Abstract
Introduction and Objective
Robot-assisted radical cystectomy (RARC) with intracorporeal urinary diversion (ICUD) has become an increasingly utilized approach to treating various bladder pathologies requiring extirpation. As surgeons have become more experienced with ICUD, especially with lesser-used diversions such as continent cutaneous reservoirs, the technique has evolved.
Methods
We describe our technique and recent advances in the practical creation of robotic ICUD with a continent catheterizable pouch (CCP) built upon the open principles of the previously described “Indiana Pouch, ” which uses the distal ileum and right colon. Modifications in anatomic mobilization and exposure, bowel segmentation using novel robotic bowel staplers, catheterizable channel creation, and addition of ileal chimney for uretero-enteric anastomoses are highlighted. The addition of the ileal chimney allows for ease of reconstruction in a fashion familiar to surgeons accustomed to performing intracorporeal ileal conduit and, therefore, may result in lower ureteroenteric stricture rates. Table 1 demonstrates the supplies used intraoperatively. Use of indocyanine green to assess vascularity in bowel and ureter intraoperatively is demonstrated. The port configurations are demonstrated using the DaVinci ® Xi platform. Also described are short-term outcomes of our initial experience.
Results
Eleven consecutive patients (5 female) who have undergone ICUD with CCP were included. Of the eleven seven had malignant indications (bladder or urethral cancer) while 4 were for benign causes (2 radiation cystitis 2 interstitial cystitis). Mean blood loss was 235cc (range 100–500cc) and mean operative time was 8.5 h (range 7–13). There were no conversions to an open procedure and no patient required a blood transfusion. Hospital stay was 7.2 days on average (range 4–18) with no 30-day post-discharge readmissions. One patient had a Clavien grade 3 or greater complication at 30 days (Table 2). No urine leaks or bowel leaks were observed and no patien experienced stomal stenosis or uretero-enteric stenosis. At three months follow up, all patients were continent and satisfied with their diversion.
Conclusions
RARC with CCP ICUD is a safe and effective approach to bladder removal and reconstruction. As more surgeons utilize RARC, growing attention to techniques of intracorporeal reconstruction will allow further implementation of this technique to cystectomy patients. Patients with adequate renal function (glomerular filtration rate of 40 mL/min or greater) and hepatic function, who understand the requirement for regular clean intermittent-catheterization and who possess mental acuity and manual dexterity to empty their pouch 4–6 times daily should be offered CCP ICUD as a reconstructive option following RARC.
Keywords: Robotic continent cutaneous diversion, Robotic cystectomy, Bladder cancer
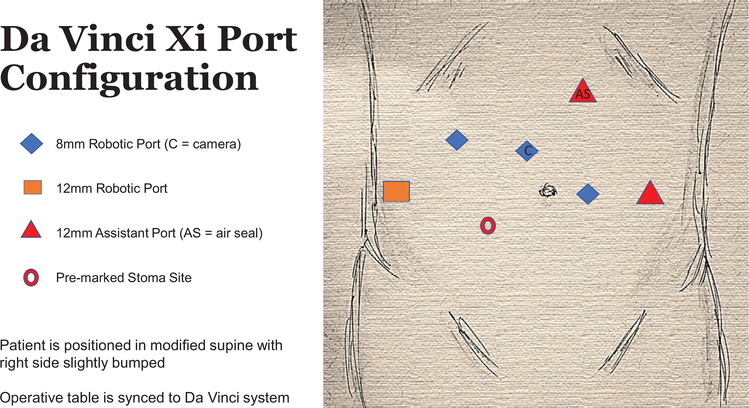
Fig. 1.
DaVinci Xi Port configuration.
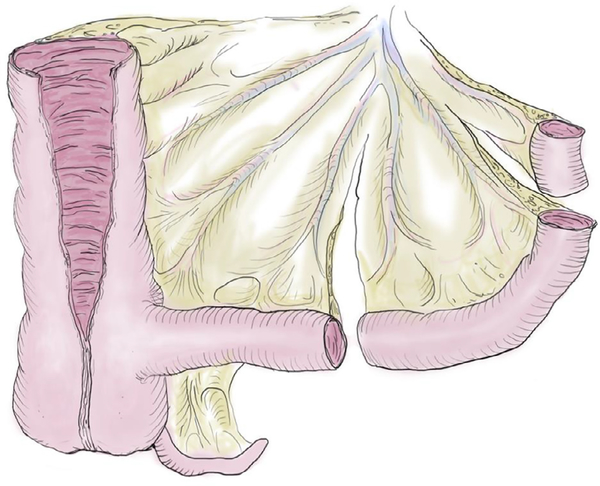
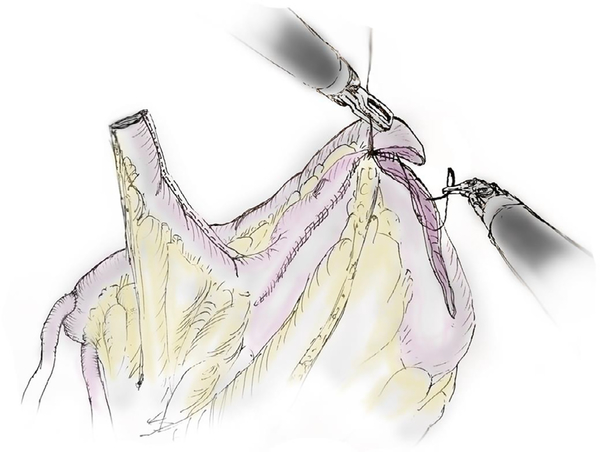
Fig. 9.
Final configuration of continent cutaneous diversion with addition of ileal chimney.
Table 1.
Supplies.
| Robotic instruments | Fenestrated bipolar graspers Monopolar scissors Vessel sealer Tip-up fenestrated grasper Endowrist stapler (45-mm or 60-mm bowel load) DeBakey forceps Potts scissors Large needle drivers Large clip (weck) applier |
| Ports | 8-mm robotic cannula (4) 12-mm assistant port 12-mm assistant port (air seal) 2-mm mini port; covidien |
| Staplers | 60-mm load (3.5 mm and 2.5 mm) |
| Sutures | Pre-marked 2–0 polyglactin for intracorporeal measuring 3–0 polyglactin SH 2–0 silk SH 4–0 polyglactin 2–0 stratafix poliglecaprone 0-polyglactin on CT1 0-polyglactin ties |
| Tubes | 7Fr ×90 cm single-J ureteral stents 22Fr rusch hematuria catheter 14Fr stomal catheter (capped) 19Fr bulb-suction drain |
| Additional | Carter–Thomason 12-mm endocatch bag10-mm endocatch bag |
Table 2.
Patient and operative characteristics.
| N = 11 | |
|---|---|
| Indication | Malignancy: 7 (64%) Radiation cystitis: 2 (18%) Interstitial cystitis: 2 (18%) |
| Female | 5 (45%) |
| Mean BMI | 25.4 |
| Mean EBL (mL) | 235 (range 100–500) |
| Mean operative time (h) | 8.5 (range 7–13) |
| Mean hospital length of stay (days) | 7.2 (range 4–18) |
| Open conversion | 0 (0%) |
| Continent at last follow-up | 11 (100%) |
| 30d readmissions | 1 (9%) |
| 30d major complications (Clavien–Dindo ≥ 3) | 1 (9%) |
Supplementary Material
Fig. 2.
Bowel segmentation. Approximately 30 cm of ascending colon is selected. A 10-cm segment of terminal ileum is measured for the catheterizable channel. The adjacent 10-cm segment is isolated for creation of the ileal chimney. A proximal 2–3 cm segment is excised and discarded to allow for separation of the ileocolonic anastomosis from the pouch.
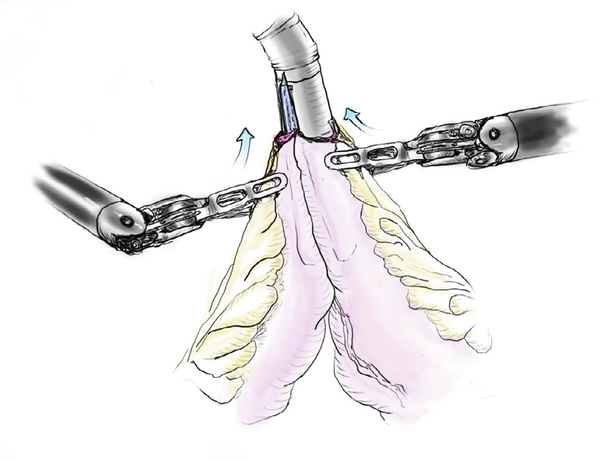
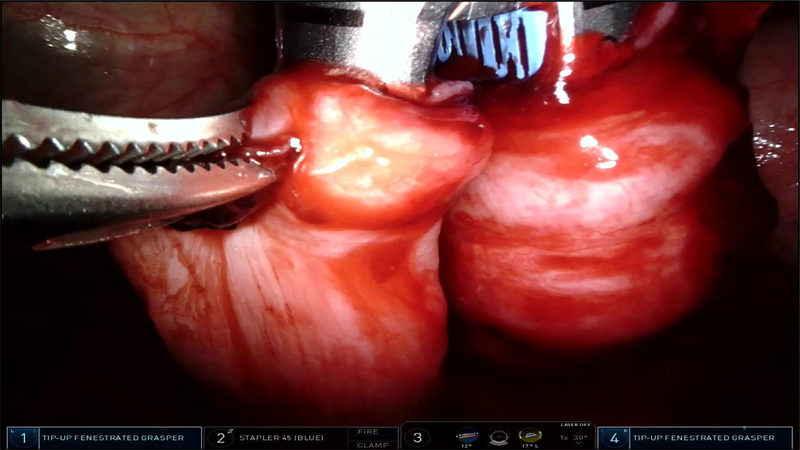
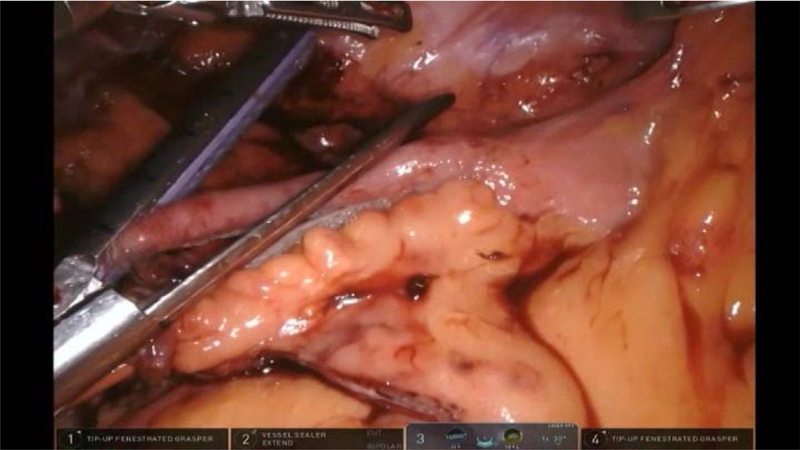
Fig. 3.
45-mm robotic stapler used to perform ileocolonic anastomosis.
Fig. 4.
45-mm robotic stapler used to perform ileocolonic anastomosis.
Fig. 5.
Tapering of efferent limb.
Fig. 6.
Use if Indocyanine Green to confirm vascularity of ureters prior to implantation.
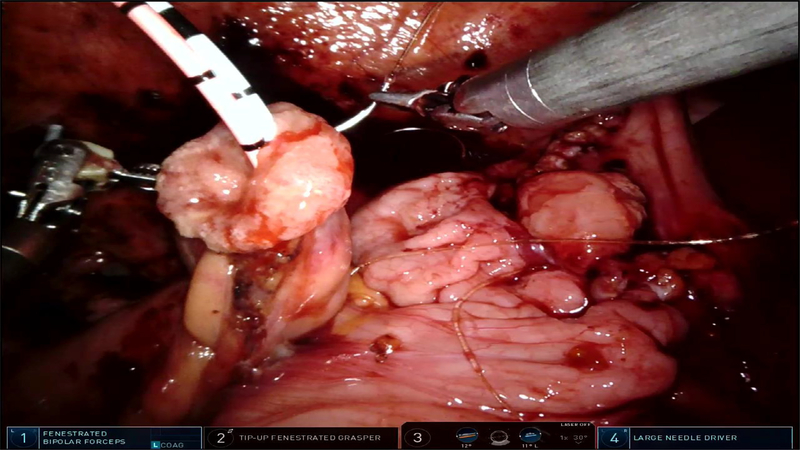
Fig. 7.
Securing afferent chimney to pouch.
Fig. 8.
Completing the pouch.
Acknowledgments
Funds
This research was supported in part by a Cancer Center Support Grant (P30-CA008748) from the National Institutes of Health/National Cancer Institute and the Sidney Kimmel Center for Prostate and Urologic Cancers.
Footnotes
Declartion of Competing Interest
None.
Supplementary material
The video related to this article can be found online at: doi: 10.1016/j.urolvj.2019.100020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.