Abstract
Background
Permanent pacing is the therapy of choice for treating severe and/or symptomatic bradyarrhythmias. The number of very elderly patients receiving pacemakers is increasing and little is known about survival in this specific subgroup. This study is aimed at assessing the actual survival of patients requiring pacing therapy at age > 85 years and investigating variables associated with death.
Methods
Between 2010 and 2017, 572 patients aged ≥ 85 years underwent pacemaker implantation for conventional bradycardia indications in Department of Cardiology, S. Chiara Hospital, Italy.
Results
Thirty percent of patients were ≥ 90-year-old and comorbidities were frequent. Fifty-seven percent of patients required pacing for prognostic reasons (acquired atrioventricular block), and the remaining for relief of bradycardia symptoms. A dual-chamber pacemaker was implanted in 34% of patients. The 5-year survival was 45% (standard error: 3%), and the 8-year survival was 26% (standard error: 4%). The risk of death was similar in patients who received pacemaker for symptom relief and for prognostic reasons in the overall population (HR = 1.19, 95% CI: 0.93–1.52, P = 0.156), as well as in the ≥ 90-year-old group (HR = 1.39, 95% CI: 0.92–2.11, P = 0.102). At multivariate analysis, following variables were associated with death: higher age, lower ejection fraction, dementia/dysautonomia and diagnosis of cancer. The pacing indication and the implantation of a single chamber pacemaker were not associated with worse prognosis.
Conclusions
This study showed a good life expectancy in patients aged ≥ 85 years who received a pacemaker. Strong risk factors for all-cause death were non-cardiac. Pacemaker therapy seems a clinically effective therapeutic option to improve survival and to control bradyarrhythmia-related symptoms in very elderly patients.
Keywords: Mortality, Pacemaker, The elderly
1. Introduction
Permanent pacing is the therapy of choice for treating severe bradyarrhythmia.[1] The number of very elderly patients receiving pacemakers is increasing,[2] but little is known about survival in this specific subgroup and about possible factors associated with worse prognosis. The assumption of persistent pacemaker benefit in very elderly patients is questionable, as any advantage of the device on arrhythmic death may be largely attenuated by non-arrhythmic mortality. However, European guidelines[1] do not consider any specific age limit for pacemaker implantation.
This study was aimed at assessing the actual survival of patients requiring pacing therapy at age of 85 years or more and investigating variables associated with death.
2. Methods
2.1. Study population
We retrospectively enrolled all consecutive patients in whom pacemaker implantation had been performed from January 2010 to December 2017 in Department of Cardiology, S. Chiara Hospital, Italy, and who were 85 years old or more at the time of implantation. Patients were required to have standard indications for permanent single- or dual-chamber pacing. The study was approved by the local ethics committee and informed consent was obtained from all patients. Baseline evaluation included demographics and medical history, clinical examination, 12-lead electrocardiogram and echocardiographic evaluation of left ventricular ejection fraction. Devices and pacing leads were implanted by means of standard techniques. Optimization of pacing parameters and pharmacological treatments were based on clinical evaluation by the attending physicians. During follow-up, patients returned for regular clinic visits. Mortality data were obtained by means of hospital file review or direct telephone contact.
2.2. Statistical analysis
Descriptive statistics are reported as means ± SD for normally distributed continuous variables, or medians with 25th to 75th percentiles in the case of skewed distribution. Categorical data were expressed as percentages. Mortality rates were summarized by constructing Kaplan-Meier curves, and the distributions of the groups were compared by means of a log-rank test. Cox regression was used to analyze possible predictors of death. All variables associated to a P-value < 0.05 on univariate analysis were entered into the multivariate regression analysis. A P-value < 0.05 was considered significant for all tests. All statistical analyses were performed by using STATISTICA software, version 7.1 (StatSoft, Inc., Tulsa, OK, USA).
3. Results
From January 2010 to December 2017, a total of 572 patients aged ≥ 85 years (mean age: 88 ± 3 years) with a standard indication for permanent pacing underwent single- or dual-chamber pacemaker implantation in Department of Cardiology, S. Chiara Hospital, Italy. Table 1 shows baseline clinical variables. Thirty percent of patients were ≥ 90 years old, 7% had an ejection fraction lower than 45%, 76% had arterial hypertension, 47% had history of atrial fibrillation. Pacemaker was implanted for atrioventricular block in 325 (57%) and for relief of bradycardia symptoms in 247 (43%). A dual-chamber pacemaker was implanted in 195 (34%) of patients.
Table 1. Demographics and baseline clinical parameters of the study population.
| Parameter | n = 572 |
| Age, ≥ 90-year-old | 169 (30%) |
| Male gender | 272 (48%) |
| Ejection fraction (EF) | |
| EF < 35% | 17 (3%) |
| 35% ≤ EF < 45% | 23 (4%) |
| 45% ≤ EF < 55% | 40 (7%) |
| EF ≥ 55% | 492 (86%) |
| Previous myocardial infarction | 70 (12%) |
| History of atrial fibrillation | 266 (47%) |
| Severe aortic stenosis | 35 (6%) |
| Moderate-severe mitral insufficiency | 85 (15%) |
| Arterial hypertension | 434 (76%) |
| Previous transient ischemic attack/Stroke | 92 (16%) |
| Diabetes | 108 (19%) |
| Chronic kidney disease | 168 (29%) |
| Vascular disease | 195 (34%) |
| Dementia/dysautonomia | 87 (15%) |
| Diagnosis of cancer | 37 (6%) |
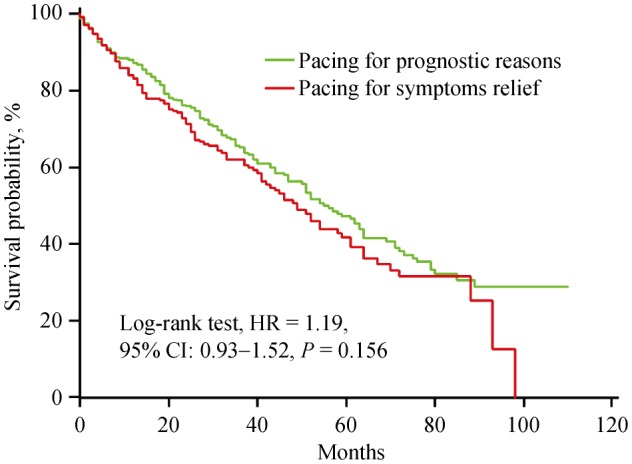
During a median follow-up of 37 months (25th to 75th percentile: 22, 58), 271 (47%) patients died for any reason. The 5-year survival was 45% (standard error: 3%), and the 8-year survival was 26% (standard error: 4%). The risk of death was higher in ≥ 90-year-old patients (HR = 1.69, 95% CI: 1.28–2.24, P < 0.001) (Figure 1). However, it was similar in patients who received pacemaker for symptom relief and for prognostic reasons in the overall population (HR = 1.19, 95% CI: 0.93–1.52, P = 0.156) (Figure 2), as well as in the ≥ 90-year-old group (HR = 1.39, 95% CI: 0.92–2.11, P = 0.102).
Figure 1. Kaplan-Meier estimates of time to death, stratified by age group: < 90-year-old versus ≥ 90-year-old.
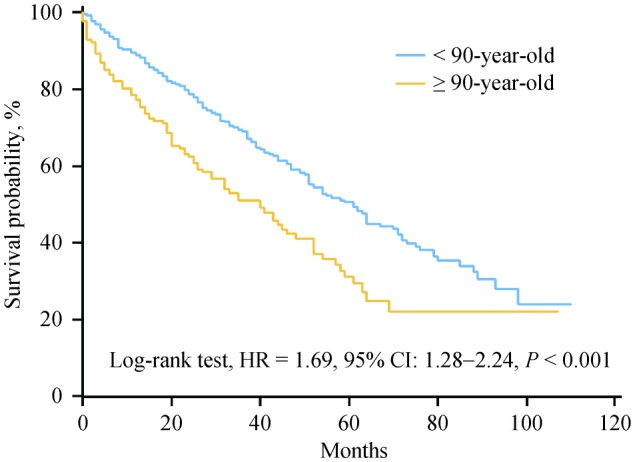
Figure 2. Kaplan-Meier estimates of time to death, stratified by pacing indication: prognostic reasons (acquired atrioventricular block) versus bradycardia symptoms relief.
Baseline parameters were evaluated by means of univariate and multivariate analyses in order to assess their ability to predict the occurrence of death during follow-up, as reported in Table 2. On multivariate analysis, higher age, lower ejection fraction, dementia/dysautonomia and diagnosis of cancer were confirmed as independent predictors of death. The pacing indication (prognostic reasons versus symptoms relief) and the implantation of a dual-chamber pacemaker were not associated with worse prognosis.
Table 2. Univariate and multivariate analyses of factors predicting death in the study population.
| Variables | Univariate analysis |
Multivariate Analysis |
||||
| HR | 95% CI | P-value | HR | 95% CI | P-value | |
| Age | 1.10 | 1.06–1.14 | < 0.001 | 1.09 | 1.05–1.13 | < 0.001 |
| Male gender | 0.96 | 0.75–1.21 | 0.731 | - | - | - |
| Ejection fraction < 55% | 0.60 | 0.43–0.84 | 0.003 | 1.35 | 1.14–1.61 | < 0.001 |
| Previous myocardial infarction | 1.08 | 0.75–1.56 | 0.691 | - | - | - |
| History of atrial fibrillation | 1.19 | 0..94–1.51 | 0.151 | - | - | - |
| Severe aortic stenosis | 1.58 | 0.95–2.61 | 0.079 | - | - | - |
| Moderate-severe mitral insufficiency | 1.31 | 0.97–1.78 | 0.078 | - | - | - |
| Arterial hypertension | 0.75 | 0.57–0.98 | 0.036 | 0.82 | 0.62–1.08 | 0.155 |
| Previous transient ischemic attack/Stroke | 1.04 | 0.74–1.46 | 0.805 | - | - | - |
| Diabetes | 1.30 | 0.97–1.74 | 0.086 | - | - | - |
| Chronic kidney disease | 1.42 | 1.10–1.82 | 0.007 | 1.27 | 0.98–1.66 | 0.071 |
| Vascular disease | 1.11 | 0.86–1.42 | 0.432 | - | - | - |
| Dementia/dysautonomia | 1.55 | 1.14–2.11 | 0.006 | 1.43 | 1.03–1.97 | 0.032 |
| Diagnosis of cancer | 1.60 | 1.01–2.51 | 0.045 | 1.61 | 1.01–2.58 | 0.049 |
| Bradycardia symptoms | 1.19 | 0.94–1.51 | 0.159 | - | - | - |
| Dual-chamber pacemaker | 0.60 | 0.46–0.78 | < 0.001 | 0.80 | 0.60–1.07 | 0.133 |
4. Discussion
This study showed a high survival in patients aged 85 years or more who received a pacemaker. Strong risk factors for all-cause death were not cardiac in nature. Moreover, we observed no survival difference between different indications for pacemaker implantation.
The proportion of elderly patients requiring pacemaker implantation has increased over the years due to the augmented life expectancy. In our region, the life expectancy for 85 years old people was 5.6 years for males and 7.2 years for females in 2010; and it was 6.2 years for males and 7.6 years for females in 2017.[3] Nonetheless, clinical evidence on the outcome of pacemaker therapy in very old patients is limited, mostly outdated and related to in-hospital mortality.[4]–[9] The observed 5-year survival was 45% in our patients aged 85 years or more. It compares well with previous studies on patients ≥ 80 years that showed a survival in the range between 40% and 49%.[6],[8] The survival after implantation was relatively high also in the subgroup of nonagenarians (more than 30% at five years), though it was obviously lower than that of younger patients. In addition to the age, other variables associated with survival were non-cardiac factors, i.e., dementia/dysautonomia and diagnosis of cancer. While, previous study found the presence of diabetes to be associated with all-cause mortality.[8] These results are expected, indeed these comorbidities are prevalent in elderly patients and are linked to frequent non-arrhythmic death.[8] Non-arrhythmic mortality may attenuate the benefits of pacemaker therapy and make pacemaker implantation a less cost-effective choice in very old patients.[10] We also observed an association between death and lower ejection fraction. The same association was observed in younger pacemaker recipients.[11] Similarly, congestive heart failure was previously shown to be a predictor of mortality in elderly patients.[6],[8] Nonetheless, only a minority of patients had depressed left ventricular function at implantation (14% of patients with ejection fraction < 55%) in the present study. This may explain the lack of association between pacing mode (single-versus dual-chamber) and survival. Indeed, the effects of right ventricular pacing on left ventricular function are more evident in patients with preexisting ventricular dysfunction.[12] In previous trials of pacemaker therapy,[13]–[15] in which most patients had normal systolic function, the time to the first heart failure event attributed to right ventricular apical pacing was between three years and five years. In the Mode Selection Trial (MOST),[16] about 10% of patients who received pacemakers for standard bradycardia indications experienced a heart failure hospitalization during a median follow-up of three years. It seems therefore that patients with a low-risk substrate (normal ejection fraction, no history of heart failure or myocardial infarction) well tolerate ventricular desynchronization due to ventricular pacing. In younger patients long-term pacing can lead to an unfavorable course over time, while no influence on prognosis can be detected in elderly patients. Our findings on the lack of association between pacing mode and survival also confirm that elderly patients may not benefit from more sophisticated pacemakers, particularly if the higher complication rate of dual-chamber systems is taken into consideration.[14] This is in contrast with what has recently been reported in the literature.[17]
In agreement with previous studies,[8],[18],[19] we observed no survival difference between different indications for pacemaker implantation. Cardiac pacing is not known to prolong survival in patients with sinus node dysfunction, and it is currently used only to relieve their symptoms attributed to bradycardia.[1] Nonetheless, we observed that the survival was similar between patients with sinus node disease and those with atrioventricular block, which receive pacemaker therapy for prognostic reasons even if asymptomatic. We observed this result in all patients as well as in the subgroup of nonagenarians.
4.1. Limitations
This study was not intended to investigate efficacy of pacing therapy in the elderly, which would require a randomized clinical trial. In addition, the cause of death was not determined in the study population. Dementia or dysautonomia were reported as a clinical impression during the admission visit and not confirmed using mini mental test or other specific tests. The main limitation of the present study is the retrospective design of the analysis. Indeed, some variability in the selection or management of patients during the inclusion period may have influenced the results. However, the study was carried out in a single center, the operators in charge of patient selection, device implantation and clinical management did not change during the study period, and all the patients included were consecutive.
4.2. Conclusions
This study showed a high survival in patients aged 85 years or more who received a pacemaker. Strong risk factors for all-cause death were non-cardiac in nature, and pacemaker therapy seemed a clinically effective therapeutic option for patients implanted for either prognostic reasons (atrioventricular block) or for relief of bradycardia symptoms.
Acknowledgments
All authors had no conflicts of interest to disclose.
References
- 1.European Society of Cardiology (ESC), European Heart Rhythm Association (EHRA) Brignole M, et al. 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: the task force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA) Europace. 2013;15:1070–1118. doi: 10.1093/europace/eut206. [DOI] [PubMed] [Google Scholar]
- 2.Proclemer A, Ghidina M, Gregori D, et al. Trend of the main clinical characteristics and pacing modality in patients treated by pacemaker: data from the Italian Pacemaker Registry for the quinquennium 2003-07. Europace. 2010;12:202–209. doi: 10.1093/europace/eup346. [DOI] [PubMed] [Google Scholar]
- 3.Provincia Autonoma di Trento Home Page. [(accessed on Sept 2019)]. http://www.statistica.provincia.tn.it.
- 4.Strauss HD, Berman ND. Permanent pacing in the elderly. Pacing Clin Electrophysiol. 1978;1:458–464. doi: 10.1111/j.1540-8159.1978.tb03507.x. [DOI] [PubMed] [Google Scholar]
- 5.Elizabeth JE, Green GJ. Permanent pacemakers in nonagenarians. Postgrad Med J. 1991;67:663–665. doi: 10.1136/pgmj.67.789.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shen WK, Hayes DL, Hammill SC, et al. Survival and functional independence after implantation of a permanent pacemaker in octogenarians and nonagenarians. A population-based study. Ann Intern Med. 1996;125:476–480. doi: 10.7326/0003-4819-125-6-199609150-00008. [DOI] [PubMed] [Google Scholar]
- 7.Schmidt B, Brunner M, Olschewski M, et al. Pacemaker therapy in very elderly patients: long-term survival and prognostic parameters. Am Heart J. 2003;146:908–913. doi: 10.1016/S0002-8703(03)00453-8. [DOI] [PubMed] [Google Scholar]
- 8.Udo EO, van Hemel NM, Zuithoff NP, et al. Long-term outcome of cardiac pacing in octogenarians and nonagenarians. Europace. 2012;14:502–508. doi: 10.1093/europace/eur329. [DOI] [PubMed] [Google Scholar]
- 9.Mandawat A, Curtis JP, Mandawat A, et al. Safety of pacemaker implantation in nonagenarians: an analysis of the healthcare cost and utilization project-nationwide inpatient sample. Circulation. 2013;127:1465e1–1465e2. doi: 10.1161/CIRCULATIONAHA.113.001434. [DOI] [PubMed] [Google Scholar]
- 10.Jahangir A, Shen WK, Neubauer SA, et al. Relation between mode of pacing and long-term survival in the very elderly. J Am Coll Cardiol. 1999;33:1208–1216. doi: 10.1016/s0735-1097(99)00005-4. [DOI] [PubMed] [Google Scholar]
- 11.Mazza A, Bendini MG, Leggio M, et al. Incidence and predictors of heart failure hospitalization and death in permanent pacemaker patients: a single-centre experience over medium-term follow-up. Europace. 2013;15:1267–1272. doi: 10.1093/europace/eut041. [DOI] [PubMed] [Google Scholar]
- 12.Lieberman R, Padeletti L, Schreuder J, et al. Ventricular pacing lead location alters systemic hemodynamics and left ventricular function in patients with and without reduced ejection fraction. J Am Coll Cardiol. 2006;48:1634–1641. doi: 10.1016/j.jacc.2006.04.099. [DOI] [PubMed] [Google Scholar]
- 13.Andersen HR, Nielsen JC, Thomsen PE, et al. Long-term follow-up of patients from a randomised trial of atrial versus ventricular pacing for sick-sinus syndrome. Lancet. 1997;350:1210–1216. doi: 10.1016/S0140-6736(97)03425-9. [DOI] [PubMed] [Google Scholar]
- 14.Connolly SJ, Kerr CR, Gent M, et al. Effects of physiologic pacing versus ventricular pacing on the risk of stroke and death due to cardiovascular causes. Canadian Trial of Physiologic Pacing Investigators. N Engl J Med. 2000;342:1385–1391. doi: 10.1056/NEJM200005113421902. [DOI] [PubMed] [Google Scholar]
- 15.Lamas GA, Lee KL, Sweeney MO, et al. Ventricular pacing or dual-chamber pacing for sinus-node dysfunction. N Engl J Med. 2002;346:1854–1862. doi: 10.1056/NEJMoa013040. [DOI] [PubMed] [Google Scholar]
- 16.Sweeney MO, Hellkamp AS. Heart failure during cardiac pacing. Circulation. 2006;113:2082–2088. doi: 10.1161/CIRCULATIONAHA.105.608356. [DOI] [PubMed] [Google Scholar]
- 17.Krzemień-Wolska K, Tomasik A, Wojciechowska C, et al. Prognostic factors in patients with an implanted pacemaker after 80 years of age in a 4-year follow up. Gerontology. 2018;64:107–117. doi: 10.1159/000481504. [DOI] [PubMed] [Google Scholar]
- 18.Pyatt JR, Somauroo JD, Jackson M, et al. Long-term survival after permanent pacemaker implantation: analysis of predictors for increased mortality. Europace. 2002;4:113–119. doi: 10.1053/eupc.2002.0233. [DOI] [PubMed] [Google Scholar]
- 19.Brunner M, Olschewski M, Geibel A, et al. Long-term survival after pacemaker implantation. Prognostic importance of gender and baseline patient characteristics. Eur Heart J. 2004;25:88–95. doi: 10.1016/j.ehj.2003.10.022. [DOI] [PubMed] [Google Scholar]


