Abstract
The significance of Nadi Pariksha is well understood and effectively used by Ayurveda practioners for assessing Tridoshas and various physiological and psychological states of the patient. The traditional texts Sarangadhara Samhita, YogaRatnakara, Basavarajeeyam and Bhavaprakasha have discussed the details of Nadi Pariksha in succinct set of slokas. Ayurveda has thousands of years of rich experience in Nadi Pariksha with strong literature support but is subjective in nature and the need for studying nadi with a scientific approach is well understood. Recently, pulse wave velocity has gained significant research interest as it is considered to be a strong indicator of cardiovascular disease; however, the relevance of pulse wave analysis to Nadi Pariksha has not been studied. In this review, traditional methods of Nadi Pariksha as defined in Ayurveda classics and the recent advances in pulse wave analysis are discussed. As per classical texts, qualities or properties of pulse such as pulse movement (gati), speed of the pulse (vega), stability of the pulse (sthiratva) and hardness of the artery (kathinya) play major role in Nadi Pariksha and in the current review these properties were analyzed and compared with the modern pulse parameters namely pulse wave velocity, pulse rate variability and arterial stiffness. The significance of pulse wave velocity in cardiovascular studies is discussed and the need for extending these studies to Ayurveda is highlighted.
Keywords: Gati, Kathinya, Pulse wave velocity
1. Introduction
Ayurveda is well known for Nadi Pariksha and classical texts have emphasized its significance in assessment of Tridoshas which are the basis of disease diagnosis and prognosis [1], [2], [3], [4]. There is a precise description of dosha predominance in the texts which can be sensed from specific locations on radial artery and accordingly vata dosha is felt at the root of the thumb which can be sensed with index finger, next to it is pitta dosha which can be sensed with middle finger followed by kapha dosha sensed by ring finger. As per ayurveda balanced Tridoshas represent the sound health and vitiated doshas lead to diseases. According to Yoga Ratnakara all the diseases can be diagnosed from Nadi and it was compared with strings of veena playing all the ragas which signifies the importance of Nadi Pariksha [3]. The speed, stability and gati of the pulse vary with the aggravated doshas and assessing such variations with Nadi Pariksha is an art and science of its own. The traditional ayurvedic practitioners were adept in pulse based diagnosis and used to diagnose the diseases effectively by just placing fingers on the radial artery.
Ayurveda has rich experience in pulse based diagnosis but it is subjective in nature and is highly dependent on skill of the physician. In recent past there is a growing research interest in acquiring the pulse from Tridosha locations and analyzing the pulse wave forms scientifically in the context of ayurveda. The pulse patterns of vata, pitta and kapha doshas were studied in detail by Upadhyaya as part of the clinical and experimental studies on Nadi Pariksha using Dudgeon Sphygmograph [5]. It was a detailed study covering the systematic review of ayurvedic literature, hemodynamics and statistical analysis of pulse patterns representing vata, pitta and kapha doshas of normal and diseased persons. The mean pulse rate and mean pulse pressure were studied across vata, pitta and kapha doshas and the significance of pulse parameters rate, rhythm, volume, force, tension, character and hardness of the artery were analyzed in the context of ayurveda. In similar lines Vasant has analyzed the physiological significance of pulse parameters gati (movement), vega (rate), tala (rhythm), bala (force), tapamana (temperature), akruti (volume and tension) and kathinya (consistency of the vessel wall) across vata, pitta and kapha doshas [6].
These initial studies accentuated the importance of the pulse parameters in analyzing Tridoshas in more scientific way compared to qualitative analysis. In this review the pulse measuring locations used in Tridosha analysis were highlighted and qualities or properties of Nadi as explained in ayurveda classics were discussed. The physiological significance of qualities of Nadi was analyzed and compared them with the modern pulse parameters which includes pulse wave velocity, arterial stiffness and pulse rate variability. Recent advances in pulse wave analysis were highlighted and the relevance of pulse wave analysis techniques to Nadi Pariksha was underscored. As part of the review various pulse measuring instruments used in current research and its application to Tridosha analysis were discussed. Traditional practices in Nadi Pariksha were manual and there were no instruments available for measuring the pulse whereas modern pulse wave analysis makes use of instruments both in clinical and research applications. In this review the role of modern instruments in studying the traditional pulse parameters was discussed.
The ancient texts of ayurveda were included in the study of Nadi Pariksha. The ayurveda texts included were Sarangadhara Samhita, Yoga Ratnakara, Basavarajeeyam and Bhavaprakasha. Nadi Vijnana by Upadhyaya and Secrets of the Pulse by Vasant were also included in the study of traditional practices of Nadi Pariksha. A detailed search was undertaken using key words Nadi, Nadi Pariksha in pubmed, google scholar, science direct and google. The search yielded only six papers which discussed Nadi Pariksha [7], [8], [9], [10], [11], [12], [13] as per classical texts and there were no papers discussing the relevance of recent advances in pulse wave analysis to Nadi Pariksha which underlines the need for a comprehensive review of Nadi Pariksha.
2. Pulse parameters
Traditionally Nadi Pariksha was done by sensing the pulse at three locations on radial artery and assessing doshas from palpation of the pulse. The qualities or properties of the Nadi are vital in assessing doshas as part of Nadi Pariksha. The classical texts have emphasized the significance of gati, a unique quality of the pulse, as part of Nadi Pariksha and as per texts gati plays a key role in disease diagnosis [1], [2], [3], [4]. There is no equivalent term for gati in modern medicine and pulse movement is the closely matching term in modern medicine which can be associated to gati. There are many other qualities of pulse apart from gati (pulse movement) which texts have highlighted and in this review the gati and other qualities of pulse were discussed in detail.
As per Ashtanga Hridayam guru (heavy), manda (slow), hima (cold), snigdha (unctuous), slakshna (smooth), sandra (solid), mridu (soft), sthira (stable), sukshma (subtle), visada (non slimy) and their opposites laghu (light), tikshna (quick, fast), usna (hot), ruksha (dry), khara (roughness) drava (liquid), kathina (hard), cala (moving), sthula (big), picchila (slimy) are twenty qualities or gunas which play key role in disease diagnosis and specifically in assessing doshas [14]. The qualities of pulse also need to be understood from these properties and the review of classical texts revealed that the texts have used the terms manda (slow), vega (fast), sthira (stable), capala (unstable), kathina (hard), sukshma (subtle) and picchila (slimy) while explaining the qualities of pulse [1], [2], [3], [4]. The texts have explained the significance of the pulse properties, but in qualitative manner which is subjective in nature and the need for quantitative description of these properties is well understood in the light of evidence based research. This necessitates the review of pulse properties defined in classical texts with a view to understand the physiological significance of the pulse and identify the modern pulse parameters which can be associated to the traditional pulse properties.
The qualities manda (slow), vega (fast), sthira (stable), capala (unstable) and kathina (hard) are of research significance as these qualities or properties are measurable and can be associated to modern pulse parameters. The terms manda (slow) and vega (fast) correspond to the speed or velocity of the pulse and in Sarangadhara Samitha while explaining Nadi Pariksha vidhi the term vega is used for increased pulse rate and ksheena and manda are the terms used for decreased pulse rate [4]. The term vega can be closely associated to speed of velocity of the pulse and can be associated to modern pulse parameters such as pulse rate and pulse wave velocity.
The stability of the pulse has been dealt with in detail in the texts while explaining Nadi Pariksha and the texts have used terms sthir (stable) and capal (unstable) while explaining the stability of the pulse [3], [4]. The stability is referred as sthiratva in doshadi vijnaniya adhyaha (sutrasthana) of Ashtanga Hridayam while explaining prakruta dosha karma [14]. The texts have not used the term sthiratva while explaining Nadi Pariksha but this term can be used to represent the stability of the pulse and can be closely associated to modern parameter pulse rate variability. As stable pulse is more rhythmic in nature the term tala which corresponds to rhythm can also be used to represent stability of the pulse and Vasant has used the term tala in Secrets of the Pulse [6]. In this review the term sthiratva has been used to represent the stability of the pulse as it is used in most of the classical texts.
The texts have used the term kathinya to explain the hardness of the artery and reference to kathinya is available only in Basavarajeeyam. In dviteeya prakarana of Basavarajeeyam while explaining the signs of mrityu nadi the term kathinya has been used and in triteeya prakarana of Basavarajeeyam the term kathinya is used to explain the nature of kapha [1]. The term kathin (hard) represented as kathinya corresponds to hardness of the artery and can be closely associated to modern pulse parameter arterial stiffness. Vasant [6] has used the term consistency of the vessel wall to explain kathinya whereas Upadhyaya [5] has used the term condition of the vessel wall for the same. In this review the term hardness of the artery is used to represent kathinya and is associated to arterial stiffness which is measurable and has research significance.
In summary gati (pulse movement), vega (speed of the pulse), sthiratva (stability of the pulse) and kathinya (hardness of the artery) are identified as measurable qualities of Nadi which can be closely associated to modern pulse parameters pulse movement, pulse wave velocity, pulse rate variability and arterial stiffness respectively. In this review the qualities of Nadi have been discussed in line with the modern pulse parameters with a view to bring out the physiological significance behind Nadi Pariksha.
2.1. Gati (pulse movement)
The dosha predominance can be well assessed with gati which is a very unique way of diagnosis in ayurveda wherein the movement of the pulse has been compared with the movement of animals, birds and reptiles. According to the texts the movement of vata pulse, well known as sarpa gati, will be curved resembling movement of snake (sarpa) and leech (jaluka). The curved and zigzag nature of movement is the significance of vata pulse and in Basavarajeeyam the vata pulse has been explained to be of vakra and kutil in nature which signifies the curved movement [1]. Bhavaprakasha has not compared the gati with the movement of animals or birds but similar to Basavarajeeyam explained it to be of vakra in nature [2]. The movement of pitta pulse, well known as manduka gati, was compared with the movement of frog which will be hopping and jumping in nature and was explained with the words capal and utplutya which signifies the jumping nature. The slow movement (manda gati) is the significance of kapha pulse, well known as hamsa gati, which has been compared with the movement of swan. The ayurveda texts have explained the gati of the pulse when more than one dosha is present and according to the texts gati will be of sarpa and manduka in nature if both vata and pitta doshas are in aggravation, similarly it will be of sarpa and hamsa in nature if vata and kapha doshas are in aggravation and will be of manduka and hamsa in nature if pitta and kapha doshas are in aggravation. It is quite evident from the texts that gati plays a significant role in assessing the dosha predominance and traditional ayurveda doctors were adept in assessing gati from nadi.
2.1.1. Pulse movement
The traditional practice of assessing gati has been in practice for thousands of years but it is very subjective in nature and in the current context of evidence based research it is important to assess the nature of gati in scientific manner with a clear understanding of its physiological significance. Upadhyaya as part of his clinical and experimental studies on Nadi Pariksha discussed the physiological significance of gati from rate, volume and character of the pulse and according to him vata pulse signifies the rate of the pulse to be fast, volume to be small and character to be curvilinear resembling sarpa gati, if the rate is slow, volume to be high and character is of jumping in nature it resembles pitta pulse and slow rate with volume in between vata and pitta resembles kapha pulse [5]. In another study by Joshi, nadi patterns of healthy and diseased persons were analyzed using computational models with promising results [12]. These initial studies highlight the physiological significance of gati but needs thorough validation to establish the physiological significance of gati and its nature across Tridoshas in various states of the health. As it is quite evident from the texts that gati plays an important role in assessing dosha, it is utmost important that current research in ayurveda should focus on the ways of validating gati in a measurable way.
2.2. Vega (speed of the pulse)
The speed of the pulse is another aspect which ayurveda has laid much importance in understanding various physiological, psychological and pathological states of the person. According to Sarangadhara and Bhavaprakasha [2], [4], the increase in lust and anger result into fast nadi and on the other hand nadi will be slow due to the increase in sorrow and fear. Sarangadhara has related the speed of the nadi to digestive fire and said nadi will be fast when the digestive fire is active and will be slow when the digestive fire is weak. Traditionally ayurveda doctors used to assess speed of the pulse from nadi but now with the advent of bio medical instruments measuring the speed of pulse has become simple and sophisticated. The pulse rate is well known measure of the speed of pulse and has been widely used in clinical practice which gives initial assessment of state of the health but warrants the need for further investigations to diagnose the disease. Pulse wave velocity is another parameter with significant research interest and can be associated to vega and there is a need to study this parameter in the context of ayurveda.
2.2.1. Pulse wave velocity
The blood flows faster in aorta compared to peripheral network and the speed varies from meters per second in aorta to mm per second in peripheral network. The velocity of the pulse wave is termed as pulse wave velocity (PWV) and normally ranges from 5 to 15 m/s. In the recent past pulse wave velocity (PWV) is considered as an indicator of cardiovascular risk and has gained significant research interest [15]. The longitudinal studies have shown that aortic PWV is a strong predictor of future cardiovascular events and all cause mortality [16]. The longitudinal studies on aortic and carotid stiffness in predicting the cardio-vascular disease are listed in Table 1 [17]. The European Society of Hypertension and European Society of Cardiology has suggested a threshold exceeding 12 m/s as a conservative estimate of significant alterations in aortic function of hypertensive patients and later the threshold has been adjusted to 10 m/s considering the true anatomical distance traveled by pulse wave [18]. The studies on the subjects with hypertension, end stage renal disease and geriatrics have confirmed the predictive value of aortic PWV especially in assessing the cardiovascular events [19], [20], [21].
Table 1.
Longitudinal studies on aortic and carotid stiffness.
| Measurement site | Type of patient (Reference) | Follow up (years) | Mean age |
|---|---|---|---|
| Aortic PWV (Regional arterial stiffness) | End Stage Renal Disease [19] | 6 | 51 |
| Hypertension [21] | 9.3 | 50 | |
| Elderly (>70) [20] | 2.5 | 87 | |
| End Stage Renal Disease [48] | 5.2 | 55 | |
| Hypertension [29] | 5.7 | 51 | |
| Impaired Glucose Tolerance [49] | 10.7 | 51 | |
| Hypertension [50] | 7.9 | 51 | |
| Elderly [51] | 4.6 | 74 | |
| General Population [15] | 10 | 64 | |
| General Population [52] | 9.4 | 55 | |
| Elderly [53] | 4.1 | 72 | |
| Ascending aorta (invasive) | Recurrent acute Coronary Heart Disease [54] | 3 | 55 |
| Carotid stiffness (local stiffness) | End Stage Renal Disease [55] | 2.1 | 58 |
| End Stage Renal Disease [56] | 7.9 | 43 |
The studies have shown significant results with pulse wave velocity in modern medicine and in the context of ayurveda the role of PWV in Tridosha analysis need to be explored. The pulse wave velocity may not be directly related to vega defined in traditional text but can be closely associated to it and the variations in doshas can be studied by measuring the pulse wave velocity. The dosha predominance has been discussed in classical texts of ayurveda and according to the texts kapha dominance can be seen in childhood, pitta dominance in middle age and vata dominance in old age. Secondly as per ayurveda nature of vata corresponds to fastness, pitta corresponds to medium speed and kapha corresponds to slowness. The studies have shown that the pulse wave velocity measured using carotid femoral technique increases with age and hence pulse wave velocity can be considered as an important pulse parameter in studying dosha dominance and classifying doshas. Carotid femoral technique is gold standard and as a first step it can be used to study the pulse wave velocity in the context of Tridosha analysis.
2.3. Sthiratva (stability of the pulse)
The ayurveda classics have discussed the stability of the pulse in detail with a mention of intermittent nadi which will be sometimes slow, sometimes fast and sometimes stops in between. Basavarajeeyam has used the term sthitva sthitva to explain the intermittent pulse while explaining the qualities of sannipatha nadi [1]. As per the texts nadi which is intermittent in nature and is sensed in the locations other than the specified place indicates to be fatal which may lead to early death of the patient. Basavarajeeyam [1] and Yoga Ratnakara [3] have termed it as asadhya nadi and as per Basavarajeeyam it is the nature of mrityu nadi also. The stability of the pulse also depends on various physiological and psychological states of the person. According to Sarangadhara Samhita nadi will be strong and steady in healthy persons and the nadi of a hungry person will be irregular when compared to that of a person who has just taken the food [4].
2.3.1. Pulse rate variability
Traditionally rhythm of the pulse is felt from the palpation of the pulse which is more qualitative in nature but with instruments it is possible now to acquire the pulse as time series enabling the rhythm of the pulse to be analyzed in quantitative manner. In the recent past there is a growing research interest in studying pulse rate variability (PRV) as surrogate marker of heart rate variability (HRV) [22], [23], [24]. There are no equivalent terms in traditional texts which can be compared with PRV but intermittent nadi can be closely associated to PRV as the nature of intermittent nadi can be well understood by looking into pulse rate variability and missing peaks, beat to beat alterations in pulse interval are some of the important parameters which can explain the intermittent nadi. The beat to beat alterations of the pulse wave acquired using Nadi Tarangini showed significant variations across different age groups and disorders [25]. The arterial pulse intervals (API), analyzed across time domain, frequency domain and non linear measures showed significant variations across age and disorders [26]. The stability or rhythm of the pulse has a significant role in Nadi Pariksha but there was no detailed description in the texts about its association with Tridoshas. As the pulse acquisition has become much more sophisticated there is a need to study the association of pulse rate variability with Tridoshas. An indepth study of intermittent nadi is the need of the day as it is considered to be serious as per the texts and extending PRV analysis to Tridoshas can be a significant step in Nadi Pariksha.
2.4. Kathinya (hardness of artery)
The hardness of the artery is closely associated to kathinya and only Basavarajeeyam has discussed the nature of kathin nadi in detail [1]. As per Basavarajeeyam vata nadi will be hard and the hardness of the artery has been explained with the words kathor and kathin whereas the hardness of the artery due to pitta and kapha doshas was not mentioned. The hardness (kathin) and roughness (khara) of the artery corresponds to vata dosha as per ayurveda and Basavarajeeyam compared vata nadi with string of veena which signifies the hardness of the vata nadi. The blood flow in hardened arteries will be fast compared to normal arteries which implies that vata pulse will be fast which is in agreement with ayurveda. According to Basavarajeeyam if nadi is kathin, very slow moving in a curved manner, if it is displaced from its original position then it is considered as mrityu nadi and is an indicator for early death of the patient.
2.4.1. Arterial stiffness
The arteries stiffen due to age and atherosclerosis and recently the arterial stiffness measured from pulse wave velocity (PWV) has gained significant research importance as it is considered to be strong predictor of cardio-vascular events [16], [27] and Alberto et al. have discussed in detail the role of arterial pulse wave analysis in cardiovascular risk assessment [28]. A longitudinal study by Boutouyrie provides the first direct evidence that the aortic stiffness is an independent predictor of primary coronary events in hypertensive patients [29] and in another independent study by Laurent, the aortic stiffness is confirmed to be in an independent predictor of all cause and cardiovascular mortality in hypertensive patients [21]. The pulse wave velocity, a surrogate measure of arterial stiffness, closely corresponds to the description of mrityu nadi.
The stiffness index (SI) is a measure of arterial stiffness and is measured from radial artery which closely corresponds to the volume pulse measured using photoplethysmograph (PPG). The SI measured from digital volume pulse (DVP) of PPG is strongly associated to cardiovascular risk score emphasizing the significance of its utility in cardiovascular risk stratification [30]. In our previous study we have seen that the SI measured from radial artery using Nadi Tarangini, a pulse acquisition system, has shown significantly high values at vata location for diabetes compared to non-diabetes and SI was negatively correlated to fasting plasma glucose in non diabetes subjects [31]. The study has shown SI at pitta location was significantly high compared to vata and kapha locations which might be due to the fact that the average age of the subjects both in diabetes and non-diabetes groups is around 50 years a pitta dominant age. Nadi Tarangini has three linearly placed pressure transducers which can be placed on the Tridosha locations of radial artery and the pulse will be acquired from vata, pitta and kapha locations. The advantage of such a system is that the arterial stiffness measured from three locations can be analyzed simultaneously and initial studies with Nadi Tarangini have shown that the arterial stiffness varies significantly across vata, pitta and kapha locations. The pressure wave as it propagates from central to peripheral arteries gets amplified at peripheral artery due to multiple reflections from various reflection sites and the reflection sites are closer to peripheral arteries when compared to central arteries. As a result due to the pulse amplification, peripheral arteries do not give accurate results in cardiovascular studies and hence the arterial stiffness measured from peripheral arteries was not used as a surrogate for aortic and carotid stiffness [17] and there are very limited cardiovascular studies with radial artery. As radial artery plays a major role in ayurveda, SI measured from radial artery can be considered as significant parameter in Tridosha analysis. As the significance of arterial stiffness is well understood from the texts of ayurveda and also from the recent studies, there is a need to study the arterial stiffness in the context of Tridosha analysis.
3. Pulse locations
Ayurveda has laid much emphasis on sensing the pulse at radial artery primarily to assess doshas but it has not limited the pulse location to just radial artery but has clearly defined that the pulse can be sensed from eight locations. The classical text Basavarajeeyam has mentioned about eight locations to sense nadi and accordingly there are two at radial artery, two at ankle, two at neck region and two at nasal region [1]. It is also mentioned that the knowledge of vata, pitta and kapha doshas can be obtained from radial artery and Nadi Pariksha based on radial artery has been widely practiced as it is important to assess Tridoshas for any disease diagnosis and treatment. Though radial artery plays a major role in disease diagnosis and treatment, nadi at neck and nasal regions was also considered as important nadi in diagnosis and prognosis of disease. The fear, sorrow, anger, lust and fever are some of the symptoms which can be sensed from the nadi at neck and similarly the diseases pertaining to head, eyes and ears can be diagnosed from the nadi at nose. The status of life and health, fever and its relief are sensed from nadi at ankle. It is evident from the literature of Ayurveda that nadi pariksha has a major role in disease diagnosis and is not limited to radial artery but extended to other arteries.
As per modern physiology pulse is palpated at radial, carotid, femoral, brachial and ankle arteries and this is in line with the description in ayurveda except that there was no mention of femoral artery in ayurveda and arteries at nasal region in modern physiology are not highlighted. The significance of radial artery based pulse diagnosis is well understood in ayurveda and has been widely practiced but the nadi at other locations are not explored much. On the other hand the radial artery has a very limited role in modern medicine and is limited to just measuring the pulse rate whereas they have given much emphasis on carotid, femoral, brachial and ankle arteries which were widely used in measuring the pulse wave velocity.
4. Pulse measurement techniques and instruments
The pulse parameters and their analysis play key role in disease diagnosis in both ayurveda and modern medicine. In the evidence based research, pulse measurement techniques and the instruments used for such measurements are very critical. There are multiple pulse measurement techniques for assessing arterial stiffness from central and peripheral arteries. The pulse wave velocity and stiffness index are measures of arterial stiffness and techniques are developed to assess arterial stiffness from pulse wave velocity and stiffness index. The standard pulse wave velocity measurement techniques are carotid femoral pulse wave velocity (cfPWV) and brachial ankle pulse wave velocity (baPWV). The carotid and femoral arteries are used for pulse wave velocity measurement in carotid femoral pulse wave velocity (cfPWV) technique whereas brachial and ankle arteries are used for pulse wave velocity measurement in brachial ankle pulse wave velocity (baPWV) technique. Stiffness Index (SI) is measured from the radial artery. In this section pulse measurement techniques and instruments used for measurement were discussed.
4.1. Carotid femoral pulse wave velocity (cfPWV) technique
The measurement of pulse wave velocity using carotid femoral pulse wave velocity is the standard technique and is considered to be non invasive, robust and reproducible method for assessing the arterial stiffness [32]. The carotid femoral pulse wave velocity (cfPWV) has gained significant research interest in the recent past and the pulse wave velocity measured with cfPWV technique is considered as gold standard [18]. In cfPWV technique pulse wave will be obtained at carotid and femoral arteries and the distance between these two arteries will be recorded. The pulse wave velocity, a surrogate measure of arterial stiffness, is considered as the ratio of distance between carotid and femoral arteries to the time taken for the pulse to travel from carotid to femoral arteries [32].
| Pulse Wave Velocity = Distance/pulse transit time from carotid to femoral |
The advantage with the cfPWV is that it is a gold standard but the process of measuring the arterial stiffness requires good amount of skill in acquiring the pulse [33]. The cfPWV technique is a non invasive, robust and reproducible method and is widely used in epidemiological studies [32].
The pulse transit time and measurement of distance between carotid and femoral arteries need to be understood while assessing pulse wave velocity using cfPWV. The pulse transit time is measured using foot to foot method wherein foot is considered to be the end of the diastole. The distance between carotid and femoral arteries is measured physically and is considered as an estimate of the true distance traveled by the pulse wave but the inaccuracies in the distance measured may lead to errors in the absolute value of PWV. As the true distance traveled by the pulse is critical for PWV it is recommended that the distance from carotid artery to sternal notch is subtracted either from the total distance between carotid and femoral arteries or from the distance between sterna notch to femoral artery [32].
4.2. Carotid femoral pulse wave velocity (cfPWV) measuring instruments
There are number of devices available today to measure the pulse wave velocity using cfPWV technique. Complior from Alam Medical, SphygmoCor from Atcor Medical, PulsePen from Dia Tecne, Vasera from Fucuda Denshi Co Ltd, Vicorder from Skidmore Medical Ltd are some of the instruments used for measuring the pulse wave velocity [34]. Complior and SphygmoCor are widely used in PWV based studies [35] and the way pulse transit time and distance between arteries are computed varies between these two devices.
The Complior (Alam-Medical, France) is based on pressure transducers and the pulse at carotid and femoral arteries is acquired simultaneously. The correlation algorithm is applied between the two simultaneous pulse recordings to determine the pulse transit time. The distance traveled by pulse is obtained by directly measuring the distance between carotid and femoral arteries [32], [35].
In the SphygmoCor system (Artcor, Sydney, Australia) high fidelity applanation tonometers are used for pulse acquisition and the pulse is acquired at carotid artery along with the ECG recording followed by femoral pulse acquisition with simultaneous ECG recording. The pulse transit time is computed by subtracting the time difference between ECG and carotid pulse peak from the time difference between ECG and femoral pulse peak. The distance traveled by the pulse is computed by subtracting the distance between sternal notch to carotid artery from the distance between sternal notch to femoral artery [32], [35].
The PulsePen [34] is another device which uses two methods in assessing the pulse wave velocity. In the first method two tonometers are used and the pulse is acquired simultaneously at both carotid and femoral arteries. This is similar to the method used in Complior. In the second method only one tonometer is used wherein pulse is acquired from carotid and femoral arteries separately and synchronized with ECG. This method is similar to SphygmoCor.
The Vasera [34] uses cardio-ankle vascular index (CAVI) as an index for arterial stiffness measurement but this device needs further validation. The Vicorder [34] is similar to Complior but the algorithms used are not clear and this device also needs further validation.
There are many other devices and methods used in assessing arterial stiffness and the abridged version of expert consensus document on arterial stiffness has summarized them [32]. Apart from the standard non imaging techniques the ultrasound and Magnetic Resonance Imaging (MRI) are the imaging methods used in assessing pulse wave velocity using which the path length can be directly measured which is the biggest advantage but is very expensive solution [36]. Recently many devices have come to the market but it is important to verify the scientific validity of such instruments before using them in research [34].
4.3. Brachial ankle pulse wave velocity (baPWV) technique
The brachial ankle pulse wave velocity (baPWV) is another technique introduced in Japan in 2000 to measure the pulse wave velocity from brachial and ankle arteries [37] The complexities involved in arterial stiffness measurement with cfPWV technique have been addressed in baPWV. The pulse wave velocity is measured in baPWV by connecting volume plethysmographic sensors to the cuffs connected to brachial and ankle locations. The pulse wave velocity is computed as the ratio of virtual arterial length between these two arteries to the pulse transit time from brachial to ankle arteries [37]. The virtual arterial length is estimated from the height of the subject which eliminates the need for physically measuring the distance between arteries [38].
The virtual arterial length is computed as shown below.
| Path length from heart to brachium (Lb) = 0.2195*height of the person (cm) − 0.20734 |
| Path length from heart to ankle (La) = 0.8129*height of the person (cm) + 12.238 |
| Virtual arterial path length = La − Lb |
The pulse acquisition and physical distance measurement have been extremely simplified in baPWV due to which it has gained significant clinical interest but there are number of questions and concerns on the measurement of arterial stiffness using baPWV which Sugawara has addressed thoroughly in his review [37]. The height based arterial path length computation grossly overestimates the actual path length resulting in overestimation of PWV values when compared with the arterial path length measured using MRI [39] but height based path length can be converted to actual length with an adjustment factor as PWV measured from height based path length is linearly correlated to PWV measured from actual path length [37]. As the baPWV technique is simple to use and pulse wave velocity is strongly correlated to pulse wave velocity measured using cfPWV, it has gained much of clinical and research interest and number of studies have been done using this technique [37], [40], [41], [42].
4.4. Brachial ankle pulse wave velocity (baPWV) measuring instruments
There are not many devices available for measuring pulse wave velocity using baPWV technique and AT-form PWV/ABI (Colin, Kamaki, Japan) and VP-2000 (Colin, Kamaki, Japan) are the devices widely used by researchers for measuring pulse wave velocity. The baPWV measuring devices consist of volume plethysmographic and oscillometric sensors, electrocardiogram and phonocardiogram. The volume pulse is measured using volume plethysmographic sensors, blood pressure is measured using oscillometric sensors, electrocardiogram is used to synchronize pulse at brachial and ankle arteries and phonocardiogram is used to detect the heart sound. In baPWV pulse wave velocity is measured by connecting volume plethysmographic sensors to the cuffs connected to brachial and ankle [40].
4.5. Stiffness index from radial artery
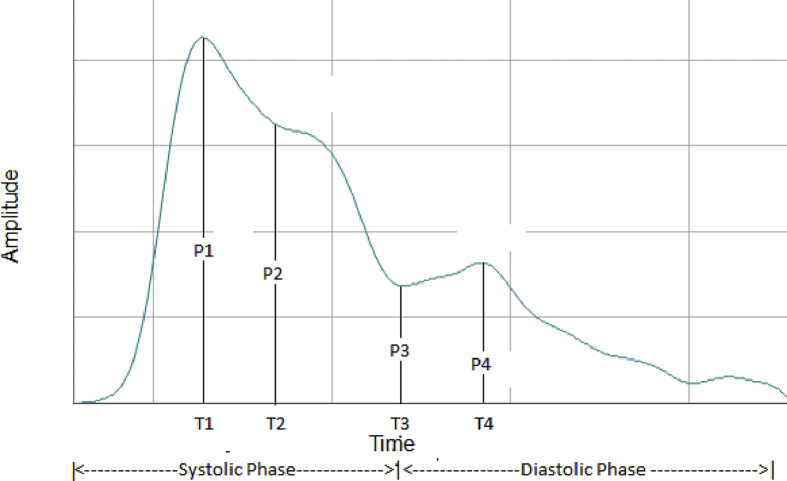
The arterial stiffness can be measured from radial artery also but the mechanism to measure the stiffness is different when compared to cfPWV and baPWV techniques. The pulse wave acquired from radial artery is composed of forward and reflected waves as shown in Fig. 1 wherein a peak appears in the forward wave during systolic phase of the pulse and a peak corresponding to reflected wave appears in diastolic phase of the pulse. The time taken for diastolic peak from the systolic peak depends on the stiffness of the arteries and height of the person. Hence stiffness index (SI) is measured as the ratio of height of the person to the time difference between systolic and diastolic peaks [43]. The pulse wave measured from radial artery is closely associated to the digital volume pulse measured from PPG and is related to it by a transfer function [44]. Hsein-Tsai have demonstrated the significant correlation between the stiffness index measured using PPG and radial artery [43]. Initial studies have shown promising results with radial artery but the significance of arterial stiffness measured from radial artery yet to be established. As per ayurveda kathinya is closely associated to arterial stiffness and there is a need to extend the studies on arterial stiffness to Tridosha analysis.
Fig. 1.
Pulse wave acquired using Nadi Tarangini, representing various peaks and time periods of the radial pulse. P1 = pulse amplitude at systolic peak; P2 = pulse amplitude at inflection point; P3 = pulse amplitude at dicrotic notch; P4 = pulse amplitude at Diastolic Peak; Time periods T1, T2, T3, T4 are measured from start of the systolic phase. T1 = time period at systolic peak; T2 = time period at inflection point; T3 = time period at dicrotic notch; T4 = time period at diastolic peak. SI = height of the person (cm)/(T4 − T1].
4.6. Stiffness index from radial artery
The sensor and semiconductor technologies have advanced further and precise pulse acquisition systems are available to measure the pulse at radial artery which resulted in resurgence of traditional Tridosha analysis in a more scientific manner. Nadi Tarangini [45], Nadi Yantra [46] and Nadi Pariksha Yantra [47] are some of the instruments available to acquire the pulse at Tridosha locations simultaneously. Nadi Tarangini is a pulse based acquisition system based on linearly spaced pressure transducers which converts the pulse pressure to electrical signal and provides the pulse wave in the form of time series [45]. The pulse wave acquired using Nadi Tarangini is similar to digital volume pulse from PPG with clear systolic and diastolic peaks in place.
As pulse measurement is well established and studies have shown significant results there is a need to extend these techniques and devices to the studies of ayurveda with a view to bring the physiological significance of Nadi Pariksha to limelight. The pulse wave velocity, pulse rate variability and arterial stiffness are some of the parameters which can be studied in the context of ayurveda and the scope can be increased further to analyze various other parameters which can add value to Nadi Pariksha.
5. Conclusion
Ayurveda has thousands of years of experience in Nadi Pariksha and classical texts have emphasized the significance of Nadi in disease diagnosis and prognosis. The texts have explained the nature of nadi and its variations in a very qualitative manner using the traditional parameters gati, vega, sthira, capala and kathinya. The traditional parameters are closely associated to the modern parameters such as pulse wave velocity, pulse rate variability and hardness of the artery which was discussed in this review thoroughly. It is important to study these modern parameters in the context of ayurveda to bring the hidden secrets of Nadi Pariksha to limelight. There is a dire need for extending the recent advancements in pulse measurement techniques and instruments to develop the framework for Nadi Pariksha and bring the scientific approach to pulse based diagnosis which is the need of the day.
Sources of funding
None.
Conflict of interest
None
Acknowledgments
We express our sincere thanks to S-VYASA in supporting this study.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
References
- 1.Basavarajeeyam Rangacharya V. 2007. Central council of research in ayurveda and siddha, New Delhi. [Google Scholar]
- 2.Murthy . vol. I. Chowkambha Krishnada Academy; Varanasi: 2008. (Bhavaprakasa of Bhavamisra). [Google Scholar]
- 3.SSB M . 2nd ed. vol. I. Chowkhamba Sanskrit Series Office; Varanasi: 2011. Yoga Ratnakara. [Google Scholar]
- 4.Murthy P.H.C. 2nd ed. Chowkhamba Sanskrit Series Office; Varanasi: 2007. Śārṅgadhara Samhita of Śārṅgadharacārya. [Google Scholar]
- 5.Upadhyaya . Chaukhamba Sanskrit Pratishthan; Delhi: 2009. Nadi Vijnana. [Google Scholar]
- 6.Vasant Dattatray L. Motilal Banarsidass Publishers; New Delhi: 2007. Secrets of the pulse. [Google Scholar]
- 7.Venkat Shivudu A critical review on ayurvedic diagnostic methods. 2015;6(2):134–149. [Google Scholar]
- 8.Dadhich N.K., Pooja S. A comprehensive knowledge on Nadi Pariksha. 2016;1(2):190–195. [Google Scholar]
- 9.Gaddam D.A. Survey on Nadi Pareeksha for early detection of several diseases & computational models using nadi patterns. Int J Comput Sci Inf Technol [Internet] 2015;6(4):3424–3425. www.ijcsit.com Available from: [Google Scholar]
- 10.Gouda D.H.P., Raju G., MB S. Sharangadhara's Nadi Pareeksha and its implications in ayurveda. J Ayurveda Integr Med Sci [Internet] 2016;1(3) http://www.jaims.in/index.php/jaims/article/view/66 Available from: [Google Scholar]
- 11.Shashirekha H.K., Sukumar B.S. An interpretation of Nadi Pariksha with reference to Kala. 2014;2 [Google Scholar]
- 12.Joshi R.R. Diagnostics using computational nadi patterns. Math Comput Model. 2005;41(1):33–47. [Google Scholar]
- 13.Prasad G.P., Bharati K., Swamy R.K. Some important aspects of nadipariksha from basavarajiyam. Anc Sci Life [Internet] 2004;24(1):27–29. http://www.ncbi.nlm.nih.gov/pubmed/22557147%5Cnhttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC3330914 Available from: [PMC free article] [PubMed] [Google Scholar]
- 14.Murthy K.R.S. Krishnadas Academy; Varanasi: 2007. Astanga Hridayam. [Google Scholar]
- 15.Shokawa T., Imazu M., Yamamoto H., Toyofuku M., Tasaki N., Okimoto T. Pulse wave velocity predicts cardiovascular mortality: findings from the Hawaii-Los Angeles-Hiroshima study. Circ J [Internet] 2005;69(3):259–264. doi: 10.1253/circj.69.259. http://www.ncbi.nlm.nih.gov/pubmed/15731528 Available from: [DOI] [PubMed] [Google Scholar]
- 16.Vlachopoulos C., Aznaouridis K., Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness. A systematic review and meta-analysis. J Am Coll Cardiol. Elsevier Inc. 2010;55(13):1318–1327. doi: 10.1016/j.jacc.2009.10.061. [DOI] [PubMed] [Google Scholar]
- 17.Laurent S., Cockcroft J., Van Bortel L., Boutouyrie P., Giannattasio C., Hayoz D. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27(21):2588–2605. doi: 10.1093/eurheartj/ehl254. [DOI] [PubMed] [Google Scholar]
- 18.Mancia G., Fagard R., Narkiewicz K., Redon J., Zanchetti A., Böhm M. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013;34(28):2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 19.Blacher J., Guerin A.P., Pannier B., Marchais S.J., Safar M.E., London G.M. Impact of aortic stiffness on survival in end-stage renal disease. Circulation [Internet] 1999;99(18):2434–2439. doi: 10.1161/01.cir.99.18.2434. http://www.ncbi.nlm.nih.gov/pubmed/10318666 Available from: [DOI] [PubMed] [Google Scholar]
- 20.Meaume S., Benetos A., Henry O.F., Rudnichi A., Safar M.E. Aortic pulse wave velocity predicts cardiovascular mortality in subjects >70 years of age. Arterioscler Thromb Vasc Biol. 2001;21(12):2046–2050. doi: 10.1161/hq1201.100226. [DOI] [PubMed] [Google Scholar]
- 21.Laurent S., Boutouyrie P., Asmar R., Gautier I., Laloux B., Guize L. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension (Dallas, Tex 1979) 2001;37(5):1236–1241. doi: 10.1161/01.hyp.37.5.1236. [DOI] [PubMed] [Google Scholar]
- 22.Constant I., Laude D., Murat I., Elghozi J.L. Pulse rate variability is not a surrogate for heart rate variability. Clin Sci (Lond) 1999;97(4):391–397. [PubMed] [Google Scholar]
- 23.Hayano J., Barros A.K., Kamiya A., Ohte N., Yasuma F. Assessment of pulse rate variability by the method of pulse frequency demodulation. Biomed Eng Online. 2005;4:62. doi: 10.1186/1475-925X-4-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mirza M., Lakshmi A.N.R. A comparative study of pulse rate variability and heart rate variability in healthy subjects. Int J Biomed Adv Res [Internet] 2012;3(8):640–644. http://www.ncbi.nlm.nih.gov/pubmed/22350367 Available from: [Google Scholar]
- 25.Joshi A., Chandran S., Jayaraman V.K., Kulkarni B.D. Arterial pulse system: modern methods for traditional Indian medicine. Conf Proc Annu Int Conf IEEE Eng Med Biol Soc IEEE Eng Med Biol Soc Annu Conf [Internet] 2007 Jan;2007:608–611. doi: 10.1109/IEMBS.2007.4352363. http://www.ncbi.nlm.nih.gov/pubmed/18002029 Available from: [DOI] [PubMed] [Google Scholar]
- 26.Joshi A.J., Chandran S., Jayaraman V.K., Kulkarni B.D. Arterial pulse rate variability analysis for diagnoses. 2008 19th Int Conf Pattern Recognit [Internet]. Ieee. 2008 Dec:1–4. http://ieeexplore.ieee.org/lpdocs/epic03/wrapper.htm?arnumber=4761757 Available from: [Google Scholar]
- 27.Zoungas S., Asmar R.P. Arterial stiffness and cardiovascular outcome. Clin Exp Pharmacol Physiol. 2007;34(7):647–651. doi: 10.1111/j.1440-1681.2007.04654.x. [DOI] [PubMed] [Google Scholar]
- 28.Avolio A.P., Butlin M., Walsh A. Arterial blood pressure measurement and pulse wave analysis–their role in enhancing cardiovascular assessment. Physiol Meas [Internet] 2010 Jan;31(1):R1–R47. doi: 10.1088/0967-3334/31/1/R01. http://www.ncbi.nlm.nih.gov/pubmed/19940350 Available from: [cited 2016 May 31] [DOI] [PubMed] [Google Scholar]
- 29.Boutouyrie P, Tropeano AI, Asmar R, Gautier I, Benetos A, Lacolley P, et al. Aortic stiffness is an independent predictor of primary coronary events in hypertensive patients: a longitudinal study. 2002;10–15. [DOI] [PubMed]
- 30.Gunarathne A., Patel J.V., Hughes E.A., Lip G.Y.H. Measurement of stiffness index by digital volume pulse analysis technique: clinical utility in cardiovascular disease risk stratification. Am J Hypertens [Internet] 2008 Aug;21(8):866–872. doi: 10.1038/ajh.2008.207. http://www.ncbi.nlm.nih.gov/pubmed/18551104 Available from: [cited 2016 May 31] [DOI] [PubMed] [Google Scholar]
- 31.Kumar P.V.G., Deshpande S., Joshi A., More P., Nagendra H.R. Association of arterial stiffness measured from Tridoshas with diabetes – a cross sectional study. 2016;2(6):218–223. [Google Scholar]
- 32.Laurent S., Cockcroft J., Van Bortel L., Boutouyrie P., Giannattasio C., Hayoz D. Abridged version of the expert consensus document on arterial stiffness. Artery Res. 2007;1(1):2–12. doi: 10.1093/eurheartj/ehl254. [DOI] [PubMed] [Google Scholar]
- 33.Butlin M., Qasem A., Battista F., Bozec E., McEniery C.M., Millet-Amaury E. Carotid-femoral pulse wave velocity assessment using novel cuff-based techniques: comparison with tonometric measurement. J Hypertens [Internet] 2013;31(11):2237–2243. doi: 10.1097/HJH.0b013e328363c789. http://www.ncbi.nlm.nih.gov/pubmed/24077246 Available from: [discussion 2243] [DOI] [PubMed] [Google Scholar]
- 34.Rajzer M.W., Wojciechowska W., Klocek M., Palka I., Brzozowska-Kiszka M.M., Kawecka-Jaszcz K. Comparison of aortic pulse wave velocity measured by three techniques: Complior, SphygmoCor and Arteriograph. J Hypertens. 2008;26(10):2001–2007. doi: 10.1097/HJH.0b013e32830a4a25. [DOI] [PubMed] [Google Scholar]
- 35.Salvi P. Springer; 2012. Pulse waves how vascular hemodynamics affects blood pressure [Internet]www.springer.com Available from: [Google Scholar]
- 36.Pereira T., Correia C., Cardoso J. Novel methods for pulse wave velocity measurement. J Med Biol Eng. 2015;35(5):555–565. doi: 10.1007/s40846-015-0086-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sugawara J., Tanaka H. Brachial-ankle pulse wave velocity : myths, misconceptions, realities. 2015;8566:106–113. doi: 10.1159/000430771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tseng Y., Lin Y., Hsu J. 2015. Association of brachial-ankle pulse wave velocity with atherosclerosis and presence of coronary artery disease in older patients; pp. 1369–1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sugawara J., Hayashi K., Tanaka H. Arterial path length estimation on brachial-ankle pulse wave velocity: validity of height-based formulas. J Hypertens [Internet] 2014;32(4) doi: 10.1097/HJH.0000000000000114. http://journals.lww.com/jhypertension/Fulltext/2014/04000/Arterial_path_length_estimation_on_brachial_ankle.25.aspx Available from: [DOI] [PubMed] [Google Scholar]
- 40.Yamashina A., Tomiyama H., Takeda K., Tsuda H., Arai T., Hirose K. Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens Res. 2002;25(3):359–364. doi: 10.1291/hypres.25.359. [DOI] [PubMed] [Google Scholar]
- 41.Wu N., Cai X., Ye K., Li Y., He M., Zhao W. Association between Brachial-Ankle pulse wave velocity and cardiac autonomic neuropathy in type 2 diabetes. Diabetol Metab Syndr [Internet] 2014;6(1):82. doi: 10.1186/1758-5996-6-82. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4132900&tool=pmcentrez&rendertype=abstract Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Katakami N., Osonoi T., Takahara M., Saitou M., Matsuoka T.A., Yamasaki Y. Clinical utility of brachial-ankle pulse wave velocity in the prediction of cardiovascular events in diabetic patients. Cardiovasc Diabetol [Internet] 2014;13(1):128. doi: 10.1186/s12933-014-0128-5. http://www.ncbi.nlm.nih.gov/pubmed/25186287 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wu H.T., Lee C.H., Liu A.B., Chung W.S., Tang C.J., Sun C.K. Arterial stiffness using radial arterial waveforms measured at the wrist as an indicator of diabetic control in the elderly. IEEE Trans Biomed Eng. 2011;58(2):243–252. doi: 10.1109/TBME.2010.2084087. [DOI] [PubMed] [Google Scholar]
- 44.Millasseau S.C., Guigui F.G., Kelly R.P., Prasad K., Cockcroft J.R., Ritter J.M. Noninvasive assessment of the digital volume pulse. Comparison with the peripheral pressure pulse. Hypertension. 2000;36(6):952–956. doi: 10.1161/01.hyp.36.6.952. [DOI] [PubMed] [Google Scholar]
- 45.Joshi A., Kulkarni A., Chandran S., Jayaraman V.K., Kulkarni B.D. Nadi Tarangini: a pulse based diagnostic system. Conf Proc IEEE Eng Med Biol Soc [Internet] 2007 Jan;2007:2207–2210. doi: 10.1109/IEMBS.2007.4352762. http://www.ncbi.nlm.nih.gov/pubmed/18002428 Available from: [DOI] [PubMed] [Google Scholar]
- 46.Abhinav Sareen M., Kumar M., Anand S., Salhan A., Santhosh J. Nadi Yantra: a robust system design to capture the signals from the radial artery for non-invasive diagnosis. 2nd Int Conf Bioinforma Biomed Eng iCBBE 2008. 2008;2009(November):1387–1390. [Google Scholar]
- 47.Roopini N. Design & development of a system for Nadi Pariksha. 2015;4(6):465–470. [Google Scholar]
- 48.Shoji T., Emoto M., Shinohara K., Kakiya R., Tsujimoto Y., Kishimoto H. Diabetes mellitus, aortic stiffness, and cardiovascular mortality in end-stage renal disease. J Am Soc Nephrol [Internet] 2001;12(10):2117–2224. doi: 10.1681/ASN.V12102117. http://www.ncbi.nlm.nih.gov/pubmed/11562410 Available from: [DOI] [PubMed] [Google Scholar]
- 49.Cruickshank K., Riste L., Anderson S.G., Wright J.S., Dunn G., Gosling R.G. Aortic pulse-wave velocity and its relationship to mortality in diabetes and glucose intolerance: an integrated index of vascular function? Circulation. 2002;106(16):2085–2090. doi: 10.1161/01.cir.0000033824.02722.f7. [DOI] [PubMed] [Google Scholar]
- 50.Laurent S., Katsahian S., Fassot C., Tropeano A.I., Gautier I., Laloux B. Aortic stiffness is an independent predictor of fatal stroke in essential hypertension. Stroke. 2003;34(5):1203–1206. doi: 10.1161/01.STR.0000065428.03209.64. [DOI] [PubMed] [Google Scholar]
- 51.Sutton-Tyrrell K., Najjar S.S., Boudreau R.M., Venkitachalam L., Kupelian V., Simonsick E.M. Elevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adults. Circulation. 2005;111(25):3384–3390. doi: 10.1161/CIRCULATIONAHA.104.483628. [DOI] [PubMed] [Google Scholar]
- 52.Hansen T.W., Staessen J.A., Torp-Pedersen C., Rasmussen S., Thijs L., Ibsen H. Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation. 2006;113(5):664–670. doi: 10.1161/CIRCULATIONAHA.105.579342. [DOI] [PubMed] [Google Scholar]
- 53.Mattace-Raso F.U.S., Van Der Cammen T.J.M., Hofman A., Van Popele N.M., Bos M.L., Schalekamp M.A.D.H. Arterial stiffness and risk of coronary heart disease and stroke: the Rotterdam Study. Circulation. 2006;113(5):657–663. doi: 10.1161/CIRCULATIONAHA.105.555235. [DOI] [PubMed] [Google Scholar]
- 54.Stefanadis C., Dernellis J., Tsiamis E., Stratos C., Diamantopoulos L., Michaelides A. Aortic stiffness as a risk factor for recurrent acute coronary events in patients with ischaemic heart disease. Eur Heart J [Internet] 2000;21(21):390–396. doi: 10.1053/euhj.1999.1756. http://www.idealibrary.com Available from: [DOI] [PubMed] [Google Scholar]
- 55.Blacher J., Pannier B., Guerin A.P., Marchais S.J., Safar M.E., London G.M. Carotid arterial stiffness as a predictor of cardiovascular and all-cause mortality in end-stage renal disease. Hypertension [Internet] 1998;32(3):570–574. doi: 10.1161/01.hyp.32.3.570. http://hyper.ahajournals.org/cgi/doi/10.1161/01.HYP.32.3.570 Available from: [DOI] [PubMed] [Google Scholar]
- 56.Barenbrock M., Kosch M., Jöster E., Kisters K., Rahn K.-H., Hausberg M. Reduced arterial distensibility is a predictor of cardiovascular disease in patients after renal transplantation. J Hypertens [Internet] 2002;20(1) doi: 10.1097/00004872-200201000-00012. http://journals.lww.com/jhypertension/Fulltext/2002/01000/Reduced_arterial_distensibility_is_a_predictor_of.12.aspx Available from: [DOI] [PubMed] [Google Scholar]