at least partially methylated [35]. Thus, reductions in FMRP, if of sufficient magnitude, could result in some degree of intellectual deficit even within the premutation range [32, 36, 37]. It is also unclear to what extent unmethylated FM alleles, which are capable of producing substantial quantities of FMR1 mRNA [38, 39], have the capacity to produce FMRP from the expanded-repeat mRNA due to the inefficiency of translation from RNAs containing FM CGG repeats [8]. Early studies of individual fibroblast clones or lymphoblastoid lines suggested that FM alleles above ~300 CGG (either methylated or unmethylated) do not express FMRP [8, 14, 40, 41]. Kaufmann et al. [42] also reported low FMRP levels (10.3 ± 1.7% of normal levels) for subjects with FM alleles, although the FM CGG-repeat sizes were not reported. More recently, Pretto et al. [43] observed that males with a fully methylated FM allele had essentially no FMRP expression (by Western blot analysis). In one of their cases, a size- and methylation-mosaic male with a methylated 180 CGG-repeat allele and unmethylated ~200–270 CGG-repeat alleles had substantial FMRP, reinforcing the idea that FM alleles under ~300 CGG repeats, if unmethylated, are still capable of producing some FMRP.
Confounding the association between FMRP levels and intellectual deficit are numerous reports of males described as being of average to above average intellectual level, or mildly affected, with partially methylated alleles in the FM range [44–54]. However, part of the difficulty in assessing the relationship between IQ and genotype/FMRP expression has been distinguishing individuals who harbor exclusively FM alleles from those who possess both FM and premutation (PM; 55–200 CGG repeats) alleles. Indeed, newer studies have revealed that the majority of individuals with FM alleles are mosaics for allele size, harboring both unmethylated PM alleles and FM alleles [55–58], with such individuals retaining the capability of producing at least some FMRP. The other confound associated with studies of FMRP after 1995 has been the use of the immunocytochemical method [59] to assess the presence/absence of FMRP. Although the immunocytochemical method remains perfectly valid as a measure of fractional inactivation (e.g., gene deletion; activation ratio in females), its use as a surrogate measure for relative FMRP level (i.e., % FMRP(+) cells ≡ FMRP relative level) can lead to large uncertainties in FMRP levels because FMRP levels within each cell are not quantitated.
The question of how much FMR1 gene activity–and FMRP production–is possible in the FM range is of critical importance in determining whether efforts to reactivate FM alleles [60–69] will ultimately succeed in producing enough FMRP to have a positive effect on brain and cognitive function. However, the more immediate question, and the focus of the current study, concerns the relationship between cognitive ability and FMRP levels, irrespective of CGG-repeat size: how much FMRP is necessary for borderline to average intellectual functioning? The relevance of this question extends beyond the fragile X-associated disorders to other forms of neurodevelopmental and neuropsychiatric dysfunction, as exemplified by lowered FMRP levels in the brains of those with autism/ASD [70–72] and major psychiatric disorders, including depression and schizophrenia [73, 74].
More recently, several approaches have been developed to provide more quantitative estimates of FMRP levels from human cells/tissues. Iwahashi et al. [75] utilized an enzyme-linked immunosorbent assay (ELISA) for FMRP. Using this assay, the range of FMRP detected in the subjects with hypermethylated full-mutation alleles was 0.48% to 4.45% (n = 6) of levels observed in control males. The highest FMRP value (4.45%) corresponded to a subject with one of the smallest FM alleles (285 CGG repeats), adding support to the notion that only alleles under ~300 CGG repeats are capable of producing significant amounts of FMRP. Iwahashi et al. [76] also observed slightly higher FMRP levels (1.07% to 13.02% of control mean levels), where the higher FMRP levels could be based on smaller unmethylated FM alleles (<300 CGG repeats), as well as contributions from PM alleles. In aggregate, previous studies [58, 77, 78] indicate that significant FMRP expression arises primarily from PM alleles and not from FM alleles of greater than ~300 CGG repeats, regardless of methylation. Therefore, in discussing cases of high IQ with moderate FMRP levels, it is highly likely that individuals may be harboring size-mosaic FMR1 alleles.
In the current work, we have applied the method of fluorescence resonance energy transfer (FRET) [69, 79] to the study of the relationship between FMRP level and IQ in 184 cases with CGG lengths spanning from normal to the FM range. We observed an FMRP-level threshold, at ~70% of the mean value for those with normal CGG repeats, above which IQ no longer depends on FMRP level. For FMRP levels that exceed ~35% of the mean FMRP level among those in the normal CGG-repeat range, the upper 95%-ile for IQ values for the current cohort approaches 85 (lower bound for normal IQ range), suggesting that this level of FMRP may be sufficient for supporting its role in attaining normal intellectual functioning.
Materials and methods
Subjects
The Institutional Review Board of the University of California, Davis, approved all study protocols and written informed consent forms associated with this research. Written consent was obtained from study subjects. The subjects of this study initially included 195 individuals (121 males and 74 females; 161 white, 1 black, 5 Hispanic/Latino, 4 multi-ethnic, 2 Asian, 2 others, and 20 unknown) recruited to the University of California Davis Health MIND Institute’s Fragile X Clinical and Research Center between 2007 and 2018 as participants in studies of fragile X-associated disorders. Eleven individuals (9 males and 2 females) were subsequently excluded based on secondary, known genetic neurodevelopmental disorders, a point mutation [80], and/or dysmorphic features atypical for FXS; all of those individuals had FMRP levels within the normal range (the point mutation was detected by Western blot but not by FRET assay) but were not used for further analyses.
Full thickness skin biopsies from the left posterior shoulder area were obtained with a 3 mm punch under local anesthesia with lidocaine. The biopsies were placed in RPMI 1640 (Gibco) culture media, stored at 4°C, and processed within 24 hours. The samples were diced into approximately 15 pieces under sterile conditions on a culture plate. The pieces were distributed among three culture dishes containing 60:40 RPMI 1640:Amnio MAXTM-C100 Basal Medium (Gibco, Grand Island, NY, USA) and 15% AmnioMAXTM-C100 Supplement (Gibco). Fibroblasts were allowed to grow out from the tissue pieces for 2–3 weeks, followed by growth for no more than three passages. Cells were frozen down using 10% dimethyl sulfoxide (DMSO) in 60:40 media until needed.
IQ measures
Intellectual functioning was measured using the Wechsler Intelligence Scale for Children, Third or Fourth Edition (WISC-III or WISC-IV; Pearson, London), or the Stanford Binet Intelligence Scales, Fifth Edition (SB-5; Harcourt, San Antonio), for children ages 8–17 years, and using the Wechsler Adult Intelligence Scale, Third or Fourth Edition (WAIS-III or WAIS-IV), or the SB-5 for adults ages 18 years and up. As the assessments spanned many protocols and years of data collection, multiple test types and editions were used. IQ data were not adjusted for floor effects [81, 82], since only a single individual had an IQ with a floored score (IQ = 40).
Fibroblast culture
Fibroblast lines used for the current study were derived from biopsies performed over an 11-year period (2007–2018). The choice of dermal fibroblasts over peripheral blood cells was made because we have found the stability of the protein is greater during isolation from fibroblasts than for isolation from peripheral blood mononuclear cells (data not shown), presumably due to residual proteases in peripheral blood granulocytes and other lysed cell types or contributions from PBMCs that have been damaged during the freezing process. The constancy of the mean FMRP levels among normal controls across this period indicated that there was no effect of the duration of storage on the FMRP levels produced following revival and culture. To provide an equal starting point for measurements of FMRP levels, cryopreserved fibroblast lines were thawed and expanded in 60:40 media until 70–80% confluent, at which time each line was frozen at 500,000 cells/ml. A 20-year-old control male fibroblast line was used as a fiducial for all FRET plates, and FMRP levels were stable throughout the years it was tested. Five aliquots of the fibroblast line at passage five were pooled and distributed over 10 T-175 flasks, followed by growth until cells were 80–90% confluent, at which time cells were pooled and frozen down at 500,000 cells/ml.
Genotyping
Genomic DNA isolation was performed on cultured fibroblast cells using the Gentra Puregene genomic DNA purification kit (Qiagen, Redwood City, CA; catalog number 158389). One-hundred to 250 ng of DNA was used to genotype each sample using AmplideX® PCR/CE FMR1 kit (Qiagen, Redwood City, CA; cat. no.158389). PCR fragments were sent for fragment analysis on the ABI 3130xl Capillary Electrophoresis Genetic Analyzer in the College of Biological Sciences UCDNA Sequencing Facility at UC Davis. Peaks were analyzed and sized using Peak Scanner 2 (Applied Biosystems; Foster City, CA).
Western blot analysis
To analyze the point mutation case, 1016–15, (nominal concentrations of 8 μg and 16 μg total protein) was determined by bicinchoninic acid (BCA) assay (Pierce; Rockford, IL; cat. no. 23225) for each sample and was run on a Criterion™ TGX Any kD™ Precast Gel (BioRad; Hercules, CA; cat. no. 567–1125) alongside 5 μl of Chameleon Duo Pre-stained Protein Ladder (LI-COR; Lincoln, NE; cat. no. 928–60000) (marker) for 30 min at 25 mA and then 1.5 h at 150 V. Proteins were transferred to a nitrocellulose membrane at 30 V overnight at 4°C. The membrane was blocked in 1:1 PBS:Odyssey® Blocking Buffer (LI-COR; 927–40000) for 1 h at room temperature. Mouse anti-FMRP (Millipore; Burlington, MA; cat. no. MAB2160; Lot no. 2548166) primary antibody in blocking buffer, supplemented with 0.1% Tween-20, was applied to the membrane at 1:5,000 overnight at 4°C. Subsequently, IRDye® 800CW Goat anti-Mouse (LI-COR; cat. no. 926–32210; Lot no. C50316-03) secondary antibody in blocking buffer, supplemented with 0.1% Tween-20, was applied to the membrane at 1:20,000 for 1.5 h at room temperature. Membrane was visualized on the LI-COR Odyssey Infrared Imager.
FRET analysis
Fibroblasts (500,000 cells/ml) were thawed and seeded overnight at 100,000 cells/well into 24-well plates with RPMI 1640. The cells were grown overnight in 5% CO2, ambient O2. At the 24-h mark, samples were rinsed with Dulbecco's phosphate-buffered saline and lysed directly on the plate with 50 μl 1X Cisbio Human FMRP assay lysis buffer + Roche cOmpleteTM Ultra Protease Inhibitor Tablets (MilliporeSigma, Burlington, MA) for 2 h while rocking. FMRP quantification utilized the Cisbio Human FMRP assay (63ADK038PEC0; Anti-FMRP-K Lot no. 110514K; Anti-FMRP-d2; Lot no. 110514D; CisbioUS, Bedford, MA) and followed the manufacturer’s protocol. The assay uses homogeneous time-resolved fluorescence technology, as developed for quantification of FMRP [69, 79, 83]. The method uses two FMRP-specific monoclonal antibodies conjugated to fluorescent dyes; the donor was labeled with Eu2+-Cryptate and an acceptor designated d2. The time-resolved aspect of the assay exploits the long fluorescence decay times of the Eu2+-Cryptate donor fluor, such that FRET measurements do not occur until all sources of short-fluorescence-lifetime fluorescence (including from direct excitation of the acceptor) have decayed. Ten microliters of protein lysate were used in either triplicate or quadruplicate in a 384-well Opti-Plate (Perkin Elmer, Boston, MA), plus 10 μL homogeneous time-resolved fluorescence technology pre-mixed antibodies. Samples were incubated overnight in the dark and then read on the PerkinElmer VictorX5. Total protein concentrations were determined using the Thermo Fisher Micro BCA Assay (Thermo Fisher; Waltham, MA; cat. no. 23235). FMRP values were determined from interpolating FRET expression on a standard curve using a fiducial cell line. The BCA values were used to determine the ratio of interpolated FMRP to total protein. Finally, we have assessed the accuracy of the measurements by analyzing the coefficient of variation (CV) for each FMRP determination [CV (%) = 100 x σ/FMRP] (S1 Fig). For FMRP values above 20% of the mean FMRP among fibroblast lines with normal CGG repeat alleles, the CV is generally less than 20%; for FMRP levels from 1 to 10% of the normal mean level, the CV values range from ~20–100%. That is, for an FMRP level of 2%, a CV of 50% would represent a range of 1–3% for FMRP.
Statistical analysis
All statistical analyses of data were conducted using SAS 9.4 (SAS Institute, Cary, NC). Results were expressed as mean ± standard deviation of mean. Group differences in means for quantitative measures were determined by analysis of variance (ANOVA) by sex. Proportions were compared between groups using Fisher’s exact test. Correlations of CGG-repeat size and FMRP level with IQ measures were assessed with Pearson’s correlation. Trend analyses of the relationship of IQ against FMRP level were conducted using a locally weighted regression (LOESS) and a piecewise linear regression, with adjustment for age and sex as needed. LOESS is a nonparametric regression technique that smooths the dependent variable (IQ) in a moving fashion and requires nonlinearity assumptions that are typical for conventional linear regression methods [84]. The LOESS smoothing parameter was inspected to identify the value, which minimized error but did not overfit the data. The LOESS smoothing parameter incorporates both the tightness of the fit and model complexity. Root mean square error (RMSE) and residuals were calculated for the LOESS fit across the entire data range. After LOESS fit was performed, the LOESS smoothing curve was inspected to identify possible change points for a piecewise linear regression through recursive partitioning to split data into two homogenous subsets based on a given change point. This process was to minimize the RMSE with the selected smoothing curve and was applied to each IQ measure. The final decision regarding which change point for a piecewise linear model should be applied to each IQ measure was made with consideration given to both the total RMSE and physical fit. The final piecewise linear regression chosen for each IQ measure was selected by considering the total RMSE, the best fit of the curve, and the visual appeal of the combined LOESS and piecewise linear regression curves. Two-tailed P-values less than 0.05 were considered statistically significant as appropriate.
Results
Demographics of the individuals providing dermal fibroblast samples for the current study
A total of 195 fibroblast samples were cultured from punch skin biopsies from adults (74 females and 121 males). Eleven cases, with secondary known genetic neurodevelopmental disorders, a point mutation in one case, and/or dysmorphic features atypical for FXS but with normal FMRP levels, were subsequently excluded from statistical analyses, as previously mentioned. Descriptive statistics of the 184 participants used for this present study are presented in Table 1. One of the 11 excluded cases (1016–15), a severely affected ten-year-old male [Full scale IQ (FSIQ), 40; Performance (PIQ), 42; Verbal IQ (VIQ), 43] with a point mutation and a normal CGG repeat [80], is displayed in Fig 1 but was excluded from regression analyses because the point mutation prevented detection of the protein using the FRET assay.
Table 1. Descriptive statistics of patient characteristics, by sex.
| Variable | All | Females | Males | P-value* |
|---|---|---|---|---|
| N (%) | 184 | 72 (39%) | 112 (61%) | |
| Age | 46.98 ± 21.88 | 46.92 ± 19.92 | 47.02 ± 23.15 | 0.9757 |
| CGG-repeat size | 90.68 ± 65.13 | 76.41 ± 37.18 | 100.14 ± 77.09 | 0.0185 |
| Allele class, N | 0.2429 | |||
| Normal | 22 | 9 | 13 | |
| Gray | 11 | 4 | 7 | |
| Pre | 130 | 55 | 75 | |
| Mosaic | 11 | 2 | 9 | |
| Full | 9 | 1 | 8 | |
| Missing | 1 | 1 | 0 | |
| PIQ | 100.22 ± 19.60 | 103.23 ± 16.95 | 98.28 ± 20.98 | 0.0976 |
| VIQ | 108.07 ± 21.15 | 109.21 ± 17.30 | 107.33 ± 23.56 | 0.5594 |
| FSIQ | 102.71 ± 21.86 | 105.11 ± 17.87 | 101.16 ± 24.03 | 0.2326 |
* Significance of difference between males vs. females.
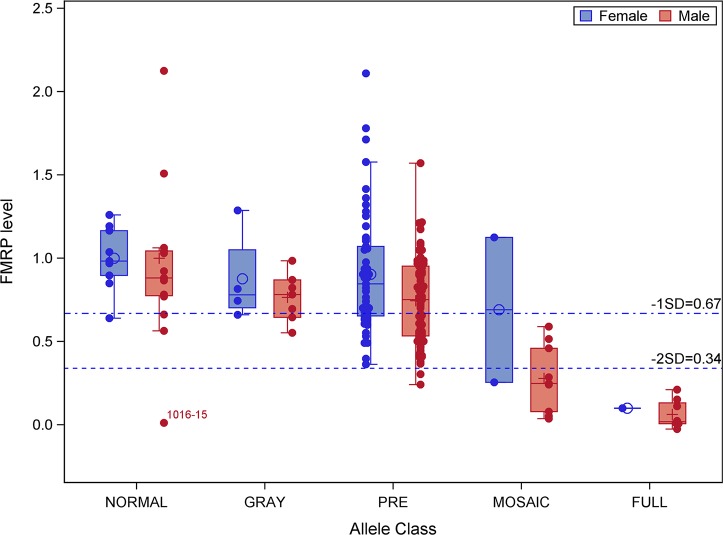
Fig 1. Distribution of FMRP levels within each allele class.
Dashed lines indicate the values of FMRP 1 SD and 2 SD (as indicated) below the relative mean level (= 1.0) of those with normal CGG-repeat alleles (see, also: Fig 2). Individual 1016–15 has a normal CGG repeat (21 CGG) but has a point mutation within the FMRP coding region [80] that prevented detection by the FRET assay (See: S2 Fig).
The distributions of FMRP levels across allele classes are displayed in Fig 1, where all FMRP values for normal or gray-zone (~46–54 CGG repeats) alleles for the current, relatively small dataset, are well above the threshold value for the normal full-scale IQ (FSIQ) range; the sole exception is a normal CGG-repeat allele that harbors a point mutation in the FMRP coding sequence [80]. This case is interesting in that the FRET assay is unable to detect the mutant protein even though the protein is produced at normal levels by Western (S2 Fig). A much broader distribution is evident among PM alleles, where larger alleles are associated with lower FMRP levels (correlation coefficient R = -0.22, P = 0.0103). FM alleles are all associated with FMRP levels below the threshold level corresponding to FSIQ = 85 in the fitting model represented in Fig 2, in keeping with the general observation that all males with FM alleles have some degree of cognitive impairment. An important, albeit less well-defined, allele class is that comprising mosaic alleles, since individuals within this class often have multiple alleles with variable proportions in PM and FM ranges, and with variable degrees of methylation of individual alleles (Fig 1).
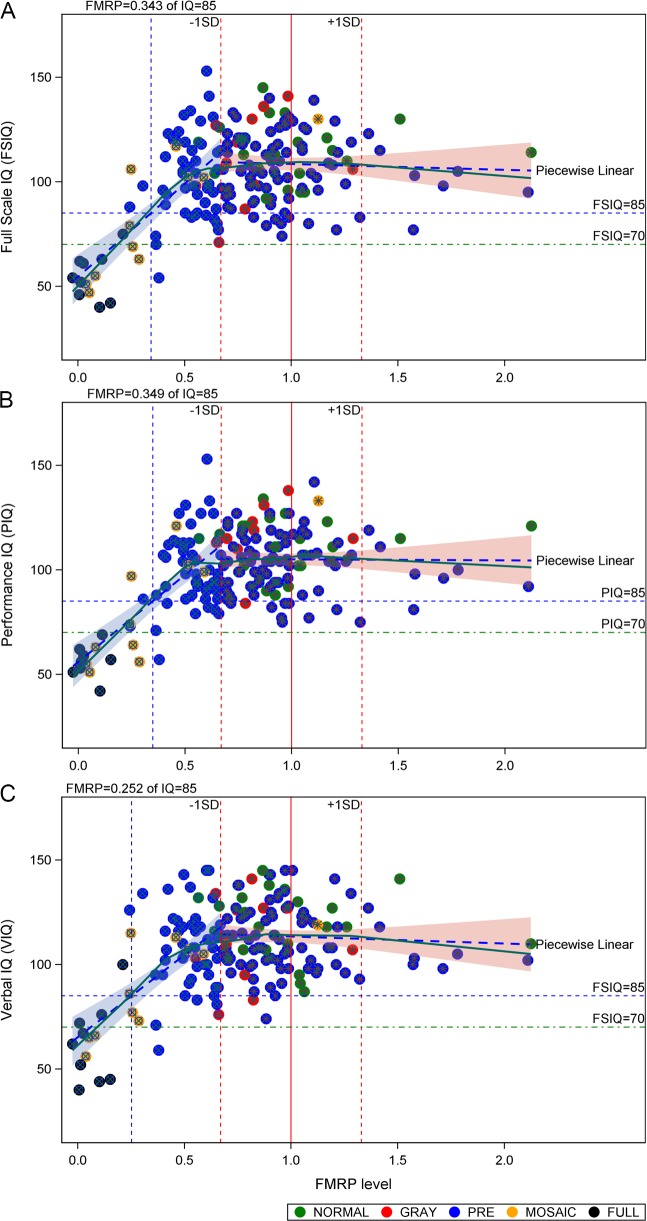
Fig 2. Dependence of IQ on FMRP levels in cultured dermal fibroblasts, accounting for sex as a covariate.
(A) FSIQ, (B) PIQ, and (C) VIQ were determined using age-appropriate instruments as delineated in the Methods section. FMRP levels were determined using FRET. All FMRP levels were normalized to the mean value of FMRP levels (= 1.0) among individuals with normal CGG repeats, excluding the FMR1 point mutation (1016–15). Data displayed are for both males and females since there is no significant differential dependence of the regression lines on sex (P > 0.05, see S1 Table); separate regression analyses for males and for females are displayed in S3A–S3F Fig. Symbols specify allele classes as indicated. Plus/minus 1 SD for FMRP levels are indicated as red vertical dashed lines. Lower limit of normal IQ (= 85) and borderline IQ (= 70) are indicated as horizontal blue and green dashed lines, respectively. The FMRP level at which the regression line for IQ passes 85 is indicated by a vertical (blue) dashed line.
The FMRP-dependence of IQ is piecewise linear, with a threshold value for FMRP-dependence approximately one SD below the normal mean level
For the current dataset, the transition from a strong dependence of IQ on FMRP to its independence of FMRP levels occurs at a value of FMRP approximately 1 SD below its mean value among individuals harboring normal CGG-repeat alleles (Fig 2). This relationship holds for both Verbal and Performance IQs (VIQ, PIQ), as well as for FSIQ. Moreover, this piecewise linear behavior remained intact even after adjusted for age and sex and in sex-specific analyses (S3 Fig and S2 Table). For participants with FMRP levels below the -1 SD inflection point, IQ measures steeply decrease with further decreases of FMRP levels. An important feature of this dataset is that the regression line for IQ passes the lower end of the normal IQ range (IQ = 85) at approximately 2 SD below the normal mean FMRP level and passes the cut-off for intellectual disability (IQ = 70) at approximately 2.5 SD below the normal mean level of FMRP (Fig 2 and Table 2).
Table 2. Piecewise regression models assessing the relationships between X = FMRP level (normalized to normal controls) and Y = IQ, and estimated FMRP levels corresponding to IQ = 85 and 70.
| IQ Measure | FMRP below -1SD | FMRP above -1SD | ||||||
|---|---|---|---|---|---|---|---|---|
| Fitted Regression Model | P-value | R2 value | Estimated FMRP levels | Fitted Regression Model | P-value | R2 value | ||
| IQ = 70 | IQ = 85 | |||||||
| Full Scale IQ | FSIQ = 54.48 + 88.97 FMRP | < 0.0001 | 0.481 | 0.174 | 0.343 | FSIQ = 111.24–2.78 FMRP | 0.6326 | 0.0021 |
| Performance IQ | PIQ = 55.90 + 83.32 FMRP | < 0.0001 | 0.5063 | 0.169 | 0.349 | PIQ = 105.45–0.48 FMRP | 0.9274 | 0.0001 |
| Verbal IQ | VIQ = 65.13 + 78.68 FMRP | <0.0001 | 0.3965 | 0.062 | 0.252 | VIQ = 116.72–3.36 FMRP | 0.5502 | 0.0033 |
Discussion
In the current study, we quantified levels of FMRP in a cohort of 184 subjects using the method of homogeneous, time-resolved FRET [83] and have related these levels to age-appropriate IQ measures. We found that the distribution of relative FMRP levels among normal controls is broadly similar to equivalent distributions determined in platelets [77] and in dried blood spots [78]. Two features of the FMRP–IQ relationship are noteworthy. First, there is a threshold level of FMRP at approximately 70% (-1 SD) of the mean FMRP level for those with normal CGG-repeat alleles, above which there is no further dependence of IQ on FMRP levels—that is, a potential state of sufficiency such that further increases above the threshold do not relate to further cognitive gain. Thus, based on this cross-sectional analysis, attempts to further increase FMRP in normal individuals would not be expected to yield changes in cognitive processes underlying IQ. Indeed, further increases in FMRP well beyond the normal range may lead to behavioral dysfunction, as demonstrated in animal models [85, 86]. Second, for FMRP levels below the threshold, there is a strong, positive relationship between FMRP levels and cognitive abilities. Although the number of cases in this range is small in the current study, the approximate linear relationship suggests that an FMRP level of only about one-third of the normal mean level is sufficient to support a mean IQ level at the lower end of the normal IQ range (= 85), and that an FMRP level of only 10–20% of normal would support a mean IQ at the borderline level. In aggregate, these observations support the idea that even relatively modest increases in FMRP, as obtained through efforts to induce its expression, could have a beneficial effect on cognitive outcomes. Similar conclusions have been drawn following introduction of FMR1 transgenes into Fmr1 knockout mice for both audiogenic seizure activity [87] and for motor/behavioral functions [88].
A further implication of the current work is the expectation of the range of IQs within the FM range. Among the eight males that harbored FM alleles without evidence of smaller PM alleles, FMRP levels ranged from 0 to 21% relative of the normal mean FMRP level. The 21% level was associated with a relatively small FM allele (250 CGG repeats) and a borderline IQ (FSIQ = 70). The remaining individuals (FMRP = 0–15%) all had FSIQs ranging from 40 to 62. Given the small number of individuals with FM alleles, these results must be viewed as provisional; however, they should serve to underscore the need for careful determination of both FMRP levels and genotype before declaring FM alleles to be associated with IQ levels in the normal range. IQs in the normal range for apparent FM alleles are actually more likely reflective of cryptic mosaicism, where–depending on the nature of size and methylation mosaicism–IQs can reach or exceed the lower level of the normal IQ range (Fig 1). This complex issue will require larger studies of both mosaic and FM cases to establish a more quantitative relationship between allele type and IQ, since the level of FMRP will depend not only on the size range for multiple alleles but also the relative abundance of each allele, as well as their separate extents of methylation. Absent such studies, we feel it more appropriate to establish the relationship between FMRP, which reflects the accumulated effects of allele types, and IQ.
The observed relationship between FMRP and IQ below the -1 SD threshold may have implications for the general population. Our observations tentatively suggest that FMRP levels would need to be reduced to about -2 SD from the normal mean (~34%) to have an average IQ at the lower boundary of the normal IQ range (IQ = 85). Thus, were our current observations to hold for much larger cohorts, we would predict that about 2–3% of the general population would have an IQ below 85 as a consequence of lowered FMRP. Of course, there are many causes of intellectual disability other than FXS, but we do not know the relationship of FMRP to intellectual deficit in most of the other disorders. Admittedly, these extrapolated predictions are highly provisional since they are based on a very small dataset; they should be viewed primarily from the standpoint of encouraging larger studies. However, two points follow from our observations. First, Bernard et al. [89] demonstrated in a normal rat model that early life seizures reduce dendritic FMRP at/near synapses, with a corresponding shift of FMRP to the neuronal soma, despite an apparent increase in overall hippocampal FMRP [90]. Thus, the occurrence of early-life seizure creates a functional deficit of FMRP for synaptic functioning in the rat, with the corresponding reduction of cognitive function. For a normal child, a single seizure is not likely to substantially reduce cognitive strength, though in wildtype mice, single seizures have been demonstrated to affect long-term cognitive outcomes [91]; however, for a child whose FMRP levels are already low, early-life seizures could have a profound effect on cognitive function, underscoring the need for aggressive treatment of seizure activity in a child with fragile X syndrome or PM involvement. The second, broader implication of the current study concerns the reports of reduced levels of FMRP in individuals with major psychiatric disorders, where FMRP levels down to ~25% of normal have been observed in individuals with schizophrenia [73, 74]. The critical question for this latter instance is whether intrinsically low FMRP levels predispose to major psychiatric disorders or whether the processes involved with those disorders drive a reduction in FMRP. Resolution of this issue will have important ramifications for treatment of both psychiatric disorders and for fragile X syndrome.
In one of the most comprehensive analysis of the association between FMRP and IQ (derived from the Wechsler scales) in 290 individuals with full or PM alleles, Loesch et al. [92] utilized the immunocytochemical staining method of Willemsen et al. [59], which uses the fraction of lymphocytes staining positive for FMRP as a surrogate measure for relative FMRP concentration. As noted by Willemsen et al. [59], whereas this approach is useful for distinguishing individuals with FXS who do not produce FMRP from those with FMRP levels in the normal range (cf. Fig 1B of [92]), the staining method does not measure relative FMRP levels per se. Not surprisingly, therefore, Loesch et al. [92] observed a very large variance in the percent of FMRP-positive cells at all IQ levels, ranging from approximately 0–55% at IQ = 40 to 50–95% at IQ = 100, which diminished the portion of the variance that could be attributed to a dependence of cognitive measures on FMRP. Many FM alleles reported in this and previous studies are likely to be cryptic mosaics [58], where broad distributions of alleles may remain undetected, but which in aggregate would contribute to FMRP production.
Several limitations are inherent in the current study, foremost among them being the relatively small size of the sample cohort. While we believe that the general conclusions regarding the relationship between FMRP and IQ are sound, our observations and interpretations underscore the need for much larger sample cohorts. In this regard, because individuals were recruited through ongoing studies of families with fragile X syndrome and associated disorders, there is always the possibility of unrecognized bias both in the subjects with fragile X PM and FM alleles, and also in terms of the characteristics of controls, some of whom are unaffected (normal FMR1 gene) family members. We note in this regard that mean IQ values for the normal controls are generally well above 100. Due to the retrospective nature of the study and wide age range of participants, data from several different IQ tests were used. Although these tests utilize the same scoring metric for standardization (mean = 100, SD = 15) and measure general intelligence, they vary in their coverage of subdomains of intelligence and rely on different normative samples, and therefore systematic bias in scores is possible across tests. This bias may have introduced some unwanted error in our analyses. Studies utilizing the same test across all participants would likely yield stronger correlations between FMRP and IQ scores.
Also, given that the heritability of intelligence in the general population is as high as 80% [93], an important limitation of this and other studies examining the association between FMRP and IQ is that they have generally not accounted for factors such as parental IQ or shared environmental factors. For example, while a person with modest but significant reduction in FMRP may have an IQ in the broad normal range, this level of cognitive function may be very substantially below what is expected based on mean parental IQ [42]. Dyer-Friedman et al. [94] demonstrated that mean parental IQ was significantly associated with offspring IQ in both normal siblings and females with the FM but not in males with the FM, possibly indicating that the background environmental and genetic effects on IQ are stronger among those with less severe deficits and more variable FMRP levels. Thus, future studies seeking to obtain better estimates of the effects of the FMRP deficit should account for these shared factors if possible.
Another fundamental limitation of the current work, as with many other studies of CNS-based phenotypes (e.g., the relationship between IQ and brain FMRP levels), is the necessity of using a peripheral measure of relative FMRP level (normalized to mean FMRP among those with normal CGG repeats) as a surrogate for the brain relative FMRP level. This approach is based on the lack of accessibility of the CNS measures and thus assumes that the relative peripheral and brain FMRP levels have the same dependence on CGG repeat, and that the CGG repeat and methylation status are comparable in peripheral and brain tissues; this latter assumption is the basis for clinical testing for fragile X-associated disorders and is likely to be generally but not universally true. One approach to evaluate the validity of this assumption is to assess the magnitude of the residuals for IQ as a function of relative FMRP level. For FMRP levels that are greater than -1 SD (Fig 2), the IQ distribution becomes independent of FMRP level, and the residuals thus depend on other factors (e.g., background gene effects, environmental factors); however, for further decreases in FMRP below -1 SD, where IQ is strongly dependent on FMRP level, substantial differences in peripheral and brain FMRP levels would be expected to result in larger IQ residuals. We have analyzed this issue by plotting the residuals (S4 Fig) as a function of FMRP, demonstrating that there is no evidence of an increase in the residuals for IQ. This observation suggests that, at least as a first approximation, the use of peripheral FMRP measures to gauge IQ is reasonable.
Finally, the potential implications we describe regarding whether therapeutically driven changes in FMRP may or may not contribute to cognitive changes at different levels of FMRP expression are based upon cross-sectional data; longitudinal data collected from individuals over time would be needed to test the validity of these interpretations.
Supporting information
FMRP levels are normalized to the groupwise mean FMRP level for fibroblasts with normal CGG repeats (designated FMRP norm,ctrl).
(TIF)
Western blot analysis of the expression of FMRP in fibroblast lines from male patients with a control allele (Control), control allele with a point mutation (Point), or FM allele (Full). The control sample is the fiducial used for FRET plates in this study. The point mutation sample is 1016–15.
(TIF)
Females: (A) FSIQ, (B) PIQ, and (C) VIQ; Males: (D) FSIQ, (E) PIQ, and (F) VIQ. IQs were determined using age-appropriate instruments as delineated in the Methods section. FMRP levels were determined using FRET. All FMRP levels were normalized to the mean value of FMRP levels (= 1.0) among individuals with normal CGG repeats (<45 CGG repeats), excluding the FMR1 point mutation (1016–15). Symbols specify allele classes as indicated. Plus/minus 1 SD for FMRP levels are indicated as red vertical dashed lines. Lower limit of normal IQ (= 85) and borderline IQ (= 70) indicated as horizontal blue and green dashed lines, respectively. The FMRP level at which the regression line for IQ passes 85 is indicated by a vertical (blue) dashed line.
(TIF)
(A) Males only; (B) both males and females.
(TIF)
(DOCX)
(DOCX)
Western blot analysis of the expression of FMRP in fibroblast lines from male patients with a control allele (Control), control allele with a point mutation (Point), or FM allele (Full). The control sample is the fiducial used for FRET plates in this study. The point mutation sample is 1016–15. Unused wells are marked with an “X”. Raw image was captured using Near-infrared (NIR) fluorescence on LI-COR Odyssey (800 nm channel).
(TIF)
Acknowledgments
This study was partially supported by NICHD R01 HD036071 (RH), the Azrieli Foundation (PJH and RJH), and the MIND Institute Intellectual and Developmental Disabilities Research Center U54 HD079125 (KK). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Data Availability
All relevant data will be published as supporting information.
Funding Statement
This study was partially supported by NICHD HD036071 (RJH), the Azrieli Foundation (PJH and RJH), and the MIND Institute Intellectual and Developmental Disabilities Research Center U54 HD079125 (KK). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Hagerman RJ, Berry-Kravis E, Hazlett HC, Bailey DB Jr., Moine H, Kooy RF, et al. Fragile X syndrome. Nat Rev Dis Primers. 2017;3:17065 Epub 2017/09/30. 10.1038/nrdp.2017.65 [DOI] [PubMed] [Google Scholar]
- 2.Mila M, Alvarez-Mora MI, Madrigal I, Rodriguez-Revenga L. Fragile X syndrome: An overview and update of the FMR1 gene. Clin Genet. 2018;93(2):197–205. Epub 2017/06/16. 10.1111/cge.13075 [DOI] [PubMed] [Google Scholar]
- 3.Hagerman RJ, Protic D, Rajaratnam A, Salcedo-Arellano MJ, Aydin EY, Schneider A. Fragile X-Associated Neuropsychiatric Disorders (FXAND). Front Psychiatry. 2018;9:564 10.3389/fpsyt.2018.00564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramirez-Cheyne JA, Duque GA, Ayala-Zapata S, Saldarriaga-Gil W, Hagerman P, Hagerman R, et al. Fragile X syndrome and connective tissue dysregulation. Clin Genet. 2019;95(2):262–7. Epub 2018/11/11. 10.1111/cge.13469 [DOI] [PubMed] [Google Scholar]
- 5.Pieretti M, Zhang FP, Fu YH, Warren ST, Oostra BA, Caskey CT, et al. Absence of expression of the FMR-1 gene in fragile X syndrome. Cell. 1991;66(4):817–22. Epub 1991/08/23. 10.1016/0092-8674(91)90125-i [DOI] [PubMed] [Google Scholar]
- 6.Sutcliffe JS, Nelson DL, Zhang F, Pieretti M, Caskey CT, Saxe D, et al. DNA methylation represses FMR-1 transcription in fragile X syndrome. Hum Mol Genet. 1992;1(6):397–400. Epub 1992/09/01. 10.1093/hmg/1.6.397 [DOI] [PubMed] [Google Scholar]
- 7.Devys D, Biancalana V, Rousseau F, Boue J, Mandel JL, Oberle I. Analysis of full fragile X mutations in fetal tissues and monozygotic twins indicate that abnormal methylation and somatic heterogeneity are established early in development. Am J Med Genet. 1992;43(1–2):208–16. Epub 1992/04/01. 10.1002/ajmg.1320430134 [DOI] [PubMed] [Google Scholar]
- 8.Feng Y, Zhang F, Lokey LK, Chastain JL, Lakkis L, Eberhart D, et al. Translational suppression by trinucleotide repeat expansion at FMR1. Science. 1995;268(5211):731–4. Epub 1995/05/05. 10.1126/science.7732383 [DOI] [PubMed] [Google Scholar]
- 9.Schaeffer C, Bardoni B, Mandel JL, Ehresmann B, Ehresmann C, Moine H. The fragile X mental retardation protein binds specifically to its mRNA via a purine quartet motif. EMBO J. 2001;20(17):4803–13. Epub 2001/09/05. 10.1093/emboj/20.17.4803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brown V, Jin P, Ceman S, Darnell JC, O'Donnell WT, Tenenbaum SA, et al. Microarray identification of FMRP-associated brain mRNAs and altered mRNA translational profiles in fragile X syndrome. Cell. 2001;107(4):477–87. 10.1016/s0092-8674(01)00568-2 [DOI] [PubMed] [Google Scholar]
- 11.Darnell JC, Van Driesche SJ, Zhang C, Hung KY, Mele A, Fraser CE, et al. FMRP stalls ribosomal translocation on mRNAs linked to synaptic function and autism. Cell. 2011;146(2):247–61. 10.1016/j.cell.2011.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maurin T, Lebrigand K, Castagnola S, Paquet A, Jarjat M, Popa A, et al. HITS-CLIP in various brain areas reveals new targets and new modalities of RNA binding by fragile X mental retardation protein. Nucleic Acids Res. 2018;46(12):6344–55. Epub 2018/04/19. 10.1093/nar/gky267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Suhl JA, Chopra P, Anderson BR, Bassell GJ, Warren ST. Analysis of FMRP mRNA target datasets reveals highly associated mRNAs mediated by G-quadruplex structures formed via clustered WGGA sequences. Hum Mol Genet. 2014;23(20):5479–91. Epub 2014/05/31. 10.1093/hmg/ddu272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Siomi H, Siomi M, Nussbaum R, Dreyfuss G. The protein product of the fragile X gene, FMR1, has characteristics of an RNA-binding protein. Cell. 1993;74(2):291–8. Epub 1993/07/30. 10.1016/0092-8674(93)90420-u [DOI] [PubMed] [Google Scholar]
- 15.Bardoni B, Schenck A, Mandel JL. The Fragile X mental retardation protein. Brain Res Bull. 2001;56(3–4):375–82. Epub 2001/11/24. 10.1016/s0361-9230(01)00647-5 [DOI] [PubMed] [Google Scholar]
- 16.Zalfa F, Eleuteri B, Dickson KS, Mercaldo V, De Rubeis S, di Penta A, et al. A new function for the fragile X mental retardation protein in regulation of PSD-95 mRNA stability. Nat Neurosci. 2007;10(5):578–87. Epub 2007/04/10. 10.1038/nn1893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ascano M Jr., Mukherjee N, Bandaru P, Miller JB, Nusbaum JD, Corcoran DL, et al. FMRP targets distinct mRNA sequence elements to regulate protein expression. Nature. 2012;492(7429):382–6. Epub 2012/12/14. 10.1038/nature11737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fernandez E, Rajan N, Bagni C. The FMRP regulon: from targets to disease convergence. Front Neurosci. 2013;7:191 Epub 2013/10/30. 10.3389/fnins.2013.00191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kenny P, Ceman S. RNA Secondary Structure Modulates FMRP's Bi-Functional Role in the MicroRNA Pathway. Int J Mol Sci. 2016;17(6). 10.3390/ijms17060985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sears JC, Broadie K. Fragile X Mental Retardation Protein Regulates Activity-Dependent Membrane Trafficking and Trans-Synaptic Signaling Mediating Synaptic Remodeling. Front Mol Neurosci. 2017;10:440 10.3389/fnmol.2017.00440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Banerjee A, Ifrim MF, Valdez AN, Raj N, Bassell GJ. Aberrant RNA translation in fragile X syndrome: From FMRP mechanisms to emerging therapeutic strategies. Brain Res. 2018;1693(Pt A):24–36. 10.1016/j.brainres.2018.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.D'Annessa I, Cicconardi F, Di Marino D. Handling FMRP and its molecular partners: Structural insights into Fragile X Syndrome. Prog Biophys Mol Biol. 2019;141:3–14. 10.1016/j.pbiomolbio.2018.07.001 [DOI] [PubMed] [Google Scholar]
- 23.Leboucher A, Pisani DF, Martinez-Gili L, Chilloux J, Bermudez-Martin P, Van Dijck A, et al. The translational regulator FMRP controls lipid and glucose metabolism in mice and humans. Mol Metab. 2019;21:22–35. 10.1016/j.molmet.2019.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alpatov R, Lesch BJ, Nakamoto-Kinoshita M, Blanco A, Chen S, Stutzer A, et al. A chromatin-dependent role of the fragile X mental retardation protein FMRP in the DNA damage response. Cell. 2014;157(4):869–81. Epub 2014/05/13. 10.1016/j.cell.2014.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dockendorff TC, Labrador M. The Fragile X Protein and Genome Function. Mol Neurobiol. 2019;56(1):711–21. Epub 2018/05/26. 10.1007/s12035-018-1122-9 [DOI] [PubMed] [Google Scholar]
- 26.Contractor A, Klyachko VA, Portera-Cailliau C. Altered Neuronal and Circuit Excitability in Fragile X Syndrome. Neuron. 2015;87(4):699–715. Epub 2015/08/21. 10.1016/j.neuron.2015.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ferron L. Fragile X mental retardation protein controls ion channel expression and activity. J Physiol. 2016;594(20):5861–7. Epub 2016/02/13. 10.1113/JP270675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Castagnola S, Delhaye S, Folci A, Paquet A, Brau F, Duprat F, et al. New Insights Into the Role of Cav2 Protein Family in Calcium Flux Deregulation in Fmr1-KO Neurons. Front Mol Neurosci. 2018;11:342 Epub 2018/10/16. 10.3389/fnmol.2018.00342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hessl D, Rivera SM, Reiss AL. The neuroanatomy and neuroendocrinology of fragile X syndrome. Ment Retard Dev Disabil Res Rev. 2004;10(1):17–24. Epub 2004/03/03. 10.1002/mrdd.20004 [DOI] [PubMed] [Google Scholar]
- 30.Gothelf D, Furfaro JA, Hoeft F, Eckert MA, Hall SS, O'Hara R, et al. Neuroanatomy of fragile X syndrome is associated with aberrant behavior and the fragile X mental retardation protein (FMRP). Ann Neurol. 2008;63(1):40–51. Epub 2007/10/13. 10.1002/ana.21243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Swanson MR, Wolff JJ, Shen MD, Styner M, Estes A, Gerig G, et al. Development of White Matter Circuitry in Infants With Fragile X Syndrome. JAMA psychiatry. 2018;75(5):505–13. Epub 2018/04/05. 10.1001/jamapsychiatry.2018.0180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tassone F, Hagerman RJ, Taylor AK, Gane LW, Godfrey TE, Hagerman PJ. Elevated levels of FMR1 mRNA in carrier males: a new mechanism of involvement in the fragile-X syndrome. Am J Hum Genet. 2000;66(1):6–15. Epub 2000/01/13. 10.1086/302720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kenneson A, Zhang F, Hagedorn CH, Warren ST. Reduced FMRP and increased FMR1 transcription is proportionally associated with CGG repeat number in intermediate-length and premutation carriers. Hum Mol Genet. 2001;10(14):1449–54. Epub 2001/07/13. 10.1093/hmg/10.14.1449 [DOI] [PubMed] [Google Scholar]
- 34.Ludwig AL, Espinal GM, Pretto DI, Jamal AL, Arque G, Tassone F, et al. CNS expression of murine fragile X protein (FMRP) as a function of CGG-repeat size. Hum Mol Genet. 2014;23(12):3228–38. Epub 2014/01/28. 10.1093/hmg/ddu032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pretto DI, Mendoza-Morales G, Lo J, Cao R, Hadd A, Latham GJ, et al. CGG allele size somatic mosaicism and methylation in FMR1 premutation alleles. J Med Genet. 2014;51(5):309–18. Epub 2014/03/05. 10.1136/jmedgenet-2013-102021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wheeler A, Raspa M, Hagerman R, Mailick M, Riley C. Implications of the FMR1 Premutation for Children, Adolescents, Adults, and Their Families. Pediatrics. 2017;139(Suppl 3):S172–S82. Epub 2017/08/18. 10.1542/peds.2016-1159D [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chonchaiya W, Au J, Schneider A, Hessl D, Harris SW, Laird M, et al. Increased prevalence of seizures in boys who were probands with the FMR1 premutation and co-morbid autism spectrum disorder. Hum Genet. 2012;131(4):581–9. Epub 2011/10/18. 10.1007/s00439-011-1106-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tassone F, Hagerman RJ, Loesch DZ, Lachiewicz A, Taylor AK, Hagerman PJ. Fragile X males with unmethylated, full mutation trinucleotide repeat expansions have elevated levels of FMR1 messenger RNA. Am J Med Genet. 2000;94(3):232–6. Epub 2000/09/20. [DOI] [PubMed] [Google Scholar]
- 39.Tassone F, Hagerman RJ, Taylor AK, Hagerman PJ. A majority of fragile X males with methylated, full mutation alleles have significant levels of FMR1 messenger RNA. J Med Genet. 2001;38(7):453–6. Epub 2001/07/04. 10.1136/jmg.38.7.453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Verheij C, de Graaff E, Bakker CE, Willemsen R, Willems PJ, Meijer N, et al. Characterization of FMR1 proteins isolated from different tissues. Hum Mol Genet. 1995;4(5):895–901. Epub 1995/05/01. 10.1093/hmg/4.5.895 [DOI] [PubMed] [Google Scholar]
- 41.Devys D, Lutz Y, Rouyer N, Bellocq JP, Mandel JL. The FMR-1 protein is cytoplasmic, most abundant in neurons and appears normal in carriers of a fragile X premutation. Nat Genet. 1993;4(4):335–40. 10.1038/ng0893-335 [DOI] [PubMed] [Google Scholar]
- 42.Kaufmann WE, Abrams MT, Chen W, Reiss AL. Genotype, molecular phenotype, and cognitive phenotype: correlations in fragile X syndrome. Am J Med Genet. 1999;83(4):286–95. Epub 1999/04/20. [PubMed] [Google Scholar]
- 43.Pretto D, Yrigollen CM, Tang HT, Williamson J, Espinal G, Iwahashi CK, et al. Clinical and molecular implications of mosaicism in FMR1 full mutations. Front Genet. 2014;5:318 Epub 2014/10/04. 10.3389/fgene.2014.00318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McConkie-Rosell A, Lachiewicz AM, Spiridigliozzi GA, Tarleton J, Schoenwald S, Phelan MC, et al. Evidence that methylation of the FMR-I locus is responsible for variable phenotypic expression of the fragile X syndrome. Am J Hum Genet. 1993;53(4):800–9. Epub 1993/10/01. [PMC free article] [PubMed] [Google Scholar]
- 45.Loesch DZ, Huggins RM, Bui QM, Taylor AK, Pratt C, Epstein J, et al. Effect of fragile X status categories and FMRP deficits on cognitive profiles estimated by robust pedigree analysis. Am J Med Genet A. 2003;122A(1):13–23. 10.1002/ajmg.a.20214 [DOI] [PubMed] [Google Scholar]
- 46.Merenstein SA, Shyu V, Sobesky WE, Staley L, Berry-Kravis E, Nelson DL, et al. Fragile X syndrome in a normal IQ male with learning and emotional problems. J Am Acad Child Adolesc Psychiatry. 1994;33(9):1316–21. 10.1097/00004583-199411000-00014 [DOI] [PubMed] [Google Scholar]
- 47.Hagerman RJ, Hull CE, Safanda JF, Carpenter I, Staley LW, O'Connor RA, et al. High functioning fragile X males: demonstration of an unmethylated fully expanded FMR-1 mutation associated with protein expression. Am J Med Genet. 1994;51(4):298–308. Epub 1994/07/15. 10.1002/ajmg.1320510404 [DOI] [PubMed] [Google Scholar]
- 48.Rousseau F, Robb LJ, Rouillard P, Der Kaloustian VM. No mental retardation in a man with 40% abnormal methylation at the FMR-1 locus and transmission of sperm cell mutations as premutations. Hum Mol Genet. 1994;3(6):927–30. Epub 1994/06/01. 10.1093/hmg/3.6.927 [DOI] [PubMed] [Google Scholar]
- 49.Smeets HJ, Smits AP, Verheij CE, Theelen JP, Willemsen R, van de Burgt I, et al. Normal phenotype in two brothers with a full FMR1 mutation. Hum Mol Genet. 1995;4(11):2103–8. 10.1093/hmg/4.11.2103 [DOI] [PubMed] [Google Scholar]
- 50.Lachiewicz AM, Spiridigliozzi GA, McConkie-Rosell A, Burgess D, Feng Y, Warren ST, et al. A fragile X male with a broad smear on Southern blot analysis representing 100–500 CGG repeats and no methylation at the EagI site of the FMR-1 gene. Am J Med Genet. 1996;64(2):278–82. [DOI] [PubMed] [Google Scholar]
- 51.Steyaert J, Borghgraef M, Legius E, Fryns JP. Molecular-intelligence correlations in young fragile X males with a mild CGG repeat expansion in the FMR1 gene. Am J Med Genet. 1996;64(2):274–7. [DOI] [PubMed] [Google Scholar]
- 52.Wang Z, Taylor AK, Bridge JA. FMR1 fully expanded mutation with minimal methylation in a high functioning fragile X male. J Med Genet. 1996;33(5):376–8. Epub 1996/05/01. 10.1136/jmg.33.5.376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wöhrle D, Salat U, Gläser D, Mücke J, Meisel-Stosiek M, Schindler D, et al. Unusual mutations in high functioning fragile X males: apparent instability of expanded unmethylated CGG repeats. J Med Genet. 1998;35(2):103–11. Epub 1998/03/21. 10.1136/jmg.35.2.103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Winarni TI, Schneider A, Borodyanskara M, Hagerman RJ. Early intervention combined with targeted treatment promotes cognitive and behavioral improvements in young children with fragile x syndrome. Case Rep Genet. 2012;2012:280813 Epub 2012/10/18. 10.1155/2012/280813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chen L, Hadd A, Sah S, Filipovic-Sadic S, Krosting J, Sekinger E, et al. An information-rich CGG repeat primed PCR that detects the full range of fragile X expanded alleles and minimizes the need for southern blot analysis. J Mol Diagn. 2010;12(5):589–600. Epub 2010/07/10. 10.2353/jmoldx.2010.090227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Filipovic-Sadic S, Sah S, Chen L, Krosting J, Sekinger E, Zhang W, et al. A novel FMR1 PCR method for the routine detection of low abundance expanded alleles and full mutations in fragile X syndrome. Clin Chem. 2010;56(3):399–408. Epub 2010/01/09. 10.1373/clinchem.2009.136101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yrigollen CM, Martorell L, Durbin-Johnson B, Naudo M, Genoves J, Murgia A, et al. AGG interruptions and maternal age affect FMR1 CGG repeat allele stability during transmission. J Neurodev Disord. 2014;6(1):24 Epub 2014/08/12. 10.1186/1866-1955-6-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jiraanont P, Kumar M, Tang HT, Espinal G, Hagerman PJ, Hagerman RJ, et al. Size and methylation mosaicism in males with Fragile X syndrome. Expert Rev Mol Diagn. 2017;17(11):1023–32. 10.1080/14737159.2017.1377612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Willemsen R, Mohkamsing S, de Vries B, Devys D, van den Ouweland A, Mandel JL, et al. Rapid antibody test for fragile X syndrome. Lancet. 1995;345(8958):1147–8. 10.1016/s0140-6736(95)90979-6 [DOI] [PubMed] [Google Scholar]
- 60.Chiurazzi P, Pomponi MG, Pietrobono R, Bakker CE, Neri G, Oostra BA. Synergistic effect of histone hyperacetylation and DNA demethylation in the reactivation of the FMR1 gene. Hum Mol Genet. 1999;8(12):2317–23. 10.1093/hmg/8.12.2317 [DOI] [PubMed] [Google Scholar]
- 61.Chiurazzi P, Neri G. Pharmacological reactivation of inactive genes: the fragile X experience. Brain Res Bull. 2001;56(3–4):383–7. Epub 2001/11/24. 10.1016/s0361-9230(01)00571-8 [DOI] [PubMed] [Google Scholar]
- 62.Pietrobono R, Pomponi MG, Tabolacci E, Oostra B, Chiurazzi P, Neri G. Quantitative analysis of DNA demethylation and transcriptional reactivation of the FMR1 gene in fragile X cells treated with 5-azadeoxycytidine. Nucleic Acids Res. 2002;30(14):3278–85. Epub 2002/07/24. 10.1093/nar/gkf434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tabolacci E, De Pascalis I, Accadia M, Terracciano A, Moscato U, Chiurazzi P, et al. Modest reactivation of the mutant FMR1 gene by valproic acid is accompanied by histone modifications but not DNA demethylation. Pharmacogenet Genomics. 2008;18(8):738–41. Epub 2008/07/16. 10.1097/FPC.0b013e32830500a1 [DOI] [PubMed] [Google Scholar]
- 64.Bar-Nur O, Caspi I, Benvenisty N. Molecular analysis of FMR1 reactivation in fragile-X induced pluripotent stem cells and their neuronal derivatives. Journal of molecular cell biology. 2012;4(3):180–3. 10.1093/jmcb/mjs007 [DOI] [PubMed] [Google Scholar]
- 65.Tabolacci E, Palumbo F, Nobile V, Neri G. Transcriptional Reactivation of the FMR1 Gene. A Possible Approach to the Treatment of the Fragile X Syndrome. Genes. 2016;7(8). 10.3390/genes7080049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Xie N, Gong H, Suhl JA, Chopra P, Wang T, Warren ST. Reactivation of FMR1 by CRISPR/Cas9-Mediated Deletion of the Expanded CGG-Repeat of the Fragile X Chromosome. PLoS One. 2016;11(10):e0165499 10.1371/journal.pone.0165499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Li M, Zhao H, Ananiev GE, Musser MT, Ness KH, Maglaque DL, et al. Establishment of Reporter Lines for Detecting Fragile X Mental Retardation (FMR1) Gene Reactivation in Human Neural Cells. Stem Cells. 2017;35(1):158–69. Epub 2016/07/17. 10.1002/stem.2463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Haenfler JM, Skariah G, Rodriguez CM, Monteiro da Rocha A, Parent JM, Smith GD, et al. Targeted Reactivation of FMR1 Transcription in Fragile X Syndrome Embryonic Stem Cells. Front Mol Neurosci. 2018;11:282 10.3389/fnmol.2018.00282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kumari D, Gazy I, Usdin K. Pharmacological Reactivation of the Silenced FMR1 Gene as a Targeted Therapeutic Approach for Fragile X Syndrome. Brain Sciences. 2019;9(2). Epub 2019/02/15. 10.3390/brainsci9020039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Fatemi SH, Folsom TD. The role of fragile X mental retardation protein in major mental disorders. Neuropharmacology. 2011;60(7–8):1221–6. Epub 2010/11/27. 10.1016/j.neuropharm.2010.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fatemi SH, Folsom TD, Kneeland RE, Liesch SB. Metabotropic glutamate receptor 5 upregulation in children with autism is associated with underexpression of both Fragile X mental retardation protein and GABAA receptor beta 3 in adults with autism. Anatomical record (Hoboken, NJ: 2007). 2011;294(10):1635–45. Epub 2011/09/09. 10.1002/ar.21299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wegiel J, Brown WT, La Fauci G, Adayev T, Kascsak R, Kascsak R, et al. The role of reduced expression of fragile X mental retardation protein in neurons and increased expression in astrocytes in idiopathic and syndromic autism (duplications 15q11.2-q13). Autism Res. 2018;11(10):1316–31. Epub 2018/08/15. 10.1002/aur.2003 [DOI] [PubMed] [Google Scholar]
- 73.Fatemi SH, Kneeland RE, Liesch SB, Folsom TD. Fragile X mental retardation protein levels are decreased in major psychiatric disorders. Schizophr Res. 2010;124(1–3):246–7. Epub 2010/08/24. 10.1016/j.schres.2010.07.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kovacs T, Kelemen O, Keri S. Decreased fragile X mental retardation protein (FMRP) is associated with lower IQ and earlier illness onset in patients with schizophrenia. Psychiatry Res. 2013;210(3):690–3. Epub 2013/01/22. 10.1016/j.psychres.2012.12.022 [DOI] [PubMed] [Google Scholar]
- 75.Iwahashi C, Tassone F, Hagerman RJ, Yasui D, Parrott G, Nguyen D, et al. A quantitative ELISA assay for the fragile X mental retardation 1 protein. J Mol Diagn. 2009;11(4):281–9. Epub 2009/05/23. 10.2353/jmoldx.2009.080118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Iwahashi CK, Yasui DH, An HJ, Greco CM, Tassone F, Nannen K, et al. Protein composition of the intranuclear inclusions of FXTAS. Brain. 2006;129(Pt 1):256–71. Epub 2005/10/26. 10.1093/brain/awh650 [DOI] [PubMed] [Google Scholar]
- 77.Lessard M, Chouiali A, Drouin R, Sebire G, Corbin F. Quantitative measurement of FMRP in blood platelets as a new screening test for fragile X syndrome. Clin Genet. 2012;82(5):472–7. Epub 2011/10/14. 10.1111/j.1399-0004.2011.01798.x [DOI] [PubMed] [Google Scholar]
- 78.LaFauci G, Adayev T, Kascsak R, Kascsak R, Nolin S, Mehta P, et al. Fragile X screening by quantification of FMRP in dried blood spots by a Luminex immunoassay. J Mol Diagn. 2013;15(4):508–17. Epub 2013/05/11. 10.1016/j.jmoldx.2013.02.006 [DOI] [PubMed] [Google Scholar]
- 79.Schutzius G, Bleckmann D, Kapps-Fouthier S, di Giorgio F, Gerhartz B, Weiss A. A quantitative homogeneous assay for fragile X mental retardation 1 protein. J Neurodev Disord. 2013;5(1):8 Epub 2013/04/04. 10.1186/1866-1955-5-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sitzmann AF, Hagelstrom RT, Tassone F, Hagerman RJ, Butler MG. Rare FMR1 gene mutations causing fragile X syndrome: A review. Am J Med Genet A. 2018;176(1):11–8. 10.1002/ajmg.a.38504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sansone SM, Schneider A, Bickel E, Berry-Kravis E, Prescott C, Hessl D. Improving IQ measurement in intellectual disabilities using true deviation from population norms. J Neurodev Disord. 2014;6(1):16 Epub 2014/01/01. 10.1186/1866-1955-6-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hessl D, Nguyen DV, Green C, Chavez A, Tassone F, Hagerman RJ, et al. A solution to limitations of cognitive testing in children with intellectual disabilities: the case of fragile X syndrome. J Neurodevelop Disord. 2009;1(1):33–45. Epub 2009/10/30. 10.1007/s11689-008-9001-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kumari D, Swaroop M, Southall N, Huang W, Zheng W, Usdin K. High-Throughput Screening to Identify Compounds That Increase Fragile X Mental Retardation Protein Expression in Neural Stem Cells Differentiated From Fragile X Syndrome Patient-Derived Induced Pluripotent Stem Cells. Stem Cells Transl Med. 2015;4(7):800–8. 10.5966/sctm.2014-0278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Cleveland WS. Robust Locally Weighted Regression and Smoothing Scatterplots. J Am Stat Assoc. 1979;74(368):829–36. 10.1080/01621459.1979.10481038 [DOI] [Google Scholar]
- 85.Arsenault J, Gholizadeh S, Niibori Y, Pacey LK, Halder SK, Koxhioni E, et al. FMRP Expression Levels in Mouse Central Nervous System Neurons Determine Behavioral Phenotype. Hum Gene Ther. 2016;27(12):982–96. Epub 2016/10/19. 10.1089/hum.2016.090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Peier AM, McIlwain KL, Kenneson A, Warren ST, Paylor R, Nelson DL. (Over)correction of FMR1 deficiency with YAC transgenics: behavioral and physical features. Hum Mol Genet. 2000;9(8):1145–59. Epub 2000/04/18. 10.1093/hmg/9.8.1145 [DOI] [PubMed] [Google Scholar]
- 87.Musumeci SA, Calabrese G, Bonaccorso CM, D'Antoni S, Brouwer JR, Bakker CE, et al. Audiogenic seizure susceptibility is reduced in fragile X knockout mice after introduction of FMR1 transgenes. Exp Neurol. 2007;203(1):233–40. Epub 2006/09/30. 10.1016/j.expneurol.2006.08.007 [DOI] [PubMed] [Google Scholar]
- 88.Gholizadeh S, Arsenault J, Xuan IC, Pacey LK, Hampson DR. Reduced phenotypic severity following adeno-associated virus-mediated Fmr1 gene delivery in fragile X mice. Neuropsychopharmacology. 2014;39(13):3100–11. Epub 2014/07/08. 10.1038/npp.2014.167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bernard PB, Castano AM, O'Leary H, Simpson K, Browning MD, Benke TA. Phosphorylation of FMRP and alterations of FMRP complex underlie enhanced mLTD in adult rats triggered by early life seizures. Neurobiol Dis. 2013;59:1–17. Epub 2013/07/09. 10.1016/j.nbd.2013.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Holley AJ, Hodges SL, Nolan SO, Binder M, Okoh JT, Ackerman K, et al. A single seizure selectively impairs hippocampal-dependent memory and is associated with alterations in PI3K/Akt/mTOR and FMRP signaling. Epilepsia Open. 2018;3(4):511–23. 10.1002/epi4.12273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hodges SL, Reynolds CD, Nolan SO, Huebschman JL, Okoh JT, Binder MS, et al. A single early-life seizure results in long-term behavioral changes in the adult Fmr1 knockout mouse. Epilepsy Res. 2019;157:106193 Epub 2019/09/15. 10.1016/j.eplepsyres.2019.106193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Loesch DZ, Huggins RM, Hagerman RJ. Phenotypic variation and FMRP levels in fragile X. Ment Retard Dev Disabil Res Rev. 2004;10(1):31–41. Epub 2004/03/03. 10.1002/mrdd.20006 [DOI] [PubMed] [Google Scholar]
- 93.Plomin R, Deary IJ. Genetics and intelligence differences: five special findings. Mol Psychiatry. 2015;20(1):98–108. Epub 2014/09/17. 10.1038/mp.2014.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Dyer-Friedman J, Glaser B, Hessl D, Johnston C, Huffman LC, Taylor A, et al. Genetic and environmental influences on the cognitive outcomes of children with fragile X syndrome. J Am Acad Child Adolesc Psychiatry. 2002;41(3):237–44. 10.1097/00004583-200203000-00002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
FMRP levels are normalized to the groupwise mean FMRP level for fibroblasts with normal CGG repeats (designated FMRP norm,ctrl).
(TIF)
Western blot analysis of the expression of FMRP in fibroblast lines from male patients with a control allele (Control), control allele with a point mutation (Point), or FM allele (Full). The control sample is the fiducial used for FRET plates in this study. The point mutation sample is 1016–15.
(TIF)
Females: (A) FSIQ, (B) PIQ, and (C) VIQ; Males: (D) FSIQ, (E) PIQ, and (F) VIQ. IQs were determined using age-appropriate instruments as delineated in the Methods section. FMRP levels were determined using FRET. All FMRP levels were normalized to the mean value of FMRP levels (= 1.0) among individuals with normal CGG repeats (<45 CGG repeats), excluding the FMR1 point mutation (1016–15). Symbols specify allele classes as indicated. Plus/minus 1 SD for FMRP levels are indicated as red vertical dashed lines. Lower limit of normal IQ (= 85) and borderline IQ (= 70) indicated as horizontal blue and green dashed lines, respectively. The FMRP level at which the regression line for IQ passes 85 is indicated by a vertical (blue) dashed line.
(TIF)
(A) Males only; (B) both males and females.
(TIF)
(DOCX)
(DOCX)
Western blot analysis of the expression of FMRP in fibroblast lines from male patients with a control allele (Control), control allele with a point mutation (Point), or FM allele (Full). The control sample is the fiducial used for FRET plates in this study. The point mutation sample is 1016–15. Unused wells are marked with an “X”. Raw image was captured using Near-infrared (NIR) fluorescence on LI-COR Odyssey (800 nm channel).
(TIF)
Data Availability Statement
All relevant data will be published as supporting information.