Abstract
Objective:
People with serious mental illness have dramatically reduced life expectancy that is largely attributed to elevated rates of chronic medical conditions. Several group interventions have been developed and implemented in recent years in order to improve health and wellness among people with mental health conditions. Unfortunately, attendance in these interventions is often low, and there is limited understanding of factors that influence patient engagement in this treatment modality.
Method:
Participants (N=242) were enrolled in one of two group-based health and wellness treatment programs. Using descriptive statistics and regression, we assessed treatment attendance and a range of potential predictors of attendance.
Results:
We found lower attendance among people who were younger, people with more medical conditions, and people with more emergency room visits in the six months prior to the beginning of treatment. Younger age was a particularly strong predictor of low attendance and was the only variable significantly associated with attending zero treatment sessions.
Conclusions and Implications for Practice:
These results highlight the need for strategies to improve engagement of patients with poorer objective indicators of medical health, and patients with younger age.
Keywords: Wellness, Serious mental illness, Engagement, Attendance, Veterans
People with serious mental health conditions such as schizophrenia, schizoaffective disorder, and posttraumatic stress disorder have a dramatically reduced average life expectancy and elevated rates of chronic medical conditions (Das Munshi et al., 2017; Liu et al., 2017; Olfson et al., 2015; Walker et al., 2015). A number of group therapy interventions have been developed with the goal of improving physical health outcomes for people with mental health conditions. Evidence suggests such programs can be effective. For example, randomized controlled trials have documented that the physical health-focused group therapy programs ACHIEVE (Daumit et al., 2013), Living Well (Muralidharan et al., 2018), and HARP (Druss et al., 2010; Druss et al., 2018) improve a range of health-related outcomes in people with serious mental illness.
One major barrier to implementation of physical health interventions is client attendance. Attendance rates for behavioral interventions tend to be low across modalities (Bellack et al., 2009; Kreyenbuhl, Nossel, and Dixon, 2009) and physical health interventions are no exception. For example, a randomized controlled trial of ACHIEVE found that just 77 of the 246 sessions that were offered were attended, with between 27% and 52% of patients attending zero sessions in a 30-day period (Daumit et al., 2013). HARP, a less intensive treatment consisting of six sessions total, found that 30% of patients attended three or fewer sessions (Druss et al., 2018). Attendance is a key variable in intervention research as failure to attend negates access to the intervention and may indicate issues with the intervention content or structure, and increased treatment attendance may lead to improved client outcomes and make treatment planning more efficient. For this reason, it would be beneficial for researchers and practitioners to build an improved understanding of factors affecting treatment attendance.
Research on attendance in physical health intervention groups is limited, but studies have tried to identify factors that predict general mental health treatment attendance among adults with serious mental illness. Most consistently identified predictors of attendance include demographic variables, mental health symptoms, psychosocial, physical, and cognitive functioning, and patient motivation/activation. Women, White/non-Hispanic, older, and more educated individuals are more likely to engage in treatment (Kreyenbuhl 2009; Kukla et al., 2014; Maura & Weisman de Mamani, 2017). Mental health symptoms associated with greater engagement include less severe mood, positive, and negative symptoms (Kukla et al., 2014) and being more likely to recognize the often chronic yet manageable course of serious mental illness (Shah et al., 2009; Tait et al., 2003); individuals with current substance use disorders are less likely to attend treatment sessions (Brown et al., 2011). Better psychosocial functioning and beliefs that treatment can improve psychosocial functioning and quality of life are likely to increase treatment attendance (Jochems et al., 2017; Kreyenbuhl et al., 2009). Individuals with higher levels of cognitive functioning and those who are more effortful when completing cognitive tasks are also more likely to engage in treatment (Kukla et al., 2014; Moore et al., 2015). Lastly, individuals with serious mental illness are more likely to engage in treatment if they perceive it as having value and a recovery focus (Bryce et al., 2018; Gudjonsson et al., 2011).
Although predictors of overall attendance in mental health treatment is well-documented in the literature, these predictors presumably vary by modality and treatment targets, and few studies have examined predictors of attendance in physical health treatment groups among adults with serious mental health conditions. While research has highlighted predictors of treatment attendance in general, Roberts and Bailey (2010) found that no studies had specifically explored predictors of participation in lifestyle interventions in this population. However, they reported that the literature points to several possible barriers (e.g., mental health symptoms, limited support, negative staff attitudes) and facilitators (e.g., less severe symptomatology, greater support, more knowledge of problematic health behaviors, and staff participation) to lifestyle treatment engagement. Since this published review, several studies have examined predictors of attendance in smoking cessation treatment, finding that attendance was related to psychiatric symptoms (e.g., higher rates of psychiatric symptoms; Travaglini et al., 2017); social factors (e.g., being around more non-smokers, greater encouragement to quit; Aschbrenner et al., 2015); and treatment factors (e.g., less positive smoking culture in treatment programs, prior smoking cessation services; Trainor & Leavy, 2017; Travaglini et al., 2017). Marital status has also been examined as a predictor, with study findings differing in terms of whether being married is associated with a greater (McCarthy et al., 2007) or lower (Travaglini et al., 2017) likelihood of engagement. Interestingly, one study of an obesity intervention disseminated to Veterans Affairs hospitals across the United States found that veterans with serious mental illness had greater participation than veterans without serious mental illness, despite being screened less often (Littman et al., 2015).
There is a dearth of research looking at factors affecting attendance in physical health interventions, particularly group programs. To explore predictors of attendance in treatment groups focused on improving physical health for people with serious mental illness, we evaluated predictors of treatment attendance in a large sample of patients randomly assigned to two different group-based health and wellness interventions. Because of the lack of previous research, these analyses were largely exploratory. We test and report each variables’ independent relationship with attendance before fitting a multivariate model, in addition to testing whether predictors of attendance varied between the two group programs.
Method
Participants.
Participants were recruited from outpatient programs at VA Medical Centers in the Mid-Atlantic region (see Table 1 for demographic characteristics), including two urban centers and one rural center, through review of clinic and program rosters, clinician referrals, and recruitment flyers posted in clinic waiting areas. A partial HIPAA waiver was obtained to allow review of charts to confirm eligibility. Interested and eligible participants completed written informed consent and completed baseline assessments before being randomized to treatment condition. All study procedures were approved by the appropriate institutional review boards.
Table 1.
Participant characteristics
| Gender | N | % |
|---|---|---|
| Male | 210 | 87 |
| Female | 32 | 13 |
| Race | ||
| Black | 151 | 62 |
| White | 69 | 29 |
| Asian | 4 | 2 |
| Other | 18 | 7 |
| Ethnicity | ||
| Hispanic | 5 | 2 |
| Non-Hispanic | 235 | 98 |
| Education | ||
| No High School | 17 | 7 |
| High School | 82 | 34 |
| Some College | 97 | 40 |
| College | 20 | 8 |
| Graduate School | 26 | 11 |
| Employment | ||
| Full-time | 12 | 5 |
| Part-time | 18 | 7 |
| Not employed | 212 | 88 |
| Psychiatric | ||
| Diagnosis (some | ||
| with >1 diagnosis) | ||
| Schizophrenia | 29 | 12 |
| Schizoaffective | 38 | 16 |
| disorder | ||
| Bipolar disorder | 86 | 35 |
| Major Depression | ||
| Disorder with | 12 | 5 |
| Psychotic Features | ||
| Psychosis NOS | 12 | 5 |
| Post-Traumatic | 71 | 29 |
| Stress Disorder | ||
| Health Status and Behaviors | ||
| Diabetes | 91 | 38 |
| Arthritis | 187 | 77 |
| Respiratory Diseases | 27 | 11 |
| Cardiovascular | 36 | 15 |
| Diseases | ||
| Current smoker | 94 | 43 |
| Alcohol use in past | 63 | 28 |
| 30 days | ||
| Number of classes of chronic medical conditions | ||
| Mean (SD) | 3.4 (1.7) | |
| Range | 0–7 | |
| Body Mass Index | ||
| Mean (SD) | 31.1 (6.5) | |
| Range | 17.7–51.7 | |
| Age | ||
| Mean (SD) | 57.75 (7.75) | |
| Range | 30–75 |
The present study utilized baseline assessment and attendance data from a large randomized controlled trial (RCT) comparing two manualized, 12-session, group-based interventions focused on health and wellness (main outcomes reported in Muralidharan et al., 2018): Living Well, a skills-based intervention tailored to promote medical illness self-management behaviors among adults with serious mental illness (cofacilitated by a non-peer Masters-level study interventionist and a peer support specialist), and Medical Illness Education and Support, a didactic intervention that provided information about general health and wellness and facilitated solely by a non-peer Masters-level study interventionist. Participants (N=242; demographics reported in Table 1) were adults engaged in mental health services at a study site, with a medical record psychiatric diagnosis of schizophrenia spectrum disorder, bipolar disorder, major depression with psychotic features, and/or post-traumatic stress disorder, and a co-occurring chronic medical condition. Exclusion criteria included lack of capacity to consent, serious cognitive impairment, and current participation in a psychosocial treatment trial at the investigators’ home research center.
Participant payment for this study was linked to filling out assessments, which were administered separately from group times. Attendance had no effect on payment or ease of payment study participants, and participants could attend zero treatment sessions while still being paid the maximum amount possible.
Measures.
All measures for the current study were collected at the baseline assessment. Basic demographic and psychosocial data were collected from participants. Items from the National Health and Nutrition Examination Survey III (CDC, 1993) were used to collect information on current and lifetime medical conditions.
Self-reported physical and mental health functioning was measured using the relevant subscales from the 12-item Short-Form Health Survey (SF-12; Ware et al., 1996), a widely used instrument with good psychometrics in this population (Salyers et al., 2000). Higher scores indicate better functioning.
The Patient Activation Measure (PAM; Hibbard et al., 2004) was used to assess self-reported ability to actively participate in treatment encounters. This measure has shown good reliability and validity in hospitalized multimorbid patients (Schmaderer et al., 2015). Higher scores indicate greater activation. In the current sample, Cronbach’s alpha for the PAM was 0.88.
The 18-item Multidimensional Health Locus of Control measure was used to assess expectations about control of one’s health (Wallston, Strudler Wallston, & DeVellis, 1978). Specifically, we used the internal health locus of control subscale. Cronbach’s alpha for this subscale in the sample was 0.72.
Total score on the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS; Randolph et al., 1998) was used to measure memory, language, and attention abilities, and has demonstrated reliability in serious mental illness (Wilk et al., 2002, 2004).
Emergency room service use was extracted from the electronic medical record for the six months prior to baseline. For the purposes of regression analyses, the ER count variable was log-transformed.
Diagnostic information was extracted from chart review and coded into the following six (not mutually exclusive) overarching groups: PTSD, Schizophrenia, Schizoaffective disorder, Bipolar disorder, Major Depressive Disorder with Psychotic Features, or Psychosis Not Otherwise Specified. Although we tested diagnosis as a predict of attendance, it should be noted that we did not perform a diagnostic clinical interview and the reliability of diagnostic determinations made on the basis of chart review may be low.
Analysis Plan.
Treatment attendance is typically operationalized by number of sessions attended (continuous) and/or attendance to any session (yes/no binary; Kreyenbuhl, Nossel, and Dixon, 2009); therefore, we analyze both outcomes by regressing predictors on attendance of a non-zero number of sessions, as well as number of sessions attended (using logistic regression for the binary outcome, and analyzing number of sessions attended after restricting the dataset to those people who attended any sessions). We performed these analyses in two steps. First, we fit separate multilevel regressions (with participants embedded within therapy groups) to test whether attendance could be predicted from measured demographic and psychosocial variables. Second, we fit a multivariate multilevel regression using only those variables that were shown to significantly predict attendance on their own in order to determine whether those variables predicted unique variance in session attendance.
As a final step, we tested the extent to which the relationship between identified predictors and attendance depended upon the intervention type (Living Well versus Medical Illness Education and Support). To do so, we added interaction effects to the multivariate model.
Results
Participants.
Participant demographic and clinical information is displayed in Table 1. The modal participant in the study was middle-aged or older, non-Hispanic black, male, unemployed, with a high school or some college education.
Distribution of session attendance.
The distribution of number of attended sessions is given in Figure 1. Out of 12 possible sessions, the median number of sessions attended was six (mean 5.9, standard deviation=4.4). The distribution appears relatively uniform apart from a large number of zeros representing the 17.7% of participants who were randomized to an intervention but did not attend any sessions.
Figure 1.
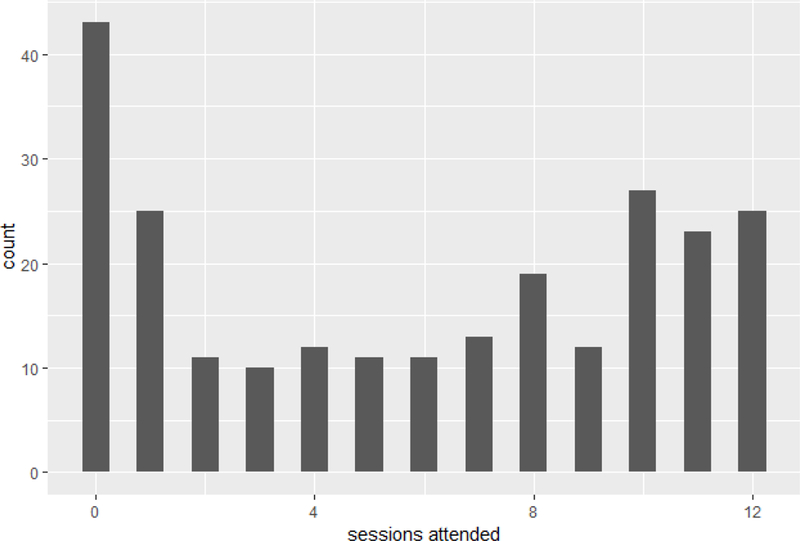
Frequency histogram of number of sessions attended
Predictors of attendance.
A series of multilevel logistic models (with participants embedded within groups) were fit to test whether demographic or psychosocial variables were predictive of attending one or more (i.e., non-zero) sessions, and whether these variables were predictive of attending a greater number of sessions. Variables tested were age, race, gender, education, diagnosis, PAM total scores, SF-12 physical health and mental health scales, Internal Health Locus of Control (IHLC), RBANS total scores, number of (medical or psychiatric) ER visits in previous six months, and number of medical conditions. We found that only age (p=.01) and ER visits (p=.03) were predictive of attending at least one session, with higher likelihood of attendance predicted by older age and fewer ER visits. Conditional on attending at least one session, greater attendance was associated with significantly better self-reported baseline physical health (p=.03) and mental health (p=.03), greater patient activation (p=.04), greater age (p=.0002), fewer ER visits in the previous six months (p=.002), and fewer medical conditions (p=006).
As a second step, we entered all significant variables into multivariate regression models to assess for unique relationships with attendance. Age continued to significantly predict attending at least one session (p=.03) but ER visits did not (p=.06). Attendance of a greater number of sessions was also associated with significantly fewer ER visits in the previous six months (p=.004), older age (p=.0004), and fewer medical conditions (p=.03). The effect of patient activation and self-reported mental and physical health dropped to non-significance in the multivariate model.
As an aid to interpretation of the multivariate models, Figure 2 plots observed and model-predicted attendance of a non-zero number of sessions at different ages, and Figure 3 plots model-predicted number of attended sessions given age, number of ER visits, and number of medical conditions.
Figure 2.
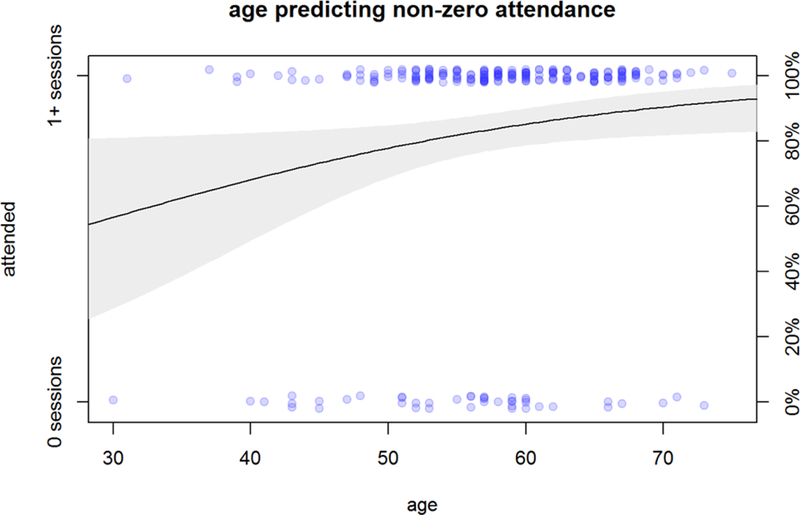
Note. Points indicate observed values (vertically jittered). Line gives modeled probability of attending a non-zero number of sessions across age groups. For example, 30-year-olds have a 57% likelihood of attending any sessions, whereas 70-year-olds have a 90% likelihood.
Figure 3. Number of sessions attended, conditional on attending any sessions.
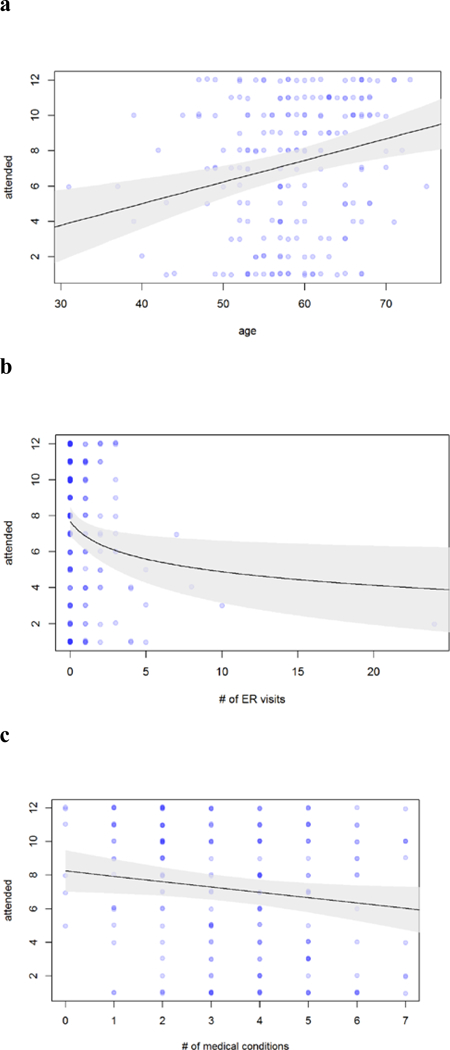
Note. Points indicate observed values (restricted to participants who attended any sessions). Lines give model-predicted number of attended sessions (conditional on attending any sessions) for different values of the predictor variables after holding other predictor variables constant.
Variation by group.
To test for any variation by group in the relationship between the identified predictors and attendance, we added interaction effects to the multivariate model between each variable and group (Living Well versus Medical Illness Education and Support). No interaction effects were significant, suggesting insufficient evidence of variation in any of these effects by group.
Discussion
Effective treatment engagement is crucial to the implementation of behavioral health interventions for people with serious mental health concerns (Bellack et al., 2009; Kreyenbuhl, Nossel, and Dixon, 2009). The current study examined factors that predict treatment attendance in two group interventions intended to improve overall health, a domain of critical importance given the high rates of mortality and medical comorbidity measured in this population (Das Munshi et al., 2017; Liu et al., 2017; Olfson et al., 2015; Walker et al., 2015). Controlling for other variables, we found that attendance in a greater number of group sessions was significantly associated with older age, fewer medical conditions, and fewer emergency room visits in the six months prior to the start of the group. Coming to group at least once (versus never appearing) was significantly predicted by older age alone.
These findings suggest areas where clinicians may be able to improve treatment attendance for group interventions targeting health among people with serious mental health concerns. We are particularly concerned by the lower engagement measured among patients with poorer objective indicators of medical health. It may be necessary to make special adjustments for patients who have a particularly high number of comorbid medical conditions and/or are heavy users of emergency services (e.g., 5+ visits in six months; see Figure 3). For this cohort, outreach and coordination with medical providers may be especially effective given their high rates of contact. Additionally, clinicians with experience delivering these group interventions (e.g., the first and last authors of this manuscript) have observed that patients who are in especially poor health sometimes find it stressful and/or physically difficult to come to groups, which suggests possible solutions such as more assertive case management or modifications to allow the content of the group to be deliverable remotely.
Older age was the sole variable that significantly predicted both attendance in any sessions and attendance in a greater number of sessions, even after accounting for number of medical conditions and self-reported physical health. Older adults with serious mental illness report that addressing chronic medical conditions is an area of high priority (Bartels et al., 2009), so it may be that the older participants in the present sample were more motivated to engage in a group with a physical health focus. Alternatively, given that social isolation is prevalent among older adults (Cornwell & Waite, 2009), and that older adults with serious mental illness have even smaller and less satisfactory social networks than their same-age counterparts without mental illness (Meesters et al., 2010), older participants in the present study may have been particularly motivated by the social aspect of the interventions. Group-based interventions with an integrated emphasis on physical health concerns could be a powerful way to engage this population in holistic and recovery-oriented care.
These results also highlight the need to better direct health related programming to individuals with serious mental illness who are in middle age, rather than solely older adults. Health-related psychosocial interventions have a lot to offer younger participants. The conditions that eventually lead to poor health and death for people with serious mental illness, such as diabetes and heart disease, start early and develop over years of poor health behaviors including smoking, obesity, and lack of physical activity (Parks et al., 2006). Thus health-related interventions may be particularly relevant to middle-aged individuals with serious mental illness, especially those helping them learn to address conditions early on and to develop sound management skills that they can carry into the future. Reduced attendance by younger individuals may be related to their perceiving that they do not have serious health problems or that there is plenty of time for them to change their health behaviors in the future. Targeting younger individuals with SMI with the message that early intervention and management can lead to improved functioning and better health as they age may help increase attendance. Similarly, those with more complex health problems may believe that they have little to gain from a group intervention and that their health is already too compromised for them to manage. These individuals may need a different approach to engagement – one that incorporates strategies such as motivational interviewing to help individuals explore how participating in health-related interventions fits in with one’s personal values and goals, and how learning practical tools and skills can improve health and wellness.
There were several limitations to the present study that should be considered. The sample was mostly male, older (mean age: 58, minimum: 30), and all were veterans, limiting generalizability to other populations. The age range was relatively restricted, with most participants being between 40 and 60, which could reduce the generalizability of the age-related findings. Also, all participants were individuals currently attending mental health treatment at a study site; thus predictors identified here may not generalize to those not engaged in mental health care. Additionally, interpretation of our findings was limited by our sample size and the choice of statistical models. For example, it is plausible that people who attend just one session are in some cases qualitatively distinct from people who attend zero or two sessions (e.g., they may have been particularly dissatisfied with the “feel” of the treatment), but with only 25 people attending just one session we did not feel justified in statistically modeling these participants as a third group. Finally, engagement may have been limited relative to non-veteran populations due to the high number of other overlapping treatment options available to veterans. Future studies are needed to more completely characterize factors affecting treatment engagement for people with serious mental health concerns, particularly for interventions targeting physical health.
Impact.
Research suggests that health and wellness among people with serious mental health conditions may be improved through participation in empirically validated group-based health and wellness interventions. However, these interventions tend have low attendance. In this large study, we found lower treatment attendance among people who were younger, people with more medical conditions, and people who used lots of emergency services. Our research suggests the need for improved strategies to increase treatment attendance by these groups (who may be the most likely to benefit).
Acknowledgments:
This research was supported by the Department of Veterans Affairs Health Services Research and Development Service.
Dr. Phalen and Dr. Travaglini are supported by supported by the Department of Veterans Affairs Office of Academic Affiliations Advanced Fellowship Program in Mental Illness Research and Treatment.
Dr. Muralidharan is supported by VA Rehabilitation Research and Development Career Development Award IK2RX002339.
Footnotes
Disclosures
The authors have no conflicts of interest to disclose.
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or other affiliated institutions.
References
- Aschbrenner KA, Naslund JA, Shevenell M, Mueser KT, & Bartels SJ (2016). Feasibility of behavioral weight loss treatment enhanced with peer support and mobile health technology for individuals with serious mental illness. Psychiatric Quarterly, 87(3), 401–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartels SJ, & Pratt S (2009). Psychosocial rehabilitation and quality of life for older adults with serious mental illness: recent findings and future research directions. Current opinion in psychiatry, 22(4), 381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellack AS, Bowden CL, Bowie CR, Byerly MJ, Carpenter WT, Copeland LA, … & Dixon LB (2009). The expert consensus guideline series: adherence problems in patients with serious and persistent mental illness. Journal of Clinical Psychiatry, 70(SUPPL. 4), 1–48. [PubMed] [Google Scholar]
- Brown CH, Bennett ME,Li L, &Bellack AS (2011). Predictors of initiation and engagement in substance abuse treatment among individuals with co-occurring serious mental illness and substance use disorders. Addictive behaviors, 36(5), 439–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryce SD, Lee SJ, Ponsford JL, Lawrence RJ, Tan EJ, & Rossell SL (2018). The impact of intrinsic motivation on session attendance and reliable cognitive improvement in cognitive remediation in schizophrenia. Schizophrenia research, 202, 354–360. [DOI] [PubMed] [Google Scholar]
- Cornwell EY, & Waite LJ (2009). Social disconnectedness, perceived isolation, and health among older adults. Journal of health and social behavior, 50(1), 31–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das-Munshi J, Chang CK, Dutta R, Morgan C, Nazroo J, Stewart R, & Prince MJ (2017). Ethnicity and excess mortality in severe mental illness: a cohort study. The Lancet Psychiatry, 4(5), 389–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daumit GL, Dickerson FB, Wang NY, Dalcin A, Jerome GJ, Anderson CA, … & Oefinger M (2013). A behavioral weight-loss intervention in persons with serious mental illness. New England Journal of Medicine, 368(17), 1594–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Druss BG, Zhao L, Silke A, Bona JR, Fricks L, Jenkins-Tucker S, … & Lorig K (2010). The Health and Recovery Peer (HARP) Program: a peer-led intervention to improve medical self-management for persons with serious mental illness. Schizophrenia research, 118(1–3), 264–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Druss BG, Singh M, von Esenwein SA, Glick GE, Tapscott S, Tucker SJ, … & Sterling EW (2018). Peer-Led Self-Management of General Medical Conditions for Patients With Serious Mental Illnesses: A Randomized Trial. Psychiatric Services, 69(5), 529–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galon P, & Graor CH (2012). Engagement in primary care treatment by persons with severe and persistent mental illness. Archives of psychiatric nursing, 26(4), 272–284. [DOI] [PubMed] [Google Scholar]
- udjonsson GH, Savona CS, Green T, & Terry R (2011). The recovery approach to the care of mentally disordered patients. Does it predict treatment engagement and positive social behaviour beyond quality of life?. Personality and Individual Differences, 51(8), 899–903. [Google Scholar]
- Jochems EC, Duivenvoorden HJ, van Dam A, van der Feltz-Cornelis CM, & Mulder CL (2017). Motivation, treatment engagement and psychosocial outcomes in outpatients with severe mental illness: a test of Self-Determination Theory. International journal of methods in psychiatric research, 26(3), e1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreyenbuhl J, Nossel IR, Dixon LB. Disengagement from mental health treatment among individuals with schizophrenia and strategies for facilitating connections to care: A review of the literature. Schizophrenia Bulletin. 2009;35(4):696–703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreyenbuhl J, Nossel IR, & Dixon LB (2009). Disengagement from mental health treatment among individuals with schizophrenia and strategies for facilitating connections to care: a review of the literature. Schizophrenia bulletin, 35(4), 696–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littman AJ, Damschroder LJ, Verchinina L, Lai Z, Kim HM, Hoerster KD, … & Goodrich DE (2015). National evaluation of obesity screening and treatment among veterans with and without mental health disorders. General Hospital Psychiatry, 37(1), 7–13. [DOI] [PubMed] [Google Scholar]
- Liu NH, Daumit GL, Dua T, Aquila R, Charlson F, Cuijpers P, … & Gaebel W (2017). Excess mortality in persons with severe mental disorders: a multilevel intervention framework and priorities for clinical practice, policy and research agendas. World psychiatry, 16(1), 30–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maura J, Weisman de Mamani A. Mental health disparities, treatment engagement, and attrition among racial/ethnic minorities with severe mental illness: A review. Journal of Clinical Psychology in Medical Settings. 2017;24(3–4):187–210 [DOI] [PubMed] [Google Scholar]
- McCarthy JF, Blow FC, Valenstein M, Fischer EP, Owen RR, Barry KL, … & Ignacio RV (2007). Veterans Affairs Health System and mental health treatment retention among patients with serious mental illness: evaluating accessibility and availability barriers. Health services research, 42(3p1), 1042–1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meesters PD, Stek ML, Comijs HC, de Haan L, Patterson TL, Eikelenboom P, & Beekman AT (2010). Social functioning among older community-dwelling patients with schizophrenia: a review. The American Journal of Geriatric Psychiatry, 18(10), 862–878. [DOI] [PubMed] [Google Scholar]
- Moore RC, Davine T, Harmell AL, Cardenas V, Palmer BW, & Mausbach BT (2013). Using the repeatable battery for the assessment of neuropsychological status (RBANS) effort index to predict treatment group attendance in patients with schizophrenia. Journal of the International Neuropsychological Society, 19(2), 198–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muralidharan A, Brown CH, Peer JE, Klingamen EA, Hack SM, Li L, Walsh MB, and Goldberg RW (2018). Living Well: An Intervention to Improve Medical Illness Self-Management Among Individuals With Serious Mental Illness Psychiatric Services, Advance Online Publication. doi: 10.1176/appi.ps.201800162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olfson M, Gerhard T, Huang C, Crystal S, & Stroup TS (2015). Premature mortality among adults with schizophrenia in the United States. JAMA psychiatry, 72(12), 1172–1181. [DOI] [PubMed] [Google Scholar]
- Parks J, Svendsen D, Singer P, Foti ME, & Mauer B (2006). Morbidity and mortality in people with serious mental illness. Alexandria, VA: National Association of State Mental Health Program Directors (NASMHPD) Medical Directors Council, 25(4). [Google Scholar]
- Roberts SH, & Bailey JE (2011). Incentives and barriers to lifestyle interventions for people with severe mental illness: a narrative synthesis of quantitative, qualitative and mixed methods studies. Journal of Advanced Nursing, 67(4), 690–708. [DOI] [PubMed] [Google Scholar]
- Shah P, Hull T, Riley GA. Associations between the Illness Perception Questionnaire for Schizophrenia and engagement in treatment in a secure setting. Clinical Psychologist. 2009;13(2):69–74 [Google Scholar]
- Staring ABP, Van der Gaag M, Koopmans GT, Selten JP, Van Beveren JM,Hengeveld MW, … & Mulder CL (2010). Treatment adherence therapy in people with psychotic disorders: randomised controlled trial. The British Journal of Psychiatry, 197(6), 448–455. [DOI] [PubMed] [Google Scholar]
- Tait L, Birchwood M, & Trower P (2003). Predicting engagement with services for psychosis: insight, symptoms and recovery style. The British Journal of Psychiatry, 182(2), 123–128. [DOI] [PubMed] [Google Scholar]
- Travaglini LE, Li L, Brown CH, & Bennett ME (2017). Predictors of smoking cessation group treatment engagement among veterans with serious mental illness. Addictive behaviors, 75, 103–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker ER, McGee RE, & Druss BG (2015). Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA psychiatry, 72(4), 334–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallston KA, Strudler Wallston B, & DeVellis R (1978). Development of the multidimensional health locus of control (MHLC) scales. Health education monographs, 6(1), 160–170. [DOI] [PubMed] [Google Scholar]


