Abstract
Patient: Male, 30-day-old
Final Diagnosis: Thoracoschisis
Symptoms: Respiratory distress
Medication: —
Clinical Procedure: —
Specialty: Surgery
Objective:
Congenital defects/diseases
Background:
Thoracoschisis is a very rare congenital birth defect defined by the herniation of intra-abdominal organs through a defect in the thoracic wall. Though often associated with other birth defects as a part of the “limb-body wall complex” deformities, thoracoschisis has very rarely been reported as an isolated finding.
Case Report:
Here we present the case of a 30-day-old term male infant with an isolated left thoracoschisis managed successfully by primary closure. The patient was monitored postnatally in the Neonatal Intensive Care Unit (NICU) of Maputo Central Hospital because of the presence of a herniated mass through a left chest wall defect below the left nipple. Computed tomography (CT) scans suggested the presence of a left diaphragmatic hernia, left rib agenesis, and herniation of an unidentifiable intra-abdominal organ through the anterior left chest wall. On day of life (DOL) 30, when global health outreach pediatric surgeons arrived at the hospital, the decision was made to operate on the child. The mass was found to be of liver origin, the exposed tissue was excised, and primary closure of the chest wall was accomplished. The patient’s postoperative course involved a wound infection that resolved favorably with treatment, allowing for discharged home on postoperative day (POD) 17 in stable condition.
Conclusions:
Our case report highlights the importance of recognizing this rare condition and directing appropriate surgical care.
MeSH Keywords: Congenital Abnormalities; Congenital, Hereditary, and Neonatal Diseases and Abnormalities; Hernia; Mass Chest X-Ray; Pediatrics
Background
Thoracoschisis is a rare congenital birth abnormality consisting of the herniation of intra-peritoneal organs through a defect in the thoracic wall. Thoracoschisis is classified as a part of the “Limb-Body Wall Complex” (LBWC) deformities, being more commonly associated with other birth defects such as limb agenesis, anterior thoracic wall deformities, phocomelia, and diaphragmatic hernias [1–6]. However, of the 14 total reported cases of thoracoschisis, 5 cases had no other related abnormalities [7–11].
The etiology behind thoracoschisis is still unidentified, but the presence of the other associated LBWC deformities gives insight into the timing at which these deformities likely develop [10]. Initial theories behind the pathogenesis of LBWC deformities include abnormal embryonic folding, formation of amniotic bands that interfere with limb development, rupture of amniotic sacs, and vascular malformations [3,12,13].
Diagnosis of the full extent of the defect differs on a case-by-case basis, but usually involves chest radiography (CXR) or computed tomography (CT) scans [4]. Exploratory operations are often necessary as it is sometimes unclear whether there is an elevated hemidiaphragm or a diaphragmatic hernia [8,10]. Prenatal diagnosis of thoracoschisis has been successfully demonstrated using 2D and 3D ultrasound [14]. Treatment of thoracoschisis is varied but involves primary management to assure hemodynamic and respiratory stability, followed by imaging for diagnosis, and finally either surgical reduction of abdominal contents through subcostal incision or gastroschisis-like silo bags. This is followed by closure of the thoracic wall, re-approximation of separated ribs, or plans to do staged reconstruction of the thoracic wall post-operatively [10,11]. In this case report we present a rare instance of a term male infant with an isolated left-sided thoracoschisis and rib agenesis.
Case Report
During a one-week global health outreach to Maputo, Mozambique, a 30-day old male infant was identified in the NICU of Maputo Central Hospital, Mozambique with a 3×3 cm mass overlying the left chest wall located below the left nipple (Figure 1). The mass was nonreducible, contiguous with the surrounding skin, and covered by friable granulation tissue. Upon further examination of the chest wall, there was a large surrounding defect in the rib cage around the protruding mass. There were no underlying palpable ribs at the location of the mass and no pectoral muscle present on the affected side. In addition, there was an accessory nipple complex located inferior to the mass. The rest of the physical examination was unremarkable.
Figure 1.

Showing the 3×3 cm herniation of the left lobe of the liver overlying the left chest wall.
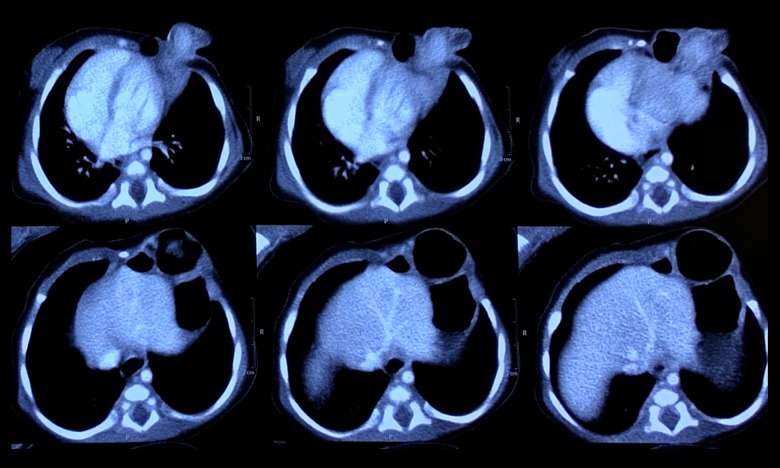
Upon review of the patient’s medical records we discovered that the infant was born by means of vaginal delivery to an otherwise healthy 20-year-old female in Tete province, Mozambique. Of note, she had received no prenatal care and contracted malaria during the first trimester of pregnancy. Immediately after birth the child was stable, needing no ventilatory assistance. He was subsequently transferred to Maputo Central Hospital NICU for further management of the left chest wall mass. The patient was evaluated by an echo-cardiography, which was deemed normal, as well as CXR and a CT of his chest (Figure 2), which delineated a possible left-sided diaphragmatic hernia, with multiple partial rib agenesis surrounding the area of the chest wall herniation. It was unclear based on the CT images whether the herniated mass contained parts of the left liver or lung.
Figure 2.
Axial CT images demonstrating herniation and rib agenesis.
The decision was made to take the child to the operating room (OR) for definitive repair. As the initial images were suggestive of an associated left diaphragmatic hernia, we approached the repair by left subcostal incision (Figure 3). It became immediately obvious that the diaphragm was very high in the left chest, but was intact and without a defect. Next, we tried to reduce the mass back into the abdominal cavity, but without success. Mobilization of the mass from the chest wall was accomplished by a combination of blunt and electrocautery dissection. Upon further inspection, we determined that the mass was originating from the left lobe of the liver. At this point, we decided to excise the exposed tissue at the level of the chest wall and allow the liver to retract back into the abdomen. The chest wall was then closed in layers (Figure 4). Postoperative recovery was complicated by the presence of an infection at the wound site, which subsequently resolved with antibiotic treatment, allowing for discharge on POD 17.
Figure 3.

A subcostal incision was made to address the presumed left-sided diaphragmatic hernia.
Figure 4.

After reduction and closure of the thoracic wall defect, as well as the subcostal incision. * Note the presence of an accessory nipple complex located inferior to the chest wall defect.
Discussion
Thoracoschisis is a very rare congenital abnormality, having only been reported 14 other times in the medical literature (Table 1). In direct contrast to thoracoabdominoschisis, thoracoschisis is not a midline defect and does not involve the abdominal wall. Davies et al. first described it in 1977 as being associated with chest wall malformations and diaphragmatic hernias [1]. Since then, other cases have been noted to be associated with limb abnormalities, being classified as a part of the group of defects known as “Limb-Body Wall Complex” (LBWC) deformities [3]. Only 5 of the reported cases of thoracoschisis have had no other related defects, termed “isolated thoracoschisis”. Our case falls into the category of isolated thoracoschisis.
Table 1.
Thoracoschisis: a review of literature.
| Reference | Year | Gender | Defect location | Content | Associated malformation | Survival |
|---|---|---|---|---|---|---|
| Davies et al. [1] | 1977 | Female | Left third intercostal | Left liver lobe, stomach, transverse colon | No left forearm, syndactyly, dextrocardia | Alive |
| Bamforth et al. [15] | 1992 | Female | Left sixth rib | Left liver lobe | Left Poland anomaly, scapula hypoplastic, no humerus, no ulna, no radius, dextrocardia | Alive |
| Derbent et al. [6] | 2001 | Female | Right second to fourth rib | Liver, intestine | LBWC, other deformations not able to be defined | Intrauterine Death |
| Biri et al. [2] | 2006 | Female | Left | Left liver lobe | Left forearm agenesis, right arm-hand agenesis | Died at Birth |
| Karaman et al. [7] | 2011 | Male | Left eighth intercostal | Liver, transverse colon, omentum | None | Alive |
| Bhattacharyya et al. [5] | 2012 | Female | Right | Riedel liver lobe, stomach, small intestine | Agenesis of the right upper limb, right upper quadrant abdominal wall defect | Died at Birth |
| Eck et al. [16] | 2015 | Male | Right fifth–eight ribs | Liver, intestine, omentum | Right fourth digit abnormality | Alive |
| McKay et al. [17] | 2015 | Female | Left eighth intercostal | Riedel liver lobe, omentum | Positional deformity of left hand & palmar contractures of the fingers | Alive |
| Seleim et al. [8] | 2015 | Male | Left 4th intercostal | Riedel liver lobe, stomach, intestine | None | Died 2 days post operative |
| Travers et al. [9] | 2016 | Female | Left rib aplasia | Mesenchymal hamartoma | None | Alive |
| de Grijs et al. [10] | 2017 | Female | Left of fourth–sixth ribs | Liver, stomach, transverse colon | None | Alive |
| Vujovic et al. [4] | 2017 | Female | Right first intercostal | Riedel liver lobe | Hypoplasia of the right arm and incomplete hand duplication | Alive |
| Hanafi et al. [14] | 2017 | Male | Left third and fourth ribs | Left liver lobe, stomach, spleen, intestine | Radial aplasia, unilateral polydactyly and syndactyly | Died at DOL 3 |
| Harris et al. [11] | 2017 | Male | Left Ribs | Liver | None | Alive |
In a similar case report of isolated thoracoschisis, Saleim et al. noted an elevated left hemi-diaphragm, with a 3×2 cm thoracic wall defect in the 4th intercostals space. The herniated contents of the thoracoschisis were the liver, stomach, and small bowel. Because the small bowel was involved, a gastroschisis-like silo bag was created to assist in reduction [8].
In some cases, as described by Karaman et al. and Grijs et al., the herniated tissue, consisting of either liver, stomach, omen-tum, or transverse colon, was able to be separated from adhesions to the chest wall, so a simple reduction and primary repair was successful [7,10]. Our case falls more into the group of cases described by Travers et al. and Harris et al., in which the external herniated tissue, mainly liver, needed to be resected prior to reduction [9,11]. These 2 reports are similar to our case, as the only tissue herniated through the thoracic wall defect was part of the liver.
An important distinction between different cases of isolated thoracoschisis is the presence of rib agenesis. In reports by Harris et al., Saleim et al., and Karaman et al., there was an enlarged intercostal space between the ribs, but no rib agenesis was present [7,8,11]. In comparison, Grijs et al. and Travers et al. noted segmental agenesis of the involved ribs [9,10]. To the best of our knowledge, the present case is the third reported case of isolated thoracoschisis with rib agenesis.
Current survival rates of all forms of thoracoschisis are about 66%, and are mainly dependent on the associated malformations (Table 1). Of the 5 reported cases of thoracoschisis that resulted in death, 1 was intrauterine with undiagnosed associated malformation, 3 were associated with limb malformations, and 1 was isolated [2,5,6,8,14]. For those that survived reduction of the herniated contents, no post-operational complications were noted. Those with rib cage and limb malformations were scheduled for reconstructive surgery.
Conclusions
Isolated thoracoschisis with rib agenesis is a very rare congenital abnormality, which, to the best of our knowledge, has only being described 2 other times in the medical literature. Our case demonstrates a less severe form of isolated thoracoschisis that was successfully managed by primary surgical repair.
Footnotes
Conflict of interest
None.
References:
- 1.Davies MRQ, Rode H, Cywes S. “Thoracoschisis” associated with an ipsi-lateral distal phocomelia and an anterolateral diaphragmatic hernia – A case report. J Pediatr Surg. 1977;125:755–57. doi: 10.1016/0022-3468(77)90413-4. [DOI] [PubMed] [Google Scholar]
- 2.Biri A, Korucuoğlu U, Turp A, et al. A new syndrome with prenatally diagnosed thoracoschisis, hiatal hernia and extremities’ agenesis: Case report. Genet Couns. 2006;17(2):161–65. [PubMed] [Google Scholar]
- 3.Van Allen MI, Curry C, Gallagher L. Limb body wall complex: I. Pathogenesis. Am J Med Genet. 1987;28(3):529–48. doi: 10.1002/ajmg.1320280302. [DOI] [PubMed] [Google Scholar]
- 4.Vujovic D, Sretenovic A, Raicevic M, et al. Thoracoschisis associated with Limb Body Wall Complex. APSP J Case Rep. 2017;8(3):19. doi: 10.21699/ajcr.v8i3.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhattacharyya NC, Gogoi M, Deuri PK. Thoracoschisis with limb agenesis. J Indian Assoc Pediatr Surg. 2012;17:78–79. doi: 10.4103/0971-9261.93972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Derbent M, Balci S. Thoracoschisis associated with diaphragmatic hernia in a 31-week-old stillbirth. Turk J Pediatr. 2001;43:269–71. [PubMed] [Google Scholar]
- 7.Karaman I, Karaman A, Erdogan D, et al. The first male with thoracoschisis: Case report and review of the literature. J Pediatr Surg. 2011;46:2181–83. doi: 10.1016/j.jpedsurg.2011.08.016. [DOI] [PubMed] [Google Scholar]
- 8.Seleim H, ElFiky M, Fares A, Elbarbary M. Isolated thoracoschisis: Case report and review of literature. Eur J Pediatr Surg Rep. 2015;3(1):40–42. doi: 10.1055/s-0034-1396013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Travers CP, Hamm JA, Cleveland S, et al. Thoracoschisis secondary to a mesenchymal hamartoma associated with diaphragmatic eventration. Case Reports in Perinatal Medicine. 2016;5(2):141–44. [Google Scholar]
- 10.de Grijs D, Israelyan N, DeVore GR, et al. An unusual occurrence of isolated thoracoschisis. J Pediatr Surg Case Rep. 2017;16:43–45. [Google Scholar]
- 11.Harris J, Zhang Y, Patel S, et al. A rare case of thoracoschisis. J Neonatal Surg. 2017;6(3):65. doi: 10.21699/jns.v6i3.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Torpin R. Amniochorionic mesoblastic fibrous strings and amnionic bands. Associated constricting fetal malformations or fetal death. Am J Obstet Gynecol. 1965;91(1):65–75. doi: 10.1016/0002-9378(65)90588-0. [DOI] [PubMed] [Google Scholar]
- 13.Streeter GL. Focal deficiencies in fetal tissues and their relation to intrauterine amputations. Contributions to Embryology. 1930;22:3–44. [Google Scholar]
- 14.Hanafi HR, Zakaria ZA. Prenatal diagnosis of thoracoschisis and review of literature. Case Rep Obstet Gynecol. 2017;2017:9821213. doi: 10.1155/2017/9821213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bamforth JS, Fabian C, Machin G, Honore L. Poland anomaly with a limb body wall disruption defect: Case report and review. Am J Med Gen. 1992;43(5):780–84. doi: 10.1002/ajmg.1320430504. [DOI] [PubMed] [Google Scholar]
- 16.Eck DL, Maryak BN, Poulos ND, et al. Thoracoschisis: Case report and review of the literature. Ann Pediatr Surg. 2015;11(2):143–46. [Google Scholar]
- 17.McKay JD, Parker CM, Loewen J, et al. Thoracoschisis: A case report and review of literature. Fetal Pediatr Path. 2015;34(5):307–14. doi: 10.3109/15513815.2015.1051254. [DOI] [PubMed] [Google Scholar]