Abstract
Objective
To examine whether cardiovascular disease (CVD) is associated with depression status.
Methods
29,328 participants from baseline of Canadian Longitudinal Study for Aging were categorized into four groups of depression status. Group 1: no depression (reference); Group 2: currently with depression symptom (CES-D10 score ≥ 10, negative self-reported depression); Group 3: self-reported depression with no current symptom (CES-D10 score < 10, positive self-reported depression); and Group 4: self-reported depression with current symptom (CES-D10 score ≥ 10, self-reported depression). Six self-reported CVDs were grouped into two related disorders, i.e., heart related disorders (HRD) including heart disease, myocardial infarction, and angina; and peripheral/vascular related disorders (PRD) including hypertension, stroke, and peripheral vascular disease. Adjusted odds ratios (ORs) were used to evaluate the associations between depression and CVDs.
Results
17.3% of participants had self-reported depression, 15.3% were with current depression symptom, 10.5% were with HRD and 34.4% were with PRD. After adjusting for variables of demographics, sex, lifestyles, and comorbidities, compared to reference, people in Group 2 had a slightly increased odds, but most of them were not statistically significant; the ORs (95% CI) were 1.36 (1.18–1.58, P < 0.0001) for HRD and 1.20 (1.09–1.32, P < 0.001) for PRD in Group 3; for people in Group 4, the ORs (95% CI) were 1.31 (1.08–1.61, P < 0.01) for HRD and 1.17 (1.02–1.34, P < 0.05) for PRD. Sex- and age-stratified analyses suggested that the increased ORs were more prevalent in men and people aged < 65 years.
Conclusions
Seniors with self-reported depression are associated with an increased risk of CVDs, the association varies by depression status, sex and age.
Keywords: Age, Cardiovascular diseases, CES-D10 score, Clinic depression, Sex
1. Introduction
With remarkable improvements in public health and medical services, Canadians are living longer than most people in the world.[1] As a result, approximately 17% of the Canadian population are 65 years or older in the 2016 census[2] and one in four of Canadians will be expected to be seniors by 2036.[3] However, with a rapidly aging population, there is no doubt to see an increase in prevalence of chronic diseases, particularly cardiovascular diseases (CVDs). In the 2016 report of Chief Officer of Public Health, it estimated that 7.1% Canadians aged 50–64 years, and 18.3% aged over 65 years in 2014 were reported to live with CVD.[4] As psychological factors play an important role in the development and occurrence of CVD, and vascular depression due to CVD may lead to and/or exacerbate depression among seniors.[5] The coexistence of CVD and depression diminishes the quality of life, indeed leads to poor health outcomes, compounds disability and increases the risk of death.[6] Therefore, a number of screening tools for detecting depression in early stage have been developed.[7] The Center for Epidemiological Studies Depression (CES-D) scale is one of them with a common self-reporting scale to measure the current level of depressive symptomatology in a general population.[8] When being diagnosed with clinical depression, only approximately 60% of people received either pharmacotherapy or psychotherapy or both.[9] Consequently, some of them are expected to be with remission but others continue to be depressed due to a lack of treatment or treated ineffectively.[10] It is unclear, however, whether the cardiovascular depression risk association varies by people's depression status. In addition, women, in comparison with men, are more likely to experience depression and, in general, higher prevalence of depression is more prevalent among young people.[11] Therefore, when examining the cardiovascular risk association with depression, one may need to take these factors into account as well. Using the Canadian Longitudinal Study on Aging (CLSA) data, which was initiated in 2012 and a large, national, long-term study,[12] we aimed to address these issues.
2. Methods
2.1. Canadian Longitudinal Study on Aging
Approximately 51,000 men and women aged 45–85 years (mean age: 60 years) across Canada have been recruited at baseline of the CLSA through two sub-cohorts in the CLSA, i.e., “Tracking cohort”, which recruited approximately 20,000 people, and “Comprehensive cohort”, which recruited the rest over 30,000 CLSA participants. The detailed description of the CLSA can be found elsewhere.[12] Since only questionnaire used in the “Comprehensive cohort” asked information related to clinical depression, we used it to examine the association between history of depression status and CVD. After cleaning missing information on depression and CVD, a total of 29,328 men and women were included in this analysis. This study was approved for a secondary data analysis by the Research Ethics Board of Brock University.
2.2. Measurements
2.2.1. Clinical depression
All participants from the “Comprehensive cohort” were surveyed at the baseline through a questionnaire at the in-home interview. Under the section of chronic conditions, information of long-term conditions that are expected to last, or have already lasted, six months or more and that have been diagnosed by a health professional was collected. Depression was then determined by a positive response to the question “Has a doctor ever told you that you suffer from clinical depression?”.
2.2.2. Currently potential depressed
Additionally, all participants were surveyed with the CES-D10, a short form of the regular CES-D,[13] to detect current depressive symptomatology that helps to identify clinically important depression with a good level of sensitivity.[14] The overall CES-D10 score ranges from 0 to 30 with a score ≥ 10 suggesting current depressive illness, which needs to be further assessed.
Based on the response to the clinical depression question and CES-D10 score, all participants were then grouped into one of the four groups of history of depression status, i.e., Group 1: no depression (negative response to the clinical depression question and CES-D10 score < 10); Group 2: current depression symptom (negative response to the clinical depression question and CES-D10 score ≥ 10); Group 3: positive depression but without current depression symptom (positive response to the clinical depression question and CES-D10 score was < 10); and Group 4: potential, recurrent depression (positive response to the clinical depression question and CES-D10 score ≥ 10).
2.2.3. Cardiovascular disease
Under the section of chronic condition, there were six questions related to CVD, i.e., (a) Heart disease: “Has a doctor ever told you that you have heart disease (including congestive heart failure, or chronic heart failure)?”; (b) Hypertension: “Has a doctor ever told you that you have high blood pressure or hypertension?”; (c) Angina: “Has a doctor ever told you that you have angina (or chest pain due to heart disease)?”; (d) Stroke: “Has a doctor ever told you that you have experienced a stroke or cerebrovascular accident (CVA)?”; (e) Myocardial infarction: “Has a doctor ever told you that you have had a heart attack or myocardial infarction?”; and (f) Peripheral vascular disease: “Has a doctor ever told you that you have peripheral vascular disease or poor circulation in your limbs?”. They were then grouped into two categories: the first one is heart related disorders (HRD), which included heart disease, angina, and myocardial infarction; the second one is peripheral/vascular related disorders (PRD), which included high blood pressure or hypertension, stroke or CVA, and peripheral vascular disease.
2.2.4. Covariates
The following covariates were considered when modeling the association between CVD and depression: age (years), sex (male vs. female), education (< post-secondary; post-secondary or some college degree; and bachelor's degree or above), marital status (married or living with a partner vs. other), immigrant status (yes vs. no), ethnicity (Caucasian vs. other), annual household income (< $20,000; $20,000–$50,000; $50,000–$100,000; ≥ $100,000), alcohol use (non-drinker; less than once a month; more than once a week during the past 12 months). Smoking (non-smoker; former smoker; current smoker), number of close friends, moderate physical activity over 30 minutes per day over the past 7 days (yes vs. no), body mass index (BMI, kg/m2), and co-morbidity (number of other chronic diseases reported).
2.3. Statistical analyses
Weighted analysis was conducted for all analyses to ensure generalizability. For the univariate analysis, ANOVA was used for continuous variables, and Chi-square test for categorical variables. Odds ratio (OR) with 95% CI from multiple logistic models were used to examine the risk association of CVDs with depression status. HRD and PRD were each introduced individually as a dependent variable into the model and four groups of depression status assigned as the main independent variables with Group 1 as the reference group. Three models were created with model 1 adjusting for age, sex, and ethnicity; model 2 further adjusting for BMI, marital status, education, income, immigration status, number of close friends, and life style factors (alcohol, smoking, and physical activity); and model 3 further adjusting for the number of other co-morbid diseases. Sex-stratified analysis was conducted to examine whether the risk association between depression status and CVD was similar between sexes. To examine whether there is a risk association pattern in different age group, the risk association between depression status and CVD was also analyzed by age strata, i.e., aged 45–54 years, 55–64 years, 65–74 years, and ≥ 75 years, respectively. All analyses were conducted using SAS 9.4 (SAS Institute Inc., Cary, NC, USA). Statistical significance was set at two-sided alpha equal or less than 0.05.
3. Results
Overall, 17.3% of subjects were determined having a positive history of depression, and 15.3% had current depression symptom (i.e., CES-D10 score ≥ 10). The proportions of the four groups based on depression question and CES-D10 score are: 73.9% of participants in Group 1 (no depression); 9.9% were in Group 2 (current depression symptom); 10.6% were in Group 3 (depression without current symptom); and 5.6% were in Group 4 (potential, recurrent depression). In addition, 38.5% of them reported having at least one of the six self-reported CVDs, or 10.5% of participants were with HRD and 34.4% with PRD.
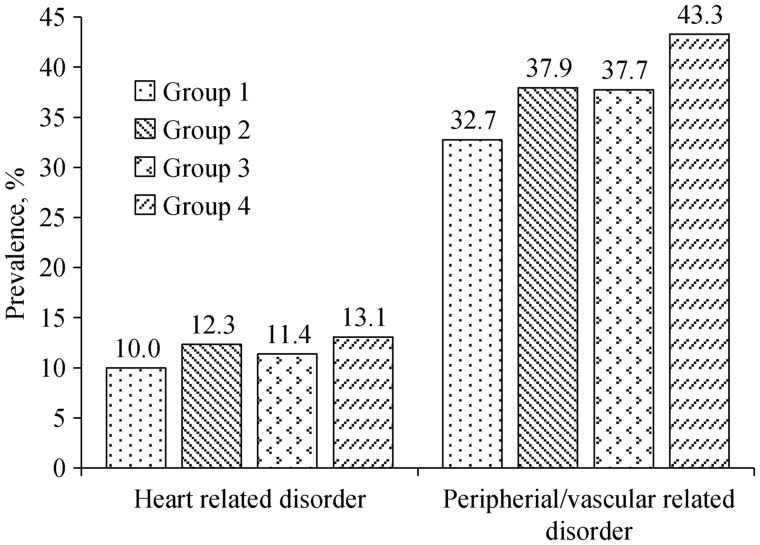
Table 1 shows the selected characteristics of the participants at baseline. Compared to individuals in Group 1 (no depression), persons in Groups 2–4 were more likely to be younger (except Group 2, which had a similar mean age as those in Group 1), women, and current smokers. They also had higher proportions of annual house income < $20,000, lower proportions of living with spouse/partner, of reporting moderate physical activity over 30 minutes per day, but higher mean levels of BMI, of comorbid diseases, and of fewer close friends. The differences for variables among groups in table 1 were all statistically significant at P-value less than 0.001. Figure 1 shows the prevalence of HRD and PRD by depression status. Clearly, compared to those without depression, individuals in other groups were with much higher prevalence of either HRD or PRD and those in Group 4 (potential, recurrent depression) in particular.
Table 1. Selected characteristics for 29,328 participants from the baseline data of the CLSA Comprehensive Cohort by depression status.
| Variable | Depression status |
P-value | |||
| Group 1 n = 21586 | Group 2 n = 2942 | Group 3 n = 3119 | Group 4 n = 1681 | ||
| Average age, yrs | 59.6 | 59.9 | 58.3 | 57.9 | *** |
| Female | 46.5% | 56.6% | 63.5% | 63.2% | *** |
| Married or living with partner | 79.5% | 67.8% | 70.8% | 57.1% | *** |
| White | 95.6% | 94.0% | 97.6% | 97.5% | *** |
| Education | *** | ||||
| Less than post-secondary | 19.6% | 26.1% | 18.0% | 26.4% | |
| Some college degree | 31.6% | 35.9% | 35.9% | 37.7% | |
| Bachelor's degree or above | 48.8% | 38.0% | 46.0% | 35.8% | |
| Immigrated | 18.3% | 21.9% | 13.6% | 15.6% | *** |
| Annual house income | *** | ||||
| < $20,000 | 3.0% | 9.4% | 5.5% | 15.2% | |
| $20,000–$50,000 | 16.5% | 25.7% | 21.2% | 27.3% | |
| $50,000–$100,000 | 33.2% | 34.6% | 34.3% | 32.1% | |
| ≥ $100,000 | 47.4% | 30.4% | 39.0% | 25.4% | |
| Alcohol intake during past 12 months | *** | ||||
| Non-drinker | 9.6% | 14.7% | 12.7% | 18.4% | |
| Less than once in a month | 10.2% | 15.6% | 12.0% | 17.6% | |
| More than once in a week | 80.2% | 69.7% | 75.4% | 64.0% | |
| Smoking | *** | ||||
| Non-smoker | 34.9% | 29.9% | 30.0% | 28.1% | |
| Former smoker | 57.5% | 57.2% | 59.8% | 53.7% | |
| Current Smoker | 7.6% | 12.9% | 10.2% | 18.2% | |
| Moderate Physical activity over 30 minutes | 14.4% | 10.3% | 11.6% | 10.5% | *** |
| Average BMI, kg/m2 | 27.5 | 28.0 | 28.5 | 29.7 | *** |
| Average of close friend | 5.6 | 4.6 | 4.8 | 3.9 | *** |
| Average of comorbid diseases | 2.4 | 3.1 | 3.0 | 3.7 | *** |
***P < 0.0001. BMI: body mass index; CLSA: Canadian Longitudinal Study on Aging. Group 1: CES-D10 score < 10 and negative clinical depression history; Group 2: CES-D10 score ≥ 10 and negative clinical depression history; Group 3: CES-D10 score < 10 and positive clinical depression history; Group 4: CES-D10 score ≥ 10 and positive clinical depression history.
Figure 1. Prevalence of HRD and PRD by history of depression status.
HRD: heart related disorders; PRD: peripheral/vascular related disorders.
The adjusted OR (95% CI) for HRD and PRD are shown in Table 2. Compared to those without depression (Group 1), all other groups showed an increased odds significantly regardless which disorder was in model 1, in which age, sex, and ethnicity were adjusted. The increased odds still existed after further adjusting for covariates including BMI, marital status, education, income, immigration status, number of close friends, and life style factors (model 2), and further adjusting for other comorbidities (model 3). However, the ORs were attenuated and no more statistical significant ORs were found in model 3 for people in Group 2 (current depression symptom); while people in Group 3 (depression without current symptom) had 36% higher odds for HRD [OR (95% CI) = 1.36 (1.18–1.58), P < 0.0001] and 20% higher odds for PRD [1.20 (1.09–1.32), P < 0.001], and people in Group 4 (potential, recurrent depression) were similar to those in Group 3 [1.31 (1.08–1.61), P < 0.01 for HRD and 1.17 (1.02–1.34), P < 0.05 for PRD].
Table 2. Adjusted OR (95% CI) of HRD and PRD by history of depression status for participants from the CLSA Comprehensive Cohort at baseline.
| Model 1 (n = 29,061) |
Model 2 (n = 25,197) |
Model 3 (n = 22,774) |
|||||||
| OR | 95% CI | P-value | OR | 95% CI | P-value | OR | 95% CI | P-value | |
| HRD | |||||||||
| Group 1 | 1.00 | 1.00 | 1.00 | ||||||
| Group 2 | 1.39 | 1.23–1.58 | < 0.0001 | 1.21 | 1.05–1.39 | 0.01 | 1.12 | 0.95–1.31 | NS |
| Group 3 | 1.55 | 1.37–1.76 | < 0.0001 | 1.44 | 1.25–1.64 | < 0.0001 | 1.36 | 1.18–1.58 | < 0.0001 |
| Group 4 | 2.01 | 1.71–2.36 | < 0.0001 | 1.53 | 1.28–1.83 | < 0.0001 | 1.31 | 1.08–1.61 | < 0.01 |
| PRD | |||||||||
| Group 1 | 1.00 | 1.00 | 1.00 | ||||||
| Group 2 | 1.30 | 1.19–1.41 | < 0.0001 | 1.15 | 1.04–1.27 | < 0.005 | 1.07 | 0.96–1.18 | NS |
| Group 3 | 1.46 | 1.34–1.58 | < 0.0001 | 1.29 | 1.18–1.41 | < 0.0001 | 1.20 | 1.09–1.32 | < 0.0005 |
| Group 4 | 1.88 | 1.69–2.09 | < 0.0001 | 1.36 | 1.20–1.54 | < 0.0001 | 1.17 | 1.02–1.34 | < 0.03 |
CI: confidence interval; CLSA: Canadian Longitudinal Study on Aging; HRD: heart related disorders; NS: non-statistical significance; OR: odds ratio; PRD: peripheral/vascular related disorders. Group 1: CES-D10 score < 10 and negative clinical depression history; Group 2: CES-D10 score ≥ 10 and negative clinical depression history; Group 3: CES-D10 score < 10 and positive clinical depression history; Group 4: CES-D10 score ≥ 10 and positive clinical depression history. Model 1: adjusted for age, sex, and ethnicity; Model 2: further adjusted for body mass index, marital status, education, income, immigrant status, number of close friends, and life style factors (alcohol, smoking, and physical activity); Model 3: further adjusted for comorbidities.
Table 3 shows the adjusted ORs (95% CIs) by sex separately. The covariates adjusted included all covariates aforementioned in model 3 except for sex. Compared to the reference (Group1), people in Group 2 showed no difference in either HRD or PRD. While people in Group 3 showed a comparable ORs between sexes, the ORs of HRD were 1.47 (95% CI: 1.19–1.82) for women and 1.26 (95% CI: 1.03–1.55) for men, and the ORs of PRD were 1.22 (95% CI: 1.08–1.38) for women and 1.18 (95% CI: 1.01–1.37) for men. The increased odds were observed for both sexes in Group 4 for HRD and PRD, but only ORs in men showed statistically significant, the ORs (95% CIs) for HRD and PRD were 1.39 (1.08–1.84) and 1.28 (1.03–1.58), respectively.
Table 3. Adjusted OR (95% CI) of HRD and PRD by sex and history of depression status for participants from the CLSA Comprehensive Cohort at baseline.
| HRD |
PRD |
|||
| OR | 95% CI | OR | 95% CI | |
| Female (n = 11,293) | ||||
| Group 2 (n = 1179) | 1.13 | 0.89–1.44 | 1.07 | 0.93–1.24 |
| Group 3 (n = 1560) | 1.47 | 1.19–1.82 | 1.22 | 1.08–1.38 |
| Group 4 (n = 780) | 1.27 | 0.95–1.69 | 1.12 | 0.94–1.33 |
| Male (n = 11,481) | ||||
| Group 2 (n = 902) | 1.11 | 0.90–1.37 | 1.04 | 0.89–1.22 |
| Group 3 (n = 909) | 1.26 | 1.03–1.55 | 1.18 | 1.01–1.37 |
| Group 4 (n = 405) | 1.39 | 1.05–1.84 | 1.28 | 1.03–1.58 |
Adjusted covariates include age, ethnicity, body mass index, marital status, education, income, immigrant, alcohol, smoker, physical activity, number of close of friend, and comorbidities. CI: confidence interval; CLSA: Canadian Longitudinal Study on Aging; HRD: heart related disorders; OR: odds ratio; PRD: peripheral/vascular related disorders. Group 1(reference): CES-D10 score < 10 and negative clinical depression history; Group 2: CES-D10 score ≥ 10 and negative clinical depression history; Group 3: CES-D10 score < 10 and positive clinical depression history; Group 4: CES-D10 score ≥ 10 and positive clinical depression history.
The adjusted ORs (95% CIs) of HRD and PRD by age strata are shown in Table 4. The covariates adjusted in the model included all variables aforementioned. Compared to those without depression (Group 1), people in Group 2, regardless which age stratum they were, showed no differences in the odds of HRD, and it was similar in PRD except that those aged 55–64 years showed a significant increase odds [OR (95% CI) = 1.25 (1.04–1.51)]. For people in Group 3, increased odds have been observed in all age strata, but only those aged 55–64 years showed statistical significance for HRD [OR (95% CI) = 1.79 (1.34–2.38)] and PRD [OR (95% CI) = 1.23 (1.05–1.43)]. For people in Group 4, the significantly increased odds was only observed among people aged 55–64 years for HRD [OR (95% CI) = 1.64 (1.21–2.33)].
Table 4. Adjusted OR (95% CI) of HRD and PRD by age groups and history of depression status for participants from the CLSA Comprehensive Cohort.
| HRD |
PRD |
|||
| OR | 95% CI | OR | 95% CI | |
| Age 44–55 yrs (n = 6163) | ||||
| Group 2 (n = 572) | 1.10 | 0.78–1.55 | 1.00 | 0.84–1.19 |
| Group 3 (n = 705) | 1.79 | 1.34–2.38 | 1.23 | 1.05–1.43 |
| Group 4 (n = 358) | 1.04 | 0.68–1.60 | 1.18 | 0.95–1.46 |
| Age 55–65 yrs (n = 7725) | ||||
| Group 2 (n = 681) | 1.21 | 0.91–1.60 | 1.25 | 1.04–1.51 |
| Group 3 (n = 984) | 1.15 | 0.89–1.48 | 1.11 | 0.95–1.30 |
| Group 4 (n = 471) | 1.64 | 1.21–2.23 | 1.14 | 0.91–1.43 |
| Age 65–75 yrs (n = 5414) | ||||
| Group 2 (n = 430) | 1.12 | 0.81–1.54 | 0.95 | 0.74–1.22 |
| Group 3 (n = 567) | 1.19 | 0.90–1.58 | 1.20 | 0.96–1.49 |
| Group 4 (n = 260) | 1.08 | 0.71–1.64 | 1.08 | 0.77–1.51 |
| Age over 75 yrs (n = 3472) | ||||
| Group 2 (n = 398) | 1.01 | 0.74–1.39 | 0.94 | 0.71–1.25 |
| Group 3 (n = 213) | 1.37 | 0.93–2.02 | 1.14 | 0.78–1.66 |
| Group 4 (n = 96) | 0.87 | 0.47–1.61 | 0.94 | 0.54–1.66 |
Adjusted covariates include age, sex, ethnicity, body mass index, marital status, education, income, immigrant, alcohol, smoker, physical activity, number of close of friend, and comorbidities. Group 1 (reference): CES-D10 score < 10 and negative clinical depression history; Group 2: CES-D10 score ≥ 10 and negative clinical depression history; Group 3: CES-D10 score < 10 and positive clinical depression history; Group 4: CES-D10 score ≥ 10 and positive clinical depression history. CI: confidence interval; CLSA: Canadian Longitudinal Study on Aging; HRD: heart related disorders; OR: odds ratio; PRD: peripheral/vascular related disorders.
4. Discussion
The findings from this study follow a line with the previous studies that clinical depression is more prevalent in women[15],[16] and more likely to be comorbid with CVDs.[17],[18] However, our results also suggest that the cardiovascular risk profile in a senior population may vary by history of depression status, sex, and age. For example, those in Group 4 (potential, recurrent depression) had the highest prevalence in either HRD or PRD than other groups even they were much younger and more likely to be women. A unhealthy profile, i.e., more likely to be a smoker, physically less active, with a higher BMI, less number of close friends, and more number of comorbidities may partially explain why these people had more prevalent cardiovascular problems. Yet after taking these factors into account, compared to people who had no depression (Group 1), they still had much higher increased odds for HRD and PRD. When the risk association was further examined by sex and age, the high cardiovascular risk association were more likely to be appeared in men, and more prevalent among younger adults. Our results are not contradictory to the findings from some cohort studies, in which they found that younger women with a suspected or established coronary artery disease (CAD) when depressed had substantially higher risk for CAD death;[19] or younger women with depression at the baseline had a much higher risk for ischemic heart disease death during the follow-up.[20] Our results may simply reflect the fact that at a given moment, mid-aged men with potential, recurrent depression are more likely to be with CVD related disorders. This goes alone with the results from a US adults' national representative sample, which suggest that lifetime depression at baseline may promote CVD through potentiating traditional cardiovascular risk factors.[21]
For individuals in Group 2, who might be with current depression symptom, even they were the oldest group among all four groups, their cardiovascular risk profile was similar to the reference (Group 1) even being analyzed by sexes. When examined by age stratum, however, a significantly increase odds ratio was observed among people aged 55–64 years for PRD. Literature indicates that compare to younger people, seniors are less likely to be depressed in population and also the gap of depression prevalence between sexes becomes insignificant when aging;[11] but on the other hand, depression is more common among seniors with CVD.[22] Our results suggest that those who were with current depression symptom were more likely to be older, but their CVD profile was similar to those without depression.
People in Group 3, depression without current symptom, had a similar demographic profile as those in Group 4, i.e., younger and more likely to be women but a slightly better lifestyle profile (i.e., less likely to be current smokers and slightly more active, and also had more friends). However, they had significantly higher adjusted odds for HRD and PRD, especially after further adjusting for comorbidity (model 3). Literature indicates that depression is a significant independent risk factor for incidence coronary heart disease and cardiovascular morbidity and mortality among individuals with an established heart disease.[23] There is no absolute conclusion whether treating depression will reduce risk for cardiac events among people with heart disease, but results from a recent study suggest that treating depression may reduce risk for major adverse cardiovascular events.[24] The results for this group in our study show that people with a positive history of depression but currently without symptom had a comparable cardiovascular profile as those who were potentially, recurrently depressed. All this suggests that a positive history of clinical depression is associated with an increased risk for CVDs, but it may need longitudinal study to examine the effectiveness treatment of depression on the risk of CVD.
This study shows a comprehensive picture of the relationship between CVD profile and depression status, which may help identifying the potential cardiovascular events for people with different depression status, thus form a more effective measure to deal with CVD risk among people with depression.
4.1. Limitations
Several limitations need to be noted when interpreting the findings. Firstly, this was a cross-sectional analysis of baseline data from the CLSA and any observed risk association cannot be interpreted as a causal-effect relationship; this would be particularly true among senior population, in which there is a potential overlap between CVD related disorders and depression symptoms; therefore, it is hard to distinguish which one comes first. Secondly, clinical depression was not determined using the Diagnostic and Statistical Manual of Mental Disorders but a positive response to the question of clinical depression history. Thus, it may have some misclassification between groups. In addition, a positive response to the clinical depression question may just indicate a lifetime clinical depression, but the CLSA doesn't have information to indicate what might be the type of depression disorder. Furthermore, whether people with recent depression episode were at a higher CVD risk than those who had it years ago or vice versa may need to be further studied in the future. Last but not least, the categories of CVD determined by the questions used in the CLSA may also be tricky since it relies on participant's self-report and cannot be verified the type of the disease, for example, for heart disease, it doesn't tell us whether it was a coronary heart disease or a congenital heart disease; for hypertension, it is unclear whether it was a primary or a secondary one, though coronary heart disease and primary hypertension are much more prevalent in the senior population. Thus, grouping these CVD related disorders into two broader categories, i.e., HRD and PRD, might only provide an alternative approach to examine the risk association between CVDs and depression. The strengths of the study may include large sample size with a broad representation of the Canadian senior population, which provided enough power to detect cardiovascular risk associations with depression categories, and the examination of the risk association by sex and age stratum allows us to estimate what potential role they play in the observed associations.
4.2. Conclusions
In conclusion, adults with depression are associated with an increased risk for CVDs and the risk association may vary by their depression status, sex and age.
Acknowledgments
This study was supported by the Government of Canada through the Canadian Institutes of Health Research (CIHR) under grant (LSA 9447 and the Canada Foundation for Innovation). All authors had no conflicts of interest to disclose and the opinions expressed in this manuscript are the author's own and do not reflect the views of the Canadian Longitudinal Study on Aging (CLSA). This research was made possible using the data/biospecimens collected by the CLSA, and the CLSA Baseline Tracking Dataset 3.3, Baseline Comprehensive Dataset 3.2, under Application Number 171003, to conduct. The CLSA is led by Drs. Parminder Raina, Christina Wolfson and Susan Kirkland.
References
- 1.WHO. World Health Statistics 2016: monitoring health for the SDGs. Annex B: tables of health statistics by country, WHO region and globally retrieved. World Health Organization; 2016. [Google Scholar]
- 2.Satistics Canada. Age and sex, and type of dwelling data: key results from the 2016 census. Statistics Canada; 2017. [Google Scholar]
- 3.Statistics Canada. Canada year book, population and demography: an aging population. Statistics Canada: 2012. [Google Scholar]
- 4.Chief Officer. Health status of Canadians 2016: report of the Chief Public Health Officer: how are we unhealthy? cardiovascular disease. Canada PHAo; 2016. [Google Scholar]
- 5.Dhar AK, Barton DA. Depression and the link with cardiovascular disease. Front Psychiatry. 2016;7:33. doi: 10.3389/fpsyt.2016.00033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kang HJ, Kim SY, Bae KY, et al. Comorbidity of depression with physical disorders: research and clinical implications. Chonnam Med J. 2015;51:8–18. doi: 10.4068/cmj.2015.51.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MacMillan HL, Patterson CJ, Wathen CN, et al. Screening for depression in primary care: recommendation statement from the Canadian Task Force on Preventive Health Care. CMAJ. 2005;172:33–35. doi: 10.1503/cmaj.1030823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vilagut G, Forero CG, Barbaglia G, et al. Screening for depression in the general population with the Center for Epidemiologic Studies Depression (CES-D): a systematic review with meta-analysis. PLoS One. 2016;11:e0155431. doi: 10.1371/journal.pone.0155431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Craven MA, Bland R. Depression in primary care: current and future challenges. Can J Psychiatry. 2013;58:442–448. doi: 10.1177/070674371305800802. [DOI] [PubMed] [Google Scholar]
- 10.Collins KA, Westra HA, Dozois DJ, et al. Gaps in accessing treatment for anxiety and depression: challenges for the delivery of care. Clin Psychol Rev. 2004;24:583–616. doi: 10.1016/j.cpr.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 11.Patten SB, Williams JV, Lavorato DH, et al. The association between major depression prevalence and sex becomes weaker with age. Soc Psychiatry Psychiatr Epidemiol. 2016;51:203–210. doi: 10.1007/s00127-015-1166-3. [DOI] [PubMed] [Google Scholar]
- 12.Raina PS, Wolfson C, Kirkland SA, et al. The Canadian longitudinal study on aging (CLSA) Can J Aging. 2009;28:221–229. doi: 10.1017/S0714980809990055. [DOI] [PubMed] [Google Scholar]
- 13.Kimberlin CL, Pendergast JF, Berardo DH, et al. Issues related to using a short-form of the Center for Epidemiological Studies-Depression Scale. Psychol Rep. 1998;83:411–421. doi: 10.2466/pr0.1998.83.2.411. [DOI] [PubMed] [Google Scholar]
- 14.Björgvinsson T, Kertz SJ, Bigda-Peyton JS, et al. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment. 2013;20:429–436. doi: 10.1177/1073191113481998. [DOI] [PubMed] [Google Scholar]
- 15.Goldstein JM, Holsen L, Huang G, et al. Prenatal stress-immune programming of sex differences in comorbidity of depression and obesity/metabolic syndrome. Dialogues Clin Neurosci. 2016;18:425–436. doi: 10.31887/DCNS.2016.18.4/jgoldstein. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kessler RC, McGonagle KA, Nelson CB, et al. Sex and depression in the National Comorbidity Survey. II: Cohort effects. J Affect Disord. 1994;30:15–26. doi: 10.1016/0165-0327(94)90147-3. [DOI] [PubMed] [Google Scholar]
- 17.Glassman AH. Depression and cardiovascular comorbidity. Dialogues Clin Neurosci. 2007;9:9–17. doi: 10.31887/DCNS.2007.9.1/ahglassman. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Halaris A. Comorbidity between depression and cardiovascular disease. Int Angiol. 2009;28:92–99. [PubMed] [Google Scholar]
- 19.Shah AJ, Ghasemzadeh N, Zaragoza-Macias E, et al. Sex and age differences in the association of depression with obstructive coronary artery disease and adverse cardiovascular events. J Am Heart Assoc. 2014;3:e000741. doi: 10.1161/JAHA.113.000741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shah AJ, Veledar E, Hong Y, et al. Depression and history of attempted suicide as risk factors for heart disease mortality in young individuals. Arch Gen Psychiatry. 2011;68:1135–1142. doi: 10.1001/archgenpsychiatry.2011.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Polanka BM, Berntson J, Vrany EA, et al. Are cardiovascular risk factors stronger predictors of incident cardiovascular disease in U.S. adults with versus without a history of clinical depression? Ann Behav Med. 2018;52:1036–1045. doi: 10.1093/abm/kay007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang Y, Chen Y, Ma L. Depression and cardiovascular disease in elderly: current understanding. J Clin Neurosci. 2018;47:1–5. doi: 10.1016/j.jocn.2017.09.022. [DOI] [PubMed] [Google Scholar]
- 23.Carney RM, Freedland KE. Depression and coronary heart disease. Nat Rev Cardiol. 2017;14:145–155. doi: 10.1038/nrcardio.2016.181. [DOI] [PubMed] [Google Scholar]
- 24.Lavoie KL, Paine NJ, Pelletier R, et al. Relationship between antidepressant therapy and risk for cardiovascular events in patients with and without cardiovascular disease. Health Psychol. 2018;37:989–999. doi: 10.1037/hea0000602. [DOI] [PubMed] [Google Scholar]